 Donor biological materials and excipients of animal origin are important components in the production of biomedical cell products (BMCPs).
Donor biological materials and excipients of animal origin are important components in the production of biomedical cell products (BMCPs).
Abstract
Donor biological materials and excipients of animal origin are important components in the production of biomedical cell products (BMCPs). Their quality ensures the stability, safety, effectiveness and purity of the final product. This review discusses quality requirements for biological excipients intended for the production of biomedical cell products, in terms of the necessary information that should be included in the BMCP registration dossier during state registration and is subject to expert assessment during quality control. Considering that there is currently no production of biomedical cell products in the Russian Federation, the authors considered international approaches to ensuring the safety of donor material and excipients for the manufacturing of human cell- and tissue-based products (BMCP analogues).
The main problem with using biomedical cell products (BMCPs) is the risk of direct transmission of an infectious disease. The risk level depends on a variety of factors, e.g. whether the drug is autologous or allogeneic; whether the cells and tissues were received from a bank; whether they were transported or processed in a room where cells and tissues from various organs are stored; and how intensively they were processed. There is a possibility of contamination of the final product with viruses, mycoplasmas, bacteria, fungi and prions through the source materials (especially those of biological origin) or during the production.
To guarantee the provision of safe and reliable cells and tissues, it is necessary to regulate the procurement, production, testing and storage of all cells intended for administration to humans.
The key approaches to adventitious agent assay worldwide are:1
1. Conducting appropriate screening for donors and biological material, including fetal material, to prevent transmission of infectious agents.
2. Quality control of biological reagents, as well as products of cell lines (CLs) and feeder cells used when working with cell cultures that are potential sources of contamination.
3. Control of the environment, working conditions, and laboratories for processing and storage of CLs.
4. Testing security modes for cell banks.
The purpose of this review is to consider the requirements (both foreign and domestic) for (raw) materials of biological origin used in the manufacturing of human cell- and tissue-based products (BMCP analogues), since the registration dossier requires the manufacturer of BMCPs to provide a process flowchart, as well as a general summary of the safety assessment of the starting materials, to the regulatory authority/control laboratory. The following requirements for biological material donors and excipients are fundamental criteria for the safe use of BMCPs.
Requirements for biological material donors
All human cells (including reproductive ones) can transmit infectious diseases. Therefore, thorough testing is necessary in order to avoid their transfer from donor to recipient. In the past, donors were tested for the absence of immunodeficiency (HIV) and viral hepatitis viruses, mainly hepatitis B and C. Those tests were based on the detection of antibodies generated by the donor in response to a viral infection. Further studies have shown that antibody detection is impossible if reactive antibodies are absent. But it is possible that the individual has already been infected with a viral infection, and moreover, has already developed viremia.2 Hepatitis C virus and HIV are potential agents from this category, where testing an individual for the presence of reactive antibodies shows a negative result, but viremia is observed for several months before seroconversion.3 Based on this, it seems relevant to conduct analyses using the technique of amplification of nucleic acids (PCR, polymerase chain reaction) along with tests for the presence of antibodies to some viruses. Although the prevalence of human hepatitis B and C viruses, HIV, and T-cell lymphotropic virus (HTLV) is lower among tissue donors than in the general population, the probability of undetected viremia during collection is higher among tissue donors than among blood donors.4,5 Adding methods such as PCR to the process of screening donor tissues and testing the CLs resulting from them, will reduce the risk of infection among stem cell recipients.6
Thus, at present, global approaches to donor screening are based on two main methods: antibody detection and PCR. Table 1 presents an approximate list of infections that can be transmitted through donor tissues and currently available tests for their identification.1,7,8
Table 1. The list of infections that can be transmitted through donor tissue and currently available tests for their identification1,7,8 .
| Name of the infection | Screening test |
| Human immunodeficiency virus types 1 and 2 (HIV-1, HIV-2) | Anti-HIV-1,2; PCR |
| Hepatitis B (HBV) | HBsAg; anti-HBc; PCR |
| Hepatitis C (HCV) | Anti-HCV; PCR |
| Syphilis (Treponema pallidum) | Treponema-specific antibodies; PCR |
| Human T-cell lymphotropic virus types I and II (HTLV-I, HTLV-II) | Anti-HTLV-I and anti-HTLV-II |
| Cytomegalovirus infection (CMV) | IgG anti-CMV |
| Infectious mononucleosis (Epstein–Barr virus) | PCR |
| Transmissible spongiform encephalopaties (TSEs) (Creutzfeldt–Jacob disease) | Western blot; PCR |
| Neisseria gonorrhoeae a | Culture test |
| Chlamydia trachomatis a | IgG anti-Chlamydia |
aFor donors of reproductive cells and tissues.
European Union
In the EU, donor selection requirements are based on an analysis of the risks associated with the use of specific human cells/tissues. Risks should be identified by medical examination, biological testing, post-mortem examination for deceased donors, or any other relevant studies.9
If the extracted tissues and/or cells will be stored or cultured, living donors of autologous material have to meet the requirements for an allogeneic living donor. Allogeneic living donors should be selected on the basis of their health and medical history provided in the questionnaire and survey conducted by a qualified and trained medical professional in accordance with the approved requirements. Such an assessment should include relevant factors that can help identify and screen individuals whose donation may endanger the health of recipients. Also, the donation process should not endanger the health and life of the donor. In cases of cord blood or amniotic membrane donation, this applies to both the mother and the child. The selection criteria for allogeneic living donors should be established and documented by the institution in which the donation process takes place, depending on the particular type of tissue or cells.9
Also, the EU legislation on tissues and cells sets minimum requirements for testing donors for infectious diseases.8 Regardless of the source of biological material (intravital or posthumous, autologous or allogeneic donation), it should be tested for HIV-1, HIV-2, HIV-1,2 antibodies, hepatitis B, HBsAg, anti-HBc, hepatitis C and anti-HCV, and syphilis. If it tests positive for antibodies to HBc and negative for HBsAg, further studies are needed to assess the risk of using the donor material.
Under certain circumstances, additional testing may be required depending on the donor's history and the characteristics of the tissue or donor cells (e.g. testing for malaria, CMV, toxoplasma, infectious mononucleosis, Trypanosoma cruzi, etc.). Antibody testing for HTLV-I should only be performed for donors living in areas of high prevalence, or if there were sexual partners originating in such areas, or if the donor's parents come from these areas.8
When using cells from different donors, one should take into account the probability of increasing the risk of unwanted immunological reactions in the recipient, as well as an increased risk of transmission of a disease. Depending on the source of cells or tissues, it is necessary to take into account other risk factors, e.g. radioactive exposure in the past, and to conduct appropriate testing.10
USA
In 1997, the FDA proposed a new approach to the regulation of products similar to BMCP. According to these requirements, as well as the guidelines introduced in subsequent years, donor eligibility must be determined for all donors of cells or tissues by screening and testing the donors for certain infectious agents and diseases, with the exception of the following cases:7
1) Cells and tissues for autologous use.
2) Reproductive cells or tissues for reproductive use.
3) Cryopreserved cells or tissues for reproductive use, provided that.
a) Additional donation is not available, for example, due to infertility of the donor.
b) Appropriate measures are taken to verify the donor(s) prior to transfer to the recipient.
In the case of donation of an embryo or cells derived from an embryo, it is required to determine eligibility for both the oocyte donor and the sperm donor.
The medical organization facilitating the donation must establish and maintain procedures for all the stages of testing, screening, determining donor eligibility and ensuring compliance with all other relevant requirements.
All cell and tissue donors must be tested for infectious diseases using FDA-approved tests.7 In accordance with the requirements, all human cells and tissues are tested for HIV-1, 2, hepatitis B and C viruses, transmissible spongiform encephalopathy (TSE) (including Creutzfeldt–Jakob disease), and syphilis. Additional testing for HTLV-I, II is necessary for biological material containing leukocytes. Reproductive cells or tissues should also be tested for Chlamydia trachomatis and Neisseria gonorrhea. These are the essential tests; additional testing depends on the risk of transmission of diseases to the recipient or to people who may be in contact with the donor, product, or recipient (e.g. medical personnel).
Other countries
In most other countries, the requirements for determining the eligibility criteria for donors and donor material are similar to these of the EU and the US. The general approach is based on three stages:
1) Donor screening – conducting an assessment based on the medical and social history of the donor, a physical examination, results of any diagnostic procedures and, if applicable, an autopsy.
2) Donor testing – laboratory tests to determine.
a) Presence of certain infectious diseases (Table 2).
Table 2. List of essential tests for donors in different countries.
| EU | USA a | Japan b | Korea | Australia | Canada | Taiwan | |
| HIV-1 | + | + | + | + | + | + | + |
| HIV-2 | + | + | + | + | + | + | + |
| Hepatitis B virus | + | + | + | + | + | + | + |
| Hepatitis C virus | + | + | + | + | + | + | + |
| Syphilis | + | + | + | + | + | + | + |
| HTLV-I | + | + d | + | + | + | + d | – |
| HTLV-II | – | + d | – | – | – | + d | – |
| CMV | – | + d | + | – | – | + d | – |
| Chlamydia trachomatis c | + | + | – | – | + | + | – |
| Neisseria gonorrhoeae c | – | + | – | – | – | – | – |
aOnly for allogeneic donor material.
bAllogeneic donor material requires additional testing for parvovirus B19, Epstein–Barr virus, and West Nile fever virus.
cOnly for reproductive cells and tissues.
dOnly for donor material containing leukocytes.
b) Compatibility with recipients (e.g. determination of HLA (human leukocyte antigens)).
c) Determining the degree of functionality and viability of cells or tissues (e.g. when receiving donor material from corpses).
3) Donor eligibility assessment – an assessment based on the results of screening and testing of donors.
According to WHO recommendations, in some countries it is also recommended to conduct screening for other blood-borne infections:
– In endemic areas: malaria, Chagas disease, HTLV, West Nile fever, Ebola hemorrhagic fever.
– In non-endemic areas, for donors who live in, or visit, endemic areas: malaria, Chagas disease, HTLV, West Nile and Ebola fevers.
– Other emerging and recurring infections (e.g. Creutzfeldt–Jakob disease, dengue and chikungunya fevers) or infections posing a threat to certain groups of recipients (e.g. CMV).11
In some cases it is necessary to indicate the viral load for latent viruses (herpes simplex virus, CMV, Epstein–Barr virus, human herpesviruses type 6, 7, and 8, human polyomaviruses (JC and BK), parvovirus B19, and transfusion transmitted virus (TTV)), all of which can be detected in humans from early childhood and are potential contaminants of cells taken from healthy donors. Since these viruses are ubiquitous, their presence in donors poses no risk for most patients. For example, the maximum allowed amount of parvovirus B19 in the blood of the donor is 105 genomic equivalents per dose administered to a human. However, in some cases these viruses can be dangerous. For example, transplantation of heart cells or tissues from CMV-positive donors can be fatal for a recipient who was not previously affected by this virus.1
An additional assessment of the risk of transmission of viral infections from the donor can be carried out, depending on the types of transplanted cells and their characteristic infections. For example, lung tissue may carry respiratory adenoviruses, influenza viruses, and respiratory syncytial virus.1
Russian Federation
In March 2018, Order No. 125n of the Ministry of Health of Russia “On Approving the Procedure for Medical Examination of a Donor of Biological Material and a List of Contraindications (Absolute and Relative) for Obtaining Biological Material” came into effect.12 It defines the procedure for medical examination of living donors of biological material intended for production of BMCPs (among other things, for the purpose of conducting preclinical and/or clinical studies).
In accordance with the order, all donors should be tested for HIV-1, HIV-2, hepatitis B and C, and syphilis. The list of contraindications for donation of biological material for production of BMCPs is presented in Table 3.
Table 3. List of contraindications for donation of biological material for production of BMCPs12.
| For production of … | Absolute contraindications | Relative contraindications |
| Allogeneic BMCPs | 1. History of diseases of unknown etiology2. History of cancers3. History of Creutzfeldt–Jakob disease, or suspicion thereof4. History of rapidly progressive dementia5. A history of transplantation of the cornea or dura mater6. Undocumented neurosurgery with incisions on the dura mater7. History of treatment with drugs derived from the human pituitary gland8. The presence in the blood of antibodies to human immunodeficiency viruses HIV-1 and HIV-2, hepatitis B and C viruses (except a history of vaccination against viral hepatitis)9. History of syphilis10. History of chronic systemic autoimmune diseases that can affect the quality of biological material | 1. Infectious diseases of any etiology (including tuberculosis), or a local infection process (as of the date of the donation, until the end of the infection process)2. Treatment with immunosuppressive drugs at the moment of donation of blood cells or red bone marrow (as of the date of the donation of biological material, until the restoration of blood cell lineage)3. Treatment with drugs that can affect the quality of the biological material (as of the date of the donation of biological material, until after 6 biological half-lives of the drug, in accordance with the instructions for use of the drug)4. Exposure of the donor to poisonous or toxic substances5. Preventive vaccination with live virus vaccines (for 1 year after vaccination)6. Pregnancy (as of the date of the donation of biological material)7. Breastfeeding (as of the date of the donation of biological material) |
| Autologous BMCPs | 1. Risk of undesirable reactions or diseases caused by the donation of biological material which exceed the potential benefits of the BMCP made from the donated material2. Diseases (conditions) adversely affecting the quality of biological material | 1. Acute infectious diseases that pose a threat to those around the donor (as of the date of the donation, until the end of the infection process) |
As a result of the study, the following approaches to donor testing can be distinguished:
1. All donors are tested for: hepatitis B and C, HIV-1, HIV-2, syphilis (Treponema pallidum), TSEs (including Creutzfeldt–Jakob disease).
2. Additional testing is performed if medically required, e.g. CMV (for whole organs and allogeneic bone marrow donors), toxoplasma (for donors of the heart, liver and bone marrow), etc.
3. There is an extended list of tests for donors of leukocyte-enriched cells and tissues: HTLV-I, II, hepatitis C virus and CMV, which are considered cell-associated viruses; hepatitis A and E viruses are also included in the list of virus groups posing a risk of transmission from donor to recipient.
4. Additional testing for donors of reproductive cells and tissues: Neisseria gonorrhoeae and Chlamydia trachomatis.
5. Detection of some microbial agents depending on the geographical location and epidemiological situation in the world: endemic viruses and new emerging infections.
Requirements for media, serums and other excipients used in the production of biomedical cell products
Various reagents (or excipients), many of which are unique or complex, are used in the production of BMCPs. Federal Act 180 stipulates that “excipients are substances of inorganic or organic origin used in the development and production of a biomedical cell product”.13 These include serums, culture media, digestive enzymes (e.g. trypsin, collagenase, etc.), growth factors, cytokines, monoclonal antibodies, antibiotics and other chemicals, as well as feeder cells. The defining property of such reagents is their absence in the final product.
According to relevant organizations of the EU, USA, Australia (EMA, FDA, TGA) and other countries, as well as WHO recommendations, the quality of reagents can affect the stability, safety, effectiveness and purity of the final product. Many of these excipients are used to ensure viability, growth, or manifestation of certain biochemical effects of certain cell populations, although the mechanism of action of some substances has not yet been fully studied. Thus, if they remain in the finished product, they can have unintended consequences (immune response, toxic effects or deterioration of the effectiveness of cell- and tissue-based drugs) after administration to the patient. In addition, during the production of BMCPs, any excipient of human or animal origin can become the primary source of adventitious agents. Careful control of materials used in the production is necessary to prevent undesirable consequences, as well as to ensure maximum safety, efficiency and consistency of the final product.14
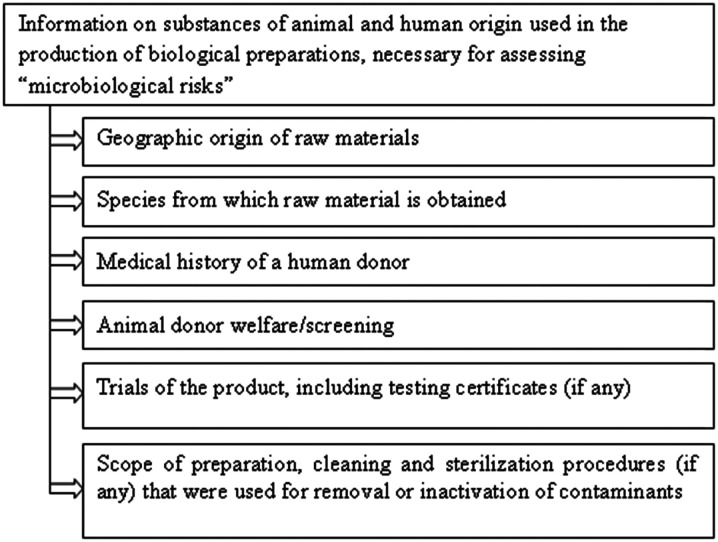
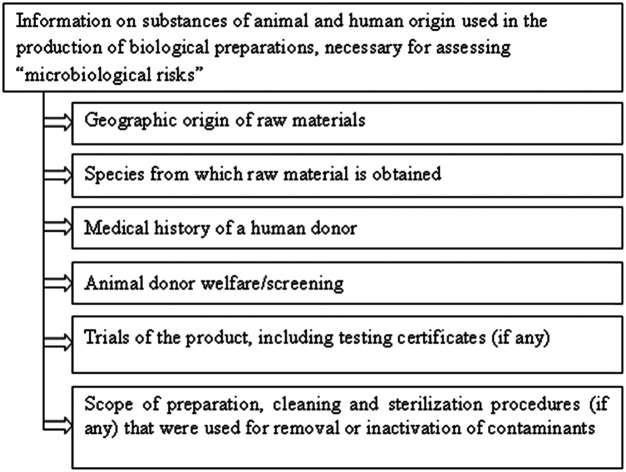
According to the WHO recommendation on the evaluation of animal cell cultures used as substrates for the production of biological products, as well as in the descriptions of cell banks, close attention should be paid to sources of raw materials, their preparation, handling, testing and quality control.15 When creating cultures, isolating a new cell line, creating banks and manufacturing products, all materials of biological origin used for cultivation that come into close contact with cells should be subjected to the appropriate tests specified in the risk identification section of regulatory documentation. This helps establish the quality of the material and the absence of microbiological contamination, and evaluate the suitability of the material for use in production. It is important to evaluate the “microbiological risks” carried by each reagent of human or animal origin that is used in the process of cultivation (Fig. 1).
Fig. 1. Evaluation of “microbiological risks” of excipients.15.
In accordance with §1271.210 of FDA Guidance for Industry the following records should be presented for each reagent:16,17
• Records of the receipt of each reagent, including the type, quantity, manufacturer, lot number, date of receipt, and expiration date.
• Records of the verification of each reagent, including test results or, in the case of vendor verification, a certificate of analysis (COA) from the vendor. It's recommended to use FDA-approved, or refined, or other materials intended for clinical use, if available. If the excipient is not approved by the FDA (or if there are no generally accepted standards), additional information on production and/or testing may be required to evaluate the safety and quality of the material. The amount of testing will depend on the particular reagent and how it is used in the manufacturing process.
• Records of the stage of the manufacturing process at which the reagent is used.16,17
See Table 4 for an example of presentation of information about the reagent.
Table 4. Example of a table for providing information on reagents.
| Name of the reagent | Type | Manufacturer | Lot number, dates | Quality (certificates etc.) | Production stage |
The EMA Guidelines for cell-based drugs and TGA documents practically do not differ from the American ones in terms of general requirements for reagents.10,18,19
Animal-derived reagents in America are regulated, among other regulatory documents, by the requirements for the ingredients of animal origin used for production of biologics. All the documents contain a mandatory requirement for such reagents, i.e. the adoption of measures to reduce the risk of BSE transmission. A certificate or documents containing certain information must be provided.
According to Resolution No. 26 (adopted during the 86th General Session of the World Assembly, May 2018), the World Organization for Animal Health (OIE) classifies countries based on BSE risk (Table 5).
Table 5. OIE classification of countries by BSE risk.
| 1. Negligible BSE risk | |||||
| Argentina | Costa Rica | Hungary | Liechtenstein | Norway | Slovakia |
| Australia | Croatia | Iceland | Lithuania | Panama | Slovenia |
| Austria | Cyprus | India | Luxembourg | Paraguay | Spain |
| Belgium | Czech Republic | Israel | Malta | Peru | Sweden |
| Brazil | Denmark | Italy | Mexico | Poland | Switzerland |
| Bulgaria | Estonia | Japan | Namibia | Portugal | The Netherlands |
| Chile | Finland | Korea (Rep. of) | New Zealand | Romania | USA |
| Colombia | Germany | Latvia | Nicaragua | Singapore | Uruguay |
| 2. Controlled BSE risk | |||||
| Canada | France | Ireland | |||
| Chinese Taipei | Greece | ||||
| 3. Zones with a negligible BSE risk | |||||
| China (People's Rep. of): a zone designated by the Delegate of China in a document addressed to the Director General in November 2013, consisting of the People's Republic of China with the exclusion of Hong Kong and Macau | |||||
| United Kingdom: two zones consisting of Northern Ireland and Scotland, as designated by the Delegate of the United Kingdom in documents addressed to the Director General respectively in September and October 2016 |
| 4. Zone with a controlled BSE risk | |||||
| United Kingdom: a zone consisting of England and Wales as designated by the Delegate of the United Kingdom in documents addressed to the Director General in September and October 2016 |
All participating countries recognized the presence of risk or risk zones in accordance with Chapter 11.4 of the Terrestrial Animal Health Code.20 All other countries and zones have no official OIE status in terms of BSE risk.
In Europe, there is a European Food Safety Authority (EFSA) classification of countries by level of geographical BSE risk (GBR level) (Table 6).21
Table 6. EFSA classification of countries by geographical BSE risk (GBR)23.
| GBR level | Presence of one or more cattle clinically or pre-clinically infected with the BSE agent in a geographical region/country | GBR of the country/region |
| Current status | ||
| I | Highly unlikely | Australia, Argentina, Botswana, Brazil, Chile, Costa Rica, Iceland, Namibia, New Zealand, Nicaragua, Panama, Paraguay, Salvador, Singapore, Swaziland, Uruguay, Vanuatu |
| II | Unlikely but not excluded | Columbia, India, Kenya, Mauritius, Nigeria, Norway, Pakistan, Sweden |
| III | Likely but not confirmed or confirmed at a lower level | Albania, Austria, Belgium, Canada, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Japan, Latvia, Lithuania, Luxembourg, Mexico, the Netherlands, Poland, Romania, San Marino, SAR, Slovakia, Slovenia, Spain, Switzerland, Turkey, USA |
| IV | Confirmed at a higher level | Portugal, UK |
If possible, reagents of human and animal origin should be avoided and replaced with synthetic alternatives with a well-defined composition. It is preferable to use raw materials of animal origin from countries with a low BSE risk (according to OIE) and with a geographical risk level I (according to EFSA).
Serum
There are special requirements for certain reagents, including serum. WHO recommends that source(s) of bovine serum and its testing methods be approved by the national regulatory authority/control laboratory. The manufacturer is responsible for ensuring the quality of the serum used to create cell banks and biological products. The manufacturer of the drug can test for adventitious agents and inactivate the serum after acquiring it from the manufacturer. Alternatively, the manufacturer of the drug can certify a certain seller of serum and purchase it after careful regular checks.15
According to WHO recommendations and the EMA Guideline on the use of bovine serum in the manufacture of human biological medicinal products, bovine serum should be tested for adventitious agents such as bacteria, fungi, mycoplasmas (M. arginini and M. laidlawii), prions and viruses, before it can be used to create the master and working cell banks. Particular attention should be given to bovine viruses that can be zoonotic or oncogenic (e.g. viral diarrhea (BVDV), polyomavirus, circoviruses, rabies virus, adenovirus infection (BAV), parvovirus infection (BPV), respiratory syncytial virus (BRSV), infectious rhinotracheitis virus (IBR), type 3 parainfluenza virus (PI3), type 3 reovirus (REO3), Cache Valley virus, bluetongue virus (BTV) and epizootic hemorrhagic disease virus).15,22,23
Serum samples are usually tested for antibodies to viruses; however, additional PCR testing for the presence of the pathogen is possible. One peculiarity of serum sampling should be borne in mind: the volume of the test sample is much smaller than the batch size which is obtained by combining serum from many animals (the difference is about 1000 : 1). Therefore, the causative agents of viral infections may not get into the serum sample during testing, and the possibility of a direct check of the cell bank for bovine viruses should be considered.15
In order to guarantee a decrease in the activity of adventitious agents that are not detectable during manufacture and quality control, to a level that is recognized as acceptable by the national regulatory authority/control laboratory, the serum must be inactivated using high temperature or γ-radiation.15,17,19
If the serum is inactivated by any method in the manufacturing process, it should be tested for the presence of adventitious agents before inactivation; otherwise the chances of detecting extraneous contaminants are reduced. If viruses are detected, such a serum can be used only after mandatory identification of the virus and detection of an amount that can be effectively inactivated. If signs of viral contamination are detected in sera that are not subject to the inactivation procedure, these sera are unsuitable. A manufacturer has the right to use a serum that has not undergone inactivation, but is obliged to test it for adventitious agents using modern technologies. In the event that foreign agents are detected, the manufacturer must provide evidence that the cell banks created using this serum are not contaminated with the detected viruses.15 It should be noted that it's not permissible to use bovine serum in which the above-listed agents were detected for BMCP production.
For the use of serum obtained from other (not bovine) animal species, one should consult with the national regulatory authority/control laboratory about testing methods appropriate for the species.15
If human AB serum is used (e.g. for production of genetically modified cells ex vivo), one should make sure that it is obtained from donor blood or plasma according to the established rules in appropriate medical organizations licensed for such work. Since plasma is not tested as extensively as blood products intended for infusion, it is recommended to ensure the safety of the AB serum used in production. For example, if a serum is obtained from original plasma, the risk of an infectious disease can be reduced by additional testing for the appropriate transfusion-transmitted infections. A viral inactivation or clearance may be a suitable alternative.17 It is preferable to use autologous sera (if possible) rather than allogeneic ones.10
In addition to the aforementioned documents, serum requirements are presented in pharmacopoeial articles in Europe and the USA.24,25
Table 7 provides information on sera from certificates of analysis from different manufacturers.
Table 7. Examples of information provided in serum analysis certificates from different manufacturers.
| Manufacturer | Country | Purpose | Method of inactivation | Sterility, mycoplasmas, endotoxins | Testing for viruses | BSE risk |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Life Technologies | USA | For in vitro diagnostics | Thermally inactivated | + | For antibodies to BVDV, BPV, BAV, BRSV, BTV, rabies virus, reovirus | The serum is obtained in accordance with procedures approved by the US Department of Agriculture |
| Australia | N/a | |||||
| For cytopathic effect: IBR | ||||||
| For the presence of a hemadsorbing agent: PI3 | ||||||
| Brazil | BVDV, IBR, PI3 | |||||
| HyClone | USA | N/a | Not inactivated | + | For antibodies to BVDV, BPV, BAV, BRSV, BTV, rabies virus, reovirus | The serum is obtained in accordance with procedures approved by the US Department of Agriculture. Complies with Ph. Eur. 2011 5.2.8 |
| For cytopathic effect: IBR | USA has a geographical BSE risk level III (EFSA) and a “negligible BSE risk” (OIE) | |||||
| Atlas Biologicals | USA | For production. Not intended for therapeutic use | γ-Irradiated | + | For the presence of a hemadsorbing agent: PI3 | The serum is obtained in accordance with procedures approved by the US Department of Agriculture. All source materials were obtained from healthy animals without detectable diseases, and were not combined with materials of the specified risk |
| SAFC | USA | Animals from whom the serum was collected, were tested by the USDA and deemed eligible for slaughter | ||||
| Australia | Not inactivated | Serum was not collected from cattle in countries with reported cases of BSE | ||||
| Gibco | New Zealand | For in vitro diagnostics | Thermally inactivated | + | Same as above | N/a |
| MP Biomedicals | USA | Only for study | Thermally inactivated | + | BVDV, IBR, PI3 | |
| Sigma-Aldrich | Colombia | Manufacturing | Thermally inactivated | + | BVDV, IBR, PI3 |
Trypsin
Trypsin should also be tested for bacteria, fungi, mycoplasmas (M. arginini (bull), M. laidlawii (bull) and M. hyorhinis (pig)) and viral pathogens, including parvoviruses and circoviruses of cattle or pigs, if necessary. Tests for porcine adenovirus, transmissible viral gastroenteritis, porcine hemagglutinating encephalitis virus, bovine viral diarrhea, reoviruses, rabies virus, porcine anellovirus, Porcine circovirus, porcine bocavirus, porcine hepatitis E virus, porcine reproductive and respiratory syndrome, encephalomyocarditis virus, and possibly other viruses, may also be needed. Particular attention should be paid to viruses that can be carried by material obtained from pigs and can be zoonotic or oncogenic. Testing methods must be approved by the national regulatory authority/control laboratory.15,17,23
The manufacturer is responsible for the quality of trypsin, as well as for the quality of sera. If possible, recombinant trypsin should be used. However, it is also at risk of contamination, and therefore should be evaluated using the same criteria as any other reagent of biological origin.15
Like serum series, trypsin series are prepared from the pancreas of many species of animals. Most swine trypsin series contain the genetic sequences of type 1 parvovirus and circoviruses, so they should be inactivated by γ-irradiation. However, it is believed that these viruses are relatively resistant to inactivation.
For the use of trypsin derived from other animal species, one should consult with the national regulatory authority/control laboratory about appropriate testing methods.
If the manufacturer already used the trypsin before creating cell banks (when receiving the substrate of animal cells or during passaging), then the cell bank (master or working) should be tested for porcine parvovirus or for corresponding adventitious agents characteristic of other animal species from which the reagent was obtained. If trypsin is not used in the subsequent stages of production, then this test will not need to be repeated, since the cell bank has already been tested and found to be free of porcine parvovirus (or other relevant agents).
Other culture media additives
The quality of biologically active additives for culture media, e.g. growth factors, cytokines and antibodies, should be reflected in the certificates of analysis containing proof of their identity, purity, sterility and biological activity, as well as the absence of adventitious agents.10 It is important to ensure their traceability, evaluate and, if necessary, reduce the microbiological risk. If an alternative synthetic analogue or recombinant form exists – such as, for example, recombinant human albumin – consideration should be given to their use.
Antibiotics
It is recommended to avoid using penicillin and other beta-lactam antibiotics because of their ability to cause sensitization in patients.10
Feeder cells
In some protocols, feeder cells are used for cultivation. This practice is worrying because these cells may contain adventitious agents or cause adverse reactions. When possible, free isolation of cells is necessary, as well as their cultivation, or using a membrane between the feeder layer and stem cell culture, since this increases the viral safety of cell therapy drugs, BMCP analogues.26 Feeder cells need to be examined and/or validated for their suitability for the intended use.10
Conclusions
The assessment of the registration dossier in terms of expert quality evaluation for BMCPs should include, among other things, an expert evaluation of the production process, BMCP quality control methods, and the requirements for the quality of excipients (quality/compliance certificates, passports, specifications for excipients).
Thus, there are general requirements for biological material donors in various countries, and the main stated requirement is a comprehensive study of the history of the donor in order to identify any infectious diseases and the donor's environment, and to establish exclusion criteria to ensure the safety of persons involved in the collection, production and use of materials, as well as that of patients (recipients) who will be treated with drugs based on donor material.
Requirements for the reagents used in the production of cell therapy drugs, BMCP analogues, can be summarized as follows:
• Using reagents with a certificate of analysis, as well as those classified as “for clinical use”.
• Conformity of reagents to pharmacopoeial articles, as far as possible.
• Traceability of reagents of animal and human origin.
• Audit and qualification of the supplier to verify compliance with the requirements (preferably several trusted suppliers).
Conflicts of interest
There are no conflicts to declare.
Acknowledgments
The study was conducted as part of the state assignment to FSBI “SCEEMP” of the Ministry of Health of the Russian Federation No. 056-00023-18-02 for conducting applied research (state registration number AAAA-A18-118021590045-2).
References
- Cobo F., Stacey G. N., Hunt C., Cabrera C., Nieto A., Montes R., Cortes J. L., Catalina P., Barnie A., Concha A. Appl. Microbiol. Biotechnol. 2005;68:456–466. doi: 10.1007/s00253-005-0062-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitzler W. E., Runkel S. Clin. Lab. 2001;47:219–222. [PubMed] [Google Scholar]
- Stramer S. L., Glynn S. A., Kleinman S. H. Vox Sang. 2005;88:68–69. [Google Scholar]
- Dodd R. Y., Stramer S. L., Aberle-Grasse J., Notari E. Dev. Biol. 2000;102:19–27. [PubMed] [Google Scholar]
- Dodd, IV R. Y., Notari E. P., Stramer S. L. Transfusion. 2002;42:975–979. doi: 10.1046/j.1537-2995.2002.00174.x. [DOI] [PubMed] [Google Scholar]
- Zou S., Dodd R. Y., Stramer S. L., Strong M. D. N. Engl. J. Med. 2004;351:751–759. doi: 10.1056/NEJMoa032510. [DOI] [PubMed] [Google Scholar]
- Eligibility Determination for Donors of Human Cells, Tissues, and Cellular and Tissue-Based Products (HTC/Ps), Guidance for Industry, Food and Drug Administration, 2007. [PubMed]
- Directive 2006/17/EC of the European Parliament and of the Council, Official Journal of the European Union, 2006.
- Directive 2004/23/EC of the European Parliament and of the Council, Official Journal of the European Union, 2004.
- Guideline on human cell-based medicinal products, European Medicines Agency, 2007.
- Donor blood screening for blood-borne infections, The Recommendations, World Health Organization, 2010.
- Order of the Ministry of Health of Russia dated March 27, 2018 N 125H, “On approval of the procedure for medical examination of a donor of biological material and a list of contraindications (absolute and relative) for obtaining biological material”, 2018.
- Federal Law, On Biomedical Cellular Products, 2016.
- 1043, Ancillary materials for cell, gene, and tissue-engineered products, USP 41 - NF 36, 2017.
- Recommendations for the evaluation of animal cell cultures as substrates for the manufacture of biological medicinal products and for the characterization of cell banks, WHO Technical Report Series, 2003, vol. 978, pp. 79–187. [Google Scholar]
- Current Good Tissue Practice (CGTP) and Additional Requirements for Manufacturers of Human Cells, Tissues, and Cellural and Tissue-Based Products (HTC/Ps), Guidance for Industry, Food and Drug Administration, 2011.
- Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), Draft Guidance for Industry, Food and Drug Administration, 2018.
- ARGB Appendix 4 – Guidance on TGO 88, Australian Regulatory Guidelines for Biologicals (ARGB), Therapeutic Goods Administration, 2014.
- Dossier requirements for Class 2,3 and 4 biologicals, Australian Regulatory Guidelines for Biologicals (ARGB), Therapeutic Goods Administration, 2018.
- Terrestrial animal health code, World Organisation for Animal Health, 2019.
- Harris D. A. Curr. Top. Microbiol. Immunol. 2004;284:222. [Google Scholar]
- Guideline on the use of bovine serum in the manufacture of human biological medicinal products, European Medicines Agency, 2013, pp. 1–8.
- Melnikova E. V., Merkulova O. V., Chaplenko A. A., Rachinskaya O. A., Semenova I. S., Merkulov V. A., Olefir Y. V. Russian Journal of Biopharnaceuticals. 2017;9:27–35. [Google Scholar]
- Monograph No 04/2006:2262, Monograph for Bovine Serum, European Pharmacopoeia, 9th edn, 2016.
- 1024, Bovine serum, USP 41 - NF 36, 2017.
- Herberts C. A., Kwa M. S. G., Hermsen H. P. H. J. Transl. Med. 2011;9:29. doi: 10.1186/1479-5876-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]