Abstract
Background: Encrusted uropathy (EU) is a rare disease caused by urea-splitting bacteria, most commonly Corynebacterium urealyticum, whose incidence is increasing. Standard treatment is based on pathogen-directed antibiotic therapy, urinary diversion, bladder instillations, and surgical resection of urinary calcifications.
Case Presentation: We present the case of a 60-year-old man with symptomatic bilateral encrusted pyelitis and cystitis with acute renal failure. We initially treated the patient with antibiotic therapy, urinary diversion, and oral acidification with acetohydroxamic acid, achieving negative urinary cultures. Because of the persistence of encrusted pyelitis, the patient was discharged on oral l-methionine 500 mg bid and 12 months later the encrustations had almost disappeared. Finally, we performed right retrograde intrarenal surgery to remove a persistent small calcification.
Conclusion: Oral urinary acidification with l-methionine is a valid treatment for urinary encrustations in EU, with no complications reported. Complete resolution of the calcifications may be achieved without the need for invasive processes and unnecessary manipulation of the urinary system.
Keywords: encrusted uropathy, urinary acidification, Corynebacterium urealyticum
Introduction and Background
Encrusted uropathy (EU) is a rare disease characterized by urothelial calcification. It is associated with chronic inflammation induced by urea-splitting bacteria, most frequently Corynebacterium urealyticum (CU). The incidence of infection with CU has been increasing, as reported by Sánchez-Martín and associates1 in 2015. Although EU is related to immunosuppression and a previous history of urologic procedures, it can appear in healthy patients.
Diagnosis should be considered in the presence of sterile pyuria, alkaline urinary pH (up to 9), struvite or apatite crystalluria, and calcifications of the urinary system, which are detected primarily by CT. When EU is suspected, prolonged urine cultures should be performed (>48 hours) on special medium (Columbia blood agar in enriched CO2). There is no consensus on treatment, but multiple options have been suggested, including antibiotic therapy, urinary diversion, acidifying instillations, and calcification resection.
Urease-splitting bacteria hydrolyze urea to form ammonia and tend to increase urinary pH. There are >40 uropathogenic urease-splitting bacteria,2 CU being the most common in the context of EU. CU can be found in the skin in 12% of healthy persons and up to 30% of hospitalized patients.3 It is an opportunistic gram-positive bacterium, strictly aerobic and of slow growth. Generally it affects immunocompromised, chronically ill, or multioperated patients, whose symptoms may vary from asymptomatic bacteriuria (0.2% of urine cultures) to urologic sepsis.
When EU has developed, many local and general symptoms associated with urothelial calcification1 may appear, among which urinary obstruction and calcified pyelitis are the most common caused by the high density of urine, detachment of calcifications, urolithiasis formation, and ureteral stricture. In conjunction with interstitial edema, these conditions may lead to acute renal failure.
In this study we report the case of a patient with EU treated with chronic l-methionine as oral acidifying treatment, in whom almost complete resolution of the calcifications was achieved. As far as we know, this is the first case report in the literature to show that oral urinary acidification is a treatment option for calcifications in EU.
Case Presentation
We present the case of a 60-year-old male Caucasian patient with a history of dyslipidemia and hyperuricemia. In December 2016, urolithiasis had been diagnosed in him in another country as having bilateral kidney stones because of left nonobstructive pyelonephritis with secondary septic shock requiring transitory hemodialysis, orotracheal intubation, and vasoactive drugs. No urologic procedures had been performed.
He was referred to our center in 2018 for treatment with a former CT scan that showed bilateral kidney stones, with a stone measuring 2 cm on the right side, and left renal atrophy. Radioisotope renography revealed that the right kidney contributed 84% of total renal function, whereas the left kidney contributed only 16%. The baseline creatinine was 250 μM. The patient was placed on the waiting list for right percutaneous nephrolithotomy (PCNL).
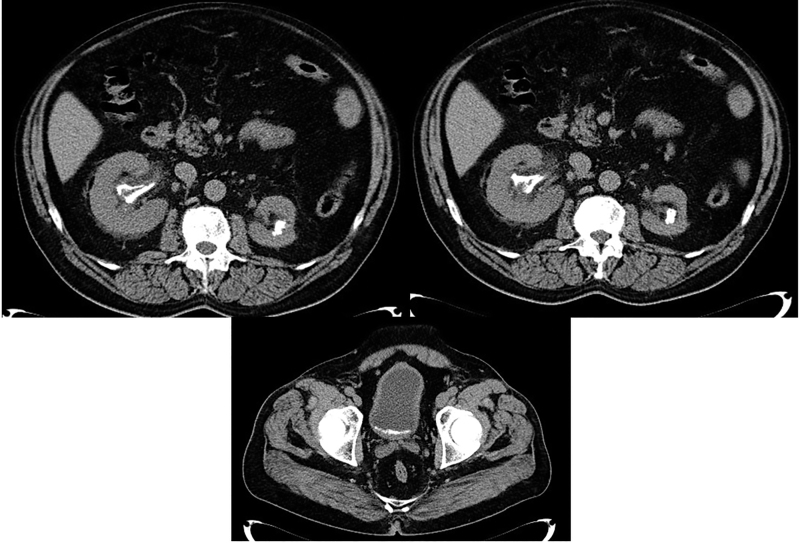
A few weeks later the patient attended the emergency department because of intense lower urinary tract symptoms and fever of 38°C without back pain. Physical examination was normal, but he presented thick mucus-like urine, with sterile pyuria and urinary pH of 8. The blood test showed acute renal insufficiency (creatinine 594 μM) and blood pH of 7.25. Neither leukocytosis nor hydronephrosis was observed. CT scan showed bilateral nonobstructive encrusted pyelitis as well as encrusted cystitis of the posterior bladder wall (Fig. 1). Based on suspicion of CU infection and an increase in the urinary pH to 8, we started oral linezolid 600 mg bid and a bladder catheter was placed. Urine culture showed >100,000 CFU/mL of CU, which is sensitive only to linezolid, vancomycin, and teicoplanin. A right 12F Mono J stent was placed to promote urinary drainage.
FIG. 1.
CT scan before treatment.
After 5 days of antibiotic therapy, renal function improved (creatinine 329 μM) although the patient had required a hemodialysis session. When normal blood pH was achieved, acidifying treatment was commenced. Oral acetohydroxamic acid, a urease inhibitor, was administered and maintained for 30 days (250 mg/24 hours) in conjunction with oral linezolid. After 2 weeks of treatment, urine culture was negative and urinary pH had fallen to 5.5. During acidifying treatment, the blood pH and magnesium were monitored with blood tests every 48 hours, with no complications reported. A right Double-J stent was placed, and the patient was discharged on oral l-methionine (one 500 mg tablet every 12 hours) before planned PCNL.
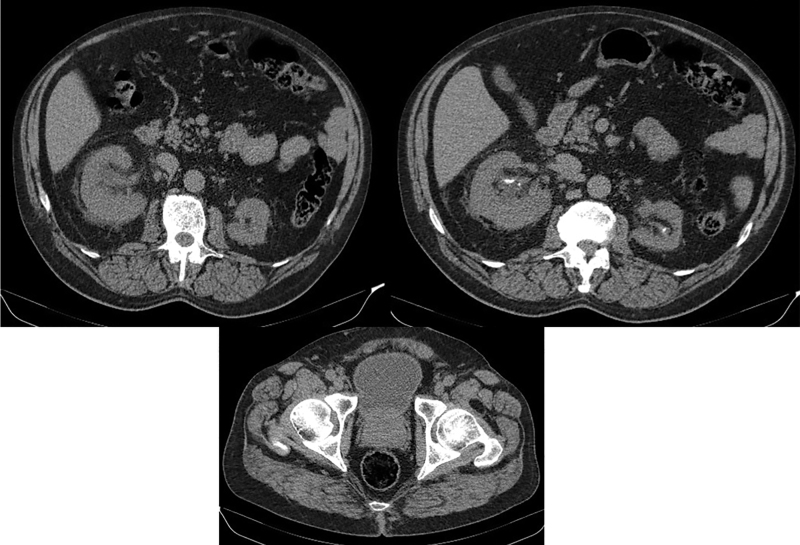
At 2 months after the initiation of l-methionine treatment, the first kidney, ureter, and bladder ultrasonography showed a substantial improvement in the encrusted pyelitis. It was decided to remove the Double-J stent and the percutaneous surgery was canceled. In consensus with the patient, and under close monitoring, oral acidification treatment was continued for a year, at which time a CT scan showed great improvement in the EU, with a residual 7-mm calcification (Fig. 2), which was finally removed by right retrograde intrarenal surgery. During this period creatinine levels were stable and urinary pH ranged between 5 and 5.5. CU was never found again.
FIG. 2.
CT scan after 1 year treatment with oral l-methionine.
Currently, the patient remains asymptomatic, without oral acidification, with negative urinary cultures and with chronic stabilized renal failure (creatinine 297 μM).
Discussion and Literature Review
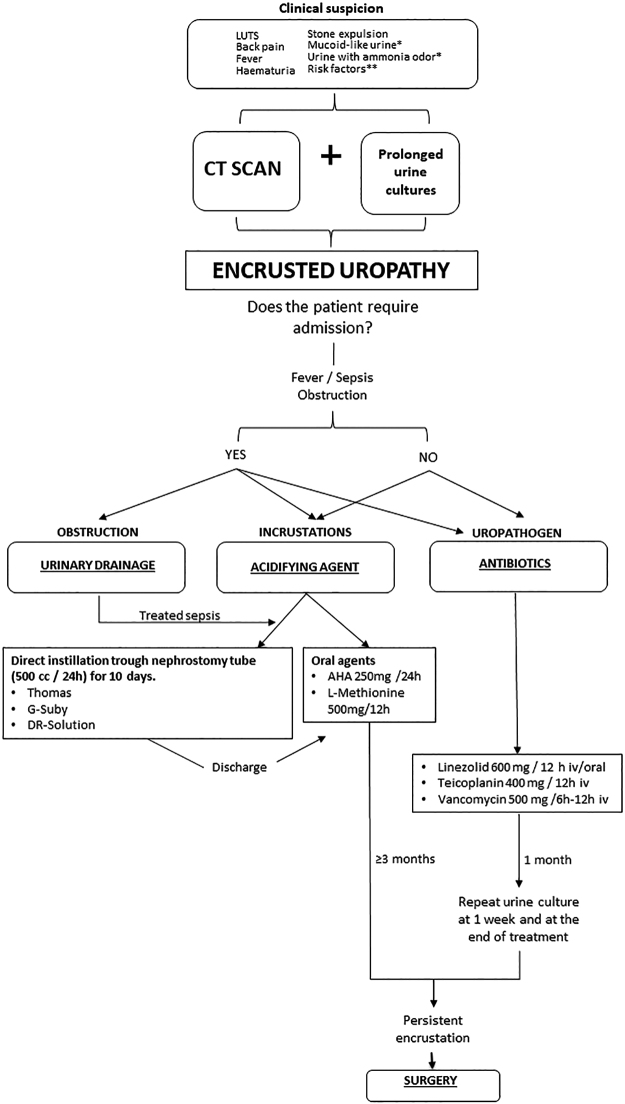
The treatment of EU because of CU infection is multimodal and many treatment options have been suggested, including antibiotic therapy, urine acidification, urinary diversion, and resection of the calcifications. Specific antibiotic therapy such as linezolid, teicoplanin, or vancomycin has been shown to normalize urine culture within the first week, with rapid patient recovery. Although antibiotic therapy alone generally halts the encrustation process, it does not reduce the already formed calcifications, which must be treated with acidifying treatment or resected. Given the increase in the incidence of EU because of CU infection, we have created a treatment guideline for EU in our center (Fig. 3).
FIG. 3.
Encrusted uropathy guideline of our center. *Highly suggestive symptoms of urease positive germs. **Immunosuppressed, hospitalized, broad spectrum antibiotic therapy, urologic pathology analysis, urologic manipulation, and catheters. AHA = acetohydroxamic acid; CU = Corynebacterium urealyticum; EU = encrusted uropathy.
One of the main challenges in the management of the EU is diagnosis and institution of early treatment. In this case we suspected EU as soon as the CT scan had been performed, and appropriately instructed our microbiology department to look for CU or other bacteria that can produce EU. Urologists must have EU in mind to carry out tests such as prolonged urine cultures that will avoid missing CU diagnosis; they also need to be aware that EU can appear in association with other bacterial infections other than CU.
With regard to the choice of antibiotic treatment, it is to be noted that vancomycin and teicoplanin may cause renal insufficiency. In our center, to achieve maximum preservation of renal function, we normally avoid the use of glycopeptide antibiotics and instead commence treatment with oral linezolid 600 mg every 12 hours. Linezolid is not nephrotoxic, does not need monitoring, and has the advantage that bioavailability is the same with oral and intravenous administration. In addition, to control the formation of new calcifications, a urease inhibitor such as acetohydroxamic acid can help.
After diagnosis, if the patient suffers from a high degree of EU or hydronephrosis, a nephrostomy tube or a ureteral catheter is recommended for the purpose of further acidifying instillations and to promote urinary drainage. Surgery is usually reserved for obstructive uropathy that does not resolve with medical therapy. Ureteroscopy may be performed to treat ureteral calcifications, whereas percutaneous nephrolithotomy may be an option in the presence of bulky kidney calcifications. In general, endourology is not effective against EU as encrustations adhere to the mucosa, causing fibrosis and edema, and tend to bleed during the procedure.
The off-label use of the acidifying Thomas solution, Suby G solution, and DR solution (containing N-acetylcysteine, acetohydroxamic acid, and aztreonam) has been described, as has that of other nonacidifying irrigations such as dimethyl sulfoxide. Although these are usually well tolerated, their effectiveness with respect to calcifications is variable. When used, all instillations require to be administered one kidney at a time, with close monitoring of renal function, acid–base balance, magnesium levels, and possible presence of candiduria.
In this patient, a Mono J stent was placed to facilitate urine drainage, but no acidifying instillations were administered. Acetohydroxamic acid was employed for 1 month without changes in renal calcifications. The use of l-methionine 500 mg/12 hours as the oral acidifying method4 administered within Lit-Control® pH Down (Devicare) almost completely removed the EU and reduced the risk of stent encrustation.
Conclusion
EU is a severe disease that requires rapid diagnosis. Treatment is multimodal based on antibiotic therapy and local treatment of the urinary tract encrustations. In the reported case, the use of oral urinary acidification with l-methionine was effective in removing the EU.
Abbreviations Used
- AHA
acetohydroxamic acid
- EU
encrusted uropathy
- CU
Corynebacterium urealyticum
- CT
computed tomography
- PCNL
percutaneous nephrolithotomy
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Sabiote L, Emiliani E, Kanashiro AK, Balañà J, Mosquera L, Sánchez-Martín FM, Millán F, Alonso C, Palou J, Angerri O (2020) Oral acidification with l-methionine as a noninvasive treatment for encrusted uropathy, Journal of Endourology Case Reports 6:3, 143–146, DOI: 10.1089/cren.2019.0164.
References
- 1. Sánchez-Martín FM, López-Martínez JM, Kanashiro-Azabache A, et al. . Corynebacterium urealyticum: Increased incidence of infection and encrusted uropathy. Actas Urol Esp 2016;40:102–107 [DOI] [PubMed] [Google Scholar]
- 2. Meria P, Desgrippes A, Arfi C, Le Duc A. Encrusted cystitis and pyelitis. J Urol 1998;160:3–9 [PubMed] [Google Scholar]
- 3. Ulloa MT. Corynebacterium urealyticum Rev Chilena Infectol 2009;26:548. [PubMed] [Google Scholar]
- 4. Torrecilla C, Fernández-Concha J, Cansino JR, et al. Randomized clinical trial on urinary pH monitoring and nutraceutical intervention in the prevention of ureteral stent incrustation. In: Abstract World Congress of Endourology, 2019