High mortality has been reported among patients with haematological malignancies (HMs) and coronavirus disease 2019 (COVID-19), providing the impetus for heightened infection prevention strategies among patients with HMs during the COVID-19 pandemic [1]. Various infection prevention measures have been introduced during the ongoing pandemic, such as visitor restrictions and universal masking [2]. Outside of the outbreak setting, however, patients with HMs remain susceptible to common respiratory viral infections (RVIs) [3]. The impetus provided by the COVID-19 pandemic for implementation of heightened infection prevention measures on haematology units may potentially reduce transmission of hospital-associated RVIs (HA-RVIs) as an unintended positive consequence.
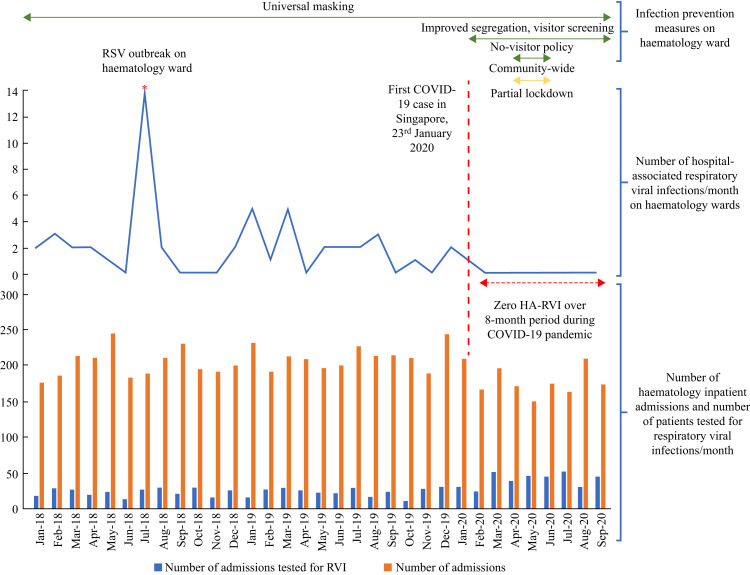
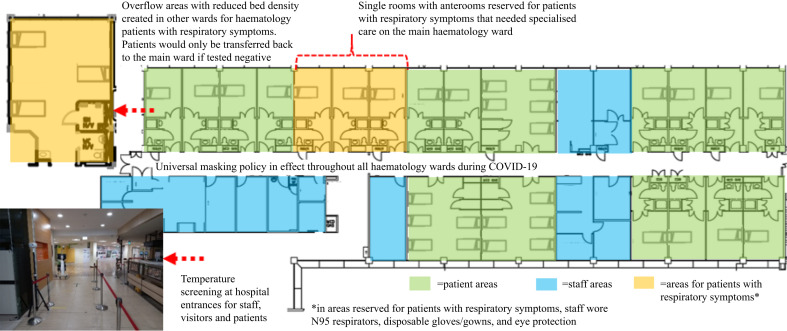
From January 23rd, 2020 onwards, a COVID-19 containment strategy was implemented on the haematology wards of Singapore General Hospital (SGH), the largest tertiary hospital in Singapore (Figure 1 ). Our institution also runs an active stem-cell-transplant (HSCT) service. Pre-pandemic, patients with HMs were predominantly nursed in multi-bedded open-plan general wards, with single rooms prioritized for neutropenic patients (Figure 2 ). A universal masking policy was in-place on the haematological wards pre pandemic. Despite universal masking, RVI outbreaks were still recorded in 2015, 2016, and 2018, disproportionately affecting patients in the multi-bedded cohorted cubicles (Figure 2). During the COVID-19 pandemic, additional infection-prevention measures were introduced (Figure 1, Figure 3 ) [4]. Symptomatic patients were segregated in cohorted cubicles with reduced bed density and temporary partitions erected between beds; healthcare workers (HCWs) wore disposable gowns, gloves, eye protection and masks while attending to patients (Figure 3) [4,5]. All symptomatic inpatients were tested for COVID-19 and 16 common RVIs via multiplex PCR testing. HSCT recipients were also tested pre transplant. Cases were categorized as HA-RVI if RVI was identified beyond the maximum incubation period from the time of admission [6,7]. All visitors were screened for fever and respiratory symptoms; symptomatic visitors were denied entry. Initially, visitor limitations were implemented (one-visitor policy); from April 7th, 2020 to June 2nd, 2020, no visitors were allowed during the ‘lockdown’ period when all schools and workplaces were closed as part of community-based measures to mitigate transmission. Visitor restrictions were suspended in conjunction with the lifting of ‘lockdown’, and progressively relaxed to allow a maximum of five visitors from June 19th, 2020. We evaluated changes in the incidence of HA-RVI among haematology inpatients after the introduction of COVID-19 containment measures, subsequent relaxation of community-wide ‘lockdown’, and lifting of visitor restrictions in-hospital. Waiver of informed consent for publication was approved by our hospital's Institutional Review Board (CIRB 2020/2436).
Figure 1.
Rates of hospital-associated respiratory viral infection (RVI) among haematology inpatients and layout of haematology wards before and during the COVID-19 pandemic. The standard multiplex polymerase chain reaction assay for common respiratory viral infections included: influenza A and B, human parainfluenza virus (HPIV) 1/2/3/4, respiratory syncytial virus (RSV) subtypes A and B, human metapneumovirus (hMPV), human coronavirus (HCoV) (229E/NL63/OC43), rhinovirus A/B/C, enterovirus, adenovirus and human bocavirus (HboV) 1/2/3/4.
Figure 2.
Layout of haematology ward prior to COVID-19 pandemic.
Figure 3.
Layout of haematology ward during COVID-19 pandemic.
Prior to the COVID-19 outbreak, from January 2018 to January 2020, the incidence of HA-RVI on haematology wards was 9.05 cases per 10,000 patient-days (52 cases, 57,480 patient-days). Despite universal masking, an outbreak of respiratory syncytial virus occurred in the haematology ward in July 2018, involving 10 patients and four staff. After introduction of visitor screening/improved segregation, incidence of HA-RVI fell to 0.64 cases per 10,000 patient-days (one case, 15,706 patient-days); this decline was statistically significant (incidence rate ratio (IRR): 0.07; 95% confidence interval (CI): 0.002–0.41; P = 0.005). Notably, the incidence of HA-RVI on the haematology wards fell to zero over an eight-month period; an observation unprecedented in the preceding two years (Figure 1). This observation came despite increased testing for RVIs, due to heightened vigilance for respiratory symptoms (Figure 1). Zero HA-RVI was maintained even after reversal of community-based measures (‘lockdown’) and after visitor restrictions were relaxed. To date, no definitive evidence of nosocomial transmission of COVID-19 has been reported at our institution; COVID-19 cases among HCWs remained low (0.13%, 17/13,066) and were predominantly attributed to community acquisition [4]. Over the same period, rates of community-acquired RVI among haematology inpatients remained static, at 32.6 cases per 1000 admissions (169 cases, 5177 admissions) pre pandemic, versus 28.4 cases per 1000 admissions (40 cases, 1404 admissions) during the COVID-19 pandemic (IRR: 0.87; 95% CI: 0.60–1.24; P = 0.44).
Respiratory viruses are unlikely to be transmitted exclusively by droplet or by contact; addition of contact precautions to droplet precautions for symptomatic patients could potentially account for the reduction in HA-RVI [7]. Furthermore, screening of symptomatic visitors eliminates a potential source of transmission [6]. Whereas previous studies did not demonstrate a significant decrease in HA-RVI when either enhanced isolation precautions (contact and droplet precautions) or visitor screening was deployed, we demonstrated a significant reduction in HA-RVI when both measures were deployed in tandem [6,7]. Although previous studies have demonstrated significant decreases in community-acquired RVI as a result of community-based COVID-19 control measures, likely because patients with HMs were already encouraged to practice social distancing, masking, and good hand hygiene pre pandemic, rates of community-acquired RVI among haematology inpatients at our institution remained static during the pandemic [8]. Zero HA-RVI was already attained prior to the imposition of community-wide ‘lockdown’ measures and sustained even after reversal of ‘lockdown’; furthermore, as driving pressures for HA-RVI (admissions for community-acquired RVI) remained static throughout the pandemic, the substantial decreases in HA-RVI were likely attributable primarily to the hospital-based measures introduced for COVID-19 control. Infection prevention measures originally meant for COVID-19 have value in mitigating HA-RVI among patients with HMs and should be continued even after the pandemic is over.
Acknowledgements
We thank our colleagues for their unstinting efforts against COVID-19.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Passamonti F., Cattaneo C., Arcaini L., Bruna R., Cavo M., Merli F. Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. Lancet Haematol. 2020;7:e737–e745. doi: 10.1016/S2352-3026(20)30251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klompas M., Morris C.A., Sinclair J., Pearson M., Shenoy E.S. Universal masking in hospitals in the Covid-19 era. N Engl J Med. 2020;382:e63. doi: 10.1056/NEJMp2006372. [DOI] [PubMed] [Google Scholar]
- 3.Chemaly R.F., Shah D.P., Boeckh M.J. Management of respiratory viral infections in hematopoietic cell transplant recipients and patients with hematologic malignancies. Clin Infect Dis. 2014;59:S344–S351. doi: 10.1093/cid/ciu623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wee L.E., Sim X.Y.J., Conceicao E.P., Aung M.K., Tan K.Y., Ko K.K.K. Containing COVID-19 outside the isolation ward: the impact of an infection control bundle on environmental contamination and transmission in a cohorted general ward. Am J Infect Control. 2020;48:1056–1061. doi: 10.1016/j.ajic.2020.06.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wee L.E., Conceicao E.P., Sim X.Y.J., Aung M.K., Tan K.Y., Wong H.M. Minimizing intra-hospital transmission of COVID-19: the role of social distancing. J Hosp Infect. 2020;105:113–115. doi: 10.1016/j.jhin.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mermel L.A., Jefferson J.A., Smit M.A., Auld D.B. Prevention of hospital-acquired respiratory viral infections: assessment of a multimodal intervention program. Infect Control Hosp Epidemiol. 2019;40:362–364. doi: 10.1017/ice.2018.337. [DOI] [PubMed] [Google Scholar]
- 7.Rubin L.G., Kohn N., Nullet S., Hill M. Reduction in rate of nosocomial respiratory virus infections in a children’s hospital associated with enhanced isolation precautions. Infect Control Hosp Epidemiol. 2018;39:152–156. doi: 10.1017/ice.2017.282. [DOI] [PubMed] [Google Scholar]
- 8.Tan J.Y., Conceicao E.P., Sim X.Y.J., Wee L.E., Aung M.K., Venkatachalam I. Public health measures during COVID-19 pandemic reduced hospital admissions for community respiratory viral infections. J Hosp Infect. 2020;106:387–389. doi: 10.1016/j.jhin.2020.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]