Abstract
Objective:
Medical events such as myocardial infarction and cancer diagnosis can induce symptoms of posttraumatic stress disorder (PTSD). The optimal treatment of PTSD symptoms in this context is unknown.
Methods:
A literature search of 6 biomedical electronic databases was conducted from database inception to November 2018. Studies were eligible if they used a randomized design and evaluated the effect of treatments on medical event-induced PTSD symptoms in adults. A random effects model was used to pool data when two or more comparable studies were available.
Results:
Six trials met full inclusion criteria. Studies ranged in size from 21 to 81 patients, and included patients with PTSD induced by cardiac events, cancer, HIV, multiple sclerosis, and stem cell transplantation. All trials assessed psychological interventions. Two trials comparing a form of exposure-based cognitive behavioral therapy (CBT) with assessment-only control found that CBT resulted in lower PTSD symptoms [Hedges’s g = −0.47, (95% CI −0.82 – −0.12), p = .009]. A third trial compared imaginal exposure (another form of exposure-based CBT) with an attention control and found a trend toward reduced PTSD symptoms. Three trials compared eye movement desensitization and reprocessing (EMDR) with active psychological treatments (imaginal exposure, conventional CBT, and relaxation therapy), and found that EMDR was more effective.
Conclusion:
CBT and EMDR may be promising approaches to reducing PTSD symptoms due to medical events. However, additional trials are needed in this patient population.
Keywords: posttraumatic stress disorder, medical event-induced PTSD, treatment, cognitive behavioral therapy, psychotherapy, eye-movement desensitization and reprocessing
Introduction
Posttraumatic stress disorder (PTSD) can occur after experiencing a traumatic event and involves symptoms of re-experiencing of the event, avoidance of trauma-related stimuli, negative alterations in thoughts and feelings, and hyperarousal [1]. Research has traditionally focused on PTSD that develops in response to external traumatic events such as military combat, natural disasters, and sexual assault. However, a growing body of literature supports the existence of PTSD induced by internal threats in the form of acute medical events [2, 3, 4].
Life-threatening disease was included as a potentially traumatic event that could induce PTSD in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders [5]. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders clarified that only medical events or illnesses that are sudden or catastrophic are capable of triggering PTSD [1]. Medical-event induced PTSD symptoms subsequently have been described in several patient populations. Cardiovascular events such as myocardial infarction and stroke, for example, can be extremely frightening and traumatic as they often have a sudden onset, may lead to death or serious bodily harm, and may cause patients to feel helpless [6]. A recent review of the empirical research on cardiac event-induced PTSD found that PTSD symptoms that manifest after cardiac events resemble PTSD symptoms induced by external events, and the authors suggest that similar types of interventions may be useful [4]. A meta-analysis by Edmondson et al. estimated the prevalence of clinically significant PTSD symptoms after an acute coronary syndrome (ACS) to be approximately 12% [7]. Prevalence estimates in the year after stroke are even higher, with 1 in 4 patients developing elevated PTSD symptoms [8]. There have also been studies assessing PTSD symptoms in cancer patients. Cancer patients frequently report feelings of fear, horror, and helplessness after cancer diagnosis. Cues associated with cancer treatment can elicit nightmares and intrusive thoughts in these patients [9].
It is worth noting that there has been significant debate over whether PTSD is the correct diagnostic entity for this phenomenon. [4, 10, 11]. However, regardless of the diagnostic label, it is clear that the symptoms that patients are experiencing have serious adverse effects on health outcomes. For example, patients with cardiac event-induced PTSD symptoms have lower medication adherence and appear to be at double the risk of recurrent cardiac events and mortality [12, 13, 7, 4]. Stroke survivors who develop PTSD symptoms are nearly three times more likely to be nonadherent to medication as compared to stroke survivors without PTSD [14]. HIV patients with PTSD symptoms have lower adherence to antiretroviral medications and increased rates of disease progression [15].
The optimal treatment of medical event-induced PTSD symptoms remains unknown. Both psychotherapy and pharmacotherapy approaches have been used to treat PTSD in other patient populations [16, 17, 18]. Evidence has most strongly supported the use of trauma-focused psychotherapies in treating PTSD in general [16, 19, 20]. Trauma-focused psychotherapy is any therapy that utilizes cognitive, emotional, or behavioral techniques to facilitate the processing of a traumatic event; many of these therapeutic approaches include cognitive behavioral therapy (CBT) techniques such as exposure to trauma-related memories, images, cues, and cognitive restructuring [17, 19, 21]. Examples of these treatments that have received some of the strongest empirical support are prolonged exposure and cognitive processing therapy [16, 19, 20]. Eye movement desensitization and reprocessing (EMDR) incorporates cognitive behavioral and psychodynamic therapies, but also utilizes dual attention stimuli, such as saccadic eye movements; there is some debate in the field regarding which treatment elements are most associated with treatment response [20, 21, 22]. Benefits of psychodynamic psychotherapy, interpersonal therapy, and pharmacologic therapy (e.g., sertraline, venlafaxine) for treating PTSD have also been observed in some studies, but the degree of empirical support is not as strong as for trauma-focused psychotherapies [19, 20, 23, 24].
It is not yet clear if these treatments are effective in treating PTSD symptoms induced by medical events. Despite similarities, medical event-induced PTSD symptoms may also differ from those due to external traumatic events given the often future-oriented, rather than retrospective, nature of symptoms such as re-experiencing and avoidance [25]. While PTSD that develops in response to combat or a natural disaster is generally focused on past events, PTSD symptoms triggered by medical events often center on the fear of medical event recurrence [25, 26]. This may lead to differences in how patients respond to psychological treatments that are generally effective in treating PTSD due to other types of traumas. There may also be differences in the acceptability of treatment among patients whose PTSD symptoms developed due to an acute medical event, many of whom are identified in medical settings and are not ordinarily seeking psychological treatment. Finally, in the case of pharmacotherapy, there may be difference in side effects or other adverse effects from psychotropic medications in those with PTSD symptoms and comorbid medical disease. Though there have been several systematic reviews on medical event-induced PTSD, they have not reviewed treatment modalities [27, 28, 29]. A meta-analysis on cardiac-disease-induced PTSD included a subsection on treatment, referring to two studies that examined trauma-focused cognitive behavioral therapy, but the effects were modest due to a lack of power [4]. One other prior review focused on early interventions to prevent PTSD [30]. To our knowledge, there has been no systematic review that focuses on the treatment of medical event-induced PTSD symptoms. Therefore, we performed a systematic review to explore the current understanding of the effectiveness of interventions for reducing medical event-induced PTSD symptoms.
Method
Search strategy
This systematic review was conducted under the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria. The systematic review was registered on PROSPERO, the international prospective register of systematic reviews (PROSPERO 2016:CRD42016037666). A literature search of six biomedical electronic databases (Ovid MEDLINE, EMBASE, The Cochrane Library, CINAHL, PsycINFO, and PILOTS) was conducted from database inception to November 2018. All relevant subject headings and free-text terms were used to represent PTSD AND either medical illness, OR specific medical conditions. Terms were applied to limit to randomized controlled trials (RCTs) (see Appendix for complete search strategies). Ongoing studies were sought through clinicaltrials.gov and the WHO International Clinical Trials Registry Platform. Additional records were identified by scanning the reference lists of relevant studies and by employing the Similar Articles feature in PubMed and the Cited Reference Search in ISI Web of Science. The searches were not limited by language.
Eligibility criteria
To be eligible for this review, studies had to fulfill the following inclusion criteria: (1) randomized design; (2) include patients with PTSD symptoms induced by medical events including a diagnosis of a life-threatening illness; and (3) include patients over age 18. The exclusion criteria were: (1) studies that examined PTSD secondary to being a caregiver; and (2) studies that examined PTSD induced by a non-medical event which resulted in medical conditions (e.g., burns from a fire or combat-related injuries). Studies that included a mixed population of patients (i.e., those with PTSD induced by a medical event and those with PTSD induced by other causes) were also excluded unless the medical event-induced PTSD group could be analyzed separately. Two investigators from the study team, who were either physicians or psychologists, assessed study eligibility based on abstract and then full text review, with consensus achieved with a third author at each step of the review.
Data extraction
Two investigators independently extracted data from the eligible studies. Key data extracted included: the title of the study, the first author, the year and country of publication, the study sample size, the demographic characteristics of the study sample (age, gender, race, marital status, and education level), the description of the PTSD intervention, the description of the control group, the duration of the trial, the diagnostic tool used to assess PTSD symptoms, and the intervention effect estimates on PTSD symptoms or diagnosis. When necessary information was not reported in the study, we attempted to contact the authors for further details.
Quality evaluation
The quality of each study was assessed using the Cochrane Risk of Bias Assessment Tool for RCTs [31]. This tool assesses quality by examining six domains of bias: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Each study was classified as either low risk of bias, high risk of bias, or unclear risk of bias in each of these domains by two independent investigators. Discrepancies were resolved by consensus.
Statistical analysis
When the outcome was differences in PTSD symptoms between intervention and control groups, means and standard deviations (SDs) for each arm were extracted. If SD was not available, we calculated it using the sample size and confidence intervals (CIs).
Results
Literature search
Figure 1 shows the flow of the literature search and selection strategy used in the systematic review. A total of 4,485 studies were identified, of which four duplicates were removed. 223 studies were selected for full-text review after screening titles and abstracts, of which 217 were excluded. Six articles were ultimately included in the systematic review.
Figure 1.
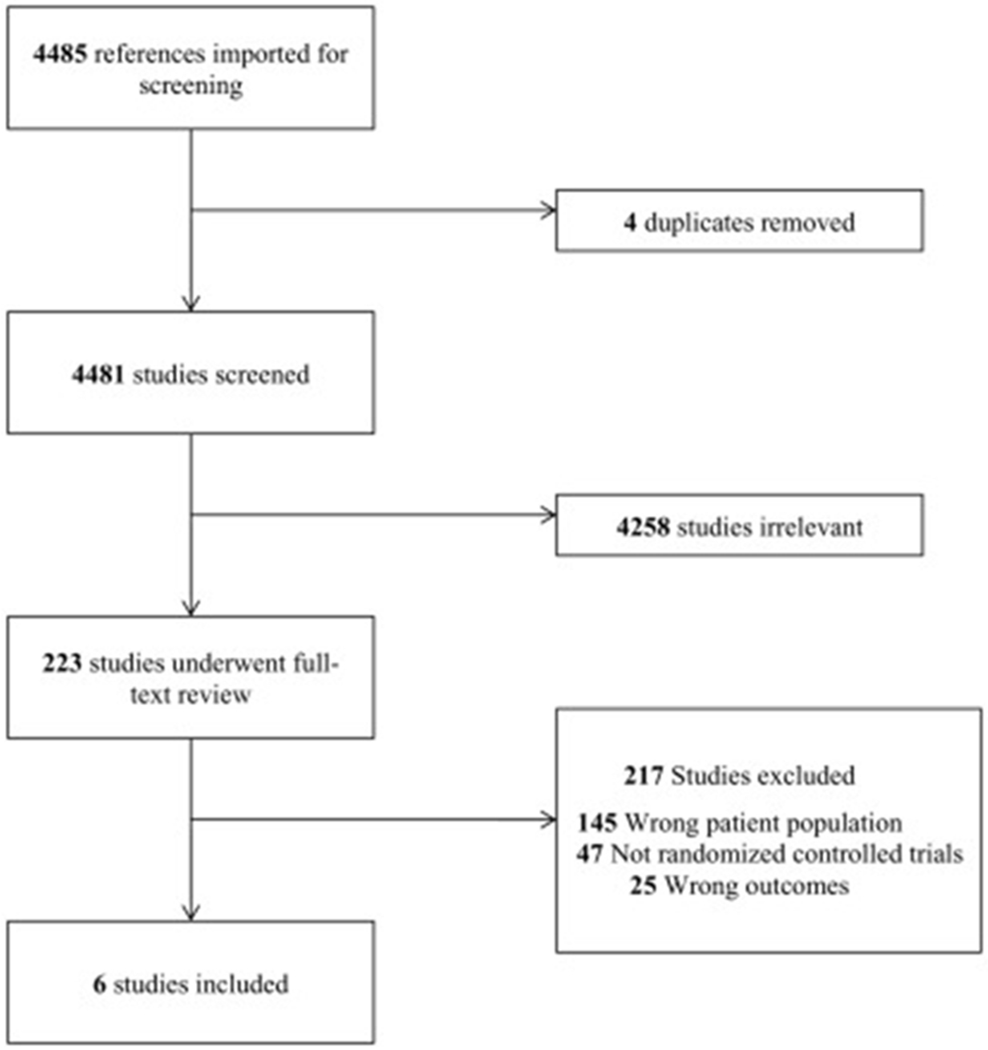
Flowchart of the systematic literature review.
Several noteworthy studies did not meet full eligibility criteria based on their study design. A study by Shemesh and colleagues assessed the effect of CBT in patients with PTSD after myocardial infarction and found that CBT was associated with a reduction in PTSD symptoms [32]. This study was excluded, however, as it used a pre-post design and did not randomly allocate participants to a comparator group. Additionally, a study by Jordan and colleagues examined a multimodal psychotherapeutic intervention, which included CBT, EMDR, and psychoeducation, for patients who experienced electric storm induced-PTSD from their implantable cardioverter defibrillator [33]. However, this article was a feasibility study without randomization or a control group and was therefore excluded. Several other studies examined diverse and interesting interventions, including intensive care unit diaries, lipophilic beta blockers in patients with shocks from their implantable intracardiac defibrillators, and light versus heavy sedation in the intensive care unit, but they were not included in this review given they were not randomized controlled trials [34, 35, 36].
Characteristics of included studies
The six eligible articles were all RCTs investigating the efficacy of psychological interventions designed to treat medical event-induced PTSD. Table 1 summarizes the characteristics of the studies. The sample sizes ranged from 21 to 81 patients. Patients were included based on the presence of PTSD symptoms due to medical illness; these symptoms were assessed in different ways, ranging from self-report scales to diagnostic interviews with clinicians. The medical illnesses that led to PTSD symptoms included: acute cardiac events (2), HIV diagnosis (1), cancer diagnosis (1), stem cell transplantation for hematologic or lymphoid malignancy (1), and progressive or relapsing-remitting multiple sclerosis (1).
Table 1.
Characteristics of Included Studies
| Source | Country | Medical illness of patients | PTSD inclusion at baseline | n | Treatments studied | No. of sessions; format | Outcome assessor | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Arabia et al. (2011) | Italy | Cardiac event | IES-R > 22 | 42 | EMDR vs. IE | 8 sessions by a doctoral- level therapist | IES-R | Post intervention-6 months |
| Capezzani et al. (2013) | Italy | Cancer | DSM-IV criteria | 21 | EMDR vs. CBT | 8 sessions by a psychotherapist | CAPS, IES-R | 1 month |
| Carletto et al. (2016) | Italy | Multiple Sclerosis | DSM-IV criteria | 42 | EMDR vs. RT | 10 sessions by a clinician or psychotherapist | CAPS, IES-R | 6 months |
| DuHamel et al. (2010) | US | Stem cell transplant | PCL-C +/− PTSD symptoms on the BSI | 81 | CBT vs. assessment only control | 10 telephone sessions by a post-doctoral fellow | PCL-C | 6 months-12 months |
| Pacella et al. (2012) | US | HIV | PDS | 43 | PE vs. assessment. Only control | 10 sessions by a post-doctoral fellow | PSS-I | Post intervention-3 months |
| Shemesh et al. (2011) | US | Cardiac event | DSM-IV criteria | 51 | IE vs. attention control | 3-5 sessions by a psychiatrist or psychologist | IES, PDS | Post intervention |
Note. Abbreviations: IES-R, Impact of Events Scale-Revised; DSM, Diagnostic Statistical Manual of Mental Disorders; PCL-C, PTSD Checklist-Civilian Version; BSI, Brief Symptom Index; PDS, Posttraumatic Diagnostic Scale; CAPS, Clinician Administered PTSD Scale; PSS-I, PTSD Symptom Scale-Interview; IE, Imaginal Exposure; RT, Relaxation Therapy
Three trials tested the efficacy of types of exposure-based CBT (conventional CBT, prolonged exposure, and imaginal exposure) versus a control group (assessment-only groups or educational attention control sessions). Three trials compared EMDR with other active treatments (imaginal exposure, conventional CBT, and relaxation therapy). The number of treatment sessions provided in the studies ranged from 3 to 10 sessions over 4 to 16 weeks. The studies utilized follow-up periods ranging from immediately post-intervention (4 weeks) to 12 months later. Additionally, the studies measured PTSD symptoms in several different ways. Some studies used the Clinician-Administered PTSD Scale (CAPS), a semi-structured diagnostic interview, whereas others used self-report symptom questionnaires, including the original and revised versions of the Impact of Event Scale (IES, IES-R), the PTSD Symptom Scale Interview (PSS-I), the PTSD Checklist-Civilian Version (PCL-C), and the Posttraumatic Stress Diagnostic Scale (PDS).
Risk of bias assessment
The six articles varied in terms of risk of bias (Table 2). Several common potential sources of bias were identified. Blinding of participants was not possible given the nature of the psychological interventions, as participants knew whether they were receiving EMDR, CBT, or no therapy. Blinding of outcome assessors was also frequently not possible given the participants themselves were the assessors on self-report questionnaires. Additionally, in the case of studies evaluating EMDR, two out of the three were published in specialty journals focused on this treatment modality.
Table 2.
Risk of Bias of Included Studies
| Study | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | |
|---|---|---|---|---|---|---|---|
| Random Sequence Generation | Allocation Concealment | Blinding of participants and personnel | Blinding of outcome assessors | Incomplete outcome data | Selective outcome reporting | Other risk of bias | |
| Arabia (2011) | Unclear | Unclear | High | Unclear | Low | Low | Unclear |
| Capezzani (2013) | Unclear | Unclear | High | Unclear | Low | Low | Unclear |
| Carletto (2016) | Low | Unclear | High | Low | High | Low | Unclear |
| DuHamel (2010) | Low | Low | High | Unclear | Low | Low | Low |
| Pacella (2012) | Low | Low | High | Low | High | Low | Low |
| Shemesh (2011) | Low | Low | High | High | Low | High | Low |
Efficacy of exposure-based CBT versus control
Three studies compared the efficacy of a type of exposure-based CBT versus a control group (Figure 2) [12, 37, 38]. The study by DuHamel and colleagues [36] tested telephone-administered CBT versus an assessment-only condition in patients with PTSD related to hematopoietic stem cell transplantation for hematologic or lymphoid malignancy. Eighty-nine patients were enrolled in the study, and 5.8% of eligible patients declined to participate. Ten CBT sessions were administered over a period of 10 to 16 weeks. The sessions were administered by postdoctoral psychology research fellows trained in CBT who were supervised by senior CBT clinicians. The intervention sessions focused on psychoeducation regarding illness-related PTSD symptoms and CBT, self-monitoring of maladaptive beliefs, guided exposure to cues associated with PTSD symptoms, communication skills training, and relaxation training. Eight patients dropped out of the study (9.0%). The mean number of sessions attended by the patients was 8.36 out of 10 (SD = 3.27). Post-intervention, the patients in the CBT group had significantly lower PCL-C scores compared to the patients in the control group (MCBT=28.34, Mcontrol = 33.03, p=.02). Additionally, the patients in the CBT group had significantly lower scores on the PCL-C subscales of intrusive thoughts (MCBT = 8.62, Mcontrol = 10.36, p=.01) and avoidance (MCBT = 2.98, Mcontrol = 4.13, p<001), but not on the subscales of hyperarousal or numbing. Also, at the 12-month follow up, the CBT group was associated with lower odds of PTSD diagnosis than the control group (OR = 1.07, 95% CI 1.01 – 2.41, p = .04).
The study by Pacella and colleagues [38] randomized patients with elevated HIV-induced PTSD symptoms to prolonged exposure versus a weekly monitoring/wait list control group. Fifty-eight patients were enrolled in the study, and the refusal rate was not reported. Ten prolonged exposure sessions were administered biweekly over five weeks. The sessions were conducted by two psychology post-doctoral fellows who received training and were supervised by experts in prolonged exposure. Therapy sessions followed standard prolonged exposure protocol [39] and focused on education about common reactions to trauma, breathing retraining, repeated imaginal exposure to the traumatic event, repeated in-vivo exposure to situations encountered in daily life that were avoided due to the traumatic memory, and discussion of negative posttraumatic cognitions. The patients in the weekly monitoring/wait list control group continued with usual care and were also contacted once per week for five weeks to monitor symptoms. Fifteen patients dropped out of the study (26.0%), all in the prolonged exposure group, leading to a sample size of 43 patients. The patients in the prolonged exposure group experienced a greater decrease in HIV-related PSS-I scores compared to the patients in the control group, both immediately post-intervention and at 3-month follow-up (MPE = 8.30, Mcontrol = 24.13, p < .001 and MPE = 7.32, Mcontrol = 20.46, p < .001, respectively).
The study by Shemesh and colleagues [12] examined patients with PTSD symptoms due to a cardiovascular event, including myocardial infarction, cardiac catheterization, coronary artery bypass graft, angioplasty, cardiac stenting, pacemaker insertion, stroke, or heart valve replacement. These patients were randomized to three to five sessions of imaginal exposure or to a control group that included one to three educational sessions on medication adherence. Sixty patients were enrolled in the study, and 1.6% of eligible patients refused participation in the study. Imaginal exposure sessions were administered by a licensed psychiatrist or psychologist trained in trauma-focused CBT. They were monitored by a doctoral-level study coordinator who determined treatment fidelity to be above 90%. Nine patients dropped out of the study (15.0%), leading to a final sample size of 51 patients. This study did not publish quantitative data on psychiatric outcomes separately by group given that it was a small study and was underpowered to detect treatment effects. However, the authors noted that PTSD symptoms (as measured on the IES) improved more in the imaginal exposure group compared to the control group, although this difference was not statistically significant.
Efficacy of EMDR versus active treatments
Three studies compared EMDR with an active treatment [40, 41, 42]. A study by Arabia and colleagues compared EMDR with imaginal exposure in patients with PTSD induced by life-threatening cardiac events, including cardiac surgery, myocardial infarction, and cardiac arrest [40]. Forty-two patients were enrolled in this study. The refusal rate was not reported. Ten sessions of EMDR or imaginal exposure were delivered to the patients over a period of five weeks. Treatments were carried out by the same doctoral-level therapist with training in both forms of treatment. The therapist was a certified EMDR supervisor, and no fidelity checks were conducted by outside evaluators. Imaginal exposure fidelity was evaluated by an expert and was found to be satisfactory. EMDR treatment used eye movement tracking while addressing memories of the cardiac event and associated triggers, as well as anticipatory anxiety related to future incidents. No between-session homework was assigned. Imaginal exposure sessions consisted of the participants visualizing the traumatic event and recounting it out loud. However, no processing of the imaginal exposure was conducted, and no homework (e.g., at-home daily imaginal exposure) was assigned. Eight patients dropped out of the study after the one-month follow up, but before the six-month follow up (19.1%). In this study, EMDR was associated with significantly lower PTSD symptoms compared to imaginal exposure at 5 weeks and 6 months, as measured by the IES-R (5 weeks: MIE = 19.67, MEMDR = 12.10, p = .002; 6 months: MIE = 13.64, MEMDR= 7.95, p = .03, respectively).
The pilot study by Capezzani and colleagues [40] tested EMDR versus CBT in patients with PTSD symptom due to various types of cancer, including breast, colon, uterus, thyroid, melanoma, lung, and stomach cancer. Twenty-one patients were enrolled in this study. No eligible patients refused participation. Patients in this study received eight weekly treatment sessions. EMDR and CBT sessions were provided by the same psychotherapist who was experienced in both techniques. EMDR treatments used eye movement tracking and focused on psychoeducation, identification and reprocessing of disturbing cancer memories, and reduction of distress. CBT treatments varied depending on the presenting PTSD symptoms of each patient but could include a combination of visualization, imaginal and/or in vivo exposure, relaxation techniques, cognitive restructuring, shifting of attention techniques, and maintenance of new behavioral patterns. There was no attrition at follow up. This study found that the IES-R scores at 1-month posttreatment were significantly lower in the EMDR group compared to the CBT group (MCBT = 46.60, MEMDR = 20.55, p = .002). Additionally, the EMDR group scored significantly lower on the CAPS Criterion B subscale (intrusion) posttreatment compared to the CBT group (MCBT = 15.30, MEMDR = 6.18, p = .004). There were no significant posttreatment differences between the EMDR and CBT groups on the CAPS Criterion C subscale (avoidance) or Criterion D subscale (hyperarousal).
The study by Carletto and colleagues [41] randomized patients with PTSD symptoms related to progressive or relapsing-remitting multiple sclerosis. The patients were randomized to either EMDR or relaxation therapy. Fifty patients were enrolled in the study, and 21.2% of eligible patients refused to participate. All patients received 10 sessions over 12 to 15 weeks. EMDR sessions were administered by three experienced clinicians supervised by a certified senior EMDR instructor. EMDR sessions used eye movement tracking and focused on stabilization techniques and recall of traumatic images related to the illness. Relaxation therapy was administered by two experienced psychotherapists (MSc or higher). Relaxation treatment included visualization, diaphragmatic breathing, and progressive muscle relaxation. Eight patients dropped out of the study (16.0%), leading to a sample size of 42 patients. There were no significant differences in PTSD symptoms (as measured on the CAPS and IES-R) between the two groups at 6 months. However, PTSD remitted in a greater proportion of patients in the EMDR group than in the relaxation therapy group after 6 months [5/22, 22.7% versus 0/20, 0%; p=.05).
Discussion
Our systematic review found that there were relatively few RCTs investigating treatment of medical event-induced PTSD. We identified only six RCTs that tested psychotherapy interventions, and none that evaluated pharmacotherapy or other types of treatment. There were two notable findings from our review of eligible trials: (1) exposure-based CBT interventions were associated with significantly lower PTSD symptoms posttreatment compared to control groups, and (2) EMDR may be superior to other active treatments, although the strength of evidence for this finding was viewed as weak. These studies included patients with PTSD induced by several different medical events, including cardiac events, cancer, HIV, and neurologic disease. There were no studies examining treatment of patients with PTSD secondary to critical illness requiring intensive care unit stays and mechanical ventilation, even though there are a growing number of articles showing a high prevalence of elevated PTSD symptoms in this patient population [43, 44]. The included studies tested several types of CBT (including conventional CBT, prolonged exposure, imaginal exposure), as well as EMDR.
Guidelines generally recommend trauma-focused psychotherapy as first-line treatment for PTSD [16]. The Department of Veterans Affairs (VA) recommends trauma-focused psychotherapy over pharmacotherapy, specifically endorsing prolonged exposure, cognitive processing therapy, CBT, and EMDR [17]. The American Psychological Association (APA) strongly recommends CBT, cognitive therapy, and prolonged exposure therapy, and suggests the use of EMDR, in treating PTSD patients [18]. A meta-analysis by Watts and colleagues concluded that cognitive therapy, exposure therapy and EMDR were all effective in treating PTSD, with large effect sizes (g=1.63, 1.08. and 1.01), respectively [17]. Our systematic review suggests that these therapies are also effective in treating PTSD symptoms due to medical events. The effect size in this patient population is not known because the significant amount of heterogeneity between the studies prevented us from pooling their data. Further studies are needed to estimate how effective these treatments are in this patient population, and if other distinct treatments are needed.
Limitations
There were several limitations to this systematic review. There were few RCTs on this topic, and those that were published had small sample sizes. The studies included in this review varied in terms of risk of bias. In addition, the studies frequently assessed PTSD symptoms by self-report questionnaires rather than by diagnostic interviews. Given that patients were unblinded, the patients knew if they were receiving EMDR, CBT, or a control group, and this may have caused them to underreport or overreport PTSD symptoms. There is also the question of how many patients with PTSD symptoms also had other psychiatric comorbidities such as depression and anxiety, and how these may have affected the results. There was variability in the duration of follow-up, ranging from immediately post-intervention to 12 months afterwards. This limited the understanding of the sustained response of any treatment effects over time. Finally, there was a substantial degree of heterogeneity among the studies that prevented pooling of the data. The studies differed in terms of the medical illnesses of the patients included, and it is possible that the effectiveness of a treatment varies according to the type of medical event (i.e., cardiac arrest versus cancer diagnosis). There was also heterogeneity in terms of the interventions tested, the control groups utilized, and the measures of PTSD symptoms. In particular, two of the three studies compared CBT with an assessment-only control group; the lack of an attention control limited the interpretability of the active ingredients in the CBT interventions.
Given the substantial number of patients with medical event-induced PTSD symptoms, larger RCTs are needed to determine more conclusively whether trauma-focused psychotherapy interventions should be recommended for treating PTSD symptoms induced by medical events. The field would also benefit from interviewing those with medical event-induced PTSD symptoms to learn their preferences for therapy for this condition. Given that the traumatic medical events often occur in the medical setting (e.g., presenting to the emergency department with these events, prolonged hospital stays for treatment of these events), there may be unique opportunities to intervene more rapidly to prevent the onset of PTSD in the first place.
Conclusions
The optimal treatment of PTSD symptoms induced by medical events remains unclear. This systematic review demonstrates that well-designed RCTs of evidence-based treatments are still needed in this patient population. The results from the few existing trials suggest that types of exposure-based CBT (including conventional CBT, prolonged exposure, and imaginal exposure) and EMDR may be effective in treating PTSD symptoms due to medical events. Given the small number of studies evaluating treatments in this patient population, there is a need for further research on the efficacy of psychotherapy in those with medical event-induced PTSD symptoms.
Supplementary Material
Highlights.
Medical event-induced PTSD has been described in several patient populations
Few trials exist that investigate treatments for PTSD symptoms induced by medical events
In this systematic review, both cognitive behavioral therapy and eye movement desensitization and reprocessing were associated with decreased PTSD symptoms
Acknowledgments:
This work was supported by the National Heart, Lung, and Blood Institute (R01 HL123368, R01 HL117832, and R01 HL132347).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests Statement
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf and the authors have no competing interests to report.
References
- [1].American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- [2].Kutz I, Garb R, & David D (1988). Post-traumatic stress disorder following myocardial infarction. Gen Hosp Psychiatry, 10, 169–76. [DOI] [PubMed] [Google Scholar]
- [3].Shalev AY, Schreiber S, Galai T, & Melmed RN (1993). Post-traumatic stress disorder following medical events. Br J Clin Psychol., 32, 247–53. [DOI] [PubMed] [Google Scholar]
- [4].Vilchinsky N, Ginzburg K, Fait K, & Foa EB (2017). Cardiac-disease-induced PTSD (CDI-PTSD): A systematic review. Clin Psychol Rev., 55, 92–106. [DOI] [PubMed] [Google Scholar]
- [5].American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- [6].Kutz I, Shabtai H, Solomon Z, Neumann M, & David D (1994). Post-traumatic stress disorder in myocardial infarction patients: prevalence study. Isr J Psychiatry Relat Sci., 31, 48–58. [PubMed] [Google Scholar]
- [7].Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, et al. (2012). Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One., 7, e38915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Edmondson D, Richardson S, Fausett JL, Falzon L, Howard VJ, et al. (2013). Prevalence of PTSD in survivors of stroke and transient ischemic attack: a meta-analytic review. PLoS One., 8, e66435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Smith MY, Redd WH, Peyser C, & Vogl D (1999). Post-traumatic stress disorder in cancer: a review. Psychooncology, 8, 521–537. [DOI] [PubMed] [Google Scholar]
- [10].Kangas M (2013). DSM-5 Trauma and Stress-Related Disorders: Implications for Screening for Cancer-Related Stress. Front Psychiatry, 4, 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cordova MJ, Riba MB, Spiegel D (2017). Post-traumatic stress disorder and cancer. Lancet Psychiatry, 4, 330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Shemesh E, Annunziato RA, Weatherley BD, Cotter G, Feaganes JR, et al. (2011). A randomized controlled trial of the safety and promise of imaginal exposure in patients with posttraumatic stress disorder resulting from cardiovascular illness. J Clin Psychiatry, 72, 168–174. [DOI] [PubMed] [Google Scholar]
- [13].Edmondson D, Rieckmann N, Shaffer JA, Schwartz JE, Burg MM, et al. (2011). Posttraumatic stress due to an acute coronary syndrome increases risk of 42-month major adverse cardiac events and all-cause mortality. J Psychiatr Res., 45, 1621–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kronish IM, Edmondson D, Goldfinger JZ, Kezhen F, & Horowitz CR (2012). Post-traumatic stress disorder and adherence to medications in survivors of stroke and transient ischemic attacks. Stroke, 43, 2192–2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Boarts JM, Sledjeski EM, Bogart LM, & Delahanty DL (2006). The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS Behav., 10, 253–61. [DOI] [PubMed] [Google Scholar]
- [16].Institute of Medicine (IOM). (2008). Treatment of posttraumatic stress disorder: an assessment of the evidence. Washington, DC: The National Academies Press. [Google Scholar]
- [17].Department of Veterans Affairs / Department of Defense (VA/DOD). (2017). VA/DOD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder.
- [18].American Psychological Association. (2017). Clinical practice guideline for the treatment of PTSD. Washington, DC: American Psychological Association. [Google Scholar]
- [19].Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, et al. (2016). Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systematic review and meta-analyses to determine first-line treatment. Depress Anxiety, 33, 792–806. [DOI] [PubMed] [Google Scholar]
- [20].Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, et al. (2013). Meta-analysis on the efficacy of treatments for posttraumatic stress disorder. J Clin Psychiatry, 74, e541–50. [DOI] [PubMed] [Google Scholar]
- [21].Bisson J & Andrew M (2007). Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Syst Rev., 3. [DOI] [PubMed] [Google Scholar]
- [22].Davidson PR & Parker KC (2001). Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol, 2, 305–316. [DOI] [PubMed] [Google Scholar]
- [23].Levi O, Bar-Haim Y, Kreiss Y, & Fruchter E (2015). Cognitive-behavioral therapy and psychodynamic psychotherapy in the treatment of combat-related post-traumatic stress disorder: a comparative effectiveness study. Clin Psychol Psychother., 23, 298–307. [DOI] [PubMed] [Google Scholar]
- [24].Markowitz JC, Petkova E, Neria Y, Van Meter PE, Zhao Y, et al. (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. Am J Psychiatry, 172, 430–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Edmondson D (2014). An enduring somatic threat model of posttraumatic stress disorder due to acute life-threatening medical events. Soc Personal Psychol Compass, 8, 118–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Moye J & Rouse SJ (2015). Posttraumatic stress in older adults: when medical diagnoses or treatments cause traumatic stress. Psychiatr Clin North Am., 38, 45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kangas M, Henry JL, & Bryant RA (2002). Posttraumatic stress disorder following cancer: a conceptual and empirical review. Clin Psychol Rev, 22, 499–524. [DOI] [PubMed] [Google Scholar]
- [28].Abbey G, Thompson SB, Hickish T, & Heathcote D (2015). A meta-analysis of prevalence rates and moderating factors for cancer-related posttraumatic stress disorder. Psychooncology, 24, 371–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Tedstone JE & Tarrier N (2003). Posttraumatic stress disorder following medical illness and treatment. Clin Psychol Rev, 23, 409–448. [DOI] [PubMed] [Google Scholar]
- [30].Birk J, Sumner JA, Haerizadeh M, Heyman-Kantor R, Falzon L, Gonzalez C, et al. (2019). Early interventions to prevent posttraumatic stress disorder symptoms in survivors of life-threatening medical events: A systematic review. J Anxiety Disord, 64, 24–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Higgins JPT & Green S Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 http://handbook.cochrane.org.
- [32].Shemesh E, Koren-Michowitz M, Yehuda R, Milo-Cotter O, Murdock E, et al. (2006). Symptoms of posttraumatic stress disorder in patients who have had a myocardial infarction. Psychosomatics, 47, 231–239. [DOI] [PubMed] [Google Scholar]
- [33].Jordan J, Titscher G, Peregrinova L, & Kirsch H (2013). Manual for the psychotherapeutic treatment of acute and posttraumatic stress disorders following multiple shocks from implantable cardioverter defibrillator (ICD). Psychosoc Med., 10 Doc09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Aitken LM, Rattray J, Hull A, Kenardy JA, Brocque RL et al. (2013). The use of diaries in psychological recovery from intensive care. Critical Care, 17, 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Bhuvaneswar CG, Ruskin JN, Katzman AR, Wood N, & Pitman RK (2014). Pilot Study of the effect of lipophilic versus hydrophilic beta-adrenergic blockers being taken at the time of intracardiac defibrillator discharge on subsequent PTSD symptoms. Neurobiol Learn Mem, 112, 248–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Croxall C, Tyas M, & Garside J (2014). Sedation and its psychological effects following intensive care. British Journal of Nursing, 23, 800–804 [DOI] [PubMed] [Google Scholar]
- [37].DuHamel KN, Mosher CE, Winkel G, Labay LE, Rini C et al. (2010). Randomized clinical trial of telephone-administered cognitive-behavioral therapy to reduce post-traumatic stress disorder and distress symptoms after hematopoietic stem-cell transplantation. J Clin Oncol., 28, 3754–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Pacella ML, Armelie A, Boarts J, Wagner G, Jones T et al. (2012). The impact of prolonged exposure on PTSD symptoms and associated psychopathology in people living with HIV: a randomized test of concept. AIDS Behav., 16, 1327–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Foa EB, Rothbaum BO, Riggs DS, and Murdock TB (1991). Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive behavioral procedures and counseling. J Consult Clin Psychol, 59, 715–23. [DOI] [PubMed] [Google Scholar]
- [40].Arabia E, Manca ML, & Solomon RM (2011). EMDR for survivors of life-threatening cardiac events: results of a pilot study. J EMDR Pract Res, 5, 2–13. [Google Scholar]
- [41].Capezzani L, Ostacoli L, Cavallo M, Carletto S, Fernandez I et al. (2013). EMDR and CBT for cancer patients: comparative study of effects on PTSD, anxiety, and depression. J EMDR Pract Res., 7, 134–43. [Google Scholar]
- [42].Carletto S, Borghi M, Bertino G, Oliva F, Cavallo M et al. (2016). Treating post-traumatic stress disorder in patients with multiple sclerosis: a randomized controlled trial comparing the efficacy of eye movement desensitization reprocessing and relaxation therapy. Front Psychol., 7, 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Bienvenu OJ & Gerstenblith TA (2017). Posttraumatic stress disorder phenomena after critical illness. Crit Care Clinics, 33, 649–658. [DOI] [PubMed] [Google Scholar]
- [44].Svenningsen H, Egerod I, Christensen D, Tonnesen EK, Frydenberg M, et al. (2015). Symptoms of posttraumatic stress after intensive care delirium. Biomed Res Int., 876947. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


