Abstract
Previous geographically limited studies have shown differential impact of COVID-19 on Hispanic individuals. Data were obtained from the Centers for Disease Control and Prevention. We performed multivariate Poisson regression assessing risk of hospitalization and death in Hispanic White (HW), Hispanic Black (HB), and Hispanic Multiracial/Other (HM) groups compared to non-Hispanic Whites (NHW). The relative risk of hospitalization was 1.35, 1.58, and 1.50 (p < 0.001) for HW, HB, and HM individuals respectively when compared to NHW. Relative risk of death was 1.36, 1.72, 1.68 (p < 0.001) times higher in HW, HB, and HM compared to NHW. HW, HB, and HM individuals also had significantly increased risk of requiring mechanical ventilation and ICU admission when compared to NHW. Hispanic individuals are more likely to be hospitalized and die from COVID-19 infection than White, which underscores the need for more precise data and policies aimed at unique Hispanic groups to decrease disparities.
Electronic supplementary material
The online version of this article (10.1007/s10903-020-01111-5) contains supplementary material, which is available to authorized users.
Keywords: Hispanic, Intersectionality, Disparities, COVID-19
Introduction
As the novel coronavirus 2019 (COVID-19) pandemic continues in the United States, it has become apparent that Hispanic populations are overrepresented among deaths from the disease [1–3]. Despite representing about 18.3% of the population [4], most recent weighted estimates from the Centers for Disease Control and Prevention (CDC) show that Hispanic populations make up 26.9% of the overall COVID-19 deaths [5]. Representation among cases and deaths vary by state, but among those with the largest Hispanic populations (California, Texas, and Florida), there are large disparities in deaths from the disease [2, 5].
Hispanic and Latinx designation is a politically constructed label [6] used to describe a large group of ancestries from a wide range of countries and nationalities. Those who identify as Hispanic or Latinx may choose vastly different race indicators on Census and hospital admission forms. In the 2010 Census, 37% of Hispanic individuals chose “other” race, while about half picked one of the standard categories (White, Black, etc.) [7]. While most hospitals collect race and ethnicity data, there is wide variation in how this information is detailed. Some hospitals collect information based on patient reports, staff observation, or other unreported methods [8, 9]. Because of the limitations in the data set in our study, we will refer to these groups according to their hospital reported Hispanic designation, while understanding the incompleteness of the designation and the large array of groups that make up the Hispanic and Latinx community.
Other health disparities in the Hispanic population are well documented. Hispanic individuals are overrepresented in cases of preventable diseases including diabetes, heart disease, cirrhosis, and certain types of cancer [10–14], several of which are known risk factors for COVID-19. These comorbidities have been linked to socioeconomic disparities and other factors related to social determinants of health relative to where they live [10, 11], which too are largely a result of historical and current discriminatory policies and practices [15]. Hispanic individuals are nearly twice as likely as non-Hispanic Whites to live in poverty and are generally uninsured or underinsured [16], limiting access to preventative care.
With only limited reports of overrepresentation of COVID-19 infections among Hispanic populations, we sought to use national case-level data from the CDC to understand the outcomes of Hispanic groups infected with COVID-19.
Methods
Data Sources
We obtained information on individual cases of COVID-19 infection from the CDC Case Surveillance Task Force and Surveillance Review and Response Group (SRRG) [17]. The dataset covers case reports between April 5, 2020, when COVID-19 was added to the Nationally Notifiable Condition List, through May 18, 2020 when the dataset was downloaded. Individual-based variables include case status, race, ethnicity, age group, presence of comorbidities (provided as a binary variable), hospitalization, need for intensive care unit (ICU), mechanical ventilation, and death. This dataset relies on passive reporting and, as such, has a significant number of missing and unknown values.
Case Selection and Outcomes of Interest
Given the complex nature of Hispanic identity in the United States, we compared Hispanic White (HW), Hispanic Black (HB), and Hispanic Multiracial/Other (HM) designation to the reference non-Hispanic White (NHW). Cases were limited to those with the reported race and ethnicity variables and we excluded those with race or ethnicity that was unknown or not reported (173,317 and 122,799 individuals respectively). Imputation of race and ethnicity were not feasible given the limitation of associated covariates. Primary outcomes were hospitalization and death due to COVID-19 infection. Additionally, differences in ICU admission and need for mechanical ventilation were evaluated.
Statistical Analysis
We performed multivariate Poisson regression with robust error variance to assess the impact of the race/ethnicity exposures to the outcomes of interest in a step-wise fashion. Model 1 assessed the unadjusted odds of the exposure on the outcome, and models 2–4 controlled for sex, age group, and comorbidities, respectively. This approach was used to assess the effect of each covariate on the exposure/outcome association. The stepwise table is available in Supplemental Table 2. Predicted margins of the outcomes of interest from the fully adjusted regression model were then plotted for each race/ethnicity category across age groups in order to assess disparities between the different groups at varying ages. Furthermore, we performed sensitivity analyses comparing HB individuals to non-Hispanic Black (NHB) individuals in order to understand the differential impact of Hispanic ethnicity and Black race designations.
There were a significant number of unknown values for the outcomes of interest and associated covariates. Assessments in the main analysis were performed using complete data only. A sensitivity analysis of unknown values was performed separately.
Differences in baseline characteristics were analyzed using Chi2 tests. An α = 0.05 was set as the level of significance. All analyses were performed in STATA 16 [18]. This study was deemed Non-Human Subjects Research by the Boston University Institutional Review Board.
Results
The analyzed cohort consisted of 78,323 individuals (Table 1). HW patients were the largest Hispanic group (13%), followed by HM (11%), and HB (2%). The HB group had the highest percentage of females (53%), while HM had the least (45%). HB individuals had the largest burden of comorbidities (51%) and hospitalizations (45%). The HM group had more frequent ICU admissions (10%), incidence of mechanical ventilation (10%), and death (16.1%).
Table 1.
Demographic and clinical characteristics
| Non-Hispanic White (n = 58,092) | Hispanic White (n = 10,415) | Hispanic Black (n = 1475) |
Hispanic multiple/other (n = 8341) |
|
|---|---|---|---|---|
| Laboratory confirmed cases, n (%) | 58,076 (99.9) | 10,413 (99.9) | 1,475 (99.9) | 8340 (99.9)21\ |
| Female, n (%) | 28,393 (49.0) | 5097 (49.0) | 781 (53.0) | 3713 (44.5) |
| Age, n (%) | ||||
| 0–9 | 279 (0.5) | 107 (1.0) | 13 (0.9) | 64 (0.8) |
| 10–19 | 933 (1.6) | 252 (2.4) | 25 (1.7) | 165 (2.0) |
| 20–29 | 6366 (11.0) | 1350 (13.0) | 170 (11.5) | 995 (11.9) |
| 30–39 | 7364 (12.7) | 1788 (17.2) | 233 (15.8) | 1342 (16.1) |
| 40–49 | 7663 (13.2) | 1969 (18.9) | 251 (17.0) | 1765 (21.2) |
| 50–59 | 10,291 (17.7) | 2040 (19.6) | 279 (18.9) | 1657 (19.9) |
| 60–69 | 10,060 (17.3) | 1430 (13.7) | 236 (16.0) | 1247 (15.0) |
| 70–79 | 7281 (12.5) | 860 (8.3) | 150 (10.2) | 680 (8.2) |
| 80 + | 7855 (13.5) | 619 (5.9) | 118 (8.0) | 426 (5.1) |
| Comorbidities present, n (%) | ||||
| Yes | 16,157 (27.8) | 3624 (34.8) | 753 (51.1) | 2880 (34.5) |
| No | 6670 (11.5) | 1046 (10.0) | 77 (5.2) | 996 (11.9) |
| Unknown | 35,265 (60.7) | 5745 (55.2) | 645 (43.7) | 4465 (53.3) |
| Hospitalization, n (%) | ||||
| Yes | 16,427 (28.3) | 3395 (32.6) | 666 (45.2) | 3357 (40.3) |
| No | 23,555 (40.6) | 3178 (30.5) | 201 (13.6) | 2806 (33.6) |
| Unknown | 18,110 (31.2) | 3842 (36.9) | 608 (41.2) | 2178 (26.1) |
| ICU admission, n (%) | ||||
| Yes | 2763 (4.8) | 586 (5.6) | 92 (6.2) | 870 (10.4) |
| No | 10,631 (18.3) | 1962 (18.8) | 124 (8.4) | 1416 (17.0) |
| Unknown | 44,698 (76.9) | 7867 (75.5) | 1259 (85.4) | 6055 (72.6) |
| Ventilator support, n (%) | ||||
| Yes | 2058 (3.5) | 490 (4.7) | 91 (6.2) | 825 (9.9) |
| No | 9527 (16.4) | 1780 (17.1) | 104 (7.1) | 1074 (12.9) |
| Unknown | 46,507 (80.1) | 8145 (78.2) | 1280 (86.8) | 6442 (77.2) |
| Death, n (%) | ||||
| Yes | 7810 (13.4) | 1229 (11.8) | 231 (15.7) | 1343 (16.1) |
| No | 21,266 (36.6) | 3103 (29.8) | 209 (14.2) | 2822 (33.8) |
| Unknown | 29,016 (50.0) | 6083 (58.4) | 1035 (70.2) | 4176 (50.1) |
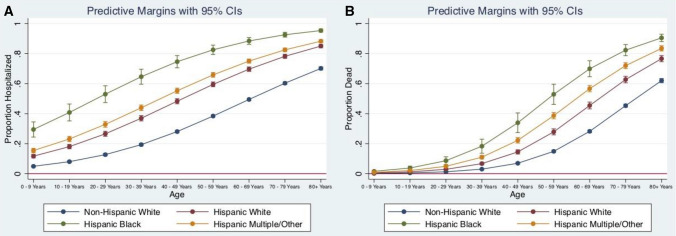
The unadjusted risk of hospitalization was higher for all Hispanic groups as compared to NHW (Table 2). After controlling for sex, age group, and the presence of comorbidities HW individuals had 1.35 times (95% CI 1.32, 1.38, p < 0.001), HB 1.58 times (95% CI 1.53, 1.64, p < 0.001), and HM 1.50 times (95% CI 1.46, 1.54, p < 0.001) increased risk of hospitalization compared to NHW. Predicted proportions of hospitalizations remained different between race/ethnicity groups across all age groups (Fig. 1a).
Table 2.
Unadjusted (RR) and adjusted (aRR) relative risk of outcomes of interest
| Hospital admission | Death | ICU admission | Mechanical ventilation | |||||
|---|---|---|---|---|---|---|---|---|
| RR (95% CI) n = 73,143 |
aRR (95% CI) n = 36,146 |
RR (95% CI) N = 50,812 |
aRR (95% CI) n = 24,653 |
RR (95% CI) N = 22,838 |
aRR (95% CI) n = 15,688 |
RR (95% CI) N = 19,949 |
aRR (95% CI) n = 14,651 |
|
| Non-Hispanic White | Reference group | |||||||
| Hispanic White |
1.26** (1.22, 1.29) |
1.35** (1.32, 1.38) |
1.06* (1.00, 1.11) |
1.36** (1.31, 1.43) |
1.11* (1.03, 1.21) |
1.30** (1.18, 1.42) |
1.22** (1.11, 1.33) |
1.51** (1.38, 1.65) |
| Hispanic Black |
1.87** (1.80, 1.94) |
1.58** (1.53, 1.64) |
1.95** (1.78, 2.14) |
1.72** (1.59, 1.86) |
2.06** (1.76, 2.42) |
2.27** (1.96, 2.63) |
2.63** (2.25, 3.07) |
2.59** (2.26, 2.97) |
| Hispanic Multiple/other |
1.33** (1.29, 1.36) |
1.50** (1.46, 1.54) |
1.20** (1.14, 1.26) |
1.68** (1.61, 1.75) |
1.84** (1.73, 1.96) |
2.06** (1.93, 2.21) |
2.45** (2.29, 2.61) |
2.55** (2.39, 2.72) |
CI Confidence interval
*p < 0.05
**p < 0.001
Fig. 1.
Predicted proportion of a hospitalizations and b deaths within each racial/ethnic subgroup
Similarly, Hispanic groups had a higher unadjusted risk of COVID-19 related mortality when compared to NHW (Table 2). After controlling for the previously listed covariates, the adjusted risk of death was 1.36 (95% CI 1.31, 1.43, p < 0.001), 1.72 (95% CI 1.59, 1.86, p < 0.001) and 1.68 (95% CI 1.61, 1.75, p < 0.001) times higher in HW, HB, and HM, respectively, as compared to their NHW counterparts (Table 2). There were no differences in mortality between the race/ethnicity groups at younger ages (< 19 years of age), but disparities in mortality between race/ethnicity groups grew advanced age (Fig. 1b).
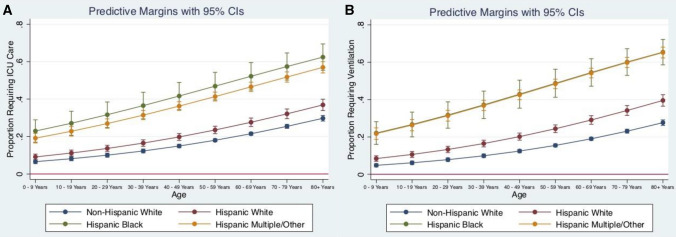
The adjusted relative risk of ICU admission, controlling for previously listed covariates, was 1.30 for HW (95% CI 1.18, 1.42, p < 0.001), 2.27 for HB (95% CI 1.96, 2.63, p < 0.001), and 2.06 for HM (95% CI 1.93, 2.21, p < 0.001) (Table 2). The plotted margins for each of the racial groups show statistically similar values for the HB and HM cohorts across all age groups (Fig. 2a). There were no statistically significant differences between HW and NHW among younger age groups, but the disparities between the two increased at advanced age.
Fig. 2.
Predicted proportion of a ICU admissions and b those requiring mechanical ventilation within each racial/ethnic subgroup
There were similar differences in mechanical ventilation for these groups. After controlling for confounders, the adjusted relative risk was 1.51 (95% CI 1.38, 1.65, p < 0.001), 2.59 (95% CI 2.26, 2.97, p < 0.001), and 2.55 (95% CI 2.39, 2.72, p < 0.001) for HW, HB, and HM respectively as compared to NHW (Table 2). There was no significant difference between HB and HM across all age groups (Fig. 2b). However, HW, HB, and HM continued to have higher risk of requiring mechanical ventilation across all age groups when compared to NHW.
To better understand the increased odds of negative outcomes among HB individuals, we compared them to NHB while controlling for sex, age group, and presence of comorbidities (Supplemental Table 1). HB patients had a 1.12 times increased adjusted risk (95% CI 1.19, 1.28) of hospitalization compared to their non-Hispanic counterparts. HB patients also had a 1.33 times increased risk (95% CI 1.15, 1.53) of ICU admission and a 1.35 times increased adjusted risk (95% CI 1.18, 1.54) of requiring mechanical ventilation compared to NHB patients. Finally, HB patients had a 1.27 times increased risk (95% CI 1.19, 1.36) of death as compared to their non-Hispanic counterparts.
The sensitivity analysis of unknown values performed is presented in the supplement. Overall, unknown values were equally distributed across the outcomes of interest within each racial/ethnic group, suggesting uniform underreporting for certain cases (Supplemental Table 3). However, HW, HB, and HM groups had a higher likelihood of unknown values compared to NHW in all outcomes except for hospitalization where the HM group has a lower likelihood of unknown values.
Discussion
In this retrospective study of all cases reported to the CDC between April 5 and May 18, 2020, we show significant differences in hospitalization and death, as well as ICU admissions and mechanical ventilation in Hispanic groups as compared to non-Hispanic Whites. Additionally, we demonstrate large variability in outcomes between different Hispanic racial subgroups. In the provided dataset, the Hispanic population was divided into Hispanic black (HB), Hispanic white (HW), and Hispanic multiracial (HM). After controlling for the available confounders, significantly worse outcomes were noted in HB individuals for hospitalization (RR 1.58), death (RR 1.72), ICU admission (RR 2.27), and need for mechanical ventilation (RR 2.59), as compared to their Non-Hispanic White (NHW) counterparts. Overall, HB and HM individuals fared worse than HW and NHW individuals on the outcomes of interest.
This investigation underscores the importance of standardizing the identification of U.S. Hispanic subpopulations in hospital records. Self-identification of race on official records is variable and has been shown to depend on nativity status, length of stay in the U.S., language spoken, and where individuals feel they fit within the set framework [19]. These differences are unlikely to be genetic in origin given the broad range of hereditary ancestries within these politically-derived groups. However, without geographic or socioeconomic data, it is difficult to understand the impact of the built environment on these differences.
Prior research on health disparities in Hispanic communities show that, prior to COVID19, they were already at higher risk of diabetes, heart disease, cirrhosis, and certain types of cancer [10–14], disparities that stem from socioeconomic status (SES), poverty, and unequal access to services [14]. In the case of COVID-19, it is likely that poverty, cramped and crowded living conditions [4], poor access to preventative care, and insurance status likely play a role in these disparities [16]. Additionally, Hispanic individuals make up a large proportion of essential workers [20] during this pandemic and are significantly less able to work from home compared to other groups [21], increasing their risk of contracting the disease.
We show that, of all groups studied, HB individuals have the worst outcomes related to COVID-19. In the U.S., HB individuals have been shown to socially be viewed similarly to NHB individuals [11]. This view may lead to similar racial discrimination, segregation, and other marginalizing effects that impact the health outcomes of HB similarly to those of NHB individuals [22, 23]. Most troubling in the analysis, however, were worse outcomes seen among Hispanic Black patients compared to their non-Hispanic Black counterparts, suggesting that there may be further factors beyond racial discrimination and segregation that uniquely affect the HB population. Intersectionality is a theoretical framework based in critical race theory that posits that multiple social categories (in this case, ethnicity and race) intersect at the level of individual experience to reflect multiple interlocking systems of oppression at the social-structural level [24]. For HB individuals, they may be subject to increased exposure to the damaging effects of racism, nativism, and xenophobia. Acknowledging the existence of multiple intersecting identities is critical in understanding health disparities for populations from multiple historically oppressed groups [24]. Previous studies have shown that ethnic and racial identities of HB individuals have an impact on health outcomes [25–27] and disparities in access to care [28]. It has been hypothesized that these disparities, in part, result from societal forces that lead to discrimination [28, 29].
Given that approximately 50% of Hispanic individuals in the U.S. are immigrants, it is plausible to think that immigration status may have an effect on these observed disparities. While Public Charge determination specifically does not included COVID-19 testing or treatment in the public benefits that count against an applicant [30], it does preclude many from obtaining social services that may be necessary for preventative care and other public services including Supplemental Nutrition Assistance Program (SNAP) benefits and unemployment benefits and has deterred many immigrants from seeking healthcare. Lack of access to these public benefits and services for immigrants may make them more susceptible to severe COVID-19-related symptoms [32]. As immigration status dictates access to public benefits unequally across the US, the relationship between immigration status, healthcare access and COVID-19 risk merits further research.
In addition, Hispanic and Black populations have been subject to decades of housing and economic segregation, upstream factors that can lead to unequal rates of chronic disease and poor access to healthcare. In contrast, recent evidence from a Veterans Affairs study showed no difference in mortality between black/Hispanic and white veterans, groups who have more similar socioeconomic and insurance status [31]. Further, predicted margins of outcomes by age show that disparities between the different subgroups are less apparent at younger age and widen in older age groups. This seems to reinforce the idea that these are not biologically constructed disparities in politically constructed groups, but rather due to explicit or structural discrimination that compound over time to make these groups more susceptible to disease.
Our study has important limitations that should be considered in its interpretation. Firstly, this retrospective data relies on passive surveillance from state and local authorities. Reporting relies on COVID-19 testing, which may not be available to asymptomatic patients. Thus, absolute reported numbers likely underestimate the number of cases, while overestimating the proportion of each group who experienced the outcomes of interest. Similarly, there may be differences between groups attributable to differential access to testing based on race and ethnicity. As compared to U.S. Census data [34], however, our data show overrepresentation of these Hispanic groups, suggesting that these groups may be tested more often than NHW groups. Without geographic data we are unable to assess the built environment associated with these different groups. Further, the available data on comorbidities reported in this data set was limited to a binary variable with low levels of reporting, which does not allow robust analysis of individual comorbidities and leaves room for confounding variables.
There are a large number of missing values in this dataset, likely from incomplete reporting from local authorities. Overall information on missing data is presented in Supplemental Table 3 and risks of missing data for each subgroup and outcome of interest are presented in Supplemental Table 4. Generally HW and HM groups had a proportionally higher number of missing variables for the outcomes of interest, which were higher than that of NHW. HB groups had the highest proportion of missing variables. Given these trends, we are possibly underestimating the true effect of the outcome of interest in these groups given the overrepresentation of unknown values and the poor outcomes noted in the primary analysis. However, it is also possible that these individuals were minimally symptomatic, precluding reporting of the outcomes. The amount of missing data in this dataset points to the need for better tracking of race and ethnicity data at the level of local reporting.
Public Health Implications
This study is among the first to use nationally representative COVID-19 case data to characterize the differential impact of COVID-19 on Hispanic groups within the U.S. Despite missing data due to incomplete reporting from local authorities, our study shows higher odds of hospitalization and death, as well as ICU admissions and mechanical ventilation, among Hispanic groups as compared to NHW. These findings need to be further investigated in the context of geographic and socioeconomic indicators with more complete race and ethnicity tracking in order to elucidate the underlying factors contributing to these disparities. Additionally, the multiplicative impact of Hispanic and Black designation on negative COVID-19-related outcomes warrants further investigation and should be considered when shaping public health initiatives, as interventions targeted broadly to Hispanics may not be sufficient [28]. Overall, this analysis shows that Hispanic communities should not be considered solely in the aggregate, and that each of these Hispanic communities have been impacted more by COVID-19 than non-Hispanic White in the U.S., which should direct further crisis response and policy decision-making.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Funding
Michael Poulson is supported by a T32 training grant (HP10028). Alaina Geary and Miriam Neufeld are supported by a T32 training grant (GM86308).
Compliance with Ethical Standards
Conflict of interest
The authors have no financial nor personal disclosures or conflict of interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bibbins-Domingo K. This time must be different: disparities during the COVID-19 pandemic. Ann Intern Med [Internet]. 2020; 19–21. https://annals.org/aim/fullarticle/2765523/time-must-different-disparities-during-covid-19-pandemic. [DOI] [PMC free article] [PubMed]
- 2.Azar KMJ, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities In outcomes among COVID-19 patients in a large health care system In California. Health Aff (Millwood). 2020; https://www.ncbi.nlm.nih.gov/pubmed/32437224. [DOI] [PubMed]
- 3.Krouse HJ. COVID-19 and the Widening Gap in Health Inequity. Otolaryngol Head Neck Surg. 2020;194599820926463. https://www.ncbi.nlm.nih.gov/pubmed/32366172. [DOI] [PubMed]
- 4.U.S. Census Bureau QuickFacts: United States. Census Bureau QuickFacts. 2020 [cited 2020 May 22]. https://www.census.gov/quickfacts/fact/table/US/RHI725218.
- 5.COVID-19 Provisional Counts - weekly updates by select demographic and geographic characteristics. Centers for Disease Control and Prevention. 2020 [cited 2020 May 22]. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/#Race_Hispanic.
- 6.Zambrana R, Dill BT. Disparities in Latina health: an intersectional analysis. Gender, race, class, Heal Intersect approaches. 2006;192–227.
- 7.Parker K, Horowitz JM, Morin R, Lopez MH. Hispanic racial identity: multidimensional issue for Latinos. Pew Research Center’s Social & Demographic Trends Project. 2019 [cited 2020 May 24]. https://www.pewsocialtrends.org/2015/06/11/chapter-7-the-many-dimensions-of-hispanic-racial-identity/.
- 8.Pittman MA, Pierce D, Hasnain-Wynia R. Who, when, and how: the current state of race, ethnicity, and primary language data collection in hospitals. The Commonwealth Fund. 2004.
- 9.Gomez SL, Le GM, West DW, Satariano WA, O’Connor L. Hospital policy and practice regarding the collection of data on race, ethnicity, and birthplace. Am J Public Health. 2003;93(10):1685–1688. doi: 10.2105/AJPH.93.10.1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31(1):99–112. doi: 10.1093/epirev/mxp008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cuevas AG, Dawson BA, Williams DR. Race and skin color in Latino health: an analytic review. Am J Public Health. 2016;106(12):2131–2136. doi: 10.2105/AJPH.2016.303452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aponte J. Health disparities and Hispanics. Hisp Heal Care Int. 2017;15(2):2017. doi: 10.1177/1540415317708513. [DOI] [PubMed] [Google Scholar]
- 13.Miller KD, Goding Sauer A, Ortiz AP, Fedewa SA, Pinheiro PS, Tortolero-Luna G, et al. Cancer statistics for Hispanics/Latinos, 2018. CA Cancer J Clin. 2018;68(6):425–445. doi: 10.3322/caac.21494. [DOI] [PubMed] [Google Scholar]
- 14.Hispanic Health. Centers for Disease Control and Prevention. 2015.
- 15.Colen CG, Ramey DM, Cooksey EC, Williams DR. Racial Disparities in health among nonpoor African Americans and Hispanics: the role of acute and chronic discrimination. Soc Sci Med. 2018;199:167–180. doi: 10.1016/j.socscimed.2017.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Profile: Hispanic/Latino Americans [Internet]. U.S. Department of Health and Human Services. 2019 [cited 2020 May 24]. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64.
- 17.COVID-19 Case Surveillance Data Access, Summary, and Limitations. Centers Dis Control Prev COVID-19 Response. (Version Date: May 18, 2020.).
- 18.Stata Statistical Software: Release 14. College Station, TX: StataCorp LP.
- 19.Borrell LN. Racial identity among hispanics: implications for health and well-being. Am J Public Health. 2005;95(3):379–381. doi: 10.2105/AJPH.2004.058172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kearney A, Muñana C. Taking stock of essential workers. Kaiser Family Foundation. 2020.
- 21.Gould E, Shierholz H. Not everybody can work from home: Black and Hispanic workers are much less likely to be able to telework. Economic Policy Institute. 2020.
- 22.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1016/S0033-3549(04)50068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poulson M, Geary A, Annesi C, Allee L, Kenzik K, Sanchez S, et al. National disparities in COVID-19 outcomes between Black and White Americans. J Natl Med Assoc. 2020 doi: 10.1016/j.jnma.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bowleg L. The problem with the phrase women and minorities: interesectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bediako PT, BeLue R, Hillemeier MM. A comparison of birth outcomes among black, Hispanic, and black Hispanic women. J Racial Ethn Health Disparities. 2015;2(4):573–582. doi: 10.1007/s40615-015-0110-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan HMR, Gabbidon K, Abdool-Ghany F, Saxena A, Gomez E, Stewart TS-J. Health disparities between black Hispanic and black non-Hispanic cervical cancer cases in the USA. Asian Pac J Cancer Prev. 2014;15(22):9719–9723. doi: 10.7314/APJCP.2014.15.22.9719. [DOI] [PubMed] [Google Scholar]
- 27.Banegas MP, Li CI. Breast cancer characteristics and outcomes among Hispanic black and Hispanic white women. Breast Cancer Res Treat. 2012;134(3):1297–1304. doi: 10.1007/s10549-012-2142-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.LaVeist-Ramos TA, Galarraga J, Thorpe RJ, Bell CN, Austin CJ. Are black Hispanics black or Hispanic? Exploring disparities at the intersection of race and ethnicity. J Epidemiol Community Health. 2012;66(7):e21. doi: 10.1136/jech.2009.103879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burgos G. The (in)significance of race and discrimination among Latino youth: the case of depressive symptoms. Sociol Focus. 2009;42(2):152–171. doi: 10.1080/00380237.2009.10571348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Public Charge. Immigrant Legal Resource Center. 2019. https://www.ilrc.org/public-charge-legal-services-toolkit. Accessed July 10,2020.
- 31.Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT, Skanderson M, et al. COVID-19 by race and ethnicity: a national cohort study of 6 million United States Veterans. medRxiv Prepr Serv Heal Sci [Internet]. 2020;1–17. https://www.ncbi.nlm.nih.gov/pubmed/32511524%0A, https://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC7273292.
- 32.Ross J, Diaz CM, Starrels JL. The Disproportionate Burden of COVID-19 for Immigrants in the Bronx, New York JonathanRoss, MD,. JAMA Intern Med. 2020;E1–E2. 10.1001/jamainternmed.2020.2131. [DOI] [PubMed]
- 33.El Chaar M, King K, Lima AG. Are black and Hispanic persons disproportionately affected by COVID-19 because of higher obesity rates? Surg Obes Relat Dis. 2020;16:1096–9. doi: 10.1016/j.soard.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010. 2011;23. https://www.census.gov/population/race/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.