Abstract
Penile calciphylaxis, a rare manifestation of calcific uremic arteriolopathy, is infrequently reported in the literature. Surgical management has demonstrated similar outcomes as conservative management in terms of mean survival time. Therefore, the benefits of surgical intervention for this disease remain controversial. In this report, we present a case of penile calciphylaxis in a hemodialysis-dependent patient with end stage renal disease (ESRD). The interest of this case lies in the severity of illness on initial presentation, which precluded the possibility of conservative management and necessitated penectomy as a means of halting disease progression and improving patient quality of life.
Keywords: Penile calciphylaxis, Penectomy, ESRD
Introduction
Calcific uremic arteriolopathy (CUA), also known as systemic calciphylaxis, is an uncommon but severe disease that carries a high risk of morbidity and mortality. It is typically reported in patients with ESRD who are on chronic hemodialysis, with an incidence of 1–5% in this patient population.1 Other risk factors include: diabetes mellitus, obesity, warfarin use, calcium and vitamin D supplementation, and hypercoagulable disease states (protein C/S deficiency).1 Currently, the pathophysiology of CUA is incompletely understood. It has been attributed to metabolic dysregulation of phosphorous and calcium, likely due to a secondary hyperparathyroid state associated with ESRD. This dysregulation leads to medial calcification, thrombosis, and obliteration of small arterioles.1 Penile involvement is a poor prognostic indicator of disease progression and, given its rarity, is not frequently reported in the literature. Here, we present the case of a patient with advanced penile calciphylaxis in the setting of ESRD and hemodialysis.
Case presentation
A 56-year old man with ESRD, hemodialysis-dependent, presented to the emergency department complaining of 1 day acute, left above-knee stump pain, as well as one month of vague, worsening groin pain. A month prior to presentation, he had a left above-knee amputation. His medical history included long-standing diabetes mellitus type II (DM II) and hypertension.
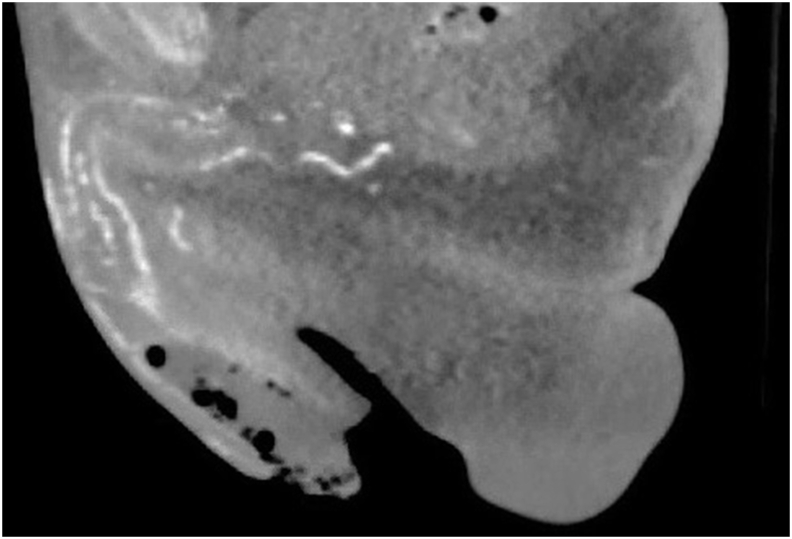
On examination, the patient was alert and oriented, with stable vital signs. Examination of the left lower extremity revealed dehiscence at the staple lines with foul-smelling pus. Genitourinary examination of his circumcised penis was notable for dry, gangrenous glans and distal phallus with a midshaft hypospadias, as well as crepitus and fluctuance of the mid-distal corpora. Laboratory analysis was significant for leukocytosis to 14.21 K/u. Computerized tomography (CT) of the pelvis (Fig. 1) demonstrated gas within the penile shaft with overlying soft tissue swelling, concerning for necrotizing infection.
Fig. 1.
CT of the pelvis (sagittal view) revealing foci of gas in corporal body of the penis, with overlying soft tissue swelling.
Given these urgent findings, the patient was started on broad spectrum antibiotics and was consented for surgery. Intraoperatively, the distal glans was found to be completely necrotic, with greater than 75% of the penile corpora filled with pus, and the proximal penile shaft was found to be viable (Fig. 2). The patient underwent a partial penectomy with urethroplasty. Intraoperative penile and wound cultures were positive for multi-resistant Citrobacter and the patient was started on appropriate antibiotic therapy. Surgical pathology of the partially resected penis revealed extensive necrosis and acute inflammation, with calcification within the vascular walls and parenchyma. The patient remained on antibiotics and had an uncomplicated postoperative course. He was discharged against medical advice on postoperative day 12 and has not followed up.
Fig. 2.
Intraoperative picture showing the completely necrotic distal glans with viable proximal shaft.
Discussion
Penile calciphylaxis is a life-threatening and rare manifestation of systemic calciphylaxis that can result in necrosis, gangrene, and fatal sepsis. Progression to penile ischemic gangrene has an especially poor prognosis in patients with ESRD and diabetes, with a 6-month mortality rate of >60%.2 Clinical exam findings include painful, violaceous lesions; hardened, subcutaneous nodules; ulceration; and/or necrotic appearance of the penile glans and/or shaft.3 Laboratory analysis may reveal elevated levels of PTH and abnormalities in serum calcium and/or phosphate,4 although our patient did not demonstrate these abnormalities.
The conservative management of penile calciphylaxis mirrors that of both non-penile cutaneous CUA and noncutaneous CUA, the latter of which is rare and is typically accompanied by cutaneous lesions. Conservative management of less severe cases of penile calciphylaxis consists of local wound debridement, analgesia, and normalization of metabolic dysregulation. Both sodium thiosulfate (STS), proposed to have antioxidant and chelating properties, and hyperbaric oxygen therapy (HBOT), which promotes cutaneous tissue healing, have shown some utility in non-penile CUA. Their moderate success in these patients has led to their use in several cases of penile calciphylaxis. However, more research is needed to establish their efficacy in this particular disease manifestation. In those suffering from severe hyperparathyroidism, parathyroidectomy is a possible means of correcting calcium deposition, although there is no consensus regarding its overall mortality benefit.5
Surgical intervention targeting the penile lesions is with either partial or total penectomy with urinary diversion. However, given that penile involvement indicates a severe presentation of systemic calciphylaxis and carries a high rate of mortality, the benefits of surgical treatment remain controversial. These have been debated in the literature, and penectomy has not demonstrated a clear advantage over conservative interventions in terms of prolonging mean time until death.3,5 Moreover, penectomy, like any surgery, carries operative and postoperative risks, which may be magnified in immunocompromised patients with multiple comorbidities.
Nonetheless, it has been proposed that in patients who are at high risk of progression of gangrene and sepsis, penectomy may be necessary for survival. Additionally, it has been suggested as a means of improving patient quality of life through alleviating the physical and psychological symptoms of gangrene, such as intractable pain and penile autoamputation.5 Therefore, penectomy may be deemed an appropriate treatment choice on a case-by-case basis.
In the case of our patient, the decision to intervene surgically was based on pain severity, fluctuance of the penile shaft, extent of penile necrosis, and the foci of gas revealed on imaging. The severity and extent of his disease obviated the possibility for conservative management, and, intraoperatively, the finding of a pus-filled corpora confirmed the need to proceed with partial penectomy. The fact that this patient was full code also influenced our decision-making process. Because this patient desired definitive treatment that would most effectively halt the spread of infection and alleviate pain, we decided that surgical management, rather than conservative management, was more likely to confer these potential benefits. Unfortunately, given the high disease mortality and frequent lack of long term follow up, data on the incidence and risk of proximal recurrence of lesions after either type of treatment is sparse.
Conclusions
Penile calciphylaxis is represents a highly fatal disease that warrants immediate attention. Surgical intervention should be considered for those with a high risk of disease progression for which penectomy would act as an infectious source control and improve patient quality of life. We conclude that in the case of our patient, partial penectomy was a judicious management option for this severe case.
Funding
None.
Declaration of competing interest
None.
Acknowledgements
None.
References
- 1.Rogers N.M., Coates P.T.H. Calcific uraemic arteriolopathy: an update. Curr Opin Nephrol Hypertens. 2008;17(6):629–634. doi: 10.1097/MNH.0b013e32830f4566. [DOI] [PubMed] [Google Scholar]
- 2.Gabel C., Chakrala T., Shah R. Penile calciphylaxis: a retrospective case-control study. J Am Acad Dermatol. May 2020 doi: 10.1016/j.jaad.2020.05.042. [DOI] [PubMed] [Google Scholar]
- 3.Karpman E., Das S., Kurzrock E.A. Penile calciphylaxis: analysis of risk factors and mortality. J Urol. 2003;169(6):2206–2209. doi: 10.1097/01.ju.0000064334.85656.a1. [DOI] [PubMed] [Google Scholar]
- 4.Budisavljevic M.N., Cheek D., Ploth D.W. Calciphylaxis in chronic renal failure. J Am Soc Nephrol. 1996;7(7) doi: 10.1681/ASN.V77978. [DOI] [PubMed] [Google Scholar]
- 5.David R., Nowicki J., Lee J., Dean N. Penile gangrene due to calciphylaxis: a multidisciplinary approach to a complex clinical challenge. BMJ Case Rep. 2019;12(12) doi: 10.1136/bcr-2019-232138. [DOI] [PMC free article] [PubMed] [Google Scholar]