Abstract
Objectives:
The purpose of this study was to examine age-related effects on esophageal transit times (ETT) among healthy adult participants.
Methods:
A total of 175 healthy, non-dysphagic participants underwent a modified barium swallow study (MBSS), and ETT was recorded for two standardized swallowing tasks. Differences across age groups were determined using Kruskal–Wallis test. Relationships between an Esophageal Clearance (Modified Barium Swallow Impairment Profile Component 17) score and ETT were also explored.
Results:
No significant differences were observed in ETT across age groups for nectar-thickened liquid (P = .335) or pudding (P = .231) consistencies. No significant differences were observed between males and females in ETT for either the nectar (P = .112) or pudding trial (P = .817). For nectar, the mean ETT for patients with Component 17 scores of 2 or greater were significantly higher than that of participants with a score of 0 (P < .0001). For pudding, participants with a score >0 demonstrated significantly higher mean ETT compared to participants with a score of 0 (with P = .0008 and P < .0001, respectively).
Conclusion:
Study findings failed to support age-related or sex-related differences in ETT for two standardized swallowing tasks administered during a MBSS in healthy individuals. The normative values following a standardized protocol in this study provide guidance in clinical interpretation of esophageal function.
Keywords: esophageal transit time, healthy, adults, MBSImP, presbyphagia
Introduction
Esophageal dysfunction is a common complaint and finding in patients referred for swallowing evaluation by speech-language pathologists.1 Therefore, esophageal visualization is increasingly becoming a standard component when patients are referred for modified barium swallow studies (MBSSs). Esophageal changes resulting from the aging process have previously been reported, including reduced esophageal peristaltic and upper and lower esophageal sphincter pressures, redirection of bolus flow, increased esophageal residue, increased transit time, and other esophageal structural anomalies.2–8 The term “presbyesophagus” was coined in the 1960s to refer to esophageal musculature deterioration resulting from healthy aging.7 The timing of bolus passage through the esophagus, or esophageal transit time (ETT), may be one useful temporal measure for assessing esophageal function.
Miles and colleagues2 investigated ETT across three swallowing conditions (20 ml thin liquid, 5 ml paste, and barium pill) under videofluoroscopy in 118 healthy adults ranging from 20 to 98 years of age. Results revealed ETT for 20 ml of thin liquid significantly increased with age; however, this finding was not observed for the paste and or pill trials. While this work contributes to normative values using a standardized protocol and assists with clinical interpretation of esophageal visualization during videofluoroscopy, the wide variations of ETT during the paste and pill trials make it increasingly difficult to distinguish normal variance from dysfunction. Additionally, radiation exposure time was limited to 60 seconds per swallow trial, and therefore, ETT may have been underestimated when bolus remains in the esophagus beyond this time limit. Further investigation of ETT in larger cohorts of healthy adults will continue to improve accuracy of normative ranges, particularly across standardized videofluoroscopic protocols routinely used in clinical settings such as the Modified Barium Swallow Impairment Profile (MBSImP).9–10 The MBSImP assesses 17 physiologic components of swallowing, including one component related to esophageal clearance (Component 17) assessed in the anteroposterior viewing plane.9–10 Component 17 is derived from two trials administered in the anteroposterior viewing plane – 5 ml nectar-thickened liquid and 5 ml pudding.9–10
The purpose of this study was to examine aging effects on ETT observed during videofluoroscopy in the upright position and anteroposterior viewing plane during standardized administration of two swallowing trials in healthy, non-dysphagic adults. Furthermore, we investigated sex differences on ETT, and the relationship between ETT and Esophageal Clearance score (MBSImP Component 17). Consistent with previous evidence,2 we did not anticipate to find age or sex differences on ETT. We did hypothesize, however, that higher ETTs would be associated with higher (worse) Component 17 scores.
Methods
This study received approval after full review by the Institutional Review Board and Department of Radiology at the university where data collection occurred. Informed consent procedures were in accordance with the ethical standards of the responsible committee on human experimentation. Written informed consent was obtained from all study participants prior to initiation of study procedures.
Participants
Participants in this study included a normative dataset of 195 healthy, non-dysphagic, community-dwelling adults who underwent a modified barium swallow study (MBSS) as part of a larger study investigating aging effects on oropharyngeal swallowing function. Inclusion criteria were as follows: (1) ≥21 years of age; (2) no history of dysphagia or current swallowing complaints; and (3) able to drink thin liquids and eat solid foods as part of a regular diet without restrictions. Exclusion criteria included participant report of: (1) known allergies to barium or materials used during MBSS; (2) upper aerodigestive tract surgical procedures (eg, head or neck resections); (3) large hiatal hernia (>2 cm); (4) pulmonary disease (eg, chronic obstruction pulmonary disease); (5) head and neck cancer; (6) neurological insult/disease (eg, stroke, Parkinson’s disease); and/or (7) pregnancy or suspected pregnancy. Participants were recruited via word-of-mouth and advertisements within the community surrounding the university where data collection occurred.
Modified Barium Swallow Study
Each standing participant was initially positioned in a lateral view with visualization of the oropharyngeal region and the cervical esophagus. Participants were administered 10 barium swallowing trials (Varibar®, Bracco Diagnostics, Inc.) of increasing volume and viscosity following the previously published MBSImP standardized procedure.9–10 Participants were then repositioned into the anteroposterior viewing plane and subsequently presented with a 5 ml nectar-thickened (300 centipoize (cps), 40% weight/volume (w/v)) liquid trial via spoon and a 5 ml pudding (5750 cps, 40% w/v) trial via spoon per MBSImP protocol.9–10 Continuous fluoroscopy was used and recordings were made with a resolution of 30 digital frames per second. A digital recording device (Digital Swallowing Workstation Model 7100, Kay Elemetrics Corp.; TIMS DICOM System, TIMS Medical) connected to a fluoroscopy system (GE Healthcare; GE Precision 500 FP model) was used for image signal acquisition, digital storage, and data retrieval. Only the two standardized trials administered in the anteroposterior viewing plane (5 ml nectar and 5 ml pudding) were extracted for purposes of the current study.
Measures
MBSS recordings were converted to .avi files. Files were viewed using QuickTime Player and analyzed using real-time and frame-by-frame viewing. ETT onset was operationally defined at the first frame when the bolus entered the esophagus at the level of the inferior segment of the true vocal folds to the frame when the bolus head passed through the lower esophageal sphincter (LES) (Figure 1). Author LC calculated ETT in seconds.
Figure 1.
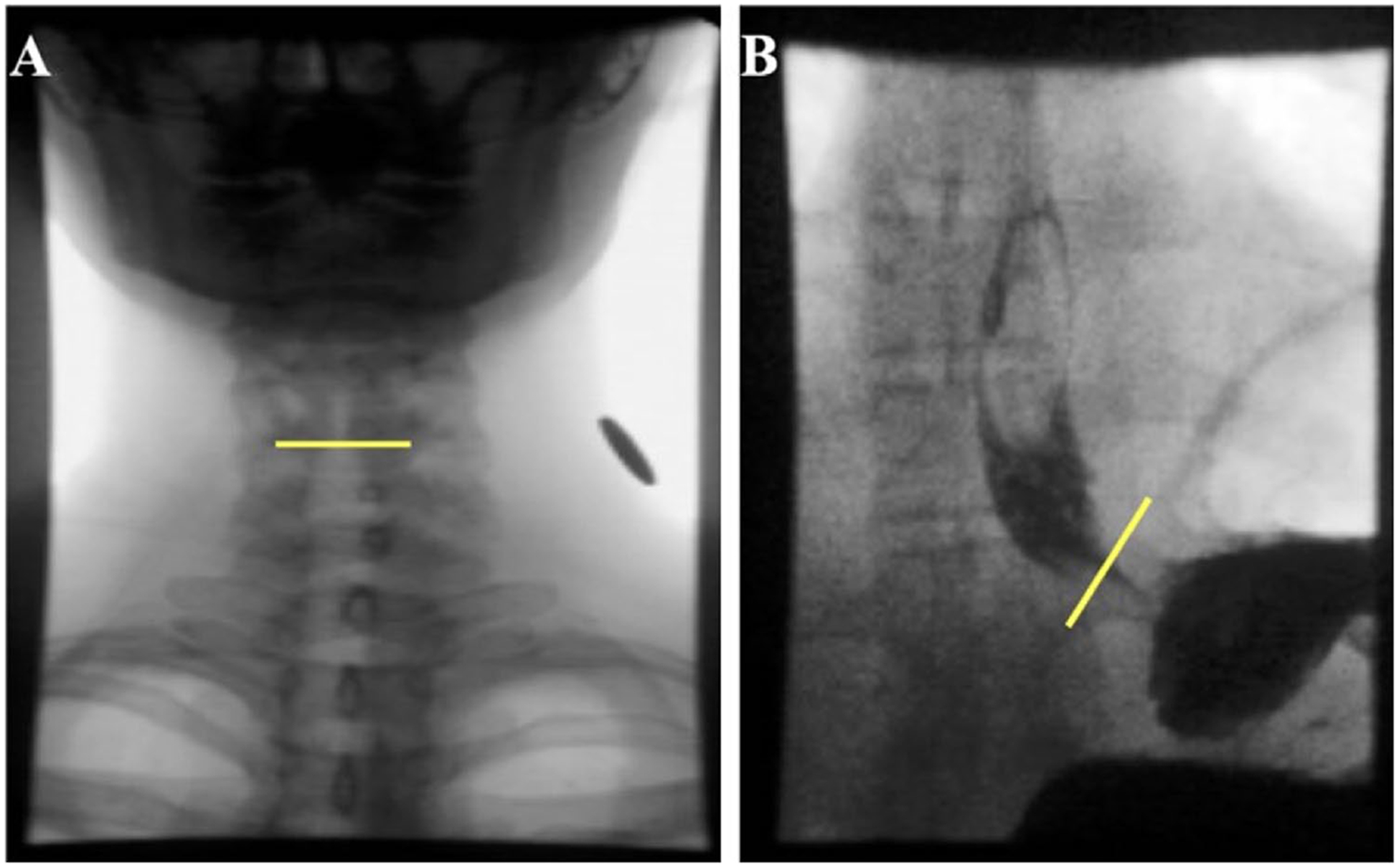
Calculation of ETT (seconds). (A) Yellow line indicates inferior edge of true vocal folds. ETT was initiated at the first frame when the bolus entered the esophagus at the level of the inferior segment of the true vocal folds. (B) ETT was terminated when bolus head passed lower esophageal sphincter.
Two speech-language pathologists (authors KLG and KHD) with dysphagia expertise and combined experience of over 20 years provided the MBSImP Component 17 scores using consensus scoring. Component 17 scoring system is as follows: 0 = complete esophageal clearance or esophageal coating; 1 = esophageal retention; 2 = esophageal retention with retrograde flow below pharyngoesophageal segment (PES); 3 = esophageal retention with retrograde flow through PES; and 4 = minimal to no esophageal clearance.9–10 Thus, higher scores indicate worse functioning. A score of 4 was assigned when the first swallow did not clear the bolus through the LES. The bolus cleared on a subsequent swallow but this was not recorded, and per scoring protocol,9–10 only the first swallow was interpreted.
ETT Reliability
To establish inter-rater reliability, 20% of MBSS recordings were randomly selected and ETT was calculated by author KLG. Pearson’s correlation coefficient revealed high inter-rater agreement (r = 0.987, P < .0001).
Data Analysis
Descriptive measures were calculated across both swallowing tasks. Participants were grouped across four age groups: 21 to 39 years, 40 to 59 years, 60 to 79 years, and 80 years and older. The Kruskal–Wallis Test and Mann–Whitney U Test were used to test whether significant differences exist in ETT across age groups and between sexes, respectively. The relationship between MBSImP Component 17 score and ETT was studied using Spearman’s correlation coefficient, and the mean ETT values were compared among different MBSImP Component 17 scores. Because of the low cell frequencies in the higher MBSImP component score categories, scores were reduced to 0, 1, and 2 (with the latter including scores 2 and greater) for purposes of analysis. Two-tailed P-values <.05 determined statistical significance.
Results
Twenty participants were excluded when ETT could not be calculated for either swallow task due to one or more of the following reasons: a liquid wash or double swallow to clear bolus from esophagus was recorded which precluded reliable ETT calculation for initial swallow; fluoroscopy was turned off prior to bolus entrance through LES; or poor visualization (eg, dark) of esophageal bolus movement. Therefore, a total of 175 participants (98 females, 77 males) were included in the analysis. Demographic information is provided in Table 1. Overall mean (± SD) ETTs for nectar and pudding trials were 6.7 (±2.8) and 8.2 (±4.2) seconds, respectively.
Table 1.
Participant Demographics.
| Variable | Total |
|---|---|
| Age (years) | |
| Mean ± SD | 46.3 ± 17.2 |
| Range | 21–89 |
| Sex | |
| Female | 98 (56%) |
| Male | 77 (44%) |
| Race | |
| White/Caucasian | 127 (72.6%) |
| Black/African-American | 41 (23.4%) |
| Other | 7 (4.0%) |
| Ethnicity | |
| Non-Hispanic/Non-Latino | 171 (97.7%) |
| Hispanic/Latino | 4 (2.3%) |
Frequency and percent are presented unless otherwise reported.
Esophageal Transit Times across Age Groups
Descriptive statistics for ETT across age groups are provided in Table 2. Findings revealed no significant differences in ETT across age groups for either the nectar (X2 = 3.39, df = 3, P = .335) or pudding trial (X2 = 4.30, df = 3, P = .231). Results remained nonsignificant after collapsing the two oldest age groups. Scatterplots further demonstrating the lack of association between age and ETT for both nectar and pudding trials are provided in Figure 2.
Table 2.
Comparison ETT (seconds) Across Age Groups and Between Sexes for Nectar and Pudding Consistencies.
| Nectar | Pudding | |||
|---|---|---|---|---|
| Mean ± SD (95% CI) | Range | Mean ± SD (95% CI) | Range | |
| 21 −39 years (n = 65) | 6.8 ± 3.7 | 4.0–27.0 | 8.8 ± 4.6 | 4.9–26.8 |
| (5.9, 7.8) | (7.5, 10.1) | |||
| 40–59 years (n = 66) | 6.8 ± 2.4 | 3.7–19.1 | 8.4 ± 4.4 | 4.2–26.8 |
| (6.1, 7.4) | (7.2, 9.6) | |||
| 60–79 years (n = 38) | 6.2 ± 1.3 | 4.1–10.3 | 7.3 ± 3.3 | 4.5–23.7 |
| (5.7, 6.6) | (6.2, 8.5) | |||
| 80+ years (n = 6) | 6.6 ± 2.2 | 4.7–10.1 | 6.8 ± 0.9 | 5.5–7.4 |
| (3.8, 9.3) | (5.4, 8.2) | |||
| Female (n = 98) | 6.4 ± 2.1 | 4.1–19.1 | 8.4 ± 4.4 | 4.5–26.8 |
| (5.9, 6.9) | (7.4, 9.4) | |||
| Male (n = 77) | 7.0 ± 3.5 | 3.7–27.0 | 8.0 ± 3.9 | 4.2–26.8 |
| (6.1, 7.8) | (7.0, 9.0) | |||
Figure 2.
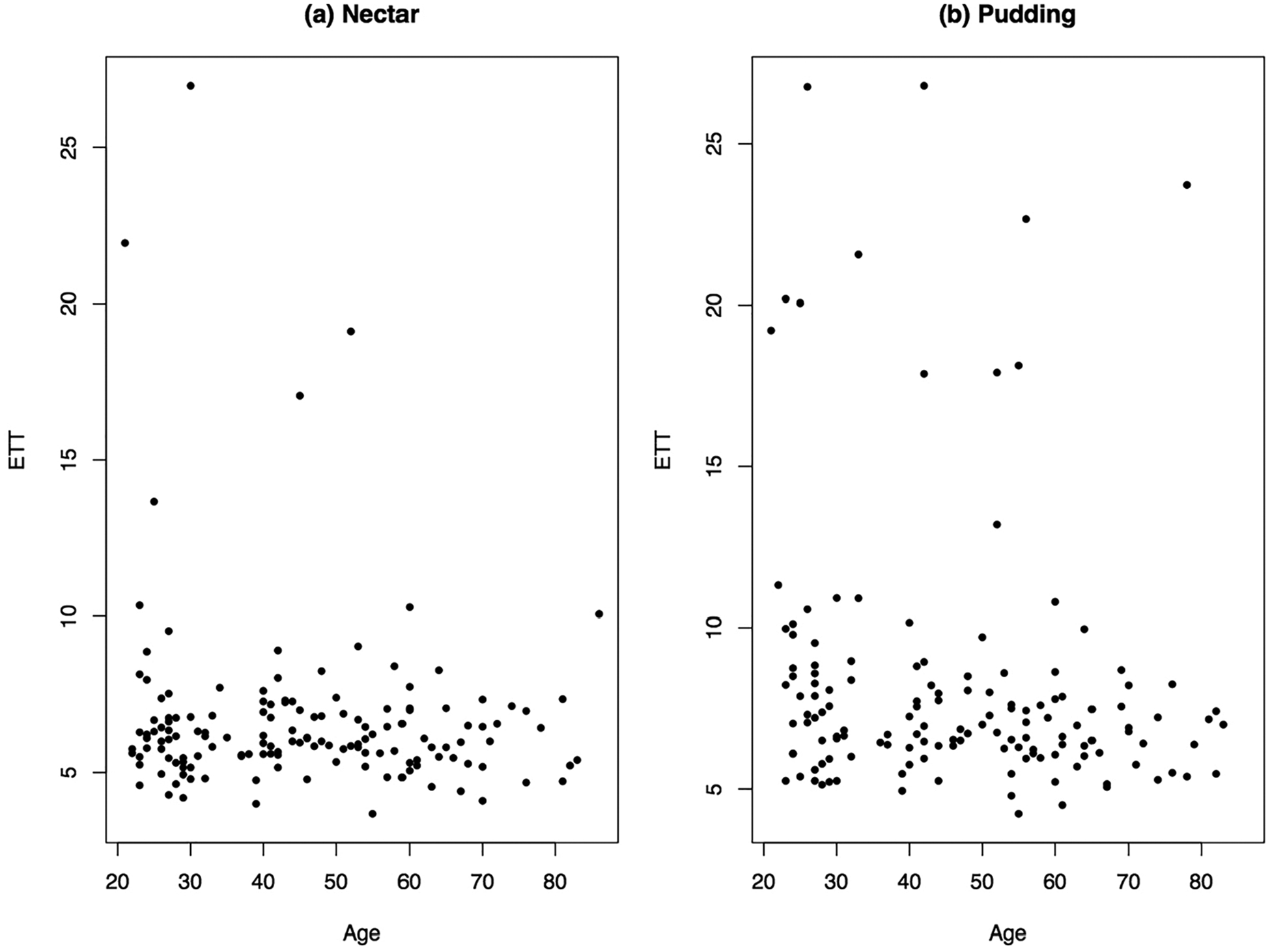
Scatterplots comparing age and ETT (seconds) across nectar (A) and pudding (B) trials.
Esophageal Transit Times between Sexes
Descriptive information for ETT between sexes is provided in Table 2. No significant differences were observed between sexes in ETT for either the nectar (W = 2409, P = .112) or pudding trial (W = 2516, P = .817).
MBSImP Component 17 and ETT
Distribution of raw MBSImP 17 component scores are provided in Table 3. Majority of participants earned a score of 0 across both nectar and pudding trials. There was a significant positive relationship between MBSImP Component 17 scores and ETT for both nectar (Spearman rho = 0.26, P = .001) and pudding (Spearman rho = 0.339, P < .0001) trials (Figure 3). For nectar consistency, the mean ETT for patients with scores 2 or greater, were significantly higher than participants with a score of 0 (W = 285, P = .0008). All patients with an ETT >15 seconds also were observed to esophageal scores 2 and greater on the nectar task. For pudding consistency, participants with a score of 1 demonstrated significantly higher mean ETT compared to participants with a score of 0 (W = 1303.5, P = .04). Similarly, participants with a score of 2 and greater had significantly higher mean ETT compared with participants with a score of 0 (W = 258, P < .0001). All patients with an ETT >15 seconds also were observed to esophageal scores >0 on the pudding task. If esophageal scores increased by 1, the average increase for ETT was 1.4 and 2.2 seconds for nectar and pudding trials, respectively (t = 4.831, df = 147 for nectar and t = 4.825, df = 137 for pudding; both with P < .0001).
Table 3.
Distribution of Raw MBSImP Component 17 Scores Across Nectar and Pudding Consistencies.
| 0 | 1 | 2 | 4 | |
|---|---|---|---|---|
| Nectar (N = 175) | 114 (65) | 43 (25) | 15 (9) | 3 (2) |
| Pudding (N = 140) | 80 (46) | 41 (23) | 19 (11) | 0 (0) |
| 21 −39 years | ||||
| Nectar (n = 65) | 42 (65) | 20 (31) | 3 (5) | 0 (0) |
| Pudding (n = 53) | 28 (53) | 16 (30) | 9 (17) | 0 (0) |
| 40–59 years | ||||
| Nectar (n = 66) | 41 (62) | 14 (21) | 9 (14) | 2 (3) |
| Pudding (n = 51) | 27 (53) | 16 (31) | 8 (16) | 0 (0) |
| 60–79 years | ||||
| Nectar (n = 38) | 28 (74) | 7 (18) | 2 (5) | 1 (3) |
| Pudding (n = 31) | 22 (71) | 7 (23) | 2 (6) | 0 (0) |
| 80+ years | ||||
| Nectar (n = 6) | 3 (50) | 2 (33) | 1 (17) | 0 (0) |
| Pudding (n = 5) | 3 (60) | 2 (40) | 0 (0) | 0 (0) |
Frequency and rounded percent are presented. A score of 3 is not represented in since no participant earned this score.
Abbreviations: ETT, esophageal transit time; MBSImP, Modified Barium Swallow Impairment Profile.
Figure 3.
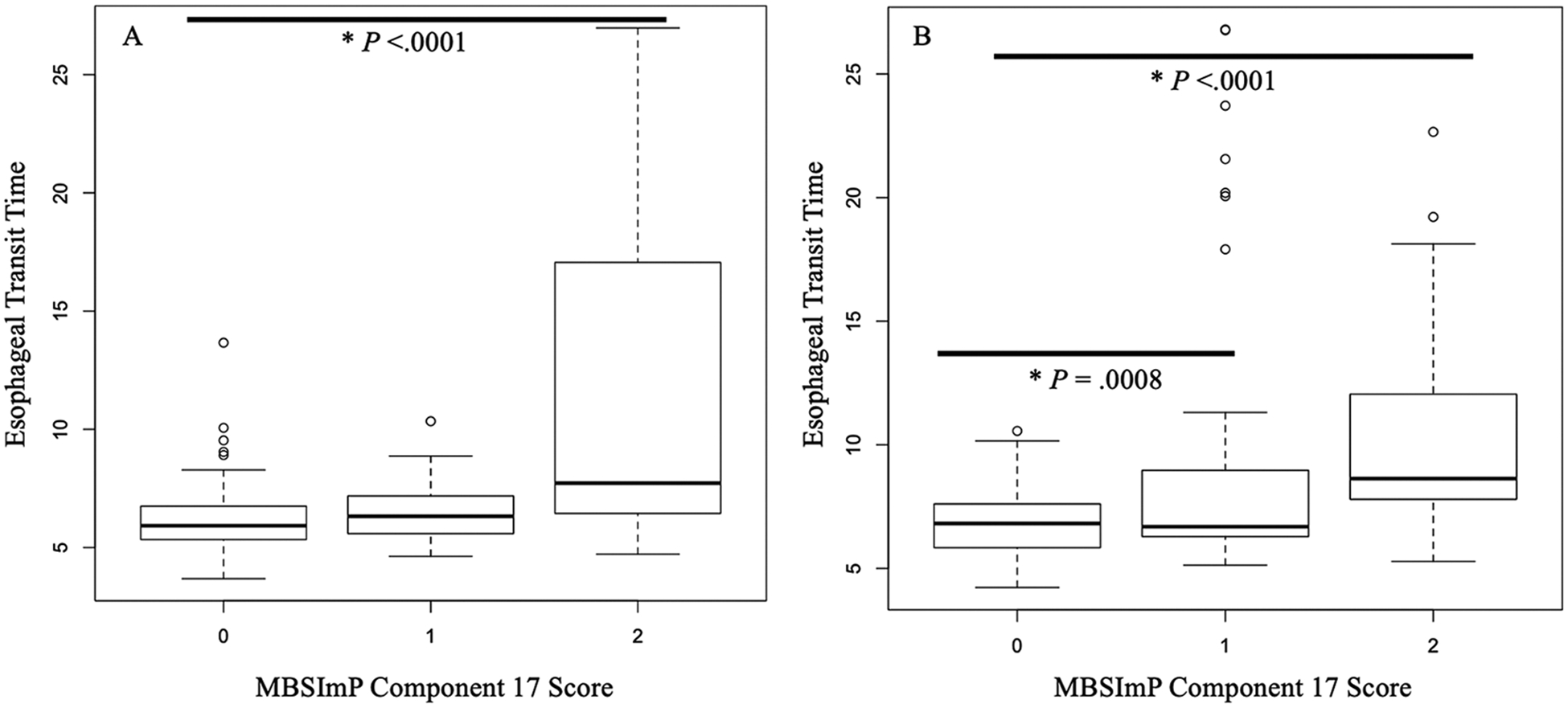
(A) Boxplots comparing ETT (seconds) across MBSImP Component 17 scores for nectar swallowing trial. Circle indicates outlier. (B) Boxplots comparing ETT (seconds) across MBSImP Component 17 scores for pudding swallowing trial. Circle indicates outlier.
Discussion
The swallow continuum is initiated when a bolus enters the mouth and terminates when it reaches the stomach. Therefore, esophageal visualization is a crucial component of a comprehensive swallow assessment employing imaging techniques.13 This study contributes to the current literature by providing normative data for ETT using a protocol standardized for consistency and volume (5 ml nectar and 5 ml pudding), participant positioning (standing) and viewing plane anteroposterior in healthy adults. Variability in ETT ranges were observed across age groups for both standardized swallowing tasks tested, similar to previous reports.2 Current study findings failed to support statistically significant age-related differences in ETT. Participants under the age of 60 years tended to have longer ETTs with larger variations than those older than 60, but again, these results were not significant. Similarly, unpublished data failed to reveal significant aging effects for Component 17. Lack of aging effects in the current study compared to the aging effects observed in Miles et al2 may be attributed to the different consistencies/volumes used. Miles and colleagues observed a significant age effect during large volume of thin liquid. Unfortunately, the current study did not evaluate ETT in thin liquid trials since thin liquid trials are not administered in the anteroposterior viewing plane using the standardized MBSImP protocol. However, our findings corroborate the results reported by Miles and colleagues2 which did not find an age-related effect on their paste trial (similar to the pudding consistency in the current study). Although current study findings also failed to support statistically significant sex-related differences in ETT, females were observed to have smaller ETTs compared to males for the nectar consistency, but the opposite trend was observed for pudding.
Longer ETTs were associated with higher scores on MBSImP Component 17, suggesting longer bolus transit times through the esophagus may indicate esophageal dysfunction. MBSImP Component 17 describes the presence of material remaining in the esophagus in the upright position and whether there is retrograde flow of contrast material, and if so, to what level (above or below the pharyngoesophageal segment (PES)). The component is included on the MBSImP because of the evidence supporting associations between esophageal impairment and oropharyngeal swallowing impairment.11–12 Esophageal swallowing function is multifactorial with timing of bolus clearance representing only one factor. For example, Component 17 scores of (2), esophageal retention with retrograde flow below the level of the PES, and (3), esophageal retention with retrograde flow above the level of the PES, may have a similar ETT, but the clinical implications related to severity and airway invasion risk differ. Complete esophageal assessment requires examination of esophageal structure and motility pressures that go beyond the scope of the MBSS and include a team of specialists including radiologists, gastroenterologists and otolaryngologists.
Limitations
Despite the large sample size of 175 in the current study, only six participants formed the oldest age category (80+ years). A larger cohort of healthy adults 80 years and older would allow further exploration of aging effects on ETT. Another limitation includes the selected standardized barium contrast agents (ie, one trial each of 5 ml nectar and 5 ml pudding), which provide normative data for only those clinicians using the same viscosities (cps), volumes and radiopacities (w/v). Thus, the ETTs presented in the current study are only comparable to those using the same protocol and interpretation method. Further, previous evidence revealed positional influences on ETT with gravitational influences resulting in shortening ETT in the upright position.14 Comparisons with other studies, therefore, can only be made with studies also incorporating upright positioning. Next, we did not screen for gastroesophageal reflux disease (GERD). Patients with gastroesophageal reflux disease have demonstrated with slower bolus transit times.15 Future studies should specifically evaluate for GERD and its impact on ETTs. Lastly, studies were excluded if the patient required a double swallow or liquid wash to clear the esophagus or if fluoroscopy was turned off prior to bolus head passing through the LES. One can assume these patients likely demonstrated with increased ETT, resulting from either requiring a behavioral intervention to clear esophageal stasis or if there was concern for further radiation exposure. Therefore, we were unable to determine the exact upper limits of ETTs for all participants across both swallow trials limiting the range of ETT data reported here.
Despite these limitations, current study findings contribute to development of a normative database for ETT. These values are essential in providing guidance and information when monitoring esophageal bolus transport during videofluoroscopy, specifically related to classification of what is normal versus abnormal esophageal swallowing patterns. Accordingly, substantial deviations from normative data should not be equated with typical aging and should encourage clinicians to refer for further assessment.7
Conclusion
Esophageal imaging is recommended to be routinely performed during MBSS. Normative data for ETTs are needed to enhance clinical interpretation and subsequent referral and intervention. This study examined ETTs in a large sample of healthy, non-dysphagic, community-dwelling adults. Overall, current study findings failed to support age-related or sex-related differences in ETT for two standardized swallowing tasks administered during a MBSS. Ongoing investigation accruing individuals 80 years and older will address the current study limitations relative to imbalance in the sample across age categories and between sexes. This will further contribute to development of a normative database for ETT observed in the upright position under videofluoroscopy allowing clinicians to make timely referrals when suspected abnormalities are observed.
Acknowledgments
The authors would like to acknowledge Mrs. Julie Blair and Dr. R. Jordan Hazelwood for their assistance with data collection and scoring. Further, the authors would like to acknowledge Ms. Brittni Carnes and Mr. Cephus Simmons for their assistance with data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this work was supported by the Veterans Affairs [RR&D 1IK1RX001628-01A to K.G.]; American Speech-Language-Hearing Foundation to K.G.; and the National Institutes of Health, [NIH/NCATS TL1R000061 to K.G., [NIH/NIDCD 1K24DC12801] to B.M-H.].
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Miles A, McMillan J, Ward K, Allen J. Esophageal visualization as an adjunct to the videofluoroscopic study of swallowing. Otolaryngol Head Neck Surg. 2015;152(3):488–493. [DOI] [PubMed] [Google Scholar]
- 2.Miles A, Clark S, Jardine M, Allen J. Esophageal swallowing timing measures in healthy adults during videofluoroscopy. Ann Otol Rhinol Laryngol. 2016;125(9):764–769. [DOI] [PubMed] [Google Scholar]
- 3.Grishaw EK, Ott DJ, Frederick MG, Gelfand DW, Chen MYM. Functional abnormalities of the esophagus: a prospective analysis of radiographic findings relative to age and symptoms. Am J Roentgenol. 1996;167(3):719–723. [DOI] [PubMed] [Google Scholar]
- 4.Grande L, Lacima G, Ros E, et al. Deterioration of esophageal motility with age: a manometric study of 79 healthy subjects. Am J Gastroenterol. 1999;94(7):1795–1801. [DOI] [PubMed] [Google Scholar]
- 5.Jou J, Radowsky J, Gangnon R, et al. Esophageal clearance patterns in normal older adults as documented with videofluoroscopic esophagram. Gastroenterol Res Prac. 2009;2009:1–6. doi: 10.1155/2009/965062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lock G. Physiology and pathology of the oesophagus in the elderly patient. Best Pract Res Clin Gastroenterol. 2001;15(6):919–941. [DOI] [PubMed] [Google Scholar]
- 7.Jardine M, Miles A, Allen J. A systematic review of physiological changes in swallowing in the oldest old [published online ahead of print September 5, 2019]. Dysphagia. doi: 10.1007/s00455-019-10056-3 [DOI] [PubMed] [Google Scholar]
- 8.Robbins J, Bridges AD, Taylor A. Oral, pharyngeal and esophageal motor function in aging. GI Motil Online. 2006. doi: 10.1038/gimo39 [DOI] [Google Scholar]
- 9.Martin-Harris B, Brodsky MB, Michel Y, et al. MBS measurement tool for swallow impairment – MBSImp: establishing a standard. Dysphagia. 2008;23(4):392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin-Harris B, Humphries K, (Focht) Garand KL. The modified barium swallow impairment profile (MBSImP™©) – innovation, dissemination and implementation. Perspect Swallow Dis (SIG13). 2017;2(13):129–138. [Google Scholar]
- 11.Gullung JL, Hill EG, Castell DO, Martin-Harris B. Oropharygneal and esophageal swallowing impairments: their association and the predictive value of the modified barium swallow impairment profile and combined multichannel intraluminal impedance-esophageal manometry. Ann Otol Rhinol Laryngol. 2012;121(11):738–745. [DOI] [PubMed] [Google Scholar]
- 12.Allen JE, White C, Leonard R, Belafsky PC. Comparison of esophageal screen findings on videofluoroscopy with full esophagram results. Head Neck. 2012;34(2): 264–269. [DOI] [PubMed] [Google Scholar]
- 13.Watts S, Gaziano J, Jacobs J, Richter J. Improving the diagnostic capability of the modified barium swallow study through standardization of an esophageal sweep protocol. Dysphagia. 2019;34(1):34–42. [DOI] [PubMed] [Google Scholar]
- 14.Cordova-Fraga T, Sosa M, Wiechers C, et al. Effects of anatomical position on esophageal transit time: a bio-magnetic diagnostic technique. World J Gastroenterol. 2008;14(37):5707–5711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cho YK, Choi M-G, Lim CH, et al. Impaired esophageal bolus transit in patients with gastroesophageal reflux disease and abnormal esophageal acid exposure. Gut Liver. 2012;6(4):440–445. [DOI] [PMC free article] [PubMed] [Google Scholar]


