Abstract
Background: Retrograde intrarenal surgery (RIRS) has emerged as a viable and safe option for renal stones <2 cm. Because of its high efficiency and relative safety, experienced endourologists have applied it to even larger stones. We present a case of arteriocaliceal fistula, which is a rare postoperative complication of RIRS.
Case Presentation: A 52-year-old man with a rich history of endourologic procedures and extracorporeal shockwave lithotripsy caused by inferior caliceal calculi was subjected to RIRS. This was complicated by transient intraoperative hemorrhage, followed by recurrent hematuria and clot retention several days postoperatively. Renal arteriography revealed the presence of an arteriocaliceal fistula. This was completely resolved with selective arterial embolization.
Conclusion: This case highlights that early detection and timely intervention are crucial to avoid serious consequences of post-RIRS hemorrhage resulting from arteriocaliceal fistula.
Keywords: urology, endourology, nephrolithiasis, surgical complication, retrograde intrarenal surgery
Introduction and Background
The endoscopic management of renal stone disease has evolved over the years. Initially, it was limited to percutaneous nephrolithotomy (PCNL) which was shown to be efficacious and safe for stones >2 cm. More recently, retrograde intrarenal surgery (RIRS) was introduced and became a safe alternative for smaller stones measuring 1–2 cm, which were recalcitrant to extracorporeal shockwave lithotripsy (SWL) therapy.1
As more endourologists gained experience with RIRS, they eventually applied it to even larger stones >2 cm, achieving yet a stone-free rate of 91% with a mean of 1.45 procedures per patient. This success rate was similar among several countries with different economic profiles (developed and underdeveloped).
The complication rates associated with RIRS range between 9% and 25%, but the vast majority are low grade (Clavien–Dindo I and II) and self-limited, rarely requiring further interventions. High-grade complications are rare (<1%) and are usually associated with ureteral avulsion and sepsis.2
Case Report
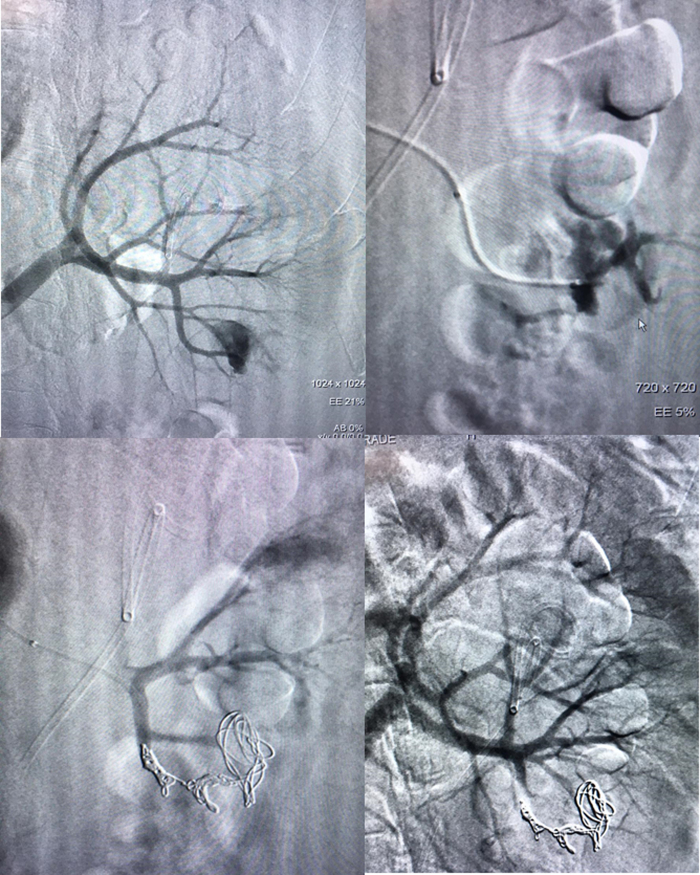
A 52-year-old male patient, without clinical comorbidities, presented with a rich medical history of nephrolithiasis. He had undergone a PCNL 19 years ago, followed by four RIRS procedures and several SWLs. During case evaluation, an abdominal CT scan (Fig. 1) revealed an inferior caliceal calculus measuring 1.6 cm at the lower pole of the left kidney and RIRS was performed. First, we performed a left ureteroscopy with a rigid Karl Storz 6.5–9F, 43 cm ureterorenoscope, guided by a previously introduced hydrophilic HiWire™ Nitinol (0.035”/150 cm) guidewire and a (0.035”/145 cm) Universa® Soft Roadrunner Guide Wire, which was coaxially introduced into the ureteroscope. This was followed by a retrograde pyelogram that documented the collecting system anatomy, the stone, and its location. We proceeded with ureter cannulation with a Flexor® Ureteral Access Sheath (ID: 9.5F OD: 11.5F/45 cm) that was done under continuous fluoroscopy from the bladder to the ureteropelvic junction. We used an optic Karl Storz Flex-X2 7.5F uretero-reno-fiberscope to access the collecting system and the OptiLite™ 273 μm Single Use Holmium Laser Fiber connected to an Odyssey 30™ Holmium Laser System to fragment the stones. Dusting fragmentation mode was used and parameters of the laser were set ranging from 8 to 12 Hz of frequency, 0, 8–1 J energy, and pulse duration of 750 μm.
FIG. 1.
Left kidney lower pole stone.
After partial fragmentation of the stone that was obstructing the lower calix, a larger mass of smaller stones was identified. Unfavorable caliceal anatomy (acute infundibulopelvic angle and a narrow infundibulum) resulted in additional technical difficulties. After 120 minutes of laser lithotripsy and several maneuvers trying to basket the stones, the procedure was stopped because of excessive bleeding.
A Universa Soft Ureteral Stent (4.7F/22–32 cm) with hydrophilic coating was introduced through the guidewire, and its correct position was confirmed by radioscopy. A three-way indwelling Foley catheter was installed with continuous saline irrigation. The patient was discharged on the first postoperative day (POD) without hematuria and with spontaneous satisfactory micturition after removal of the catheter.
The patient presented to the emergency department on the fifth POD with fever, hematuria, and acute urinary retention. Urinalysis revealed urinary tract infection, and intravenous antibiotic therapy (ceftriaxone) was started, followed by cystoscopy. No active bleeding was identified during the procedure and the intravesical clots were completely evacuated. We opted not to use a Foley catheter.
Despite these measures, the patient persisted with hematuria and presented with a new episode of acute urinary retention, which was resolved after bedside aspiration of small clots through a new three-way indwelling Foley catheter followed by continuous bladder irrigation with saline.
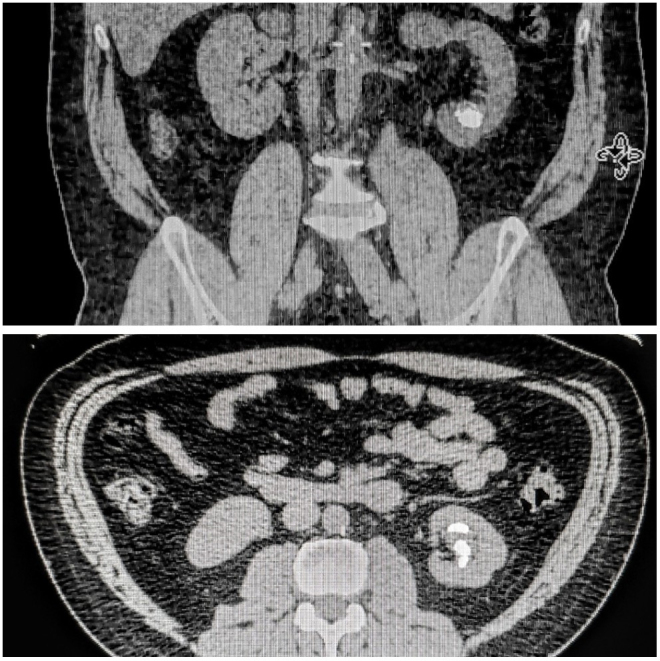
Arteriography was performed to investigate vascular lesions, and showed an arteriocaliceal fistula (Fig. 2), which was treated with superselective artery embolization by an interventional radiologist. No further procedures or blood transfusions were required. Patient hemoglobin levels decreased from 12.39 to 10.9 g/dL in 2 days, from the admission to the definitive procedure. He was discharged from the intensive care unit on the next day with mild hematuria. An ultrasound scan ruled out residual clots and he was discharged from the hospital 2 days after the procedure, with removal of the Foley catheter. The ureteral stent was removed after 15 days and the patient remains without further complaints so far.
FIG. 2.
Arteriography showing arteriocaliceal fistula followed by ultraselective embolization with spring.
Discussion
Vascular complications after RIRS have been previously described in the literature, most of them regarding hematuria (usually self-limited) and perirenal hematomas. Some of the reported cases were life threatening and additional surgical procedures were often required, including superselective embolization and even nephrectomy. We found only one previous case report of arteriovenous fistula, which was treated with coil embolization, and no case of arteriocaliceal fistula after RIRS has been reported so far.3
Vascular fistulae to the collecting system (arterio-pyelic or arteriocaliceal) are rare and may occur after invasive and complex urologic procedures, such as kidney transplant or percutaneous lithotripsy. Contributing factors to fistulae formation include iatrogenic lesions and increased pressure inside the collecting system, leading to forniceal rupture. A fatal case was described after an attempt to dilate a ureter obstruction after a renal transplant—the patient died after septic shock because of bloodstream contamination. At our best knowledge, our case is the first arteriocaliceal fistula after RIRS described in the literature.3
RIRS is a safe procedure and its complications are usually self-limited or easily manageable. However, as shown in this case and in previously reported cases, more complex outcomes can occur and even lead to life-threatening conditions.4
In our opinion, lower pole topography, history of previous surgeries that may have distorted collecting system anatomy, excessive maneuvers inside the kidney, and prolonged operative time may have led to an increased risk of significant vascular trauma in this particular case.
In addition, the abdominal CT scan shows that the stones appear to be abnormally lodged within the parenchyma of the kidney. This brings the suspicion of a pseudoaneurysm after previous procedures that may have resolved spontaneously by residual stone plugging. By this theory, the RIRS may have only unroofed the previously existing aneurysm.
Regardless of the presented case, RIRS remains a safe procedure because of laser characteristics—particularly its penetration depth of up to 1 mm. Complications as the one we described earlier are unlikely to occur.
Conclusion
We described a rare case of life-threatening complication of arteriocaliceal fistula after RIRS that was completely resolved by angioembolization. Despite its low occurrence rate, surgeons may consider vascular fistula as a differential diagnosis in patients with gross hematuria after RIRS.
Acknowledgments
The authors thank my colleague Alexandre Ziomkowski for the support during all the process of the article preparation. The authors are grateful to Dr. Breno Dauster for helping conducting the case and orientation and reviewing process. The authors are especially thankful to Dr. André Costa Matos who helped with all the reviewing and finalization process and selection of journal to publish.
Abbreviations Used
- CT
computed tomography
- PCNL
percutaneous nephrolithotomy
- POD
postoperative day
- RIRS
retrograde intrarenal surgery
- SWL
extracorporeal shockwave lithotripsy
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Silva Simões Estrela JR, Azevedo Ziomkowski A, Dauster B, Costa Matos A (2020) Arteriocaliceal fistula: a life-threatening condition after retrograde intrarenal surgery, Journal of Endourology Case Reports 6:3, 241–243, DOI: 10.1089/cren.2020.0004.
References
- 1. Türk C, Petřík A, Sarica K, et al. . EAU guidelines on diagnosis and conservative management of urolithiasis. Eur Urol 2016;69:468–474 [DOI] [PubMed] [Google Scholar]
- 2. Somani BK, Giusti G, Sun Y, et al. . Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: The Clinical Research Office of Endourological Society URS Global study. World J Urol 2017;35:675–681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cindolo L, Castellan P, Primiceri G, et al. . Life-threatening complications after ureteroscopy for urinary stones: Survey and systematic literature review. Minerva Urol Nefrol 2017;69:421–431 [DOI] [PubMed] [Google Scholar]
- 4. Cindolo L, Castellan P, Marco C, et al. . Mortality and flexible ureteroscopy: Analysis of six cases 2015. World J Urol 2016;34:305–310 [DOI] [PubMed] [Google Scholar]