Abstract
A 42-year-old man exhibiting hypoxia was diagnosed with coronavirus disease 2019. He had medical histories of type 2 diabetes, hyperlipidemia, hyperuricemia, and gout attack. He received favipiravir for compassionate use for 14 days. Subsequently, he showed increased uric acid levels and developed acute gouty arthritis. Favipiravir may induce not only hyperuricemia but also acute gouty arthritis. It should therefore be used with caution in patients with a history of gout and those with hyperuricemia, especially when used at a higher dose and for a longer duration than is typical.
Keywords: acute gouty arthritis, coronavirus disease 2019 (COVID-19), favipiravir, hyperuricemia, severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2)
Introduction
Favipiravir, a pyrazine derivative that inhibits viral RNA-dependent RNA polymerase, was originally developed for influenza in Japan (1). At present, this drug is approved only for novel influenza in Japan. However, considering its broad-spectrum antiviral effect, favipiravir has been used in cases of Ebola or a severe fever with thrombocytopenia in clinical trials (2). In addition, it has begun to be used for coronavirus disease 2019 (COVID-19) for compassionate use or in clinical trials, mainly in Japan and China, despite its unproven effectiveness (3, 4).
One of the major adverse events of favipiravir in humans is hyperuricemia apart from potential teratogenicity and embryotoxicity (5). Nonetheless, the blood uric acid level increases only temporarily after favipiravir treatment, and gout attack is considered unlikely to occur (6). In fact, gout attack related to favipiravir use has never been reported.
We herein report a 42-year-old man who was diagnosed with COVID-19 and eventually developed acute gouty arthritis during favipiravir treatment.
Case Report
This 42-year-old man complained of a 1-week history of a fever, general malaise, and shortness of breath. He had medical histories of type 2 diabetes, hyperlipidemia, hyperuricemia, and gout attack and was on alogliptin benzoate, luseogliflozin, rosuvastatin, and febuxostat treatment. His hyperuricemia was well controlled, with no gout attack for more than one year.
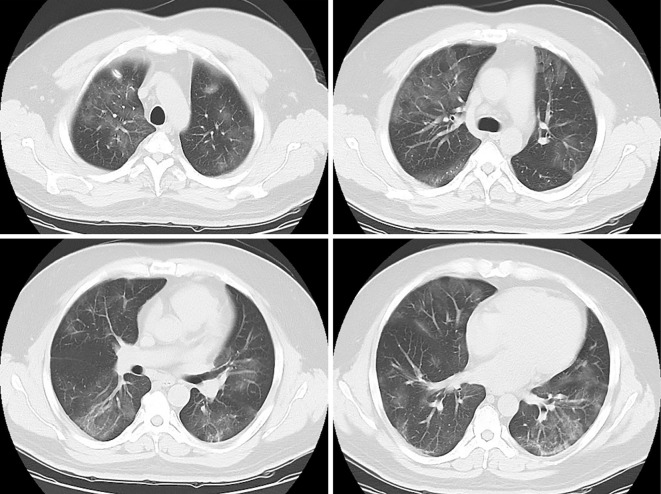
His vital signs on admission were as follows: blood pressure, 114/65 mmHg; heart rate, 116 beats/min; body temperature, 36.5 °C; respiratory rate, 18 breaths/min; and oxygen saturation with 2 L of oxygen, 95%. His uric acid level was 6.0 mg/dL. Computed tomography revealed a diffusely distributed crazy-paving appearance on both lungs (Fig. 1). A polymerase chain reaction analysis for severe acute respiratory syndrome coronavirus 2 was performed on admission, and the patient tested positive on hospital day 3.
Figure 1.
Computed tomography. Findings showed a diffusely distributed crazy-paving appearance on both lungs.
On hospital day 3, favipiravir was started for compassionate use (1,800 mg twice a day on administration day 1 and 800 mg twice a day after). His fever improved, and all of his symptoms disappeared on hospital day 5. However, on hospital day 13, his uric acid level elevated up to 8.3 md/dL. Favipiravir was continued for 2 weeks until hospital day 16. On hospital day 15, he felt pain on his left foot. A physical examination revealed a reddish and swollen left metatarsophalangeal (MTP) joint (Fig. 2). He was then clinically diagnosed with acute gouty arthritis and prescribed nonsteroidal anti-inflammatory drugs (NSAIDs). The pain and swelling improved until hospital day 20. Subsequently, the patient recovered and was discharged on hospital day 22.
Figure 2.

Image of acute gouty arthritis. A physical examination revealed a swollen left metatarsophalangeal joint.
Written informed consent was obtained from the patient for publication of this case report.
Discussion
The clinical course of our patient suggests that favipiravir treatment may induce not only hyperuricemia but also acute gouty arthritis. With a longer duration of administration and higher dose of treatment, these adverse effects may become aggravated.
Hyperuricemia is a major adverse event induced by favipiravir, possibly caused by both excessive uric acid production and decreased uric acid excretion. Regarding the mechanism, favipiravir and its metabolite, favipiravir hydroxide, inhibit organic anion transporter (OAT) 1 and OAT3, leading to the decreased tubular secretion of uric acid, and favipiravir hydroxide also enhances uric acid reabsorption mediated by a urate transporter, collectively resulting in decreased uric acid excretion (6). Favipiravir treatment transiently increases uric acid levels (6). However, data concerning favipiravir-induced hyperuricemia causing clinical manifestations are unavailable (6). In our patient, the uric acid levels increased after the favipiravir treatment commenced, and acute gouty attack even occurred during such treatment. Favipiravir may therefore induce not only hyperuricemia but also acute gouty arthritis as a clinical manifestation.
A longer duration and higher dose of favipiravir treatment may induce acute gouty arthritis. In 2014 in Japan, favipiravir was approved for novel influenza, and the usual adult dosage is 1,600 mg administered orally twice daily on day 1, followed by 600 mg orally twice daily from day 2 to day 5 (5). This regimen was selected by most of the previous clinical trials of favipiravir for influenza (7). In our patient, we administered 1,800 mg of favipiravir orally twice daily on day 1, followed by 800 mg orally twice daily from day 2 to day 14 according to the interim guidance of the Japanese Society of Infectious Diseases (8). Theoretically, given that uric acid is elevated dose-dependently and transiently, a higher dose and a longer duration of this drug can worsen the adverse effects. Thus, caution should be paid when favipiravir, with higher doses and longer duration, is used for COVID-19.
The efficacy and safety of favipiravir for patients with COVID-19 have not been sufficiently confirmed. A recent open-label control study showed that favipiravir resulted in a better therapeutic response for COVID-19 in terms of disease progression and viral clearance than lopinavir/ritonavir (9). However, that study was not a randomized control trial (RCT), and ongoing RCTs have not yet reached the desired conclusion. Our patient had severe bilateral pneumonia and hypoxia; we therefore administered favipiravir for compassionate use and conducted an observational study. However, further research is necessary to confirm the effectiveness of favipiravir as a therapeutic option for COVID-19.
One limitation of our case report concerns the clinical diagnosis of acute gouty arthritis. For an accurate diagnosis, arthrocentesis should be performed. However, the presence of MTP joint pain, which occurred after the elevation of uric acid levels and improved right after taking NSAIDs, strongly suggested that the patient indeed had acute gouty arthritis. Through the use of a previously developed diagnostic rule (10), this patient obtained a total score indicating high gout probability.
In conclusion, we herein report the case of a patient with COVID-19 who exhibited elevated uric acid levels and developed acute gouty arthritis during favipiravir treatment. Favipiravir should thus be administered with caution in patients with gout history and those with hyperuricemia, especially when used at a higher dose and for a longer duration than usual.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Furuta Y, Gowen BB, Takahashi K, Shiraki K, Smee DF, Barnard DL. Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antiviral Res 100: 446-454, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Furuta Y, Komeno T, Nakamura T. Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proc Jpn Acad Ser B Phys Biol Sci 93: 449-463, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edagawa S, Kobayashi F, Kodama F, et al. Report of 15 cases of Covid-19 including 3 cases requiring mechanical ventilation. Transfer 10:13, 2020 [updated 2020 Mar 19; cited 2020 May 7]. Available from: http://www.kansensho.or.jp/uploads/files/topics/2019ncov/covid19_casereport_en_200402.pdf [DOI] [PMC free article] [PubMed]
- 4. Khambholja K, Asudani D. Potential repurposing of Favipiravir in COVID-19 outbreak based on current evidence. Travel Med Infect Dis Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avigan (favipiravir) [prescribing information]. Toyama Chemical Co. Ltd., Tokyo, Japan, 2014. [Google Scholar]
- 6.Japanese Pharmaceuticals and Medical Devices Agency (PMDA).Report on the Deliberation Results [Internet]. [updated 2014 Mar 4; cited 2020 May 7]. Available from: https://www.pmda.go.jp/files/000210319.pdf
- 7. Hayden F, Shindo N. Influenza virus polymerase inhibitors in clinical development. Curr Opin Infect Dis 32: 176-186, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. The Japanese Association for Infectious Diseases. Interim guidance of antiviral drugs for COVID-19 Ver1. 2020 [Internet]. [updated 2020 Feb 26; cited 2020 Mar 13]. Available from: http://www.kansensho.or.jp/uploads/files/topics/2019ncov/covid19_antiviral_drug_200227.pdf (in Japanese)
- 9. Cai Q, Yang M, Liu D, et al. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Janssens HJ, Fransen J, Van de Lisdonk EH, van Riel PL, van Weel C, Janssen M. A diagnostic rule for acute gouty arthritis in primary care without joint fluid analysis. Arch Intern Med 170: 1120-1126, 2010. [DOI] [PubMed] [Google Scholar]