Abstract
Purpose:
The purpose was to determine the real-world efficacy of phacoemulsification cataract surgery and Hydrus microstent in Black and Afro-Latinx patients with glaucoma.
Methods:
A retrospective noncomparative single-center study of 76 Black and Afro-Latinx patients with glaucoma who underwent phacoemulsification cataract surgery and Hydrus microstent placement for treatment of glaucoma at single practice. Investigated parameters were intraocular pressure (IOP), number of medications, mean deviation on visual field test, and visual acuity. Patients were also subgrouped into mild, moderate, and advance glaucoma for further analysis.
Results:
We reviewed a total of 76 patients who had 6 months of follow up in the study. The mean number of medications decreased significantly from 2.6 ± 1.5 preoperatively to 0.72 ± 1.4 in 6 months (p < 0.0010), while IOP decreased from 14.7 ± 3.7 to 13.9 ± 4.3 (p = 0.25). At 6 months, 55 patients (74%) of all patients were medication free (n = 27, 84.4% mild glaucoma; n = 17, 70.8% moderate glaucoma; n = 10, 50% advance glaucoma). There was significant improvement in visual acuity (p < 0.00010) and stabilization of mean deviation on visual field test (baseline −9.2; 6 months −9.1; p = 0.22). The most common adverse effect was a transient IOP spike and transient corneal edema (n = 6, 7.9%; n = 6, 7.9%, respectively) with spontaneous resolution in all cases. No sight-threatening complications were reported at 6 months.
Conclusion/clinical relevance:
This 6-month retrospective study demonstrated the efficacy of phacoemulsification cataract surgery and Hydrus microstent in reducing the medication burden while maintaining lower IOP in Black and Afro-Latinx patients with glaucoma.
Keywords: Black patients, cataract surgery, glaucoma, Hydrus microstent, microinvasive glaucoma surgery
Introduction
Age-related cataract is the most prevalent and leading cause of blindness in the world.1 Glaucoma is the second most prevalent eye condition worldwide with projected 111.8 million people between the ages of 40 and 80 years affected in 2040.2 Cataract surgery continues to be the most frequently performed procedure among Medicare beneficiaries; however, Schein and colleagues3 reported a 30% lower rate of cataract surgery among Black patients compared with their White counterparts when adjusted for age and sex. The prevalence of glaucoma is higher in Black and Afro-Latinx communities compared with Whites.4 The intraocular pressure (IOP)-lowering effects of phacoemulsification cataract surgery has been well documented.5
There is a progressive increase in lens mass,6 and anterior movement of the lens zonules adjacent to the posterior iris with aging. The increase in lens size results in compression of the trabecular meshwork (TM) and the Schlemm canal which leads to elevation in IOP.7 In addition, there is increasing pigment liberation from lens zonules-iris rubbing against iris pigment epithelium contact due to iridolenticular contact exacerbated during accommodation (Figure 1).8 The pigment liberation leads to obstruction of the TM and further contributes to elevating IOPs (Figure 2).8 There is an association between elevated IOP and the development of glaucoma. Cataract surgery lowers IOP and prevents against lens-induced glaucoma.9
Figure 1.
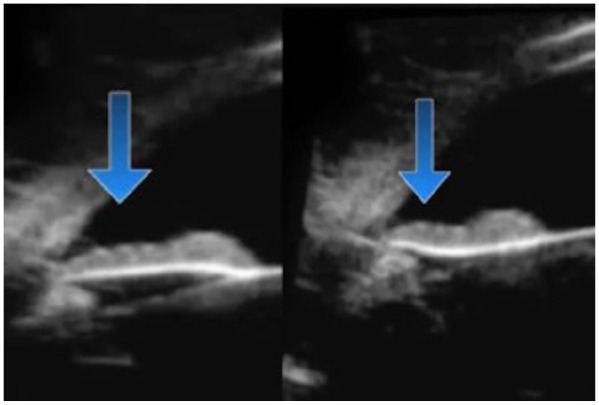
Increased irido-zonular contact during accommodation.
Figure 2.
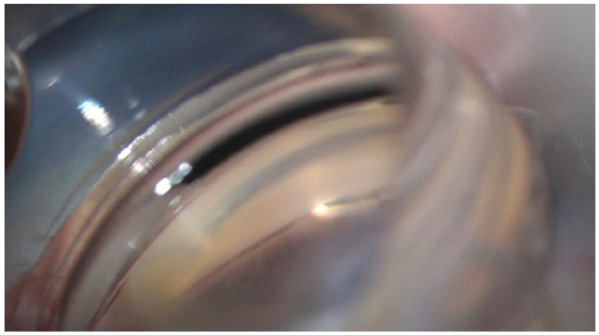
Hydrus inserter in front of the heavily pigmented trabecular meshwork.
Currently, management of glaucoma includes ocular hypotensive medications, laser, and incisional surgery. Initial management of glaucoma with ocular hypotensive medications has only been partially successful to lower IOP because of poor patient compliance and ocular side effects; unfortunately, many patients with glaucoma still progress with medical therapy.10,11 The IOP-lowering effect of laser surgery decreases in efficacy with time, and patients will often require additional medical therapy. Patients treated with laser are also predisposed to adverse effects of iritis and pressure spikes.12
The gold standard incisional surgery, trabeculectomy, and aqueous shunt surgery, although very effective in reducing IOP, have a higher risk of complications compared with the current medical and laser therapy. The ab externo approach used to create a filtration bleb in these procedures predisposes patients to a lifelong risk of endophthalmitis and bleb-related ocular surface issues.13 There has recently been a paradigm shift toward earlier cataract surgery and microinvasive glaucoma surgery (MIGS) to safely lower IOP and reduce medication burden in patients with glaucoma. This is due to the enhanced safety profile of cataract surgery and MIGS. Cataract surgery alone can lower IOP up to 2.22 mmHg [95% confidence interval (CI): 1.93–2.52 mmHg; p < 2 × 10−16] in early glaucoma patients.14 In addition, in glaucoma patients, IOP can be lowered further when combined with trabecular bypass surgery.15–18 These new surgical techniques and devices enhance aqueous outflow effectively and safely without the formation of blebs. Among them are iStent (Glaukos), iStent inject (Glaukos), OMNI (Sight Sciences), Kahook Dual Blade (New World Medical), and Hydrus (Ivantis, Inc, Irvine, CA).
Combination cataract surgery and MIGS devices dramatically lower IOP levels and reduced the number of medications used in recent studies and are increasingly becoming the mainstay treatment for mild to moderate glaucoma.19 The HORIZON study showed excellent IOP lowering in the cataract surgery–alone group from 25.3 ± 2.9 to 19.3 ± 4.2 mmHg. This was significantly enhanced in the combined cataract surgery and Hydrus microstent implantation group to 17.5 ± 3.9 mmHg.20 The COMPARE study showed that patients with Hydrus microstent used fewer medications with a high surgical success rate compared with the 2-iStent device group (preoperative IOP 2-iStent 19.1 ± 3.6 mmHg, Hydrus 19.0 ± 2.5 mmHg; 12-month 2-iStent IOP 18.1 ± 3.7 mmHg, Hydrus 17.3 ± 3.7 mmHg).21
Although clinical trials with a 2-year follow-up period showed efficacy of Hydrus microstent, the real-world efficacy of Hydrus microstent has not been studied in a predominately Black and Afro-Latinx population. Hydrus is currently Food and Drug Administration (FDA) approved in the United States for use together with cataract surgery for patients with mild to moderate open-angle glaucoma. Here, we report the real-world efficacy of cataract extraction and Hydrus microstent placement in Black and Afro-Latinx patients.
Methods
This is a retrospective noncomparative study of 76 consecutive Black and Afro-Latinx patients with glaucoma who underwent phacoemulsification cataract surgery and Hydrus microstent placement for treatment of glaucoma at single practice in New York, USA, between December 2018 and December 2019. The ethnic makeup of the patients was reflective of the local community. The study was approved by the Institutional Review Board at the New York Eye and Ear Infirmary of Mount Sinai, New York, USA (IRB-19-02948); in addition, the study adhered to the tenets of the Declarations of Helsinki. All the patients provided written informed consent for evaluation and surgery.
All patients had a full ophthalmological assessment that included visual acuity (VA), Goldmann applanation tonometry, slit-lamp examination, gonioscopy, optic nerve assessment with Zeiss Cirrus 5000 HD-OCT, and visual field (VF) examination with Zeiss Humphrey Visual Field Analyzer 3 (Dublin, California, USA). The indications for Hydrus microstent glaucoma surgery were to reduce IOP and to reduce reliance on IOP-lowering medications at the time of cataract surgery in eyes with significant cataract (cortical and nuclear sclerosis grades 1–4) and medically treated glaucoma while avoiding the formation of a filtering bleb and its associated risk profile. We included consecutive cases that were done with open angles or partially open angles with indentation gonioscopy in the nasal quadrant. We excluded patients who had uveitic, neovascular glaucoma, and angle closure without the TM visible on indentation gonioscopy.
The main outcome measures were IOP reduction and decrease in ocular hypotensive medications after the surgery. Safety was evaluated by tabulating both solicited and unsolicited adverse events from the intraoperative period through the last follow-up. The patients were stratified into subgroups: mild, moderate, and advance based on the Hodapp–Parrish–Anderson criteria to assess the efficacy of phacoemulsification and Hydrus microstent.
All glaucoma medications were stopped in the operative eye on the day of surgery. After the procedure, patients were prescribed prednisolone acetate 1% (Allergan, Dublin, Ireland) ophthalmic solution one drop every 6 h, ofloxacin 0.3% (Rising, Saddle Brook, New Jersey, USA) one drop every 6 h, and ketorolac 0.5% (Allergan, Dublin, Ireland) one drop every 8 h. Baseline and operative data were reviewed prior to the day of surgery, and the clinical course was assessed at day 1, 1, 3, and 6 months, postoperatively. Individual IOP goals were tailored to each individual patient postoperatively, and IOP-lowering medications were withdrawn or added as deemed necessary.
Statistics
The hypothesis is that cataract surgery combined with the Hydrus microstent implant would reduce glaucoma medicine burden and maintain lower IOP. Data analysis was done with Microsoft excel (Microsoft, Redmond, Washington, USA) and Prism GraphPad (GraphPad, Seattle, Washington, USA). We used a paired t test for analysis. In this study, the significance threshold was set at p ⩽ 0.05.
Instrument
The Hydrus microstent (Figure 3) is a biocompatible material made of nickel–titanium alloy and thermally set to fit the curvature of the Schlemm canal. It is made to be placed ab interno through the TM into the Schlemm canal (Figure 4) with the inlet residing in the anterior chamber (AC). The Hydrus microstent is able to dilate and scaffold a quadrant of the Schlemm canal upon placement. The device is able to drain aqueous through the resistant TM into the collecting channels via the Schlemm canal.19
Figure 3.

Hydrus stent.
Figure 4.

Hydrus microstent bypassing obstructed trabecular meshwork.
Procedure
Patients were administered preoperative prednisolone acetate 1% (Allergan, Dublin, Ireland) QID and ofloxacin (Rising, Saddle Brook, NJ, USA) QID starting 3 days prior to surgery. After the eye was prepped with betadine and draped, topical anesthesia was applied, and a clear corneal phacoemulsification was performed with implantation of an intraocular lens. Endocoat (Abbott, Chicago, Illinois, USA) was placed in the eye to deepen the angle. A paracentesis was made 2.5 clock hours to the right of the corneal incision and Endocoat was placed on the cornea. The patient’s head was tilted away from the surgeon about 45°, and the microscope was tilted toward the surgeon about 45°. A direct gonio lens (Katena, Troy Hills, New Jersey, USA) was placed on the eye, and the microscope was focused down to obtain a direct view of the nasal angle structures. If peripheral anterior synechiae partially obstructed the view of the TM, a cyclodialysis spatula was used to gently perform goniosynechialysis for 1–2 clock hours to expose the TM. The presence of viscoelastic served as a tamponade for any heme and preserved visibility. The Hydrus microstent was passed into the AC through the paracentesis. Using the device injector, the TM was incised with the tip of the delivery cannula and the microstent was threaded into the Schlemm’s canal (SC) over a span of approximately 90°. Upon visual confirmation of proper device positioning in the canal, the delivery system was withdrawn and the ophthalmic viscosurgical device removed and replaced with a balanced salt solution. Intracameral injection of diluted Vigamox (Alcon, Geneva, Switzerland) with the balanced saline solution 50/50 1cc was given via the paracentesis at the end of the procedure. In all patients, we noticed the angle was open nasally after cataract surgery or was opened partially with synechialysis with a cyclodialysis spatula 1–2 clock hours for Hydrus insertion.
Results
A total of 76 patients were included in the study. Baseline characteristics of study patients are presented in Table 1. The mean age for the study participants was 70.7 ± 9.4 years. Women outnumbered men in the ratio of 1.17:1.0, and the left eye-to-right eye procedure ratio was 1.05:1.0. The mean baseline preoperative IOP was 14.7 ± 3.7 mmHg with a mean use of 2.6 ± 1.5 ocular hypotensive medications. Of all the patients, 98% were using one or more ocular hypotensive medication and 31.6% were using four or more medications (Table 1).
Table 1.
Baseline characteristics of study participants who underwent phacoemulsification cataract surgery and Hydrus microstent.
| Variable | Category | Statistics |
|---|---|---|
| Age (years) | Mean (SD) | 70.7 ± 9.4 |
| Sex, n (%) | Male | 35 (46%) |
| Female | 41 (54%) | |
| Eye, n (%) | Right | 37 (48.7%) |
| Left | 39 (51.3%) | |
| Baseline IOP (mmHg) | Mean (SD) | 14.7 ± 3.7 |
| Ocular hypotensive medications | Mean (SD) | 2.6 ± 1.5 |
| Patients using ocular hypotensive medications, n (%) | 0 | 2(2.6%) |
| 1 | 24 (31.6%) | |
| 2 | 10 (13.2%) | |
| 3 | 16 (21.1%) | |
| ⩾4 | 24 (31.6%) | |
| Visual acuity (logMAR) | Mean ± SD | 0.36 ± 0.12 |
| MD on VFT (dB) | Mean ± SD | −9.2 ± 7.7 |
| Type of glaucoma | POAG | 44 (57.9%) |
| ACG | 30 (39.5%) | |
| Pigmentary | 1 (1.3%) | |
| Mixed | 1 (1.3%) |
ACG, angle-closure glaucoma; IOP, intraocular pressure; MD, mean deviation; n, number of patients; POAG, primary open-angle glaucoma; SD, standard deviation; VFT, visual field test.
At each postoperative visit, there was a significant drop in the number of medications compared with preoperative values. There was significant decrease in IOP at postoperative day 1 and 3 months only (p < 0.00010; p = 0.0022, respectively; Table 2). The mean IOP and number of medications at postoperative day 1 were 11.2 ± 4.1 mmHg and zero medication, representing a 23.8% drop in IOP and 100% drop in medication use, respectively. At 1 month, the IOP was at baseline values with 93.5% reduction in the number of medications. The IOP trended down at 3 months postoperatively with a mean IOP at 13.3 ± 3.2 (9.5% drop from the baseline) on 0.63 ± 1.2 (75.8% decrease from the baseline) number of medications. At 6 months, the trend continues with a 5.4% drop in the mean IOP (mean IOP at 6 months = 13.9 ± 4, p = 0.25) and 72% decrease in the number of medications (mean medication at 6 months = 0.72 ± 1.4, p < 0.00010).
Table 2.
Main outcome measures, IOP, BCVA, number of ocular hypotensive medications, and mean deviation on visual field at preoperative and follow-up visits for all patients.
| Timepoint | IOP (mmHg) | Ocular hypotensive medications | BCVA | Visual field test | |||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean ± SD | p value | N | Mean ± SD | p value | LogMAR (mean ± SD) | p value | Mean deviation ± SD (dB) | |
| Preoperative | 76 | 14.7 ± 3.7 | – | 76 | 2.6 ± 1.5 | – | 0.36 ± 0.12 | – | −9.21 ± 7.71 |
| Postoperative day 1 | 76 | 11.2 ± 4.1 | <0.00010 | 76 | 0 | – | – | – | – |
| 1 month | 74 | 14.9 ± 5.0 (range:6–36) | 0.83 | 74 | 0.17 ± 0.74 | <0.00010 | 0.21 ± 0.33 | <0.00010 | – |
| 3 months | 71 | 13.3 ± 3.2 | 0.0022 | 71 | 0.63 ± 1.2 | <0.00010 | 0.18 ± 0.39 | <0.00010 | – |
| 6 months | 76 | 13.9 ± 4.3 | 0.25 | 76 | 0.72 ± 1.4 | <0.00010 | 0.17 ± 0.38 | <0.00010 | −9.11 ± 8.16 (p = 0.22) |
BCVA, best-corrected visual acuity; IOP, intraocular pressure; n, number of patients; SD, standard deviation.
The subgroup analysis is presented in Table 3. Patients were stratified into mild, moderate, or advance glaucoma according to the Hodapp–Parrish–Anderson criteria. The mild glaucoma group (n = 32) had a baseline mean IOP of 15.8 ± 3.9 mmHg on 2.3 ± 1.4 medications. The average mean deviation on VF was −3.1 ± 1.6 dB. The moderate glaucoma group (n = 24) had a mean IOP of 13.8 ± 2.7 mmHg on 2.6 ± 1.5 medications. The average mean deviation on VF was −9.2 ± 2.1 dB. There were a total of 20 patients with advanced glaucoma. The average mean deviation on VF for this group was −20.3 ± 5.5 dB with a mean IOP of 14.4 ± 3.8 mmHg on 3.1 ± 1.6 medications.
Table 3.
Intraocular pressure and number of medications at preoperative visit and follow-up times for patients with mild, moderate, and advance glaucoma who underwent phacoemulsification cataract surgery and Hydrus microstent.
| Mild/early glaucoma | Moderate glaucoma | Advance glaucoma | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | IOP (mean ± SD; mmHg) | Number of Medications (mean ± SD) | N | IOP (mean ± SD; mmHg) | Number of Medications (mean ± SD) | N | IOP (mean ± SD; mmHg) | MEDS (mean ± SD) | |
| Preoperative | 32 | 15.8 ± 3.9 | 2.3 ± 1.4 | 24 | 13.8 ± 2.7 | 2.6 ± 1.5 | 20 | 14.4 ± 3.8 | 3.1 ± 1.6 |
| Postoperative day 1 | 32 | 11.4 ± 4.0 | 0 | 24 | 11.5 ± 5.1 | 0 | 20 | 10.6 ± 3.1 | 0 |
| 1 month | 32 | 15.3 ± 5.7 | 0.13 ± 0.71 | 22 | 13.8 ± 3.5 | 0.13 ± 0.61 | 18 | 15.2 ± 5.5 | 0.15 ± 0.67 |
| 3 months | 30 | 13.6 ± 3.6 | 0.23 ± 0.77 | 23 | 13.0 ± 2.6 | 0.74 ± 1.1 | 18 | 12.7 ± 2.7 | 1.0 ± 1.3 |
| 6 months | 32 | 14.0 ± 2.9 | 0.44 ± 1.1 | 24 | 12.9 ± 2.8 | 0.58 ± 0.97 | 20 | 13.9 ± 3.9 | 1.1 ± 1.4 |
IOP, intraocular pressure; SD, standard deviation.
Patients with mild glaucoma had the most reduction in the number of medications (1 month 94.3%, 3 months 90%, and 6 months 80.9%). The mean IOP decreased by 27.8% at postoperative day 1, 3.2% at 1 month, 13.9% at 3 months, and 11.4% at 6 months. The moderate group saw a reduction in the number of medications: 95% at 1 month, 71.5% at 3 months, and 77.7% at 6 months. Patients in this group saw a 16.7% reduction in IOP at postoperative day 1 with a return to baseline mean IOP at 1 month, 5.8% drop at 3 months, and 6.5% drop at 6 months. The advance glaucoma group had the least reduction in number of medications at 3 months (67.7%) and 6 months (64.5%). The mean IOP saw a 26.4% reduction at postoperative day 1, a decrease of 11.8% at 3 months, and 3.5% at 6 months (Table 3).
The number of all patients on no medications increased from 2.6% at baseline to 72.4% at 6 months (mild 79.4%, moderate 70.8%, and advance 50.0%; Table 4).
Table 4.
Number of patients medication free at preoperative visit and follow-up times after phacoemulsification cataract surgery and Hydrus stent.
| Baseline | 1 month | 3 months | 6 months | |
|---|---|---|---|---|
| All patients | 2 (2.6%) | 73 (96.1%) | 54 (76.1%) | 55 (72.4%) |
| Mild glaucoma | 2 (5.0%) | 31 (96.9%) | 27 (90.0%) | 27 (84.4%) |
| Moderate glaucoma | 0 (0%) | 21 (95.5%) | 15 (65.2%) | 17 (70.8%) |
| Advance glaucoma | 0 (0%) | 19 (95.0%) | 10 (55.6%) | 10 (50.0%) |
Adverse events were non-sight threatening and self-limited. Generally, only trace blood refluxed into the AC upon insertion of the Hydrus microstent and resolved spontaneously in all cases typically within the first postoperative week. Postoperatively, IOP spikes (IOP increase greater than 10 mmHg or IOP ⩾ 30 mmHg), mild posterior capsule opacification, hyphema, iris adhesion/block, peripheral anterior synechiae, transient corneal edema, cystoid macular edema (CME), device malposition, and obstruction were noted. No adverse events required secondary interventions (Table 5).
Table 5.
Complications/adverse effects of Hydrus microstent MIGS.
| Adverse effect | Number | Percent |
|---|---|---|
| Intraocular pressure spike | 6 | 7.9 |
| Corneal edema | 6 | 7.9 |
| Hyphema | 1 | 1.3 |
| Device obstruction | 1 | 1.3 |
| Iris adhesion/block | 2 | 2.6 |
| Grade 1 cells in AC | 1 | 1.3 |
| Cystoid macular edema | 2 | 2.6 |
| Device malposition | 1 | 1.3 |
| Secondary cataract | 1 | 1.3 |
| Iridodialysis | 1 | 1.3 |
| Residual Healon | 1 | 1.3 |
| Device in supraciliary space | 1 | 1.3 |
| PAS, others | 0 | 0 |
AC, anterior chamber; MIGS, microinvasive glaucoma surgery; PAS, peripheral anterior synechiae.
Discussion
Elevation in IOP is often associated with the progression of glaucoma. Aggressive control of IOP has been suggested for the control of VF progression.22 The increasing costs of medications, lack of access globally, nonadherence to ocular medications, and the emergence of MIGS make Hydrus microstent study particularly important. Our study patients, Blacks and Afro-Latinx, have a higher rate of blindness from glaucoma compared with White Latinx and White persons.23 In addition, the literature on MIGS in predominantly Black population is limited with major studies like the COMPARE trial and the HORIZON including only 1.3% and 8%–12.2%, respectively (participant of European descent 65.3% and 78.9%–81.8%, respectively).19,21 Our study looks at a reported efficacious MIGS in a population with the highest prevalence of glaucoma and blindness.
This retrospective noncomparative study demonstrated the efficacy of Hydrus microstent in significantly reducing medication burden while maintaining lower IOP during a 6-month period in Blacks and Afro-Latinx with glaucoma. The greatest reduction in medication burden was seen in mild glaucoma patients, with 79.4% of patients medication free. The advance glaucoma patients were able to maintain lower IOPs (8–14 mmHg) on less medication at 6 months (64.5% decrease in the number of medications, 50% medication free) without any sight-threatening complications. The Hydrus microstent facilitates aqueous outflow through a dilated Schlemm canal and open unobstructed collecting channels without damaging the TM.24,25 The Hydrus is 8 mm in length and spans 3 clock hours. Schlemm canal MIGS like Hydrus is subject to the IOP floor created by resistance distal to the Schlemm canal. Although the presence of the IOP floor prevents hypotony, it creates a threshold for IOP reduction after intervention.26 In our study, the mean preoperative IOP was 14.7 ± 3.7 mmHg. After 6 months of follow-up, the mean was 13.9 ± 4.3 mmHg (p = 0.25). In this real-world retrospective study, we noticed an insignificantly lesser change in IOP (in all subgroups) compared with the HORIZON study because we did not do a medication washout. However, the number of medications decreased significantly (p < 0.0010). Fea and colleagues demonstrated similar efficacy in a multicenter study of 67 patients with primary open-angle glaucoma patients who underwent phacoemulsification and Hydrus microstent insertion. At the 2-year follow-up, 64% of the patients were medication free with a mean IOP of 15.5 mmHg (−19% change from the baseline).27
Recently, Rhee and colleagues presented a 4-year follow-up data from the HORIZON study. They showed that 65% of the Hydrus patients were medication free at 4 years compared with 41% in the control group (p < 0.001). Mean unmedicated IOP in the Hydrus group was 16.7 mmHg (baseline medicated IOP = 17.9 mmHg) and 17.2 mmHg in the control group (baseline medicated IOP = 18.1 mmHg). There was a significant reduction in risk of surgical events in the Hydrus group (log rank p = 0.015) and lower probability of event (2.1% in the Hydrus group, 6% in controls, hazard ratio = 0.289, 95% CI: 0.106–0.836, p = 0.022). They did not notice any significant increase in endothelial cell loss after the 3-month follow-up. Hydrus microstent has long-term efficacy without sight-threatening effects.
Our study shows the efficacy of cataract surgery and Hydrus microstent in Black and Afro-Latinx patients with mild, moderate, and advance glaucoma. The effect was greatest among mild glaucoma patients compared with advance glaucoma patients. All the patients were able to achieve their IOP target goals on either no medication or less medication. No additional surgeries were required. In patients with angle closure, cataract surgery can allow greater access to the TM with removal of the massive natural lens. Residual peripheral anterior synechia can be gently removed with a cyclodialysis spatula for 1–2 clock hours to allow insertion of the Hydrus stent. Also, in chronic angle-closure patients, we hypothesize that cataract surgery contributes to the reduction in medication burden. In patients with advance glaucoma, there could be preexisting distal damage to collector channels and aqueous veins that lead to the requirement of additional medical therapy.
The complications of Hydrus microstent insertion in this study included transient hyphema, peripheral anterior synechiae, device malposition, device obstruction, transient IOP spike, and secondary surgical interventions.19,21,24,28,29 In this study, the most reported complications of the Hydrus microstent were transient IOP spikes and transient corneal edema (Table 5). The corneal edema was as a result of phacoemulsification of hard cataract lenses and they all resolved.
Study limitations
Limitations of the study include its nonrandomized nature, small sample size, and limited follow-up period. Nonetheless, the study provides real-world evidence of the efficacy and complications of the Hydrus microstent in Black and Afro-Latinx patients with glaucoma.
Conclusion
The Hydrus microstent implantation and phacoemulsification cataract surgery demonstrated a significant decrease in ocular hypotension medication in Black and Afro-Latinx patients with mild, moderate, and advanced glaucoma. The procedure has an excellent safety profile similar to other MIGS devices. Further long-term studies are needed to confirm the efficacy and safety seen in our study.
Acknowledgments
The authors thank Louis R. Pasquale MD for his editorial assistance and Harriet Lloyd from the Einhorn Clinical Research Center at New York Eye and Ear Infirmary of Mount Sinai for administrative support. Finally, the authors thank the staff at Advance Eye Care of New York for their assistance and support.
Footnotes
Authorship: All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: D.L. declares being a consultant to Aerie, Bausch Health and Ivantis. G.N. and C.N. report no disclosure.
Data availability: The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
ORCID iD: Gideon Nkrumah  https://orcid.org/0000-0003-1855-4610
https://orcid.org/0000-0003-1855-4610
Contributor Information
Daniel Laroche, Advanced Eyecare of New York, 49 West 127th Street, New York, NY 10027, USA; Department of Ophthalmology, New York Eye and Ear Infirmary, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Gideon Nkrumah, School of Medicine, University of Pittsburgh, Pittsburgh, PA, USA; Advanced Eyecare of New York, New York, NY, USA.
Chester Ng, Advanced Eyecare of New York, New York, NY, USA.
References
- 1. Klein R, Klein BE. The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci 2013; 54: ORSF5–ORSF13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014; 121: 2081–2090. [DOI] [PubMed] [Google Scholar]
- 3. Schein OD, Cassard SD, Tielsch JM, et al. Cataract surgery among Medicare beneficiaries. Ophthalmic Epidemiol 2012; 19: 257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Racette L, Wilson MR, Zangwill LM, et al. Primary open-angle glaucoma in blacks: a review. Surv Ophthalmol 2003; 48: 295–313. [DOI] [PubMed] [Google Scholar]
- 5. Mansberger SL, Gordon MO, Jampel H, et al. Reduction in intraocular pressure after cataract extraction: the Ocular Hypertension Treatment Study. Ophthalmology 2012; 119: 1826–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bron AJ, Vrensen GF, Koretz J, et al. The ageing lens. Ophthalmologica 2000; 214: 86–104. [DOI] [PubMed] [Google Scholar]
- 7. Chen Z, Sun J, Li M, et al. Effect of age on the morphologies of the human Schlemm’s canal and trabecular meshwork measured with swept-source optical coherence tomography. Eye 2018; 32: 1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moroi SE, Lark KK, Sieving PA, et al. Long anterior zonules and pigment dispersion. Am J Ophthalmol 2003; 136: 1176–1178. [DOI] [PubMed] [Google Scholar]
- 9. Sitoula RP, Sarkar I, Nayak D, et al. Lens induced glaucoma: an experience in tertiary eye care center in eastern Nepal. Nepal J Ophthalmol 2016; 8: 161–166. [DOI] [PubMed] [Google Scholar]
- 10. Tsai T, Robin AL, Smith JP., 3rd An evaluation of how glaucoma patients use topical medications: a pilot study. Trans Am Ophthalmol Soc 2007; 105: 29–33; discussion 33–35. [PMC free article] [PubMed] [Google Scholar]
- 11. Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology 2009; 116: 191–199. [DOI] [PubMed] [Google Scholar]
- 12. Leahy KE, White AJ. Selective laser trabeculoplasty: current perspectives. Clin Ophthalmol 2015; 9: 833–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gedde SJ, Heuer DK, Parrish RK, 2nd, et al. Review of results from the Tube Versus Trabeculectomy Study. Curr Opin Ophthalmol 2010; 21: 123–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Qassim A, Walland MJ, Landers J, et al. Effect of phacoemulsification cataract surgery on intraocular pressure in early glaucoma: a prospective multi-site study. Clin Exp Ophthalmol 2020; 48: 442–449. [DOI] [PubMed] [Google Scholar]
- 15. Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the Kahook Dual Blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma 2018; 27: 849–855. [DOI] [PubMed] [Google Scholar]
- 16. Le JT, Bicket AK, Wang L, et al. Ab interno trabecular bypass surgery with iStent for open-angle glaucoma. Cochrane Database Syst Rev 2019; 3: CD012743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Malvankar-Mehta MS, Iordanous Y, Chen YN, et al. iStent with phacoemulsification versus phacoemulsification alone for patients with glaucoma and cataract: a meta-analysis. PLoS ONE 2015; 10: e0131770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Samet S, Ong JA, Ahmed IIK. Hydrus microstent implantation for surgical management of glaucoma: a review of design, efficacy and safety. Eye Vis 2019; 6: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Samuelson TW, Chang DF, Marquis R, et al. A Schlemm canal microstent for intraocular pressure reduction in primary open-angle glaucoma and cataract: the HORIZON study. Ophthalmology 2019; 126: 29–37. [DOI] [PubMed] [Google Scholar]
- 20. Jones J, Koch DD, Vold S, et al. Results from the United States cohort of the HORIZON trial of a Schlemm canal microstent to reduce intraocular pressure in primary open-angle glaucoma. J Cataract Refract Surg 2019; 45: 1305–1315. [DOI] [PubMed] [Google Scholar]
- 21. Ahmed IIK, Fea A, Au L, et al. A prospective randomized trial comparing Hydrus and iStent microinvasive glaucoma surgery implants for standalone treatment of open-angle glaucoma: the COMPARE study. Ophthalmology 2020; 127: 52–61. [DOI] [PubMed] [Google Scholar]
- 22. Musch DC, Gillespie BW, Niziol LM, et al. Intraocular pressure control and long-term visual field loss in the Collaborative Initial Glaucoma Treatment Study. Ophthalmology 2011; 118: 1766–1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ophthalmology AAO. US eye disease statistics. AAO, https://www.aao.org/eye-disease-statistics (accessed 16 February 2020).
- 24. Fea AM, Ahmed II, Lavia C, et al. Hydrus microstent compared to selective laser trabeculoplasty in primary open angle glaucoma: one year results. Clin Exp Ophthalmol 2017; 45: 120–127. [DOI] [PubMed] [Google Scholar]
- 25. Camras LJ, Yuan F, Fan S, et al. A novel Schlemm’s canal scaffold increases outflow facility in a human anterior segment perfusion model. Invest Ophthalmol Vis Sci 2012; 53: 6115–6121. [DOI] [PubMed] [Google Scholar]
- 26. Shah M. Micro-invasive glaucoma surgery – an interventional glaucoma revolution. Eye Vis 2019; 6: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fea AM, Rekas M, Au L. Evaluation of a Schlemm canal scaffold microstent combined with phacoemulsification in routine clinical practice: two-year multicenter study. J Cataract Refract Surg 2017; 43: 886–891. [DOI] [PubMed] [Google Scholar]
- 28. Gandolfi SA, Ungaro N, Ghirardini S, et al. Comparison of surgical outcomes between canaloplasty and Schlemm’s canal scaffold at 24 months’ follow-up. J Ophthalmol 2016; 2016: 3410469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pfeiffer N, Garcia-Feijoo J, Martinez-de-la-Casa JM, et al. A randomized trial of a Schlemm’s canal microstent with phacoemulsification for reducing intraocular pressure in open-angle glaucoma. Ophthalmology 2015; 122: 1283–1293. [DOI] [PubMed] [Google Scholar]


