Abstract
This study aimed to measure the magnitude of education-related inequalities in the use of dental services among older adults (aged 50 y or older) from a sizable multicountry sample of 23 upper-middle- and high-income countries. This study used cross-sectional data from nationally representative surveys of people aged 50 y and over. Countries included in the Health and Retirement Study surveys were the following: Brazil, China, South Korea, Mexico, United States, Austria, Belgium, Croatia, Czech Republic, Denmark, Estonia, France, Germany, Greece, Italy, Israel, Luxembourg, Poland, Portugal, Slovenia, Spain, Sweden, and Switzerland. The dependent variable was the use of dental services, based on the self-report of having had a dental visit within the previous year, except for the United States and South Korea, which used 2-y recall periods. Educational level was used as the measure of socioeconomic position and was standardized across countries. Multivariate logistic regression modeling was used to evaluate the factors associated with the use of dental services, and the magnitude of education inequalities in the use of dental services was assessed using the slope index of inequality (SII) to measure absolute inequalities and the relative index of inequality for relative inequalities. The pooled prevalence of the use of dental services was 31.7% and ranged from 18.7% in China to 81.2% in Sweden. In the overall sample, the absolute difference in the prevalence of use between the lowest and highest educational groups was 20 percentage points. SII was significant for all countries except Portugal. Relative educational inequalities were significant for all countries and ranged from 3.2 in Poland to 1.2 in Sweden. There were significant education-related inequalities in the use of dental care by older adults in all countries. Monitoring these inequalities is critical to the planning and delivery of dental services.
Keywords: oral health, dental care, health services for the aged, health care disparities, socioeconomic factors, epidemiology
Introduction
Dental care is essential to good oral health, which is a fundamental component of general health and well-being (Peres et al. 2019). Long-term routine dental attendance is associated with lower dental caries experience and fewer missing teeth and better self-rated oral health (Thomson et al. 2010). Dental care is especially critical among older adults, as tooth loss is the leading global cause of disability-adjusted life years in individuals aged 60 y and over (Marcenes et al. 2013). Although this age group has the highest need for dental care (Petersen et al. 2010), these individuals have the lowest frequency of use of dental services (Peres et al. 2019). Internationally, the average prevalence of any dental service utilization is about 54% (Reda et al. 2018). Still, among older adults, it ranges from 18.1% in China (Li et al. 2018) to 81.5% in Sweden (Listl 2011). Different barriers to use have been examined, such as disabilities (Horner-Johnson et al. 2015; Watt et al. 2019) and socioeconomic factors (Palència et al. 2014; Monteiro et al. 2016; Organization for Economic Cooperation and Development [OECD] 2019), with the latter considered the most important (Monteiro et al. 2016; Vujicic et al. 2016).
Despite worldwide commitments to achieving the Sustainable Development Goals, many national plans for achieving universal health coverage do not explicitly mention access to dental care (Global Health Observatory 2020). Such attention is warranted, however, due to evidence of low levels of access to dental care in most low- and middle-income countries and even some high-income countries. Moreover, there are considerable socioeconomic inequalities in access to and use of dental care (OECD 2019; Peres et al. 2019) that are usually significantly greater in magnitude than inequalities in access to general health services (OECD 2019).
Reducing socioeconomic inequalities in the use of dental care services may have a significant impact on reducing inequalities in oral health (Shen and Listl 2018). Monitoring health inequalities is critical to implement public policies aimed at social justice (Li et al. 2018). Moreover, a comparison among countries offers insights into the extent to which socioeconomic, cultural, and institutional aspects affect the utilization of services (Listl et al. 2012; Reda et al. 2018).
Although previous studies have evaluated income-related inequalities in the use of dental services among older adults, most current cross-national evidence is primarily from high-income European countries (Listl 2011; Listl et al. 2012; Palència et al. 2014). Moreover, these findings, albeit important, explain only part of the socioeconomic inequalities observed, because monetary measures of socioeconomic position (SEP), such as income, do not capture all of the diverse aspects of well-being in low-income countries (Howe et al. 2008).
Educational attainment has been identified as one of the most powerful fundamental causes of health inequalities because it is generally established relatively early in life and therefore captures an individual’s knowledge-related assets and socioeconomic position throughout the life course. Education is associated with social opportunities that individuals may have during their lifetime, and it influences both their likelihood of employment and their income level. Education also acts intergenerationally, whereby parents’ education may affect the choices they make for their children, which, in turn, may affect their socioeconomic circumstances in adulthood (Galobardes et al. 2007). Concerning oral health, education is thought to influence the way individuals achieve and maintain oral health through the perception of the need for routine dental services and knowledge on best practices for oral health prevention (Shen and Listl 2018). Thus, it was hypothesized that the use of dental services is associated with education independent of other socioeconomic and general health characteristics. This study aimed to measure the magnitude of education-related inequalities in the use of dental services among older adults (aged 50 y or older) in a sample of 23 upper-middle- and high-income countries.
Methods
This study used cross-sectional data from nationally representative surveys of people aged 50 y and over belonging to the Health and Retirement Study (HRS) family surveys. All analyses included the most recent waves of each study that included information on the use of dental services. The surveys were conducted between 2014 and 2016 in Brazil (Brazilian Longitudinal Study of Aging [ELSI-Brazil]; Lima-Costa et al. 2018), China (Chinese Health and Retirement Longitudinal Study [CHARLS]; Zhao et al. 2014), Korea (Korean Longitudinal Study of Aging [KLoSA]; Korea Employment Information Service: KEIS 2018), Mexico (Mexican Health and Aging Study; Wong et al. 2017), continental European countries and Israel (Survey of Health and Ageing and Retirement in Europe [SHARE]; Börsch-Supan et al. 2013), and the United States (HRS; Sonnega et al. 2014). European countries included in the SHARE survey were Austria, Belgium, Croatia, Czech Republic, Denmark, Estonia, France, Germany, Greece, Italy, Luxembourg, Poland, Portugal, Slovenia, Spain, Sweden, and Switzerland. The Gateway to Global Aging Data provided all data, except for ELSI-Brazil. The platform was designed to facilitate the use of harmonized data from these studies (https://g2aging.org/). Although the Brazilian survey was not included in the Gateway, it was planned with a similar framework and protocol, thus allowing comparisons with the other studies. All surveys were approved by an institutional review board, and written informed consent was granted by all participants.
The present study included information on individuals 50 y and older from 23 countries with complete information for all variables of interest (n = 124,021).
Outcome
The use of dental services was measured based on the self-report of having had a dental visit within the previous year in all countries, except for the United States and South Korea, which used 2-y recall periods.
Covariates
Educational level was used as the measure of SEP both because it represents a fundamental cause of health inequalities and because alternative measures of SEP, such as income, may fail to capture the diverse aspects of well-being outside of high-income country contexts (Howe et al. 2008). The International Standard Classification of Education was used to standardize the educational level across countries. Education was categorized into low educational level (less than upper secondary education), middle educational level (upper secondary education and vocational training), and high educational level (tertiary education) (United Nations Educational, Scientific and Cultural Organization Institute for Statistics 2006).
Other covariates included in the analyses were sex (male, female), age group (50 to 59, 60 to 69, 70 to 79, 80+), marital status (single, partnered), any disabilities in basic activities of daily living (BADLs) (no, yes), any chronic disease (no, yes), residence (rural, urban), and private health insurance (no, yes). BADL disabilities were considered as the report of any difficulty in performing at least 1 of the following 6 activities: dressing, eating, bathing, toileting, walking across a room, and getting in/up from the bed. Chronic conditions included hypertension, diabetes, cancer, chronic lung disease (emphysema/bronchitis/chronic obstructive pulmonary disease), heart disease, stroke, and arthritis.
Statistical Analyses
Analyses were conducted for each country, and then data were pooled to generate estimates for the overall sample. First, descriptive analyses were completed for all variables, and then the frequency of use of dental services was estimated by educational level. The association between the use of dental services and independent variables for the overall sample was performed using multivariate logistic regression with findings reported using odds ratios (ORs) and the respective 95% confidence interval (CI). The magnitude of education inequalities in the use of dental services was evaluated using the slope index of inequality (SII) to measure absolute inequalities and the relative index of inequality (RII) for relative inequalities. The SII is interpreted as the absolute difference in the probability of use of dental services between the top and bottom educational groups, and RII is the relative educational difference between these probabilities. The SII and RII indices were obtained by regressing the dependent variable on the relative rank of education within each country. This rank was created by taking the midpoint of the range in the cumulative distribution at each level of education with the lowest educational level classified as 0 and the highest as 1. SII and RII values above 0 and 1, respectively, indicate that the prevalence of use was higher among individuals in the highest level of educational attainment (Mackenbach et al. 2008). To control for differences in individual-level risk factors that may vary by country, the SII and RII were then adjusted by all covariates and estimated using weighted logistic regression models (Barros and Victora 2013). A quadrant graph was used to compare the SII/RII for each country with the overall prevalence of dental services and overall SII/RII. The quadrants represent high/low SII/RII and high/low prevalence of dental service utilization. Survey sample weights were used in the analyses, which were performed using the survey mode in Stata SE 14.0 (StataCorp LP).
Results
The mean age was relatively homogeneous across countries and was 64.5 y in the pooled analysis; the female sex was more frequent in all countries. Individuals in the lowest and highest educational levels represented 66.1% and 9.9% in the overall sample, with individuals in the lowest educational level ranging from 13.2% in the United States to 85.5% in China. The highest educational level ranged from 2.7% in China to 42.8% in Denmark. The pooled prevalence of the use of dental services was 31.7% and ranged from 18.7% in China to 81.2% in Sweden (Table 1). The distribution of the sample, according to other covariates, is presented in Appendix Table 1.
Table 1.
Proportion of Older Adults Having Used Dental Care in the Previous Year, Sex and Educational Level.
| Sex | Educational Level | Dental Care | |||
|---|---|---|---|---|---|
| Male | Female | Low | High | All | |
| Country | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| Austria | 45.9 (43.6–48.1) | 54.1 (51.9–56.4) | 23.3 (21.6–25.1) | 25.0 (23.1–27.0) | 58.3 (56.1–60.5) |
| Belgium | 47.0 (45.3–48.8) | 53.0 (51.2–54.7) | 37.5 (35.9–39.2) | 34.1 (32.4–35.8) | 56.5 (54.8–58.2) |
| Brazil | 46.1 (44.9–47.4) | 53.9 (52.6–55.1) | 73.0 (71.9–74.1) | 8.3 (7.6–9.0) | 32.7 (31.5–33.9) |
| China | 48.7 (47.5–49.8) | 51.3 (50.2–52.5) | 85.5 (84.4–86.4) | 2.7 (2.3–3.2) | 18.7 (17.8–19.6) |
| Croatia | 44.6 (42.5–46.8) | 55.4 (53.2–57.5) | 61.2 (59.1–63.3) | 14.7 (13.2–16.2) | 31.9 (29.9–34.0) |
| Czech Republic | 45.5 (42.5–48.6) | 54.5 (51.4–57.5) | 36.6 (33.8–39.4) | 13.3 (11.6–15.3) | 64.0 (61.0–66.9) |
| Denmark | 47.8 (46.0–49.5) | 52.2 (50.5–54.0) | 18.5 (17.1–19.8) | 42.8 (41.1–44.5) | 81.9 (80.6–83.3) |
| Estonia | 39.4 (37.9–40.9) | 60.6 (59.1–62.1) | 25.9 (24.6–27.2) | 21.5 (20.3–22.8) | 37.4 (35.9–38.9) |
| France | 45.7 (43.9–47.6) | 54.3 (52.4–56.1) | 37.7 (36.0–39.4) | 23.9 (22.4–25.6) | 50.7 (48.9–52.5) |
| Germany | 46.2 (44.5–47.9) | 53.8 (52.1–55.5) | 13.7 (12.5–15.0) | 29.4 (27.9–30.9) | 77.0 (75.5–78.5) |
| Greece | 46.4 (44.8–47.9) | 53.6 (52.1–55.2) | 52.3 (50.8–53.8) | 20.8 (19.6–22.1) | 31.5 (30.1–33.0) |
| Israel | 46.0 (41.8–50.4) | 54.0 (49.6–58.2) | 34.5 (30.5–38.8) | 35.1 (31.2–39.2) | 30.7 (27.3–34.3) |
| Italy | 45.6 (43.8–47.4) | 54.4 (52.6–56.2) | 68.2 (66.5–69.9) | 7.5 (6.6–8.5) | 31.3 (29.6–32.9) |
| Luxembourg | 47.7 (44.6–50.9) | 52.3 (49.1–55.4) | 44.2 (41.1–47.4) | 21.8 (19.2–24.7) | 71.3 (68.4–74.1) |
| Mexico | 44.4 (42.6–46.2) | 55.6 (53.8–57.4) | 67.0 (65.2–68.8) | 10.6 (9.4–11.9) | 36.7 (34.9–38.5) |
| Poland | 44.2 (41.3–47.1) | 55.8 (52.9–58.7) | 32.4 (29.9–35.1) | 10.5 (8.8–12.5) | 27.8 (25.2–30.5) |
| Portugal | 44.9 (39.5–50.5) | 55.1 (49.5–60.5) | 78.5 (72.7–83.3) | 8.6 (6.0–12.2) | 37.2 (32.0–42.7) |
| Slovenia | 46.2 (44.3–48.1) | 53.8 (51.9–55.7) | 32.6 (30.9–34.4) | 16.9 (15.5–18.4) | 44.5 (42.6–46.4) |
| South Koreaa | 45.9 (44.5–47.3) | 54.1 (52.7–55.5) | 51.2 (49.7–52.6) | 12.4 (11.3–13.5) | 23.0 (21.8–24.2) |
| Spain | 46.4 (43.4–49.5) | 53.6 (50.5–56.6) | 76.1 (73.2–78.8) | 11.3 (9.4–13.5) | 26.9 (24.2–29.8) |
| Sweden | 47.2 (45.2–49.3) | 52.8 (50.7–54.8) | 33.2 (31.3–35.0) | 31.7 (29.7–33.7) | 81.2 (79.5–82.8) |
| Switzerland | 46.6 (44.4–48.7) | 53.4 (51.3–55.6) | 18.8 (17.2–20.4) | 16.5 (14.9–18.1) | 75.6 (73.7–77.4) |
| United Statesa | 45.8 (44.9–46.8) | 54.2 (53.2–55.1) | 13.2 (12.6–13.8) | 28.8 (27.9–29.8) | 66.2 (65.3–67.1) |
| Total (overall) | 47.5 (46.8–48.3) | 52.5 (51.7–53.2) | 66.1 (65.4–66.7) | 9.9 (9.6–10.3) | 31.7 (31.1–32.4) |
Low education = less than secondary education; Middle = secondary level complete (or vocational schooling); High = tertiary education and higher.
Use of dental services in the past 2 y.
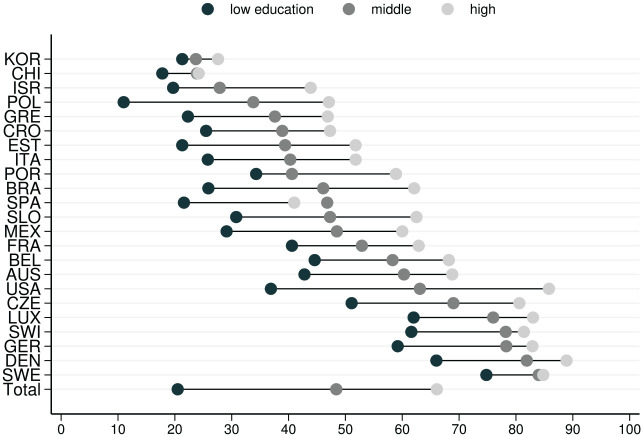
Figure 1 presents the prevalence of the use of dental services by educational level. In this figure, Poland had the lowest prevalence for the lowest educational category, and Sweden had the highest prevalence for the lowest educational category. The United States had the largest gap between educational strata, whereas Sweden, China, and Korea had the smallest educational gap.
Figure 1.
Proportion of older adults having used dental services in the previous year by educational level. Low education = less than secondary education; middle = secondary level complete (or vocational schooling); high = tertiary education and higher.
All covariates were associated with the use of dental services in the adjusted model (Table 2). The odds of having used dental services were higher among individuals with greater educational attainment. Individuals from the middle and high educational attainment levels had, respectively, 3.5 and 5.6 times higher odds of having used dental services than their counterparts with low education. The reports of any chronic disease or having private health insurance were positively associated with the use of dental services. Individuals reporting BADL limitations had 13% (OR, 0.87; 95% CI, 0.80–0.96) lower odds of dental service use than those without limitations.
Table 2.
Unadjusted and Adjusted Analyses of Factors Associated with the Use of Dental Services by Older Adults. Pooled Analysis, 23 Countries, Circa 2015.
| Recent Dental Visit | ||
|---|---|---|
| Characteristic | OR Unadjusted (95% CI) | OR Adjusted (95% CI) |
| Educational attainment | ||
| Low | 1.00 | 1.00 |
| Middle | 3.64 (3.38–3.92) | 3.05 (2.81–3.32) |
| High | 7.58 (6.88–8.35) | 5.61 (5.03–6.27) |
| Age | ||
| 50 to 59 | 1.00 | 1.00 |
| 60 to 69 | 1.10 (1.03–1.18) | 1.3 (1.20–1.41) |
| 70 to 79 | 1.05 (0.96–1.14) | 1.25 (1.13–1.38) |
| 80+ | 0.79 (0.70–0.89) | 0.91 (0.78–1.06) |
| Sex | ||
| Female | 1.00 | 1.00 |
| Male | 0.86 (0.81–0.91) | 0.74 (0.69–0.79) |
| BADL limitations | ||
| No | 1.00 | 1.00 |
| Yes | 0.67 (0.62–0.73) | 0.87 (0.80–0.96) |
| Any chronic condition | ||
| No | 1.00 | 1.00 |
| Yes | 1.18 (1.10–1.27) | 1.25 (1.15–1.35) |
| Locale of residence | ||
| Urban | 1.00 | 1.00 |
| Rural | 0.57 (0.54–0.61) | 0.85 (0.79–0.9) |
| Private health insurance | ||
| No | 1.00 | 1.00 |
| Yes | 4.15 (3.82–4.51) | 2.37 (2.18–2.57) |
BADL, basic activity of daily living; OR, odds ratio.
Positive absolute inequalities (SII) affected all countries, except Portugal, indicating that the use of dental services was greater in the highest education rank. In the overall sample, the absolute difference between the lowest and highest educational groups was 20 percentage points. The lowest SII was found in Korea (9 percentage point difference), followed by China (11 percentage point difference) and Sweden (13 percentage point difference). The highest absolute difference was in the United States (50 percentage point difference), followed by Brazil (34 percentage point difference) and the Czech Republic and Slovenia with the same SII (32 percentage point difference). Relative educational inequalities were significant for all countries and pointed in the same direction as absolute inequalities, suggesting that the better-off educational strata had more access to dental services. In the pooled analysis, the RII was 1.9 and ranged from 3.2 in Poland to 1.2 in Sweden (Table 3).
Table 3.
Adjusted RII and SII by Country.
| Country | SII | 95% CI | RII | 95% CI |
|---|---|---|---|---|
| Austria | 0.26 | 0.18 to 0.35 | 1.59 | 1.35 to 1.84 |
| Belgium | 0.27 | 0.21 to 0.33 | 1.64 | 1.44 to 1.84 |
| Brazil | 0.34 | 0.29 to 0.39 | 2.99 | 2.48 to 3.51 |
| China | 0.11 | 0.05 to 0.16 | 1.76 | 1.21 to 2.31 |
| Croatia | 0.23 | 0.16 to 0.31 | 2.14 | 1.59 to 2.68 |
| Czech Republic | 0.32 | 0.23 to 0.41 | 1.69 | 1.41 to 1.97 |
| Denmark | 0.19 | 0.14 to 0.24 | 1.27 | 1.18 to 1.35 |
| Estonia | 0.29 | 0.24 to 0.35 | 2.28 | 1.92 to 2.65 |
| France | 0.26 | 0.20 to 0.33 | 1.71 | 1.47 to 1.96 |
| Germany | 0.21 | 0.15 to 0.27 | 1.32 | 1.21 to 1.44 |
| Greece | 0.25 | 0.19 to 0.30 | 2.27 | 1.83 to 2.72 |
| Israel | 0.32 | 0.23 to 0.42 | 3.08 | 1.95 to 4.21 |
| Italy | 0.27 | 0.21 to 0.34 | 2.46 | 1.89 to 3.02 |
| Luxembourg | 0.19 | 0.07 to 0.30 | 1.31 | 1.09 to 1.53 |
| Mexico | 0.29 | 0.21 to 0.38 | 2.31 | 1.70 to 2.92 |
| Poland | 0.30 | 0.19 to 0.42 | 3.24 | 1.63 to 4.85 |
| Portugal | 0.19 | −0.07 to 0.45 | 1.7 | 0.48 to 2.92 |
| Slovenia | 0.32 | 0.25 to 0.39 | 2.14 | 1.76 to 2.51 |
| S. Korea | 0.09 | 0.03 to 0.14 | 1.47 | 1.12 to 1.82 |
| Spain | 0.28 | 0.16 to 0.40 | 2.91 | 1.46 to 4.36 |
| Sweden | 0.13 | 0.06 to 0.20 | 1.17 | 1.07 to 1.27 |
| Switzerland | 0.19 | 0.11 to 0.28 | 1.3 | 1.15 to 1.45 |
| United States | 0.50 | 0.47 to 0.53 | 2.31 | 2.16 to 2.46 |
| Total | 0.20 | 0.17 to 0.23 | 1.90 | 1.71 to 2.10 |
RII, relative index of inequality; SII, slope index of inequality.
Figure 2A and B displays the distribution of countries by inequalities indices (SII and RII) and the prevalence of dental service use. In Figure 2A, the countries with a higher prevalence concurrently with low absolute inequalities (SII) were Sweden, Denmark, Switzerland, and Luxemburg (first quadrant). The fourth quadrant includes China and Korea, which had the lowest ranks both in SII and prevalence of dental use. Three countries had a low prevalence of use of dental services and high SII (Poland, Spain, and Israel) (third quadrant). In the second quadrant, the United States had a high prevalence of the use of dental services concurrently with the highest SII among all countries.
Figure 2.
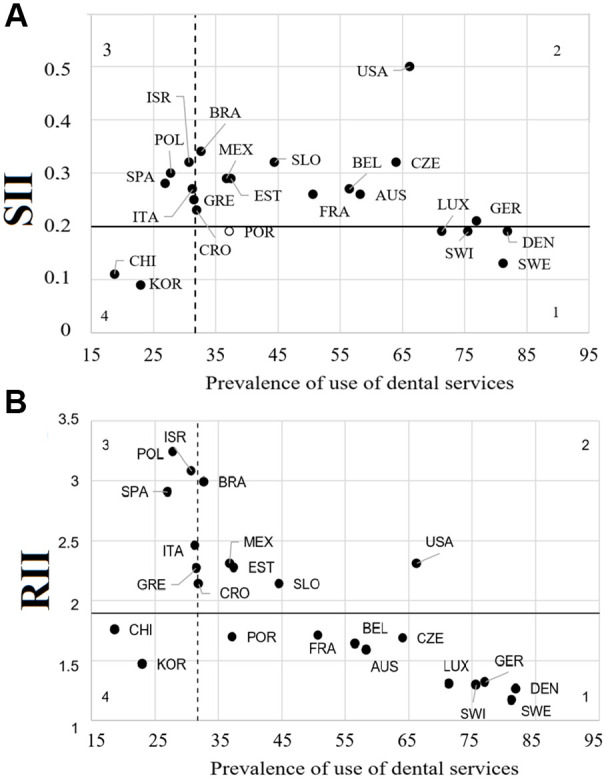
Distribution of countries by inequalities indices and the prevalence of dental service use. (A) Adjusted slope index of inequality (SII) compared to the prevalence of use of dental services and overall SII. (B) Adjusted relative index of inequality (RII) compared to the prevalence of use of dental services and overall RII. Dashed line = prevalence of recent dental visit in the pooled sample; black line = overall inequality index for the pooled sample; empty marker = country’s index is not statistically significant. Quadrant 1 = high prevalence of recent dental visit and low inequality; quadrant 2 = high prevalence of recent dental visit and high inequality; quadrant 3 = low prevalence of recent dental visit and high inequality; quadrant 4 = low prevalence of recent dental visit and low inequality.
In Figure 2B, the distribution of countries ran from the top left to the bottom right, suggesting a lower relative inequality in countries with a higher prevalence of dental care. The third and fourth quadrants included the same countries observed for the SII, meaning that China and Korea also had low RII and low prevalence of use. In contrast, Israel, Poland, and Spain had a low prevalence of dental use and a high RII. Brazil, Mexico, Estonia, Slovenia, and the United States had a higher prevalence of the use of dental services and higher RII than the overall sample. Italy, Greece, and Croatia had a high prevalence of use but almost the same RII as the total sample.
Discussion
This study is the first to address the magnitude of educational inequalities in the use of dental services among older adults living in high- and middle-income countries. Its most relevant findings are that absolute and relative educational inequalities in the use of dental services were significant in all countries except for Portugal (where the SII was not significant). Furthermore, the multiple regression model showed lower use of dental services among men, individuals affected by functional limitations, and those dwelling in rural areas. The assessment of both indices (SII and RII) was adjusted for these factors.
Fewer than one-third of individuals had a recent dental visit. This condition had a significant socioeconomic gradient, with the strata with lower educational attainment reaching an even lower prevalence of dental use, both on the absolute and relative scales. These findings support the recent call for ending the neglect of oral health worldwide that made dentistry a commodity, almost exclusively affordable to the wealthy (Watt et al. 2019).
This study underscores different pathways for overcoming financial barriers and achieving dental services. Access to health services is directly influenced by the perception of needs, which, in turn, is affected by the level of education (Andersen 1995). Accordingly, education increases health literacy by improving the understanding of diseases, treatment options, and preventive mechanisms (Shen and Listl 2018). A previous study observed that the level of education had a greater effect than purchasing power on oral health attitudes and behaviors in Brazil, including the use of dental services and tooth brushing (Bordin et al. 2017). Moreover, the level of education explained 9.2% of the overall wealth inequalities in dental care utilization in this country among older individuals (Bof de Andrade et al. 2017). In China, the proportion of income inequalities explained by education was 11.7% among individuals 45 y or older (Li et al. 2018).
Socioeconomic inequalities in oral health are mainstream in dental public health thinking (Peres et al. 2019; Watt et al. 2019). Education is a predisposing characteristic, distal in the conceptual framework explaining the utilization of health services (Babitsch et al. 2012; Okunseri et al. 2015). The educational attainment of individuals may affect their access to and use of dental services by influencing important sociocultural factors, such as the ability to pay and health-related beliefs and behaviors, which still need to be addressed further. Oral health status and the perceived need for dental services can also mediate the influence of education on health care use. Moreover, the organization of dental care (e.g., the number, location, and types of oral care providers in a country and whether there is public funding to these services) is also a critical source of potential mediating factors for the influence of education on dental care.
Countries with a strong welfare state and more redistributive policies, such as Denmark and Sweden (Listl et al. 2014), had lower absolute and relative educational inequalities in dental services. In contrast, more unequal countries, such as the United States and Brazil (Marmot 2018; Machado and Silva 2019), ranked among the highest in the SII and RII indices. Within-country inequalities in education were higher than between-country inequalities, thus highlighting the need to consider different contextual factors when planning actions to increase access to dental treatment in the local health care systems. Implementing potentially effective dental treatment may reduce the burden of oral diseases. However, it can also contribute to increasing the inequality in the distribution of disease, if the access is not immediate and effectively universal.
Implementing universal health coverage without taking into account the inverse care law (Hart 1971; Marmot 2018) raises the risk of increasing access and utilization only for the better-off social strata, who are generally those in lower need. Dental services need to remove education-based barriers to access, such as the perception of needs and cultural backgrounds, to make the services responsive to the population. In line with this argument, a previous study (Peres et al. 2012) observed that absolute inequalities in the use of dental care in the Brazilian public health system significantly reduced over a decade. However, the increase in use was higher among the wealthiest quintile of the population (35%), while the most deprived quintile had a lower increase (8%).
This study has some limitations. First, the absolute and relative indices of inequalities were not adjusted for clinical dental measures and oral health status because they were not available in all the surveys. However, the assessment was adjusted for several factors that influence the need for health care by older adults. Second, the use of dental services did not differentiate the intention of the visit (treatment or prevention). We hypothesize that the magnitude of indices assessing inequalities may rank even higher if exclusively preventive care were evaluated. Third, it is necessary to notice that the indices of inequalities are sensitive to the prevalence of the outcome (Houweling et al. 2007; World Health Organization 2013). Therefore, identifying which countries are in greater need of intervention demands a joint assessment of inequality indices and the prevalence of dental visits in each country. In particular, more attention should be given to Korea and China, which ranked the lowest in prevalence of dental visits, even though they also ranked low in SII and RII. Finally, the findings are based on cross-sectional data, which do not allow for causal inference. These points notwithstanding, education is expected to be an earlier event in the life course, thereby reducing the likelihood of reverse causality. Having used for the first time an extensive database with comprehensive information for a large number of countries with high- and middle-income economies, including 2 from Latin America, is the strength of this study.
In conclusion, absolute and relative education-related inequalities in the use of dental services were significant across all 23 countries analyzed. The continued monitoring of inequalities is essential to assess the level of achievement of universal health coverage. Older adults are a particular group to be targeted because their behaviors, attitudes, and oral health conditions may be critical indicators of how the health care systems have performed and what can be learned to improve oral health for future generations (Shen and Listl 2018).
Author Contributions
F. Bof de Andrade, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript; J.L.F. Antunes, contributed to conception, design, and data interpretation, drafted and critically revised the manuscript; F.C.D. Andrade, M.F.F. Lima-Costa, contributed to data interpretation, critically revised the manuscript; J. Macinko, contributed to conception, design, data acquisition, analysis, and interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, DS_10.1177_0022034520935854 for Education-Related Inequalities in Dental Services Use among Older Adults in 23 Countries by F. Bof de Andrade, J.L.F. Antunes, F.C.D. Andrade, M.F.F. Lima-Costa and J. Macinko in Journal of Dental Research
Acknowledgments
This analysis uses data from the Harmonized SHARE data set and Codebook (Version D.5 as of April 2019), the Harmonized CHARLS data set and Codebook (Version C as of April 2018), and the Harmonized KLoSA and Codebook (Version C as of June 2019) developed by the Gateway to Global Aging data. HRS data come from the RAND Center for the Study of Aging, with funding and support from the National Institute on Aging (NIA), and the Social Security Administration (SSA) created the RAND HRS data products. This analysis also uses Stata code from the Harmonized HRS data set and Codebook (Version A as of February 2018) and the Harmonized MHAS programming codes and Codebook (Version A). For more information, please refer to www.g2aging.org. ELSI information and programming codes were developed by the ELSI research team. The data set and documentation are public use and available at elsi.cpqrr.fiocruz.br.
Footnotes
A supplemental appendix to this article is available online.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
The National Institute on Aging (R01 AG030153, RC2 AG036619, R03 AG043052) funded the Harmonized versions of the SHARE, KLoSA, HRS, and CHARLS data used in this analysis. The Mexican Health and Aging Study (MHAS) receives support from the National Institutes of Health/National Institute on Aging (R01 AG018016). The ELSI was funded by the Brazilian Ministry of Health (grants 20836, 22566, and 23700 and 404965/2012-1).
ORCID iDs: F. Bof de Andrade  https://orcid.org/0000-0002-3467-3989
https://orcid.org/0000-0002-3467-3989
J.L.F. Antunes  https://orcid.org/0000-0003-3972-9723
https://orcid.org/0000-0003-3972-9723
F.C.D. Andrade  https://orcid.org/0000-0002-3856-3816
https://orcid.org/0000-0002-3856-3816
References
- Andersen RM. 1995. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 36(1):1–10. [PubMed] [Google Scholar]
- Babitsch B, Gohl D, von Lengerke T. 2012. Re-revisiting Andersen’s behavioral model of health services use: a systematic review of studies from 1998–2011. Psychosoc Med. 9:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barros AJ, Victora CG. 2013. Measuring coverage in MNCH: determining and interpreting inequalities in coverage of maternal, newborn, and child health interventions. PLoS Med. 10(5):e1001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bof de, Andrade F, Drumond Andrade FC, Noronha K. 2017. Measuring socioeconomic inequalities in the use of dental care services among older adults in Brazil. Community Dent Oral Epidemiol. 45(6):559–566. [DOI] [PubMed] [Google Scholar]
- Bordin D, Fadel CB, Santos CBD, Garbin CAS, Moimaz SAS, Saliba NA. 2017. Determinants of oral self-care in the Brazilian adult population: a national cross-sectional study. Braz Oral Res. 31:e115. [DOI] [PubMed] [Google Scholar]
- Börsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, Schaan B, Stuck S, Zuber S; SHARE Central Coordination Team. 2013. Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 42(4):992–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B, Lynch J, Smith GD. 2007. Measuring socioeconomic position in health research. Br Med Bull. 81–82(1):21–37. [DOI] [PubMed] [Google Scholar]
- Global Health Observatory. 2020. Universal health coverage [accessed 2020. February 10]. http://apps.who.int/gho/portal/uhc-overview.jsp
- Hart JT. 1971. The inverse care law. Lancet. 1(7696):405–412. [DOI] [PubMed] [Google Scholar]
- Horner-Johnson W, Dobbertin K, Beilstein-Wedel E. 2015. Disparities in dental care associated with disability and race and ethnicity. J Am Dent Assoc. 146(6):366–374. [DOI] [PubMed] [Google Scholar]
- Houweling TA, Kunst AE, Huisman M, Mackenbach JP. 2007. Using relative and absolute measures for monitoring health inequalities: experiences from cross-national analyses on maternal and child health. Int J Equity Health. 6:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe LD, Hargreaves JR, Huttly SR. 2008. Issues in the construction of wealth indices for the measurement of socioeconomic position in low-income countries. Emerg Themes Epidemiol. 5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Employment Information Service Employment Survey. 2018. Korea longitudinal study of aging [accessed 2018. December 27]. https://survey.keis.or.kr/eng/klosa/klosa01.jsp
- Li C, Yao NA, Yin A. 2018. Disparities in dental healthcare utilization in China. Community Dent Oral Epidemiol. 46(6):576–585. [DOI] [PubMed] [Google Scholar]
- Lima-Costa MF, de Andrade FB, de Souza PRB, Jr, Neri AL, Duarte YAO, Castro-Costa E, de Oliveira C. 2018. The Brazilian longitudinal study of aging (ELSI-BRAZIL): objectives and design. Am J Epidemiol. 187(7):1345–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Listl S. 2011. Income-related inequalities in dental service utilization by Europeans aged 50+. J Dent Res. 90(6):717–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Listl S, Moeller J, Manski R. 2014. A multi-country comparison of reasons for dental non-attendance. Eur J Oral Sci. 122(1):62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Listl S, Moran V, Maurer J, Faggion CM. 2012. Dental service utilization by Europeans aged 50 plus. Community Dent Oral Epidemiol. 40(2):164–174. [DOI] [PubMed] [Google Scholar]
- Machado CV, Silva GAE. 2019. Political struggles for a universal health system in Brazil: successes and limits in the reduction of inequalities. Global Health. 15(Suppl 1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, Kunst AE; European Union Working Group on Socioeconomic Inequalities in Health. 2008. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 358(23):2468–2481. [DOI] [PubMed] [Google Scholar]
- Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, Murray CJ. 2013. Global burden of oral conditions in 1990–2010. J Dent Res. 92(7):592–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. 2018. An inverse care law for our time. BMJ. 362:k3216. [DOI] [PubMed] [Google Scholar]
- Monteiro CN, Beenackers MA, Goldbaum M, de Azevedo Barros MB, Gianini RJ, Cesar CL, Mackenbach JP. 2016. Socioeconomic inequalities in dental health services in Sao Paulo, Brazil, 2003–2008. BMC Health Serv Res. 16(1):683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okunseri C, Garcia RI, Okunseri E, Visotcky A, Szabo A. 2015. Dental service utilization and neighborhood characteristics in young adults in the United States: a multilevel approach. J Public Health Dent. 75(4):282–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization for Economic Cooperation and Development. 2019. Health for everyone? Social inequalities in health and health systems (OECD health policy studies). Paris (France): OECD Publishing. [Google Scholar]
- Palència L, Espelt A, Cornejo-Ovalle M, Borrell C. 2014. Socioeconomic inequalities in the use of dental care services in Europe: what is the role of public coverage? Community Dent Oral Epidemiol. 42(2):97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peres KG, Peres MA, Boing AF, Bertoldi AD, Bastos JL, Barros AJ. 2012. Redução das desigualdades sociais na utilização de serviços odontológicos no Brasil entre 1998 e 2008. Rev Saúde Pública. 46(2):250–258. [DOI] [PubMed] [Google Scholar]
- Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C, et al. 2019. Oral diseases: a global public health challenge. Lancet. 394(10194):249–260. [DOI] [PubMed] [Google Scholar]
- Petersen PE, Kandelman D, Arpin S, Ogawa H. 2010. Global oral health of older people—call for public health action. Community Dent Health. 27(4, Suppl 2):257–267. [PubMed] [Google Scholar]
- Reda SM, Krois J, Reda SF, Thomson WM, Schwendicke F. 2018. The impact of demographic, health-related and social factors on dental services utilization: systematic review and meta-analysis. J Dent. 75:1–6. [DOI] [PubMed] [Google Scholar]
- Shen J, Listl S. 2018. Investigating social inequalities in older adults’ dentition and the role of dental service use in 14 European countries. Eur J Health Econ. 19(1):45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. 2014. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 43(2):576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson WM, Williams SM, Broadbent JM, Poulton R, Locker D. 2010. Long-term dental visiting patterns and adult oral health. J Dent Res. 89(3):307–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Educational, Scientific and Cultural Organization Institute for Statistics. 2006. International standard classification of education ISCED 1997. Montreal (Canada): UNESCO-UIS. [Google Scholar]
- Vujicic M, Buchmueller T, Klein R. 2016. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff Proj Hope. 35(12):2176–2182. [DOI] [PubMed] [Google Scholar]
- Watt RG, Daly B, Allison P, Macpherson LMD, Venturelli R, Listl S, Weyant RJ, Mathur MR, Guarnizo-Herreño CC, Celeste RK, et al. 2019. Ending the neglect of global oral health: time for radical action. Lancet. 394(10194):261–272. [DOI] [PubMed] [Google Scholar]
- Wong R, Michaels-Obregon A, Palloni A. 2017. Cohort profile: the Mexican Health and Aging Study (MHAS). Int J Epidemiol. 46(2):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, editor. 2013. Handbook on health inequality monitoring: with a special focus on low- and middle-income countries. Geneva (Switzerland): World Health Organization. [Google Scholar]
- Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. 2014. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 43(1):61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_0022034520935854 for Education-Related Inequalities in Dental Services Use among Older Adults in 23 Countries by F. Bof de Andrade, J.L.F. Antunes, F.C.D. Andrade, M.F.F. Lima-Costa and J. Macinko in Journal of Dental Research