Abstract
Introduction
Conditional cash transfers (CCTs) have become an important policy tool for increasing demand for key maternal and child health services in low/middle-income countries. Yet, these programs have had variable success in increasing service use. Understanding beneficiary preferences for design features of CCTs can increase program effectiveness.
Methods
We conducted a Discrete choice experiment in two districts of Uttar Pradesh, India in 2018 with 405 mothers with young children (<3 years). Respondents were asked to choose between hypothetical CCT programme profiles described in terms of five attribute levels (cash, antenatal care visits, growth-monitoring and immunisation visits, visit duration and health benefit received) and responses were analysed using mixed logit regression.
Results
Mothers most valued the cash transfer amount, followed by the health benefit received from services. Mothers did not have a strong preference for conditionalities related to the number of health centre visits or for time spent seeking care; however, service delivery points were in close proximity to households. Mothers were willing to accept lower cash rewards for better perceived health benefits—they were willing to accept 2854 Indian rupees ($41) less for a programme that produced good health, which is about half the amount currently offered by India’s Maternal Benefits Program. Mothers who had low utilisation of health services, and those from poor households, valued the cash transfer and the health benefit significantly more than others.
Conclusion
Both cash transfers and the perceived health benefit from services are highly valued, particularly by infrequent service users. In CCTs, this highlights the importance of communicating value of services to beneficiaries by informing about health benefits of services and providing quality care. Conditionalities requiring frequent health centre visits or time taken for seeking care may not have large negative effects on CCT participation in contexts of good service coverage.
Keywords: health policy, health systems, health economics
Key questions.
What is already known?
Conditional cash transfer (CCT) programmes are an important policy tool for increasing demand for key maternal and child health services.
However, CCT programmes have had variable performance in increasing use of maternal and child health services.
Factors responsible for variable performance include: low cash transfer amount, proximity to service delivery points, the influence of community and household members, trust in government programmes, cultural practices and behaviour of health workers.
What are the new findings?
Using a discrete choice experiment, we find mothers most valued the cash transfer amount, followed by the health benefit received from services.
Mothers did not have a strong preference for conditionalities related to the number of health centre visits or to the time taken for accessing care (service delivery points were in close proximity), though fewer and shorter visits are preferred.
Mothers were willing to accept lower cash rewards for better perceived health benefits.
Mothers who had low utilisation of health services, and those from poor households, valued the cash transfer and the health benefit significantly more than others.
What do the new findings imply?
Both cash transfers and the perceived health benefit from services are highly valued, particularly by infrequent users of maternal and child health services.
This highlights the importance of communicating value of services to target beneficiaries by informing about health benefits of services, as well as providing quality care.
Frequent health centre visits or longer visit duration may not have large negative effects on decisions to participate in the CCT when services are available in close proximity.
Introduction
Conditional cash transfer (CCT) programmes have become an important policy tool to increase demand for maternal and child health services. In its original conception, like in Mexico’s Prospera (formerly Progresa and Oportunidades) or Brazil’s Bolsa Familia, CCTs served as broad-based social safety nets that provided income support to poor households. To receive cash transfers beneficiaries are required to fulfil conditionalities related to use of maternal and child health services, among others. More recently in South Asia, a new type of targeted CCT programme emerged that offered cash rewards to incentivise households to use specific health services, rather than serve as a social safety net. For example, India’s Janani Surakshna Yogna (JSY) programme offers cash rewards to mothers for delivering at a health facility. In either case, CCT programmes can increase demand for health services through the income effect of additional disposable income that enables households to purchase health services or pay for transport, as well as through the conditionalities related to maternal and child health services.1
CCTs typically include a range of maternal and child health service conditionalities, such as requiring pregnant and lactating women to attend educational workshops, have prenatal and postnatal health visits, deliver in a health facility, keep mothers and child vaccinations up-to-date, have children regularly attend growth-monitoring sessions and health check-ups.2 3 Evidence from broad-based CCT programmes on service uptake has been mixed, and comparisons complicated, due to variation in CCT programme conditionalities across countries, and outcome indicators measured in evaluations. Reviews report that CCTs have had variable effects across countries.2–4 For example, in Honduras there was a 19% increase in pregnant women having at least five antenatal care (ANC) visits, but only 8% in Mexico, and no effect in El Salvador, Nepal and Guatemala, or Chile.2 3 5 There were no significant increases in pregnant women getting tetanus toxoid vaccination in Honduras and Mexico. Facility deliveries increased by 15% in Nicaragua, and births attended by skilled personnel increased by 11% in Mexico and El Salvador, but not in Guatemala and Uruguay.3 There seems to be no effect on postpartum visits in Honduras and El Salvador.3 CCTs in Colombia, Honduras and Mexico have had significant effects on increasing child immunisation. And in Chile, Colombia and Jamaica, there was an increase in children going for regular check-ups, but not so in Honduras. Among the targeted CCT programmes, India’s JSY has been found to increase institutional deliveries at public facilities by 49%, though a similar programme in Nepal increased institutional deliveries by only 4%.3 Moreover, in the JSY programme, even in the presence of cash rewards for institutional deliveries, a significant number of women deliver at home, and programme participation varies considerably subnationally.6 7
Several factors explain the variable success of CCT programmes on increasing demand for health services. For one, the cash reward offered may be lower than the minimum reward acceptable to beneficiaries to fulfil conditionalities. Other factors, such as proximity to service delivery points, the influence of community and household members, trust in government programmes, cultural practices and behaviour of health workers are also critical factors that affect programme participation.1 8 9 In particular, as Handa et al point out, increased income or conditionalities will have limited effects on demand for services because of limited supply and poor quality of services.1 Studies on India’s JSY programme report that cash incentives are an important reason why women choose to deliver in a health facility.10 However, many women choose to deliver at home due to6 perceptions of quality of care offered at health facilities (particularly for complicated deliveries), and their inability to secure transportation or companions to visit a health facility.10 The role of quality perceptions in the choice of which facility women give birth has also been highlighted in studies on facility bypassing.11
In this paper we aim to examine beneficiary preferences for attributes (ie, cash amount and conditionalities) of a targeted CCT programme focused on maternal and child health services in India. Understanding beneficiary (ie, mothers) preferences for programme design features can better align the CCT programme design with user preferences, thereby making the programme more acceptable, as well as potentially improving performance. A second objective is to examine preferences for CCT programme features among mothers who are less likely to use maternal and child health services. This is a key population whose preferences CCT programmes aim to change; as such examining their preferences will inform strategies to increase their programme participation. This study uses a discrete choice experiment (DCE), a stated-preference method and part of the conjoint analysis family, to understand user preferences for design features for a CCT program.12
The study is set in the state of Uttar Pradesh (UP) in north India, with population over 200 million and poor maternal and child health indicators. In 2015, UP had the highest infant mortality rate (64 deaths per 1000 live births) in the country, and around 65% of children 12–23 months of age received three doses of diphtheria, pertussis and tetanus vaccine.13 Further, only 26% of women received at least four antenatal check-ups, and 13% consuming iron–folic acid supplements for 100 days or more during pregnancy.13 In this context, CCT programmes can have a significant impact on uptake of maternal and child health services.
CCT programs focused on maternal and child in India
In India, CCTs are rapidly becoming important in national strategies to improve maternal and child health. State-level CCT programmes that focus on increasing demand for health services among mothers and young children have existed for several decades, though national programmes appeared more recently.14 The first national CCT programme, JSY, was launched in 2005 and provided poor women a cash incentive for delivering in a health facility. The JSY has been credited with increasing institutional deliveries and reducing perinatal and neonatal deaths, though these successes have been tempered with concerns about poor-quality services women receive when they give birth at government facilities.6
CCT programmes focused on maternal and child health are expected to undergo significant expansion in India. In 2017, the national Pradhan Mantri Matritva Vandana Yojana or the Maternity Benefit Program (MBP) was introduced with the objective of increasing healthcare use during pregnancy and early childhood.15 The MBP provides a cash transfer of 5000 Indian rupees ($71) to eligible pregnant women for their first live birth in three instalments, tied to conditionalities of pregnancy registration, at least one ANC visit, birth registration and child vaccination.16 To fulfil the MBP conditionalities, mothers need to visit the local nutrition centres (Anganwadi Center or AWC) on Village Health and Nutrition Days (VHND) held monthly. The effect the MBP has on maternal and child health and nutrition outcomes is unknown due to early stages of implementation. A recent study on a similar state-level CCT programme from Odisha state showed positive effects on use of ANC services, iron–folic acid supplementation and household food security.14 Extending CCT programmes to child nutrition is also under discussion in India and has been mooted in the government’s National Nutrition Strategy.17 18
Methods
The DCE method has been used to guide the design of health programmes, including maternal and child health, by understanding the strength of user preferences for programme design features.19–24 The DCE is a quantitative method that is useful for assessing the potential impact of strategies or programmes that have not been implemented, and understanding the relative value of, and trade-offs between, the programme attributes. It is based on what people say they will do that is, their stated preferences. The DCE methodology has its theoretical foundations in random utility framework.25 Each respondent is presented a series of hypothetical alternatives (in this case CCT programme profiles). The respondent is assumed to choose the alternative that results in the highest utility level . The utility level of a given programme is a function of a deterministic component, , as well as a random component that is based on unobservable programme attributes and individual level preference variation (). V is a function defined by the attribute levels for programme alternative i, Xi is a vector of attribute levels defining alternative i, and β is a vector of estimated coefficients. Each estimated β is a preference weight and represents the relative contribution of the attribute level to the utility that respondents assign to an alternative.12
| (1) |
Developing programme attributes and levels
A first step in the DCE study is to construct CCT programme profiles in terms of programme attributes and their levels. Our starting point in developing CCT programme attributes was that it should reflect the conditionalities of existing maternal and child health CCT programmes (ie, the MBP), as well as possible conditionalities for including nutritional services for children below 3 years of age through the Integrated Child Development Services (ICDS) programme. The MBP conditionalities are described in government documents.26 For nutrition services, we consulted officials from the Ministry of Women and Child Development, multilateral agencies in UP and other stakeholders to understand some of the key design features being considered for child nutrition cash transfer programme. Based on this information we identified five attributes for our study (table 1).
Table 1.
Attributes included in DCE for assessing willingness to participate in conditional cash transfer programme
| Attribute | Level | Description |
| 1. Antenatal care visits during pregnancy | 4 (reference) 8 12 |
Number of antenatal care visits mother would need to make to a health centre during her pregnancy; WHO and Government of India norm is eight visits |
| 2. Growth-monitoring and immunisation visits per year for children 0–3 years | 4 (reference) 8 12 |
Number of visits per year to the village nutrition centre for growth monitoring and immunisations |
| 3. Time spent on each visit (hours) | 1 (reference) 4 8 |
Total duration of visit for antenatal care or growth monitoring; it includes travel time, waiting and consultation |
| 4. Health benefit for mother and child | Poor (reference) Fair Good |
Perceived health benefit to mother or child from antenatal or growth-monitoring/immunisation services |
| 5. Cash transfer amount (INR) | 50 (reference) 3000 6000 |
Cash amount given to mother for fulfilling CCT programme conditionalities |
CCT, conditional cash transfer; DCE, discrete choice experiment; INR, Indian rupee.
The conditionalities in the MBP require the mother to register her pregnancy, receive at least one ANC check-up during pregnancy, register child’s birth and ensure her child receives the first cycle of vaccines at birth. The current policy response to address child undernutrition, the ICDS programme, provides several services targeted at mothers and children below 6 years of age through its network of AWCs in each village. These services include: supplementary food, growth monitoring and health check-ups, nutrition education, non-formal preschool education, immunisation and referral services. A CCT that included child nutrition would provide cash to households with children below 3 years of age with potential conditionalities of participating in ICDS services such as regular growth monitoring of children. Both the MBP and child growth-monitoring conditionalities can be fulfilled at the local AWC where the VHND is a focal platform for co-integrating maternal and child health services in rural communities.26
We represented conditionalities in terms of the number of annual visits to a government health centre or AWC (table 1). The first attribute is the number of ANC visits during pregnancy. The Government of India and WHO guidelines recommend women make eight ANC visits during pregnancy to achieve optimal birth outcomes.27 We used this as the middle level for the ANC visit attribute. The second attribute is the number of visits per year for children under 3 years old for growth monitoring and immunisations. The recommended number of growth-monitoring visits can be substantial. For example, the Government of India guidelines recommend weekly growth monitoring in the first month after birth and monthly monitoring until 3 years of age.28 This requires around 12 visits a year, and we used 8 visits as the midpoint level. For both the ANC and growth-monitoring visit attributes, the high and low levels were selected such that recommended number of visits were included within their range.
We included two other attributes related to health centre visits—the time spent for each visit, and the perceived health benefit for the mother and child from services (table 1). The time attribute took on three levels—1, 4 and 8 hours. This time includes both travel and consultation time. ANC visits typically take place at the AWC or government health centre located in proximity to the village. In our study sample, 80% of the mothers reported that there was an AWC centre in their village. The average time to travel to the AWC was 11 min and travel time ranged from 0 to 1.3 hours. If we added time for consultation, then we would expect the total time taken for ANC or immunisation and growth-monitoring visits to be under 4 hours.
In the Grossman model, health provides consumption benefits (utility from having health) as well as production benefits—individuals produce health by investing in healthcare, better diet, exercise and so on so that they can be healthier and more productive.29 People demand health services as a means for achieving better health. Studies on CCT programmes and our interactions with respondents during pretesting suggest that perceptions of quality of care is an important motivation for beneficiary choice of using services, or where care is sought. As such, perceptions of value or benefit derived from health services are an important driver of the decisions to participate in a programme. We attempt to capture the benefit received from ANC and child nutrition services by including a ‘health benefit’ attribute which takes on the values poor, fair or good. ‘Fair’ and ‘good’ indicate a positive health benefit from using services, while ‘poor’ is indicative of health services which caused users to be worse-off due to things like poor quality of care. These attribute levels represent the perceived health benefits that mothers received for themselves or their children by investing time and effort in undertaking ANC and growth-monitoring visits.
The cash amount indicates the amount of money a mother would receive on an annual basis for complying with the programme conditions. The cash transfer attribute had three levels—a nominal 50 Indian rupees ($0.70), 3000 Indian rupees ($43) and a high of 6000 Indian rupees ($86) per year. The upper bound of the cash transfer range was aligned with what the MBP’s offer of 5000 Indian rupees per year. The lower bound of 50 Indian rupees represents a low nominal non-zero amount.
DCE design
The five attributes, each with three levels, generated a full factorial design of 243 possible programme choice task sets. We selected 18 of the 243 task sets for the DCE using a fractional factorial two-block D-efficient experimental design having minimal overlap between attributes and level balance. Because having mothers complete 18 choice task sets can impose a substantial cognitive burden, we used a block design so that half the sampled respondents were presented with nine task sets and the other half a different nine task sets. The choice alternatives were unlabelled. CCT programme attributes and levels were included via pictorial representations to enable ease in comprehension (figure 1).
Figure 1.
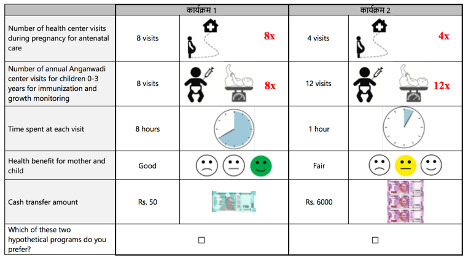
Sample task card presented to study respondents.
Each choice task set contained two CCT programme profiles and the respondents had to select one of them (figure 1). There are important pros and cons of using such a forced choice DCE (ie, where respondents have to select a specific choice profile without having the option of opting-out) design. DCEs that have an opt-out option can offer scenarios closer to what respondents might face in reality. It is not likely that every mother will participate in the CCT programme and this has also been the experience with ongoing CCT programmes in India where despite a financial incentive to deliver in a health centre, a considerable proportion of mothers choose to deliver at home. In such situations, not having an opt-out option can bias estimated attribute effects and predicted probabilities of participation.30 However, including an opt-out option also might offer an easy alternative to respondents because it poses less of a cognitive burden. Importantly, we learn nothing about respondent trade-off between programme attributes when this option is selected, one of the main concerns of this study. Initial variants of our DCE questionnaire carried an opt-out option where respondents were asked to choose between two programme profiles and were then asked if they would participate in the programme they had selected; during pretesting we found that all respondents answered in the affirmative, and this lack of variation would also not provide any information regarding trade-offs between attributes. We explore this further in the Discussion section.
Sample selection
This study was nested within a larger household survey conducted in August 2017 in two districts of UP—Hardoi and Sitapur. Administratively, each district is composed of blocks and each block of several Gram Panchayats consisting of three to seven villages. In the parent study, all Gram Panchayats were selected from Hardoi and Sitapur and one village from each was randomly sampled. Within a village, 17–18 households were randomly selected for interviews. For the present study we obtained a listing of all surveyed households in the parent study and purposively selected three blocks within these two districts which had a large number of households with children below 3 years of age (at the time of the survey). The eligibility criteria for selecting households required that they had children below 3 years of age because they would be more likely to have interactions with the health system for maternal and child health services. Data collection took place from January 2018 to February 2018. We visited listed eligible households until our target quota of 400 women with children below 3 years was achieved. A total of 541 households were visited which yielded 405 respondents. The sample was comprised of rural women.
DCE administration
Prior to conducting the DCE, respondents were shown a 3 min video that explained the purpose of the experiment and how to answer the DCE questions. The respondent was then asked three knowledge assessment questions. If the respondent did not answer correctly, another explanation of how to complete the experiment was provided. A rationality test was included as an additional task set to assess respondents’ understanding of the experiment. For this task set, the attribute levels for the alternative programmes were identical, except for the health benefit for the mother and child (poor or good in alternative programmes). Any rational decision maker would choose the programme that resulted in good health for the mother and child.
The survey was administered in Hindi by trained enumerators using tablets. The final questionnaire took approximately 45 min to complete. Informed consent was taken from all respondents.
Statistical analysis
We use mixed logit regression to estimate the probability of a respondent selecting programme alternative i from among two alternatives as12:
| (2) |
The probability of choosing programme alternative i is a function of both the attribute levels of alternative i and the attribute levels of the other profiles presented in the choice task. The probability of choosing one profile from the set of two alternatives is one minus the probability of choosing the other profile in that choice task.12 The mixed logit model explicitly models differences in preferences among respondents.
The main variables of interest are the CCT programme attributes in the DCE—the number of ANC visits during pregnancy, number of visits for child growth monitoring and immunisation per year, time spent on each visit, perceived health benefit for mother and child, and the cash transfer amount (table 1). In addition, respondents were asked about their socio-demographic background, health-seeking behaviour related to use and household assets. At the household level, a wealth index was constructed based on assets available in the household using principal component analysis.31 Poor households were defined as those in the lowest 2 quintiles of wealth.
‘Low service use’ mothers: of interest is to know the preferences of mothers who are unlikely to use desired levels of ANC and child health services. Changing the behaviour of this group so that they consume optimal levels of health services would be a key objective of the CCT programme. We define ‘low service use’ mothers as those that had less than three ANC visits or had not taken their children for any growth monitoring. Indian government norms require eight ANC visits during pregnancy, and we defined less that one visit per trimester as low use. The remaining respondents were classified as ‘adequate users’.
We first conducted exploratory data analysis and estimated univariate statistics (means, SDs) for all the variables of interest. We fit a series of mixed logit regression models using Stata V.14 software.32 We tried several ways of modelling the variables such as considering them as continuous variables, including higher order terms to capture potential non-linearities in the underlying utility function, dummy variable coding and effects-coding. We also fit models with interaction terms. The final model selection was based on the log-likelihood ratio, goodness-of-fit statistics like the Akaike information criterion and arriving at a parsimonious model.
Model 1 represents the base model in which the independent variables are the programme attributes; we model the four attributes of ANC visits, growth-monitoring visits, duration of each visit and health benefit using dummy variable coding, and the cash amount as a continuous variable. In model 2 we expand this basic model to include interaction terms between the programme attributes and ‘low service use’ individuals, that is, those who use below optimal levels of ANC and growth-monitoring services. The reference category here are the remaining mothers, that is, those with adequate service use (‘adequate users’). In model 3, we include interactions between poor respondents (identified as being in the bottom 2 quintiles of the asset distribution) and the CCT programme attributes. The reference category here are respondents who are ‘not poor’, that is, in the top-2 wealth quintiles.
Of interest is to know how much cash mothers require for a unit increase in the attribute level such as number of growth-monitoring visits, that is, the marginal willingness to accept (WTA).33 We estimate the WTA by dividing the attribute coefficients with the negative of the cash attribute coefficient. We only estimate WTA for attributes that are statistically significant.
Of interest is to know the relative importance of different programme attributes on the choices that respondents made. The attribute coefficients represent the contribution of a unit change in the attribute level to the respondents utility. Because of scale differences in the attributes, their coefficients cannot be directly compared. We estimate the utility share of each attribute by dividing the difference in coefficients between the highest and lowest attribute level by the sum of these differences across attributes. These attribute shares represent the relative importance of each attribute.12 24
We use equation (2) to estimate the predicted probability of a programme with specific attribute levels being selected. We compare the selection probability of a programme having base-level attribute levels except for the attribute level of interest, with that of a reference programme defined as one with no cash transfer, four ANC visits, four growth-monitoring visits per year, each visit being of 1 hour duration and a fair health benefit. We report the difference between the selection probability of the base programme with a programme with one attribute level changed.
Patient and public involvement
No patients were involved in this study. The public was first involved at the questionnaire design and pretesting stage, and feedback from respondents incorporated into questionnaire revisions. To lower the excessive reporting burden expressed by some respondents, the choice sets were split into two blocks. Results from this study will be shared with the UP health department.
Results
A total of 405 respondents were sampled to fulfil the sample size quota of 400 women with children below 3 years of age in the three blocks surveyed (table 2). All participants were rural residents. None of the respondents had missing data on the variables of interest. On average, women were 27 years old, just over half were literate and on average had one child under the age of 3. Mothers in our sample had relatively high levels of service uptake—most (93%) had at least one ANC visit, while only 15% of them had children under 3 years of age with no growth monitoring. The average travel time to the AWC (ie, village nutrition centre) was around 11 min, which is indicative of the proximity of ANC and growth-monitoring services to communities. The ‘low use’ group, which was 54% of the respondents, had lower levels of literacy, had more poor households, had a higher proportion of women with no or few ANC visits, and a higher proportion of children with no growth monitoring. Women in our sample have higher levels of service use than those in UP’s population—state representative surveys for 2015–2016, estimate that 69% of married women in UP had an ANC during pregnancy, and 46% of children under 3 years of age in UP received some ICDS service.13 Services at public health and nutrition facilities are free or a nominal fee charged to users.
Table 2.
Background characteristics of respondents
| All | Low use of maternal and child health services | |||
| Mean | SD | Mean | SD | |
| Household size | 6.1 | 2.44 | 6.1 | 2.35 |
| Mother’s age (years) | 26.6 | 4.44 | 26.8 | 4.65 |
| Mother can read and write (%) | 59 | 53 | ||
| Number children below 3 years of age | 1.1 | 0.29 | 1.1 | 0.27 |
| Age of youngest child (months) | 16.4 | 7.75 | 16.7 | 8.34 |
| Poor household (%) | 40 | 43 | ||
| ANC visits during last pregnancy (%) | ||||
| None | 7 | 12 | ||
| 1–3 | 65 | 78 | ||
| 4–8 | 26 | 8 | ||
| 9–15 | 2 | 2 | ||
| 100 | 100 | |||
| Children with no growth monitoring in last 12 months (%) | 15 | 28 | ||
| Travel time to nutrition (AWC) centre (minutes) | 10.7 | 11.28 | 11.5 | 11.40 |
| N (observations) | 405 | 218 | ||
AWC, Anganwadi Center.
The DCE included one choice set which served as a rationality test. Most respondents (87%) passed with failures comprising 13% of the respondents. We separately analysed respondents who failed the rationality test but did not find any differences in the results compared with the full sample. The analysis we present is based on the full sample.
Table 3 presents results of the mixed logit regression model. The regression coefficients are preference weights that reflect the contribution of the attribute levels to the utility that respondents assign to a particular programme profile.12 The SDs of the attributes capture the variance in preference weights across the sample.
Table 3.
Mixed logit regression results for discrete choice experiment
| Attributes | Level | (1) | WTA (95% CI) | (2) | (3) | |||
| Only attributes | Interaction with low service use | Interaction with poor | ||||||
| Mean | SD | Mean | SD | Mean | SD | |||
| Cash transfer amount (‘000 Indian rupees) | Cash | 0.357** | 0.393** | 0.338** | ||||
| (0.014) | (0.022) | −0.017 | ||||||
| Antenatal care visits | 8 visits | 0.032 | 0.123 | 0.057 | ||||
| (Reference: 4 visits) | (0.063) | (0.099) | (0.082) | |||||
| 12 visits | −0.070 | −0.031 | −0.045 | |||||
| (0.065) | (0.099) | (0.084) | ||||||
| Growth-monitoring visits/year | 8 visits | −0.206** | 0.118 | 144* | −0.382** | 0.352 | −0.322** | −0.262 |
| (Reference: 4 visits) | (0.066) | (0.424) | (54 to 233) | (0.105) | (0.217) | −0.086 | (0.210) | |
| 12 visits | −0.107* | −0.001 | 38* | −0.214** | −0.004 | −0.148* | −0.003 | |
| (0.063) | (0.096) | (−5 to 80) | (0.095) | (0.123) | (0.081) | (0.110) | ||
| Duration of visit (hours) | 4 hours | −0.344** | 0.001 | 321* | −0.351** | −0.036 | −0.353** | −0.015 |
| (Reference: 1 hour) | (0.062) | (0.150) | (206 to 437) | (0.096) | (0.146) | (0.081) | (0.168) | |
| 8 hours | −0.178** | 0.014 | 71* | −0.168* | 0.001 | −0.133* | 0.029 | |
| (0.061) | (0.206) | (23 to 120) | (0.095) | (0.251) | (0.079) | (0.219) | ||
| Health benefit received | Fair | 0.406** | −0.009 | −1137 | 0.485** | 0.046 | 0.495** | −0.048 |
| (Reference: poor) | (0.063) | (0.166) | (−41 to 643) | (0.097) | (0.380) | (0.081) | (0.262) | |
| Good | 1.019** | 0.599** | −2854 | 1.054** | 0.731** | 1.204** | 0.682** | |
| (0.072) | (0.104) | (–3225 to –2484) | (0.114) | (0.126) | (0.098) | (0.120) | ||
| Interaction of attribute X low service use (ref: ‘adequate service use’ /poor (ref: ‘non-poor’) | ||||||||
| Cash X | 0.186** | 0.426 | 0.337** | 0.444** | ||||
| (0.057) | (0.051) | (0.068) | (0.055) | |||||
| Growth monitoring: 8 visits X | 0.397** | 0.425 | 0.483** | −0.206 | ||||
| (0.167) | (0.337) | (0.177) | (0.557) | |||||
| Growth monitoring: 12 visits X | 0.285* | 0.049 | 0.237 | −0.059 | ||||
| (0.150) | (0.242) | (0.159) | (0.254) | |||||
| Health benefit: fair X | 0.096 | 0.423** | 0.01 | 0.250 | ||||
| (0.152) | (0.211) | (0.155) | (0.327) | |||||
| Health benefit: good X | 0.445** | −0.378 | −0.074 | 0.381 | ||||
| (0.195) | (0.268) | (0.185) | (0.304) | |||||
| Observations | 7290 | 7290 | 7290 | |||||
| Log likelihood | −1779 | −1704 | −1701 | |||||
| AIC | 3577 | 3372 | 3437 | |||||
(1)*p<0.10, **p<0.05; (2) SD is the SD ofthe random coefficient, only SD for statistically significant attributes shown; (3) SE in parenthesis; (4) WTA estimates are in rupees (US$1=INR70), WTA estimated only for statisticallysignificant attributes; (5) to be concise, interaction results are only shownfor statistically significant interaction.
*WTA estimates are per visit.
AIC, Akaike information criterion; INR, Indian rupee; WTA, willing to accept.
Model 1 is the base model and has the programme attributes as independent variables. The positive sign on the coefficients of cash transfer and health benefit attributes indicates that mothers preferred programmes with higher cash amounts and better health benefits. The size of the health benefit coefficient indicates that programmes with ‘good’ health benefit were preferred to those with ‘fair’ health benefits, and to those with ‘poor’ health benefit. The coefficient of ANC visits attribute was not statistically significant. The negative sign on the attributes of growth-monitoring visits, duration of visits indicates that mothers preferred programmes with fewer growth-monitoring visits and shorter visit durations. For growth monitoring, the sign of the coefficient indicates that 8 visits were less preferred to 12 visits. Similarly, for duration of visits, visits that took 4 hours were less preferred to visits that took 8 hours. These patterns suggest non-linearity in the utility function.34 For both the growth monitoring and visit duration attributes, it is unclear why mothers had a stronger preference for higher levels of visits or duration. The SDs of the attribute coefficients are mostly statistically insignificant (except for good health benefit) suggesting that there was insignificant variation in preferences for these attributes across the sampled respondents.
Model 2 presents the results for the interaction between the programme attributes and mothers who are infrequent users of ANC and child growth monitoring, that is, ‘low users’. The reference group is ‘adequate users.’ The interaction terms indicate if the strength of attribute preferences (ie, utility) is different for ‘low users’ compared with ‘adequate users’. The interaction terms are positive and statistically significant for the attributes of cash transfer amount, growth-monitoring visits, ‘good’ health benefit—this indicates that ‘low users’ have stronger preferences for these attributes compared with the rest of the sample. There was no difference between ‘low users’ and ‘adequate users’ for the ANC, visit duration and ‘fair’ health benefit attribute.
Model 3 presents the interactions between belonging to a poor household and programme attributes. We find a positive and statistically significant relationship between being poor and the cash transfer amount, and an increase in growth-monitoring visits from four to eight. This implies that poor households had stronger preferences for these attributes compared with non-poor households. For the remaining attributes of ANC visits, high number of growth-monitoring visits, visit duration and health benefit, there was no significant difference in preferences between poor and non-poor households.
The ratio of the attribute coefficients divided by the negative of the cash transfer amount gives the marginal rate of substitution between the programme attribute and a change in the cash transfer amount (table 3). A positive sign indicates the amount mothers are willing to accept to consume more of that attribute and a negative sign implies how much less of cash transfer that mothers are willing to accept (ie, forego) to consume more of that attribute. We report WTA estimates only for the statistically significant attributes in model 1.
Mothers in the study placed a low value per additional growth-monitoring visit in a year for children under 3 years of age—they require between 38 and 144 Indian rupees for every additional growth-monitoring visit. Respondents placed a higher monetary value on visit duration—they would need to be paid between 71 and 321 Indian rupees for each additional hour it took to complete a visit to a health centre. This represents the marginal opportunity cost of an extra hour spent seeking healthcare. Mothers highly valued the health benefit they (or their children) receive from using health services. They were willing to forgo (ie, accept a lower cash transfer amount) 1137 Indian rupees for services that produced fair, and 2854 Indian rupees for services that resulted in good health.
The relative importance of CCT programme attributes is depicted in figure 2. It indicates that mothers gave the most importance to the cash transfer amount, followed by the health benefit that they (or their children) received from using health services, visit duration, number of growth-monitoring visits and ANC visits.
Figure 2.
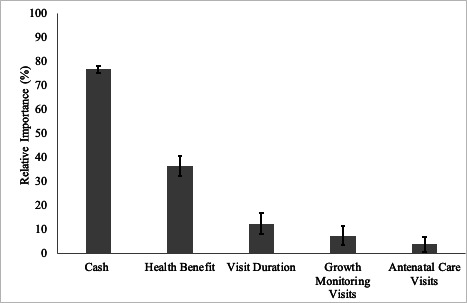
Relative importance of conditional cash transfer programme attributes.
Figure 3 presents the difference in the probability of selecting a CCT programme having the index-attribute level and all other attributes set to reference levels compared with the reference programme profile. The reference programme profile is defined as a situation with no cash transfer, four ANC visits during pregnancy, four growth-monitoring visits per year, duration of visit is 1 hour and ‘fair’ health benefit received. A cash transfer of 6000 Indian rupees, which is around what the MBP currently offers, increases the probability of selecting a programme by 80%, while a cash transfer of 3000 Indian rupees increases it by 50% compared with the reference programme profile. Programmes that had ‘good’ health benefit had a 48% higher probability of being selected, which is nearly as large as a cash transfer amount of 3000 Indian rupees. Programmes with the remaining attribute levels had a small or lower probability of being selected compared with the reference programme. For example, a programme with eight growth-monitoring visits per year lowered the probability of a programme being selected by 10%, while when the visit duration was 4 hours the programme’s probability of being selected was lower by 18 points.
Figure 3.
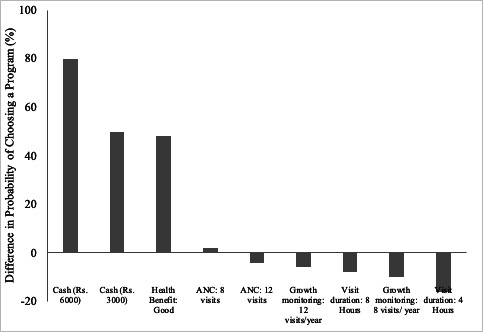
Difference in the predicted probability of selecting a CCT programme having a particular attribute and the reference program profile.*. *Reference program profile: no cash, four antenatal and growth-monitoring visits, 1 hour visit duration and fair health benefit. ANC, antenatal care; CCT, conditional cash transfer.
Discussion
CCT programmes are rapidly becoming an important policy tool in low/middle-income countries like India to increase demand for maternal and child health services. In this study, we examined the preferences of mothers with young children for attributes of a CCT programme focused on maternal and child health services (including nutrition), as revealed by their choices between hypothetical programme profiles using the DCE method. Our findings indicate that mothers valued the amount of cash transfer the most, followed by the health benefit received from services, shorter visit duration for services, growth-monitoring visits and ANC visits. Importantly, mothers did not have strong preferences for conditionalities related to number of visits to the health centre for ANC or for growth-monitoring and immunisation visits.
The finding that mothers valued the cash transfer much more than all other CCT attributes highlights the important role of financial incentives in increasing demand for health services. In this DCE, a cash transfer programme offering 6000 Indian rupees ($86), an amount currently being offered by the MBP in India, had an 80% greater probability of being selected compared with the reference programme profile (no cash incentive). Previous studies have also confirmed the power of financial incentives to increase demand for services.35 36
CCT programmes typically require beneficiaries to fulfil conditionalities to obtain cash rewards. It is important that the conditionalities do not place an excessive burden on beneficiaries otherwise they would deter participation. In this DCE, the conditionalities were framed around the number of visits for ANC, and for child immunisations and growth monitoring. This can potentially add up to a substantial number of visits given current norms—eight ANC visits during pregnancy (WHO guidelines), four visits in the first year for immunisation and monthly monitoring until 3 years of age.28 We expected that mothers would prefer fewer health centre visits, as well as shorter time spent accessing services. Our findings suggest that mothers put a low valuation on health centre visits, though they preferred fewer health centre visits for child immunisation and growth monitoring (ANC visits was statistically insignificant). The low preference for health centre visits is reflected in the low WTA estimates which suggest that mothers required between 38 Indian rupees ($0.5) and 144 Indian rupees ($2.0) per additional growth-monitoring/immunisation visit. These findings imply that even modest cash transfer amounts can increase the number of required interactions with healthcare providers given the low marginal WTA values. One reason for this finding is that service delivery points were in close proximity to households (average travel time taken to service delivery points was 11 min).
Studies on CCT programmes have noted that beneficiary use of maternal and child health services declines with distance to service delivery points.1 In our study mothers preferred to spend less time accessing health services. Further, longer visit duration was associated with lower likelihood of a programme being selected. Mothers required between 71 Indian rupees ($1) and 321 Indian rupees ($4.6) per additional hour of visit time. An implication of this is that beneficiaries who have to spend more time accessing services, due to long waiting times or have long travel times to service delivery points, need more compensation. Overall, while fewer and shorter visits are preferred, frequent health centre visits or longer visit duration may not have large negative effects on decisions to participate in the CCT programme in contexts where service coverage is high.
Mothers had a strong preference for CCT programmes which produced positive health benefits. The health benefit attribute was the second most important attribute (after cash). Further, in the DCE, programmes with the highest (‘good’) health benefit had a 48% higher likelihood of being selected, compared with the reference programme (‘fair’ health benefit, all other attributes at reference levels). To put this in context, this percentage point increase was similar to a programme that offered a cash reward of 3000 Indian rupees, compared with the reference programme. Mothers were willing to accept reductions in the cash transfer amount (ie, give up) of 1137 Indian rupees for a programme that produced ‘fair’ health benefits and 2854 Indian rupees for one that produced ‘good’ health benefits. These findings point to the importance of beneficiary perceptions of value or benefit in care-seeking decisions. For CCT programmes, therefore, communicating the value of using health services to potential beneficiaries, as well as ensuring that they receive quality services is important for increasing and maintaining demand for services. Further, because mothers are willing to accept less cash transfer amounts for improved health benefit, CCT programmes can offer smaller cash rewards without sacrificing demand if combined with demonstrated improvements in health benefits to their beneficiaries. However, it is important to note that a reduced cash amount can have negative consequences in terms of lower household income and expenditures on more or better quality food (and other health-producing services) for the mother and children, the ability of the mother to take time off work without income loss, and even lessening the empowerment the mother enjoys due to the cash reward.
An important objective of CCT programmes is to increase demand for health services particularly among individuals who consume them at below optimal levels. Our findings indicate that ‘low service users’, that is, mothers who consumed low levels of ANC during pregnancy or did not take their children for growth monitoring, valued the cash transfer, growth-monitoring visits and ‘good’ health benefit more than mothers who were not in this category. Further, mothers from poor households valued the cash transfer amount and growth-monitoring visits more than non-poor mothers. This reinforces the role that cash transfer programmes can play an encouraging demand for maternal and child health services among those groups that are at risk of underconsuming them. Importantly, the salience of positive health benefit derived from health services highlights the importance of communicating the value of health services, as well as quality of care, for increasing demand among those that underconsume these services. Quality of care in the context of CCTs has been an important issue in India. For example, the existing CCT for institutional deliveries (JSY programme) has had large effects on increasing institutional deliveries but not on maternal mortality leading critics to point out the poor quality of care that women receive when they deliver at health facilities.6
This study has several notable limitations. Because the DCE method relies on stated preferences, the respondents revealed preferences, that is, how they might actually behave when exposed to a CCT programme can be different. Second, our DCE used a forced choice design in which mothers had to choose between two programme alternatives without an opt-out option. In the real world, mothers can choose not to participate in a programme. As discussed in the DCE design section of this paper, having an opt-out option can offer scenarios closer to what respondents might face in reality. It is not likely that every mother will participate in the CCT programme. In such situations, not having an opt-out option can upwardly bias estimated attribute effects and predicted probabilities of participation.30 Our decision not to include an opt-out option was based on pragmatic considerations—during pretesting we found that no one selected the opt-out option which made its inclusion uninformative. The positive affirmation to participate in the CCT programme could be due to acquiescence bias because respondents felt that this was the appropriate answer, especially since most respondents consumed some level of focus health services (though the majority were not at recommended levels). In our sample, only 6% of mothers had no ANC during their last pregnancy, and 15% of children had not received any growth monitoring. Nevertheless, the absence of an opt-out option can potentially upwardly bias estimated programme attribute effects, though the relative importance of the attributes will likely remain the same. Another limitation is that respondents could be making choices based on few attributes (eg, cash amount). In this case, preferences for select attribute levels will be incorrectly interpreted as preference for all the attribute levels that define that CCT programme profile. This would upwardly bias the estimated utility weights (ie, regression coefficients). Further, the estimated monetary valuations of the programme attributes would be biased too. We expect this is less of an issue because we limited the number of programme attributes to five to reduce cognitive burden, as well as having a wide range of values for the cash transfer amount.
Another limitation is the limited involvement of respondents in the design of the DCE questionnaire. Our starting point for identifying attributes and their levels was the CCT programme that were currently being implemented in India. Further, based on the literature and interaction with respondents during pretesting, the perceived value of services also emerged as important factor. The ‘health benefit’ attribute is another limitation; because it is subjective and can be interpreted differently by different respondents, its use in our analysis should be interpreted with caution. The external validity of the study findings depends on how well the study sample represents the general population of UP. Comparisons with representative surveys in UP (see the Results section) show that service use outcomes in the study sample are higher compared with the state average. One reason for this could be that service delivery points were in close proximity (average of 11 min travel time) to the sampled households. As such, our study results better represent households that have easy physical access to maternal and child health services.
CCT programmes can serve as effective tools for increasing demand for maternal and child health services.37–39 Having onerous conditionalities can be detrimental to the programme goals. The cash awards can have other positive benefits in terms of increasing household income, investments in better nutrition, health and human capital, as well as empowering women in the household. The findings from this study confirm that cash rewards can have large effects on increasing demand for maternal and child health services. However, the value or benefit that beneficiaries receive from health services is also important for care-seeking decisions. As such, incentivising demand should go together with providing quality services.
Acknowledgments
The authors would like to thank Kantar Public for data collection support, Dr John Bridges for advice on the DCE methods and Dr Purnima Menon for contribution and resource support in producing this study.
Footnotes
Handling editor: Seye Abimbola
Contributors: KDR, SK, AK and DB contributed to the study design and questionnaire development. SK and AK were responsible for data collection. KDR, SK and AK led the data analysis and paper writing with contributions from DB. KDR and DB provided overall guidance to the study.
Funding: This study was funded by the Ideas Incubator Grant from the Department of International Health, Johns Hopkins University.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Ethics approval: Ethical approval was obtained from the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland and the Institutional Review Board of the Center for Media Studies in New Delhi, India.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon request. To obtain data please email Krishna D Rao (kdrao@jhu.edu).
References
- 1. Handa S, Peterman A, Seidenfeld D, et al. . Income transfers and maternal health: evidence from a national randomized social cash transfer program in Zambia. Health Econ 2016;25:225–36. 10.1002/hec.3136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ranganathan M, Lagarde M. Promoting healthy behaviours and improving health outcomes in low and middle income countries: a review of the impact of conditional cash transfer programmes. Prev Med 2012;55:S95–105. 10.1016/j.ypmed.2011.11.015 [DOI] [PubMed] [Google Scholar]
- 3. Owusu-Addo E, Cross R. The impact of conditional cash transfers on child health in low- and middle-income countries: a systematic review. Int J Public Health 2014;59:609–18. 10.1007/s00038-014-0570-x [DOI] [PubMed] [Google Scholar]
- 4. Glassman A, Duran D, Fleisher L, et al. . Impact of conditional cash transfers on maternal and newborn health. J Health Popul Nutr 2013;31:S48. [PubMed] [Google Scholar]
- 5. Fernald LCH, Gertler PJ, Neufeld LM. Role of cash in conditional cash transfer programmes for child health, growth, and development: an analysis of Mexico's Oportunidades. Lancet 2008;371:828–37. 10.1016/S0140-6736(08)60382-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Randive B, Diwan V, De Costa A. India's conditional cash transfer programme (the JSY) to promote institutional birth: is there an association between institutional birth proportion and maternal mortality? PLoS One 2013;8:e67452. Vol. 6. 10.1371/journal.pone.0067452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Powell-Jackson T, Mazumdar S, Mills A. Financial incentives in health: new evidence from India's Janani Suraksha Yojana. J Health Econ 2015;43:154–69. 10.1016/j.jhealeco.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 8. Baba-Ari F, Eboreime EA, Hossain M. Conditional cash transfers for maternal health interventions: factors influencing uptake in north-central Nigeria. Int J Health Policy Manag 2018;7:934–42. 10.15171/ijhpm.2018.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Okoli U, Morris L, Oshin A, et al. . Conditional cash transfer schemes in Nigeria: potential gains for maternal and child health service uptake in a national pilot programme. BMC Pregnancy Childbirth 2014;14:408. 10.1186/s12884-014-0408-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sidney K, Tolhurst R, Jehan K, et al. . ‘The money is important but all women anyway go to hospital for childbirth nowadays’ - a qualitative exploration of why women participate in a conditional cash transfer program to promote institutional deliveries in Madhya Pradesh, India. BMC Pregnancy Childbirth 2016;16 10.1186/s12884-016-0834-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sabde Y, Chaturvedi S, Randive B, et al. . Bypassing health facilities for childbirth in the context of the JSY cash transfer program to promote institutional birth: a cross-sectional study from Madhya Pradesh, India. PLoS One 2018;13:e0189364. 10.1371/journal.pone.0189364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hauber AB, González JM, Groothuis-Oudshoorn CGM, et al. . Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR conjoint analysis good research practices task force. Value Health 2016;19:300–15. 10.1016/j.jval.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 13. IIPS National Family Health Survey (NFHS-4), India, 2015-16: Uttar Pradesh. Mumbai: International Institute for Population Sciences, 2017. [Google Scholar]
- 14. Raghunathan K, Chakrabarti S, Avula R, et al. . Can conditional cash transfers improve the uptake of nutrition interventions and household food security? Evidence from Odisha's Mamata scheme. PLoS One 2017;12:e0188952. 10.1371/journal.pone.0188952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. GOI Ministry of Women and Child Development. [Online] Government of India. [Cited: November 5, 2018]. Available: http://www.wcd.nic.in/schemes/pradhan-mantri-matru-vandana-yojana
- 16. GOI PMMVY-CAS training. New Delhi: Ministry of Women and Child Development, Government of India, 2017. [Google Scholar]
- 17. Editorial WCD Ministry considering cash transfers under ICDS, decision soon: Secretary. [Online]. [Cited: November 5, 2018], 2017. Available: https://www.thehindubusinessline.com/economy/policy/wcd-ministry-considering-cash-transfers-under-icds-decision-soon-secretary/article9866237.ece
- 18. Ayog N. Nourishing India. New Delhi: NITI Ayog, Government of India. [Google Scholar]
- 19. Becker F, Anokye N, de Bekker-Grob EW, et al. . Women's preferences for alternative financial incentive schemes for breastfeeding: a discrete choice experiment. PLoS One 2018;13:e0194231. 10.1371/journal.pone.0194231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marti J, Bachhuber M, Feingold J, et al. . Financial incentives to discontinue long-term benzodiazepine use: a discrete choice experiment investigating patient preferences and willingness to participate. BMJ Open 2017;7:e016229. 10.1136/bmjopen-2017-016229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen T-T, Tung T-H, Hsueh Y-SA, et al. . Measuring preferences for a diabetes pay-for-performance for patient (P4P4P) program using a discrete choice experiment. Value Health 2015;18:578–86. 10.1016/j.jval.2015.03.1793 [DOI] [PubMed] [Google Scholar]
- 22. Danyliv A, Pavlova M, Gryga I, et al. . Preferences for physician services in Ukraine: a discrete choice experiment. Int J Health Plann Manage 2015;30:346–65. 10.1002/hpm.2239 [DOI] [PubMed] [Google Scholar]
- 23. Obse A, Ryan M, Heidenreich S, et al. . Eliciting preferences for social health insurance in Ethiopia: a discrete choice experiment. Health Policy Plan 2016;31:1423–32. 10.1093/heapol/czw084 [DOI] [PubMed] [Google Scholar]
- 24. Liu Y, Kong Q, de Bekker-Grob EW. Public preferences for health care facilities in rural China: a discrete choice experiment. Soc Sci Med 2019;237:112396. 10.1016/j.socscimed.2019.112396 [DOI] [PubMed] [Google Scholar]
- 25. WHO How to conduct a Discrete Choice Experiment for Health Workforce Recruitment and Retention in Remote and Rural Areas: A User Guide with case Studies. Geneva: World Health Organization, 2012. [Google Scholar]
- 26. GOI Guidelines for ASHAs/AWWs/ANMs/PRIs. New Delhi: Ministry of Health and Family Welfare, 2007. [Google Scholar]
- 27. WHO WHO Reproductive Health Library. WHO recommendation on group antenatal care. Geneva: The WHO Reproductive Health Library, World Health Organization, 2016. [Google Scholar]
- 28. NIPCCD Growth Monitoring Manual. New Delhi: National Institute of Public Cooperation and Child Development, 2009. [Google Scholar]
- 29. Grossman M. On the concept of health capital and the demand for health. J Polit Econ 1972;80:223–55. 10.1086/259880 [DOI] [Google Scholar]
- 30. Ryan M, Skåtun D. Modelling non-demanders in choice experiments. Health Econ 2004;13:397–402. 10.1002/hec.821 [DOI] [PubMed] [Google Scholar]
- 31. Filmer D, Pritchett LH. Estimating wealth effects without expenditure data--or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32. 10.1353/dem.2001.0003 [DOI] [PubMed] [Google Scholar]
- 32. StataCorp Stata statistical software: release 14. s.l. College Station, TX: StataCorp LP, 2015. [Google Scholar]
- 33. Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user's guide. Pharmacoeconomics 2008;26:661–77. 10.2165/00019053-200826080-00004 [DOI] [PubMed] [Google Scholar]
- 34. van der Pol M, Currie G, Kromm S, et al. . Specification of the utility function in discrete choice experiments. Value Health 2014;17:297–301. 10.1016/j.jval.2013.11.009 [DOI] [PubMed] [Google Scholar]
- 35. World Bank Conditinal Cash Transfers Reducing Present and Future Poverty. Washington DC: World Bank, 2009. [Google Scholar]
- 36. Giles EL, Becker F, Ternent L, et al. . Acceptability of financial incentives for health behaviours: a discrete choice experiment. PLoS One 2016;11:e0157403. 10.1371/journal.pone.0157403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bassani DG, Arora P, Wazny K, et al. . Financial incentives and coverage of child health interventions: a systematic review and meta-analysis. BMC Public Health 2013;13:S30. 10.1186/1471-2458-13-S3-S30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Leroy JL, Ruel M, Verhofstadt E. The impact of conditional cash transfer programmes on child nutrition: a review of evidence using a programme theory framework. J Dev Effect 2009;1:103–29. 10.1080/19439340902924043 [DOI] [Google Scholar]
- 39. Owusu-Addo E, Renzaho AMN, Smith BJ. The impact of cash transfers on social determinants of health and health inequalities in sub-Saharan Africa: a systematic review. Health Policy Plan 2018;33:675–96. 10.1093/heapol/czy020 [DOI] [PMC free article] [PubMed] [Google Scholar]


