Highlights
-
•
What is the primary question addressed by this study?—We performed a study to measure the change of psychological symptoms during quarantine or self-isolation for COVID-19 in a sample of Italian caregivers of people with dementia, and to investigate whether resilience levels are associated with psychological changes in the sample.
-
•
What is the main finding of this study?—Caregivers of people with dementia showed higher depression levels during the quarantine then before. Although caregivers with high resilience showed lower anxiety and depression scores at baseline, they significantly increased their anxiety levels during lockdown, while caregivers with low resilience did not.
-
•
What is the meaning of the finding?—COVID-19 pandemic and lockdown produced psychological consequences in caregivers of people with dementia; surprisingly, high levels of resilience had a negative effect on anxiety levels during the lockdown.
Key Words: Caregiver, COVID-19, dementia, depression, anxiety, resilience, burden
Abstract
Background
Caregivers of people with dementia (pwD) are at risk of depression, anxiety, and burden. COVID-19 pandemic and government-imposed lockdown as a preventive measure might increase psychological symptoms in caregivers. The authors performed a study to measure the change of psychological symptoms during quarantine or self-isolation for COVID-19 in a sample of Italian caregivers of pwD, and to investigate if the resilience is associated with psychological changes in the sample.
Methods
Eighty-four caregivers of pwD completed an online survey including questionnaires assessing depressive symptomatology and anxiety before and during the lockdown, caregiver burden and levels of resilience.
Results
The multivariate analysis of variance revealed an effect of time (before and during the lockdown) in the whole group on depression scores; a significant interaction between time and resilience was found on anxiety scores, revealing that caregivers with high resilience showed a more significant increase of anxiety levels during lockdown than caregivers with low resilience. Moreover, the regression analysis revealed that caregiver burden was associated negatively with resilience scores, and positively with higher functional dependence.
Conclusion
COVID-19 pandemic and the lockdown produced psychological consequences in caregivers of pwD, with an increase of levels of depression. Moreover, high resilience had a negative effect on anxiety levels and no effect on depressive symptomatology during the lockdown; moreover, it was associated with lower levels of caregiver burden. All caregivers, even those with high resilience levels, should be addressed to psychological interventions to reduce levels of depression, anxiety and caregiver burden.
INTRODUCTION
In late 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detected as the causative agent of COVID-19, a respiratory disease that was first noticed in China and quickly spread out in Europe and in at least 216 countries, areas or territories throughout the world.1Several studies revealed that premorbid conditions and/or older age were risk factors for COVID-19 mortality, and the pandemic was called the “geriatric emergency of 2020”.2 Among older people, people with dementia (pwD) may be at higher risk of fatal outcomes due to COVID-19 outbreak, because of the vulnerability due to their disease and to the indirect effect of pandemic on social and medical support.3 Given the extreme uncertainty of the pandemic, informal caregivers of pwD (relatives or friends who are not paid for their assistance) may face new challenges during this period: in fact, caregiving activities may be more struggling because of lockdowns imposed by governments, social distancing, difficulties in fulfill the basic needs of pwD and accessing to the National Healthcare System or private physicians during the COVID-19 pandemic. Providing care for older frail adults, and in particular for pwD, is already a stressful experience that may have a negative impact on psychological well-being;4 in fact, 34% of caregivers report depressive symptomatology and the 43.6% report high levels of anxiety.5 However, in some caregivers, psychological distress may be buffered by high levels of resilience, a multidimensional construct that reflects the ability to resist or adapt to physical and psychological challenges of caregiving.6 , 7
In a pandemic characterized by extreme uncertainty, it is possible that the lockdown may have exacerbated psychological reactions such as anxiety and depression in caregivers of pwD. Taking into account that resilience is the ability to mentally or emotionally cope with stressors,5 caregivers with a low level of resilience should be more prone to an increase of psychological symptoms. Therefore, in the present study, we evaluated possible changes in depression, anxiety in caregivers of pwD during the Italian lockdown due to COVID-19 pandemic; moreover, we explored if during lockdown the levels of depression and anxiety increased more in caregivers of pwD with a low level of resilience than in ones with a high level of resilience.
MATERIALS AND METHODS
Participants
An online survey was shared through a link on online groups dedicated to dementia patients and/or caregivers, online newspapers, associations of caregivers of pwD (i.e., caregivers of people with Alzheimer's disease, vascular dementia, frontotemporal dementia). The study was approved by the local ethical committee. The online survey started with an informed consent form. Data were collected between April 21st and May 3rd during the Italian lockdown due to Covid-19 pandemic.
Psychological Evaluation
The online survey included 1) a sociodemographic questionnaire aimed at collecting demographic information about respondents and clinical information about their relatives with dementia (i.e., type of diagnosis, level of functional dependence, disease duration), the relationship with the pwD, their caregiving habits and their lifestyle changes during the lockdown. 2) The Italian version of Hospital Anxiety and Depression Scale (HADS)8 to evaluate levels of anxiety and depressive symptomatology. The HADS scale provides two indexes to evaluate anxiety (HADS-A) and depression (HADS-D). Higher scores are indicative of higher anxiety and depression. For the purposes of this study, participants were asked to complete twice the questionnaire in order to describe how they felt immediately before the lockdown, and during the lockdown. 3) The Italian version of the Resilience Scale for Adults (RSA),9 a self-administered questionnaire that evaluates levels of resilience. The RSA provides a total score and six subscores (perception of self, planned future, social competence, structured style, family cohesion, social resources) and higher scores indicate higher levels of resilience. 4) The Italian version of Caregiver Burden Inventory (CBI),10 a multidimensional scale that evaluates multiple aspects of caregiver burden (time-dependence, developmental, physical, social, and emotional burden). Participants were asked to complete the questionnaire by taking into account how they felt during the lockdown. Higher scores are indicative of higher burden.
Statistical Analyses
Statistical analyses were performed by using SPSS Statistics version 25.0. Means and standard deviations, or percentage were used to describe continuous or categorical variables, when appropriate. A multivariate analysis of variance for repeated measures was used to evaluate 1) possible changes of depression and anxiety levels over time (before and during the lockdown) on the whole sample; 2) possible differences on levels of depression and anxiety before and during the lockdown between caregivers with high and low resilience levels. Dependent variables were HADS-D and HADS-A scores before the lockdown (time point 1) and during the lockdown (time point 2); the independent variable was the RSA level (high and low resilience). Since no cutoff was provided for the RSA scale, RSA dichotomous level was computed by calculating the median score of RSA on the whole sample; caregivers who scored under or above the median score were sorted in the low resilience or high resilience group, respectively. Partial eta square (partial η2) was calculated and used as a measure of effect size; the interpretation of the magnitudes of effect sizes was based on the following cutoffs:11 0.01, 0.06, 0.14 for small, medium, and large effect sizes, respectively. Moreover, univariate analysis of variance was performed to evaluate the effect of each independent variable on the abovementioned dependent variables.
To evaluate the association between caregiver burden during the lockdown and sociodemographic and psychological variables, multiple regression analysis (stepwise method) was performed. The standardized coefficients (beta) were calculated. CBI score was entered as dependent variable, while delta scores of HADS-D and HADS-A (during lockdown score minus prelockdown score), RSA scores, days in lockdown, years of education, employment status before the lockdown, change in working modality, type of diagnosis of dementia of pwD, level of functional dependence, disease duration of pwD, and time of care were entered as independent variables.
Moreover, an analysis of variance was performed to verify possible differences in HADS-A, HADS-D, CBI, and RSA scores between caregivers of people with Alzheimer's disease and non-Alzheimer's dementia.
To reduce the possibility of type I error, each critical p value for multiple comparison was adjusted by using the Benjamini-Hochberg procedure,12 with a false discovery rate of 0.05.
RESULTS
Eighty-four participants (71 women, 13 men) agreed to participate in the study and completed the online survey. Mean age of the sample was 48.7 years old, and mean years of education were 13.8. As regards the working status, the 54.8% of the sample was employed immediately before the lockdown; among the workers, after the lockdown, the 59.5% of the sample stopped working, the 17.9% switched to smart-working, the 2.4% reduced their working time, and the 20.2% worked in the same modality as before. All sociodemographic and clinical characteristics of the sample are depicted in Tables 1 and 2 .
TABLE 1.
Sociodemographic Characteristics of Caregivers (N = 84) and People With Dementia
| Caregivers | pwD | |
|---|---|---|
| Sex (F%) | 84.5% | 72.6% |
| Age, mean (SD) | 48.7 (11.7) | 78.5 (10.1) |
| Years of education, mean (SD) | 13.8 (3.1) | - |
| Years of disease duration, mean (SD) | - | 5.3 (3.6) |
| Diagnosis (%) | ||
| Alzheimer's disease | - | 56% |
| Vascular dementia | - | 31% |
| Frontotemporal dementia | - | 10.7% |
| Lewy body dementia | - | 2.4% |
| Level of functional dependence (%) | ||
| High | 34.5% | |
| Medium | 45.2% | |
| Low | - | 20.2% |
| Employment status (%) | ||
| Employed | 54.8% | - |
| Not employed | 45.2% | - |
| Kinship (%) | ||
| Children | 72.6% | - |
| Spouses | 11.9% | - |
| Grandchildren | 8.3% | - |
| Other | 6.0% | - |
| Time of care, mean (SD) | 12.8 (8.1) | - |
| Place of residence (%) | ||
| In the same house with the pwD | 75% | |
| In the same city of residence of the pwD | 16.7% | |
| In another city with respect to the pwD's residence | 8.3% | |
| Secondary caregivers | ||
| None | 26.2% | |
| Other relatives | 51.2% | |
| Paid carers | 22.6% |
pwD: people with dementia; F%: percentage of female participants; SD: standard deviation.
TABLE 2.
Psychological Assessment of Caregivers Before and During the Lockdown
| Whole Sample (N = 84) | Caregivers With High Resilience (N = 43) | Caregivers With Low Resilience (N = 41) | |
|---|---|---|---|
| HADS-A prelockdown | 10.06±3.79 | 8.88±3.89 | 11.29±3.30 |
| HADS-A during lockdown | 10.29±2.05 | 9.98±2.12 | 10.61±1.94 |
| HADS-D prelockdown | 9.64±3.84 | 8.30±3.63 | 11.05±3.57 |
| HADS-D during lockdown | 10.29±2.05 | 10.49±1.71 | 11.80±1.78 |
| CBI total score | 47.2±18.2 | 41.60±16.98 | 53.07±17.76 |
| RSA total score | 4.40±0.89 | 5.09±0.59 | 3.67±0.45 |
The values are expressed in mean ± standard deviation. HADS-A: anxiety subscale of Hospital Anxiety and Depression Scale; HADS-D: depression subscale of Hospital Anxiety and Depression Scale; CBI: Caregiver Burden Inventory; RSA: Resilience Scale for Adults.
Neither the caregivers nor the pwD of our sample were tested positive for COVID-19 nor they showed symptoms related to COVID-19. In order to prevent SARS-CoV-2 infection, 56% of the sample reported using disposable gloves, the 72.3% wore protective masks, the 73.8% increased the frequency of housecleaning, and the 60.7% engaged in social distancing. When asked about how much the pwD was aware of the pandemic situation, the 79.8% of the caregivers reported that his or her relative with dementia was unaware of the situation. According to their caregivers, the SARS-CoV-2 outbreak and the lockdown had an impact on the lifestyle of 50% of pwD. Moreover, when asked about the dangerousness of getting COVID-19, the 75% of the caregiver sample felt that the COVID-19 pandemic was a threat for their own health, whereas the 82.1% of the sample reported that it was a health threat for pwD.
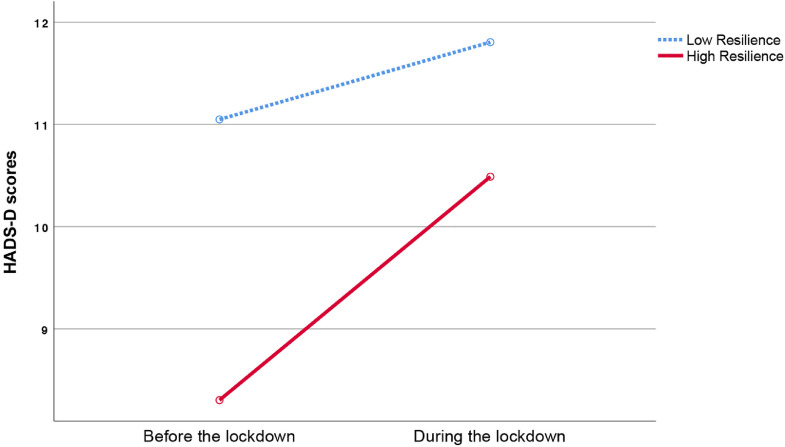
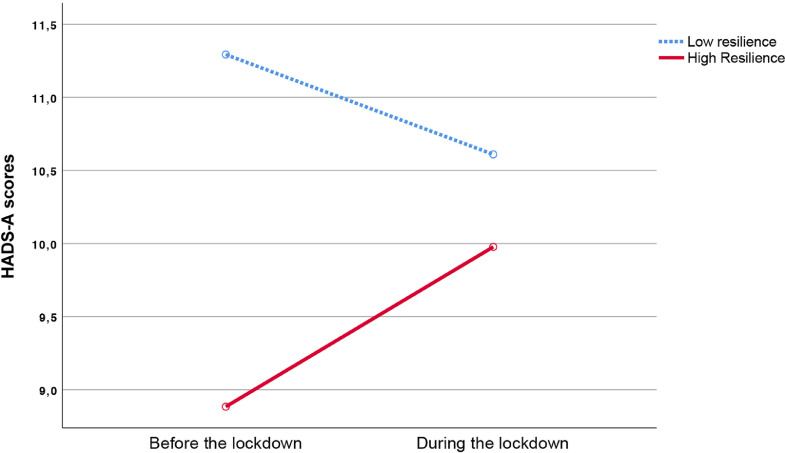
After the correction for multiple comparisons, the repeated measures multivariate analysis of variance revealed a significant: 1) main effect of resilience level between subjects (Λ = 0.795, F(2,81) = 10.445; p <0.001, partial η2 = 0.969), 2) main effect of time (Λ = 0.865, F(2,81) = 6.297, p = 0.003, partial η2 = 0.135), and 3) interaction between time and resilience (Λ = 0.910, F(2,81) = 4.013, p = 0.022, partial η2 = 0.090). The univariate analyses (Figs. 1 and 2 ) revealed a significant main effect of time on HADS-D scores (F(1,82) = 12.646, df = 1; p = 0.001, partial η2 = 0.134), but not on HADS-A scores (F(1,82) = 0.371, p = 0.544, partial η2 = 0.005), and a significant interaction between time and resilience on HADS-A scores (F(1,82) = 6.955, p = 0.010, partial η2 = 0.078), but not on HADS-D scores (F(1,82) = 2.987, p = 0.088, partial η2 = 0.035). As for the between-subjects analysis, the results revealed a significant effect of resilience levels on HADS-D (F(1,82) = 19.644, p <0.001, partial η2 = 0.193) and HADS-A (F(1,82) = 7.811, p = 0.006, partial η2 = 0.087) scores.
FIGURE 1.
Plot describing the interaction effect of resilience levels (high and low resilience) and time (before and during the lockdown) on depression subscale of the Hospital Anxiety and Depression Scale (HADS-D) scores in a sample of caregivers.
FIGURE 2.
Plot describing the interaction effect of resilience levels (high and low resilience) and time (before and during the lockdown) on anxiety subscale of the Hospital Anxiety and Depression Scale (HADS-A) scores in a sample of caregivers.
The multiple regression analysis to evaluate the possible association between CBI scores and sociodemographic and psychological variables revealed that higher CBI scores were negatively associated with RSA scores (β = -.398, t(81) = 3.644, p = 0.001) and delta score of HADS-A (β = -.280, t(81) = -2.687, p = 0.009) and positively with higher functional dependence (β = 0.340, t(81) = 3.359, p = 0.001).
Finally, a between-group analysis was performed on caregivers of people with Alzheimer's disease and non-Alzheimer's dementia and no differences were found on levels of depression and anxiety (both before and during the lockdown), resilience and caregiver burden (see Table 3 ).
TABLE 3.
Comparisons on Psychological Variables Between Caregivers of Patients With Alzheimer Disease and Non-Alzheimer Dementia
| Caregivers of People With Alzheimer Disease (N = 48) | Caregivers of People with Non-Alzheimer Dementia (N = 36) | F | p | |
|---|---|---|---|---|
| HADS-A prelockdown | 9.5 (3.45) | 10.8 (4.12) | 2.488 | 0.119 |
| HADS-A during lockdown | 10.9 (1.71) | 11.44 (2.0) | .084 | 0.772 |
| HADS-D prelockdown | 9.21 (3.8) | 10.22 (3.85) | 1.445 | 0.233 |
| HADS-D during lockdown | 10.23 (2.16) | 10.36 (1.91) | 1.817 | 0.181 |
| CBI total burden | 44.31 (15.9) | 51.06 (20.38) | 2.888 | 0.093 |
| RSA total | 4.48 (.78) | 4.29 (1.0) | 0.955 | 0.331 |
Degrees of freedom (df) = 1,82 in all models. F: F statistics ANOVA; p: probability value; HADS-A: anxiety subscale of Hospital Anxiety and Depression Scale; HADS-D: depression subscale of Hospital Anxiety and Depression Scale; CBI: Caregiver Burden Inventory; RSA: Resilience Scale for Adults. p values <0.05 are considered statistically significant.
DISCUSSION
The present study aimed at investigating levels of depressive symptomatology, anxiety, resilience, and caregiver burden in a sample of Italian dementia caregivers during the 2020 lockdown due to COVID-19 pandemic. First, when we analyzed the whole group of caregivers, we found a significant influence of time, with a medium effect size, on the severity of depressive symptoms rather than anxiety due to lockdown. Our results suggested that these psychological changes are associated with the introduction of the restrictions applied by the Government during the COVID-19 pandemic, such as social distancing and limitations in individual mobility and social activities. These restrictions may have had negative consequences on the possibility of being psychologically and emotively supported by others; low social support is associated with higher depression in caregivers, as found in several studies.13 , 14 First reports on immediate psychological responses in Italy during the lockdown revealed an increase of levels of depression and anxiety in general population.15 Our study confirmed an increase of depressive symptomatology, but not anxiety, during the lockdown. However, the divergent results on anxiety might be due to the different study sample: we focused on caregivers of pwD, whereas Mazza et al. focused on general population.
Moving on the comparisons between caregivers with high and low resilience levels, we found a large effect size of resilience on the severity of depression and anxiety in caregivers; in fact, caregivers with high resilience reported lower levels of depression and anxiety before the lockdown when compared with caregivers with low resilience. Surprisingly, we found that caregivers with high resilience reported a significant increase of levels of anxiety during the lockdown, whereas in caregivers with low resilience no significant increase of anxiety levels was found, with a medium effect size of the time × resilience interaction. Although high resilience is considered a protective factor against depression and anxiety in caregivers,16 these findings may suggest that resilience might not have a protective effect on caregivers’ psychological status during nonordinary global events, like a pandemic, and that these events may nullify the advantages of having high resilience (i.e., showing lower levels of anxious symptomatology). Our results highlight the need of developing specific programs for caregivers of pwD, even in those with high resilience, aimed at acquiring coping strategies and life skills. Moreover, since loneliness and social isolation are common features of caregiving,17 support groups and/or psychological interventions via the internet should be implemented to reduce depression and anxiety levels, especially during emergencies that affect the whole population, as in the case of COVID-19 pandemic.
Moving on results on caregiver burden, we found that lower levels of resilience and a higher functional dependence of pwD predicted higher levels of caregiver burden during the lockdown. Our results are in line with a previous study16 suggesting that resilience may be a protective factor against caregiver burden even in case of global emergencies, like the COVID-19 pandemic. On the contrary, unlike previous studies that failed to find an association between caregiver burden and functional dependency of caretakers,16 , 18 , 19 we found a significant and positive relationship. The divergence between results may be due to methodological differences in study design and/or scales to evaluate activities of daily living, or to the psychological reaction caused by the lockdown: in fact, caregivers of pwD with higher dependence on their activities of daily living may have had more difficulties in carrying on their care routine and be more psychologically and physically stressed due to the restrictions imposed by governments.
Lastly, our data offered no evidence that the diagnostic type of dementia of the patients influence levels of psychological distress and burden in caregivers, both before and during the lockdown. Previous comparative studies provided inconsistent results,20, 21, 22 probably due to different study designs and to the use of different scales to evaluate burden, depression, and anxiety, so further research is needed to further explore this topic. However, in our study we found that during the lockdown due to COVID-19 pandemic all caregivers of pwD reported the same psychological consequences, regardless of the type of diagnosis of dementia of their carers.
Our study is not exempt from limitations. First, ours is not a longitudinal study since we assessed levels of anxiety and depression by asking participants, during the lockdown, how they felt both during and before the lockdown. This may have caused a possible recall bias. However, the recall bias is more likely to occur when the time interval between two or more events is high;23 in our study, we asked to report how participants felt just before the lockdown, in order to limit the presence of the recall bias. Moreover, since participants were not cognitively assessed by means of specific screening tools, nor they completed a personality assessment, they may have underestimated or overestimated their symptoms before and during the lockdown. Finally, participants participated on a voluntary basis, so the sample may be not representative of the population.
Taken together, our results show that the COVID-19 pandemic and the lockdown as restrictive measure against COVID-19 produced psychological changes in caregivers of pwD, with an increase of levels of depression rather than of anxiety. Furthermore, we found that, even if high resilience in caregivers of pwD was associated with lower levels of caregiver burden, it had a negative effect on levels of anxiety during the lockdown, and that the magnitude of abovementioned effect sizes was medium to large, corroborating the clinical meaningfulness of our results. For these reasons all caregivers—not only those with low levels of resilience, and regardless of the clinical diagnosis of the caretaker—should be addressed to online psychological and educational programs to reduce their depressive symptomatology, anxiety, and burden levels.
AUTHORS’ CONTRIBUTIONS
MA contributed to the conception of the work, carried out the statistical analysis, and interpretation of the data for the work and wrote the draft; GS contributed to the conception of the work, interpretation of the data for the work, and wrote the draft.
Acknowledgments
DISCLOSURE
The authors have no disclosures to report.
The authors received no specific funding for this work.
References
- 1.World Health Organization. Coronavirus Disease (COVID-19) Pandemic. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed September 11, 2020.
- 2.Bonanad C, García-Blas S, Tarazona-Santabalbina FJ. Coronavirus: the geriatric emergency of 2020. Joint document of the Section on Geriatric Cardiology of the Spanish Society of Cardiology and the Spanish Society of Geriatrics and Gerontology. Rev Esp Cardiol (Engl Ed) 2020;73:569–576. doi: 10.1016/j.rec.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown EE, Kumar S, Rajji TK. Anticipating and mitigating the impact of the COVID-19 pandemic on Alzheimer's disease and related dementias. Am J Geriatr Psychiatry. 2020;28:712–721. doi: 10.1016/j.jagp.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 5.Sallim AB, Sayampanathan AA, Cuttilan A. Prevalence of mental health disorders among caregivers of patients with Alzheimer disease. J Am Med Dir Assoc. 2015;16:1034–1041. doi: 10.1016/j.jamda.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Herrman H, Stewart DE, Diaz-Granados N. What is resilience. Can J Psychiatry. 2011;56:258–265. doi: 10.1177/070674371105600504. [DOI] [PubMed] [Google Scholar]
- 7.Teahan Á, Lafferty A, McAuliffe E. Resilience in family caregiving for people with dementia: a systematic review. Int J Geriatr Psychiatry. 2018;33:1582–1595. doi: 10.1002/gps.4972. [DOI] [PubMed] [Google Scholar]
- 8.Costantini M, Musso M, Viterbori P. Detecting psychological distress in cancer patients: validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer. 1999;7:121–127. doi: 10.1007/s005200050241. [DOI] [PubMed] [Google Scholar]
- 9.Capanna C, Stratta P, Hjemdal O. The Italian validation study of the Resilience Scale for Adults (RSA) Appl. Psychol. Bull. 2015;63:16–24. [Google Scholar]
- 10.Marvardi M, Mattioli P, Spazzafumo L. The caregiver burden inventory in evaluating the burden of caregivers of elderly demented patients: results from a multicenter study. Aging Clin Exp Res. 2005;17:46–53. doi: 10.1007/BF03337720. [DOI] [PubMed] [Google Scholar]
- 11.Cohen J. 2nd ed. Academic Press; New York: 1988. Statistical Power Analysis of the Behavioral Sciences. [Google Scholar]
- 12.Benjamini Y, Hochberg Y. Controlling for false discovery rate: a practical and powerful approach to multiple testing. J. Royal Stat. Soc. Ser B. 1995;57:289–300. [Google Scholar]
- 13.Zhong Y, Wang J, Nicholas S. Social support and depressive symptoms among family caregivers of older people with disabilities in four provinces of urban China: the mediating role of caregiver burden. BMC Geriatr. 2020;20:3. doi: 10.1186/s12877-019-1403-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thielemann P, Conner N. Social support as a mediator of depression in caregivers of patients with end-stage disease. J Hosp Palliat Nurs. 2009;11:82–90. [Google Scholar]
- 15.Mazza C, Ricci E, Biondi S. A nationwide survey of psychological distress among Italian people during the. Int J Environ Res Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dias R, Simões-Neto JP, Santos RL. Caregivers’ resilience is independent from the clinical symptoms of dementia. Arq Neuropsiquiatr. 2016;74:967–973. doi: 10.1590/0004-282X20160162. [DOI] [PubMed] [Google Scholar]
- 17.Kovaleva M, Spangler S, Clevenger C. Chronic stress, social isolation, and perceived loneliness in dementia caregivers. J Psychosoc Nurs Ment Health Serv. 2018;56:36–43. doi: 10.3928/02793695-20180329-04. [DOI] [PubMed] [Google Scholar]
- 18.Cavalari KN, Hamamoto Filho PT, Caldeira SM. Functional independence of children with myelomeningocele: is it associated with the informal caregivers' burden? J Pediatr Nurs. 2017;36:232–235. doi: 10.1016/j.pedn.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Boutoleau-Bretonnière C, Vercelletto M, Volteau C. Zarit burden inventory and activities of daily living in the behavioral variant of frontotemporal dementia. Dement Geriatr Cogn Disord. 2008;25:272–277. doi: 10.1159/000117394. [DOI] [PubMed] [Google Scholar]
- 20.Yeager CA, Hyer LA, Hobbs B. Alzheimer's disease and vascular dementia: the complex relationship between diagnosis and caregiver burden. Issues Ment Health Nurs. 2010;31:376–384. doi: 10.3109/01612840903434589. [DOI] [PubMed] [Google Scholar]
- 21.Wong C, Merrilees J, Ketelle R. The experience of caregiving: differences between behavioral variant of frontotemporal dementia and Alzheimer disease. Am J Geriatr Psychiatry. 2012;20:724–728. doi: 10.1097/JGP.0b013e318233154d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D'Onofrio G, Sancarlo D, Addante F. Caregiver burden characterization in patients with Alzheimer's disease or vascular dementia. Int J Geriatr Psychiatry. 2015;30:891–899. doi: 10.1002/gps.4232. [DOI] [PubMed] [Google Scholar]
- 23.Hassan E. Recall bias can be a threat to retrospective and prospective research designs. Int J Epidemiol. 2005;3:1–7. [Google Scholar]