Abstract
Introduction
Apnea testing remains essential for the clinical evaluation of brain death determination. In patients who test positive for SARS-CoV-2, disconnecting the patient from the ventilator and introducing high flow oxygen into the endotracheal tube increases the risk for aerosolization of airway secretions and exposure of the examiner.
Methods
Case report of a patient with an intracerebral hemorrhage that evolved to significant cerebral edema and herniation, who underwent apnea test using a method involving a t-piece and an HME filter.
Results
Patient successfully pronounced brain dead using a safe method to minimize exposure to SARS-CoV-2.
Conclusion
At a time where healthcare workers are at high risk of exposure to COVID-19, the above described method is a safe process for apnea testing in declaration of brain death.
Key Words: Brain death, Apnea test, Corona virus
Introduction
Apnea testing remains essential for the clinical evaluation of brain death determination.1 In patients who test positive for SARS-CoV-2 (COVID-19), disconnecting the patient from the ventilator and introducing high flow oxygen into the endotracheal tube increases the risk for aerosolization of airway secretions and exposure of the examiner.
Case description
Patient was a 57-year-old male admitted with a right frontoparietal intracerebral hemorrhage and diagnosed with COVID-19 at the time of admission. Patient developed refractory cerebral edema and associated intracranial hypertension nonresponsive to best medical therapy. Patient proceeded to herniate and met clinical criteria for brain death. Clinical determination of brain death posed a challenge due to risk of exposure to multiple providers. We determined a safe approach to apnea testing this patient in collaboration with respiratory therapy.
The process
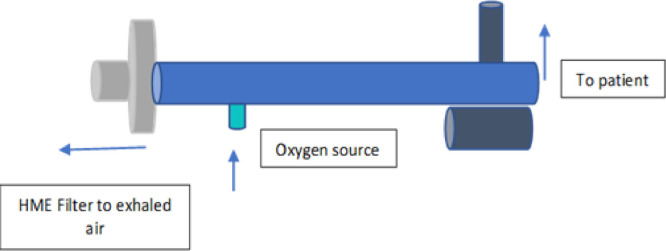
The patient was preoxygenated for 10 min with 100% FiO2 to a PaO2>200 mmHg. The endotracheal tube (ETT) was clamped close with a surgical clamp and then disconnected from the ventilator. One end of the T piece device was connected to the ETT and the other end was attached to a heat and moisture exchanger filter (HME). These filters are known to be efficacious against most respiratory viruses, including H1N1.2 Oxygen was delivered with a flow of 6L/min into the T piece through an accessory port of the T piece (Fig.1, Picture 1 and 2 ). The goal of the HME filter was to trap returning air which could be contaminated and prevent air escape through any other route. Apnea testing was performed as per the American Academy of Neurology guidelines for brain death determination. There were no episodes of desaturation noted throughout the procedure. After the test was completed, the ETT was again clamped, the T-piece disconnected, and the patient reconnected to the ventilator. Brain death was successfully determined per guidelines with appropriate rise in CO2 by 20 points within 8 min.
Fig.1.
Depiction of T-piece with HME filter. Arrows show flow of air.
Picture 1.
T-piece assembled before connection to patient.
Picture 2.
T-piece connected to patient: white arrow shows HME filter; white arrowhead shows oxygen port; green arrow shows connection to the endotracheal tube.
Conclusion
At a time where healthcare workers are at high risk of exposure to COVID-19, the above described method is a safe process for apnea testing in declaration of brain death. Recent literature has described a likely increase incidence of cerebrovascular events in COVID-19 patients. Guideline based practice remains the goal of care even in the midst of this pandemic.
References
- 1.Wijdicks Varelas P, Gronseth G. Evidence-based guideline update: determining brain death in adults. Neurology. 2010;74:1911–1918. doi: 10.1212/WNL.0b013e3181e242a8. [DOI] [PubMed] [Google Scholar]
- 2.Heuer J, Crozier T, Howard G. Can breathing Circuit filters help prevent the spread of influenza A(H1N1) virus from intubated patient. GMS Hyg Infect Control. 2013;8(1) doi: 10.3205/dgkh000209. [DOI] [PMC free article] [PubMed] [Google Scholar]