Abstract
Background:
Women with breast cancer (BC) are living longer with debilitating side effects such as cancer-related fatigue (CRF) that affect overall well-being. Yoga promotes health, well-being and may be beneficial in reducing CRF. Although there have been previous systematic reviews and meta-analyses, the effects of yoga on CRF and quality of life (QOL) remain unclear, particularly in comparison with other types of physical activity (PA). Our objective is to carry out a systematic review and meta-analysis of the effects of yoga on CRF and QOL in women with BC.
Methods:
Electronic databases were searched (MEDLINE, Embase Classic+Embase and EMB Reviews, Cochrane Central CT) from inception to May 2018. Randomized controlled trials were included if they were full text, in English, included a yoga intervention, a comparator (including non-PA usual care or alternate PA intervention), and reported on CRF or QOL. Effects of yoga were pooled using standardized mean difference (SMD) via a random effects model.
Results:
Of the 2468 records retrieved, 24 trials were included; 18 studies compared yoga to a non-PA comparator and 6 to a PA comparator. Yoga demonstrated statistically significant improvements in CRF over non-PA (SMD −0.30 [−0.51; −0.08]) but not PA (SMD −0.17 [−0.50; 0.17]) comparators. Additionally, yoga demonstrated statistically significant improvements in QOL over non-PA (SMD −0.27 [−0.46; −0.07]) but not PA (SMD 0.04 [−0.22; +0.31]) comparators.
Discussion:
This meta-analysis found that yoga provides small to medium improvements in CRF and QOL compared to non-PA, but not in comparison to other PA interventions.
Keywords: breast cancer, yoga, meta-analysis, physical activity, cancer-related fatigue, quality of life, systematic review
Background
Breast cancer (BC) is 1 of the most common cancers diagnosed in women worldwide.1 With advancements in screening and treatment for BC, the mortality rate has decreased by 48% since 1986 in Canada,2 however, in over 100 countries BC remains the leading cause of death.1 Consequently, a greater number of women are living longer following a diagnosis of BC and managing the side effects and symptoms (such as fatigue, pain, cardiovascular disease, or depression)3 from the disease and its treatment, which can cause a reduction in quality of life (QOL).
Cancer-related fatigue (CRF) is a debilitating side effect that is experienced by 42% to 100% of women with BC.4-7 CRF varies by disease stage and treatment and is the most prevalent, long-lasting and distressing symptom experienced by people with cancer.4,5,8 CRF is a multidimensional symptom that affects an individual’s physical, emotional, and mental state.9-11 Rest has been previously suggested to alleviate CRF for anyone diagnosed with cancer4; however, increasing sedentary behavior can lead to muscle atrophy and decreased cardiovascular functioning, leading to an overall decrease in physical functioning and exacerbation of fatigue.4,10,12,13 Conversely, physical activity (PA), specifically moderate to vigorous PA (MVPA), has been shown to have a positive effect on CRF in multiple trials in women with BC.14,15 However, a majority of women with BC do not meet the recommended levels of MVPA for various reasons; physical, psychosocial, environmental and organizational factors.16-18 Many people with cancer, including BC, experiencing CRF have reported fatigue as a barrier19,20 to exercise participation, as well as preferences for mild intensity physical activity including yoga.20 Furthermore, physical activity guidelines for people with cancer recommend that the volume and intensity of exercise may need to be reduced for those experiencing severe CRF (based on specific cutpoints on individual fatigue measures).7,21 It is therefore essential to understand how alternative, less intense PA may affect CRF.
Yoga, a form of exercise, is grounded in Eastern traditional practice where there are often 8 aspects to the practice,22,23 while in Western society yoga consists of the 2 main aspects of postures and breath control.24 Yoga is practiced to improve health and well-being, and is purported to affect multiple dimensions of health (physical, mental, emotional, and spiritual).22,23 In a narrative review comparing the benefits of yoga and exercise on a variety of health outcomes among healthy and diseased adults including those with cancer, Ross and Thomas found yoga had similar benefits as conventional exercise for balance, menopausal symptoms, pain, mood, stress, quality of life (QOL), and CRF. However, in a variety of healthy and chronically ill (non-cancer) populations yoga showed smaller benefits for physical fitness (eg, VO2 max, and energy expenditure)23; this may hold true for individuals diagnosed with cancer. The incorporation of multiple dimensions within the practice of yoga may explain its role in positively effecting CRF.23,24 There are a variety of types of yoga such as Hatha, Bikram, and Iyengar, which include different aspects of physical poses, breath control and meditation.25 Furthermore, yoga can be adapted specifically for individuals with cancer; yoga postures can help with strength and flexibility, breath control assists with relaxation and focus, while meditation can help to calm the mind.25
To date, 5 systematic or comparator reviews16,25-28 and 8 meta-analyses have evaluated the effects of yoga on CRF and/or QOL; of these, 3 meta-analyses evaluated the role of yoga interventions on fatigue in multiple populations including BC and 2 on QOL,27,29,30 4 meta-analyses included yoga interventions within a broader analysis of the relationship of all exercise on CRF only in individuals with cancer (including BC),5,14,31,32 and 1 meta-analysis included mindfulness stress reduction therapy as a yoga comparator in women with BC on CRF and QOL.33 The previous systematic reviews and meta-analyses were limited in their elucidation of the role of yoga exclusively to improve CRF and QOL in BC population, as yoga and/or BC were not the only focus of the reviews. Thus, it is still unclear what the effect of yoga interventions is on CRF or QOL for women with BC, and whether yoga is superior to other forms of PA. With this new evidence-based knowledge, healthcare practitioners and exercise specialists would be more equipped to provide exercise prescriptions and education to assist women with BC in reducing their CRF and improving QOL. Thus, the PICO(T) for this present study was a population of adult women diagnosed with BC, various forms of yoga as the intervention type, with both active and non-active comparators, the outcome evaluated was both CRF and QOL, and type of studies included were randomized controlled trials. The objective of this systematic review and meta-analysis is to determine the role of yoga interventions in improving CRF and QOL in women with BC compared to non-active and active comparators.
Methods
This meta-analysis followed the PRISMA guidelines34 (see Figure 1 for the PRISMA diagram). An electronic search was completed by an academic librarian (RF) of 3 databases (MEDLINE, Embase Classic+Embase and EMB Reviews, Cochrane Central Register of Controlled Trials databases) from database inception until September 2016, with an updated search performed in May 2018. Additional screening of bibliographies from a previous systematic review14 was completed to identify any missed articles from the database search; no additional articles were identified.
Figure 1.
PRISMA diagram.
Eligibility criteria for this systematic review and meta-analysis were randomized controlled trials that included full text articles published in English. Our population of interest was women, diagnosed with BC (at any stage), receiving any type of treatment, age 18 years or older. Studies included some form of yoga intervention, which could include a variety of different types of yoga (eg, Hatha, Iyengar, Restorative). Interventions could be compared to waitlist control, standard or usual care, control group, health education, supportive therapy, or another form of exercise. Studies were included irrespective of intervention length. Studies needed to measure CRF or QOL as a primary or secondary outcome using a validated scale.
Independent reviewers (MO, DS, CL) evaluated the title and abstract of all articles obtained through the electronic search to determine if a study met inclusion and exclusion criteria. Two reviewers evaluated each citation. All citations that met the inclusion criteria based on initial title and abstract review were read in full to confirm eligibility. Consensus was achieved through discussion. A standardized data extraction form was used by 3 independent reviewers (MO, DS, CL) to extract the data from eligible studies (See Supplemental Table 1). Data from each study was extracted by 2 reviewers. All disagreements were resolved by an additional reviewer (SMHA).
Reviewers extracted relevant information such as study characteristics, intervention design and outcome measures. Meta-analysis comparators were classified as non-active or active comparators. Non-active comparators consisted of control group, waitlist, usual care, health education, and supportive therapy. Active comparators consisted of physically active interventions such as aerobic training or resistance training.
Primary authors were contacted to attempt to rectify missing data from the included articles. Reference lists of previous systematic reviews and meta-analyses were reviewed. If no further data were forthcoming, missing within-group standard deviations (SD) were computed in this priority sequence: (1) from 95% confidence intervals or standard errors, when they were reported; (2) from the same group’s SD at a different time in the study; (3) from the SD in the other group in the same study; (4) by dividing the interquartile range by 1.35.35 Within-group medians were used to replace missing within-group means.35 The pooled effects of yoga on CRF and QOL, compared to a non-physically active control, were calculated using random effects models; the standardized mean difference35 was the effect measure, as studies varied in the instruments used to measure outcomes. Additionally we analyzed the effects of yoga on CRF and QOL against physical activity-based comparators in the same fashion as non-active comparators. These analyses used outcomes measured at the assessment point directly following the intervention period. Heterogeneity was assessed with the I-squared test. Subgroup analysis was completed to explore differences in treatment effects across subgroups formed by cancer treatment, frequency of yoga sessions per week, length of intervention, use of relaxation within intervention, geographical region of study, fatigue measure used, and risk of bias level. Study bias was evaluated by authors MO, SMHA, and GT with the Cochrane risk of bias tool36 and publication bias was assessed visually using funnel plots. Analyses were conducted using the metafor packages in the R statistical software (Version 3.5.0).37
Results
We identified 2468 records through the electronic search through May 2018. Following the removal of duplicates (n = 912), 1556 citations were initially screened, and 105 full-text studies were assessed for eligibility. From the full text screening, 80 studies were excluded and 24 were included22,38-58 (see Supplemental Table 2 for exclusion reasons). Authors were contacted twice by email to obtain any missing data.
Eighteen studies compared yoga to a non-active comparator, and 4 compared yoga to an active comparator for CRF, whereas ten and 2 compared yoga to a non-active comparator and active comparator for QOL, respectively (see Supplemental Table 3 for breakdown). The 24 articles were published between 2006 and 2018 and were conducted in the United States (n = 13), as well as India (n = 2), Turkey (n = 2), Germany (n = 2), Australia (n = 1), Poland (n = 1), Canada (n = 1), Belgium (n = 1) and Taiwan (n = 1). The studies included a total of 1394 women diagnosed with BC, and mean ages ranged from 45 to 69 years old. Studies predominantly assessed women who had completed BC treatment (n = 11), compared to those currently on treatment (n = 9), or a combination of current and completed treatment (n = 4).The mean intervention length across the 24 studies was 9.5 weeks, with a range of 6 to 26 weeks. Yoga sessions ranged from 30 to 90 minutes with an average session of 72 minutes. The intensity level of the yoga intervention was not clearly defined within the included studies; however, 14 studies described the yoga programs as gentle, low, or modified to participants’ abilities (see Table 1 for study descriptions). Hatha was the most common form of yoga intervention assessed (n = 16)22,39,40,43,45-48,50,53-59; additionally, Vivekanada Yoga Anusandhana Samsthana (VYASA) (n = 2),41,42 Satyanada (n = 1),49 Baba Joga (n = 1)38 and general or unspecified (n = 4)44,51,52,59 interventions were evaluated. Yoga interventions were supervised in most of the studies, only 2 studies53,57 used non-supervised interventions. Waitlist control was used in eleven studies, and 1 of those studies had a third comparison group consisting of stretching. Control or usual care comparators consisted of supportive therapy (n = 2), health/wellness education (n = 1), oncologist recommendations for exercise (n = 1) stretching exercises (n = 1), self-hypnosis (n = 1), and cognitive behavior therapy (n = 1). The active comparators comprised of physical exercise (n = 2), “rapid easy strength training” (n = 1) and aerobic training (n = 1). Data extracted from each study included can be seen in Supplementary Table 1.
Table 1.
Study Description.
| Study | Type of yoga | Total participants | Intervention | Comparator |
|---|---|---|---|---|
| Andysz et al38 | Baba Joga yoga | 28 (Yoga n = 12, Control n = 16) | Once per week for 10 weeks | Control group |
| Banasik et al60 | Iyengar yoga | 18 (Yoga n = 7, Control n = 7) | Twice per week for 8 weeks | Control group |
| Bower et al40 | Iyengar yoga | 31 (Yoga n = 16, active comparator n = 15) | Twice per week for 12 weeks | Health education |
| Chandwani et al42 | Vivekanada Yoga Anusandhana Samsthana (VYASA) | 61 (yoga n = 27, control n = 31) | Up to 2 times per week in center and 1 time at home for 6 weeks | Control group |
| Chandwani et al41 | Vivekanada Yoga Anusandhana Samsthana (VYASA) | 163 (yoga n = 53, control n = 54, active comparator n = 56) | Up to 3 times per week for 6 | Stretch group |
| Cramer et al43 | Hatha yoga | 40 (yoga n = 19, control n = 19) | Once per week for 12 weeks with certified hatha yoga instructor | Control group |
| Culos-Reed et al44 | Type not specified | 38 (yoga n = 20, control n = 18) | 7-week intervention, frequency of classes not indicated | Control group |
| Danhauer et al45 | Restorative yoga | 44 (yoga n = 22, control n = 22) | Once per week for 10 weeks with instructor | Control group |
| Gregorie et al46 | Hatha yoga | 138 (yoga n = 21, control n = 24, active comparators n = 68) | Once per week for 6 weeks | Self-hypnosis and cognitive behaviour therapy |
| Kiecolt-Glaser et al47 | Hatha yoga | 200 (yoga n = 10, control n = 100) | Twice per week for 12 weeks | Control group |
| Littman et al22 | Viniyoga | 63 (yoga n = 32, control n = 31) | At least once per week for 26 weeks | Control group |
| Lotzke et al48 | Iyengar yoga | 92 (yoga n = 45, active comparator n = 47) | At least 3 times per week for 12 weeks | Physical Exercise |
| Loudon et al49 | Satyananda yoga | 59, 28 randomized (yoga n = 15, control n = 13) | At least once in center session and daily home practice for 8 weeks | Control group |
| Moadel et al50 | Hatha yoga | 128 (yoga n = 84, control n = 44) | Once per week for 12 weeks | Control group |
| Pruthi et al51 | Type not specified | 30 (yoga n = 15, control n = 15) | Once per week for 8 weeks | Control group |
| Siedentopf et al52 | Type not specified | 75 (yoga n = 49, control n = 44) | Twice per week for 5 weeks | Control group |
| Stan et al53 | Hatha yoga | 34 (yoga n = 18, active comparator n = 16) | 3–5 times per week for 12 weeks | Rapid easy strength training |
| Taso et al54 | Anusara Yoga | 60 (yoga n = 30, control n = 30) | Twice per week for 8 weeks | Control group |
| Taylor et al55 | Restorative/Pranayama Yoga | 33 (yoga n = 14, control n = 12) | Once per week for 8 weeks | Control group |
| Vadiraja et al61 | Type not specified | 88 (yoga n = 42, active comparator n = 33) | Between 3–4 times per week (in center and home practice) for 6 weeks | Supportive therapy |
| Vadiraja et al59 | Asanas, breathing, mediation, yogic relaxation techniques | 91 (yoga n = 42, control n = 33) | Twice per week for 12 weeks | Control group |
| Winters-Stone et al57 | Restorative yoga DVD | 95 (yoga n = 47, control n = 43) | Up to three times per week for 8 weeks | Control group |
| Vardar Yağlı et al56 | Yogasana | 52 (Yoga n = 24, active comparator n = 28) | Three times per week for 6 weeks | Aerobic training |
| Vardar Yağlı and Ulger58 | Asanas | 20 (yoga n = 10, active comparator n = 10) | Once per week for 8 weeks | Physical exercise |
Of the 24 articles, 22 provided data on CRF and 12 on QOL. Fatigue was measured with multiple scales, the most common scales were Functional Assessment of Cancer Therapy (FACT)—Fatigue (FACT-F) subscale (n = 5) and Brief Fatigue Inventory (BFI, n = 5), followed by the Eastern Co-operative Oncology Group Quality of Life Questionnaire—C30 (EORTC QLQ-C30) Fatigue subscale (n = 4), Fatigue Symptom Inventory (FSI, n = 2) and Visual Analog Scale (n = 2). QOL was also measured with multiple scales, the most common being the EORTC QLQ C30 (n = 5 studies) and FACT-Breast (n = 5 studies), followed by Medical Outcomes Short Form 36 (n = 3), FACT-General (n = 2) and Lymphedema Quality of Life Questionnaire (n = 1).
Overall, the studies contained low-moderate scores for risk of bias (Figure 2 and Supplemental Figure 4). The most common methodological weaknesses were not indicating how the participants were randomized (n = 12 studies), and no indication of allocation concealment (n = 8 studies). Only 1 study indicated that participants were blinded to the study hypothesis, and 2 studies indicated some or all of the outcome assessors were blinded to group allocation. As these interventional studies required participants to actively participate in the yoga intervention, blinding participants to their intervention allocation would not be possible. Although attrition occurred within all studies, 3 studies did not provide reasons for study attrition therefore had high risk of bias; the remaining studies providing some description as to why and how it affected the outcome. Most studies had low risk for other potential sources of bias.
Figure 2.

Overview of risk of bias (n = 24 studies).
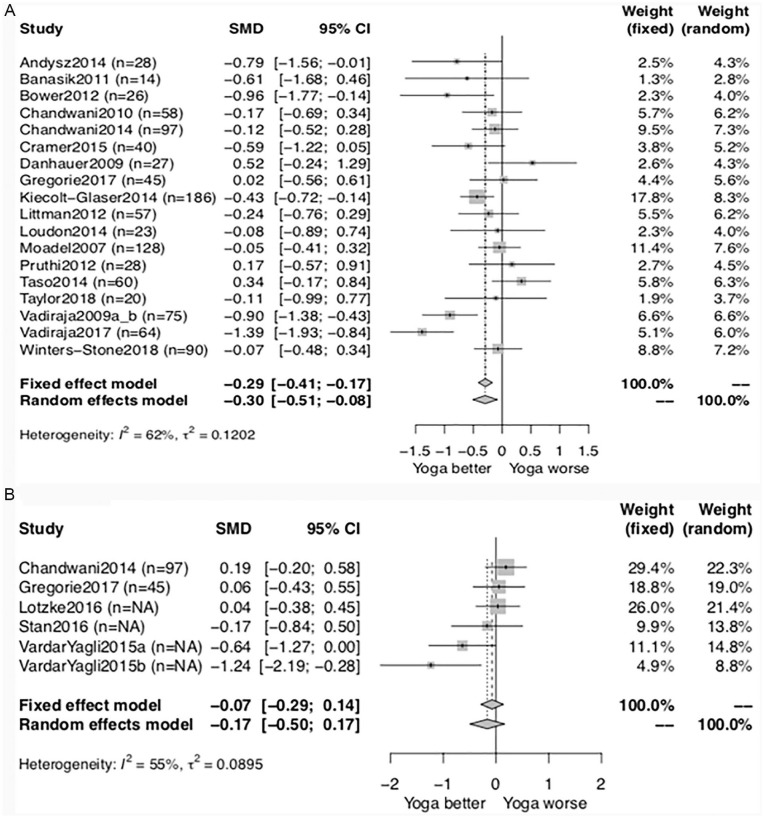
Cancer-Related Fatigue
Compared to non-active comparators (n = 18 studies), reduction of CRF with yoga had a small to moderate pooled SMD of -0.30 (95% CI -0.51, −0.08) (Figure 3A). Comparing yoga intervention to active comparators (n = 6), there was a small SMD of −0.17 (95% CI −0.50, 0.17) (Figure 3B). There was substantial heterogeneity in both analyses (vs. non-active comparators: I2 = 62%; vs. active comparators: I2 = 55%). Heterogeneity for both the control and active comparator meta-analysis was explored through subgroup analyses (see below).
Figure 3.
Forest plot for CRF using comparisons of post-values with. (A) Non-active comparators. (B) Active comparators.
Quality of Life
Compared to non-active comparators (n = 10 studies), yoga had a small to moderate beneficial effect on QOL (SMD 0.27, 95% CI 0.46, 0.07) (Figure 4A). There was low heterogeneity (I2 = 21%). Compared to active comparators, yoga had a negligible pooled effect, with a SMD of -0.04 (95% CI 0.22, −0.31) (Figure 4B). There was no heterogeneity (I2 = 0%).
Figure 4.
Forest plot for QOL using comparisons of post-values with. (A) Non-active comparators. (B) Active comparators.
Subgroup Analyses and Heterogeneity
For the CRF outcome, only the subgroups examining specific fatigue measures identified differential effects of yoga (P < .01). The FSI (n = 2), showed a larger effect size (−1.25; 95% CI −1.71, −0.8) than the EORTC QLQ-C30 fatigue item (n = 3; −0.63; 95% CI −0.96, −0.31), the BFI (n = 5, 0.00; 95% CI −0.24, +0.24), and FACT-F (n = 4; −0.12; 95% CI −0.47, +0.24) (test for between-group effect P < .001) (see supplementary Figure 1a-g). No differential effect by subgroup was found for CRF related to cancer treatment phase (P = .19), number of yoga sessions per week (P = .11), length of intervention (P = 0.97), use of relaxation within intervention (P = .85), geographical location of study (P = 0.43) or risk of bias level of the study (P = .22).
For the QOL outcome, only 1 subgroup analysis indicated a differential effect of yoga (test for between-group effect P = 0.02): the number of sessions completed per week. Specifically, yoga completed once per week resulted in a moderate effect size (0.42; 95% CI 0.20, 0.64) whereas 2 or more sessions per week had a negligible effect (0.02; 95% CI −0.24, 0.28) (See supplemental Figure 2a-e).
Discussion
This study provides a rigorous updated examination of the role of yoga on CRF and QOL for women with BC. Based on 24 trials, the meta-analysis suggests a small to moderate beneficial effect of yoga on CRF compared to a non-active group, but no benefit was found compared to an active group. Similarly, when comparing yoga to both a non-active and active group for QOL, there was a small to moderate-sized beneficial effect for QOL for yoga compared to the non-active group, but not for the active group. From the studies that described adherence to their interventions, the data suggest that participants were moderately to highly adherent with yoga and PA interventions.
There is substantial heterogeneity between these studies for the CRF outcome, however low to no heterogeneity for QOL. In the CRF subgroup analysis, it appeared that for studies examining the effect of yoga, 1 fatigue outcome measure (the FSI) may be more sensitive to change than several others, as we found substantial heterogeneity (I2 = 69%) in that subgroup analysis. This may be due in part to the FSI evaluating both physical and mental aspects of fatigue, compared to the EORTC QLQ-C30, BFI and FACT-F, which predominantly evaluate the physical aspect of fatigue.62
Our findings confirm and extend previous systematic reviews and meta-analyses. A review by Sadja et al in 201425 found that yoga may be beneficial in reducing CRF for women with BC, when compared to non-active comparator (control group). Three previous meta-analyses29,30,63 compared yoga to a range of non-active comparators (control, wait-list, supportive therapy). Boehm et al63 included 19 studies and found similar results to ours (SMD = 0.27 [0.23;0.31]), as well as Buffart et al29 (n = 15) (SMD = −0.51 [−0.79;−0.220]), compared to Lin et al30 (n = 4) who did not find statistically significant results (SMD = -0.15 [−0.29;0.09]),29,30,63 this may be due to the smaller sample size. When comparing our findings to meta-analyses that evaluated overall exercise interventions (including yoga)5,32 and exercise (with no yoga intervention)11,15 for CRF benefit, our findings also demonstrate similar results. However, none of the previous reviews evaluated yoga versus an active comparator as we have. Our findings suggest that yoga provides benefits on CRF compared to non-active comparators, similar to the literature. However, our findings additionally suggest that yoga may have similar benefits on CRF as physical activity, however yoga is better than no activity at all. This is an important finding that can be used in clinical practice to incorporate a yoga program into an expanded set of prescription options to assist women with BC in managing their CRF.
Strengths of this review include a rigorous literature search, screening and data extraction, follow-up with authors on insufficient data, and completing a study quality assessment. There are also limitations to our study, as we excluded non-English, non-randomized, non-full text publications and focused on breast cancer only studies. We used post values rather than change score values for the meta-analysis as this provided the review with more robust data for inclusion in meta-analyses. Additional limitations relate to the evidence, which require our analyses to be interpreted with caution. Such limitations included the following: multiple studies (CRF only [n = 1],52 QOL only [n = 12]39,40,46,47,51,54-59,61) were excluded from the meta-analysis due to insufficient data . We also recognize the need to be cautious in interpreting subgroup analyses because of the risk of false-positives. Any such findings would require validation in future trials. Data extraction was limited by the ways in which studies reported their results, which varied widely and included baseline and post-intervention mean and standard deviation, mean change and standard deviation, to median and interquartile range, standard error, and other variations. Additionally, many of the studies evaluated had high risk of bias in the participant and outcome assessor blinding categories/items and the number of active comparator studies was relatively small. Future research should focus on conducting phase III RCTs to help build evidence on the effects of yoga on CRF (eg, optimal “dose” and treatment duration, key elements).
This systematic review and meta-analysis will assist clinicians and researchers by providing a summary of current evidence on the effects of yoga on CRF and QOL. This meta-analysis demonstrates that yoga is beneficial in improving CRF and QOL for women with BC and that these benefits are comparable to the active comparators such as aerobic, resistance or combination of aerobic and resistance exercise. The findings from this review should encourage the recommendation of yoga as a prescription to reduce CRF. Of note, many women with BC may find yoga easier to adopt than other physical activity interventions for various reasons, such as providing benefits to managing CRF through lower intensity physical activity, and our findings confirm it to be equally efficacious for CRF and QOL outcomes. Future research should focus on studying the sensitivity of different CRF scales and understanding the barriers to implementation of yoga in the real world.
Supplemental Material
Supplemental material, Yoga_breast_ca_syst_rev_ICT_suppl_methods for The Effect of Yoga Interventions on Cancer-Related Fatigue and Quality of Life for Women with Breast Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials by Meagan O’Neill, Dominic Samaroo, Christian Lopez, George Tomlinson, Daniel Santa Mina, Catherine Sabiston, Nicole Culos-Reed and Shabbir M. H. Alibhai in Integrative Cancer Therapies
Supplemental material, Yoga_breast_ca_syst_rev_ICT_suppl_tables_figures for The Effect of Yoga Interventions on Cancer-Related Fatigue and Quality of Life for Women with Breast Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials by Meagan O’Neill, Dominic Samaroo, Christian Lopez, George Tomlinson, Daniel Santa Mina, Catherine Sabiston, Nicole Culos-Reed and Shabbir M. H. Alibhai in Integrative Cancer Therapies
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shabbir M. H. Alibhai  https://orcid.org/0000-0001-7815-6046
https://orcid.org/0000-0001-7815-6046
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [DOI] [PubMed] [Google Scholar]
- 2. Committee CCSA. Canadian Cancer Statistics 2019. Published 2019. Accessed September 1, 2019. [Google Scholar]
- 3. Ewertz M, Jensen AB. Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncol. 2011;50:187-193. [DOI] [PubMed] [Google Scholar]
- 4. Luctkar-Flude MF, Groll DL, Tranmer JE, Woodend K. Fatigue and physical activity in older adults with cancer. Cancer Nurs. 2007;30:e35-e45. [DOI] [PubMed] [Google Scholar]
- 5. Brown JC, Huedo-Medina TB, Pescatello LS, Pescatello SM, Ferrer RA, Johnson BT. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2011;20:123-133. [DOI] [PubMed] [Google Scholar]
- 6. Haas BK. Fatigue, self-efficacy, physical activity, and quality of life in women with breast cancer. Cancer Nurs. 2011;34: 322-334. [DOI] [PubMed] [Google Scholar]
- 7. Mortimer JE, Barsevick AM, Bennett CL, et al. Studying cancer-related fatigue: report of NCCN scientific research committee. J Natl Compr Canc Netw. 2010;8:1131. [DOI] [PubMed] [Google Scholar]
- 8. Husebo AM, Dyrstad SM, Mjaaland I, Soreide JA, Bru E. Effects of scheduled exercise on cancer-related fatigue in women with early breast cancer. Sci World J. 2014;2014:271828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berger AM, Gerber LH, Mayer DK. Cancer-related fatigue: implications for breast cancer survivors. Cancer. 2012;118:2261-2269. [DOI] [PubMed] [Google Scholar]
- 10. Cramp F, Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;(2):CD006145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Velthuis MJ, Agasi-Idenburg SC, Aufdemkampe G, Wittink HM. The effect of physical exercise on cancer-related fatigue during cancer treatment: a meta-analysis of randomized controlled trials. Clinical Oncology. 2010;22:208-221. [DOI] [PubMed] [Google Scholar]
- 12. Edwardson CL, Gorely T, Davies MJ, et al. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS ONE. 2012;7:e34916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Humpel N, Iverson DC. Sleep quality, fatigue and physical activity following a cancer diagnosis. Eur J Cancer Care. 2010;19:761-768. [DOI] [PubMed] [Google Scholar]
- 14. Tomlinson D, Diorio C, Beyene J, Sung L. Effect of exercise on cancer-related fatigue: a meta-analysis. Am J Phys Med Rehabil. 2014;93:675-686. [DOI] [PubMed] [Google Scholar]
- 15. Oberoi S, Robinson PD, Cataudella D, et al. Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: a systematic review and meta-analysis of randomized trials. Crit Rev Oncol Hemat. 2018;122:52-59. [DOI] [PubMed] [Google Scholar]
- 16. Smith SG, Chagpar AB. Adherence to physical activity guidelines in breast cancer survivors. Am Surgeon. 2010;76:962. [PubMed] [Google Scholar]
- 17. Ottenbacher A, Yu M, Moser RP, Phillips SM, Alfano C, Perna FM. Population estimates of meeting strength training and aerobic guidelines, by gender and cancer survivorship status: findings from the Health Information National Trends Survey (HINTS). J Phys Act Health. 2015;12:675-679. [DOI] [PubMed] [Google Scholar]
- 18. Brunet J, Taran S, Burke S, Sabiston CM. A qualitative exploration of barriers and motivators to physical activity participation in women treated for breast cancer. Disabil Rehabil. 2013;35:2038-2045. [DOI] [PubMed] [Google Scholar]
- 19. Blaney J, Lowe-Strong A, Rankin J, Campbell A, Allen J, Gracey J. The cancer rehabilitation journey: barriers to and facilitators of exercise among patients with cancer-related fatigue. Phys Ther. 2010;90:1135-1147. [DOI] [PubMed] [Google Scholar]
- 20. Blaney JM, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH. Cancer survivors’ exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire-survey. Psycho-Oncol. 2013;22:186-194. [DOI] [PubMed] [Google Scholar]
- 21. Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:243-274. [DOI] [PubMed] [Google Scholar]
- 22. Littman AJ, Bertram LC, Ceballos R, et al. Randomized controlled pilot trial of yoga in overweight and obese breast cancer survivors: effects on quality of life and anthropometric measures. Support Care Cancer. 2012;20:267-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complem Med. 2010; 16:3-12. [DOI] [PubMed] [Google Scholar]
- 24. Bower JE, Woolery A, Sternlieb B, Garet D. Yoga for cancer patients and survivors. Cancer Control. 2005;12:165-171. [DOI] [PubMed] [Google Scholar]
- 25. Sadja J, Mills PJ. Effects of yoga interventions on fatigue in cancer patients and survivors: a systematic review of randomized controlled trials. Explore. 2013;9:232-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harder H, Parlour L, Jenkins V. Randomised controlled trials of yoga interventions for women with breast cancer: a systematic literature review. Support Care Cancer. 2012;20:3055-3064. [DOI] [PubMed] [Google Scholar]
- 27. Morgan SJ. Does yoga decrease cancer-related fatigue in women with breast cancer? Systematic review of randomized controlled trials. Int J Res Med Sci. 2017;5:1180. [Google Scholar]
- 28. Sharma M, Lingam VC, Nahar VK. A systematic review of yoga interventions as integrative treatment in breast cancer. J Cancer Res Clin Oncol. 2016;142:2523-2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Buffart LM, van Uffelen JGZ, Riphagen II, et al. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2012;12:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lin KY, Hu YT, Chang KJ, Lin HF, Tsauo JY. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evid Based Complement Alternat Med. 2011;2011:659876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hilfiker R, Meichtry A, Eicher M, et al. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. BJSM Online. 2018;52:651-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mustian KM, Alfano CM, Heckler C, et al. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: A meta-analysis. JAMA Oncol. 2017;3:961-968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pan Y, Yang K, Wang Y, Zhang L, Liang H. Could yoga practice improve treatment-related side effects and quality of life for women with breast cancer? A systematic review and meta-analysis. Asia Pac J Clin Oncol. 2017;13:e79-e95. [DOI] [PubMed] [Google Scholar]
- 34. Moher D, Liberati AM, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264-269. [DOI] [PubMed] [Google Scholar]
- 35. Higgins JP. Cochrane handbook for systematic review of interventions version 5.0.1 (updated March 2011). The Cochrane Collaboration Website. Published 2010. [Google Scholar]
- 36. Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1-48. https://www.jstatsoft.org/article/view/v036i03. [Google Scholar]
- 38. Andysz A, Merecz D, Wojcik A, Swiatkowska B, Sierocka K, Najder A. Effect of a 10-week yoga programme on the quality of life of women after breast cancer surgery. Prz Menopauzalny. 2014;13:186-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Pract. 2011;23:135-142. [DOI] [PubMed] [Google Scholar]
- 40. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118:3766-3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chandwani KD, Perkins G, Nagendra HR, et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. J Clin Oncol. 2014;32:1058-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chandwani KD, Thornton B, Perkins GH, et al. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. J Soc Integr Oncol. 2010;8:43-55. [PubMed] [Google Scholar]
- 43. Cramer H, Rabsilber S, Lauche R, Kummel S, Dobos G. Yoga and meditation for menopausal symptoms in breast cancer Survivors – a randomized controlled trial. Cancer. 2015; 121:2175-2184. [DOI] [PubMed] [Google Scholar]
- 44. Culos-Reed SN, Carlson LE, Daroux LM, Hately-Aldous S. A pilot study of yoga for breast cancer survivors: physical and psychological benefits. Psycho-Oncol. 2006;15:891-897. [DOI] [PubMed] [Google Scholar]
- 45. Danhauer SC, Mihalko SL, Russell GB, et al. Restorative yoga for women with breast cancer: findings from a randomized pilot study. Psycho-Oncol. 2009;18:360-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gregoire C, Bragard I, Jerusalem G, et al. Group interventions to reduce emotional distress and fatigue in breast cancer patients: a 9-month follow-up pragmatic trial. Br J Cancer. 2017;117:1442-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kiecolt-Glaser JK, Bennett JM, Andridge R, et al. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2014;32:1040-1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lotzke D, Wiedemann F, Rodrigues Recchia D, et al. Iyengar-yoga compared to exercise as a therapeutic intervention during (neo)adjuvant therapy in women with stage I-III breast cancer: health-related quality of life, mindfulness, spirituality, life satisfaction, and cancer-related fatigue. Evid-Based Compl Alt. 2016;2016:5931816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Loudon A, Barnett T, Piller N, Immink MA, Williams AD. Yoga management of breast cancer-related lymphoedema: a randomized controlled pilot-trial. BMC Altern Med. 2014;14:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Moadel AB, Shah C, Wylie-Rosett J, et al. Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: effects on quality of life. J Clin Oncol. 2007;25: 4387-4395. [DOI] [PubMed] [Google Scholar]
- 51. Pruthi S, Stan D, Jenkins SM, et al. A randomized controlled pilot study assessing feasibility and impact of yoga practice on quality of life, mood, and perceived stress in women with newly diagnosed breast cancer. Glob Adv Health Med. 2012;1:30-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Siedentopf F, Utz-Billing I, Gairing S, Schoenegg W, Kentenich H, Kollak I. Yoga for patients with early breast cancer and its impact on quality of life – a randomized controlled trial. Geburtshilfe Frauenheilkd. 2013;73:311-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Stan DL, Croghan KA, Croghan IT, et al. Randomized pilot trial of yoga versus strengthening exercises in breast cancer survivors with cancer-related fatigue. Support Care Cancer. 2016;24:4005-4015. [DOI] [PubMed] [Google Scholar]
- 54. Taso CJ, Lin HS, Lin WL, Chen SM, Huang WT, Chen SW. The effect of yoga exercise on improving depression, anxiety, and fatigue in women with breast cancer: a randomized controlled trial. J Nurs Res. 2014;22:155-164. [DOI] [PubMed] [Google Scholar]
- 55. Taylor TR, Barrow J, Makambi K, et al. A restorative yoga intervention for African-American breast cancer survivors: a pilot study. J Racial Ethn Health Disparities. 2018;5:62-72. [DOI] [PubMed] [Google Scholar]
- 56. Vardar Yağlı N, Şener G, Arıkan H, et al. Do yoga and aerobic exercise training have impact on functional capacity, fatigue, peripheral muscle strength, and quality of life in breast cancer survivors? Integ Cancer Ther. 2015;14:125-132. [DOI] [PubMed] [Google Scholar]
- 57. Winters-Stone KM, Moe EL, Perry CK, et al. Enhancing an oncologist’s recommendation to exercise to manage fatigue levels in breast cancer patients: a randomized controlled trial. Support Care Cancer. 2018;26:905-912. [DOI] [PubMed] [Google Scholar]
- 58. Vardar Yağlı N, Ulger O. The effects of yoga on the quality of life and depression in elderly breast cancer patients. Complement Ther Clin Pract. 2015;21:7-10. [DOI] [PubMed] [Google Scholar]
- 59. Vadiraja H, Rao R, Nagarathna R, Nagendra H, Patil S, Diwakar R. Effects of yoga in managing fatigue in breast cancer patients: a randomized controlled trial. Indian J 2017;23:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of Iyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. J Am Acad Nurse Prac. 2011;23:135-142. [DOI] [PubMed] [Google Scholar]
- 61. Vadiraja HS, Rao MR, Nagarathna R, et al. Effects of yoga program on quality of life and affect in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Complement Ther Med. 2009;17:274-280. [DOI] [PubMed] [Google Scholar]
- 62. Minton O, Stone P. A systematic review of the scales used for the measurement of cancer-related fatigue (CRF). Ann Oncol. 2009;20:17-25. [DOI] [PubMed] [Google Scholar]
- 63. Boehm K, Ostermann T, Milazzo S, Bussing A. Effects of yoga interventions on fatigue: a meta-analysis. Evid Based Complement Alternat Med. 2012;2012:124703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Yoga_breast_ca_syst_rev_ICT_suppl_methods for The Effect of Yoga Interventions on Cancer-Related Fatigue and Quality of Life for Women with Breast Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials by Meagan O’Neill, Dominic Samaroo, Christian Lopez, George Tomlinson, Daniel Santa Mina, Catherine Sabiston, Nicole Culos-Reed and Shabbir M. H. Alibhai in Integrative Cancer Therapies
Supplemental material, Yoga_breast_ca_syst_rev_ICT_suppl_tables_figures for The Effect of Yoga Interventions on Cancer-Related Fatigue and Quality of Life for Women with Breast Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials by Meagan O’Neill, Dominic Samaroo, Christian Lopez, George Tomlinson, Daniel Santa Mina, Catherine Sabiston, Nicole Culos-Reed and Shabbir M. H. Alibhai in Integrative Cancer Therapies