Abstract
Introduction
Food allergy affects up to 10% of Australian children, and living with food allergic children can be challenging for parents. This study explored parental perceptions and knowledge as they navigate a new reality of keeping their child safe.
Methods
Parents of children with food allergies completed an online food allergy survey in 2015. Questions explored health knowledge, skills, and attitudes (KSAs) as well as quality of life (QoL) through the inclusion of the Food Allergy Quality of Life — Parental Burden instrument (FAQL-PB). Notification of the survey included advertisements to more than 700 randomly selected Australia-wide preschools, 44 allergy specialists, and Allergy & Anaphylaxis Australia. Responses were tabulated and analysed.
Results
Of the 400 participants who logged on, 357 commenced the survey and 318 finished. Questionnaire analysis showed that 44.1% of parents (n = 135) hesitated to use an adrenaline auto-injector and may be influenced by a classification system where symptom severity is not universally understood. While 79% would sign up to a national Anaphylaxis Registry, intention to participate in clinical trials using vaccines was disclosed by only 56%. Allergen labelling and community acceptance continue to be the most challenging aspects of managing a food allergy, and 50% of parents reported that food allergy played a role in choosing a preschool or primary school. Overall, quality of life for participants was influenced more by gender (male) and age of the child than where they lived — capital city or regional location; however, regional participants were more frustrated over lack of appreciation relating to the seriousness of food allergy (p = 0.010).
Conclusion
Results highlight the need for educational strategies for both the food allergy community and public, particularly in regional areas, since there is a perceived lack of appreciation as to the seriousness of food allergy. Educational resources and relevant networks are required to support parents and caregivers in the management of children with food allergy.
Keywords: Food allergy, Quality of life, FAQL-PB, Parental burden
Abbreviations: ABC, Australian Broadcasting Corporation; ANOVA, Analysis of variance; CA, California; FAQL-PB, Food Allergy Quality of Life – Parental Burden; GP/GPs, General Practitioner(s); KSA, Knowledge, Skills, Attitudes; LOC, Locus of control; NSW, New South Wales, Australia; NVivo Pro, NVivo Pro, QSR International Pty Ltd; PAF, Principal Axis Factoring; PRIME7, Prime Television Australia; QoL, Quality of Life; SPSS/IBM SPSS Statistics, IBM Statistical Package for the Social Sciences; VIC, Victoria, Australia; WIN Television, WIN Corporation Australia
Introduction
In recent years there has been a rise in the number of people experiencing food allergies to common foods, with more allergic reactions occurring earlier in life.1, 2, 3, 4 With no current cure for food allergy, parents must learn new strategies to prevent food allergic reactions, and this creates quality of life (QoL) challenges as parents learn to navigate the new reality of allergen avoidance.5 In this study, Australian parents reveal what it is like to live with a child who has a food allergy.
To normalise behaviour around food, parents need to be vigilant, yet guard against inadvertently creating an environment of fear, as this can impact self-confidence in their children and lead to social withdrawal and abnormal eating patterns.6,7 One starting point is to improve health literacy across the community to engender support and awareness as health messages can influence behaviour.5,8
However, to keep children safe, parents must rely on third parties, including food manufacturers, restaurant staff, other parents, and teachers. As studies show allergic reactions occur more frequently outside the home, there is a need for specialised training and greater awareness of food allergies in the hospitality and food industries.9, 10, 11
Exploring knowledge, skills, and attitudes (KSA) this study offered many insights into the challenges of managing a child with a food allergy. Topics included social engagement, medical knowledge, and schooling. The authors believe this is the first comprehensive study of Australian parents living with a child who has a food allergy, offering not only insight to daily challenges but also comparative analysis across metropolitan (capital cities), regional, and remote areas of Australia.
Methods
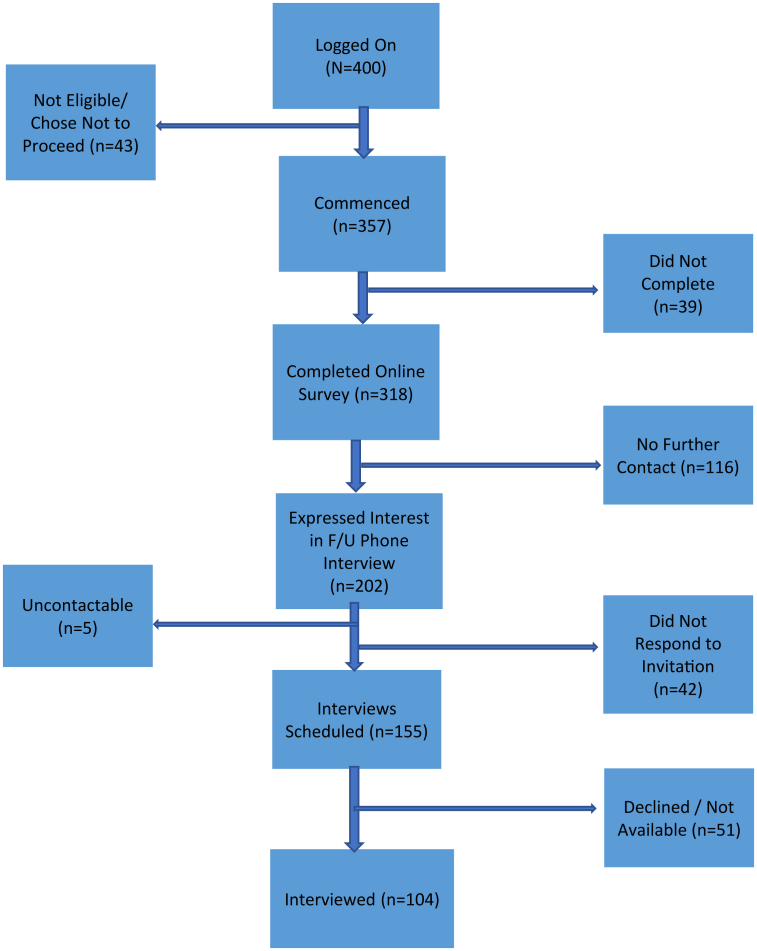
This study was conducted between 2015 and 2017, using an online platform and parental interviews. Phase one was a cross-sectional online survey hosted on the cloud-based platform, SurveyMonkey® (San Mateo CA USA) involving participants either living with food allergy (under 8 years, 8–12 years, teenagers under 19 years) or parents of children with food allergy. While phase two encouraged parents who had completed the online survey to opt-in for a phone interview, and this process is deconstructed in Fig. 1.
Fig. 1.
Recruitment of participants (leading to final interview)
Recruitment of participants (online survey)
Participants were recruited from across Australia between May and December 2015. Formal distribution channels included letters to over 700 Australian preschools (53.8% in regional locations) and 44 allergy specialists requesting promotion of the survey at the time of consultation. The survey was also promoted via the public social network site (Facebook) and private membership domains of the Australian patient support organisation, Allergy & Anaphylaxis Australia. Regional media presentations on Radio (ABC Bega and Orange, NSW) and Television News (Prime 7 and WIN Television) invited prospective participants to complete the questionnaire.
Prospective participants were encouraged to log-on and read the Participant Information Sheet (refer Supplementary File – Participant Information Sheet – Food Allergy Quality of Life). For those without internet access, contact details (email and mobile) were provided.
Collection of demographic data included: age group, gender, year, and attendance at school and presence of concomitant atopic diseases such as hay fever, asthma, and eczema. Questions also sought information on where participants lived — capital city or regional location — and who diagnosed their child’s food allergy. For parents who reported living in a regional location, the results were subdivided into small or large regional centres. Large regional centres were the top 20 most populous cities or towns (population ≥52,000) based on the 2016 Australian Census.12
Survey design
Questions measured QoL and KSAs (refer to Supplementary File - Survey Questions) with a focus on social interaction, medical awareness, labelling practices, and decisions around schooling. To underpin validity, the questionnaire also incorporated, with permission, the internationally validated (Cronbach α = 0.95) Food Allergy Quality of Life Parental Burden (FAQL-PB) questionnaire.13 This offered the opportunity to discriminate responses, with higher scores indicating a worsening QoL.
Communication and encouragement to participate complemented other strategies designed to mitigate concerns over potential non-response bias associated with online surveys and the inability to calculate response rates.14 These strategies included letters to preschools and allergy specialists explaining the importance of completing the survey as well as a follow-up letter to allergy specialists announcing an extension of the survey closing date from October to December 2015. Support from Allergy & Anaphylaxis Australia was ongoing and included featuring the WIN TV interview in July 2015, notification of the extension from October to December, and a "final call" out one week before the survey closed in mid-December.
Interview scope and process
On completion of the online survey, parents were offered the opportunity to participate in an informal follow-up phone interview. To explore attitudes and perceptions, the interview included both structured and unstructured questions. Topics covered rating precautionary allergen labels (PALs) based on risk, the giving of advice to parents starting the food allergy journey and interaction with general practitioners (GPs) when food allergy was the defining criteria. Interviewees also considered peripheral issues, such as designing an advertising slogan to enhance public awareness of food allergies.
The final question asked participants to reflect and report on something positive about living with a child who has a food allergy. This strategic change was a deliberate inclusion to protect psychological wellbeing and minimise negative sentiments that may continue well after the cessation of the interview.15,16 Where the interviewer perceived personal issues or distress, interviewees were reminded that not only could they decline and end the interview, they could also seek professional help through medical and auxiliary services.
Interview process
Interviews were scheduled from September 2015 to March 2016. To ensure consistency in approach, language and style, the principal researcher conducted all interviews. Both purpose and suitability of interview time were reaffirmed along with an option to reconvene if not suitable. All interviewees gave formal verbal consent. Transcription (hand-written) of responses was as close to verbatim as possible though occasionally some words were indecipherable or missed. Interviews were scheduled for 45 min, although averaged 55 min. On conclusion, all were thanked for their time.
Statistical/data analysis
Non-parametric tests, including chi-square goodness-of-fit test, frequency statistics, and ANOVA tests were performed for comparative analysis between participants from capital cities and regional locations, age, and gender as well as allergen. Inclusion of the FAQL-PB questionnaire13 permitted both ordinal logistical regression and independent t-tests in the exploration of relationships between QoL scores and demographic attributes.
Principal Axis Factoring was performed using the Promax with Kaiser Normalisation rotation method to determine variance and relevant factors in the questionnaire data. To compensate for missing data and remove potential inaccuracies, calculation of frequency and valid percentages were based on the number of responses divided by the number who completed the specific question. This approach accounts for the different ”N” values represented throughout.
Statistical significance was measured using α = 0.05 (SPSS IBM Statistics V24.0, IBM), a popular distinguisher for non-parametric tests and categorical data. In contrast, the data from the interview narratives were transcribed and coded using NVivo Pro 11 qualitative data analysis software (version 11; QSR International Pty Ltd) to assist in the identification of relationships to uncover the interviewee’s perception of reality. Narratives were then assigned into preliminary themes before rereading each data set to ensure the narrative was accurately assigned.17
Results
Of the 400 parents who logged on, 377 proceeded past the first question, 18 were ineligible as they did not reside in Australia, while 2 did not have an immediate family member with food allergy. All data from ineligible participants were removed from the analysis, leaving 357 participants included in the study, with 318 completing the survey. Table 1 presents the demographic profile of the study population.
Table 1.
Demographic profile – online participants and child's top 4 food allergies
| Age group | Male | % | Female | % | Peanut allergy | Tree Nut allergy | Egg allergy | Dairy allergy | Four or more food allergies |
|---|---|---|---|---|---|---|---|---|---|
| Under 8 years | 108 | 55.7 | 69 | 55.7 | 115 | 107 | 100 | 77 | 64 |
| 8–12 years | 55 | 28.3 | 32 | 25.8 | 65 | 59 | 43 | 29 | 29 |
| Teenagers | 30 | 15.5 | 21 | 16.9 | 41 | 29 | 12 | 14 | 23 |
| Unknown | 1 | 0.5 | 2 | 1.6 | 2 | 1 | 0 | 1 | 0 |
| Total (N = 318) | 194 | 61% | 124 | 39% |
QoL indices - FAQL-PB questionnaire
Results showed that internal consistency and reliability were high (Cronbach’s α = 0.96) with a mean total FAQL-PB score of 3.61 (‘somewhat of an impact’) out of a possible score of 7 across all 3 domains (a: going on vacation/holiday [mean total = 4.82], b: social activities — going to restaurants and participating in social events [mean total = 5.10]), and c: worries and anxieties over the past week [mean total = 3.53]). Differences in QoL are highlighted in the following quotes, including the importance of family support:
-
•
“become so anxious about my son’s life threating allergies that we rarely attend any family functions …. either singled out, accused of being over obsessive or face criticism for not ’just letting them give him a bit of his allergens to cure him’ awareness is lacking & most are not willing to listen which is so frustrating.” [Regional Participant No:16, Male, Under 8 years] – QoL score of 7
-
•
“as a parent, allergies in your child cause guilt, fear and serious adjustments to lifestyle” [Capital City Participant No:118, Female, Under 8 years] – QoL score of 6
-
•
“although food allergy has impacted on my family in terms of with additional stress, they have had many positive benefits too. We eat out less, which is healthier … my son has learnt to be more responsible, confident and independent.” [Capital City Participant No:306, Male, Teenager] – QoL score of 1
To investigate the underlying dimensionality and item structure for the sample population (n = 323), we performed SPSS factor analysis using Principal Axis Factoring (PAF) rotation (Kaiser normalisation), suppressing commonality scores below 0.3. Overall results identified 2 factors, accounting for 64.1% of the variance in the questionnaire. Factor 1 related to general wellbeing and health, including psychological wellbeing, whereas Factor 2 aligned more with social interaction.
Factor analysis also showed differences across locations. For those living in capital cities, 2 factors emerged, accounting for 66.2% of the variance. At the same time, regional participants’ differentiation identified 3 factors accounting for 66.8% of all variances, although there was a strong focus on psychological wellbeing. Table 2 details the factors across each group.
Table 2.
Reported concerns across locations (Factorisation).
| In the past week how troubled have you been: | Population [All]a(N = 323) |
Capital Citiesa(N = 189) |
Regional Locationsb(N = 134) |
||||
|---|---|---|---|---|---|---|---|
| Factor |
Factor |
Factor |
|||||
| 1 | 2 | 1 | 2 | 1 | 2 | 3 | |
| That your child will have an allergic reaction (Q.17) | 0.997 | 0.981 | 0.982 | ||||
| That you will not be able to help if your child has an allergic reaction (Q.13) | 0.979 | 0.960 | 0.932 | ||||
| About your child attending school, school excursions or other group activities including childcare/day care (Q.11) | 0.807 | 0.822 | 0.810 | ||||
| To leave your child in care of others (Q.8) | 0.798 | 0.810 | 0.638 | ||||
| By your concerns for your child's health (Q.12) | 0.797 | 0.738 | 0.662 | ||||
| With issues concerning your child being near others while eating (Q.16) | 0.786 | 0.784 | 0.638 | ||||
| That your child may not overcome their food allergy (Q.7) | 0.722 | 0.694 | 0.551 | 0.340 | |||
| By sadness regarding the burden your child carries because of their food allergy (Q.10) | 0.702 | 0.562 | 0.329 | 0.747 | |||
| By frustration over other's lack of appreciation for the seriousness of food allergy (Q.9) | 0.656 | 0.572 | 0.683 | ||||
| With worry that your child will not have a normal upbringing (Q.14) | 0.648 | 0.651 | 0.409 | 0.447 | |||
| By anxiety relating to your child's food allergy (Q.6) | 0.627 | 0.617 | 0.334 | 0.549 | |||
| About concerns for your child's nutrition (Q.15) | 0.492 | 0.445 | 0.543 | ||||
| If planning a holiday, how much would your choice be limited by your child's food allergy (Q.1) | 0.946 | 0.981 | 0.666 | ||||
| If planning to go to a restaurant, how much would your choice be limited by your child's food allergy (Q.2) | 0.827 | 0.856 | 0.844 | ||||
| In the past week how troubled are you about your need to spend extra time preparing meals (ie reading labels, extra time shopping, preparing extra meals) (Q.4) | 0.576 | 0.659 | 0.923 | ||||
| If planning to participate in social activities with others involving food (eg: parties) how limited would your ability be to participate (Q.3) | 0.537 | 0.676 | 0.426 | 0.570 | |||
| In the past week how troubled are you about your need to take special precautions before going out of the home with your child (Q.5) | 0.431 | 0.471 | 0.345 | 0.551 | 0.798 | ||
Extraction Method: Principal Axis Factoring.
Rotation Method: Promax with Kaiser Normalisation.
Rotation converged in 3 iterations.
Rotation converged in 5 iterations
Although location did not significantly influence QoL, small differences emerged between capital cities (n = 189) and regional locations (n = 134). For those living in capital cities, the mean total QoL was better at 3.58 compared to 3.66 for regional locations (p = 0.723). Small regional towns had the best mean total QoL score of 3.54 compared to 3.80 for those living in large regional towns. Although regional locations were not statistically significant when an independent t-test was performed (p = 0.464), different parental challenges may exist when managing a child with a food allergy, including access to support services. However, with 8 participants excluded in this analysis between large and small regional towns, further research is warranted.
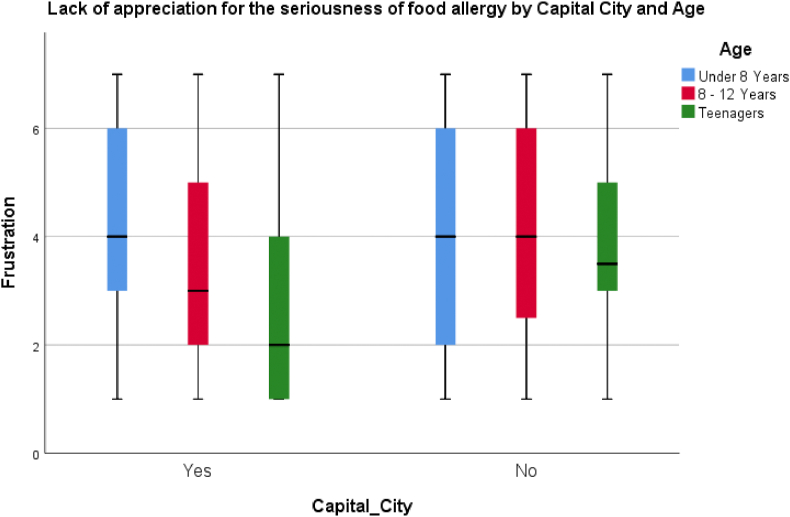
One such challenge where differences did emerge was whether others in the community took the child’s food allergy seriously. Here location was not significant. However, a lack of appreciation by others in the community was also influenced by age, and Fig. 2 illustrates this.
Fig. 2.
Frustration as to lack of appreciation of food allergy seriousness
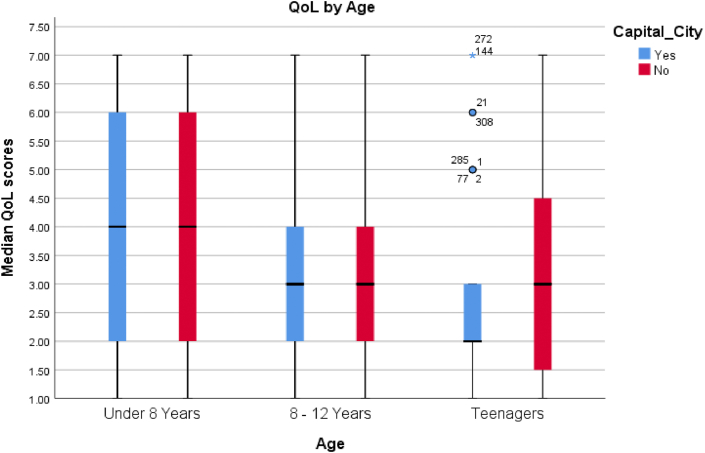
Mean total QoL scores were also worse for participants managing 4 or more of the top 7 allergens (peanut, tree nut, egg, dairy, wheat, soy, and seafood) compared to those needing to manage either 1 (p < 0.001) or 2 of these allergens (p = 0.001). Similarly, parents who concurrently managed peanuts, tree nuts, eggs, and dairy, the mean QoL score was 4.11 compared to 3.09 for those managing peanut and/or tree nut allergies, and this was statistically significant. However, significance was not found between parents managing these 4 allergens and those managing an egg and/or dairy allergy and this may be why, all but 1 of the 17 FAQL-PB questions, was significant when a one-way ANOVA test was performed. For parents managing an egg allergy (n = 156), the one FAQL-PB question where participants were less concerned was “not being able to help their child if they were having an allergic reaction” (p = 0.069). For those managing a dairy allergy (n = 126), the trend was toward being less concerned about “food allergies becoming more serious” (p = 0.059). In contrast, parents who reported a peanut allergy (n = 225), the only significant question was “how troubled have you been by sadness regarding the burden your child carries because of their food allergy?” (p = 0.007), while there was no significant difference for those managing a tree nut allergy (n = 197). However, irrespective of the type or number of allergens, one of the most influential characteristics, when a factorial ANOVA test was performed, was age (p = 0.002). Fig. 3 shows the distribution of parental mean QoL scores based on age and location, while Table 3 shows the significant differences across all FAQL-PB questions for the different age groups.
Fig. 3.
Parental mean QoL by age and location
Table 3.
QoL differences by child age
| QoL differences measured by age group | ||||||
|---|---|---|---|---|---|---|
| FAQL – PB Questions | Sum of Squares | Df | Mean Square | F | Sig. | |
| Needing to take special precautions before going out (Q.5) | Between Groups | 29.876 | 2 | 14.938 | 4.310 | 0.014 |
| Within Groups | 1081.406 | 312 | 3.466 | |||
| Total | 1111.283 | 314 | ||||
| Anxiety (Q.6) | Between Groups | 62.986 | 2 | 31.493 | 8.702 | 0.000 |
| Within Groups | 1129.186 | 312 | 3.619 | |||
| Total | 1192.171 | 314 | ||||
| Not overcoming food allergy (Q.7) | Between Groups | 34.252 | 2 | 17.126 | 4.248 | 0.015 |
| Within Groups | 1253.799 | 311 | 4.032 | |||
| Total | 1288.051 | 313 | ||||
| Leaving your child in the care of others (Q.8) | Between Groups | 118.796 | 2 | 59.398 | 14.538 | 0.000 |
| Within Groups | 1274.715 | 312 | 4.086 | |||
| Total | 1393.511 | 314 | ||||
| Lack of appreciation by others as to seriousness (Q.9) | Between Groups | 37.626 | 2 | 18.813 | 4.536 | 0.011 |
| Within Groups | 1277.570 | 308 | 4.148 | |||
| Total | 1315.196 | 310 | ||||
| Concerns for your child's health (Q.12) | Between Groups | 36.432 | 2 | 18.216 | 4.568 | 0.011 |
| Within Groups | 1232.155 | 309 | 3.988 | |||
| Total | 1268.587 | 311 | ||||
| Child will not have a normal upbringing (Q.14) | Between Groups | 23.940 | 2 | 11.970 | 3.238 | 0.041 |
| Within Groups | 1153.380 | 312 | 3.697 | |||
| Total | 1177.321 | 314 | ||||
| Nutrition (Q.15) | Between Groups | 23.850 | 2 | 11.925 | 3.165 | 0.044 |
| Within Groups | 1175.566 | 312 | 3.768 | |||
| Total | 1199.416 | 314 | ||||
| Child being near others while eating (Q.16) | Between Groups | 101.047 | 2 | 50.524 | 13.394 | 0.000 |
| Within Groups | 1173.131 | 311 | 3.772 | |||
| Total | 1274.178 | 313 | ||||
| Will have an allergic reaction (Q.17) | Between Groups | 42.862 | 2 | 21.431 | 5.507 | 0.004 |
| Within Groups | 1214.154 | 312 | 3.892 | |||
| Total | 1257.016 |
314 |
||||
In contrast, Table 4 shows distribution and CI intervals across the 3 FAQL-PB domains: going on holidays, social activities, and worries/anxieties over the preceding week. However, for some participants, they acknowledge that their answers may not have reflected their “normal” feelings in the preceding week:
-
•
“My feelings about a lot of the questions … will change once my child starts preschool/school. At the moment he is around me all the time so i don’t seem stressed about it all. But once he is out of my care, it will be a totally different story”. [Regional Participant No: 78, Male, Under 8 years]
-
•
“Asking about fears in ’the last week’ is not necessarily indicative of the ’norm’. Fears tend to escalate around events or situations …”. [Capital City Participant No: 289, Male, Teenager]
Table 4.
Measuring parental burden across regional and capital city participants.
| Domains | Location | N | Mean | Std. Deviation | Std. Error | 95% CI Mean |
|
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Going on holidays | Small Regional | 82 | 4.41 | 2.125 | 0.235 | 3.95 | 4.88 |
| Large Regional | 44 | 4.95 | 1.892 | 0.285 | 4.38 | 5.53 | |
| Regional Locationsa | 134 | 4.61 | 2.070 | 0.178 | 4.26 | 4.96 | |
| Capital City | 189 | 4.98 | 1.822 | 0.133 | 4.72 | 5.24 | |
| Total Holidaysa | 323 | 4.83 | 1.924 | 0.108 | 4.62 | 5.04 | |
| Social activities | Small Regional | 82 | 4.72 | 1.714 | 0.189 | 4.34 | 5.10 |
| Large Regional | 44 | 4.91 | 1.411 | 0.213 | 4.48 | 5.34 | |
| Regional Locationsa | 134 | 4.80 | 1.594 | 0.137 | 4.53 | 5.07 | |
| Capital City | 189 | 4.83 | 1.574 | 0.114 | 4.60 | 5.05 | |
| Total Social Activitiesa | 323 | 4.81 | 1.587 | 0.089 | 4.64 | 4.99 | |
| Worries and anxietiesb | Small Regional | 81 | 3.38 | 1.937 | 0.215 | 2.95 | 3.80 |
| Large Regional | 43 | 3.64 | 1.833 | 0.280 | 3.08 | 4.20 | |
| Regional Locationsa | 132 | 3.50 | 1.866 | 0.162 | 3.18 | 3.82 | |
| Capital City | 189 | 3.41 | 1.853 | 0.135 | 3.14 | 3.68 | |
| Total Worries and Anxietiesa | 321 | 3.43 | 1.868 | 0.106 | 3.23 | 3.64 | |
Total Regional Participants Including Eight whose Location was Unknown.
Worries and Anxieties – Over the Last Week
While these comments highlight individual circumstances, they also show that food allergy management is both situational and time dependent. By capturing multiple responses, the real impact of food allergy on QoL emerges.
Importance of food labelling
Parents reported allergen labelling, access to medical services and a safe school environment as the most important considerations when managing a child with food allergy. These factors were more important than research into finding a cure, the costs associated with managing food allergy or establishing an anaphylaxis register, notwithstanding 262 (n = 332, 78.9%) who thought a register was influential in raising community awareness and influencing government policies.
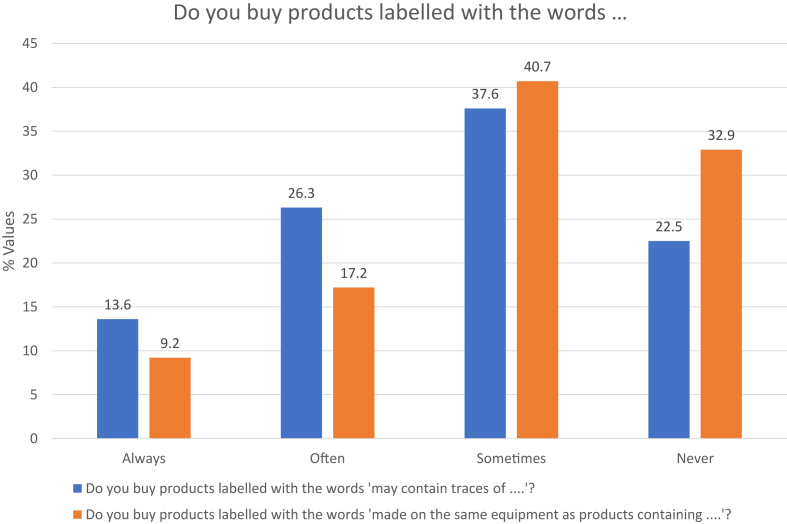
Precautionary allergen labelling (PAL) is a voluntary code adopted by Australian food manufacturers to alert consumers on the likelihood of a trace allergen being present. One of the most common PALs in Australia is “may contain traces of [allergen]”, yet 262 parents (n = 338, 77.5%) reported purchasing products with this warning. For 127 who selected they “sometime” purchased products with this label, 40 (31.5%) provided qualifying comments, including only purchasing products if manufactured in Australia. While for 34 participants (13.0%), the perception was that this label was only there to protect the manufacturer against legal action and had nothing to do with the actual risk, As expected, distribution across the 4 possible responses of ”never”, ”sometimes”, ”often” and ”always” was significant (chi-square p < 0.001).
For parents buying products with the label ”made on the same equipment” the number dropped to 67.7% (n = 226/337) inferring the wording influenced a change in purchasing behaviour. This change was statistically significant (chi-square test, p = 0.004) as parents placed more weight on this PAL wording compared to ”may contain traces of”. For those that said they ”sometimes” purchased products with this label (n = 137), the most common reason was that they had ”eaten it before” (n = 35). Others qualified the risk, reporting they only purchased one or two ”safe” products with this label, such as pasta or biscuits; if the product was manufactured in Australia; on contacting the manufacturer to assess ”actual risk”; and on advisement from their allergy specialist.
This change in risk profiling was corroborated during the interview process, with 50% of interviewees rating this label as either ”high” or ”extreme” risk, compared to 35% for ”may contain traces [allergen]”. The least risky for interviewees was the label ”manufactured in the same facility” as only 30% assigned this as a ”high” or ”extreme” risk. Fig. 4 shows how interviewees profiled the risk associated with common Australian PAL labels.
Fig. 4.
Purchasing of products labelled with … [allergen]
Medical challenges
Of the 314 parents who said their child possessed an adrenaline auto-injector, 292 (93.0%) correctly identified the sequence needed to activate. Nine parents gave an incorrect response, and 13 chose not to answer this question.
For the 306 who had used an adrenaline auto-injector, 135 (44.1%) reported they had hesitated. While multiple reasons exist why parents delay administering adrenaline, the main reason for hesitancy was ”not wanting to over-react” (n = 80, 59.3%), followed by ”symptoms have settled in the past” (n = 61, 45.2%) and the ”inability to decide” (n = 51, 37.7%). Although fear was not a major reason (n = 12, 8.8%), it did surface for those who selected ”other reasons” who also expressed uncertainty as to when to use an auto-injector, how long one should wait before administering, and at what time does a reaction become critical.
-
•
“Confusion over whether to administer before symptoms worsen, or to wait for near death!” [Regional Participant No: 172, Male, Teenager]
-
•
“When the reaction is on the cusp of moderate to severe, it is trying to decide if antihistamine will be enough. Administering adrenaline is not the challenge, so much as the resulting trip to the hospital, and organising care for siblings for a delayed onset reaction during the middle of the night.” [Capital City Participant No: 250, Male, 8–12 years]
One reason why such indecision exists could be the lack of a universal classification scheme leading parents to assess symptoms subjectively. Such differences in classifying symptom severity were confirmed, and these results are published.
GP engagement
From the 318 parents who completed the online survey, 102 interviewees answered questions on their interaction with their GP. Analysing GP engagement using a thematic approach, aided by NVivo Pro 11, identified 3 primary themes: limited assistance, power/control and trust, and supportive relationships.
When responses were coded and thematically analysed, 58 (56.8%) interviewees perceived little or no assistance from their GPs in managing their food-allergic child. Regional participants were more likely to report limited GP assistance (n = 29/42, 69.0%), while 2 never visited GPs; instead, they relied on naturopathic interventions.
For this group of interviewees, the perception was that they were not an equal partner in the relationship as they needed to overcome frustration and ridicule:
-
•
“Did not take it seriously … I was almost laughed at and told that reactions were highly unlikely.”; [Interviewee No: 16, Regional VIC, Mother of Child aged 3 years, Male, Diagnosed at 7 months]
However, it was not only the need to convince GPs that food allergy was likely but also the concern over the perception that GPs lacked the requisite knowledge in how to deal with food allergy. To overcome these perceptions, interviewees identified the need for ongoing professional development.
In contrast, the perception for 42 interviewees (41.2%) was that GP interaction focused not only on the clinical nature of symptoms but also on QoL as food allergy is more than just about managing food. For these interviewees, the doctor-patient relationship focused on equality, respect, trust, and support, with 1 interviewee reporting their GP was:
-
•
“Aware of problem and reactions … supportive, provides advice about trial availability … not made to feel silly … understands it is challenging as a parent”; [Interviewee No: 33, Regional NSW, Mother of Child aged 2 years, Male, Diagnosed at 11 months]
The key difference was whether the relationship was akin to a health partnership or a ”revolving door” experience.
Food challenges
For 188 parents (n = 334, 56.3%) who reported their child had been through a food challenge, 161 reported this was supervised. However, irrespective of whether the food challenge was supervised or unsupervised, parents reported feeling ”nervous” (n = 73, 38.8%) or ”apprehensive/fearful” (n = 44, 23.4%). Despite parents reporting these feelings, there was an overwhelming need to confirm or refute their child’s food allergy, with only 6 reporting they would not go through another food challenge.
For 94 parents, there was a positive outcome to the food challenge, as their child could now eat that food. However, distribution of feelings (”relief”, ”excitement”, ”anxious/uneasy” or ”scared”) was not equal (chi-square test, p < 0.001), with the overwhelming response being ”relief” (n = 59, 62.8%), followed by ”excitement” (n = 24, 25.5%) and ”anxious/uneasy” (n = 11, 11.7%). No parent reported feeling ”scared”. Despite being able to eat the food, 7 of the 53 participants who reported feeling ”nervous” or ”apprehensive/fearful” at the time of the food challenge remained ”anxiou”’ when reintroducing the allergenic food into their child’s diet.
Regional participants were more likely to feel ”anxious” about their child being able to eat that food (n = 5/33, 15.2%) compared to those living in capital cities (n = 6/61, 9.9%) although this was not statistically significant (chi-square test, p = 0.449). However, further research is warranted as the underlying differences could be influenced by gender as the 5 regional children were all males, by limited access to medical services or by the small sample size.
Immunotherapy
Preventing or reducing the severity of an allergic reaction is the goal of immunotherapy. For 334 participants, they responded to the question of whether parents would enrol their child in a clinical trial aimed at desensitisation. For this protocol, increased doses of the food allergen would be given, and 234 parents (70.1%) would participate in the hope of increasing the threshold before reacting (n = 177). However, of the 100 who declined, 51 thought it was ”too risky”, and 22 selected they could ”live with food avoidance”, while nine selected both reasons. Surprisingly, those from capital cities were more likely to decline (n = 64/199, 32.2%) compared to those from regional locations (n = 36/135, 26.7%), even though it was not significant (chi-square test, p = 0.282).
However, there was a significant drop (chi-square test, p < 0.001) when 332 participants were asked if they would enrol in a clinical trial using a vaccine. Of these, 186 (56.0%) said ”yes” they would enrol their child in a vaccine trial, with 149 (80.1%) in the hope of a cure. However, 71 from the 146 who declined thought this was ”too risky”. Regional participants were more likely to decline (n = 65/134, 48.6%) compared to those from capital cities (n = 81/198, 40.9%). While this was not significant (chi-square test, p = 0.122), there is the tyranny of distance and the need to travel to participating clinics.
Managing an egg allergy also surfaced as a distinguishing factor with 74 (n = 155, 47.7%) declining the opportunity to participate in a vaccine trial, compared to 93 (n = 234, 39.8%) of participants reporting an allergy to peanut (chi-square test, p = 0.124). While specific allergens may have influenced the decision to participate, parents who reported multiple allergies to 3 or more allergens the declination rate of 77 (n = 146, 52.7%) was high, although not significant (chi-square, p = 0.300).
Anaphylaxis register
Signing up to a national Anaphylaxis Register was recognised as a positive step by 262 (n = 332, 78.9%). The ability to select multiple reasons saw 2 primary reasons emerge. These were to ”influence government policies in health and education” (n = 232/262, 88.5%) and report on ”how many people are affected by food allergy” (n = 224/262, 85.5%). For those who declined, ”privacy” remained the most prominent barrier (n = 32/69, 46.4%) as parents did not know who would have access to such a register. Location played no consideration for those who declined to participate when percentages were weighted (chi-square, p = 0.624).
Increasing public awareness of food allergies
To improve education and awareness, interviewees were asked to create an advertising slogan. The purpose was left to the interviewee, and different themes emerged when analysed. Theme 1 used ”shock tactics” to convey the message that food allergy can kill, and with this, parents resorted to analogies including ”like holding a gun, it can kill!” or ‘like stepping in front of a semi-trailer doing 100 km/h". Both have graphical elements designed to shock others into taking care. Theme 2 looked at the need for education to improve awareness and revolved around "food allergy is not a myth, it is real” while Theme 3 looked for support and inclusiveness with the focus around the fact that food allergy "can be managed with your help".
Role of school in managing a child’s food allergy
The transition to school is an important milestone, and for 157 parents (n = 301, 52,2%), food allergy had influenced their choice of preschool. For many (n = 116/157, 73.9%), a primary consideration was school policies. This transition away from 24/7 parental care to preschool was challenging as they reported feeling "apprehensive/fearful” (n = 70/157) or "nervous” (n = 60/157).
Knowing their child had food allergy also influenced the decision of 119 parents (n = 119/247, 48.2%) when considering which primary school to enrol in. With 96 (80.7%) of the 119 parents reporting reliance on school policies, this was significant (chi-square test, p < 0.001). Choosing a primary school known to have other children with food allergy was also a consideration for 57 (47.9%) parents, however, less so for high school (n = 13, 43.3%).
The number of children in public government schools (n = 43, 42.6%) was lower than those in private schools (n = 53, 55.8%), with 4 preferring not to answer and 1 leaving the question blank. While there was no difference between whether the school was public or private (chi-square test, p = 0.307), distribution was significant (chi-square test, p = 0.046) with more parents living in a capital city (n = 40/64, 62.5%) choosing a private school.
Discussion
Managing food allergy is challenging as parents navigate not only different social contexts but also contextualise risk, which is dynamic and situational.4,18 One concern that parents repeatedly identified when managing food allergy was the need to trust third parties, whether this was in the school environment, social interaction with members of the public, or manufacturers. This loss of control and the need to rely on others highlights the quandaries parents face in social situations when going on holidays, eating out at restaurants, and/or leaving their child in the care of others.6,10,19 However, when parents are shunned, labelled a ”helicopter parent” or worse still, not believed, this creates a heightened sense of anxiety and fear and can significantly impact QoL, increase social isolation, and lead to feelings of guilt.6,20
Not only do parents need to convince others of the seriousness of allergens they must also rely on manufacturers to notify whether trace allergens are present, either through cross-contamination during the manufacturing process or through the supply chain.21, 22, 23 However, even where manufacturers voluntarily adopt PAL, Zurzolo et al (2018) found that the risk of an adverse food reaction to unlisted ingredients in packaged food was no lower for foods with PAL than for foods with no PAL.24 This failure to accurately declare allergens may account for why participants in our study chose to ignore these labels.
However, risk profiling based on PAL labels is not unique. Noimark et al (2009), Heffle et al (2007), and Zurzolo et al (2016) reported up to 50% of parents ignored the label ”may contain traces of nuts”,22,25,26 and although lower than our study, such differences may be influenced by the type of allergen or changing specialist advice to maintain tolerance.26 In contrast, Hefle et al (2007) and Zurzolo et al (2013) reported more parents ignored the PAL ”made on the same equipment”,25,27 and this conflicted with results from our study as fewer parents purchased products with this label. To determine if results reflect a change in behaviour over the reporting period, from pre-2013 to 2015 or a sampling error, this contradiction to previous results would benefit from further research.
However, where a food-related allergic reaction does occur, all too often parents delay using an adrenaline auto-injector. In Song et al (2014), barriers to adrenaline use were identified, including different perceptions on symptom classification.28 In another study, Kim et al (2005) found there was a positive correlation between empowerment and the ability to not only make informed decisions (P < 0.0005) but also the comfort level when using an adrenaline auto-injector.29 With 37.7% of parents reporting the ”inability to decide” as the main reason they delayed using such a device, empowering parents is crucial.
To improve outcomes, medical professionals also have an important role as they support patients, acknowledge concerns, and address information needs.30,31 However, medical professionals need to overcome findings reported by Baricic et al (2015) and Lozinsky et al (2015) where parents were made to feel as though they were overreacting and GPs failed to correlate or consider the described symptoms as food allergy.32,33 It is these perceptions that also resonated with interviewees. However, managing a child’s food allergy is also about personal conviction and how to manage uncertainty and risk.
One area of interest is how locus of control (LOC) applies to parental strategies.34,35 Parents with an internal LOC could naturally be better at managing in a crisis when compared to those who rely externally on others to take control of the situation.34,35 Knibb et al (2016) found a strong self-efficacy was an important determinant in managing food allergy, possibly accounting for over one-third of QoL variance in social activities.34 Fedele et al (2016), also identified 4 patterns of adaption based on food allergy management strategies and psychosocial functioning as parents who were optimistic had a better QoL score compared to those who reported high anxiety, a sense of loss, and hyper-vigilance.35 Results from our study support these findings as worsening QoL scores referenced ”guilt” and ”burden”, while better QoL scores identified positive aspects such as healthy eating.
Despite worsening QoL, participation rates for a vaccine trial for those managing an egg allergy was low. This low uptake may be due to hope given Peters et al (2014) demonstrated infants who could regularly tolerate baked egg were more likely to outgrow their egg allergy.36 Alternatively, it may also be that current strategies are already inducing tolerance. However, exploring the underlying reasons why worsening QoL37,38 did not equate to a search for a cure is an area for further investigation.
A key strength of this Australia-wide study was the inclusion of participants outside large metropolitan centres. The exploration of multiple topics uncovered current perceptions around health behaviours, knowledge, and perceptions, which are fundamental in safeguarding against psychosocial stressors.39 However, an open survey has limitations and included the inability to determine response rates and motivation behind those who, not only completed the online survey but also chose to be interviewed, and this may limit generalisations. Nor were we able to confirm IgE-mediated allergy status; however, the use of an adrenaline auto-injector served as a proxy.
The length of the survey and only being in English may have discouraged participants from completing the survey. To maximise participation rates in future studies, researchers should consider translated versions of the survey. Finally, as perceptions change over time, a longitudinal approach should be considered to elucidate further the parental burden of managing a child with a food allergy.
Conclusion
This study adds value to the current knowledge of QoL in managing food allergies, offering a uniquely Australian perspective. A key finding of this study was the importance of social acceptance as parents internalised risk when navigating challenges in keeping their child safe. The importance of health literacy,5,40 empowerment29,37 and external support from community members,41 and food manufacturers,21 builds confidence and overcomes parental fear as parents tackle the reported challenges when managing a child with food allergy.
Consent for publication
All authors have provided their consent for publication of this manuscript.
Availability of data and materials
The authors confirm that data and materials relevant to this manuscript are available within the manuscript and supplementary materials provided
Funding
Not applicable
Ethics
Study was approved by the Charles Sturt University Human Ethics Committee (protocol number: H2015004).
Author contributions
DS, along with CHK, MDS, and TV, developed the study design. DS, facilitated by CHK, was responsible for notification of the survey via the medical fraternity, childcare providers, the food allergy community and the patient support organisation, Australia Allergy & Anaphylaxis. DS performed the research, analysis and drafted the manuscript, which was critically reviewed by all prior to the submitted manuscript.
Acknowledgements
The authors thank all participants for taking the time to complete this survey. We also thank Allergy & Anaphylaxis Australia for their encouragement and support. D. Stockhammer is a recipient of an Australian Government Research Training Program Scholarship.
Declaration of competing interest
None.
Footnotes
Full list of author information is available at the end of the article.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.waojou.2020.100468.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Burks A.W., Tang M., Sicherer S. ICON: food allergy. J Allergy Clin Immunol. 2012;129:906–920. doi: 10.1016/j.jaci.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Benedé S., Blázquez A.B., Chiang D., Tordesillas L., Berin M.C. The rise of food allergy: environmental factors and emerging trends. Lancet. 2016;7:27–34. doi: 10.1016/j.ebiom.2016.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang M.L.K., Mullins R.J. Food allergy: is prevalence increasing? Intern Med J. 2017;47:256–261. doi: 10.1111/imj.13362. [DOI] [PubMed] [Google Scholar]
- 4.Sicherer S.H., Sampson H.A. Food allergy: a review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J Allergy Clin Immunol. 2018;141:41–58. doi: 10.1016/j.jaci.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Peterson C.C. July 2016. Psychological Aspects of Food Allergy Management. Euroscicon Food Allergy and Hypersensitivity Summit. 5 – 7. London UK. [Google Scholar]
- 6.Abrams E.M., Simons E., Roos L., Hurst K., Protudjer J.L.P. Qualitative analysis of perceived impacts on childhood food allergy on caregiver mental health and lifestyle. Ann Allergy Asthma Immunol. 2020 Jun;124:594–599. doi: 10.1016/j.anai.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 7.Woolley K., Fishbach A., Wang R.M. Food restriction and the experience of social isolation. J Pers Soc Psychol. 2019 doi: 10.1037/pspi0000223. [DOI] [PubMed] [Google Scholar]
- 8.Waters E.A., Muff J., Hamilton J.G. Multifactorial beliefs about the role of genetics and behavior in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviors. Genet Med. 2014;16:913–921. doi: 10.1038/gim.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furlong T.J., McMorris M.S., Greenhawt M.J. Self-reported allergic reactions to peanuts and tree nuts occurring in restaurants and food service establishments. J Allergy Clin Immunol. 2008;121(Suppl 1):S248. doi: 10.1016/j.jaci.2007.12.981. [DOI] [PubMed] [Google Scholar]
- 10.McAdams B., Deng A., MacLaren T. Food allergy knowledge, attitudes, and resources of restaurant employees. Br Food J. 2018;120:2681–2694. doi: 10.1108/BFJ-01-2018-0028. [DOI] [Google Scholar]
- 11.Soon J.M. ‘No nuts please’: food allergen management in takeaways. Food Contr. 2018;91:349–356. doi: 10.1016/j.foodcont.2018.04.024. [DOI] [Google Scholar]
- 12.Regional Population Growth, Australia 2015-2016. Australian Bureau of Statistics; Canberra: 2016. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3218.02015-16?OpenDocument&tabname=Summary&prodno=3218.0&issue=2015-16&num=&view [Google Scholar]
- 13.Cohen B.L., Noone S., Muñoz-Furlong A., Sicherer S.H. Development of a questionnaire to measure quality of life in families with a child with food allergy. J Allergy Clin Immunol. 2014;114:1159–1163. doi: 10.1016/j.jaci.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 14.Atif A. Geelong; 3-5 December 2012. Estimating Non-response Bias in a Web-Based Survey of Technology Acceptance: A Case Study of Unit Guide Information Systems. 23rd Australasian Conference on Information Systems. [Google Scholar]
- 15.Greenhawt M. Food allergy quality of life and living with food allergy. Curr Opin Allergy Clin Immunol. 2016;16:284–290. doi: 10.1097/ACI.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 16.Warren C.M., Otto A.K., Walkner M.M., Gupta R.S. Quality of life among food allergic patients and their caregivers. Curr Allergy Asthma Rep. 2016;16 doi: 10.1007/s11882-016-0614-9. [DOI] [PubMed] [Google Scholar]
- 17.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 18.Henwood K., Pidgeon N., Sarre S., Simmons P., Smith N. Risk, framing and everyday life: epistemological and methodological reflections from three socio-cultural projects. Health Risk Soc. 2008;10:421–438. doi: 10.1080/13698570802381451. [DOI] [Google Scholar]
- 19.Leitch I.S., Walker M.J., Davey R. Food allergy: gambling your life on a take-away food. Int J Environ Health Res. 2005;15:78–87. doi: 10.1080/09603120500062052. [DOI] [PubMed] [Google Scholar]
- 20.Shu D.M. When food is a weapon: parental liability for food allergy bullying. Marquette Law Rev. 2019;103 doi: 10.2139/ssrn.3445605. [DOI] [Google Scholar]
- 21.Allen K.J., Remington B.C., Baumert J.L. Allergen reference doses for precautionary labeling (VITAL 2.0): clinical implications. J Allergy Clin Immunol. 2014;133:156–164. doi: 10.1016/j.jaci.2013.06.042. [DOI] [PubMed] [Google Scholar]
- 22.Noimark L., Gardner J., Warner J.O. Parents’ attitudes when purchasing products for children with nut allergy: a UK perspective. Pediatr Allergy Immunol. 2009;20:500–504. doi: 10.1111/j.1399-3038.2008.00796.x. [DOI] [PubMed] [Google Scholar]
- 23.Tonkin E., Webb T., Coveney J., Meyer S.B., Wilson A.M. Consumer trust in the Australian food system – the everyday erosive impact of food labelling. Appetite. 2016;103:118–127. doi: 10.1016/j.appet.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Zurzolo G.A., Allen K.J., Peters R.L. Anaphylaxis to packaged foods in Australia. J Paediatr Child Health. 2018;54:551–555. doi: 10.1111/jpc.13823. [DOI] [PubMed] [Google Scholar]
- 25.Hefle S.L., Furlong T.J., Niemann L., Lemon-Mule H., Sicherer S., Taylor S.L. Consumer attitudes and risks associated with packaging foods having advisory labeling regarding the presence of peanuts. J Allergy Clin Immunol. 2007;120:171–176. doi: 10.1016/j.jaci.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 26.Zurzolo G.A., de Courten M., Koplin J.J., Allen K.J. Is advising food allergic patients to avoid food with precautionary allergen labelling out of date? Curr Opin Allergy Clin Immunol. 2016;16:272–277. doi: 10.1097/ACI.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 27.Zurzolo G.A., Koplin J.J., Mathai M.L., Tang M.K.L., Allen K.J. Perceptions of precautionary labelling among parents of children with food allergy and anaphylaxis. Med J Aust. 2013;198:621–623. doi: 10.5694/mja12.11669. [DOI] [PubMed] [Google Scholar]
- 28.Song T.T., Worm M., Lieberman P. Anaphylaxis treatment: current barriers to adrenaline auto-injector use. Allergy. 2014;69:983–991. doi: 10.1111/all.12387. [DOI] [PubMed] [Google Scholar]
- 29.Kim J.S., Sinacore J.M., Pongracic J.A. Parental use of EpiPen for children with food allergies. J Allergy Clin Immunol. 2005;116:164–168. doi: 10.1016/j.jaci.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 30.Shaker M., Schwartz J., Ferguson M. An update on the impact of food allergy on anxiety and quality of life. Curr Opin Pediatr. 2017;29:497–502. doi: 10.1097/MOP.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 31.Hu W., Grbich C., Kemp A. When doctors disagree: a qualitative study of doctors’ and parent views on the risks of childhood allergy. Health Expect. 2008;11:208–219. doi: 10.1111/j.1369-7625.2008.00506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baricic T.V., Catipovic M., Cetinic E.L., Krmek V., Horvat I. Parental perception, prevalence and primary care physician’s knowledge on childhood food allergy in Croatia. Children. 2015;2:305–316. doi: 10.3390/children2030305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lozinsky A.C., Meyer R., Anagnostou K. Cow’s milk protein allergy from diagnosis to management: a very different journey for General Practitioners and parents. Children. 2015;2:317–329. doi: 10.3390/children2030317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knibb R.C., Barnes C., Stalker C. Parental self-efficacy in managing food allergy and mental health predicts food allergy-related quality of life. Pediatr Allergy Immunol. 2016;27:459–464. doi: 10.1111/pai.12569. [DOI] [PubMed] [Google Scholar]
- 35.Fedele D.A., McQuaid E.L., Faino A. Patterns of adaptation to children’s food allergies. Allergy. 2016;71:505–513. doi: 10.1111/all.12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peters R.L., Dharmage S.C., Gurrin L.C. The natural history and clinical predictors of egg allergy in the first 2 years of life: a prospective, population-based cohort study. J Allergy Clin Immunol. 2014;133:485–491. doi: 10.1016/j.jaci.2013.11.032. [DOI] [PubMed] [Google Scholar]
- 37.Warren C.M., Gupta R.S., Sohn M.W. Differences in empowerment and quality of life among parents of children with food allergy. Ann Allergy Asthma Immunol. 2015;114:117–125. doi: 10.1016/j.anai.2014.10.025. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leonard S.A. Debates in allergy medicine: baked milk and egg ingestion accelerates resolution of milk and egg allergy. World Allergy Organ J. 2016;9:1. doi: 10.1186/s40413-015-0089-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gillespie C.A., Woodgate R.L., Chalmers K.I., Watson W.T. ‘Living with risk’: mothering a child with food-induced anaphylaxis. J Pediatr Nurs. 2007;22:30–42. doi: 10.1016/j.pedn.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 40.DeWalt D.A., Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(Suppl 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 41.VanderKaay S. Mothers of children with food allergy: a discourse analysis of occupational identities. J Occup Sci. 2016;23:217–233. doi: 10.1080/14427591.2015.1119713. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that data and materials relevant to this manuscript are available within the manuscript and supplementary materials provided