Abstract
Although pain is defined as a sensory and emotional experience, it is traditionally researched and clinically treated separately from emotion. Conceptual and mechanistic relationships between these constructs highlight the need for better understanding of their bi-directional influences and the value of bridging the pain and emotion research and clinical communities.
Pain is a natural, adaptive response that protects our body from actual or potential tissue injury. However, when pain persists, it can lead to suffering and to substantial clinical and economical burdens, at both personal and societal levels (Mackey and Kao, 2019). Many people consider pain to be purely physical, but since pain can be reported in the absence of noxious sensory activations, pain is actually defined as an unpleasant subjective experience with a sensory and an emotional component (www.iasp-pain.org/terminology). Indeed, mental or better yet psychological health comorbidities, especially anxiety, depression, and anger, are highly prevalent in people with chronic pain (Gatchel et al., 2007). However, how can we fully understand what pain is, if the age-old question “what is an emotion?” is still vigorously debated (Shackman and Wager, 2019)? Critically, how does this impact our understanding of the relationship between pain and emotion?
We begin by reiterating the difference between pain and nociception (Baliki and Apkarian, 2015), which is helpful when considering the complex conceptual, functional, and neurophysiological relationship between pain and emotion. We suggest several perspectives on the nature of this relationship and call for further scrutiny of their bi-directional influence. The inherent connection between pain and emotion emphasizes the need for closer interactions between the traditionally siloed fields of pain and emotion, which we believe will lead to substantial progress in the theoretical, empirical, and clinical understanding of their normative and pathological manifestations.
Differentiating Pain from Nociception
Underlining the difference between pain and nociception is crucial, since colloquially (and in many textbooks), the terms still tend to be used interchangeably. Nociception is defined as the neurophysiological process of encoding noxious stimuli that produce actual or potential tissue injury. The word noxious derives from the Latin word noxa, associated with meanings of harm, hurt, injury, and damage. Counter to the false dualistic inclination to separate subjective experiences into physical and mental categories, these words clearly associate with both somatic and emotional harms. We are hurt and in pain when we are interpersonally insulted, as when we are physically injured. Although language is key for articulating subjective experiences, we should avoid essentialism: our nervous system is the primary determinant of our experiences. We therefore highlight that nociception refers to peripheral neurophysiological pathways embedded in the sensory nervous system that encode objective information about the physical properties of various stimuli (thermal, mechanical, chemical, and/or electrical) and relay this information from the body (transduction) to the spinal cord (transmission). We refer to a normatively functioning system, though variability in the encoding process can result from pathophysiology (from birth or acquired through development or injury) or other factors impacting individual differences (genetic, neuroanatomical, and other biological or potentially psycho-socio-cultural factors). Importantly, as in other sensory modalities (vision, audition), nociception generates biological signals that mediate between events in the external world and an organism’s internal milieu. Downstream reflexive behavior is then generated to protect the organism and thus increases evolutionary fitness. In most animals, including humans, response to and modulation of nociception can occur before and probably without perception, making it highly conserved across species.
Pain is a more “reflective” process that in many cases (but not always) is a result of perceiving nociceptive information, whether the source of this input is external (e.g., an electric shock) or from within our body (e.g., a torn muscle). When the brain processes this information, we can consciously experience the stimulus as painful and ponder its location, intensity, sensory and emotional qualities, and any other characteristic feature. It is then that complex behavioral expressions (e.g., facial, bodily, verbal) might manifest. Individual differences should also be considered. One person submerging their hand in a 3°C cold-water bath cries out in anguish, rating the pain as 9 on a 0 to 10 scale from “no pain” to “worst pain imaginable,” whereas another person barely moves a muscle, rating it as a 1 on the same scale. People might experience pain differently depending on various socio-cultural factors, such as whether a supportive loved one is present in the room or whether one has been continuously exposed to discriminatory health care. Cognitions, such as thoughts (e.g., how much it hurts, whether it will end), beliefs (e.g., pain reflects tissue damage, physical exercise makes it worse), and expectations (e.g., placebo and nocebo effects) are additional important modulators of pain. Notably, we can calibrate the average kinetic energy of H2O molecules to 3°C. But can we truly know what the qualitative experience is for another person submerging their hand in water at that temperature? Can we truly know how painful it is for them? There are various philosophical perspectives on such questions. Nevertheless, we can imagine pain, bring it back to memory, or even resonate with another person’s experience and expressions of pain, considered the basis for empathic processing.
All the above emphasizes that there is no direct one-to-one relationship between nociception and pain, that pain is a learned process shaped over the lifespan, and that biological, psychological, and socio-cultural factors (and their interactions) impact both acute and chronic pain (Gatchel et al., 2007). Therefore, pain is a contextualized, multidimensional construct resulting from interactions of peripheral and central nervous systems with potential external factors, but that in itself cannot be reduced to peripheral activity in sensory pathways.
Pain and Emotion
Debates about the nature of emotion began early in religion and philosophy in both Eastern and Western ancient worlds and is still very much alive today. For example, basic emotion perspectives view emotions such as fear, sadness, and anger as unique mental states with specific underlying mechanisms that cannot be decomposed into more basic ingredients. On the other hand, constructionist perspectives do not view emotions as unique in form, function, or cause but rather as built by more basic ingredients that are not specific to emotions, such as valence and arousal. A summary of contemporary theoretical perspectives and of key open questions is beyond our current scope and is provided elsewhere (Gross and Barrett, 2011; Shackman and Wager, 2019). Nevertheless, most perspectives hold that emotional experiences are outcomes of interactions between somatovisceral patterns mediated by functionality of the peripheral nervous system, as well as cognitive processes (e.g., memory and attention) and meta-cognitive attributions (e.g., appraisals or evaluations) mediated by functionality of the central nervous system (CNS). Within the CNS, emotional states preferentially engage subcortical circuits that seem to be dedicated to adaptive behaviors, such as the fight-freeze-flight survival responses. Emotions can thus be evoked by physiological states (e.g., hunger or thirst), by events in the environment (e.g., a roaring lion or an interpersonal insult), as well as by cognitive processes (e.g., imagining, remembering, or expecting an emotion-inducing situation), making them functionally adaptive to various stressors. Theories vary in the influence given to socio-cultural and contextual factors and in the emphasis given to variability within and between emotion categories. Emotional experiences also frequently co-occur with various behavioral expressions (facial, bodily, verbal).
Clearly, the constructs pain and emotion are substantially overlapping, conceptually and functionally. Importantly, as pain cannot be reduced to the characteristics of a noxious stimulus, so an emotion such as fear cannot be reduced to a particular eliciting stimulus—a roaring lion can be a joyous experience when on a safari. Similarly, nociception can be pleasurable, such as for practitioners of masochism, and can even generate relief, as is the case in deliberate self-harming behaviors (often characterizing borderline personality disorder). This raises the question: in what way, if any, is pain different from any other emotion? One potential response is that pain is sensed by and referred to localizations within the body. However, pain can be experienced even in a limb that was amputated, as demonstrated by phantom pain. At the same time, emotions seem to have differential somatic referents within the body. Thus, perhaps it is the pattern of somatosensory referents and their associated neural manifestations that differentiates between various painful and emotional experiences, rather than the presence or absence of a somatic referent, per se.
The complexity of the pain-emotion relationship is indeed further illustrated by examining their potential underlying neural circuits using functional magnetic resonance imaging (fMRI) of the brain. Meta-analytic maps of brain activations (Figures 1A and 1B), as well as within-subject studies that incorporate experimental manipulations of both pain and emotion paired with multivariate analytic approaches (Corradi-Dell’Acqua et al., 2016; Krishnan et al., 2016), identify both functionally dissociable, as well as shared neural, coding within brain regions, such as the insula and cingulate cortices. This highlights the need to study pain and emotions together, especially their bi-directional influence, and how and which peripheral and central circuits mediate their experience.
Figure 1. Pain and Emotion: What Is their Relationship and How Can We Deepen our Understanding Thereof?
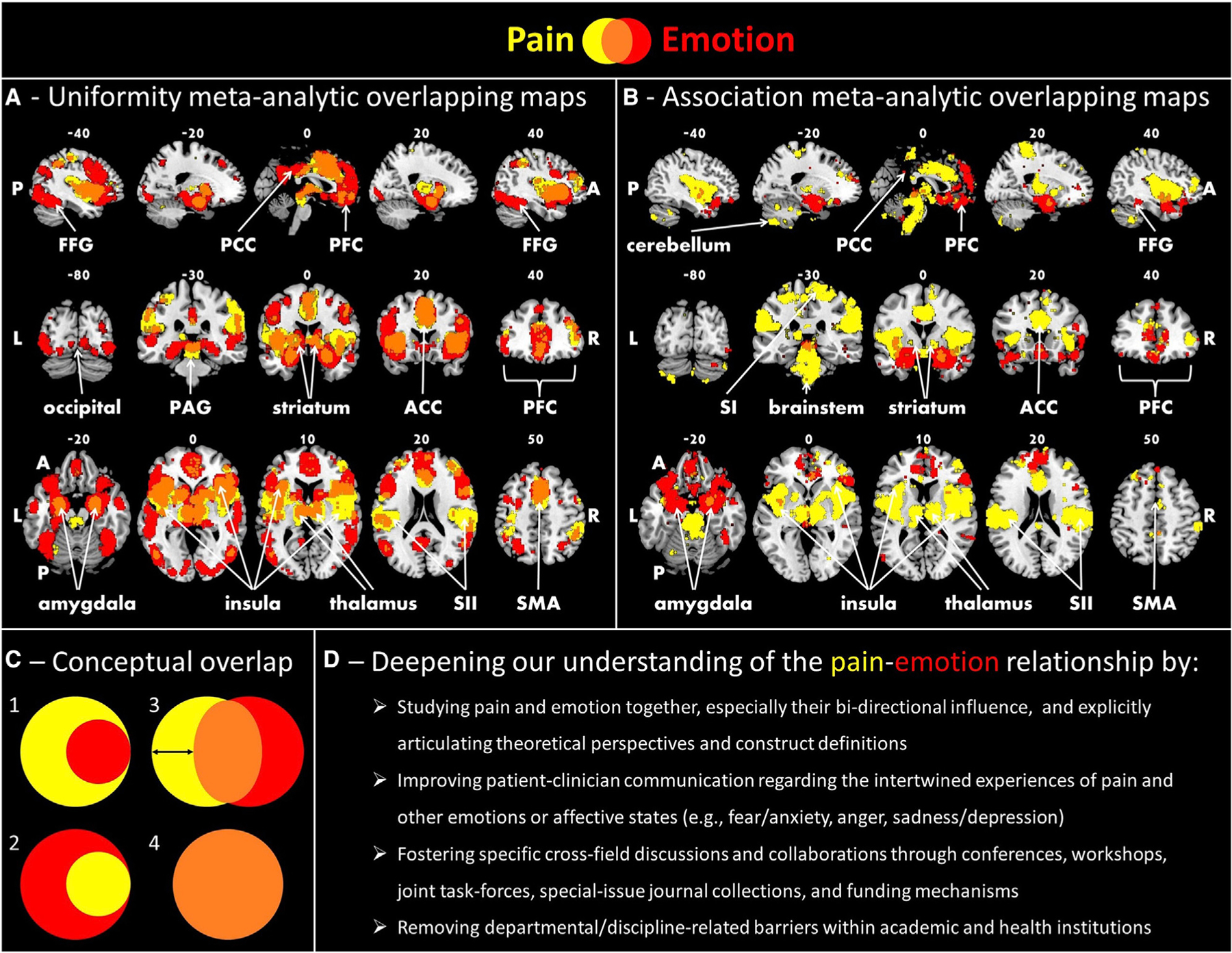
(A and B) These panels present four meta-analytic maps generated with Neurosynth (https://www.neurosynth.com), two for the term pain (yellow; 516 studies) and two for the term emotional (red; 1,708 studies). (A) displays voxels that are consistently active in studies that load highly on each of these two terms separately. (B) displays voxels that are more consistently active in studies that load highly on each of the terms separately than for studies that don’t. All maps are corrected at a false discovery rate of 0.01, with voxel intensities binarized. (A) suggests potential overlap between the two terms, as observed in brain regions classically associated with pain, such as anterior and posterior insula, anterior cingulate cortex (ACC), thalamus, and periaqueductal gray (PAG), as well as in brain regions classically associated with emotions, such as the amygdala, ventral striatum, and ventral regions of the medial prefrontal cortex (PFC). (B) suggests potential distinctions between the terms, and, as observed, some of the same regions that previously overlapped, such as the insula, cingulate, and amygdala, now seem to be specific for each of the two terms, and much less overlap is observed. In comprehending these findings, we should note potential limitations for understanding brain processing of pain and emotion—the maps do not distinguish between activations and deactivations, do not provide information about connectivity between brain regions, and are not sensitive to differences between healthy and chronic pain populations. Moreover, experimental paradigms differ between the terms, with emotion inductions mostly using visual stimuli (e.g., faces or scenes), whereas pain inductions commonly requiring physical contact (e.g., thermal or mechanical). This might suggest (B) is more reflective of sensory-specific discrimination. A conceptual consideration of the pain-emotion relationship must therefore complement and guide empirical findings. Coordinates of brain slices are in the Montreal Neurological Institute space. FFG, fusiform gyrus; PAG, periaqueductal gray; PCC, posterior cingulate cortex; SI/SII, primary/secondary somatosensory cortex; SMA, supplementary motor area; A, anterior; P, posterior; L, left; R, right.
(C) Using Venn diagrams, this panel presents potential theoretical perspectives regarding the relationship between pain and emotion. Venn1 illustrates the common view of pain as having an emotional component, in addition to sensory and other important components (e.g., cognitive, motivational, socio-cultural). It is thus challenging to conceive of pain and emotion as completely separate phenomena. On the other hand, pain could be conceptualized as a type of emotion category (Venn2), such as fear or anger. Pain could also be conceptualized as a feeling, a more rudimentary neurophysiological element (such as thirst or hunger), though controversy also exists regarding how to differentiate between feelings and emotions, which is beyond our current scope. These two perspectives suggest a vertical relationship between pain and emotion. However, a horizontal relationship between pain and emotion would define them as separate constructs with certain shared and other distinct underlying conceptual and neurophysiological processes (Venn3). Further empirical findings will determine the amount of overlap (as marked by the double-sided arrow), which might even reach complete overlap (Venn4), thereby conceptualizing experiences of pain and emotions as based on the exact same underlying mechanism.
(D) Above and beyond theoretical perspectives, we need to deepen and improve our understanding of the bi-directional relationship between pain and emotion at multiple levels of analysis (from the genetic to the socio-cultural) and considering the multiple components (e.g., sensory, motivational, etc.) of the two constructs. This panel highlights several actionable items that will support this process.
In this regard, both the insula and cingulate cortices are part of the cortical end points for interoceptive processing, the brain’s representation of the state of the body (Barrett, 2017; Damasio and Carvalho, 2013). Interoception is conceptualized as a continuous stream of sensations (some might refer to this as affect, others as feelings, though they need not be consciously perceived) that might serve as ingredients from which emotional experiences are then generated and regulated. Multiple such pathways mediate different sensations crucial for survival, such as hunger or thirst. The nociceptive pathways are considered part of these interoceptive pathways that together converge in the CNS, suggesting pain experience might similarly be generated and regulated. Nevertheless, in light of the above descriptions of pain and emotion, neither interoception in general nor nociception in particular seem either necessary or sufficient for such experiences.
Despite all these connections between pain and emotion, what makes pain so clear and confounding, maybe even unique compared to emotion, is that we do have dedicated nociceptive systems facilitating perception of noxious stimuli. Such systems were already present 500 million years ago in some of the most primitive organisms (e.g., nematodes, arthropods, and mollusks), as a set of peripheral mechanisms dedicated to promoting survival-relevant behaviors, even without the spinal cord. Subsequently, shaped by the increasing complexity and interactions of the physical and social environment, the phylogenetic evolvement of and interactions with spinal cord, brainstem, sub-cortical and cortical circuits, CNS mechanisms developed for more advanced protective behaviors that required cortical representations and interpretations. These presumably serve as a foundation for experiences such as pain, thus further adapting complex organisms to multiple environmental and contextual situations. Yet, we do not seem to have, at least as current evidence suggests, dedicated peripheral pathways for “fear-ception,” “anger-ception,” “sad-ception,” or any other emotion category.
Building Bridges
Taken together, the inherent and complex relationship between pain and emotion clearly requires further theoretical, empirical, and clinical scrutiny. Both constructs are based on primitive pathways that promote protective survival behaviors against imminent dangers. Through evolution, these pathways seemed to have crisscrossed each other, generating mechanisms that allow us to predict and respond to both real and imagined physical and psycho-social threats. Yet, if the activation thresholds of these mechanisms are too low due to sensitization, overgeneralization, or other reasons, they might negatively impact our physical, psychological, and social well-being, and potentially deteriorate to chronic maladaptive conditions.
Since both pain and emotion capture overlapping yet differential conceptual and neuroanatomical spaces, there might well be several alternative perspectives on their relationship (Figure 1C). Additional aspects of pain and emotion not touched upon here should also be integrated. For example, the involvement of pleasure and reward in experiences of pain and emotion or the endogenous opioids’ role in their generation and regulation. Considering the contribution of other biological factors, such as at the genetic, endocrine, or immune system levels and how they interact with all the other factors, is also of great importance. Ultimately, we need to better characterize the bi-directional impact that pain and emotion have on each other. For example, there is a general lack of studies directly examining how the separate induction of each impacts the current and downstream experience of the other and what neuro-physiological processes, interoceptive or other, mediate or contribute to their activation or inhibition. These efforts are imperative for people suffering from chronic pain or emotional disorders, since both populations are highly comorbid with each other.
The conceptual, mechanistic, and clinical connections between the constructs of pain and emotion should spur greater collaboration between the two historically and institutionally siloed scientific communities of pain (mostly from bio-medicine) and emotion (mostly from humanities and social sciences). Both fields ask similar questions, such as (1) do animals experience pain/emotions? (2) What changes in pain/emotions occur throughout development? (3) How are pain/emotions regulated? Or (4) what makes some people more vulnerable/resilient to pain/emotion abnormalities? Each field will benefit by incorporating within its research and clinical practice the theories, methods, and findings accumulated in the other. Clinical psychologists treating pain with various interventions, such as cognitive-behavioral therapy or mindfulness-based stress reduction, represent a focal point connecting the two fields. Further elucidating how pain and emotion interact might help us improve diagnosis and treatment. Indeed, recent advances in interventions emphasizing emotional awareness, acceptance, and expression seem to have increased benefit in providing relief for people with chronic pain (Lumley and Schubiner, 2019). Some scholars from both fields have separately begun laying out their theoretical views regarding the inter-relations of pain and emotions (Baliki and Apkarian, 2015; Barrett, 2017; Damasio and Carvalho, 2013; Gatchel et al., 2007). We believe that there are several ways to foster greater integration and synergy across these two fields (Figure 1D). This approach will ultimately (1) deepen and improve our conceptual understanding of pain and emotion and their inter-relationships, (2) support the development of novel, safe, and effective therapies, and (3) shape policy decisions that impact the lives of hundreds of millions of people suffering from pain and emotional disorders worldwide. Fundamentally, whether one is a clinician (e.g., physician, nurse), a scientist (e.g., biologist, psychologist), a humanist (e.g., philosopher, historian), or any other person, pain and emotion are more closely intertwined than we think.
ACKNOWLEDGMENTS
S.C.M. and G.G. thank the Redlich Pain Research Endowment and the Feldman Family Foundation Pain Research Fund for their financial support. The following National Institutes of Health grants provided further financial support: R01 NS109450, K24 DA029262, R01 DA035484, and P01 AT006651 (to S.C.M.); R01 MH076136, R01 DA046064, and R01 MH116026 (to T.D.W.); and P30 AG064201, R01 AG058702, UG1 CA189824, and U2C NR014637 (to F.J.K.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- Baliki MN, and Apkarian AV (2015). Nociception, Pain, Negative Moods, and Behavior Selection. Neuron 87, 474–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett LF (2017). The theory of constructed emotion: an active inference account of interoception and categorization. Soc. Cogn. Affect. Neurosci 12, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corradi-Dell’Acqua C, Tusche A, Vuilleumier P, and Singer T (2016). Cross-modal representations of first-hand and vicarious pain, disgust and fairness in insular and cingulate cortex. Nat. Commun 7, 10904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damasio A, and Carvalho GB (2013). The nature of feelings: evolutionary and neurobiological origins. Nat. Rev. Neurosci 14, 143–152. [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, and Turk DC (2007). The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol. Bull 133, 581–624. [DOI] [PubMed] [Google Scholar]
- Gross JJ, and Barrett LF (2011). Emotion Generation and Emotion Regulation: One or Two Depends on Your Point of View. Emot. Rev 3, 8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan A, Woo CW, Chang LJ, Ruzic L, Gu X, López-Solà M, Jackson PL, Pujol J, Fan J, and Wager TD (2016). Somatic and vicarious pain are represented by dissociable multivariate brain patterns. eLife 5, e15166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, and Schubiner H (2019). Psychological Therapy for Centralized Pain: An Integrative Assessment and Treatment Model. Psychosom. Med 81, 114–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey S, and Kao M-C (2019). Managing twin crises in chronic pain and prescription opioids. BMJ 364, l917. [DOI] [PubMed] [Google Scholar]
- Shackman AJ, and Wager TD (2019). The emotional brain: Fundamental questions and strategies for future research. Neurosci. Lett 693, 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]


