Abstract
Bronchoalveolar lavage (BAL) is a commonly used procedure in the evaluation of lung disease as it allows for sampling of the lower respiratory tract. In many circumstances, BAL differential cell counts have been reported to be typical of specific lung disorders. In addition, more specific diagnostic tests including molecular assays such as polymerase chain reaction (PCR) or enzyme-linked immunosorbent assay, special cytopathologic stains, or particular microscopic findings have been described as part of BAL fluid analysis. This review focuses on common cellular and molecular findings of BAL in a wide range of lung diseases. Since the performance of the first lung irrigation in 1927, BAL has become a common and important diagnostic tool. While some pulmonary disorders have a highly characteristic signature of BAL findings, BAL results alone often lack specificity and require interpretation along with other clinical and radiographic details. Development of new diagnostic assays is certain to reinforce the utility of BAL in the future. Our review of the BAL literature is intended to serve as a resource to assist clinicians in the care of patients with lung disorders.
Keywords: Bronchoalveolar lavage (BAL), bronchoscopy, cell count differential, lung disease, pneumonitis, signature
Introduction
Bronchoalveolar lavage (BAL) is a common and relatively safe diagnostic procedure for the evaluation of patients with lung disease. It often provides valuable diagnostic information when clinical history, physical exam, routine laboratory testing, pulmonary function testing and radiographic imaging are insufficient to reach a definitive diagnosis. Compared to sputum analysis, BAL allows for targeted sampling of the lower respiratory tract with less microbial contamination from the upper aerodigestive tract.
Since the first lung irrigation was performed through a rigid bronchoscope in 1927, the procedure of BAL has advanced to become safer and better tolerated (1,2). Development of the flexible bronchoscope in 1966 was a major breakthrough as bronchoscopy and BAL are now typically performed under conscious sedation. BAL is frequently paired with other bronchoscopic procedures such as endobronchial or transbronchial biopsies, transbronchial needle aspiration, bronchial brushings, and endobronchial ultrasound-guided needle aspirations. The lavage fluid can be evaluated with a variety of analytical tests including cell counts and differential, cytopathologic analysis, and cultures in addition to specific molecular and immunologic diagnostic tests.
BAL as a diagnostic procedure
Several characteristics of BAL fluid have been recognized to predict—with varying degrees of confidence—specific lung disorders. For example, with compatible clinical history and imaging, a lymphocytic-predominant BAL is adequate to support a diagnosis of pulmonary sarcoidosis or hypersensitivity pneumonitis; or in a patient with an acute alveolar opacification on chest imaging, the presence of significant BAL eosinophils can indicate acute eosinophilic pneumonia with a fair degree of certainty (3-6). However, in most instances, although the cell differential findings on BAL often lack specificity, they still may be useful in excluding certain disorders such as diffuse alveolar hemorrhage, eosinophilic lung diseases, and to a lesser degree, certain infections, thus narrowing the differential diagnosis (7). The differential cell count may even be normal in many pulmonary disorders such as chronic obstructive pulmonary disease, asthma, or some cases of drug-induced pneumonitis (8,9). Creating greater complexity, the BAL cell count differential may evolve over time depending on the stage of the disease process such as in hypersensitivity pneumonitis and cases of acute respiratory distress syndrome (ARDS) (10,11). Nevertheless, the BAL cell count and differential pattern often assists clinicians in supporting a particular diagnosis or excluding others, thereby providing helpful clues in challenging cases and improving diagnostic accuracy. In some circumstances, no characteristic cell count and differential patterns are discernable either because of variability of cell counts seen in the disease process or limited data on BAL cell counts reported in the literature. Transbronchial biopsy and especially surgical lung biopsy retain a prominent role in the formal diagnosis of several lung diseases where BAL findings are nondiagnostic (12,13).
BAL is often performed to obtain respiratory samples in suspected infections for microbiologic culture and analysis when patients are unable to expectorate sputum even after attempt at sputum induction. However, after the initiation of antibiotics, even BAL loses sensitivity for many bacterial pathogens and becomes insensitive for fastidious microbes (14). Newer diagnostic techniques including polymerase chain reaction (PCR) and other molecular assays enhance the role of BAL for identifying specific microbial infections. Among immunocompromised patients who are vulnerable to a wider range of pathogens and may not exhibit classic symptoms or radiographic findings, BAL is particularly useful; e.g., for the diagnosis of pneumocystis pneumonia. Additionally, more recent diagnostic techniques such as matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF) and PCR coupled to electrospray ionization mass spectrometry (PCR/ESI-MS) both show potential to provide rapid microbiologic results of BAL fluid that will enable clinicians to target particular organisms far sooner than conventionally possible (15,16). More recently, whole-genome sequencing, including real-time metagenomic sequencing, of BAL fluid has been used to diagnose and manage viral, bacterial, and fungal pneumonias in critically ill patients with and without immunosuppression (17,18). In addition, shotgun sequencing of BAL fluid has been used to characterize the metagenomics and microbiome of the respiratory tract of lung transplant recipients (19) and patients with chronic lung diseases (20). As whole-genome sequencing becomes more readily available in clinical laboratories, its role in the analysis of BAL fluid will likely increase.
The technique by which BAL is performed, while similar globally, may have geographic variations depending on the institution and region of the world (21). In the United States and Europe, there are efforts to standardize the collection of BAL according to consensus guidelines (13,22,23). The bronchoscope is advanced distally into the bronchopulmonary segment of interest until it occludes the bronchus, thereby “wedging” the scope. Sequential aliquots of normal saline totaling at least 100 mL (and no more than 300 mL) should be instilled and at least 30% returned for optimal sampling. A minimum 5 mL (and ideally 10–20 mL) is needed for cellular analysis (13). Strict safety standards are advised including the use of sedatives and anesthetics and diligent monitoring of patients’ vital signs, respirations, and oxygenation during the procedure (24). BAL fluid should be collected in a labeled sterile container and transported expediently to the laboratory for analysis (21). Depending on laboratory capabilities, differential cell counts are performed by flow cytometry or manually after filtration or cytocentrifugation techniques (25).
Topical anesthetics such as lidocaine are administered universally in the upper airway, larynx, and lower respiratory tree to provide comfort and decrease cough. Theoretically, there have been concerns that high levels of topical anesthetics could reduce the sensitivity of microbial cultures from the BAL (26). This appears to be true of bronchial washings, but not of BAL (27). Such discrepancy is accounted for by the much higher volumes of sterile saline used during BAL in comparison to bronchial washings, thereby diluting the concentration of any residual topical anesthetic.
The objectives here are to compile available BAL data categorized by different classes of lung diseases and also to highlight lung disorders where insufficient BAL data exist. We performed comprehensive searches on PubMed to find available data on particular BAL profiles for a given disease using the keywords of BAL, lung lavage, and the names of specific disorders. A further goal is to provide clinicians with a succinct and referenced resource to aid in the evaluation of patients who undergo BAL albeit we acknowledge that in some resource-poor countries, many of the specific molecular tests may not be readily available. The data assembled are focused on the particular patterns of BAL cellularity seen within each disease state. In many cases, there were few published studies and when present, often limited to case reports and series. Not surprisingly, we found very few published articles on BAL data of rare lung diseases or pulmonary toxicities associated with recently developed medications.
The BAL data are organized into the following categories: healthy subjects (Table 1), airways diseases (Table 2), cystic lung diseases (Table 3), pulmonary vasculitides (Table 4), interstitial lung diseases (Table 5), occupational and environmental lung diseases (Table 6), radiation-induced pneumonitis (Table 7), infectious pneumonias (Tables 8-12), drug-induced pneumonitis (Table 13), and miscellaneous lung diseases (Table 14). For infectious pneumonias, we focused primarily on microbiologic and molecular diagnostic testing available. Additionally, we tabulated diseases characterized by particular BAL cell differential (eosinophilic, lymphocytic, or neutrophilic predominance) (Table 15), diffuse alveolar hemorrhage (DAH) due to non-infectious and infectious causes (Table 16), foamy alveolar macrophages (Table 17), and a tabulation of disorders in which a signature of BAL cellular findings may be diagnostic or relatively so (Table 18). Abbreviations in the tables are defined at the bottom of Table 18. We have elected not to discuss cytologic analysis of BAL to diagnose primary lung cancer or metastatic disease in detail in the scope of this paper.
Table 1. Healthy subjects.
| Smoking status | Bronchoalveolar lavage fluid findings |
|---|---|
| Healthy non-smokers | Macrophage predominant ~85% of all white blood cells. Lymphocytes ~10%, ~5% neutrophils, <1% eosinophils, <1% basophils (28-30) |
| Healthy smokers | Smokers have increased cellularity compared to non-smokers. They also have an increased fraction of pigmented macrophages and decreased fraction of lymphocytes (29,31) |
Table 2. Airway diseases.
| Diseases | Bronchoalveolar lavage fluid findings |
|---|---|
| Allergic bronchopulmonary aspergillosis/mycosis (ABPA/ABPM) | Increased cellularity with eosinophils, lymphocytes, or neutrophils, but often remaining macrophage predominant (32). BAL Aspergillus fumigatus IgE and BAL galactomannan can also be elevated (33) |
| Asthma | Frequently increased proportion of eosinophils; but an elevated mixed pattern with increased proportions of neutrophils, lymphocytes and mast cells are also reported (9) |
| Bronchocentric granulomatosis | No data available |
| Chronic obstructive pulmonary disease (COPD) | May reveal increased cellularity and pigmented macrophages among smokers. Otherwise, no particular pattern is seen. Stable COPD may show small increases in neutrophils, eosinophils, and lymphocytes (8,34). Patients with more severe COPD may have increased percentage of neutrophils (25). Among patients with acute exacerbations of COPD, increases in neutrophils, eosinophils, and lymphocytes may be seen |
| Cystic fibrosis | Typically remain neutrophil predominant even between exacerbations (35) |
| Mournier-Kuhn syndrome (tracheobronchomegaly, bronchiectasis, and airway diverticula) | No data available |
| Primary ciliary dyskinesia | Often neutrophilic from increased frequency of recurrent bacterial infections due to the presence of bronchiectasis (36) |
| Williams-Campbell syndrome | No data available |
Table 3. Cystic lung diseases.
| Diseases | Bronchoalveolar lavage fluid findings |
|---|---|
| Birt-Hogg-Dubé syndrome | No data available |
| Lymphangioleiomyomatosis (LAM) | No specific pattern, although may have increased pigment-laden macrophages (37). Transbronchial biopsies show positivity for HMB45 and smooth muscle actin as well as nodular infiltration of pulmonary lymphatics with LAM cells (38) |
| Neurofibromatosis | Macrophage predominance (~80%) with low level eosinophilia and mast cells described in single cases of neurofibromatosis-associated lung fibrosis (39) |
| Pulmonary Langerhans cell histiocytosis (PLCH, formerly eosinophilic granuloma) | Similar to smokers, shows increased cellularity with macrophage predominance. There may also be lymphocytosis, slight neutrophilia or eosinophilia but these changes are inconsistent. Cells demonstrating +CD1a (OKT6) in ≥5% of cells are highly specific for PLCH; although sensitivity for this cutoff value is low because only ~50% of patients show this elevation of CD1a(+) cells (7,40-42). On immunohistochemistry, cells are typically also CD68 positive and langerin (CD207) positive (43). S-100 may also be positive but is nonspecific (44). Transbronchial biopsy is insensitive (10–40% sensitivity) given patchy lung involvement in PLCH (37). Langerhans cells with distinguishing Birbeck granules may be seen on electron microscopy of biopsy specimens (45) |
Table 4. Pulmonary vasculitides*.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Behçet’s disease | Increased cellularity with increased proportion of lymphocytes. Neutrophils may also be increased (46) |
| Cryoglobulinemia | Associated with lymphocyte predominance and overall increased cellularity including subtle elevations in proportions of neutrophils and occasionally eosinophils (47,48) |
| Eosinophilic granulomatosis with polyangiitis (EGPA, formerly Churg-Strauss syndrome) | Typically with increased fraction of eosinophils (≥25%) (49). Transbronchial lung biopsy has low yield |
| Granulomatous polyangiitis (GPA, formerly Wegener’s granulomatosis) | Neutrophil predominance with slight elevation in lymphocytes or eosinophils is seen in analysis of BAL fluid (50,51). Bleeding may also be present |
| Goodpasture syndrome | Lavage confirms hemosiderin-laden macrophages or acute DAH (52) |
*, all will likely have a BAL consistent with diffuse alveolar hemorrhage (DAH).
Table 5. Interstitial lung diseases.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Acute eosinophilic pneumonia (AEP) | Eosinophilia >25%, often ranging 37–54% (6,53,54) |
| Acute interstitial pneumonia (AIP) | Neutrophil predominance with occasional evidence of hemorrhage related to DAD and resultant capillary leak (13,55) |
| Chronic eosinophilic pneumonia (CEP) | Eosinophilia, often >40%, along with relatively normal percentages of lymphocytes and neutrophils, although mild to moderate increase in lymphocytes with reduced CD4:CD8 ratio may be seen (6,7,56) |
| Cryptogenic organizing pneumonia (COP) | Findings are nonspecific. Typically, there is increased cellularity in a mixed pattern with variable increases in lymphocytes, neutrophils, eosinophils, and foamy macrophages as well as occasional increases in plasma cells and mast cells (57,58). Acute fulminant cases are often neutrophilic whereas more chronic cases tend to be lymphocytic (59). Classically, the CD4:CD8 ratio is reduced, but this finding is variable (60) |
| Desquamative interstitial pneumonia (DIP) | Increased cellularity along with increases in pigmented alveolar macrophages. An increase in eosinophils and increase in neutrophils may also be seen but lymphocyte levels tend to be low (13,61,62) |
| Granulomatous lymphocytic interstitial lung disease (GLILD) | Lymphocytosis >20% was seen among 85% of patients in a small case series (63). 50% of these cases have a low CD4:CD8 ratio |
| Interstitial pneumonia with autoimmune features (IPAF), Connective tissue associated interstitial lung disease (CT-ILD, ILD associated with rheumatoid arthritis, Sjögren’s syndrome, scleroderma, dermatomyositis) | Forms of lung disease are associated with many systemic rheumatologic conditions; these have been loosely grouped together as IPAF or CT-ILD. Although findings are highly variable, increased lymphocytes are frequently reported (64). Among patients with dermatomyositis-associated ILD, lymphocytosis is often reported and more frequent in patients with MDA-5 antibody positivity (65,66). Increases of neutrophils with rheumatoid arthritis and ILD are seen and increases in neutrophils and eosinophils can be seen in ILD associated with CREST syndrome (67,68). Sjögren’s syndrome associated ILD is also frequently associated with lymphocytosis; however, presence of neutrophils is associated with worsened disease (69). Scleroderma patients with ILD frequently have variable increases in neutrophils, eosinophils, or lymphocytes (70-72) |
| Lymphocytic interstitial pneumonia (LIP) | In one series of 15 patients, average lymphocyte counts were 30% (73). Within this series 11 were diagnosed with open lung biopsy, 3 with video-assisted thoracoscopic surgery, and 1 with transbronchial lung biopsy. Molecular testing for monoclonal gene rearrangements can confirm pulmonary lymphoma (74) |
| Niemann-Pick disease | Foamy histiocytes that are Periodic acid Schiff (PAS)-positive (75) |
| Nonspecific interstitial pneumonia (NSIP) | Typically a lymphocytosis, but highly variable (76,77). There is reduced CD4:CD8 ratio, but cases of fibrotic NSIP often do not adhere to this pattern (78). Compared to UIP, NSIP typically have greater proportion of lymphocytes and similar or less percentage of neutrophils (79) |
| Pleuroparenchymal fibroelastosis (PPFE) | Normal cell counts with slight lymphocyte elevation and low levels of neutrophils and eosinophils (80) |
| Respiratory bronchiolitis interstitial lung disease (RBILD) | Identical to smokers; increased overall cellularity with heavy pigmented macrophage predominance (13,81) |
| Usual interstitial pneumonia (UIP), idiopathic pulmonary fibrosis | Increased total number of cells with a mixed pattern, often macrophage predominant with <30% total lymphocytes, variable increases in neutrophils and small increase in eosinophils (13,28,77,82). Although elevated BAL neutrophils can be associated with worsened survival, there is no consensus that BAL results portend prognosis (83) |
Table 6. Occupational & environmental lung diseases.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Asbestosis | Increased cellularity with overall increased macrophages along with increased percentages of neutrophils, eosinophils, or lymphocytes. Iron staining of sediment may show ferruginous bodies (asbestos bodies), which appear as rod-like, or elongated dumbbell shaped crystals. However, presence of these forms only confirms exposure and not necessarily the development of clinical asbestosis (84-87) |
| Berylliosis | Blood beryllium (Be) lymphocyte proliferation test (BeLPT) is used as a screening test to confirm Be exposure. Typically, there is lymphocyte predominance with characteristically positive BeLPT (88). However, smokers and immunosuppressed patients with chronic berylliosis may have a negative BAL BeLPT. Biopsy characteristically shows granulomas. |
| Byssinosis | Increased cellularity of both neutrophils and lymphocytes (89) |
| Caplan’s syndrome (rheumatoid pneumoconiosis) associated with both rheumatoid arthritis and occupational pneumoconiosis | No cell profile available other than findings of heavily pigmented macrophages (90). Biopsy shows layer of anthracotic pigment surrounding central necrotic core |
| Coal worker’s pneumoconiosis | Increased cellularity with anthracotic-pigmented macrophages. A small increase in neutrophils may be seen, especially in those with progressive massive fibrosis (91-93) |
| Hard metal lung disease (cobalt, molybdenum, nickel, titanium, tungsten exposure) | Multinucleated giant cells are typically seen, but not always. Cell count may be increased in a mixed pattern or have relative lymphocytosis or eosinophilia. Transbronchial biopsies may be analyzed for heavy metals (94-97) |
| Hypersensitivity pneumonitis (HP, also known as extrinsic allergic alveolitis) | Lymphocytosis (often >50%) with moderate neutrophilia, modest eosinophilia and mast cells. Classically, a low CD4:CD8 ratio was believed to be helpful in differentiating HP from sarcoidosis but high variability in the CD4:CD8 ratio may be seen (4,5,98-101). Levels of neutrophils in BAL decline with time after antigen exposure (10). Foamy macrophages may be seen |
| Siderosis | Hemosiderin-laden macrophages but otherwise a normal differential cell count (102,103). Elevated BAL ferritin levels have also been reported (104) |
| Silicosis | In acute silicosis, lavage is often milky appearing similar to alveolar proteinosis. Foamy macrophages with positive periodic acid Schiff (PAS) staining are characteristic. Birefringent particles consistent with silica may be seen with polarized microscopy. In chronic silicosis, biopsy may show pigmented macrophages along with silicotic nodules and parenchymal fibrosis. Abundant macrophages with an increase in lymphocytes and neutrophils can be seen. Lesions can develop into progressive massive fibrosis where the cores may become necrotic (105-107) |
Table 7. Radiation-induced pneumonitis.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Radiation-induced pneumonitis—may be a primary lung injury in a radiation treatment field or secondary injury outside the field due to radiation-primed, immune-mediated inflammation | Increase in several cell types but often a lymphocyte predominance both in irradiated and non-irradiated, contralateral lung (108,109). Radiation-induced organizing pneumonia may be seen with contralateral radiotherapy for breast cancer with a mixed pattern of increases in lymphocytes, neutrophils, eosinophils, and mast cells (7) |
Table 8. Infectious pneumonia: viruses.
| Diseases/agent | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Adenovirus | PCR is highly specific and sensitive (110). One case report with acute infection revealed neutrophil predominance (111) |
| Anellovirus | Whole-genome shotgun DNA sequencing can reveal higher abundance in lung transplant receipt compared to healthy controls; high viral load correlates with dysbiotic communities in the allograft BAL and may indicate anellovirus lung infection and portend adverse transplant outcome (19) |
| Coronavirus, Middle East respiratory syndrome strain (MERS-CoV) | Detection of coronavirus with various strain-specific PCR (112). BAL and tracheal aspirates yielded greater viral loads for MERS-coronavirus than nasopharyngeal swabs or sputum samples (113). No cell data available |
| Coronavirus, COVID-19 | Single cell RNA sequencing of BAL fluid demonstrated depletion of tissue-resident alveolar macrophages and increased monocyte-derived inflammatory macrophages (in severe disease), and increased clonal expansion of CD8+ T cells (in mild cases) (114). Increasing levels of neutrophils were associated with worsened severity of disease (114) |
| Cytomegalovirus | PCR of BAL specimens is rapid and sensitive (115). Cytopathologic changes can show characteristic Cowdry owl’s eye inclusion bodies. Serum pp65 antigen detection may be a better test for active infection than CMV PCR (116). Metagenomic next-generation sequencing showing ≥50% unique reads or any read of the virus not detected by convention means may indicate infection in critically ill patients (17) |
| Hantavirus pulmonary syndrome (Sin Nombre virus) | Capillary leak pulmonary edema with relative acellularity; immunoblasts found are activated lymphocytes with plasmacytoid features (117,118) |
| Hemorrhagic fever with renal syndrome with pulmonary involvement (Seoul hantavirus or Puumala virus) | Increased lymphocytes comprised of CD8 T cells and natural killer cells with increased expression of HLA-DR and CD25 (activation markers) as well as increased granzymes A and B (119-121). For Puumala hantavirus, alveolar macrophages with greenish, intracytoplasmic inclusions. With Seoul hantavirus, plasmacytoid and plasmablastic cells (immunoblasts) are seen (122) |
| HIV-associated pneumonitis | Lymphocytosis with associations with either LIP or NSIP (123-126) |
| Human metapneumovirus (hMPV) | No BAL cell profile available. Epithelial cell degenerative changes with eosinophilic inclusions may be seen within in the cytoplasm. hMPV RNA is detected by RT-PCR (127,128) |
| Herpes simplex (HSV-1) bronchopneumonitis | Macroscopic bronchial lesions may present as mucosal erythema and superficial ulcerations. Non-specific increases in all types of inflammatory cells are described (129-131). Multinucleated epithelial cell metaplasia (Tzanck cells) and the presence of eosinophilic nuclear inclusions with a surrounding clear halo (Cowdry bodies) that may also be seen with varicella zoster virus and cytomegalovirus infections. PCR for HSV-1 can be diagnostic. Quantitation of DNA load may predict respiratory insufficiency and perhaps mortality (132,133). Metagenomic next-generation sequencing can be used to diagnose infection in critically-ill patients (17) |
| Influenza | Neutrophilia in first week followed by subsequent lymphocytosis (134). Limited data from a series of patients with ARDS from influenza |
| Parainfluenza | Elevations in both neutrophils and lymphocytes from one case report (135) |
| Respiratory syncytial virus | Neutrophilic predominance has been described (136) |
| Varicella zoster pneumonia | Elevated cellularity and an increase in lymphocytes with a low CD4:CD8 T-cell ratio (137). Detected by PCR (138) |
Table 9. Infectious pneumonia: bacteria.
| Diseases/organisms | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Q fever (Coxiella burnetii) | PCR positive for C. burnetii DNA (repetitive element IS1111) (139) |
| Legionella | Severe L. pneumophila pneumonia revealed marked neutrophilia with increased number of lymphoblasts and activated T cells (140). BAL for Legionella DNA (16S rRNA gene) by PCR, direct fluorescent antibody test, and culture may complement urine antigen testing (141). L. pneumophila may also stain acid-fast positive (142) |
| Leptospirosis | DAH may occur with minimal or no apparent abnormality on chest radiograph and with or without renal or hepatic involvement. No definitive data on differential cell count although histopathologic findings indicate relatively modest infiltration of alveolar spaces with monocytes and neutrophils. Dark-field examination may show the spirochetes (143-146) |
| Mycoplasma pneumoniae | Increased neutrophils and T lymphocytes with greater TH2 cytokine expression; i.e., increased IL-4 and IL-4/IFN ratio compared to pneumococcal pneumonia and controls (147). PCR targeting phosphotransferase system I gene, P1 cytadhesin gene, and M. pneumoniae repetitive element (RepMP1) all have similar and good accuracy on various respiratory specimens including BAL fluid (148). DAH has also been reported (149). BAL cell profile not available |
| Plague (Yersinia pestis) | No data available |
| Tularemia (Francisella tularensis) | No data available. Culture has lower sensitivity than PCR (150) |
Table 10. Infectious pneumonia: fungi.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Aspergillus pneumonia | BAL galactomannan increases the sensitivity of test when compared to serum galactomannan (151). However, BAL galactomannan is not routinely recommended among non-immunocompromised patients due to risk of false-positive results (152). Angioinvasive aspergillosis is diagnosed based on tissue biopsy. Metagenomic next-generation/whole genome sequencing can be used to diagnose infection (17) |
| Blastomyces pneumonia | Yeast forms are ~8–15 μm in diameter with broad-based budding. Fungal culture adds to diagnostic yield of cases not diagnosed on BAL cytopathology alone (153). Specific antigen testing in BAL fluid is only 62.5% sensitive (154) |
| Candida pneumonia | Colonization frequency is quite high among critically ill and mechanically ventilated patients. No formal quantitative thresholds exist to differentiate infection from colonization (155) |
| Coccidioides pneumonia | Coccidioides immitis spherules can be seen on Papanicolaou stain. Culture of BAL fluid has higher sensitivity than microscopy alone (156). BAL cellular profiles tend to have elevations in neutrophils and may have very mild elevations in eosinophils (157). Eosinophilia is more commonly seen in peripheral blood |
| Cryptococcus pneumonia | Encapsulated yeast can be seen on microscopy, particularly when stained with India ink (158). Cryptococcal antigen testing on BAL is highly specific (159) |
| Histoplasma pneumonia | Delicate smooth branching microconidia, 2–3 μm in diameter with narrow-based budding can be seen on microscopy. Histoplasma antigen enzyme immunoassay (EIA) in BAL fluid is quite sensitive (94%) when tested in a cohort of mostly immunocompromised patients (160) |
| Pneumocystis jirovecii pneumonia (PJP) or PCP pneumonia | Cell count is nonspecific and may show relative increases in lymphocytes, neutrophils, and eosinophils. Foamy alveolar casts and P. jirovecii clusters are seen on Giemsa stain. PCR and DFA can also be sent on BAL fluid with improved yield in comparison to sputum alone (161-163) |
| Pulmonary mucor (Zygomycosis) | Ribbon-like fungal hyphae with non-septated, right-angle branching seen on Papanicolaou stains (164). In a small case series, 60% of cases were diagnosed on BAL alone and the remaining 40% were diagnosed based on transbronchial biopsy (165). Fungal stain on microscopy has higher yield than fungal culture |
Table 11. Infectious pneumonia: parasites.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Angiostrongyliasis | Eosinophilia with nematode larvae on microscopy (166) |
| Leishmaniasis | Amastigotes can be found on microscopy (167) |
| Paragonimiasis | Ova & parasite exam reveals ova which are golden yellow in color, 80 μm in length and 40–50 μm in diameter with a flat operculum (168,169) |
| Strongyloidiasis | Neutrophil predominant with rhabditiform larvae on microscopy (170,171) |
| Toxocariasis | Eosinophilia (172) |
| Toxoplasmosis | Trophozoites can be seen with Giemsa-stain (173) |
Table 12. Infectious pneumonia: mycobacteria.
| Diseases | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Tuberculosis | Acid-fast bacilli on stain and subsequent culture. Increased total number of cells and percentage of lymphocytes (174,175). Mycobacterium tuberculosis PCR can provide rapid diagnosis prior to culture results. Higher percentage of CD4+ T cells and lower percentage CD8+ T cells (and opposite findings in peripheral blood) of patients with higher clinical grade of pulmonary TB-defined by extent of lung involvement and presence of fever and weight loss (176) |
| Non-tuberculous mycobacteria (NTM) | Acid-fast bacilli on Ziehl-Neelsen stain may be seen but unusual unless mycobacterial burden is high. A single case report in a patient with Hodgkin’s lymphoma and Mycobacterium mucogenicum had a lymphocyte predominance (177). NTM lung disease is typically associated with increased percentage of lymphocytes and neutrophils (178). With Mycobacterium avium complex (MAC)-associated nodular bronchiectasis, those who were “not deteriorating” (n=8) had increased lymphocyte and neutrophils but macrophages > lymphocytes > neutrophils; in contrast, of those who were “deteriorating” (n=13), the relative percentages were neutrophils ≥ macrophages > lymphocytes (179). In 37 MAC lung disease subjects, those with neutrophil-dominant BAL had more severe radiographic disease and greater clinical deterioration than those with lymphocyte-dominant BAL (180) |
Table 13. Drug-induced pneumonitis.
| Drugs | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Adalimumab (anti-TNF monoclonal antibody) | Macrophage predominance with slight elevations in eosinophils and lymphocytes (181). Transbronchial biopsy with thickening in alveolar septa and mild to moderate lymphocytic interstitial cellularity consistent with ILD and OP |
| Alemtuzumab (anti-CD52 monoclonal antibody) | Associated with DAH and interstitial pneumonitis (182). No BAL cell profile available |
| Amiodarone | Highly variable pattern: normal to increased levels of lymphocytes, neutrophils, and eosinophils. Lymphocytosis and foamy intracytoplasmic vacuoles in alveolar macrophages (due to accumulation of phospholipids) may indicate only exposure and not necessarily toxicity (183-186). On electron microscopy, the foamy cytoplasmic vacuoles correspond to surfactant-like lamellar bodies. Cellular differential is not prognostic of outcome |
| Anagrelide | Hypersensitivity pneumonitis with BAL showing predominance of lymphocytes as well as fibrotic changes are reported (187) |
| Azathioprine | Rare association with usual interstitial pneumonitis, organizing pneumonia or DAD (188). No BAL cell profile available |
| Bevacizumab (anti-VEGF monoclonal antibody) | Associated with development of hemoptysis, pulmonary embolus, pulmonary hemorrhage and interstitial pneumonitis (189). With interstitial pneumonitis, BAL may reveal elevated lymphocytes (190) |
| Bleomycin | Neutrophilia from limited data (191) |
| Bortezomib (proteasome inhibitor) | Associated with a pattern of organizing pneumonia, bronchiolitis obliterans, pleural effusions, or DAD (192-194). No BAL cell profile available |
| Bromocriptine | Associated with pulmonary fibrosis (195). No BAL cell profile available |
| Busulfan (alkylating chemotherapeutic) | Both increases in lymphocytes or neutrophils have been reported along with atypia in type I pneumocytes (196) |
| Captopril and perindopril | Rarely, diffuse interstitial/alveolar pneumonitis has been reported which may have lymphocytic infiltration or eosinophilic pneumonia (197,198) |
| Carbamazepine | Associated with an acute pattern of hypersensitivity pneumonitis or eosinophilic pneumonia from limited data (199) |
| Carmustine (BCNU) (alkylating chemotherapeutic) | Associated with development of pulmonary fibrosis that may be early-onset or delayed. No BAL cell profile exists on patients with early-onset fibrosis. Among patients with delayed-onset, they had upper lobe predominant fibrosis and either a normal BAL differential or increase in lymphocytes (200) |
| Cetuximab (anti-EGFR monoclonal antibody) | Associated with infusion-related bronchospasm, pneumonitis, bronchiolitis, organizing pneumonia and pulmonary fibrosis (201,202). Pneumonitis was more common in patients also receiving radiation therapy for non-small cell lung cancer (203). No BAL cell profile available |
| Checkpoint inhibitors (anti-PD-1, anti-CTLA-4, anti-PD-L1) | Risk of checkpoint inhibitor pneumonitis (CIP)—consolidation, organizing pneumonia, GGO, interlobular septal thickening, and traction bronchiectasis—greater with anti-PD-1 and anti-PD-L1 than anti-CTLA4. In a meta-analysis of nearly 4,500 patients on anti-PD-1 inhibitor, the overall incidence of pneumonitis was 2.7% and the pneumonitis was more frequent and severe in patients with lung cancer or renal cell carcinoma than melanoma (204,205). In 22 patients with CIP, the mean BAL lymphocyte count was 14% (range 4–90%) (206). Another study of 30 patients with CIP determined the mean BAL lymphocytes to be 34% (1–70%) (207). High-grade CIP is associated with poor prognosis (208) |
| Chlorambucil (alkylating chemotherapeutic) | Associated with a hypersensitivity pneumonitis pattern with increased lymphocytes (209). However, if leukemic pulmonary infiltration is suspected as cause of radiographic abnormality, BAL is insensitive and lung biopsy is recommended (210) |
| Cyclophosphamide (alkylating chemotherapeutic) | Both early-onset acute pneumonitis is described along with a late-onset fibrotic disease associated with pleural thickening and DAD (211). Limited BAL cell profile data exists for either form; a patient with chronic cyclophosphamide toxicity and associated fibrosis was reported to have macrophage predominance (212) |
| Dasatinib (Tyrosine kinase inhibitor) | Pneumonitis with lymphocytosis is most commonly reported (213). Also associated with lymphocytic, typically exudative pleural effusions. Another single report with BAL neutrophilia was also reported (214) |
| Docetaxel (anti-mitotic chemotherapeutic) | Associated with a capillary leak syndrome 8–14 days after administration (215,216). No BAL cell profile available |
| Doxorubicin (topoisomerase inhibitor) | Possible association with organizing pneumonia from limited data (217). Associated with radiation recall effect |
| Erlotinib (tyrosine kinase inhibitor) | Associated with acute development of ILD with either a DAD or OP pattern (218-220). BAL with neutrophilic predominance |
| Etanercept (soluble p75 TNF receptor subunit) | Associated with development of granulomatous inflammation and a sarcoidosis-like reaction or organizing pneumonia with lymphocytic BAL (221-223) |
| Etoposide (topoisomerase II inhibitor) | Associated with DAD as well as radiation recall effect. BAL with lymphocytic predominance (224,225) |
| Everolimus (mTOR inhibitor) | HP pattern with lymphocytosis, in particular with increased CD4 cells (226,227). Biopsies may also show OP, LIP, non-necrotizing granulomatous inflammation, and vasculitis. Less commonly, an eosinophilic BAL is reported |
| Gefitinib (EGFR inhibitor) | Associated with acute ILD developing 3–7 weeks after initiating therapy. Increase in lymphocytes or eosinophils although some cases have normal cellularity and differential (228,229). Higher incidence in Japanese patients may be associated with increased EGFR mutations seen in Japan (230). Biopsies consistent with DAD |
| Gold | In one case series, 72% all had lymphocyte predominance (231). Cases can be associated with a pattern of NSIP, DAD or OP (231,232). Toxicity typically occurred 2–6 months after initiation on therapy |
| Hydroxyurea | Associated with a pattern of acute ILD or HP (233,234). No BAL cell profile available |
| Imatinib (BCR-ABL, c-Kit, and PDGFR tyrosine kinase inhibitor) | Pneumonitis. Can also cause pleural effusions and eosinophilic pneumonia. Limited BAL data reveals eosinophilia (235) |
| Ipilimumab (anti-CTLA4 monoclonal antibody) | Associated with inducing a sarcoidosis-like granulomatous disorder. Characteristically with elevated lymphocytes with a high CD4:CD8 ratio (236). Biopsy may show non-caseating granulomas or OP (237) |
| Isoniazid | Associated with a pattern of pneumonitis or lung fibrosis (238). No BAL cell profile available except for one case with eosinophilic pneumonia (239) |
| Lenalidomide | Patterns of HP, OP and eosinophilic pneumonia can be seen. Limited BAL data suggests a pattern with increased neutrophils (240,241) |
| Melphalan (alkylating chemotherapeutic) | Increased lymphocytes. Associated with development of interstitial pneumonitis and interstitial fibrosis (242,243) |
| Methotrexate | Lymphocytic predominance is quite common, but there can be a variable BAL pattern (244). Findings are nonspecific. NSIP pattern is common; however, OP and HP are also reported (245) |
| Methysergide | No BAL cell profile available. Associated with development of pulmonary and retroperitoneal fibrosis (246) |
| Nitrofurantoin | Associated with an acute and chronic form of drug injury. Acute toxicity occurs within 2 weeks often with fever, cough, dyspnea, and peripheral eosinophilia. In these acute cases, a relative increase in eosinophils was described. Chronic toxicity can occur months to years later with a pattern of NSIP and resultant fibrosis (247-249) |
| Nivolumab (anti-PD1 receptor monoclonal antibody) | Associated most frequently with pattern of OP but also HP, AIP/ARDS, and NSIP (250). Also associated with radiation recall (251). No BAL data available |
| Non-steroidal anti-inflammatory drugs (NSAIDS) | Associated with HP. No BAL data available (252) |
| Ofatumumab (anti-CD20 monoclonal antibody) | Associated with interstitial pneumonitis. Limited BAL data demonstrated lymphocyte predominance with low CD4:CD8 ratio (253,254) |
| Paclitaxel (anti-mitotic chemotherapeutic) | Increased proportion of lymphocytes and eosinophils (255,256). Pattern of HP is reported. Additionally, associated with radiation recall and may cause fibrosis |
| Pembrolizumab (anti-PD1 monoclonal antibody) | Associated with an OP pattern with increased cellularity including elevated lymphocytes and elevated neutrophils (257). One case of radiographic appearing NSIP has also been reported (258) |
| Penicillamine | Associated with interstitial pneumonitis, OP, HP and eosinophilic pneumonia (259). Hemorrhage can occur after prolonged therapy. No BAL data available |
| Phenytoin | Normal differential reported in two case reports of pneumonitis (260,261) |
| Propylthiouracil | Associated with ANCA positive vasculitis, capillaritis, and DAD (262) |
| Rituximab (anti-CD20 monoclonal antibody) | Interstitial pneumonitis, OP and ARDS are all reported. Limited BAL data suggest lymphocytosis is a common feature (263-265) |
| Sirolimus (mTOR inhibitor) | Pneumonitis characterized by lymphocyte predominance and alveolar hemorrhage is described (266,267) |
| Sorafenib (tyrosine kinase inhibitor) | Pneumonitis including AIP has been described (268). Cases may have lymphocyte predominance |
| Sulfasalazine | Eosinophilic pneumonia, HP and OP patterns have been described (269-271) |
| Sunitinib (tyrosine kinase inhibitor which blocks receptors for PDGFR and VEGFR) | Associated with recall pneumonitis and increased risk of pulmonary embolism (272). No BAL data available |
| Trastuzumab (anti-HER2 monoclonal antibody) | Pneumonitis with neutrophil predominance (273) |
| Valproic acid | Neutrophil predominance (274). Valproic acid can also be associated with an eosinophilic pleural effusion or DAH (275,276) |
Table 14. Miscellaneous lung diseases.
| Disease | Bronchoalveolar lavage fluid characteristics |
|---|---|
| Acute respiratory distress syndrome (ARDS) | BAL early in ARDS reveals extensive neutrophils (277). However, in later resolution phases, there are less neutrophils and restored numbers of macrophages (11). Relatively low numbers of lymphocytes are seen in both phases |
| Amyloidosis | No specific pattern seen; but, increased cellularity with relative elevations in lymphocytes are reported (278) |
| Chronic aspiration/lipoid pneumonia | Lipid laden macrophages are typical and can stain positive with lipid stains such as Oil Red O stain (279). Neutrophils may also be present depending on the burden of aspiration pneumonitis (280) |
| Crack-cocaine pneumonitis | Heavily pigmented turbid, gray, or black specimens due to carbonaceous material (281). Hemorrhage or elevations in eosinophils may be present in BAL (282) |
| Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH) | Lymphocytosis reported in a small case series (283) |
| Erdheim-Chester disease | Opalescent fluid predominantly comprised of foamy macrophage (histiocytes). Histiocytes are CD1a negative and langerin (CD207) negative, but positive for CD68, CD163, and Factor XIIIa (284,285). Some histiocytes are noted to have an additional intracytoplasmic membrane, termed a “double-contoured histiocyte.” |
| Heřmanský-Pudlák syndrome | Increased cellularity with normal differential. Macrophages filled with ceroid, a lipofuscin-like lipopigment, which stains orange with lipid stains and deep blue with Schmorl’s reaction (286,287) |
| Idiopathic pulmonary hemosiderosis | Consistent with DAH. In chronic pulmonary hemosiderosis, a brown-yellow tinged lavage is due to hemosiderin-laden macrophages (288) |
| Lung cancer | Historically, malignant cells in approximately 40% of cases with peripheral lesions based on older studies (289). More recently, BAL was shown to have reduced sensitivity of only 15% (290) and sensitivity declines rapidly with smaller and more peripheral lesions (291), reflecting changes in practice and advances in diagnostic bronchoscopy for suspected lung cancer |
| Pulmonary alveolar microlithiasis | May be cloudy with microliths that can be seen with microscopy. Transbronchial biopsy will yield concentric laminated microliths in alveolar space along with thickened interstitial septa (292,293). Microliths also seen with pulmonary tuberculosis and in healed varicella pneumonia |
| Pulmonary alveolar proteinosis (PAP) | Diagnostic in close to 100% of the cases. Fluid appears milky and if left standing, settles into a layer of lipoproteinaceous sediment. No particular cellular pattern on BAL is helpful for diagnosis although elevated lymphocytes or eosinophils have been reported (183,294). Cytology reveals foamy macrophages and globules that are PAS-positive for lipoproteinaceous material (295-298) |
| Pulmonary capillary hemangiomatosis | DAH with hemosiderin-laden macrophages (299). Transbronchial biopsy should be avoided given risk for hemorrhage |
| Pulmonary post-transplant lymphoproliferative disorder (PTLD), with spectrum ranging from polyclonal lymphoid hyperplasia to lymphoma with a variety of imaging findings | Typically, lymphocytic predominant that may be polyclonal or clonal B cells that are Epstein-Barr virus (EBV) positive by PCR. Screening for PTLD has been recommended by assaying for EBV by PCR in the blood or in the BAL (300,301) |
| Pulmonary veno-occlusive disease | DAH with hemosiderin-laden macrophages (302,303). Bronchoscopic appearance of intensely hyperemic lobar and segmental bronchi with longitudinal streaking has been reported. Transbronchial biopsy should be avoided given risk for hemorrhage (304) |
| Sarcoidosis | Majority of cases (90%) demonstrate increased lymphocytes with normal levels of neutrophils and eosinophils (3,5). Classically, CD4:CD8 ratio ≥2, but this ratio can be variable including cases with CD8 predominance (305). A combination of CD4:CD8 ratio ≥2, ≤1% neutrophils, and ≤1% eosinophils has a similar specificity and positive predictive value as multiple non-caseating granulomas on transbronchial biopsy in distinguishing sarcoidosis from non-sarcoidosis disease (306). BAL CD4:CD8 ratio does not predict prognosis or response to treatment |
| Electronic cigarette/vaping-associated lung injury (EVALI) | Majority of cases are linked with the use of marijuana oils or concentrates, associated with the presence of medium chain triglyceride, vitamin E acetate, and other lipids in the inhaled product (307-311). Lung diseases described with EVALI include DAD, AEP, OP, lipoid pneumonia, and HP and may present on chest CT as consolidation, GGO, and peripheral reticulations. In case series, BAL showed moderate increase in neutrophils (20–50%), mild increase in lymphocytes (0–25%), and high numbers of lipid-laden (Oil Red O stain positive) macrophages (25–75%) (312-314) |
Table 15. Diseases characterized by particular BAL cell differential.
| Eosinophilic-dominant | Lymphocytic-dominant | Neutrophilic-dominant |
|---|---|---|
| Diseases: acute eosinophilic pneumonia, allergic bronchopulmonary aspergillosis, chronic eosinophilic pneumonia, eosinophilic granulomatosis with polyangiitis, parasitic pneumonias. Drug-induced: carbamazepine, sulfasalazine, others | Diseases: berylliosis, cryoglobulinemia, granulomatous lymphocytic interstitial lung disease, HIV-associated pneumonitis, hypersensitivity pneumonitis, lymphocytic interstitial pneumonia, non-specific interstitial pneumonia, sarcoidosis, tuberculosis. Drug-induced: checkpoint inhibitors (anti-PD-1 & anti-PD-L1 > anti-CTLA-4), dasatinib, etanercept, etoposide, everolimus, gold, pembrolizumab, radiation-induced pneumonitis, sirolimus | Diseases: acute interstitial pneumonia, ARDS, initial phase, bacterial pneumonia, cystic fibrosis, granulomatous polyangiitis. Drug-induced: bleomycin, erlotinib, trastuzumab, valproic acid |
BAL, bronchoalveolar lavage.
Table 16. Diffuse alveolar hemorrhage.
| Diffuse alveolar hemorrhage due to non-infectious causes |
| DAH with pulmonary capillaritis |
| Isolated pauci-immune necrotizing pulmonary capillaritis |
| Granulomatous polyangiitis |
| Microscopic polyangiitis |
| Mixed cryoglobulinemia |
| Behcet’s syndrome |
| Henoch-Schönlein purpura |
| Goodpasture’s syndrome* |
| Pauci-immune glomerulonephritis |
| Immune-complex-associated glomerulonephritis |
| Collagen-vascular disease (systemic lupus erythematosus*, polymyositis, rheumatoid arthritis, mixed-connective tissue disease, scleroderma) |
| Primary antiphospholipid antibody syndrome |
| Acute lung transplant rejection |
| Autologous bone marrow transplantation |
| Drugs (e.g., propylthiouracil with positive anti-neutrophilic cytoplasmic antibody) |
| DAH without capillaritis |
| Idiopathic pulmonary hemosiderosis |
| Systemic lupus erythematosus* |
| Goodpasture’s syndrome* |
| Diffuse alveolar damage—e.g., after cytotoxic drug preconditioning therapy for bone marrow transplantation |
| Penicillamine—bland hemorrhage; uncommon; occurs after 1 year of therapy |
| Tuberous sclerosis |
| Trimellitic anhydride |
| Mitral stenosis |
| Coagulation disorders |
| Pulmonary veno-occlusive disease |
| Pulmonary capillary hemangiomatosis |
| Lymphangioleiomyomatosis—due to rupture of postcapillary venules, which are infiltrated by smooth muscles |
| Pulmonary embolism with infarction |
| Diffuse alveolar hemorrhage due to infectious causes (315) |
| Immunocompromised patients |
| Adenovirus |
| Cytomegalovirus |
| Invasive aspergillosis |
| Legionella |
| Mycoplasma pneumoniae |
| Strongyloides |
| Immunocompetent patients |
| Dengue |
| Hantavirus |
| Influenza A (H1N1) |
| Leptospirosis |
| Malaria |
| Staphylococcus aureus |
* Capillaritis may or may not be present. BAL typically shows bloody or pink to orange-brown color and hemosiderin-laden macrophages (which appear after 48 hours of bleeding) with intensity of the iron staining correlating well with histologic severity of DAH.
Table 17. Diseases with foamy alveolar macrophages.
| Diseases | Comments |
|---|---|
| Acute silicosis | Periodic acid-Schiff (PAS) positive foamy macrophages is likely due to phagocytosis of cellular debris of dying macrophages that have ingested silica and of damaged epithelial cells (316). Birefringent silica particles may be present |
| Amiodarone | Amiodarone interferes with the movement of phospholipids across intracellular membranes and inhibits phospholipid catabolism via inhibition of lysosomal phospholipase 2. Thus, in alveolar macrophages the accumulation of phospholipids as foamy vacuoles stain positive with Oil Red O |
| Chronic aspiration and lipoid pneumonia | Foamy macrophages that stain positive with Oil Red O stain |
| Erdheim-Chester disease | CD68 positive (and CD1a and S100 negative) foamy macrophages (considered to contain some form of lipid) although the precise cause of the accumulation is not known (317) |
| Hypersensitivity pneumonitis | Lymphocytic dominant background with foamy macrophages (318) |
| Niemann-Pick disease | Due to decreased sphingomyelinase activity, foamy histiocytes accumulate sphingomyelin and thus stain positive with Oil Red O; the sphingomyelin stain weakly positive with PAS although this may be increased with greater acidity of the periodic acid and longer time of oxidation by the acid |
| Pulmonary alveolar proteinosis | Large foamy macrophages due to accumulation of lipoproteinaceous sediment. The vacuoles stain for both lipids (Oil Red O) and polysaccharides (PAS stain) because lipids, polysaccharides, and glycolipids associate with surfactant proteins. With GM-CSF treatment, intracellular debris and extracellular lipoproteinacious material may resolve but foamy macrophages containing ingested lipoproteinacious material may remain (298). However, clinical efficacy of GM-CSF treatment is not universally proven (319) |
| Electronic cigarette/vaping-associated lung injury | Due to an acute lung injury associated with vitamin E acetate and other additives in the inhaled product |
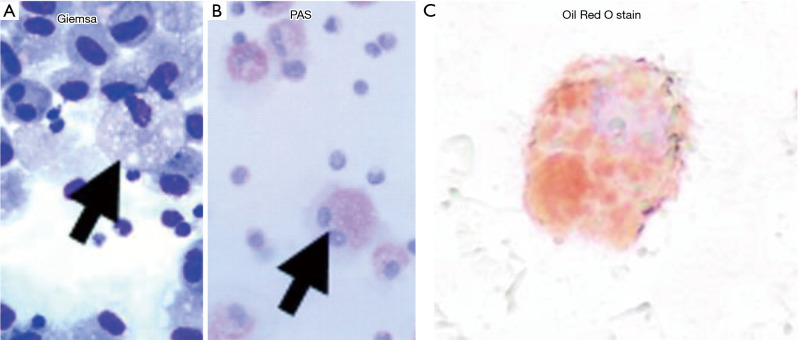
The description of “foamy macrophages” refers to the multiple, relatively large vacuoles present in the cytoplasm of BAL cells, most often the alveolar macrophages. A stain may be a “negative stain” in that it stains the structures outside of the vacuoles that comprise the intracellular “foamy” characteristics (Figure 1A,B). Since the content of the foamy vacuoles are often lipid or lipoproteinaceous material, the content of the vacuoles may be stained positively with Oil Red O (Figure 1C). Peridic acid-Schiff (PAS) stains structures outside of the vacuoles but may also stain the contents within the vacuoles if they contain glycoproteins and glycolipids since PAS stains polysaccharides.
Table 18. Diagnostic or highly suggestive BAL cellular phenotypes.
| Diseases | Key BAL fluid findings and other clinical supporting features |
|---|---|
| Acute eosinophilic pneumonia | Eosinophils >25% in the setting of acute pneumonitis. Peripheral eosinophilia may be absent or mild initially |
| Asbestosis | Iron staining of may reveal ferruginous bodies with known exposure and compatible chest imaging |
| Berylliosis | Positive BeLPT with known or suspected beryllium exposure and compatible chest imaging |
| Diffuse alveolar hemorrhage | After instillation of lavage fluid, increasing bloodier return with aspiration of serial aliquots (grossly or by RBC count). However, does not inform the specific cause of the DAH |
| Hard metal lung disease | Multinucleated giant cells with known or suspected exposure and compatible chest imaging |
| Heřmanský-Pudlák syndrome | Alveolar macrophages may show yellow-brown staining of ceroid accumulation; the ceroid material may stain weakly acid-fast positive |
| Hypersensitivity pneumonitis | Lymphocytosis >50% with known or suspected exposure (typically elevated CD8+ T cells but elevated CD4+ T cells may be seen) |
| Niemann-Pick disease | Foamy histiocytes that are PAS positive and lipid stain positive with compatible imaging of ground-glass attenuation and thickening of the interlobular septae in the lower lung zones (“crazy paving sign”). Diffuse reticular and nodular infiltrates with basal predominance and honeycombing may also be seen |
| Pulmonary alveolar microlithiasis | Presence of microliths |
| Pulmonary alveolar proteinosis | Presence of milky and turbid appearance with a thick settling layer of sediment due to the lipoproteinaceous deposits |
| Pulmonary Langerhans cell histiocytosis | ≥5% of cells positive for CD1a. S-100 positivity is supportive but less specific. Chest imaging shows cysts and nodules in an upper zone distribution in earlier phase and predominantly cysts in end-stage disease |
| Pulmonary post-transplant lymphoproliferative disorder (PTLD) | In the proper clinical context, increased B cells that are Epstein-Barr virus (EBV) positive by PCR (300,301) |
| Sarcoidosis | Lymphocyte predominant with CD4:CD8 ratio ≥2, neutrophils ≤1%, and eosinophils ≤1% may be as specific as transbronchial biopsy |
BAL, bronchoalveolar lavage; AEP, acute eosinophilic pneumonia; AIP, acute interstitial pneumonitis; ANCA, antineutrophil cytoplasmic antibodies; ARDS, acute respiratory distress syndrome; BAL, bronchoalveolar lavage; COPD, chronic obstructive pulmonary disease; CTLA-4, cytotoxic T-lymphocyte-associated protein 4; DAD, diffuse alveolar damage; DAH, diffuse alveolar hemorrhage; EGFR, epidermal growth factor receptor; GGO, ground glass opacities; HP, hypersensitivity pneumonitis; ILD, interstitial lung disease; LIP, lymphocytic interstitial pneumonitis; NSIP, non-specific interstitial pneumonitis; OP, organizing pneumonia; PAS, periodic acid-Schiff; PD-1, programmed cell death protein-1; PD-L1, programmed cell death ligand 1; PDGFR, platelet-derived growth factor receptor; PLCH, pulmonary Langerhans cell histiocytosis; VEGF, vascular endothelial growth factor.
Figure 1.
Visual detection of foamy macrophages. (A) Giemsa stain and (B) Periodic acid-Schiff (PAS) stain of BAL from a patient with pulmonary alveolar proteinosis demonstrating the “ghosts” of the foamy vacuoles [Figure modified from (298)]. A Wright-Giemsa stain is also a “negative stain” and will also accomplish the same visual effect. (C) Oil Red O stain of the BAL from a patient with electronic cigarette/vaping-associated lung injury (EVALI) showing lipid-filled vacuoles within an alveolar macrophage. Magnification: 1,000×. BAL, bronchoalveolar lavage.
BAL as a therapeutic procedure
BAL is almost exclusively used as a diagnostic tool. But a modified BAL—really more of a bronchial wash—using smaller aliquots of saline to help dislodge distal mucous plugs is likely the most common therapeutic use, especially in those with a secured airway (endotracheal tube or tracheostomy) but too debilitated to self-expectorate successfully. The best evidence for therapeutic use of BAL is for pulmonary alveolar proteinosis. In this instance, the BAL technique is modified with high volumes of sterile normal saline via a dual lumen endotracheal tube to perform a therapeutic whole lung lavage with removal of heavy lipoproteinaceous sediment from the lungs. This procedure was first described in 1963 with subsequent modifications in technique to optimize patient safety, yield of removed protein and therapeutic benefit (320). Other rare reports of therapeutic lung lavage have been described for exogenous lipoid pneumonia from milk aspiration (321) and another with kerosene aspiration (322) utilizing low volume segmental lavage with good radiographic resolution. In children with refractory Mycoplasma pneumoniae pneumonia complicated by atelectasis, therapeutic BAL was shown to significantly shorten the duration of illness, time to radiographic resolution, and length of hospital stay (323).
Conclusions
Since the first bronchial irrigation by Stitt in 1927, BAL has evolved to become an often-used diagnostic procedure throughout most of the world. With development of additional assays for microbial product (e.g., galactomannan for invasive fungal disease), immunostaining for organisms (e.g., direct fluorescent antibody for pneumocystis), and nucleic acid amplification tests for specific microbes, BAL for diagnosis of infectious disorders has made significant progress and will continue to advance further with new technologies. While differential cell count profiles and ancillary testing on BAL fluid may in themselves not be specific or diagnostic, in the proper clinical context, the BAL findings may be the deciding factor in making a confident diagnosis. For example, in a patient with home bird exposure, significant lymphocytosis on BAL and consistent imaging, a confident diagnosis of hypersensitivity pneumonitis can be made even in the absence of lung biopsy. Even when BAL results are non-diagnostic, their findings may help narrow the differential diagnosis. This review summarizes the vast array of additional characteristics and specific signature findings that can be a helpful aid to diagnosis. Herein, we present a current, succinct compilation of BAL data in a wide range of lung disease. In addition, we also listed those diseases and drug toxicities for which specific BAL data have not been reported.
In the future, it is likely that additional targeted diagnostics such as MALDI-TOF and PCR ES-M on BAL fluid will facilitate more rapid diagnosis of infectious pneumonia. Of particular interest is not only the ability to determine the etiology of infection but also to identify drug-resistant microbes. Such advances would transform the care of septic patients and also improve adherence to antibiotic stewardship. Additionally, genomic testing of BAL fluid may help clinicians differentiate patients with IPF from other forms of ILD as well as stratify patients with lung nodules into different risk groups for lung cancer. While surgical lung biopsy remains the gold standard for the diagnosis of various lung diseases, less invasive diagnostic techniques will become adopted if their yield becomes significantly more accurate. The ultimate goal would be to advance diagnostic techniques on BAL fluid to rival the sensitivity and specificity of the current gold standard of lung biopsy.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-651). EDC serves as an unpaid editorial board member of Journal of Thoracic Disease. The other author has no conflicts of interest to declare.
References
- 1.Stitt HL. Bronchial aspiration and irrigation with a hypertonic solution. J Med 1927;5:112-7. [Google Scholar]
- 2.Ahmad M, Livingston DR, Golish JA, et al. The safety of outpatient transbronchial biopsy. Chest 1986;90:403-5. 10.1378/chest.90.3.403 [DOI] [PubMed] [Google Scholar]
- 3.Drent M, Mansour K, Linssen C. Bronchoalveolar lavage in sarcoidosis. Semin Respir Crit Care Med 2007;28:486-95. 10.1055/s-2007-991521 [DOI] [PubMed] [Google Scholar]
- 4.Semenzato G, Bjermer L, Costabel U, et al. Clinical guidelines and indications for bronchoalveolar lavage (BAL): extrinsic allergic alveolitis. Eur Respir J 1990;3:945-6, 961-9. [PubMed] [Google Scholar]
- 5.Welker L, Jorres RA, Costabel U, et al. Predictive value of BAL cell differentials in the diagnosis of interstitial lung diseases. Eur Respir J 2004;24:1000-6. 10.1183/09031936.04.00101303 [DOI] [PubMed] [Google Scholar]
- 6.Sohn JW. Acute eosinophilic pneumonia. Tuberc Respir Dis (Seoul) 2013;74:51-5. 10.4046/trd.2013.74.2.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costabel U, Guzman J, Bonella F, et al. Bronchoalveolar lavage in other interstitial lung diseases. Semin Respir Crit Care Med 2007;28:514-24. 10.1055/s-2007-991525 [DOI] [PubMed] [Google Scholar]
- 8.O’Donnell R, Breen D, Wilson S, et al. Inflammatory cells in the airways in COPD. Thorax 2006;61:448-54. 10.1136/thx.2004.024463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith DL, Deshazo RD. Bronchoalveolar lavage in asthma. An update and perspective. Am Rev Respir Dis 1993;148:523-32. 10.1164/ajrccm/148.2.523 [DOI] [PubMed] [Google Scholar]
- 10.Fournier E, Tonnel AB, Gosset P, et al. Early neutrophil alveolitis after antigen inhalation in hypersensitivity pneumonitis. Chest 1985;88:563-6. 10.1378/chest.88.4.563 [DOI] [PubMed] [Google Scholar]
- 11.Nakos G, Kitsiouli EI, Tsangaris I, et al. Bronchoalveolar lavage fluid characteristics of early intermediate and late phases of ARDS. Alterations in leukocytes, proteins, PAF and surfactant components. Intensive Care Med 1998;24:296-303. 10.1007/s001340050571 [DOI] [PubMed] [Google Scholar]
- 12.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011;183:788-824. 10.1164/rccm.2009-040GL [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meyer KC, Raghu G, Baughman RP, et al. An official American Thoracic Society clinical practice guideline: the clinical utility of bronchoalveolar lavage cellular analysis in interstitial lung disease. Am J Respir Crit Care Med 2012;185:1004-14. 10.1164/rccm.201202-0320ST [DOI] [PubMed] [Google Scholar]
- 14.Kim ES, Kim EC, Lee SM, et al. Bacterial yield from quantitative cultures of bronchoalveolar lavage fluid in patients with pneumonia on antimicrobial therapy. Korean J Intern Med 2012;27:156-62. 10.3904/kjim.2012.27.2.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mok JH, Eom JS, Jo EJ, et al. Clinical utility of rapid pathogen identification using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry in ventilated patients with pneumonia: A pilot study. Respirology 2016;21:321-8. 10.1111/resp.12677 [DOI] [PubMed] [Google Scholar]
- 16.Ullberg M, Luthje P, Molling P, et al. Broad-Range Detection of Microorganisms Directly from Bronchoalveolar Lavage Specimens by PCR/Electrospray Ionization-Mass Spectrometry. PLoS One 2017;12:e0170033. 10.1371/journal.pone.0170033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Y, Sun B, Tang X, et al. Application of metagenomic next-generation sequencing for bronchoalveolar lavage diagnostics in critically ill patients. Eur J Clin Microbiol Infect Dis 2020;39:369-74. 10.1007/s10096-019-03734-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pendleton KM, Erb-Downward JR, Bao Y, et al. Rapid Pathogen Identification in Bacterial Pneumonia Using Real-Time Metagenomics. Am J Respir Crit Care Med 2017;196:1610-2. 10.1164/rccm.201703-0537LE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Young JC, Chehoud C, Bittinger K, et al. Viral metagenomics reveal blooms of anelloviruses in the respiratory tract of lung transplant recipients. Am J Transplant 2015;15:200-9. 10.1111/ajt.13031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneeberger PHH, Prescod J, Levy L, et al. Microbiota analysis optimization for human bronchoalveolar lavage fluid. Microbiome 2019;7:141. 10.1186/s40168-019-0755-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stanzel F. Bronchoalveolar lavage. In: Ernst A, Herth FJF. editors. Principles and Practice of Interventional Pulmonology. New York: Springer Science + Business Media, 2012:165-76. [Google Scholar]
- 22.Klech H, Pohl W. Technical Recommendations and Guidelines for Bronchoalveolar Lavage (BAL). Report of the European Society of Pneumonology Task Group. Eur Respir J 1989;2:561-85. [PubMed] [Google Scholar]
- 23.Du Rand IA, Blaikley J, Booton R, et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax 2013;68 Suppl 1:i1-i44. 10.1136/thoraxjnl-2013-203618 [DOI] [PubMed] [Google Scholar]
- 24.Dransfield MT, Garver RI, Weill D. Standardized guidelines for surveillance bronchoscopy reduce complications in lung transplant recipients. J Heart Lung Transplant 2004;23:110-4. 10.1016/S1053-2498(03)00098-6 [DOI] [PubMed] [Google Scholar]
- 25.Hodge SJ, Hodge GL, Holmes M, et al. Flow cytometric characterization of cell populations in bronchoalveolar lavage and bronchial brushings from patients with chronic obstructive pulmonary disease. Cytometry B Clin Cytom 2004;61:27-34. 10.1002/cyto.b.20020 [DOI] [PubMed] [Google Scholar]
- 26.Conte BA, Laforet EG. The role of the topical anesthetic agent in modifying bacteriologic data obtained by bronchoscopy. N Engl J Med 1962;267:957-60. 10.1056/NEJM196211082671903 [DOI] [PubMed] [Google Scholar]
- 27.Strange C, Barbarash RA, Heffner JE. Lidocaine concentrations in bronchoscopic specimens. Chest 1988;93:547-9. 10.1378/chest.93.3.547 [DOI] [PubMed] [Google Scholar]
- 28.Bronchoalveolar lavage constituents in healthy individuals, idiopathic pulmonary fibrosis, and selected comparison groups. The BAL Cooperative Group Steering Committee. Am Rev Respir Dis 1990;141:S169-202. [DOI] [PubMed] [Google Scholar]
- 29.Heron M, Grutters JC, ten Dam-Molenkamp KM, et al. Bronchoalveolar lavage cell pattern from healthy human lung. Clin Exp Immunol 2012;167:523-31. 10.1111/j.1365-2249.2011.04529.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jouneau S, Poineuf JS, Minjolle S, et al. Which patients should be tested for viruses on bronchoalveolar lavage fluid? Eur J Clin Microbiol Infect Dis 2013;32:671-7. 10.1007/s10096-012-1791-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karimi R, Tornling G, Grunewald J, et al. Cell recovery in bronchoalveolar lavage fluid in smokers is dependent on cumulative smoking history. PLoS One 2012;7:e34232. 10.1371/journal.pone.0034232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greenberger PA, Smith LJ, Hsu CC, et al. Analysis of bronchoalveolar lavage in allergic bronchopulmonary aspergillosis: divergent responses of antigen-specific antibodies and total IgE. J Allergy Clin Immunol 1988;82:164-70. 10.1016/0091-6749(88)90995-5 [DOI] [PubMed] [Google Scholar]
- 33.Kono Y, Tsushima K, Yamaguchi K, et al. The utility of galactomannan antigen in the bronchial washing and serum for diagnosing pulmonary aspergillosis. Respir Med 2013;107:1094-100. 10.1016/j.rmed.2013.04.007 [DOI] [PubMed] [Google Scholar]
- 34.Maestrelli P, Saetta M, Di Stefano A, et al. Comparison of leukocyte counts in sputum, bronchial biopsies, and bronchoalveolar lavage. Am J Respir Crit Care Med 1995;152:1926-31. 10.1164/ajrccm.152.6.8520757 [DOI] [PubMed] [Google Scholar]
- 35.Konstan MW, Hilliard KA, Norvell TM, et al. Bronchoalveolar lavage findings in cystic fibrosis patients with stable, clinically mild lung disease suggest ongoing infection and inflammation. Am J Respir Crit Care Med 1994;150:448-54. 10.1164/ajrccm.150.2.8049828 [DOI] [PubMed] [Google Scholar]
- 36.Burmester H, Brinkmann F, Schwerk N, et al. Bronchoscopic findings in children with primary ciliary dyskinesia: Most but not all patients have bacterial bronchitis. ERJ 2012;40. [Google Scholar]
- 37.Torre O, Harari S. The diagnosis of cystic lung diseases: a role for bronchoalveolar lavage and transbronchial biopsy? Respir Med 2010;104 Suppl 1:S81-5. 10.1016/j.rmed.2010.03.021 [DOI] [PubMed] [Google Scholar]
- 38.Bonetti F, Chiodera PL, Pea M, et al. Transbronchial biopsy in lymphangiomyomatosis of the lung. HMB45 for diagnosis. Am J Surg Pathol 1993;17:1092-102. 10.1097/00000478-199311000-00002 [DOI] [PubMed] [Google Scholar]
- 39.Meyer FJ, Teschler H, Schnabel R, et al. Bronchoalveolar lavage cytology in pulmonary fibrosis associated with neurofibromatosis. Respir Med 1996;90:365-7. 10.1016/S0954-6111(96)90135-3 [DOI] [PubMed] [Google Scholar]
- 40.Auerswald U, Barth J, Magnussen H. Value of CD-1-positive cells in bronchoalveolar lavage fluid for the diagnosis of pulmonary histiocytosis X. Lung 1991;169:305-9. 10.1007/BF02714167 [DOI] [PubMed] [Google Scholar]
- 41.Baqir M, Vassallo R, Maldonado F, et al. Utility of bronchoscopy in pulmonary Langerhans cell histiocytosis. J Bronchology Interv Pulmonol 2013;20:309-12. 10.1097/LBR.0000000000000021 [DOI] [PubMed] [Google Scholar]
- 42.Tazi A. Adult pulmonary Langerhans’ cell histiocytosis. Eur Respir J 2006;27:1272-85. 10.1183/09031936.06.00024004 [DOI] [PubMed] [Google Scholar]
- 43.Geissmann F, Lepelletier Y, Fraitag S, et al. Differentiation of Langerhans cells in Langerhans cell histiocytosis. Blood 2001;97:1241-8. 10.1182/blood.V97.5.1241 [DOI] [PubMed] [Google Scholar]
- 44.Flint A, Lloyd RV, Colby TV, et al. Pulmonary histiocytosis X. Immunoperoxidase staining for HLA-DR antigen and S100 protein. Arch Pathol Lab Med 1986;110:930-3. [PubMed] [Google Scholar]
- 45.Travis WD, Borok Z, Roum JH, et al. Pulmonary Langerhans cell granulomatosis (histiocytosis X). A clinicopathologic study of 48 cases. Am J Surg Pathol 1993;17:971-86. 10.1097/00000478-199310000-00002 [DOI] [PubMed] [Google Scholar]
- 46.Hamzaoui K, Berraies A, Kaabachi W, et al. Pulmonary manifestations in Behcet disease: impaired natural killer cells activity. Multidiscip Respir Med 2013;8:29. 10.1186/2049-6958-8-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bertorelli G, Pesci A, Manganelli P, et al. Subclinical pulmonary involvement in essential mixed cryoglobulinemia assessed by bronchoalveolar lavage. Chest 1991;100:1478-9. 10.1378/chest.100.5.1478b [DOI] [PubMed] [Google Scholar]
- 48.Manganelli P, Salaffi F, Subiaco S, et al. Bronchoalveolar lavage in mixed cryoglobulinaemia associated with hepatitis C virus. Br J Rheumatol 1996;35:978-82. 10.1093/rheumatology/35.10.978 [DOI] [PubMed] [Google Scholar]
- 49.Allen JN, Davis WB. Eosinophilic lung diseases. Am J Respir Crit Care Med 1994;150:1423-38. 10.1164/ajrccm.150.5.7952571 [DOI] [PubMed] [Google Scholar]
- 50.Hoffman GS, Sechler JM, Gallin JI, et al. Bronchoalveolar lavage analysis in Wegener’s granulomatosis. A method to study disease pathogenesis. Am Rev Respir Dis 1991;143:401-7. 10.1164/ajrccm/143.2.401 [DOI] [PubMed] [Google Scholar]
- 51.Schnabel A, Reuter M, Gloeckner K, et al. Bronchoalveolar lavage cell profiles in Wegener’s granulomatosis. Respir Med 1999;93:498-506. 10.1016/S0954-6111(99)90093-8 [DOI] [PubMed] [Google Scholar]
- 52.Ramsey J, Amari M, Kantrow SP. Pulmonary vasculitis: clinical presentation, differential diagnosis, and management. Curr Rheumatol Rep 2010;12:420-8. 10.1007/s11926-010-0136-8 [DOI] [PubMed] [Google Scholar]
- 53.Philit F, Etienne-Mastroianni B, Parrot A, et al. Idiopathic acute eosinophilic pneumonia: a study of 22 patients. Am J Respir Crit Care Med 2002;166:1235-9. 10.1164/rccm.2112056 [DOI] [PubMed] [Google Scholar]
- 54.Pope-Harman AL, Davis WB, Allen ED, et al. Acute eosinophilic pneumonia. A summary of 15 cases and review of the literature. Medicine (Baltimore) 1996;75:334-42. 10.1097/00005792-199611000-00004 [DOI] [PubMed] [Google Scholar]
- 55.Bonaccorsi A, Cancellieri A, Chilosi M, et al. Acute interstitial pneumonia: report of a series. Eur Respir J 2003;21:187-91. 10.1183/09031936.03.00297002 [DOI] [PubMed] [Google Scholar]
- 56.Pesci A, Bertorelli G, Manganelli P, et al. Bronchoalveolar lavage in chronic eosinophilic pneumonia. Analysis of six cases in comparison with other interstitial lung diseases. Respiration 1988;54 Suppl 1:16-22. 10.1159/000195475 [DOI] [PubMed] [Google Scholar]
- 57.Lazor R, Vandevenne A, Pelletier A, et al. Cryptogenic organizing pneumonia. Characteristics of relapses in a series of 48 patients. The Groupe d’Etudes et de Recherche sur les Maladles "Orphelines" Pulmonaires (GERM"O"P). Am J Respir Crit Care Med 2000;162:571-7. 10.1164/ajrccm.162.2.9909015 [DOI] [PubMed] [Google Scholar]
- 58.Poletti V, Cazzato S, Minicuci N, et al. The diagnostic value of bronchoalveolar lavage and transbronchial lung biopsy in cryptogenic organizing pneumonia. Eur Respir J 1996;9:2513-6. 10.1183/09031936.96.09122513 [DOI] [PubMed] [Google Scholar]
- 59.Cohen AJ, King TE, Jr, Downey GP. Rapidly progressive bronchiolitis obliterans with organizing pneumonia. Am J Respir Crit Care Med 1994;149:1670-5. 10.1164/ajrccm.149.6.8004328 [DOI] [PubMed] [Google Scholar]
- 60.Cazzato S, Zompatori M, Baruzzi G, et al. Bronchiolitis obliterans-organizing pneumonia: an Italian experience. Respir Med 2000;94:702-8. 10.1053/rmed.2000.0805 [DOI] [PubMed] [Google Scholar]
- 61.Ravaglia C, Tomassetti S, Casoni G, et al. BAL findings in desquamative interstitial pneumonia (DIP) and other idiopathic interstitial pneumonia (IIP). ERJ 2014;44. [Google Scholar]
- 62.Wessendorf T, Bonella F, Theegarten D, et al. Usefulness of bronchoalveolar lavage in the diagnosis of desquamative interstitial pneumonia. ERJ 2014;44. [Google Scholar]
- 63.Bouvry D, Mouthon L, Brillet PY, et al. Granulomatosis-associated common variable immunodeficiency disorder: a case-control study versus sarcoidosis. Eur Respir J 2013;41:115-22. 10.1183/09031936.00189011 [DOI] [PubMed] [Google Scholar]
- 64.Manganelli P, Bertorelli G, Fietta P, et al. Interstitial lung disease in connective tissue inflammation. Evaluation by means of bronchoalveolar lavage. Recenti Prog Med 1988;79:424-9. [PubMed] [Google Scholar]
- 65.Ikeda S, Arita M, Morita M, et al. Interstitial lung disease in clinically amyopathic dermatomyositis with and without anti-MDA-5 antibody: to lump or split? BMC Pulm Med 2015;15:159. 10.1186/s12890-015-0154-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mukae H, Ishimoto H, Sakamoto N, et al. Clinical differences between interstitial lung disease associated with clinically amyopathic dermatomyositis and classic dermatomyositis. Chest 2009;136:1341-7. 10.1378/chest.08-2740 [DOI] [PubMed] [Google Scholar]
- 67.Ishioka S, Inyaku K, Shirotani Y, et al. Bronchoalveolar lavage fluid findings in rheumatoid arthritis. Nihon Kyobu Shikkan Gakkai Zasshi 1992;30:614-8. [PubMed] [Google Scholar]
- 68.Pesci A, Bertorelli G, Manganelli P, et al. Bronchoalveolar lavage analysis of interstitial lung disease in CREST syndrome. Clin Exp Rheumatol 1986;4:121-4. [PubMed] [Google Scholar]
- 69.Salaffi F, Manganelli P, Carotti M, et al. A longitudinal study of pulmonary involvement in primary Sjogren’s syndrome: relationship between alveolitis and subsequent lung changes on high-resolution computed tomography. Br J Rheumatol 1998;37:263-9. 10.1093/rheumatology/37.3.263 [DOI] [PubMed] [Google Scholar]
- 70.Behr J, Vogelmeier C, Beinert T, et al. Bronchoalveolar lavage for evaluation and management of scleroderma disease of the lung. Am J Respir Crit Care Med 1996;154:400-6. 10.1164/ajrccm.154.2.8756813 [DOI] [PubMed] [Google Scholar]
- 71.Kowal-Bielecka O, Kowal K, Highland KB, et al. Bronchoalveolar lavage fluid in scleroderma interstitial lung disease: technical aspects and clinical correlations: review of the literature. Semin Arthritis Rheum 2010;40:73-88. 10.1016/j.semarthrit.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 72.Silver RM, Miller KS, Kinsella MB, et al. Evaluation and management of scleroderma lung disease using bronchoalveolar lavage. Am J Med 1990;88:470-6. 10.1016/0002-9343(90)90425-D [DOI] [PubMed] [Google Scholar]
- 73.Cha SI, Fessler MB, Cool CD, et al. Lymphoid interstitial pneumonia: clinical features, associations and prognosis. Eur Respir J 2006;28:364-9. 10.1183/09031936.06.00076705 [DOI] [PubMed] [Google Scholar]
- 74.Pisani RJ, Witzig TE, Li CY, et al. Confirmation of lymphomatous pulmonary involvement by immunophenotypic and gene rearrangement analysis of bronchoalveolar lavage fluid. Mayo Clin Proc 1990;65:651-6. 10.1016/S0025-6196(12)65127-1 [DOI] [PubMed] [Google Scholar]
- 75.Gülhan B, Ozçelik U, Gürakan F, et al. Different features of lung involvement in Niemann-Pick disease and Gaucher disease. Respir Med 2012;106:1278-85. 10.1016/j.rmed.2012.06.014 [DOI] [PubMed] [Google Scholar]
- 76.Shimizu S, Yoshinouchi T, Ohtsuki Y, et al. The appearance of S-100 protein-positive dendritic cells and the distribution of lymphocyte subsets in idiopathic nonspecific interstitial pneumonia. Respir Med 2002;96:770-6. 10.1053/rmed.2002.1345 [DOI] [PubMed] [Google Scholar]
- 77.Veeraraghavan S, Latsi PI, Wells AU, et al. BAL findings in idiopathic nonspecific interstitial pneumonia and usual interstitial pneumonia. Eur Respir J 2003;22:239-44. 10.1183/09031936.03.00105202 [DOI] [PubMed] [Google Scholar]
- 78.Nagai S, Kitaichi M, Itoh H, et al. Idiopathic nonspecific interstitial pneumonia/fibrosis: comparison with idiopathic pulmonary fibrosis and BOOP. Eur Respir J 1998;12:1010-9. 10.1183/09031936.98.12051010 [DOI] [PubMed] [Google Scholar]
- 79.Costabel U, Guzman J. Bronchoalveolar lavage in interstitial lung disease. Curr Opin Pulm Med 2001;7:255-61. 10.1097/00063198-200109000-00002 [DOI] [PubMed] [Google Scholar]
- 80.Oda T, Ogura T, Kitamura H, et al. Distinct characteristics of pleuroparenchymal fibroelastosis with usual interstitial pneumonia compared with idiopathic pulmonary fibrosis. Chest 2014;146:1248-55. 10.1378/chest.13-2866 [DOI] [PubMed] [Google Scholar]
- 81.Sieminska A, Kuziemski K. Respiratory bronchiolitis-interstitial lung disease. Orphanet J Rare Dis 2014;9:106. 10.1186/s13023-014-0106-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ohshimo S, Bonella F, Cui A, et al. Significance of bronchoalveolar lavage for the diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2009;179:1043-7. 10.1164/rccm.200808-1313OC [DOI] [PubMed] [Google Scholar]
- 83.Kinder BW, Brown KK, Schwarz MI, et al. Baseline BAL neutrophilia predicts early mortality in idiopathic pulmonary fibrosis. Chest 2008;133:226-32. 10.1378/chest.07-1948 [DOI] [PubMed] [Google Scholar]
- 84.Vathesatogkit P, Harkin TJ, Addrizzo-Harris DJ, et al. Clinical correlation of asbestos bodies in BAL fluid. Chest 2004;126:966-71. 10.1378/chest.126.3.966 [DOI] [PubMed] [Google Scholar]
- 85.Wallace JM, Oishi JS, Barbers RG, et al. Bronchoalveolar lavage cell and lymphocyte phenotype profiles in healthy asbestos-exposed shipyard workers. Am Rev Respir Dis 1989;139:33-8. 10.1164/ajrccm/139.1.33 [DOI] [PubMed] [Google Scholar]
- 86.Corhay JL, Delavignette JP, Bury T, et al. Occult exposure to asbestos in steel workers revealed by bronchoalveolar lavage. Arch Environ Health 1990;45:278-82. 10.1080/00039896.1990.10118746 [DOI] [PubMed] [Google Scholar]
- 87.Karjalainen A, Anttila S, Mantyla T, et al. Asbestos bodies in bronchoalveolar lavage fluid in relation to occupational history. Am J Ind Med 1994;26:645-54. 10.1002/ajim.4700260507 [DOI] [PubMed] [Google Scholar]
- 88.Balmes JR, Abraham JL, Dweik RA, et al. An official American Thoracic Society statement: diagnosis and management of beryllium sensitivity and chronic beryllium disease. Am J Respir Crit Care Med 2014;190:e34-59. 10.1164/rccm.201409-1722ST [DOI] [PubMed] [Google Scholar]
- 89.Baur X, Borsch-Galetke E, Raulf M, et al. Occupational-type exposure tests and bronchoalveolar lavage analyses in two patients with byssinosis and two asymptomatic cotton workers. Int Arch Occup Environ Health 1993;65:141-6. 10.1007/BF00405734 [DOI] [PubMed] [Google Scholar]
- 90.Schreiber J, Koschel D, Kekow J, et al. Rheumatoid pneumoconiosis (Caplan’s syndrome). Eur J Intern Med 2010;21:168-72. 10.1016/j.ejim.2010.02.004 [DOI] [PubMed] [Google Scholar]
- 91.Castranova V, Vallyathan V. Silicosis and coal workers’ pneumoconiosis. Environ Health Perspect 2000;108 Suppl 4:675-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kayacan O, Beder S, Karnak D. Cellular profile of bronchoalveolar lavage fluid in Turkish miners. Postgrad Med J 2003;79:527-30. 10.1136/pmj.79.935.527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vallyathan V, Goins M, Lapp LN, et al. Changes in bronchoalveolar lavage indices associated with radiographic classification in coal miners. Am J Respir Crit Care Med 2000;162:958-65. 10.1164/ajrccm.162.3.9909074 [DOI] [PubMed] [Google Scholar]
- 94.Mizutani RF, Goncalves C, Leao BD, et al. Hard metal lung disease - Role of bronchoalveolar lavage in the diagnosis. ERJ 2014;44. [Google Scholar]
- 95.Mizutani RF, Terra-Filho M, Lima E, et al. Hard metal lung disease: a case series. J Bras Pneumol 2016;42:447-52. 10.1590/s1806-37562016000000260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nemery B, Verbeken EK, Demedts M. Giant cell interstitial pneumonia (hard metal lung disease, cobalt lung). Semin Respir Crit Care Med 2001;22:435-48. 10.1055/s-2001-17386 [DOI] [PubMed] [Google Scholar]
- 97.Ohori NP, Sciurba FC, Owens GR, et al. Giant-cell interstitial pneumonia and hard-metal pneumoconiosis. A clinicopathologic study of four cases and review of the literature. Am J Surg Pathol 1989;13:581-7. 10.1097/00000478-198907000-00006 [DOI] [PubMed] [Google Scholar]
- 98.Caillaud DM, Vergnon JM, Madroszyk A, et al. Bronchoalveolar lavage in hypersensitivity pneumonitis: a series of 139 patients. Inflamm Allergy Drug Targets 2012;11:15-9. 10.2174/187152812798889330 [DOI] [PubMed] [Google Scholar]
- 99.Lacasse Y, Cormier Y. Hypersensitivity pneumonitis. Orphanet J Rare Dis 2006;1:25. 10.1186/1750-1172-1-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yoshizawa Y, Ohtani Y, Hayakawa H, et al. Chronic hypersensitivity pneumonitis in Japan: a nationwide epidemiologic survey. J Allergy Clin Immunol 1999;103:315-20. 10.1016/S0091-6749(99)70507-5 [DOI] [PubMed] [Google Scholar]
- 101.Ratjen F, Costabel U, Griese M, et al. Bronchoalveolar lavage fluid findings in children with hypersensitivity pneumonitis. Eur Respir J 2003;21:144-8. 10.1183/09031936.03.00035703a [DOI] [PubMed] [Google Scholar]
- 102.Bandici RM, Bandici R, Cioban GC, et al. Lung Siderosis. Med Con 2015;10:43-7. [Google Scholar]
- 103.Khalid I, Khalid TJ, Jennings JH. A welder with pneumosiderosis: a case report. Cases J 2009;2:6639. 10.1186/1757-1626-2-6639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yoshii C, Matsuyama T, Takazawa A, et al. Welder’s pneumoconiosis: diagnostic usefulness of high-resolution computed tomography and ferritin determinations in bronchoalveolar lavage fluid. Intern Med 2002;41:1111-7. 10.2169/internalmedicine.41.1111 [DOI] [PubMed] [Google Scholar]
- 105.Christman JW, Emerson RJ, Graham WG, et al. Mineral dust and cell recovery from the bronchoalveolar lavage of healthy Vermont granite workers. Am Rev Respir Dis 1985;132:393-9. [DOI] [PubMed] [Google Scholar]
- 106.Hnizdo E, Murray J, Sluis-Cremer GK, et al. Correlation between radiological and pathological diagnosis of silicosis: an autopsy population based study. Am J Ind Med 1993;24:427-45. 10.1002/ajim.4700240408 [DOI] [PubMed] [Google Scholar]
- 107.Nugent KM, Dodson RF, Idell S, et al. The utility of bronchoalveolar lavage and transbronchial lung biopsy combined with energy-dispersive X-ray analysis in the diagnosis of silicosis. Am Rev Respir Dis 1989;140:1438-41. 10.1164/ajrccm/140.5.1438 [DOI] [PubMed] [Google Scholar]
- 108.Morgan GW, Breit SN. Radiation and the lung: a reevaluation of the mechanisms mediating pulmonary injury. Int J Radiat Oncol Biol Phys 1995;31:361-9. 10.1016/0360-3016(94)00477-3 [DOI] [PubMed] [Google Scholar]
- 109.Nakayama Y, Makino S, Fukuda Y, et al. Activation of lavage lymphocytes in lung injuries caused by radiotherapy for lung cancer. Int J Radiat Oncol Biol Phys 1996;34:459-67. 10.1016/0360-3016(95)02101-9 [DOI] [PubMed] [Google Scholar]
- 110.Kadmon G, Levy I, Mandelboim M, et al. Polymerase-chain-reaction-based diagnosis of viral pulmonary infections in immunocompromised children. Acta Paediatr 2013;102:e263-8. 10.1111/apa.12207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Campbell SJ, Kynyk JA, Davis JA. Disseminated adenovirus infection causing severe ARDS. BMJ Case Rep 2017;2017. [DOI] [PMC free article] [PubMed]
- 112.Ogimi C, Waghmare AA, Kuypers JM, et al. Clinical Significance of Human Coronavirus in Bronchoalveolar Lavage Samples From Hematopoietic Cell Transplant Recipients and Patients With Hematologic Malignancies. Clin Infect Dis 2017;64:1532-9. 10.1093/cid/cix160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Memish ZA, Al-Tawfiq JA, Makhdoom HQ, et al. Respiratory tract samples, viral load, and genome fraction yield in patients with Middle East respiratory syndrome. J Infect Dis 2014;210:1590-4. 10.1093/infdis/jiu292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Liao M, Liu Y, Yuan J, et al. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat Med 2020;26:842-4. 10.1038/s41591-020-0901-9 [DOI] [PubMed] [Google Scholar]
- 115.Tan SK, Burgener EB, Waggoner JJ, et al. Molecular and Culture-Based Bronchoalveolar Lavage Fluid Testing for the Diagnosis of Cytomegalovirus Pneumonitis. Open Forum Infect Dis 2016;3:ofv212. 10.1093/ofid/ofv212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sommerwerck U, Rabis T, Anhenn O, et al. Cytomegalovirus (CMV) infection - Correlation between CMV-DNA PCR in bronchoalveolar lavage (BAL), CMV pp65 antigen load in PBMCs and clinical symptoms in lung transplant recipients. ERJ 2011;38.
- 117.Levy H, Simpson SQ. Hantavirus pulmonary syndrome. Am J Respir Crit Care Med 1994;149:1710-3. 10.1164/ajrccm.149.6.8004332 [DOI] [PubMed] [Google Scholar]
- 118.Nolte KB, Feddersen RM, Foucar K, et al. Hantavirus pulmonary syndrome in the United States: a pathological description of a disease caused by a new agent. Hum Pathol 1995;26:110-20. 10.1016/0046-8177(95)90123-X [DOI] [PubMed] [Google Scholar]
- 119.Rasmuson J, Pourazar J, Linderholm M, et al. Presence of activated airway T lymphocytes in human puumala hantavirus disease. Chest 2011;140:715-22. 10.1378/chest.10-2791 [DOI] [PubMed] [Google Scholar]
- 120.Rasmuson J, Pourazar J, Mohamed N, et al. Cytotoxic immune responses in the lungs correlate to disease severity in patients with hantavirus infection. Eur J Clin Microbiol Infect Dis 2016;35:713-21. 10.1007/s10096-016-2592-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gizzi M, Delaere B, Weynand B, et al. Another case of "European hantavirus pulmonary syndrome" with severe lung, prior to kidney, involvement, and diagnosed by viral inclusions in lung macrophages. Eur J Clin Microbiol Infect Dis 2013;32:1341-5. 10.1007/s10096-013-1885-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Roig IL, Musher DM, Tweardy DJ. Severe pulmonary involvement in a case attributed to domestically acquired Seoul hantavirus in the United States. Clin Infect Dis 2012;54:91-4. 10.1093/cid/cir748 [DOI] [PubMed] [Google Scholar]
- 123.Das S, Miller RF. Lymphocytic interstitial pneumonitis in HIV infected adults. Sex Transm Infect 2003;79:88-93. 10.1136/sti.79.2.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Doffman SR, Miller RF. Interstitial lung disease in HIV. Clin Chest Med 2013;34:293-306. 10.1016/j.ccm.2013.01.012 [DOI] [PubMed] [Google Scholar]
- 125.Griffiths MH, Miller RF, Semple SJ. Interstitial pneumonitis in patients infected with the human immunodeficiency virus. Thorax 1995;50:1141-6. 10.1136/thx.50.11.1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sattler F, Nichols L, Hirano L, et al. Nonspecific interstitial pneumonitis mimicking Pneumocystis carinii pneumonia. Am J Respir Crit Care Med 1997;156:912-7. 10.1164/ajrccm.156.3.9612050 [DOI] [PubMed] [Google Scholar]
- 127.van den Hoogen BG, van Doornum GJ, Fockens JC, et al. Prevalence and clinical symptoms of human metapneumovirus infection in hospitalized patients. J Infect Dis 2003;188:1571-7. 10.1086/379200 [DOI] [PubMed] [Google Scholar]
- 128.Vargas SO, Kozakewich HP, Perez-Atayde AR, et al. Pathology of human metapneumovirus infection: insights into the pathogenesis of a newly identified respiratory virus. Pediatr Dev Pathol 2004;7:478-86; discussion 421. 10.1007/s10024-004-1011-2 [DOI] [PubMed] [Google Scholar]
- 129.Hunt DP, Muse VV, Pitman MB. Case records of the Massachusetts General Hospital. Case 12-2013. An 18-year-old woman with pulmonary infiltrates and respiratory failure. N Engl J Med 2013;368:1537-45. 10.1056/NEJMcpc1209608 [DOI] [PubMed] [Google Scholar]
- 130.Sabugo F, Espinoza-Araya R, Meneses MF, et al. Acute herpes simplex virus 1 pneumonitis in a patient with systemic lupus erythematosus. J Clin Rheumatol 2014;20:42-4. 10.1097/RHU.0000000000000060 [DOI] [PubMed] [Google Scholar]
- 131.Tachikawa R, Tomii K, Seo R, et al. Detection of herpes viruses by multiplex and real-time polymerase chain reaction in bronchoalveolar lavage fluid of patients with acute lung injury or acute respiratory distress syndrome. Respiration 2014;87:279-86. 10.1159/000355200 [DOI] [PubMed] [Google Scholar]
- 132.Linssen CF, Jacobs JA, Stelma FF, et al. Herpes simplex virus load in bronchoalveolar lavage fluid is related to poor outcome in critically ill patients. Intensive Care Med 2008;34:2202-9. 10.1007/s00134-008-1231-4 [DOI] [PubMed] [Google Scholar]
- 133.Luyt CE, Combes A, Deback C, et al. Herpes simplex virus lung infection in patients undergoing prolonged mechanical ventilation. Am J Respir Crit Care Med 2007;175:935-42. 10.1164/rccm.200609-1322OC [DOI] [PubMed] [Google Scholar]
- 134.Faverio P, Aliberti S, Ezekiel C, et al. Influenza A/H1N1 Severe Pneumonia: Novel Morphocytological Findings in Bronchoalveolar Lavage. Interdiscip Perspect Infect Dis 2014;2014:470825. 10.1155/2014/470825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Pokharel S, Merickel CR, Alatassi H. Parainfluenza virus-3-induced cytopathic effects on lung tissue and bronchoalveolar lavage fluid in a bone marrow transplant recipient: a case report. Diagn Cytopathol 2014;42:521-4. 10.1002/dc.22951 [DOI] [PubMed] [Google Scholar]
- 136.McNamara PS, Ritson P, Selby A, et al. Bronchoalveolar lavage cellularity in infants with severe respiratory syncytial virus bronchiolitis. Arch Dis Child 2003;88:922-6. 10.1136/adc.88.10.922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shirai T, Sano K, Matsuyama S, et al. Varicella pneumonia in a healthy adult presenting with severe respiratory failure. Intern Med 1996;35:315-8. 10.2169/internalmedicine.35.315 [DOI] [PubMed] [Google Scholar]
- 138.Cowl CT, Prakash UB, Shawn Mitchell P, et al. Varicella-zoster virus detection by polymerase chain reaction using bronchoalveolar lavage specimens. Am J Respir Crit Care Med 2000;162:753-4. 10.1164/ajrccm.162.2.9912039 [DOI] [PubMed] [Google Scholar]
- 139.Rozental T, Mascarenhas LF, Rozenbaum R, et al. Coxiella burnetii, the agent of Q fever in Brazil: its hidden role in seronegative arthritis and the importance of molecular diagnosis based on the repetitive element IS1111 associated with the transposase gene. Mem Inst Oswaldo Cruz 2012;107:695-7. 10.1590/S0074-02762012000500021 [DOI] [PubMed] [Google Scholar]
- 140.Trisolini R, Lazzari Agli L, Cancellieri A, et al. Bronchoalveolar lavage findings in severe community-acquired pneumonia due to Legionella pneumophila serogroup 1. Respir Med 2004;98:1222-6. 10.1016/j.rmed.2004.04.015 [DOI] [PubMed] [Google Scholar]
- 141.Hayden RT, Uhl JR, Qian X, et al. Direct detection of Legionella species from bronchoalveolar lavage and open lung biopsy specimens: comparison of LightCycler PCR, in situ hybridization, direct fluorescence antigen detection, and culture. J Clin Microbiol 2001;39:2618-26. 10.1128/JCM.39.7.2618-2626.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Bentz JS, Carroll K, Ward JH, et al. Acid-fast-positive Legionella pneumophila: a possible pitfall in the cytologic diagnosis of mycobacterial infection in pulmonary specimens. Diagn Cytopathol 2000;22:45-8. [DOI] [PubMed] [Google Scholar]
- 143.Helmerhorst HJ, van Tol EN, Tuinman PR, et al. Severe pulmonary manifestation of leptospirosis. Neth J Med 2012;70:215-21. [PubMed] [Google Scholar]
- 144.Marchiori E, Lourenco S, Setubal S, et al. Clinical and imaging manifestations of hemorrhagic pulmonary leptospirosis: a state-of-the-art review. Lung 2011;189:1-9. 10.1007/s00408-010-9273-0 [DOI] [PubMed] [Google Scholar]
- 145.Paganin F, Gauzere BA, Lugagne N, et al. Bronchoalveolar lavage in rapid diagnosis of leptospirosis. Lancet 1996;347:1562-3. 10.1016/S0140-6736(96)90719-9 [DOI] [PubMed] [Google Scholar]
- 146.Dolhnikoff M, Mauad T, Bethlem EP, et al. Pathology and pathophysiology of pulmonary manifestations in leptospirosis. Braz J Infect Dis 2007;11:142-8. 10.1590/S1413-86702007000100029 [DOI] [PubMed] [Google Scholar]
- 147.Koh YY, Park Y, Lee HJ, et al. Levels of interleukin-2, interferon-gamma, and interleukin-4 in bronchoalveolar lavage fluid from patients with Mycoplasma pneumonia: implication of tendency toward increased immunoglobulin E production. Pediatrics 2001;107:E39. 10.1542/peds.107.3.e39 [DOI] [PubMed] [Google Scholar]
- 148.Schmitt BH, Sloan LM, Patel R. Real-time PCR detection of Mycoplasma pneumoniae in respiratory specimens. Diagn Microbiol Infect Dis 2013;77:202-5. 10.1016/j.diagmicrobio.2013.07.016 [DOI] [PubMed] [Google Scholar]
- 149.Mishra R, Cano E, Venkatram S, et al. An interesting case of mycoplasma pneumonia associated multisystem involvement and diffuse alveolar hemorrhage. Respir Med Case Rep 2017;21:78-81. 10.1016/j.rmcr.2017.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Johansson A, Berglund L, Eriksson U, et al. Comparative analysis of PCR versus culture for diagnosis of ulceroglandular tularemia. J Clin Microbiol 2000;38:22-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Boersma WG, Erjavec Z, van der Werf TS, et al. Bronchoscopic diagnosis of pulmonary infiltrates in granulocytopenic patients with hematologic malignancies: BAL versus PSB and PBAL. Respir Med 2007;101:317-25. 10.1016/j.rmed.2006.04.021 [DOI] [PubMed] [Google Scholar]
- 152.Nguyen MH, Jaber R, Leather HL, et al. Use of bronchoalveolar lavage to detect galactomannan for diagnosis of pulmonary aspergillosis among nonimmunocompromised hosts. J Clin Microbiol 2007;45:2787-92. 10.1128/JCM.00716-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Martynowicz MA, Prakash UB. Pulmonary blastomycosis: an appraisal of diagnostic techniques. Chest 2002;121:768-73. 10.1378/chest.121.3.768 [DOI] [PubMed] [Google Scholar]
- 154.Frost HM, Novicki TJ. Blastomyces Antigen Detection for Diagnosis and Management of Blastomycosis. J Clin Microbiol 2015;53:3660-2. 10.1128/JCM.02352-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.el-Ebiary M, Torres A, Fabregas N, et al. Significance of the isolation of Candida species from respiratory samples in critically ill, non-neutropenic patients. An immediate postmortem histologic study. Am J Respir Crit Care Med 1997;156:583-90. 10.1164/ajrccm.156.2.9612023 [DOI] [PubMed] [Google Scholar]
- 156.DiTomasso JP, Ampel NM, Sobonya RE, et al. Bronchoscopic diagnosis of pulmonary coccidioidomycosis. Comparison of cytology, culture, and transbronchial biopsy. Diagn Microbiol Infect Dis 1994;18:83-7. 10.1016/0732-8893(94)90070-1 [DOI] [PubMed] [Google Scholar]
- 157.Sobonya RE, Barbee RA, Wiens J, et al. Detection of fungi and other pathogens in immunocompromised patients by bronchoalveolar lavage in an area endemic for coccidioidomycosis. Chest 1990;97:1349-55. 10.1378/chest.97.6.1349 [DOI] [PubMed] [Google Scholar]
- 158.Maesaki S, Kohno S, Mashimoto H, et al. Detection of Cryptococcus neoformans in bronchial lavage cytology: report of four cases. Intern Med 1995;34:54-7. 10.2169/internalmedicine.34.54 [DOI] [PubMed] [Google Scholar]
- 159.Baughman RP, Rhodes JC, Dohn MN, et al. Detection of cryptococcal antigen in bronchoalveolar lavage fluid: a prospective study of diagnostic utility. Am Rev Respir Dis 1992;145:1226-9. 10.1164/ajrccm/145.5.1226 [DOI] [PubMed] [Google Scholar]
- 160.Hage CA, Davis TE, Fuller D, et al. Diagnosis of histoplasmosis by antigen detection in BAL fluid. Chest 2010;137:623-8. 10.1378/chest.09-1702 [DOI] [PubMed] [Google Scholar]
- 161.Dahiya S, Mathur SR, Iyer VK, et al. Diagnosis of Pneumocystis pneumonia by bronchoalveolar lavage cytology: experience at a tertiary care centre in India. Indian J Chest Dis Allied Sci 2005;47:259-65. [PubMed] [Google Scholar]
- 162.Golden JA, Hollander H, Stulbarg MS, et al. Bronchoalveolar lavage as the exclusive diagnostic modality for Pneumocystis carinii pneumonia. A prospective study among patients with acquired immunodeficiency syndrome. Chest 1986;90:18-22. 10.1378/chest.90.1.18 [DOI] [PubMed] [Google Scholar]
- 163.Jacobs JA, Dieleman MM, Cornelissen EI, et al. Bronchoalveolar lavage fluid cytology in patients with Pneumocystis carinii pneumonia. Acta Cytol 2001;45:317-26. 10.1159/000327625 [DOI] [PubMed] [Google Scholar]
- 164.al-Abbadi MA, Russo K, Wilkinson EJ. Pulmonary mucormycosis diagnosed by bronchoalveolar lavage: a case report and review of the literature. Pediatr Pulmonol 1997;23:222-5. [DOI] [PubMed] [Google Scholar]
- 165.Glazer M, Nusair S, Breuer R, et al. The role of BAL in the diagnosis of pulmonary mucormycosis. Chest 2000;117:279-82. 10.1378/chest.117.1.279 [DOI] [PubMed] [Google Scholar]
- 166.Pirisi M, Gutierrez Y, Minini C, et al. Fatal human pulmonary infection caused by an Angiostrongylus-like nematode. Clin Infect Dis 1995;20:59-65. 10.1093/clinids/20.1.59 [DOI] [PubMed] [Google Scholar]
- 167.Sidhu G. Pulmonary Manifestations of Tropical Parasitic Diseases. Medicine Update. 2013. [Google Scholar]
- 168.Lall M, Sahni AK, Rajput AK. Pleuropulmonary paragonimiasis: mimicker of tuberculosis. Pathog Glob Health 2013;107:40-2. 10.1179/2047773212Y.0000000067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Procop GW, Marty AM, Scheck DN, et al. North American paragonimiasis. A case report. Acta Cytol 2000;44:75-80. 10.1159/000326230 [DOI] [PubMed] [Google Scholar]
- 170.Apewokin S, Steciuk M, Griffin S, et al. Strongyloides hyperinfection diagnosed by bronchoalveolar lavage in an immunocompromized host. Cytopathology 2010;21:345-7. 10.1111/j.1365-2303.2010.00765.x [DOI] [PubMed] [Google Scholar]
- 171.Williams J, Nunley D, Dralle W, et al. Diagnosis of pulmonary strongyloidiasis by bronchoalveolar lavage. Chest 1988;94:643-4. 10.1378/chest.94.3.643 [DOI] [PubMed] [Google Scholar]
- 172.Roig J, Romeu J, Riera C, et al. Acute eosinophilic pneumonia due to toxocariasis with bronchoalveolar lavage findings. Chest 1992;102:294-6. 10.1378/chest.102.1.294 [DOI] [PubMed] [Google Scholar]
- 173.Jacobs F, Depierreux M, Goldman M, et al. Role of bronchoalveolar lavage in diagnosis of disseminated toxoplasmosis. Rev Infect Dis 1991;13:637-41. 10.1093/clinids/13.4.637 [DOI] [PubMed] [Google Scholar]
- 174.Ozaki T, Nakahira S, Tani K, et al. Differential cell analysis in bronchoalveolar lavage fluid from pulmonary lesions of patients with tuberculosis. Chest 1992;102:54-9. 10.1378/chest.102.1.54 [DOI] [PubMed] [Google Scholar]
- 175.Sharma SK, Pande JN, Verma K. Bronchoalveolar lavage (BAL) in miliary tuberculosis. Tubercle 1988;69:175-8. 10.1016/0041-3879(88)90018-9 [DOI] [PubMed] [Google Scholar]
- 176.Tsao TC, Chen CH, Hong JH, et al. Shifts of T4/T8 T lymphocytes from BAL fluid and peripheral blood by clinical grade in patients with pulmonary tuberculosis. Chest 2002;122:1285-91. 10.1378/chest.122.4.1285 [DOI] [PubMed] [Google Scholar]
- 177.Sugunaraj J, Greco CS, Mehta YB. Rare case of pulmonary infection by rapidly growing mycobacteria in an immunocompromised host. Am J Respir Crit Care Med 2016;193:A3753. [Google Scholar]
- 178.Yamazaki Y, Kubo K, Sekiguchi M, et al. Analysis of BAL fluid in M. avium-intracellulare infection in individuals without predisposing lung disease. Eur Respir J 1998;11:1227-31. 10.1183/09031936.98.11061227 [DOI] [PubMed] [Google Scholar]
- 179.Yamazaki Y, Kubo K, Takamizawa A, et al. Markers indicating deterioration of pulmonary Mycobacterium avium-intracellulare infection. Am J Respir Crit Care Med 1999;160:1851-5. 10.1164/ajrccm.160.6.9902019 [DOI] [PubMed] [Google Scholar]
- 180.Inomata T, Konno S, Nagai K, et al. Neutrophil predominance in bronchoalveolar lavage fluid is associated with disease severity and progression of HRCT findings in pulmonary Mycobacterium avium infection. PLoS One 2018;13:e0190189. 10.1371/journal.pone.0190189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Casanova MJ, Chaparro M, Valenzuela C, et al. Adalimumab-induced interstitial pneumonia in a patient with Crohn’s disease. World J Gastroenterol 2015;21:2260-2. 10.3748/wjg.v21.i7.2260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Sachdeva A, Matuschak GM. Diffuse alveolar hemorrhage following alemtuzumab. Chest 2008;133:1476-8. 10.1378/chest.07-2354 [DOI] [PubMed] [Google Scholar]
- 183.Akoun GM, Cadranel JL, Rosenow EC, 3rd, et al. Bronchoalveolar lavage cell data in drug-induced pneumonitis. Allerg Immunol (Paris) 1991;23:245-52. [PubMed] [Google Scholar]
- 184.Coudert B, Bailly F, Lombard JN, et al. Amiodarone pneumonitis. Bronchoalveolar lavage findings in 15 patients and review of the literature. Chest 1992;102:1005-12. 10.1378/chest.102.4.1005 [DOI] [PubMed] [Google Scholar]
- 185.Mermolja M, Rott T, Debeljak A. Cytology of bronchoalveolar lavage in some rare pulmonary disorders: pulmonary alveolar proteinosis and amiodarone pulmonary toxicity. Cytopathology 1994;5:9-16. 10.1111/j.1365-2303.1994.tb00122.x [DOI] [PubMed] [Google Scholar]
- 186.Ohar JA, Jackson F, Dettenmeier PA, et al. Bronchoalveolar lavage cell count and differential are not reliable indicators of amiodarone-induced pneumonitis. Chest 1992;102:999-1004. 10.1378/chest.102.4.999 [DOI] [PubMed] [Google Scholar]
- 187.Raghavan M, Mazer MA, Brink DJ. Severe hypersensitivity pneumonitis associated with anagrelide. Ann Pharmacother 2003;37:1228-31. 10.1345/aph.1D071 [DOI] [PubMed] [Google Scholar]
- 188.Ananthakrishnan AN, Attila T, Otterson MF, et al. Severe pulmonary toxicity after azathioprine/6-mercaptopurine initiation for the treatment of inflammatory bowel disease. J Clin Gastroenterol 2007;41:682-8. 10.1097/01.mcg.0000225577.81008.ee [DOI] [PubMed] [Google Scholar]
- 189.Patel JN, Jiang C, Hertz DL, et al. Bevacizumab and the risk of arterial and venous thromboembolism in patients with metastatic, castration-resistant prostate cancer treated on Cancer and Leukemia Group B (CALGB) 90401 (Alliance). Cancer 2015;121:1025-31. 10.1002/cncr.29169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Sekimoto Y, Kato M, Shukuya T, et al. Bevacizumab-induced chronic interstitial pneumonia during maintenance therapy in non-small cell lung cancer. Respirol Case Rep 2016;4:e00151. 10.1002/rcr2.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.White DA, Kris MG, Stover DE. Bronchoalveolar lavage cell populations in bleomycin lung toxicity. Thorax 1987;42:551-2. 10.1136/thx.42.7.551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Boyer JE, Batra RB, Ascensao JL, et al. Severe pulmonary complication after bortezomib treatment for multiple myeloma. Blood 2006;108:1113. 10.1182/blood-2006-03-011494 [DOI] [PubMed] [Google Scholar]
- 193.Dun X, Yuan Z, Fu W, et al. Severe pulmonary complications after bortezomib treatment in multiple myeloma. Hematol Oncol 2010;28:49-52. [DOI] [PubMed] [Google Scholar]
- 194.Miyakoshi S, Kami M, Yuji K, et al. Severe pulmonary complications in Japanese patients after bortezomib treatment for refractory multiple myeloma. Blood 2006;107:3492-4. 10.1182/blood-2005-11-4541 [DOI] [PubMed] [Google Scholar]
- 195.Tintner R, Manian P, Gauthier P, et al. Pleuropulmonary fibrosis after long-term treatment with the dopamine agonist pergolide for Parkinson Disease. Arch Neurol 2005;62:1290-5. 10.1001/archneur.62.8.1290 [DOI] [PubMed] [Google Scholar]
- 196.Vergnon JM, Boucheron S, Riffat J, et al. [Interstitial pneumopathies caused by busulfan. Histologic, developmental and bronchoalveolar lavage analysis of 3 cases]. Rev Med Interne 1988;9:377-83. 10.1016/S0248-8663(88)80137-1 [DOI] [PubMed] [Google Scholar]
- 197.Schatz PL, Mesologites D, Hyun J, et al. Captopril-induced hypersensitivity lung disease. An immune-complex-mediated phenomenon. Chest 1989;95:685-7. 10.1378/chest.95.3.685 [DOI] [PubMed] [Google Scholar]
- 198.Watanabe K, Nishimura K, Shiode M, et al. Captopril, an angiotensin-converting enzyme inhibitor, induced pulmonary infiltration with eosinophilia. Intern Med 1996;35:142-5. 10.2169/internalmedicine.35.142 [DOI] [PubMed] [Google Scholar]
- 199.Archibald N, Yates B, Murphy D, et al. Carbamazepine-induced interstitial pneumonitis in a lung transplant patient. Respir Med 2006;100:1660-2. 10.1016/j.rmed.2005.12.011 [DOI] [PubMed] [Google Scholar]
- 200.O’Driscoll BR, Hasleton PS, Taylor PM, et al. Active lung fibrosis up to 17 years after chemotherapy with carmustine (BCNU) in childhood. N Engl J Med 1990;323:378-82. 10.1056/NEJM199008093230604 [DOI] [PubMed] [Google Scholar]
- 201.Chua W, Peters M, Loneragan R, et al. Cetuximab-associated pulmonary toxicity. Clin Colorectal Cancer 2009;8:118-20. 10.3816/CCC.2009.n.019 [DOI] [PubMed] [Google Scholar]
- 202.Hoag JB, Azizi A, Doherty TJ, et al. Association of cetuximab with adverse pulmonary events in cancer patients: a comprehensive review. J Exp Clin Cancer Res 2009;28:113. 10.1186/1756-9966-28-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Hughes S, Liong J, Miah A, et al. A brief report on the safety study of induction chemotherapy followed by synchronous radiotherapy and cetuximab in stage III non-small cell lung cancer (NSCLC): SCRATCH study. J Thorac Oncol 2008;3:648-51. 10.1097/JTO.0b013e3181757a60 [DOI] [PubMed] [Google Scholar]
- 204.Nishino M, Giobbie-Hurder A, Hatabu H, et al. Incidence of programmed cell death 1 inhibitor-related pneumonitis in patients with advanced cancer:A systematic review and meta-analysis. JAMA Oncol 2016;2:1607-16. 10.1001/jamaoncol.2016.2453 [DOI] [PubMed] [Google Scholar]
- 205.Montani D, Seferian A, Parent F, et al. Immune checkpoint inhibitor-associated interstitial lung diseases: some progress but still many issues. Eur Respir J 2017;50:1701319. 10.1183/13993003.01319-2017 [DOI] [PubMed] [Google Scholar]
- 206.Cho JY, Kim J, Lee JS, et al. Characteristics, incidence, and risk factors of immune checkpoint inhibitor-related pneumonitis in patients with non-small cell lung cancer. Lung Cancer 2018;125:150-6. 10.1016/j.lungcan.2018.09.015 [DOI] [PubMed] [Google Scholar]
- 207.Delaunay M, Cadranel J, Lusque A, et al. Immune-checkpoint inhibitors associated interstitial lung disease in cancer patients. Eur Respir J 2017;50:1700050. 10.1183/13993003.00050-2017 [DOI] [PubMed] [Google Scholar]
- 208.Tone M, Izumo T, Awano N, et al. High mortality and poor treatment efficacy of immune checkpoint inhibitors in patients with severe grade checkpoint inhibitor pneumonitis in non-small cell lung cancer. Thoracic Cancer 2019;10:2006-12. 10.1111/1759-7714.13187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Crestani B, Jaccard A, Israel-Biet D, et al. Chlorambucil-associated pneumonitis. Chest 1994;105:634-6. 10.1378/chest.105.2.634 [DOI] [PubMed] [Google Scholar]
- 210.Hill BT, Weil AC, Kalaycio M, et al. Pulmonary involvement by chronic lymphocytic leukemia/small lymphocytic lymphoma is a specific pathologic finding independent of inflammatory infiltration. Leuk Lymphoma 2012;53:589-95. 10.3109/10428194.2011.623252 [DOI] [PubMed] [Google Scholar]
- 211.Malik SW, Myers JL, DeRemee RA, et al. Lung toxicity associated with cyclophosphamide use. Two distinct patterns. Am J Respir Crit Care Med 1996;154:1851-6. 10.1164/ajrccm.154.6.8970380 [DOI] [PubMed] [Google Scholar]
- 212.Hamada K, Nagai S, Kitaichi M, et al. Cyclophosphamide-induced late-onset lung disease. Intern Med 2003;42:82-7. 10.2169/internalmedicine.42.82 [DOI] [PubMed] [Google Scholar]
- 213.Bergeron A, Rea D, Levy V, et al. Lung abnormalities after dasatinib treatment for chronic myeloid leukemia: a case series. Am J Respir Crit Care Med 2007;176:814-8. 10.1164/rccm.200705-715CR [DOI] [PubMed] [Google Scholar]
- 214.Jasielec JK, Larson RA. Dasatinib-Related Pulmonary Toxicity Mimicking an Atypical Infection. J Clin Oncol 2016;34:e46-8. 10.1200/JCO.2013.50.1981 [DOI] [PubMed] [Google Scholar]
- 215.Alsamarai S, Charpidou AG, Matthay RA, et al. Pneumonitis related to docetaxel: case report and review of the literature. In Vivo 2009;23:635-7. [PubMed] [Google Scholar]
- 216.Read WL, Mortimer JE, Picus J. Severe interstitial pneumonitis associated with docetaxel administration. Cancer 2002;94:847-53. 10.1002/cncr.10263 [DOI] [PubMed] [Google Scholar]
- 217.Jacobs C, Slade M, Lavery B. Doxorubicin and BOOP. A possible near fatal association. Clin Oncol (R Coll Radiol) 2002;14:262. 10.1053/clon.2002.0071 [DOI] [PubMed] [Google Scholar]
- 218.Liu V, White DA, Zakowski MF, et al. Pulmonary toxicity associated with erlotinib. Chest 2007;132:1042-4. 10.1378/chest.07-0050 [DOI] [PubMed] [Google Scholar]
- 219.Makris D, Scherpereel A, Copin MC, et al. Fatal interstitial lung disease associated with oral erlotinib therapy for lung cancer. BMC Cancer 2007;7:150. 10.1186/1471-2407-7-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Vahid B, Esmaili A. Erlotinib-associated acute pneumonitis: report of two cases. Can Respir J 2007;14:167-70. 10.1155/2007/832605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Cho SK, Oh IH, Park CK, et al. Etanercept induced organizing pneumonia in a patient with rheumatoid arthritis. Rheumatol Int 2012;32:1055-7. 10.1007/s00296-009-1350-4 [DOI] [PubMed] [Google Scholar]
- 222.Miyagi R, Ideguchi H, Soga T, et al. Development of pulmonary and cardiac sarcoidosis during etanercept therapy. Int J Rheum Dis 2014;17:810-2. 10.1111/1756-185X.12178 [DOI] [PubMed] [Google Scholar]
- 223.Peno-Green L, Lluberas G, Kingsley T, et al. Lung injury linked to etanercept therapy. Chest 2002;122:1858-60. 10.1378/chest.122.5.1858 [DOI] [PubMed] [Google Scholar]
- 224.Gurjal A, An T, Valdivieso M, et al. Etoposide-induced pulmonary toxicity. Lung Cancer 1999;26:109-12. 10.1016/S0169-5002(99)00081-1 [DOI] [PubMed] [Google Scholar]
- 225.Hatakeyama S, Tachibana A, Morita M, et al. [Etoposide-induced pneumonitis]. Nihon Kyobu Shikkan Gakkai Zasshi 1997;35:210-4. [PubMed] [Google Scholar]
- 226.Mizuno R, Asano K, Mikami S, et al. Patterns of interstitial lung disease during everolimus treatment in patients with metastatic renal cell carcinoma. Jpn J Clin Oncol 2012;42:442-6. 10.1093/jjco/hys033 [DOI] [PubMed] [Google Scholar]
- 227.White DA, Schwartz LH, Dimitrijevic S, et al. Characterization of pneumonitis in patients with advanced non-small cell lung cancer treated with everolimus (RAD001). J Thorac Oncol 2009;4:1357-63. 10.1097/JTO.0b013e3181ba20b1 [DOI] [PubMed] [Google Scholar]
- 228.Ando M, Okamoto I, Yamamoto N, et al. Predictive factors for interstitial lung disease, antitumor response, and survival in non-small-cell lung cancer patients treated with gefitinib. J Clin Oncol 2006;24:2549-56. 10.1200/JCO.2005.04.9866 [DOI] [PubMed] [Google Scholar]
- 229.Kataoka K, Taniguchi H, Hasegawa Y, et al. Interstitial lung disease associated with gefitinib. Respir Med 2006;100:698-704. 10.1016/j.rmed.2005.07.015 [DOI] [PubMed] [Google Scholar]
- 230.Hotta K, Kiura K, Takigawa N, et al. Comparison of the incidence and pattern of interstitial lung disease during erlotinib and gefitinib treatment in Japanese Patients with non-small cell lung cancer: the Okayama Lung Cancer Study Group experience. J Thorac Oncol 2010;5:179-84. 10.1097/JTO.0b013e3181ca12e0 [DOI] [PubMed] [Google Scholar]
- 231.Tomioka R, King TE, Jr. Gold-induced pulmonary disease: clinical features, outcome, and differentiation from rheumatoid lung disease. Am J Respir Crit Care Med 1997;155:1011-20. 10.1164/ajrccm.155.3.9116980 [DOI] [PubMed] [Google Scholar]
- 232.Scott DL, Bradby GV, Aitman TJ, et al. Relationship of gold and penicillamine therapy to diffuse interstitial lung disease. Ann Rheum Dis 1981;40:136-41. 10.1136/ard.40.2.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Internullo M, Giannelli V, Sardo L, et al. Hydroxyurea-induced interstitial pneumonitis: case report and review of the literature. Eur Rev Med Pharmacol Sci 2014;18:190-3. [PubMed] [Google Scholar]
- 234.Sandhu HS, Barnes PJ, Hernandez P. Hydroxyurea-induced hypersensitivity pneumonitis: A case report and literature review. Can Respir J 2000;7:491-5. 10.1155/2000/297045 [DOI] [PubMed] [Google Scholar]
- 235.Peerzada MM, Spiro TP, Daw HA. Pulmonary toxicities of tyrosine kinase inhibitors. Clin Adv Hematol Oncol 2011;9:824-36. [PubMed] [Google Scholar]
- 236.Berthod G, Lazor R, Letovanec I, et al. Pulmonary sarcoid-like granulomatosis induced by ipilimumab. J Clin Oncol 2012;30:e156-9. 10.1200/JCO.2011.39.3298 [DOI] [PubMed] [Google Scholar]
- 237.Barjaktarevic IZ, Qadir N, Suri A, et al. Organizing pneumonia as a side effect of ipilimumab treatment of melanoma. Chest 2013;143:858-61. 10.1378/chest.12-1467 [DOI] [PubMed] [Google Scholar]
- 238.Chung CU, Park DI, Lee CS, et al. Isoniazid and pulmonary fibrosis. Chin Med J (Engl) 2015;128:702-3. 10.4103/0366-6999.151695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Umeda N, Inada Y, Mamoto T. [Development of eosinophilic pneumonia in a patient with latent tuberculosis infection resulting from isoniazid]. Kekkaku 2014;89:777-80. [PubMed] [Google Scholar]
- 240.Chen Y, Kiatsimkul P, Nugent K, et al. Lenalidomide-induced interstitial lung disease. Pharmacotherapy 2010;30:325. 10.1592/phco.30.3.325 [DOI] [PubMed] [Google Scholar]
- 241.Lerch E, Gyorik S, Feilchenfeldt J, et al. A case of lenalidomide-induced hypersensitivity pneumonitis. Onkologie 2010;33:249-52. 10.1159/000305213 [DOI] [PubMed] [Google Scholar]
- 242.Akasheh MS, Freytes CO, Vesole DH. Melphalan-associated pulmonary toxicity following high-dose therapy with autologous hematopoietic stem cell transplantation. Bone Marrow Transplant 2000;26:1107-9. 10.1038/sj.bmt.1702664 [DOI] [PubMed] [Google Scholar]
- 243.Westerfield BT, Michalski JP, McCombs C, et al. Reversible melphalan-induced lung damage. Am J Med 1980;68:767-71. 10.1016/0002-9343(80)90269-7 [DOI] [PubMed] [Google Scholar]
- 244.Schnabel A, Richter C, Bauerfeind S, et al. Bronchoalveolar lavage cell profile in methotrexate induced pneumonitis. Thorax 1997;52:377-9. 10.1136/thx.52.4.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Jakubovic BD, Donovan A, Webster PM, et al. Methotrexate-induced pulmonary toxicity. Can Respir J 2013;20:153-5. 10.1155/2013/527912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Silberstein SD. Methysergide. Cephalalgia 1998;18:421-35. 10.1046/j.1468-2982.1998.1807421.x [DOI] [PubMed] [Google Scholar]
- 247.Holmberg L, Boman G. Pulmonary reactions to nitrofurantoin. 447 cases reported to the Swedish Adverse Drug Reaction Committee 1966-1976. Eur J Respir Dis 1981;62:180-9. [PubMed] [Google Scholar]
- 248.Sovijärvi AR, Lemola M, Stenius B, et al. Nitrofurantoin-induced acute, subacute and chronic pulmonary reactions. Scand J Respir Dis 1977;58:41-50. [PubMed] [Google Scholar]
- 249.Padley SP, Adler B, Hansell DM, et al. High-resolution computed tomography of drug-induced lung disease. Clin Radiol 1992;46:232-6. 10.1016/S0009-9260(05)80161-8 [DOI] [PubMed] [Google Scholar]
- 250.Nishino M, Ramaiya NH, Awad MM, et al. PD-1 Inhibitor-Related Pneumonitis in Advanced Cancer Patients: Radiographic Patterns and Clinical Course. Clin Cancer Res 2016;22:6051-60. 10.1158/1078-0432.CCR-16-1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Shibaki R, Akamatsu H, Fujimoto M, et al. Nivolumab induced radiation recall pneumonitis after two years of radiotherapy. Ann Oncol 2017;28:1404-5. 10.1093/annonc/mdx115 [DOI] [PubMed] [Google Scholar]
- 252.Zitnik RJ, Cooper JA, Jr. Pulmonary disease due to antirheumatic agents. Clin Chest Med 1990;11:139-50. [PubMed] [Google Scholar]
- 253.Barber NA, Ganti AK. Pulmonary toxicities from targeted therapies: a review. Target Oncol 2011;6:235-43. 10.1007/s11523-011-0199-0 [DOI] [PubMed] [Google Scholar]
- 254.Bonanni A, Bertelli E, Panicucci C, et al. Ofatumumab-associated acute pneumonitis: Not new but still the first case. Pharmacol Res Perspect 2016;5:e00267. 10.1002/prp2.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Fujimori K, Yokoyama A, Kurita Y, et al. Paclitaxel-induced cell-mediated hypersensitivity pneumonitis. Diagnosis using leukocyte migration test, bronchoalveolar lavage and transbronchial lung biopsy. Oncology 1998;55:340-4. 10.1159/000011873 [DOI] [PubMed] [Google Scholar]
- 256.Sotiriou C, van Houtte P, Klastersky J. Lung fibrosis induced by paclitaxel. Support Care Cancer 1998;6:68-71. 10.1007/s005200050135 [DOI] [PubMed] [Google Scholar]
- 257.Fragkou P, Souli M, Theochari M, et al. A Case of Organizing Pneumonia (OP) Associated with Pembrolizumab. Drug Target Insights 2016;10:9-12. 10.33393/dti.2016.1420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Leroy V, Templier C, Faivre JB, et al. Pembrolizumab-induced pneumonitis. ERJ Open Res 2017;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Zitnik RJ, Matthay RA. Drug-Induced Lung Disease. 3 ed. Interstitial Lung Disease. Hamilton, Ontario: Mosby Yearbook, 1998. [Google Scholar]
- 260.Dixit R, Dixit K, Nuwal P, et al. Diphenylhydantoin (phenytoin)-induced chronic pulmonary disease. Lung India 2009;26:155-8. 10.4103/0970-2113.56356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Periwal P, Joshi S, Gothi R, et al. Phenytoin-induced acute hypersensitivity pneumonitis. Lung India 2015;32:631-4. 10.4103/0970-2113.168126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Dhillon SS, Singh D, Doe N, et al. Diffuse alveolar hemorrhage and pulmonary capillaritis due to propylthiouracil. Chest 1999;116:1485-8. 10.1378/chest.116.5.1485 [DOI] [PubMed] [Google Scholar]
- 263.Lioté H, Liote F, Seroussi B, et al. Rituximab-induced lung disease: A systematic literature review. Eur Respir J 2010;35:681-7. 10.1183/09031936.00080209 [DOI] [PubMed] [Google Scholar]
- 264.Ennishi D, Terui Y, Yokoyama M, et al. Increased incidence of interstitial pneumonia by CHOP combined with rituximab. Int J Hematol 2008;87:393-7. 10.1007/s12185-008-0066-7 [DOI] [PubMed] [Google Scholar]
- 265.Burton C, Kaczmarski R, Jan-Mohamed R. Interstitial pneumonitis related to rituximab therapy. N Engl J Med 2003;348:2690-1; discussion 2691. 10.1056/NEJM200306263482619 [DOI] [PubMed] [Google Scholar]
- 266.Morelon E, Stern M, Israel-Biet D, et al. Characteristics of sirolimus-associated interstitial pneumonitis in renal transplant patients. Transplantation 2001;72:787-90. 10.1097/00007890-200109150-00008 [DOI] [PubMed] [Google Scholar]
- 267.Weiner SM, Sellin L, Vonend O, et al. Pneumonitis associated with sirolimus: clinical characteristics, risk factors and outcome--a single-centre experience and review of the literature. Nephrol Dial Transplant 2007;22:3631-7. 10.1093/ndt/gfm420 [DOI] [PubMed] [Google Scholar]
- 268.Takeda H, Nishikawa H, Iguchi E, et al. Sorafenib-induced acute interstitial pneumonia in patients with advanced hepatocellular carcinoma: report of three cases. Clin J Gastroenterol 2012;5:407-12. 10.1007/s12328-012-0339-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Parry SD, Barbatzas C, Peel ET, et al. Sulphasalazine and lung toxicity. Eur Respir J 2002;19:756-64. 10.1183/09031936.02.00267402 [DOI] [PubMed] [Google Scholar]
- 270.Ulubaş B, Sahin G, Ozer C, et al. Bronchiolitis obliterans organizing pneumonia associated with sulfasalazine in a patient with rheumatoid arthritis. Clin Rheumatol 2004;23:249-51. 10.1007/s10067-003-0848-5 [DOI] [PubMed] [Google Scholar]
- 271.Valcke Y, Pauwels R, Van der Straeten M. Bronchoalveolar lavage in acute hypersensitivity pneumonitis caused by sulfasalazine. Chest 1987;92:572-3. 10.1378/chest.92.3.572 [DOI] [PubMed] [Google Scholar]
- 272.Yuasa T, Kitsukawa S, Sukegawa G, et al. Early onset recall pneumonitis during targeted therapy with sunitinib. BMC Cancer 2013;13:3. 10.1186/1471-2407-13-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Vahid B, Mehrotra A. Trastuzumab (Herceptin)-associated lung injury. Respirology 2006;11:655-8. 10.1111/j.1440-1843.2006.00907.x [DOI] [PubMed] [Google Scholar]
- 274.Kim SJ, Jhun BW, Lee JE, et al. A case of drug-induced interstitial pneumonitis caused by valproic Acid for the treatment of seizure disorders. Tuberc Respir Dis (Seoul) 2014;77:145-8. 10.4046/trd.2014.77.3.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Choi KH, Nam TS, Kim JT, et al. Valproate associated diffuse alveolar hemorrhage. Eur J Neurol 2011;18:e98-9. 10.1111/j.1468-1331.2011.03409.x [DOI] [PubMed] [Google Scholar]
- 276.Kamenetsky Z, Da’as N, Esayag Y, et al. Valproic acid-induced eosinophilic pleural effusion: a case report and review of the literature. Neurologist 2012;18:39-40. 10.1097/NRL.0b013e31823d7a6d [DOI] [PubMed] [Google Scholar]
- 277.Artigas A, Castella X. Bronchoalveolar Lavage (BAL) in Adult Respiratory Distress Syndrome (ARDS). Update in Intensive Care and Emergency Medicine. Berlin, Heidelberg: Springer, 1991. [Google Scholar]
- 278.Morgan JE, McCaul DS, Rodriguez FH, et al. Pulmonary immunologic features of alveolar septal amyloidosis associated with multiple myeloma. Chest 1987;92:704-8. 10.1378/chest.92.4.704 [DOI] [PubMed] [Google Scholar]
- 279.Corwin RW, Irwin RS. The lipid-laden alveolar macrophage as a marker of aspiration in parenchymal lung disease. Am Rev Respir Dis 1985;132:576-81. [DOI] [PubMed] [Google Scholar]
- 280.Silverman JF, Turner RC, West RL, et al. Bronchoalveolar lavage in the diagnosis of lipoid pneumonia. Diagn Cytopathol 1989;5:3-8. 10.1002/dc.2840050103 [DOI] [PubMed] [Google Scholar]
- 281.Greenebaum E, Copeland A, Grewal R. Blackened bronchoalveolar lavage fluid in crack smokers. A preliminary study. Am J Clin Pathol 1993;100:481-7. 10.1093/ajcp/100.5.481 [DOI] [PubMed] [Google Scholar]
- 282.Forrester JM, Steele AW, Waldron JA, et al. Crack lung: an acute pulmonary syndrome with a spectrum of clinical and histopathologic findings. Am Rev Respir Dis 1990;142:462-7. 10.1164/ajrccm/142.2.462 [DOI] [PubMed] [Google Scholar]
- 283.Davies SJ, Gosney JR, Hansell DM, et al. Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia: an under-recognised spectrum of disease. Thorax 2007;62:248-52. 10.1136/thx.2006.063065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Arnaud L, Pierre I, Beigelman-Aubry C, et al. Pulmonary involvement in Erdheim-Chester disease: a single-center study of thirty-four patients and a review of the literature. Arthritis Rheum 2010;62:3504-12. 10.1002/art.27672 [DOI] [PubMed] [Google Scholar]
- 285.Diamond EL, Dagna L, Hyman DM, et al. Consensus guidelines for the diagnosis and clinical management of Erdheim-Chester disease. Blood 2014;124:483-92. 10.1182/blood-2014-03-561381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Rouhani FN, Brantly ML, Markello TC, et al. Alveolar macrophage dysregulation in Hermansky-Pudlak syndrome type 1. Am J Respir Crit Care Med 2009;180:1114-21. 10.1164/rccm.200901-0023OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Takahashi K, Ishida T, Ogura G, et al. Diagnostic usefulness of bronchoalveolar lavage in Hermansky-Pudlak syndrome: a case with double lung cancers. Intern Med 2004;43:972-6. 10.2169/internalmedicine.43.972 [DOI] [PubMed] [Google Scholar]
- 288.Peros-Golubicic T, Sharma O. Clinical Atlas of Interstitial Lung Disease. 1 ed. Idiopathic Pulmonary Hemosiderosis. London: Springer-Verlag, 2006. [Google Scholar]
- 289.Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e142S-65S. [DOI] [PubMed] [Google Scholar]
- 290.Girard P, Caliandro R, Seguin-Givelet A, et al. Sensitivity of cytology specimens from bronchial aspirate or washing during bronchoscopy in diagnosis of lung malignancies:An update. Clin Lung Cancer 2017;18:512-8. 10.1016/j.cllc.2016.11.009 [DOI] [PubMed] [Google Scholar]
- 291.Zhang X, Kuang Y, Zhang Y, et al. Shifted focus of bronchoalveolar lavage in patients with suspected thoracic malignancy: an analysis of 224 patients. J Thorac Dis 2016;8:3245-54. 10.21037/jtd.2016.11.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Ahmad K, Kumar Gupta M, Dhungel K, et al. Pulmonary alveolar microlithiasis: a rare case report. Iran J Med Sci 2013;38:267-70. [PMC free article] [PubMed] [Google Scholar]
- 293.Ferreira Francisco FA, Pereira e Silva JL, Hochhegger B, et al. Pulmonary alveolar microlithiasis. State-of-the-art review. Respir Med 2013;107:1-9. 10.1016/j.rmed.2012.10.014 [DOI] [PubMed] [Google Scholar]
- 294.Inoue Y, Trapnell BC, Tazawa R, et al. Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med 2008;177:752-62. 10.1164/rccm.200708-1271OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Burkhalter A, Silverman JF, Hopkins MB, 3rd, et al. Bronchoalveolar lavage cytology in pulmonary alveolar proteinosis. Am J Clin Pathol 1996;106:504-10. 10.1093/ajcp/106.4.504 [DOI] [PubMed] [Google Scholar]
- 296.Chou CW, Lin FC, Tung SM, et al. Diagnosis of pulmonary alveolar proteinosis: usefulness of papanicolaou-stained smears of bronchoalveolar lavage fluid. Arch Intern Med 2001;161:562-6. 10.1001/archinte.161.4.562 [DOI] [PubMed] [Google Scholar]
- 297.Wang BM, Stern EJ, Schmidt RA, et al. Diagnosing pulmonary alveolar proteinosis. A review and an update. Chest 1997;111:460-6. 10.1378/chest.111.2.460 [DOI] [PubMed] [Google Scholar]
- 298.Schoch OD, Schanz U, Koller M, et al. BAL findings in a patient with pulmonary alveolar proteinosis successfully treated with GM-CSF. Thorax 2002;57:277-80. 10.1136/thorax.57.3.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.O’Keefe MC, Post MD. Pulmonary capillary hemangiomatosis: a rare cause of pulmonary hypertension. Arch Pathol Lab Med 2015;139:274-7. 10.5858/arpa.2013-0500-RS [DOI] [PubMed] [Google Scholar]
- 300.Alzghoul B, Li P, Zaki S, et al. Bronchoalveolar Lavage Flow Cytometry for the Diagnosis of Pulmonary Post-Transplant Lymphoproliferative Disorder. QJM 2020. [Epub ahead of print]. 10.1093/qjmed/hcaa124 [DOI] [PubMed] [Google Scholar]
- 301.Michelson P, Watkins B, Webber SA, et al. Screening for PTLD in lung and heart-lung transplant recipients by measuring EBV DNA load in bronchoalveolar lavage fluid using real time PCR. Pediatr Transplant 2008;12:464-8. 10.1111/j.1399-3046.2007.00835.x [DOI] [PubMed] [Google Scholar]
- 302.Montani D, Price LC, Dorfmuller P, et al. Pulmonary veno-occlusive disease. Eur Respir J 2009;33:189-200. 10.1183/09031936.00090608 [DOI] [PubMed] [Google Scholar]
- 303.Rabiller A, Jais X, Hamid A, et al. Occult alveolar haemorrhage in pulmonary veno-occlusive disease. Eur Respir J 2006;27:108-13. 10.1183/09031936.06.00054105 [DOI] [PubMed] [Google Scholar]
- 304.Matthews AW, Buchanan R. A case of pulmonary veno-occlusive disease and a new bronchoscopic sign. Respir Med 1990;84:503-5. 10.1016/S0954-6111(08)80117-5 [DOI] [PubMed] [Google Scholar]
- 305.Kantrow SP, Meyer KC, Kidd P, et al. The CD4/CD8 ratio in BAL fluid is highly variable in sarcoidosis. Eur Respir J 1997;10:2716-21. 10.1183/09031936.97.10122716 [DOI] [PubMed] [Google Scholar]
- 306.Winterbauer RH, Lammert J, Selland M, et al. Bronchoalveolar lavage cell populations in the diagnosis of sarcoidosis. Chest 1993;104:352-61. 10.1378/chest.104.2.352 [DOI] [PubMed] [Google Scholar]
- 307.Lewis N, McCaffrey K, Sage K, et al. E-cigarette Use, or Vaping, Practices and Characteristics Among Persons with Associated Lung Injury - Utah, April-October 2019. MMWR Morb Mortal Wkly Rep 2019;68:953-6. 10.15585/mmwr.mm6842e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Blount BC, Karwowski MP, Morel-Espinosa M, et al. Evaluation of Bronchoalveolar Lavage Fluid from Patients in an Outbreak of E-cigarette, or Vaping, Product Use-Associated Lung Injury - 10 States, August-October 2019. MMWR Morb Mortal Wkly Rep 2019;68:1040-1. 10.15585/mmwr.mm6845e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Taylor J, Wiens T, Peterson J, et al. Lung Injury Response Task Force. Characteristics of E-cigarette, or Vaping, Products Used by Patients with Associated Lung Injury and Products Seized by Law Enforcement - Minnesota, 2018 and 2019. MMWR Morb Mortal Wkly Rep 2019;68:1096-100. 10.15585/mmwr.mm6847e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Blount BC, Karwowski MP, Shields PG, et al. Lung Injury Response Laboratory Working Group . Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI. N Engl J Med 2020;382:697-705. 10.1056/NEJMoa1916433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Lal A, Mishra AK, Sahu KK, Vitamin E. Acetate and E-Cigarette or Vaping Product-Associated Lung Injury (EVALI): An Update. Am J Med 2020;133:e204. 10.1016/j.amjmed.2019.11.005 [DOI] [PubMed] [Google Scholar]
- 312.Henry TS, Kanne JP, Kligerman SJ. Imaging of vaping-associated lung disease. N Engl J Med 2019;381:1486-7. 10.1056/NEJMc1911995 [DOI] [PubMed] [Google Scholar]
- 313.Maddock SD, Cirulis MM, Callahan SJ, et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med 2019;381:1488-9. 10.1056/NEJMc1912038 [DOI] [PubMed] [Google Scholar]
- 314.Davidson K, Brancato A, Heetderks P, et al. Outbreaks of electronic-cigarette-associated acute lipoid pneumonia – North Carolina, July-August 2019. MMWR 2019;68:784-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.von Ranke FM, Zanetti G, Hochhegger B, et al. Infectious diseases causing diffuse alveolar hemorrhage in immunocompetent patients: a state-of-the-art review. Lung 2013;191:9-18. 10.1007/s00408-012-9431-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Sato T, Shimosato T, Klinman DM. Silicosis and lung cancer: current perspectives. Lung Cancer (Auckl) 2018;9:91-101. 10.2147/LCTT.S156376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Ozkaya N, Rosenblum MK, Durham BH, et al. The histopathology of Erdheim-Chester disease: a comprehensive review of a molecularly characterized cohort. Mod Pathol 2018;31:581-97. 10.1038/modpathol.2017.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Cordeiro CR, Jones JC, Alfaro T, et al. Bronchoalveolar lavage in occupational lung diseases. Semin Respir Crit Care Med 2007;28:504-13. 10.1055/s-2007-991523 [DOI] [PubMed] [Google Scholar]
- 319.Tazawa R, Ueda T, Abe M, et al. Inhaled GM-CSF for Pulmonary Alveolar Proteinosis. N Engl J Med 2019;381:923-32. 10.1056/NEJMoa1816216 [DOI] [PubMed] [Google Scholar]
- 320.Ramirez RJ, Schultz RB, Dutton RE. Pulmonary alveolar proteinosis. A new technique and rationale for treatment. Arch Intern Med 1963;112:419-31. 10.1001/archinte.1963.03860030173021 [DOI] [PubMed] [Google Scholar]
- 321.Nakashima S, Ishimatsu Y, Hara S, et al. Exogenous lipoid pneumonia successfully treated with bronchoscopic segmental lavage therapy. Respir Care 2015;60:e1-5. 10.4187/respcare.03225 [DOI] [PubMed] [Google Scholar]
- 322.Kim HJ, Lee WH, Jeong N, et al. Lipoid pneumonitis in a patient with an accidental ingestion of kerosene successfully treated with bronchoscopic segmental lavage and systemic steroid: Case report. Medicine (Baltimore) 2018;97:e12786. 10.1097/MD.0000000000012786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Li F, Zhu B, Xie G, et al. Effects of bronchoalveolar lavage on pediatric refractory Mycoplasma pneumoniae pneumonia complicated with atelectasis: a prospective case-control study. Minerva Pediatr 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as