Abstract
Sexual violence (SV) is a public health concern for youth. Few longitudinal studies address how experiences of SV and co-occurring depression and anxiety symptoms in early young adulthood may contribute to poorer functioning in young adulthood. Using a sample of 2,416 youth aged 18 to 20 (Time 1), we assessed past year SV and co-occurring depression and anxiety symptoms. One year later, when youth were between the ages of 20 and 22 (Time 2), participants indicated their functioning in four domains: physical health and sleep quality, substance use consequences, psychological functioning, and social functioning. Using latent class analyses, we found six participant classes at Time 1 based on SV experiences and co-occurring depression and anxiety symptoms. Classes were variable by participants’ reported degree of SV experiences and co-occurring depression and anxiety symptomology. Longitudinal analyses indicated that youth in a class that experienced high levels of both SV and co-occurring depression and anxiety at Time 1 generally reported the poorest functioning in all key domains at Time 2. However, classes where participants reported greater depression and anxiety symptoms—most often in the presence of, but at times in the absence of, SV—were consistently associated with poorer functioning for physical health, psychological functioning, and social health. Classes where participants reported greater SV—in the presence of, but at times in the absence of, depression and anxiety symptoms—were associated with greater alcohol and marijuana consequences. Findings suggest prevention of SV, accessible counseling for those that have experienced SV, and screening to identify and intervene to address depression and anxiety may all be essential to help prevent poorer functioning in young adulthood.
Keywords: sexual violence, depression, anxiety, young adults
Sexual violence (SV) is unfortunately a common form of traumatic experience. An estimated 13% to 19% of women (Breiding et al., 2014; National Victim Center and Crime Victims Research and Treatment Center, 1992; Tjaden & Thoennes, 2006) and 1% to 12% of men (Black et al., 2011; Stemple & Meyer, 2014) in the United States report having experienced SV at least once in their lifetime. SV can include both physical aspects such as forced sex or touching, and verbal aspects (known also as sexual harassment) such as sexual name-calling or requests for sexual favors (World Health Organization [WHO], 2014). SV can begin as early as middle school for both boys and girls (Craig et al., 2009; Espelage et al., 2016; Nansel et al., 2001) with increasing prevalence as youth move through late adolescence (Chiodo et al., 2009; Young et al., 2009), with some studies indicating increased prevalence rates during young adulthood, specifically among females (Clodfelter et al., 2010).
The high prevalence rates of SV among adolescents and young adults is concerning for many reasons, including the significant problems in functioning that can follow experiences of SV (Campbell et al., 2009; Davis, Tucker, et al., 2019). For example, studies show that individuals who have experienced SV victimization are at risk for long-term behavioral health problems such as substance use consequences (e.g., driving after drinking), worsening psychological disorders (Bennice et al., 2003), problems with physical functioning, and poor relationship functioning (Eom et al., 2014; Jina & Thomas, 2013; Ullman et al., 2013). In fact, trauma in the form of SV has a larger effect on well-being than any other form of traumatic experience (Kelley et al., 2009). However, not all individuals who experience SV have these behavioral health problems, and studies that have attempted to understand who is most at risk have typically focused on demographic factors (Dworkin et al., 2017). This approach, while useful for understanding basic associations between trauma-related disorders and functioning (e.g., social support and physical health), does not allow for a broader lens for understanding heterogeneity in experiences of SV. Thus, in contrast to understanding experiences of SV from an individual or experience level, some research has used a more ecological lens to emphasize that experiences of SV occur within multiple domains of functioning and that not all experiences of SV are the same.
Research over the last several decades has demonstrated that individuals who experience SV are at heightened risk for co-occurring psychological problems. For example, in an early review, Campbell et al. (2009) reported that 13% to 49% of individuals with a history of SV victimization met criteria for an anxiety disorder and between 13% and 51% met criteria for depression. This suggests that heterogeneity in experiences of SV, depending on whether the individual is also experiencing comorbid depression/anxiety symptoms, may be important to consider in understanding the potential effects of SV on long-term behavioral health outcomes.
The associations between SV victimization and subsequent health risk behaviors can be understood from the broad theoretical framework of Problem Behavior Theory (Jessor & Jessor, 1977), which states that a youth’s social environment provides opportunities to learn risk and problem behaviors as well as normative expectations of problem behaviors (Jessor, 1992). One of the major caveats of Problem Behavior Theory is that health risks (e.g., mental health and behavioral health) compound and cluster together because they likely serve similar social or psychological developmental functions, especially when healthy coping behaviors are not available. Thus, youth who have experienced SV may have difficulty assessing or responding to increased risk (e.g., monitoring mental health symptoms), and these impaired responses may increase vulnerability to long-term problems across social, psychological, and physical health domains. For example, experiences of SV and co-occurring mood and anxiety symptoms have been associated with immediate and long-term behavioral health problems (Chiodo et al., 2012; Hatchel et al., 2018; Jina & Thomas, 2013; Zinzow et al., 2011). Social Stress Process Theory may also explain heterogeneity in experiences of SV and mental health. It posits that various forms of stress from one or more sources can accumulate over time and influence individual well-being (Pearlin et al., 1981). This theory distinguishes between the catalyst (i.e., stressors such as experiences of SV) and the individual’s maladaptive response to those stressors (i.e., distress such depression, anger, aggression, and risk-taking behaviors). In general, prior work suggests that stressors, in the absence of adequate resources (e.g., effective coping strategies and social supports), can proliferate and directly (or indirectly) harm one’s mental health (LeBlanc et al., 2015). More specifically, experiences of victimization can lead to both internalizing (e.g., depression and anxiety) and externalizing (e.g., deviant behavior and substance use) problems among adolescents and young adults (Margolin & Gordis, 2000; Sabri, 2012; Taylor & Weems, 2009). More severe forms of victimization, such as SV, have also been associated with a host of physical, mental, and social health problems (Dworkin et al., 2017; Sabri, 2012). However, much of the prior work has assessed effects of victimization typology on subsequent mental health problems versus understanding heterogeneity in co-occurring experiences of SV and mental health symptoms and their association with behavioral health.
This study examined heterogeneity in SV and co-occurring psychopathology (anxiety and depression) to investigate whether SV has a narrow (or broad) effect on domains of functioning in the absence (or presence) of co-occurring depression and anxiety symptoms. Our study moves the field forward by examining co-occurring symptoms of anxiety and depression with diverse experiences of SV (both assaults and harassment) during early young adulthood (age 18–20) on key domains of functioning 1 year later (age 20–22). We utilized latent class analysis (LCA) to examine the association of experiences of SV (both assaults and harassment) and co-occurring symptoms of depression and anxiety with functioning in four key domains: physical health and sleep quality (general health status, past month sleep quality), substance use consequences (frequency of past month alcohol and marijuana consequences), psychological functioning (posttraumatic stress disorder [PTSD] symptoms and satisfaction with life), and social functioning (quality of peer relationships and satisfaction with friends). Guided by the theoretical and empirical literature on this topic, we hypothesized that recent experiences of SV in early young adulthood would predict poorer functioning across all four domains 1 year later, with stronger effects among those who reported co-occurring depression and anxiety symptoms. Understanding how the co-occurrence of depression, anxiety, and experiences of SV uniquely contribute to subsequent functioning in these domains has implications for early intervention efforts.
Method
Participants and Procedures
This study utilized data from two waves of a large multi-wave study of adolescents and young adults. Participants were initially recruited in grades 6 and 7 (ages 11–13) in 2008 for an evaluation of a voluntary after-school alcohol and other drug prevention program, CHOICE, which was conducted in 16 middle schools in Southern California (D’Amico et al., 2012). Schools were selected across three school districts to obtain a racially/ethnically diverse sample. Details of the larger study, including participation and retention rates across all 10 waves, are published elsewhere (D’Amico et al., 2016, 2018; Dunbar et al., 2018). Briefly, students completed surveys about their alcohol and drug use behavior, attitudes, and beliefs in classrooms for the first five waves (Fall 2008, Spring 2009, Fall 2009, Spring 2010, and Spring 2011). As students moved from the 16 middle schools to over 200 high schools, annual surveys were conducted online. Retention rates ranged from 61% to 91% across all waves, with 90% retention from Wave 9 to 10 (waves analyzed in this article). If a participant did not complete a wave of data collection, they were still eligible to complete all subsequent waves. That is, they did not “dropout” of the study once they missed a survey wave; rather we fielded the full sample at every wave so that all participants had an opportunity to participate in each individual survey. Demographics (e.g., gender and race/ethnicity) and substance use (e.g., alcohol and marijuana) at the previous wave did not predict attrition at wave 10, similar to what we have found at earlier waves (D’Amico et al., 2016, 2018; Dunbar et al., 2018).
For this study, we utilized Wave 9 (herein Time 1) when participants were between the ages of 18 and 20 and Wave 10 (herein Time 2) when participants were between 20 and 22. To control for prior SV victimization and mental health symptoms, we adjusted for these measures at Wave 8. Note that only participants who were at least 18 years old were administered the survey items about SV. Accounting for missingness and skip patterns of variables needed for analyses, our final analytic sample was 2,416.
Measures
SV victimization at Time 1.
A modified version of the American Association of University Women’s Sexual Harassment Survey (Hill & Kearl, 2011) was used to assess experiences of SV victimization during the past year (Rinehart et al., 2017). Participants answered six items to assess unwanted verbal sexual harassment (i.e., sexual comments, sexual rumor spreading, and showing sexual pictures), and forced sexual contact/assault (i.e., touching in a sexual way, physically intimidating in a sexual way, and forcing to do something sexual). Participants were asked to consider how often in the past year these experiences happened to them (i.e., “Never,” “1 or 2 times,” “3 or 4 times,” “5 or 6 times,” and “7 or more times”). Items were coded as never experienced in the past year (0) and experienced in the past year (1). These items were assessed at Time 1 as predictors, and also 1 year prior (at Wave 8) to control for previous SV victimization.
Depression and anxiety symptoms at Time 1.
The Patient Health Questionnaire (PHQ-8; Kroenke et al., 2009) asked participants to indicate how often in the past 2 weeks they experienced eight symptoms of depression, such as “feeling, down, depressed or hopeless” and “little interest or pleasure in doing things.” Internal reliability of the scale was adequate in the sample (α = 0.91). The Generalized Anxiety Disorder scale (GAD-7; Spitzer et al., 2006) assessed seven symptoms of general anxiety experienced in the past 2 weeks, such as “feeling nervous, anxious, or on edge” and “not being able to stop or control worrying.” Internal reliability of the scale was adequate in the sample (α = 0.94). Items from the PHQ-8 and the GAD-7 were coded as not experienced in the past 2 weeks (0; “not at all”) and experienced in the past 2 weeks (1; “several days,” “more than half the days,” and “nearly every day”). These items were assessed at Time 1 as predictors, and also 1 year prior (at Wave 8) to control for previous mental health symptoms.
Key Domains of Functioning at Time 2.
The four domains of functioning were physical health and sleep quality, substance use consequences, psychological functioning, and social functioning. These domains were assessed at Time 2 as outcomes, and also 1 year prior (at Time 1) to control for previous functioning.
Physical health and sleep quality.
General health was assessed with one item from the Short-Form Health Survey asking participants: “In general, would you say your health is …” with response options ranging from 1 “excellent” to 5 “poor” (Ware et al., 1996). Higher scores on this measure indicated poorer health. Sleep quality was assessed with an item that asked participants “During the past month, how would you rate your overall sleep quality?” with response options ranging from 1 “very good” to 4 “very bad” (Buysse et al., 1989). Higher scores indicated poorer sleep quality.
Substance use consequences.
The substance use domain focused on past year consequences for alcohol and marijuana (Center for Behavioral Health Statistics and Quality, 2016). Nine alcohol consequences were selected from two measures used with adolescents and young adults: the Project ALERT Youth Survey (Tucker et al., 2003) and the Brief Young Adult Alcohol Consequences Questionnaire (Kahler et al., 2005). Example items are “You got into a fight or argument because of drinking alcohol” and “You passed out from drinking.” Ten marijuana consequences were selected from the Project ALERT Youth Survey (Ellickson et al., 2003; Tucker et al., 2003) and the Marijuana Consequences Questionnaire (Simons et al., 2012), such as “You missed school, work, or other obligations because of using marijuana” and “You had trouble remembering things because of using marijuana.” Responses of “1 time,” “2 times,” “3–5 times,” “6–9 times,” “10–19 times,” and “20 or more times” were coded as “yes” for the dichotomized version of each consequence item, and a response of “never” was coded as “no.” The nine dichotomous alcohol consequences items and the 10 dichotomous marijuana consequences items were summed to create alcohol and marijuana consequence composites, respectively, with higher scores indicating greater number of problems experienced. Internal reliability was adequate in the sample for each scale (Time 1: α = .91 for alcohol and α = 0.92 for marijuana; Time 2: α = 0.89 for alcohol and α = 0.91 for marijuana).
Psychological functioning.
PTSD symptoms were assessed with the Primary Care PTSD scale (PC-PTSD-5; Prins et al., 2016), which contains five items encompassing the five main symptoms resulting from traumatic events: nightmares, avoidance, hyperarousal, emotional numbing/detachment from others, and guilt/shame about the traumatic event(s). Internal reliability of the scale was adequate in the sample (Time 1: α = 0.82; Time 2: α = 0.80). Participants were first asked if they experienced any traumatic events; they did not necessarily fill out the items based on experience of SV items assessed at Time 1. Only participants who reported experiencing any traumatic event in their lifetime filled out the PC-PTSD-5. The Satisfaction with Life Scale (SWLS; Diener et al., 1985) contained five items such as “I am satisfied with my life” and “So far I have gotten the important things I want in life” that were rated from 1 “strongly disagree” to 7 “strongly agree.” Responses are summed, with higher scores on the measure indicating greater satisfaction with life. Internal reliability was adequate (Time 1: α = 0.94; Time 2: α = 0.92).
Social functioning.
We assessed peer relationship functioning with the PROMIS peer relationships item bank (Dewalt et al., 2013), which contained eight items such as “I was able to count on my friends” and “I felt accepted by other people my age.” Participants indicated how much each item was true for them in the past month, with response options from 1 “never” to 5 “always.” Internal reliability of the scale was adequate in the sample (Time 1: α = 0.96; Time 2: α = 0.96). We assessed satisfaction with friends with three items that were included as part of the Project ALERT Youth Survey. Youth rated how satisfied they were with “the amount of togetherness you have with your friends,” “the support and understanding your friends give you,” and “the amount you talk things over with your friends” from 1 “poor” to 5 “excellent.” Internal reliability was adequate in the sample (Time 1: α = 0.95; Time 2: α = 0.95).
Analytic Plan
We conducted a LCA using data from Time 1 on reports of SV, depression symptoms, and anxiety symptoms. We used the manual three-step approach (Nylund-Gibson et al., 2014) using Mplus, version 8.0 (Muthén & Muthén, 2010) to extract classes. To determine the best fitting solution, we estimated separate models that fit one to seven latent class solutions. To assess which model best fit the data, we considered several indicators including: negative 2 log likelihood (−2LL), Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), the sample size–adjusted Bayesian Information Criteria (aBIC), the Lo–Mendell–Rubin–adjusted likelihood ratio test (LMRT), and the bootstrapped likelihood ratio test (BLRT). The −2LL, AIC, BIC, and aBIC are all log likelihood measures for which lower values indicate better fit (Nylund et al., 2007).
We assessed outcomes 1 year later (Time 2) across emergent classes. That is, we sought to understand how aspects of physical health and sleep quality, substance use consequences, psychological functioning, and social functioning at Time 2 varied across emergent classes of SV victimization, depression, and anxiety at Time 1. We used the manual three-step auxiliary BCH approach, which uses a pseudo-class Wald chi-square test, to assess mean differences between classes on outcomes. This approach ensures that measurement of latent classes is not influenced by inclusion of covariates by fixing parameters of the latent classes. All models controlled for factors shown to be associated with sexual victimization: participant sex (female reference; (Dario & O’Neal, 2018), race/ethnicity (non-Hispanic white reference; Kalof, 2000), age (centered on grand mean; Felson & Cundiff, 2014), mother’s education (e.g., proxy for socio-economic status; Korupp et al., 2002; Mellins et al., 2017), college status (Sinozich & Langton, 2014), and sexual orientation (Coulter et al., 2017; Kosciw et al., 2016). We also controlled for whether participants had received the middle school intervention as part of the larger study. Finally, we controlled for the Time 1 values of each outcome domain and the prior wave (Wave 8) values for each variable entered into the mixture model (i.e., SV, depression, and anxiety). Across both waves of data, missing data never exceeded 10.1%. Mplus adjusts for missing data using a maximum likelihood estimator under the assumption that data are missing at random and uses all available data for each participant.
Results
Sample Description
Table 1 contains demographic information for participants, as well as prevalence of SV in the sample, means for outcomes in the four domains of functioning at Time 2, and means of the depression and anxiety scales at Time 1. Overall, at Time 1, 55.8% of participants reported experiencing at least one type of SV victimization, and nearly 28.7% experienced multiple types of SV victimization (M = 1.60, SD = 1.97). Furthermore, 71% of participants reported at least one depressive symptom (M = 4.94, SD = 5.27) and 65.6% reported experiencing at least one anxiety symptom (M = 4.36, SD = 5.22).
Table 1.
Descriptive Characteristics of the Sample.
| Variable | M (SD) or n (%) |
|---|---|
| Demographics at Time 1 | |
| Age | 19.4 (0.76) |
| Female, n (%) | 1,447 (51.7) |
| African American, n (%) | 61 (2.2) |
| White, n (%) | 538 (19.2) |
| Multi-race, n (%) | 269 (9.6) |
| Hispanic, n (%) | 1,215 (43.4) |
| Asian/Pacific Islander, n (%) | 542 (19.4) |
| Native American, n (%) | 38 (1.3) |
| Mother’s education–did not finish high school, n (%) | 388 (13.9) |
| Mother’s education—finished high school or some college, n (%) | 814 (29.1) |
| Mother’s education—finished college or higher, n (%) | 1,370 (48.9) |
| Currently attending college part- or full-time, n (%) | 1,878 (74.9) |
| Straight sexual orientation, n (%) | 2,118 (75.6) |
| Sexual violence victimization at Time 1, n (%) | |
| Any victimization | 1,337 (55.8) |
| Made unwelcome sexual comments, jokes, or gestures | 1,188 (42.4) |
| Spread sexual rumors about you | 544 (19.4) |
| Touched you in an unwelcome way | 721 (25.8) |
| Showed you sexy or sexual pictures that you did not want to see | 571 (20.4) |
| Physically intimidated you in a sexual way | 452 (16.1) |
| Forced you to do something sexual when you did not want to | 365 (13.0) |
| Depression and anxiety at Time 1 | |
| Depression (PHQ-9 score) | 4.94 (5.27) |
| Anxiety (GAD-7 score) | 4.36 (5.22) |
| Physical health and sleep quality at Time 2 | |
| General health | 2.50 (1.01) |
| Sleep quality | 2.19 (0.77) |
| Substance use consequences at Time 2 | |
| Alcohol consequences | 1.80 (2.35) |
| Marijuana consequences | 1.09 (2.17) |
| Psychological functioning at Time 2 | |
| PTSD | 2.07 (1.82) |
| Satisfaction with life | 11.3 (3.45) |
| Social functioning at Time 2 | |
| Peer relationship functioning | 31.2 (7.61) |
| Satisfaction with friends | 11.3 (3.45) |
PHQ-9 = Patient Health Questionnaire; PTSD = Post Traumatic Stress Disorder; GAD-7 = Generalized Anxiety Disorder scale.
Note. 89 participants did not know mother’s education (3.3%). Means for depression and anxiety scales ranged from 0 to 24 and from 0 to 21, respectively, with higher scores indicating greater frequency of symptoms. Mean of the general health scale represented “very good” health with a range of 1–5. Mean of the sleep scale represented “fairly good” sleep quality with a range of 1–4. Means for the substance use problems indicate the mean number of consequences experienced of a total of nine alcohol consequences and nine marijuana consequences (range: 0–9). Mean for PTSD indicates that of the participants who experienced a traumatic event in their lifetime, they reported a mean of the two of the five PTSD symptoms in the past month (range: 0–5). Those who reported no lifetime traumatic events received a score of 0 on the scale. Satisfaction with Life scores could range from 0 to 35, with higher scores indicating greater satisfaction with life. Scores on the peer relationship scale could range from 8 to 40 and scores on the satisfaction with friends scale could range from 3 to 15, with higher scores indicating better social health.
LCA
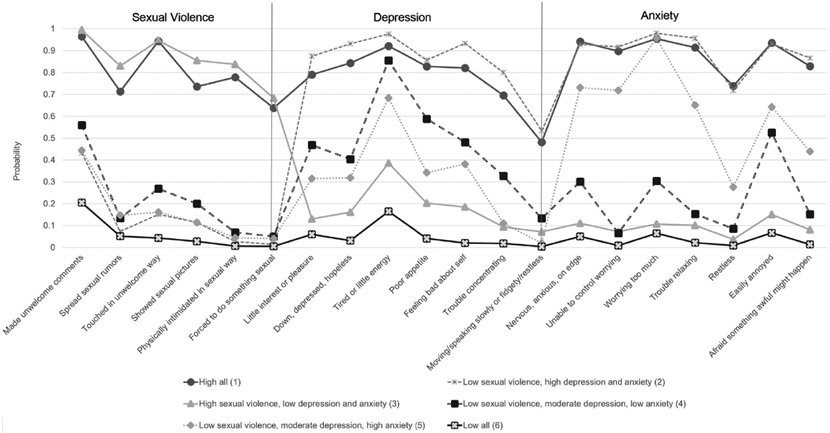
We present model fit indices for the LCA up to seven classes in Table 2. Based on model fit indices and substantive analysis of the plotted profiles, we chose the six-class solution. Figure 1 presents the item probability plot of endorsing SV, depression, and anxiety items. We describe each of the six classes below.
Table 2.
Model Fit Statistics for Latent Class Analysis at Time 1.
| Model | −2 Log likelihood |
AIC | BIC | aBIC | Entropy | LMRT |
p value |
BLRT |
p value |
|---|---|---|---|---|---|---|---|---|---|
| One class | 45,926.132 | ||||||||
| Two class | 45,926.132 | 46,012.13 | 4.626.618 | 46,126.99 | 0.929 | 13,129.465 | .000 | 13,205.73 | .000 |
| Three class | 43,343.472 | 43,365.47 | 43,744.11 | 43,537.59 | 0.894 | 2675.122 | .000 | 2690.661 | .000 |
| Four class | 42,377.776 | 42,551.78 | 43,058.57 | 42,782.15 | 0.864 | 852.743 | .000 | 857.697 | .000 |
| Five class | 41,627.636 | 41,845.64 | 42,480.59 | 42,134.27 | 0.86 | 745.807 | .000 | 750.139 | .000 |
| Six class | 411,645.512 | 41,307.53 | 42,070.64 | 41,654.42 | 0.855 | 578.744 | .001 | 582.106 | .000 |
| Seven class | 40,660.158 | 40,966.16 | 41,857.42 | 41,371.30 | 0.847 | 383.147 | .71 1 | 385.373 | .000 |
Note. AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; aBIC = adjusted Bayesian Information Criterion; LMRT = Lo–Mendell–Rubin Likelihood Ratio Test; BLRT = Parametric Bootstrapped Likelihood Ratio Test.
Figure 1.
Six class solution for sexual violence, depression, and anxiety items at Time 1.
Class 1: High all.
This class represented 13% (n = 242) of the sample. Participants in this class had high endorsement of SV, depression, and anxiety items. For example, they endorsed high probability of “someone made unwelcome sexual comments, jokes, or gestures to me” (0.97 probability), “someone forced me to do something sexual” (0.64), and “someone touched me in an unwelcome way” (0.94). The high all class also had high endorsement of depression items (range = 0.48–0.92 probability) and anxiety items (range = 0.82–0.94 probability) symptoms.
Class 2: Low SV, high depression, and anxiety symptoms.
This class represented 18% (n = 341) of the sample. In general, individuals experienced little SV (range: 0.01–0.43), though there was a 0.43 probability that individuals in this class reported “someone made unwelcome sexual comments, jokes, or gestures to me.” For depression, youth had the highest endorsement of all the classes for all eight of the depression symptoms, including “feeling down, depressed, and hopeless” (0.93), “little interest or pleasure” (0.87), and “feeling bad about yourself, or that you are a failure, or have let yourself or your family down” (0.93). Participants in this class also had high endorsement of anxiety symptoms, such as “not being able to stop or control worrying” (0.98), “feeling nervous, anxious, or on edge” (0.93), and “becoming easily annoyed or irritable” (0.93).
Class 3: High SV, low depression, and anxiety symptoms.
Individuals in this class represented 8% (n = 152) of the sample. Participants in this class reported similar rates of SV as the high all class and reported the highest probability of experiencing all six specific SV items. For example, they endorsed the highest probability of “someone made unwelcome sexual comments, jokes, or gestures to me” (0.99 probability), “someone forced me to do something sexual” (0.68), and “someone touched me in an unwelcome way” (0.95). However, participants in this class reported few depression (range = 0.07–0.39) and anxiety symptoms (range = 0.04–0.11), with the highest peak for the depression item of “feeling tired or having little energy” (0.39 probability).
Class 4: Low SV, moderate depression, and low anxiety.
Individuals in this class represented 16% (n = 312) of the sample. This class had relatively low endorsement of SV items (range = 0.05–0.55), though there was a 0.55 probability endorsing “someone made unwelcome sexual comments, jokes, or gestures to me.” Depression symptom endorsement was moderate, ranging from a probability of 0.13 for “moving or speaking so slowly that other people could have noticed” to 0.86 for “tired or little energy.” There was low endorsement of anxiety symptoms, ranging from a probability of 0.06 for “not being able to stop or control worrying” to a probability of 0.53 for “becoming easily annoyed or irritable.”
Class 5: Low SV, moderate depression, and high anxiety.
This class represented 14% (n = 273) of the sample. Similar to Classes 2 and 4, those in Class 5 had relatively low endorsement of any SV items, though again the item “someone made unwelcome sexual comments, jokes, or gestures to me” had a moderate probability (0.44). Depression symptoms were endorsed at similar rates as Class 4 (range = 0.02–0.68). However, anxiety symptom endorsement was relatively high with most individuals endorsing “worrying too much about different things” (0.96) and high numbers reporting other symptoms such as “not being able to stop or control worrying” (0.72) and “feeling nervous, anxious, on edge” (0.73).
Class 6: Low all.
The low all class represented 31% (n = 602) of the sample. Participants in this class had the lowest endorsement of all SV (range = 0.00–0.13), depression (range = 0.01–0.14), and anxiety (range = 0.01–0.05) items.
Key Domains of Functioning at Time 2
We assessed how functioning across domains was related to emergent classes. Because of the large number of comparisons across classes, we plotted means and confidence intervals of each outcome by class membership and a table to denote significant differences between classes (see Figures 2-5).
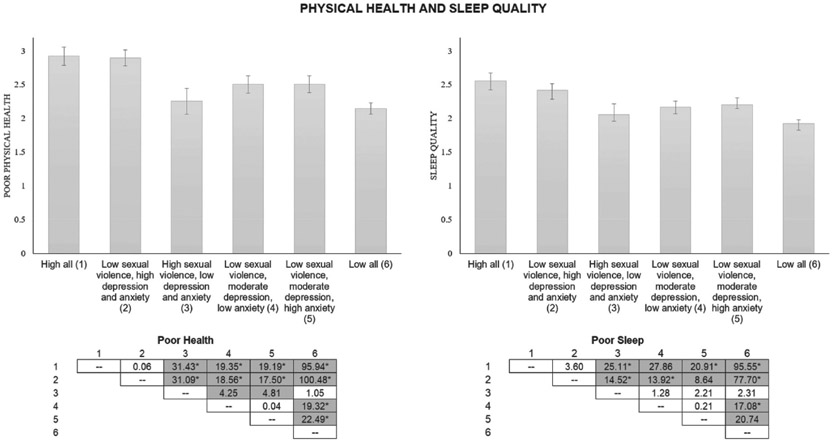
Figure 2.
Means, confidence intervals, and chi-square values by Time 1 class for the physical health domain at Time 2. Note. Figure vertical bars represent mean values on the physical health measures for each of the indicated groups. Higher scores represent worse physical health. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05. *Pairwise comparison is robust to Bonferroni correction (p = .0004).
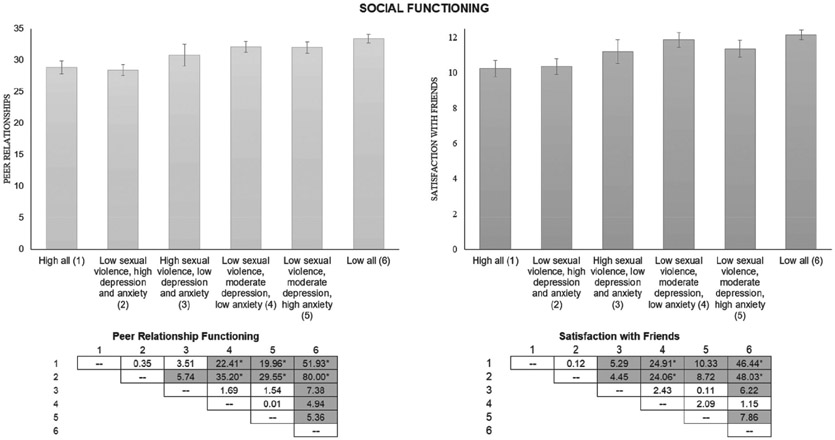
Figure 5.
Means, confidence intervals, and chi-square values by Time 1 class for the social health domain at Time 2. Note. Figure vertical bars represent mean values on the social functioning measures for each of the indicated groups. Higher scores represent better social health. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05. * Pairwise comparison is robust to Bonferroni correction (p = .0004).
Physical health and sleep quality.
Figure 2 displays the two items used for self-reported general health and sleep quality. Both items showed similar patterns across classes, such that the combination of greater experiences of SV and concurrent heightened depression and anxiety symptomology—the high all class (Class 1)—was associated with poorer health and sleep compared to all other classes except for the low SV, high depression, and anxiety class (Class 2), which was similarly associated with poorer health and sleep than the other classes. Low reported anxiety and depression, as reported in the high SV, low depression, and anxiety class (Class 3) and the low all class (Class 6), appeared to protect against poor health and poor sleep regardless of experiences of SV. That is, participants in the low all class (Class 6) reported the least degree of poor health and poor sleep compared to all other classes, but this was not significantly different from participants in the high SV, low depression, and anxiety class (Class 3). For poor health, participants in the high SV, low depression, and anxiety class (Class 3) reported significantly better health than the low SV, moderate depression, and low anxiety (Class 4) and low SV, moderate depression, and high anxiety (Class 5) classes.
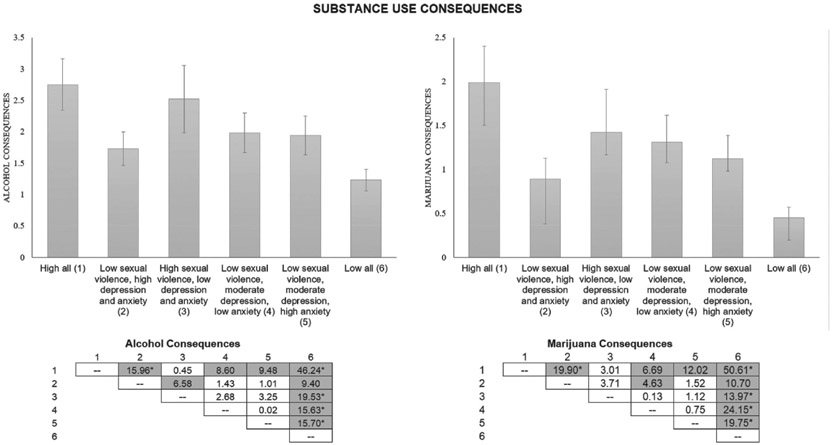
Substance use consequences.
Overall, experiencing SV was a common experience for those reporting greater alcohol and marijuana consequences 1 year later (see Figure 3). Participants in the high all class (class 1) reported significantly more alcohol and marijuana use consequences than all other classes except the high SV, low depression, and anxiety class (Class 3). The low all class (Class 5) reported the least amount of alcohol and marijuana use consequences, with significant differences between this class and all others for both substances. For alcohol consequences, participants in the high SV, low depression, and anxiety class (Class 3) reported significantly greater alcohol consequences than the low SV, high depression, and anxiety class (Class 2). For marijuana consequences, participants in the low SV, moderate depression, and low anxiety (Class 4) reported significantly greater marijuana consequences than the low SV, high depression, and anxiety class (Class 2).
Figure 3.
Means, confidence intervals, and chi-square values by Time 1 class for the substance use consequences domain at Time 2. Note. Figure vertical bars represent mean number of consequences for each of the indicated groups. Higher scores represent a greater number of consequences. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05. *Pairwise comparison is robust to Bonferroni correction (p = .0004).
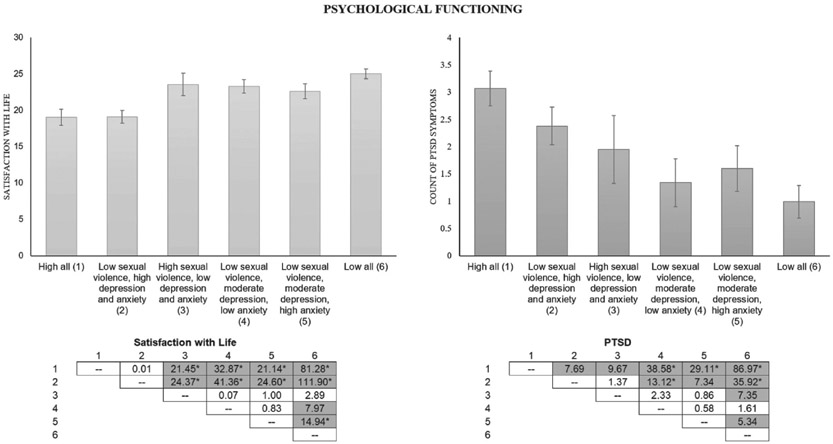
Psychological functioning.
Patterns were similar, but not identical, across classes for satisfaction with life and PTSD (see Figure 4). Satisfaction with life was similar to physical health, whereby experiencing more depression and anxiety symptoms (in the presence of SV or not) was associated with lower reported satisfaction with life 1 year later. Both participants in the high all class (Class 1) and the low SV high depression, and anxiety class (Class 2) reported significantly lower satisfaction with life than the other four classes. Those in the low all class (Class 6) also reported greater satisfaction with life than those in the low SV, moderate depression, and low anxiety (Class 4) and low SV, moderate depression, and high anxiety (Class 5) classes. For PTSD, either experiencing SV or reporting high levels of depression and anxiety symptoms was associated with greater reported PTSD symptoms 1 year later, though those who reported a combination of experiences of SV and concurrent heightened depression and anxiety symptomology (high all; Class 1) were significantly higher on PTSD symptoms than all other classes. The low SV, high depression, and anxiety class (Class 2) reported higher PTSD symptoms than the low SV, moderate depression, and low anxiety (Class 4), the low SV, moderate depression, and high anxiety (Class 5), and the low all (Class 6) classes, but not the high SV, low depression, and anxiety class (Class 3), who reported greater PTSD symptoms than the low all class (Class 6).
Figure 4.
Means, confidence intervals, and chi-square values by Time 1 class for the psychological functioning domain at Time 2. Note. Figure vertical bars represent mean values on the psychological functioning measures for each of the indicated groups. Higher scores on the Satisfaction with Life figure represent higher reported scores on the Satisfaction with Life Scale. Higher scores on the PTSD figure represent a greater number of reported PTSD symptoms. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05. *Pairwise comparison is robust to Bonferroni correction (p = .0004).
Social functioning.
Participants across all classes reported generally good social functioning, with patterns again indicating that reporting more depression and anxiety symptoms at Time 1 was associated with poorer functioning at Time 2 (see Figure 5). Those in the low SV high depression, and anxiety class (Class 2) reported the worst peer relationship functioning; significantly worse than all classes except the high all class (Class 1). Participants in the high all (Class 1) reported significantly worse peer relationship functioning and satisfaction with friends than the low SV, moderate depression, and low anxiety (Class 4), the low SV, moderate depression, and high anxiety (Class 5), and the low all (Class 6) classes. Participants in the high all (Class 1) also reported significant poorer satisfaction with friends than the high SV, low depression, and anxiety class (Class 3). Participants in the low all class (Class 6)reported the best social functioning, with higher scores on peer relationship functioning than all five other classes, and significantly greater satisfaction with friends than all other classes except the low SV, moderate depression, and low anxiety (Class 4).
Discussion
In general, several decades of research on SV has attempted to understand how experiences of SV relate to various forms of psychopathology and, generally, demographic characteristics that may increase or mitigate long-term risk. Exploring these associations is vital to our basic understanding of traumatic experiences and their effect of psychological functioning; however, heterogeneity exists in both the stressor-specific experience as well as the distress following SV. That is, while SV has been shown in meta-analyses to be directly associated with various forms of psychopathology (Dworkin et al., 2017), few studies have assessed how co-occurring psychopathology and experiences of SV relate to various behavioral health domains of functioning. This study sought to uncover heterogeneity in SV and co-occurring psychopathology (anxiety and depression) to examine whether SV has a narrow (or broad) effect on domains of functioning in the absence (or presence) of co-occurring psychopathology.
In line with our aims, we found noteworthy heterogeneity in experiences of SV and co-occurring depression and anxiety, which resulted in six different classes. More than two thirds of young adults reported experiencing some form of SV in the past year. Two classes were represented by high levels of SV, but varying levels of depression and anxiety. In fact, the two classes with high endorsement of SV reported experiencing all five items (e.g., unwelcome comments, touched in a sexual way, spread sexual rumors, was shown sexual pictures, physically intimidated in a sexual way, and forced to do something sexual) regardless of the level of depression and/or anxiety. This is noteworthy for practitioners and researchers, as it shows that youth, when exposed to SV victimization, are not experiencing SV in just one way, but in multiple ways. Prior theoretical and empirical work on poly-victimization theory support our findings such that nearly 50% of youth report experiencing more than one past year victimization typology (Finkelhor et al., 2013), and youth who experience multiple types of victimization are also at higher risk of maladaptive, long-term, outcomes (Davis, Dworkin, et al., 2018, 2019, 2020).
As expected, young adults who reported both experiences of SV and co-occurring depression/anxiety symptoms also reported the poorest functioning across all domains 1 year later: physical health and sleep quality, substance use consequences, psychological functioning, and social functioning. However, there are some unique contributions of this work that support both a narrow as well as a broad effect of SV and associated psychopathology on domains of functioning. Among the unique contributions of this work is the finding that greater reports of depression and anxiety symptoms—most often in the presence of, but at times in the absence of, SV—were associated with poorer functioning across three of the four domains. These results are in direct support of Social Stress Processing Theory, which posits that experiences of SV and co-occurring psychopathology have tremendous variation, and more importantly, have effects on a variety of health domains. For example, in support of a more broad effect of SV, we turn to physical health and sleep quality. Specifically, emergent classes with high endorsement of depression and anxiety symptomatology appeared to be consistently associated with worse physical health and poorer sleep quality compared to classes with low to moderate depression or anxiety (again, either with or without experiences SV). Thus, in this study, depression and anxiety appear to be the driving factors contributing to poor physical health and sleep quality. Prior work has noted effects of depression, and to a lesser extent, anxiety on sleep problems and physical health (Alfano et al., 2009; Roberts & Duong, 2014). Across the world, depression symptoms are consistently linked to poor health outcomes. For example, in a WHO survey, between 10% and 23% of adults with an acute or chronic physical health problem had comorbid depression, with depression symptoms having the largest effect on worsening self-reported health scores (Moussavi et al., 2007).
Furthermore, reporting more depression and anxiety symptomatology was consistently associated with greater reports of PTSD symptoms, poor satisfaction with life, and poor peer relationships 1 year later. Prior meta-analyses have shown that experiences of SV are associated with increased risk of developing PTSD as well as other psychological disorders (e.g., depression and anxiety; Dworkin et al., 2017). Our results partially support this prior work such that, while youth in the high all class did report the highest number of PTSD symptoms, individuals in the class with high SV, but with low depression and anxiety, did not report more PTSD symptoms than any of the other emergent classes. This indicates that SV was likely a driving factor for PTSD symptoms in our sample; however, those most at risk were individuals who reported co-occurring depression and anxiety symptoms. This is further supported such that youth in the high SV, but low depression and anxiety class, report significantly higher psychological functioning (in general) than youth reporting high all or those reporting low SV but high depression and anxiety. Depression and anxiety have been shown to be key predictors of poor sleep (Alvaro et al., 2013; Papadimitriou & Linkowski, 2005), poor mental health (Copeland et al., 2009; Fergusson & Woodward, 2002), and poor social functioning (Hirschfeld et al., 2000; Kupferberg et al., 2016; Olatunji et al., 2007). Our results continue to support these findings, and add an important caveat—while depression and anxiety symptoms appear to be driving poor physical, psychological, and social health, the addition of experiencing SV appears to amplify these problems. Our findings indicate that early detection of anxiety and depression symptoms in young adulthood is important, as it could help improve functioning across a variety of domains as these young people age.
However, in support of a narrower effect of SV on behavioral health, experiences of SV—in the presence of, but more often in the absence of, depression and anxiety symptoms—were most consistently associated with subsequent alcohol and marijuana consequences. Substance use, in general, has been conceptualized as a strategy to reduce negative affect following experiences of SV (Acierno et al., 1999; Kilpatrick et al., 1997; Testa et al., 2010). Prior work supports our findings, such that problematic substance use is more likely to be present among individuals with co-occurring disorders (Kramer et al., 2014; Stewart et al., 2016). Problematic substance use can be a result of SV for young people, but using substances at high levels can also put individuals at greater risk for subsequent sexual victimization (Devries et al., 2014; Parks et al., 2014; Shorey et al., 2016; Weiner et al., 2005). As discussed, prevention of SV in young adulthood is essential, but it is also important to make substance use counseling and prevention efforts widely available to youth, especially for those who experience SV. Our findings suggest that having methods for early detection of depression and anxiety are important, as these symptoms affect behavior and health in diverse ways regardless of SV experiences. Improving screening and increasing access to referral and treatment are essential to reduce the risk of poor outcomes in young adulthood.
This study is not without limitations. First, we do not know if depression and anxiety symptoms reported at Time 1 were a result of any SV experienced at Time 1, as the measures did not allow for temporality of assessment. Likewise, we do not know when the SV reported at Time 1 occurred; thus, we are not able to conclude that the SV at Time 1 led to PTSD symptoms at Time 2. This is important because it may take months for PTSD symptoms to develop after SV (Chivers-Wilson, 2006; Tiihonen Möller et al., 2014). We also did not ask participants if any of the outcomes at Time 2 were perceived as being caused by SV. Although we used validated measures for all predictors and outcomes, data are based on self-report. Furthermore, dichotomizing SV items does not take into account the frequency of these experiences, which may contribute to more severe mental health symptomology. Finally, although the assessment of both verbal and physical SV is a strength of this study, other forms of sexual harassment (e.g., cyber/internet-based sexual harassment; Chawki et al., 2015; Kowalski et al., 2014) are becoming more prominent, but were not assessed in this study. Sexual victimization in all forms is an unaddressed problem that warrants continued research and early programmatic efforts.
In conclusion, this study suggests that past year experiences of SV, along with concurrent depression and anxiety symptoms, can affect functioning across a variety of health domains 1 year later during early young adulthood. Early detection of mental health problems in conjunction with experiences of SV is vitally important, and addressing both mental health and SV may help decrease subsequent problems by helping youth access resources early on in the process of recovery. Experiences of SV may exacerbate already high levels of depression and anxiety symptoms. Thus, prevention of SV in all forms (assaults and harassment), coupled with greater access to mental health care during early adulthood, appear important to prevent poorer functioning in young adulthood. In particular, social support and social health appear to be crucial factors that should be incorporated into treatment planning (Davis, Tucker, et al., 2019; Kennedy & Prock, 2018; Relyea & Ullman, 2015). Primary care providers, mental health specialists, teachers, and law enforcement can encourage young people who disclose SV victimization to seek services that address both SV experiences and mental health, while also helping them obtain needed social support to help mitigate negative outcomes in the long term.
Acknowledgments
The authors wish to thank Kirsten Becker and Jennifer Parker for overseeing the data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by three grants from the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health (grant nos. R01AA016577, R01AA020883, and R01AA025848: D’Amico).
Biography
Jordan P. Davis is an assistant professor at the University of Southern California, and an associate director of the USC Center for Artificial Intelligence in Society, and an associate director of research for the USC Center for Mindfulness Science. His major research interests focus on development from adolescence to young adulthood and how early life trauma experiences influence developmental outcomes such as substance use and mental health.
Eric R. Pedersen is a senior behavioral scientist at the RAND Corporation. His research interests are primarily in areas of young adult/adolescent alcohol use and comorbid mental health disorders. He has received funding to develop brief, online interventions to reduce alcohol misuse among young adult populations such as college students and recent veterans. He is interested in finding ways to prevent alcohol misuse and promote treatment engagement among nontreatment-seeking young adults.
Anthony Rodriguez is a quantitative psychologist/psychometrician and associate behavioral scientist at the RAND Corporation. His quantitative methodological research has focused on structural equation modeling (SEM), item response theory (IRT), and latent growth models. A major focus of his research has tackled issues of dimensionality, reliability, and assessment scoring. He has also investigated and developed alternative IRT models designed to address and model non-normality in latent traits and errors. Aside from psychometric endeavors, his substantive interests have resulted in extensive collaborations at RAND and UCLA spanning ethnic/racial disparities in longitudinal adolescent alcohol, marijuana, cigarette, and e-cigarette use.
Joan S. Tucker is a senior behavioral scientist at the RAND Corporation. She conducts research primarily in the areas of substance use and sexual risk behavior. Her work on substance use includes identifying developmental trajectories of substance use, risk factors for initiation and escalation, and short- and long-term consequences of use during adolescence and young adulthood. Much of Tucker’s recent research has focused on developing and evaluating brief interventions for substance use and sexual risk behaviors in vulnerable populations.
Rachana Seelam, MPH, is a Research Programmer in the Research Programming Group at RAND in Santa Monica, CA. Ms. Seelam has focused her work on hospital process improvement and the prevention of adverse hospital-associated outcomes. While at RAND, Ms. Seelam has worked on a variety of health-related projects involving surveys, various administrative datasets, and medical record data, utilizing both her programming skills and statistical knowledge to clean, manage, and analyze data.
Regina Shih is director, Social and Behavioral Policy Program, and a senior behavioral and social scientist at the RAND Corporation. She currently has three primary research areas: aging and disability policy, environmental health, and behavioral health. Her aging policy work includes (a) examining the effects of a long-term care rebalancing initiative; (b) examining age-friendly initiatives on the resilience of older adults to disasters; (c) developing a national blueprint for dementia long-term care; and (d) developing instruments to assess medication reconciliation for postacute care settings. Her behavioral health work includes (a) studying the impacts of poor sleep and developing recommendations for the DoD to improve sleep programs and policies in the military; and (b) identifying multilevel risk and protective factors for adolescent substance use and risk behaviors.
Elizabeth J. D’Amico is a senior behavioral scientist at the RAND Corporation and a licensed clinical psychologist. D’Amico is nationally recognized for her work developing, implementing, and evaluating interventions for adolescents. She is a member of the Motivational Interviewing Network of Trainers (MINT), and the interventions she has developed all utilize motivational interviewing (MI). She has evaluated several MI interventions with adolescents and young adults in a variety of settings, including middle schools, primary care, homeless shelters, and teen court. She recently developed and tested a group intervention for urban Native American adolescents that integrated MI and traditional healing practices. She has also conducted epidemiological work to examine predictors and consequences of adolescent substance use. She is the principal investigator of a large longitudinal study that examines substance use patterns more than 14 years among youth from sixth grade through age 24. Her most recent work has focused on the effects of medical marijuana advertising on adolescents’ marijuana use.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Acierno R, Resnick H, Kilpatrick DG, Saunders B, & Best CL (1999). Risk factors for rape, physical assault, and posttraumatic stress disorder in women: Examination of differential multivariate relationships. Journal of Anxiety Disorders, 13(6), 541–563. [DOI] [PubMed] [Google Scholar]
- Alfano CA, Zakem AH, Costa NM, Taylor LK, & Weems CF (2009). Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depression and Anxiety, 26(6), 503–512. [DOI] [PubMed] [Google Scholar]
- Alvaro PK, Roberts RM, & Harris JK (2013). A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep, 36(7), 1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennice JA, Resick PA, Mechanic M, & Astin M (2003). The relative effects of intimate partner physical and sexual violence on post-traumatic stress disorder symptomatology. Violence and Victims, 18(1), 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, & Stevens MR (2011). The national intimate partner and SV survey: 2010 summary report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Breiding MJ, Smith SG, Basile KC, Walters ML, Chen J, & Merrick MT (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—National intimate partner and sexual victimization survey, United States, 2011. Morbidity and Mortality Weekly Report. Surveillance Summaries, 63, 1–18. [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- Campbell R, Dworkin E, & Cabral G (2009). An ecological model of the impact of sexual assault on women’s mental health. Trauma, Violence, & Abuse, 10(3), 225–246. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51). https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf
- Chawki M, Darwish A, Khan MA, & Tyagi S (2015). Sexual harassment in cyberworld. In Chawki M, Darwish A, Khan MA, & Tyagi S (Eds.), Cybercrime, digital forensics and jurisdiction (pp. 65–78). Springer. [Google Scholar]
- Chiodo D, Crooks CV, Wolfe DA, McIsaac C, Hughes R, & Jaffe PG (2012). Longitudinal prediction and concurrent functioning of adolescent girls demonstrating various profiles of dating violence and victimization. Prevention Science, 13(4), 350–359. [DOI] [PubMed] [Google Scholar]
- Chiodo D, Wolfe DA, Crooks C, Hughes R, & Jaffe P (2009). Impact of sexual harassment victimization by peers on subsequent adolescent victimization and adjustment: A longitudinal study. Journal of Adolescent Health, 45(3), 246–252. [DOI] [PubMed] [Google Scholar]
- Chivers-Wilson KA (2006). Sexual assault and posttraumatic stress disorder: A review of the biological, psychological and sociological factors and treatments. McGill Journal of Medicine, 9, 111–118. [PMC free article] [PubMed] [Google Scholar]
- Clodfelter TA, Turner MG, Hartman JL, & Kuhns JB (2010). Sexual harassment victimization during emerging adulthood: A test of routine activities theory and a general theory of crime. Crime & Delinquency, 56(3), 455–481. [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, & Angold A (2009). Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry, 66(7), 764–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter RW, Mair C, Miller E, Blosnich JR, Matthews DD, & McCauley HL (2017). Prevalence of past-year sexual assault victimization among undergraduate students: Exploring differences by and intersections of gender identity, sexual identity, and race/ethnicity. Prevention Science, 18(6), 726–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig W, Harel-Fisch Y, Fogel-Grinvald H, Dostaler S, Hetland J, Simons-Morton B, … Pickett W (2009). A cross-national profile of bullying and victimization among adolescents in 40 countries. International Journal of Public Health, 54(2), 216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Rodriguez A, Tucker JS, Pedersen ER, & Shih RA (2018). Planting the seed for marijuana use: Changes in exposure to medical marijuana advertising and subsequent adolescent marijuana use, cognitions, and consequences over seven years. Drug and Alcohol Dependence, 188, 385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Zhou AJ, Shih RA, & Green HD Jr. (2012). Preventing alcohol use with a voluntary after school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prevention Science, 13(4), 415–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, & Pedersen ER (2016). Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: Examining use patterns from age 11 to 17. Addiction, 111, 1825–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dario LM, & O’Neal EN (2018). Do the mental health consequences of sexual victimization differ between males and females? A general strain theory approach. Women & Criminal Justice, 28(1), 19–42. [Google Scholar]
- Davis JP, Dumas TM, Merrin GJ, Espelage DL, Tan K, Madden D, & Hong JS (2018). Examining the pathways between bully victimization, depression, academic achievement, and problematic drinking in adolescence. Psychology of Addictive Behaviors, 32(6), 605–616. [DOI] [PubMed] [Google Scholar]
- Davis JP, Dworkin ER, Helton J, Prindle J, Patel S, Dumas TM, & Miller S (2019). Extending poly-victimization theory: Differential effects of adolescents’ experiences of victimization on substance use disorder diagnoses upon treatment entry. Child Abuse & Neglect, 89, 165–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Ingram KM, Merrin GJ, & Espelage DL (2020). Exposure to parental and community violence and the relationship to bullying perpetration and victimization among early adolescents: A parallel process growth mixture latent transition analysis. Scandinavian Journal of Psychology, 61, 77–89. [DOI] [PubMed] [Google Scholar]
- Davis JP, Tucker JS, Dunbar MS, Pedersen ER, & D’Amico EJ (2019). Longitudinal effects of gendered verbal harassment victimization on substance use in young adulthood [Manuscript submitted for publication]. [Google Scholar]
- Devries KM, Child JC, Bacchus LJ, Mak J, Falder G, Graham K, Watts C, & Heise L (2014). Intimate partner violence victimization and alcohol consumption in women: A systematic review and meta-analysis. Addiction, 109(3), 379–391. [DOI] [PubMed] [Google Scholar]
- Dewalt DA, Thissen D, Stucky BD, Langer MM, Morgan Dewitt E, Irwin DE, … Varni JW (2013). PROMIS Pediatric Peer Relationships Scale: Development of a peer relationships item bank as part of social health measurement. Health Psychology, 32(10), 1093–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, & Griffin S (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Menon SV, Bystrynski J, & Allen NE (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, & Longshore DL (2003). New inroads in preventing adolescent drug use: Results from a large-scale trial of Project ALERT in middle schools. American Journal of Public Health, 93(11), 1830–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eom E, Restaino S, Perkins AM, Neveln N, & Harrington JW (2014). Sexual harassment in middle and high school children and effects on physical and mental health. Clinical Pediatrics, 54(5), 430–438. [DOI] [PubMed] [Google Scholar]
- Espelage DL, Hong JS, Rinehart S, & Doshi N (2016). Understanding types, locations, & perpetrators of peer-to-peer sexual harassment in US middle schools: A focus on sex, racial, and grade differences. Children and Youth Services Review, 71, 174–183. [Google Scholar]
- Felson RB, & Cundiff PR (2014). Sexual assault as a crime against young people. Archives of Sexual Behavior, 43(2), 273–284. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, & Woodward LJ (2002). Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry, 59(3), 225–231. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2013). Violence, crime, and abuse exposure in a national sample of children and youth: An update. JAMA Pediatrics, 167(7), 614–621. [DOI] [PubMed] [Google Scholar]
- Hatchel T, Espelage DL, & Huang Y (2018). Sexual harassment victimization, school belonging, and depressive symptoms among LGBTQ adolescents: Temporal insights. American Journal of Orthopsychiatry, 88, 422–430. [DOI] [PubMed] [Google Scholar]
- Hill C, & Kearl H (2011). Crossing the line: Sexual harassment at school. ERIC. [Google Scholar]
- Hirschfeld R, Montgomery SA, Keller MB, Kasper S, Schatzberg AF, Möller HJ, … Bourgeois M (2000). Social functioning in depression: A review. The Journal of Clinical Psychiatry, 61, 268–275. [DOI] [PubMed] [Google Scholar]
- Jessor R (1992). Risk behavior in adolescence: A psychosocial framework for understanding and action. Developmental Review, 12(4), 374–390. [DOI] [PubMed] [Google Scholar]
- Jessor R, & Jessor SL (1977). Problem behavior and psychosocial development: A longitudinal study of youth. Academic Press. [Google Scholar]
- Jina R, & Thomas LS (2013). Health consequences of SV against women. Best Practice & Research: Clinical Obstetrics & Gynaecology, 27(1), 15–26. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, & Read JP (2005). Toward efficient and comprehendsive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research, 29(7), 1180–1189. [DOI] [PubMed] [Google Scholar]
- Kalof L (2000). Ethnic differences in female sexual victimization. Sexuality and Culture, 4(4), 75–98. [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, & Flood AM (2009). A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress, 22(3), 227–235. [DOI] [PubMed] [Google Scholar]
- Kennedy AC, & Prock KA (2018). “I still feel like I am not normal”: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence, & Abuse, 19(5), 512–527. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, & Best CL (1997). A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology, 65(5), 834–847. [DOI] [PubMed] [Google Scholar]
- Korupp SE, Ganzeboom HB, & Van Der Lippe T (2002). Do mothers matter? A comparison of models of the influence of mothers’ and fathers’ educational and occupational status on children’s educational attainment. Quality and Quantity, 36(1) 17–42. [Google Scholar]
- Kosciw JG, Greytak EA, Giga NM, Villenas C, & Danischewski DJ (2016). The 2015 National School Climate Survey: The experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. ERIC. [Google Scholar]
- Kowalski RM, Giumetti GW, Schroeder AN, & Lattanner MR (2014). Bullying in the digital age: A critical review and meta-analysis of cyberbullying research among youth. Psychological Bulletin, 140(4), 1073–1137. [DOI] [PubMed] [Google Scholar]
- Kramer MD, Polusny MA, Arbisi PA, & Krueger RF (2014). Comorbidity of PTSD and SUDs: Toward an etiologic understanding. In Ouimette P & Read JP (Eds.), Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders (pp. 53–75). American Psychological Association. [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. [DOI] [PubMed] [Google Scholar]
- Kupferberg A, Bicks L, & Hasler G (2016). Social functioning in major depresssive disorder. Neuroscience & Biobehavioral Reviews, 69, 313–332. [DOI] [PubMed] [Google Scholar]
- LeBlanc AJ, Frost DM, & Wight RG (2015). Minority stress and stress pro-liferation among same-sex and other marginalized couples. Journal of Marriage and Family, 77(1), 40–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolin G, & Gordis EB (2000). The effects of family and community violence on children. Annual Review of Psychology, 51(1), 445–479. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Walsh K, Sarvet AL, Wall M, Gilbert L, Santelli JS, … Hirsch JS (2017). Sexual assault incidents among college undergraduates: Prevalence and factors associated with risk. PLOS ONE, 12(11), Article e0186471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, & Ustun B (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet, 370(9590), 851–858. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2010). Mplus: Statistical analysis with latent variables: User’s guide. [Google Scholar]
- Nansel TR, Overpeck M, Pilla RS, Ruan WJ, Simons-Morton B, & Scheidt P (2001). Bullying behaviors among US youth: Prevalence and association with psychosocial adjustment. Journal of the American Medical Association, 255(16), 2094–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Victim Center and Crime Victims Research and Treatment Center. (1992). Rape in America: A report to the nation.
- Nylund-Gibson K, Grimm R, Quirk M, & Furlong M (2014). A latent transition mixture model using the three-step specification. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 439–454. [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling: A multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- Olatunji BO, Cisler JM, & Tolin DF (2007). Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review, 27(5), 572–581. [DOI] [PubMed] [Google Scholar]
- Papadimitriou GN, & Linkowski P (2005). Sleep disturbance in anxiety disorders. International Review of Psychiatry, 17(4), 229–236. [DOI] [PubMed] [Google Scholar]
- Parks KA, Hsieh Y-P, Taggart C, & Bradizza CM (2014). A longitudinal analysis of drinking and victimization in college women: Is there a reciprocal relationship? Psychology of Addictive Behaviors, 28(4), 943–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, … Tiet QQ (2016). The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 51(10), 1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, & Mullan JT (1981). The stress process. Journal of Health and Social behavior, 337–356. [PubMed] [Google Scholar]
- Relyea M, & Ullman SE (2015). Unsupported or turned against: Understanding how two types of negative social reactions to sexual assault relate to postassault outcomes. Psychology of Women Quarterly, 39(1), 37–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinehart SJ, Espelage DL, & Bub KL (2017). Longitudinal effects of gendered harassment perpetration and victimization on mental health outcomes in adolescence. Journal of Interpersonal Violence. Advance online publication. 10.1177/0886260517723746 [DOI] [PubMed] [Google Scholar]
- Roberts RE, & Duong HT (2014). The prospective association between sleep deprivation and depression among adolescents. Sleep, 57(2), 239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabri B (2012). Severity of victimization and co-occurring mental health disorders among substance using adolescents. Child & Youth Care Forum, 41(1), 37–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, McNulty JK, Moore TM, & Stuart GL (2016). Being the victim of violence during a date predicts next-day cannabis use among female college students. Addiction, 111(3), 492–498. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Merrill JE, & Read JP (2012). Dimensions and severity of marijuana consequences: Development and validation of the Marijuana Consequences Questionnaire (MACQ). Addictive Behaviors, 37(5), 613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinozich S, & Langton L (2014). Rape and sexual assault victimization among college-age females, 1995-2015. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Lowe B (2006). A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine, 166, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Stemple L, & Meyer IH (2014). The sexual victimization of men in America: New data challenge old assumptions. American Journal of Public Health, 104(6), e19–e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Grant VV, Mackie CJ, & Conrod PJ (2016). Comorbidity of anxiety and depression with substance use disorders. The Oxford Handbook of Substance Use and Substance Use Disorders, 2, 149–186. [Google Scholar]
- Taylor LK, & Weems CF (2009). What do youth report as a traumatic event? Toward a developmentally informed classification of traumatic stressors. Psychological Trauma: Theory, Research, Practice, and Policy, 1(2), 91–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Hoffman JH, & Livingston JA (2010). Alcohol and sexual risk behaviors as mediators of the sexual victimization–revictimization relationship. Journal of Consulting and Clinical Psychology, 78(2), 249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiihonen Möller A, Bäckström T, Söndergaard HP, & Helström L (2014). Identifying risk factors for PTSD in women seeking medical help after rape. PLOS ONE, 9(10), Article e111136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjaden PG, & Thoennes N (2006). Extent, nature, and consequences of rape victimization: Findings from the National Violence Against Women Survey. U.S. Department of Justice, Office of Justice Programs, National Institute of Justice. [Google Scholar]
- Tucker JS, Orlando M, & Ellickson PL (2003). Patterns and correlates of binge drinking trajectories from early adolescence to young adulthood. Health Psychology, 22(1), 79–87. [DOI] [PubMed] [Google Scholar]
- Ware J Jr., Kosinski M, & Keller SD (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. [DOI] [PubMed] [Google Scholar]
- Weiner MD, Sussman S, Sun P, & Dent C (2005). Explaining the link between violence perpetration, victimization and drug use. Addictive Behaviors, 30(6), 1261–1266. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2014). Global status report on violence prevention 2014.
- Young AM, Grey M, & Boyd CJ (2009). Adolescents’ experiences of sexual assault by peers: Prevalence and nature of victimization occurring within and outside of school. Journal of Youth and Adolescence, 38(8), 1072–1083. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Amstadter AB, McCauley JL, Ruggiero KJ, Resnick HS, & Kilpatrick DG (2011). Self-rated health in relation to rape and mental health disorders in a national sample of college women. Journal of American College Health, 59(7), 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]