Abstract
To analyze the stress distribution of the maxillary central incisor with oblique fracture, repaired by different methods, using 3-dimensional finite element analysis. From the biomechanical point of view, it is expected to provide a reference for clinical selection of restoration method which is more conducive to stress distribution and preservation of dental tissue as much as possible.
Use cone beam CT and finite element software to establish the finite element models of the maxillary central incisor with oblique fracture, and then create models according to 5 repairing methods(A. fiber post-core-crown group; B. cast post-core-crown group; C.3 mm deep endocrown; D.4 mm deep endocrown; E.5 mm deep endocrown)after root canal treatment, and analyze the Von Mises equivalent stress and maximum principal stress distribution and peak value of each model.
When the height of dentin ferrule was fixed, the value of the Von Mises equivalent stress and the maximum principal stress in residual tooth tissue: group A was the highest, and there was no significant difference in group B, C, D and E. And the stress distribution area of 5 groups were the same. In prosthodontic layer: group B was the highest, while group A was the lowest, and the stress peak slightly increased with the increase of depth in group C, D and E. And the 5 groups were with the same stress distribution area as well. In adhesive layer: group A was the highest, while group B was the lowest, and there was little difference among group C, D and E. Group A was concentrated in 1/3 of the post tip, while group B,C,D and E were concentrated in 1/3 of the post and the post tips.
Complete and high enough dentin ferrule is a requirement for repairing heavily defected maxillary central incisor with fiber post-core crown and cast post-core crown. When the dentin ferrule is incomplete, the stress distribution of the endocrown is more excellent than post-core-crown. And the endocrown with a depth of 3 mm retainer may be the best repair method. As for post-core crown restoration, the cast post-core crown is more favorable for the uniform distribution of residual tooth tissue than the fiber post-core crown.
Keywords: dentin ferrule, endocrown, maxillary central incisor, post-core-crown, 3-dimensional finite element analysis
1. Introduction
The anterior teeth are prone to deep oblique fracture, especially in pediatric patients. The residual root or crown is often irregular, and it is difficult to prepare a complete dentin ferrule with sufficient height clinically. Furthermore, the lateral force on the maxillary central incisor during food cutting process poses a great challenge to the repair method. So the restoration should be functionally optimal to bear high stress concentration (eg, patients with seizures).[1] Teeth with large defects are usually repaired by post-core-crown after root canal treatment.[2] The use of fiber or cast post requires the preparation of the root canal, which may reduce the flexural resistance of the remaining teeth.[3] Endocrown is a ceramic restoration workpiece comprising the entire crown and an integrated apically protruding retention part. The underside and retention part of the bulk endocrown are designed and machined to fit to an ‘endo-preparation’or ‘root preparation’ which is done in case of non-vital endodontically treated teeth showing complete loss of their coronal hard tissues.[4] Since they are produced from a single piece, endocrown presents the advantage of reducing the interface of the restorative system in clinical work.[5] In general, it is recommended to use endocrown in the case of supragingival defect, short and narrow root canal or limited occlusal space.[6] However there is only a few studies concentrated on endocrown in the anterior teeth.[7] And there is no agreement on which material or technique is most effective in repairing teeth after root canal treatment.[8] In this study, finite element method was used to investigate the stress distribution of the maxillary central incisor with oblique fracture, which was repaired by different methods, providing a reference for clinical selection of restoration methods that were more conducive to the stress distribution and preserve as much tooth tissue as possible from the perspective of biomechanics.
2. Materials and methods
2.1. Experimental equipments and materials
Complete right maxillary central incisor extracted due to periodontitis (provided by the Department of Maxillofacial Surgery, Affiliated Stomatological Hospital of Southwest Medical University, with informed consent of the patient), cone beam CT (Siemens, Germany), Mimics19.0(Materialise, Belgium), Geomagic 2015(Raindrop Geomagic), Solidworks 2014 (Dassault Systemes S.A, France), ANSYS 17.0 software (ANSYS)
2.2. Solid and FE models preparation
The complete right maxillary central incisor extracted due to periodontitis was selected (the size was conformed to the national average data, specifically the length of crown was 10 mm, the length of root was 12.5 mm, and the mesiodistal dimension of the crown was 8.5 mm), and was embedded with polymethy methacrylate to form a 2 cm diameter and 4 cm height cylindrical block, for cone beam CT scanning. The embedded wax block was fixed on the dental cone beam CT occlusal frame to ensure that the tooth was within the scanning range, and the long axis of the tooth was perpendicular to the scanning section. The thickness of scanning layer was 200 μm, and the parameters were 90Kv,10mAs. The scanning detector scanned a circle around the long axis of the tooth, and the scanning data were output in DICOM format. The alveolar bone was outputted from the CT data of healthy patients in DICOM format, and the alveolar bone model of central incisor was established and preserved by Mimics software.
Imported the CT data into Mimics 19.0 software, and then defined sagittal plane, coronal plane and cross section respectively, and distributed multiple pieces of DICOM sequence data in an orderly manner. The grayscale images of teeth, cortical bone and cancellous bone (the CT data of alveolar bone come from healthy patients) can be obtained in it. First of all, the resolution and smoothness of the image were improved by preprocessing the image. Especially for the bone marrow cavity, the discontinuous area should be removed, and the selection tool of Mimics software was used to regularize the bone marrow cavity. Then, the image was segmented and the models of tooth, cortical bone and cancellous bone were extracted. Use the dynamic region growth method of the software, by setting thresholding the models of alveolar bone and teeth were established, and then merged and saved in STL file format.[9]
The STL file of the maxillary central incisor and alveolar bone model was imported into the Geomagic 2015 software, and the migration command and Boolean algorithm were used to generate the periodontal membrane model with a thickness of 0.2 mm and the cortical bone model with a thickness of 2 mm, respectively. Then the automatic curved surface was used to obtain the solid geometric model of the tooth- periodontal ligament-cortical bone-cancellous bone saved in IGS format. In Solidworks 2014, the model of 3 M Rely Fiber Post(medium), cast post, and endocrown was established through sketch command and stretch command. Fiber post model: diameter 1.6 mm, taper 0.08, taper length 10 mm, total length 20 mm; The height of the core was 8 mm, and the crown edge was a 90° shoulder with a width of 1 mm. The shoulder was located at the cemento–enamel junction. The shape of the all-ceramic crown was made according to the shape of the crown in vitro, and the root tip retained the 4 mm gutta pertscha. Endocrown model: The retainer diameter was 2 mm, the axial wall abducted at an Angle of 2°, the depth of the retainer was 3 mm,4 mm,5 mm respectively. The edge formed an annular butt-joint shoulder retainer and the orifice of root canal was sealed with flowing resin 1 mm below the retainer. The resin adhesive layer of 0.1 mm thick was simulated outside the fiber post, cast post and endocrown. All solid models were exported in x_t format and the above geometric models were imported into the finite element analysis software ANSYS Workbench 17.0. Tetrahedral elements were used for mesh division. The number of units and nodes generated was shown in Table 1. The schematic diagram of the model grid was shown in Figure1.
Table 1.
The number of nodes and units of each model.
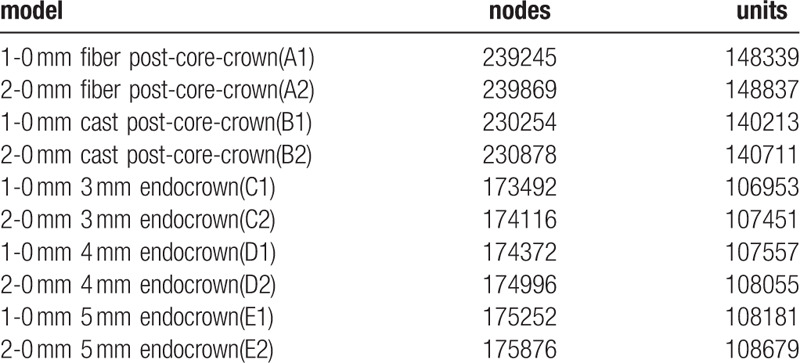
Figure 1.
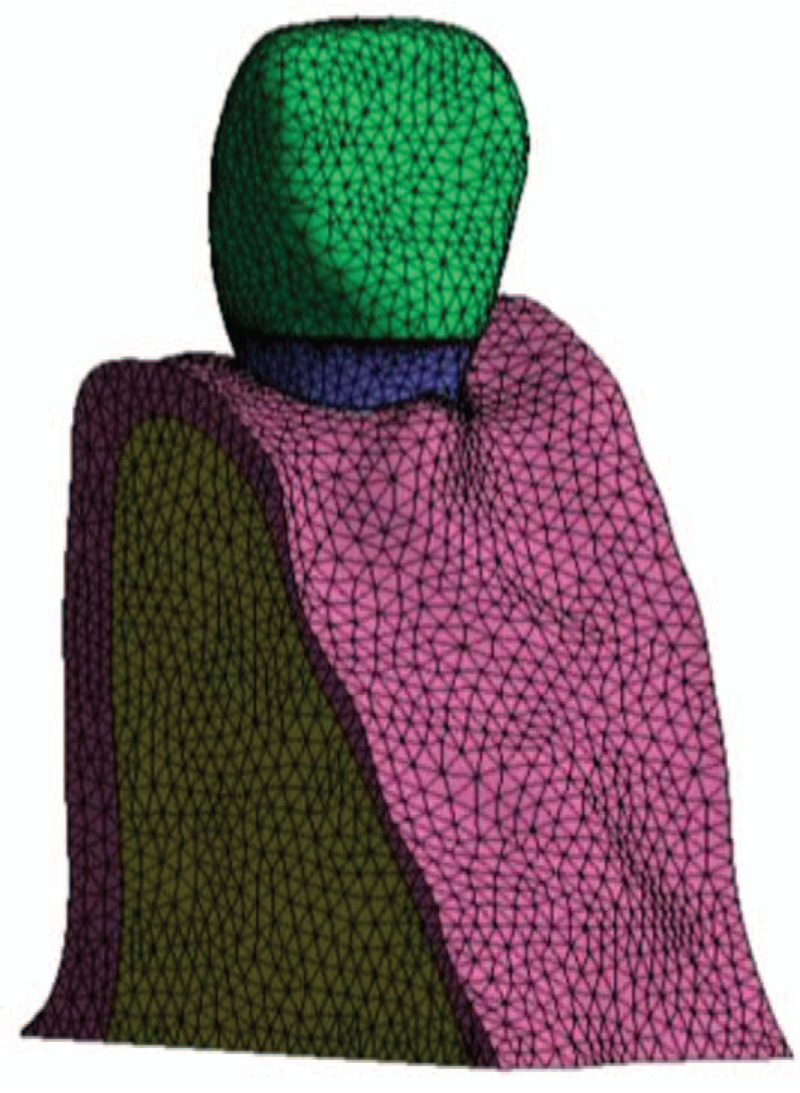
Grid diagram of a complete model.
2.3. Model design and group
An oblique fracturing crown model of the maxillary central incisor was established, and the height of the tooth at cemento–enamel junction was set as 0 mm. The mesial-distal remaining tooth height is:1 to 0 mm,2 to 0 mm. Five groups of models were established according to different repair methods:
-
A.
fiber post-core-crown group
-
B.
cast post-core-crown group
-
C.
3 mm deep endocrown
-
D.
4 mm deep endocrown
-
E.
5 mm deep endocrown
A1, B1, C1, D1, E1 represent tooth with 1 mm high dentin ferrule repaired by 5 different repairing methods, respectively. And A2, B2, C2, D2, E2 represent tooth with 2 mm high dentin ferrule.
2.4. Experimental assumptions, boundary conditions, and parameter Settings
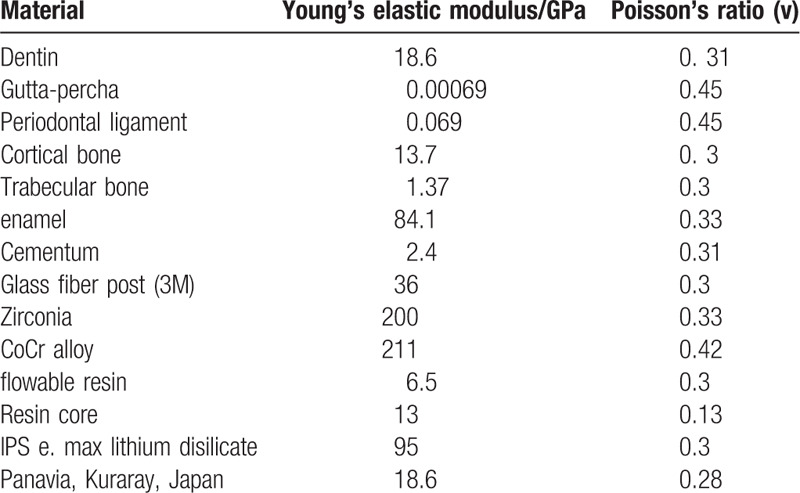
The materials and tissues in the model were assumed to be linear elastomers with continuous homogeneous isotropy and meet the conditions of small deformation, the continuous interface of each part of the model was set as a fixed contact boundary condition, and the specific mechanical parameters of each material were shown in Table 2; Among them, Panavia F adhesive (Panavia, Kuraray, Japan) can be used as a high efficiency adhesive, which can be used for fiber or cast post-core-crown, and also endocrown.[5] And endocrowns made by lithium disilicate–based ceramics are considered as the best restorative materials[10,11] because of their adhesive properties.
Table 2.
Material mechanical parameters.
2.5. Loading method
The maximum bite force of the maxillary central incisor averaged 12.0 kg (117.6N).[12] The experiment simulated clinical occlusal loading: a static loading force of 100 N in the direction of 45 with the axis of the tooth was applied at the junction of cutting 1/3 and middle 1/3 of the lingual surface of the porcelain crown, and the loading area was 2 mm2.
2.6. Stress analysis methods and indicators
The distribution and stress peak of the Von Mises stress and the maximum principal stress in residual dental tissue, dental prosthesis and adhesive layer in each group were recorded and analyzed.
3. Results
The distribution and value of the Von Mises equivalent stress of the residual dentin, dental prosthesis and adhesive layer of each model which repaired by different methods was shown in Figure 2 and Figure 3
Figure 2.
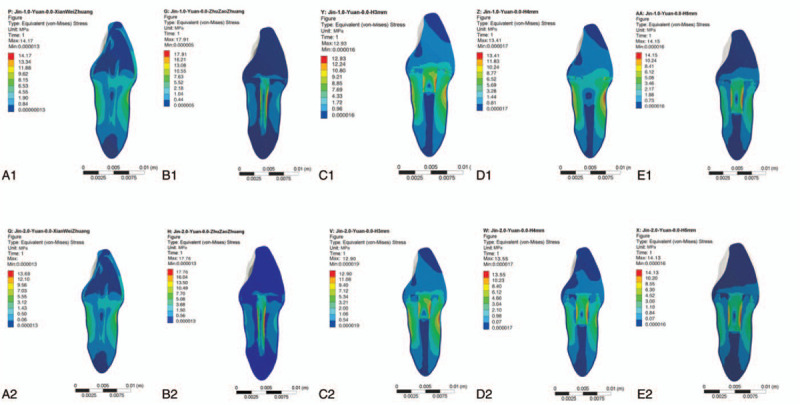
The Von Mises stress of the oblique defective maxillary central incisor restored with different methods.
Figure 3.

The Von mises stress value and the maximum principal stress value of each layer in each model.
From the figure above:
-
(1)
When the height of dentin ferrule was fixed, the value of the Von Mises equivalent stress of the remaining tooth tissue in group A was the highest, and the other 4 groups, repairing by different restoration methods, were close to each other. The concentration area of the equivalent stress was the neck of labial root, and the concentration area of the maximum principal stress was the middle 1/3 of lingual root.
-
(2)
When the height of dentin ferrule was fixed, the value of the Von Mises equivalent stress and the maximum principal stress of the dental prosthesis, repairing by different restoration methods: B>E>D>C>A. The concentration area of the equivalent stress was the middle 1/3 of labial root of fiber/cast post and the retainer of endocrown. The concentration area of the maximum principal stress was the middle 1/3 of lingual root.
-
(3)
When the height of dentin ferrule was fixed, the value of the Von Mises equivalent stress and the maximum principal stress on the adhesive layer, repairing by different restoration methods: group A was the highest, and group B was the lowest, the value of both the Von Mises equivalent stress and the maximum principal stress was close among group C, D, and E.
-
(4)
When repaired by the same method, although the dentin ferrule height was different, both the value and the concentration area of the Von Mises equivalent stress of the remaining tooth tissue and the dental prosthesis were close, respectively. And the value and concentration area of the adhesive layer in group A and group B were almost the same. Only the value of adhesive layer was of significant difference among group C, D and E. The equivalent stress values of the 1 mm dentin ferrule model were higher than that of the 2 mm dentin ferrule model, 3.89%,2.65%, and 3.61%, respectively.
4. Discussion
The maxillary central incisor is at the front of the dental arch and is most vulnerable to trauma.[13] Vilela et al[14] used the finite element method to simulate the right central incisor which subjected to external forces perpendicular to the labial and analyzed the stress distribution in the central incisor and adjacent lateral incisors, canines and alveolar bones. During impact on the central incisor, the adjacent teeth showed root displacement. Considerable stress concentrations were observed on the palatal surfaces and proximal and labial surfaces of teeth adjacent to the traumatized incisor.
At present, there are few researches on which method is most beneficial to the stress distribution of the oblique fracture of the maxillary central incisor. The clinicians need to consider how different repair methods and materials affect the residual dentin stress. The 3-dimensional finite element analysis has obvious advantages in the selection of different repair methods and materials for tooth defects.[15]
4.1. The difference and significance of the Von Mises equivalent stress and the maximum principal stress peak in each layer of the model
In the both 2 height ferrule models, the peak value of equivalent stress and the maximum principal stress of the cast post-core-crown were the largest, which was because the elastic modulus was the largest and the stress was concentrated in the post due to the absorption of external force; while the fiber post, because its elastic modulus was the closest to the dentin, formed a whole stress structure composed of root-adhesive layer-post, and the stress could pass through the adhesive layer along the fiber post when subjected to external force. This was consistent with the research of scholar F.R. Verri et al.[16] Therefore, the equivalent stress value of the adhesive layer of group A was higher than that of the other 4 groups, and the possibility of adhesive fragmentation was the largest. Failure of fiber post occured at the interface between post and adhesive layer,[17] and the possibility of fiber post falling off was the greatest under the long-term masticatory force. So for the large-area defect central incisors with oblique fracture, the cast post-core-crown was better than the fiber 1.
The equivalent stress and the maximum principal stress of endocrown in group C, D and E were between group A and B, and the stress peak slightly increased with the increase of depth. This was consistent with the research of scholar M. Einhorn et al.[18]
In this study, there was no difference in the stress peak and concentration area of both group A and B between 1 mm high ferrule and 2 mm ferrule, which was contrary to many clinical trials.[19] Studies have shown that the maintenance of 1.5 to 2 mm improve the stress distributions in the root dentin and along the post-dentin interface.[19–21] Computational and in-vitro analysis showed that a circumferential or uniform ferrule creates a better stress distribution to the root dentin and post interface.[22] However, the ferrule of the model in this experiment was incomplete and oblique. It was demonstrated that incomplete ferrule involving higher than 75% of tooth circumference could increase only in 5% the successful rate of restoration.[23]
However, in group C, D and E, there were different stress peaks due to the height of the dentin ferrule, which may be related to the fact that the endocrown adopted the butt-joint edge without the dentin ferrule and shoulder preparation, while conventional post-core-crown with dentin ferrule caused the loss of sound enamel and dentin tissues that would be important for proper bonding of the restoration,[24] thus more tooth tissue of the neck was preserved and was more conducive to the uniform distribution of stress in the neck.[25] This result is consistent with scholar Ramírez-Sebastià, A, who found that the presence of a post, post length and crown material had no effect on the restoration's fracture resistance.[7]
4.2. The difference and significance of the concentration area of the Von Mises equivalent stress and the maximum principal stress in each layer of the model
Repaired by 5 different restoration methods, the equivalent stress concentration area of the remaining tooth tissue was the labial neck, and the maximum principal stress concentration area was 1/3 of the lingual side; The equivalent stress concentration area of the prosthodontics was mainly 1/3 of the labial side of the fiber/cast post and endocrown retainer, and the maximum principal stress concentration area was mainly 1/3 of the lingual side of the dental prosthesis; The equivalent stress of the adhesive layer in group A was concentrated in middle 1/3 of the root, while that in group B was concentrated in 1/3 of the root and the post tip. If the adhesive layer was broken here and would causes: 1). Post-core loosens, forming lever force in the root canal, resulting in root longitudinal crack; 2). Direct contact with the inner wall of root canal, the resultant force directly acts on the root through the post, resulting in root fracturing. Many previous studies[26] have found that the main reason for the failure of cast post-core-crown was the occurrence of apical 1/3 or middle 1/3 root fracturing and longitudinal fracturing. In group C, D, and E, the stress on adhesive layer was concentrated on the tip of the endocrown retainer. If the tooth was broken, the fracture position was on the neck of the tooth, and the affected tooth could be repaired again by crown lengthening surgery or orthodontic traction.[27] The results of concentration area may be explained as follows:[24] The traditional restoration usually uses materials with different elastic modulus, that is, the post part uses metal or glass-reinforced fibers, and the core / crown part uses composite resin material or ceramic. Considering that the stiffness mismatch among dentin, adhesive layer and restoration may affect the stress distribution, the more the number of interfaces between different materials, the lower the stress distribution. The monolithic nature of the endocrown supports more stress loads than the multi-interface of the traditional restoration.
Therefore, the endocrown was better than the cast post-core-crown for the large-defect of central incisors with oblique fracture.
The results showed that different retainer depths of the endocrown had no significant influence on the stress value and distribution. Therefore, sticking to the principle of minimally invasive treatment,[28] the remaining tooth tissue should be retained as much as possible, so endocrown with a depth of 3 mm retainer was the optimal choice.
Although the finite element method has been widely used in the department of prosthodontics and has significant advantages in mechanical analysis, the finite element method can not truly simulate the complex situation in the mouth. The conditions set by the finite element analysis method are too ideal, and this study only analyzes an ideal stress situation, in addition, this study only analyzes the static load, but in the actual mastication process, the maxillary central incisor is mostly subjected to dynamic impact load, which will affect the accuracy of the study. With the progress of finite element technology, we can use it to study biomechanics more deeply. The results of this study also need to be confirmed by further clinical trials and mechanical tests in vitro.
5. Conclusion
Complete and high enough dentin ferrule is a requirement for repairing heavily defected maxillary central incisor with fiber or cast post-core crown. When the dentin ferrule is incomplete, the stress distribution of the endocrown is more excellent than post-core-crown. And the endocrown with a depth of 3 mm retainer may be the best repair method. As for post-core crown restoration, the cast post-core crown is more favorable for the uniform distribution of residual tooth tissue than the fiber post-core crown.
Author contributions
Conceptualization: Xixi Li.
Formal analysis: Ting Kang, Danting Zhan, Jing Xie.
Funding acquisition: Ling Guo.
Investigation: Ting Kang, Danting Zhan, Jing Xie.
Project administration: Xixi Li.
Supervision: Xixi Li.
Writing – original draft: Xixi Li.
Writing – review & editing: Ling Guo.
Footnotes
Abbreviations: CBCT = Cone beam CT, CEJ = cemento–enamel junction.
How to cite this article: Li X, Kang T, Zhan D, Xie J, Guo L. Biomechanical behavior of endocrowns vs fiber post-core-crown vs cast post-core-crown for the restoration of maxillary central incisors with 1 mm and 2 mm ferrule height: A 3D static linear finite element analysis. Medicine. 2020;99:43(e22648).
This study is supported by CSA-W2019, the Western Clinical Research Foundation for the Promotion of Oral Health and the Development of Stomatology of the Chinese Stomatological Association; Award ID: CSA-W2019-07; Recipient: Ling Guo. This study was approved by the human subjects ethics board of the Stomatological Hospital Affiliated to Southwest Medical University.
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files.
References
- [1].Staderini E, Patini R, Guglielmi F, et al. How to manage impacted third molars: germectomy or delayed removal? a systematic literature review. Medicina (Kaunas) 2019;55:00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Schwendicke F, Stolpe M. Cost-effectiveness of different post-retained restorations. J Endod 2017;43:709–14. [DOI] [PubMed] [Google Scholar]
- [3].Junqueira RB, de Carvalho RF, Marinho CC, et al. Influence of glass fibre post length and remaining dentine thickness on the fracture resistance of root filled teeth. Int Endod J 2017;50:569–77. [DOI] [PubMed] [Google Scholar]
- [4].Bindl A, Mormann WH. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years--preliminary results. J Adhes Dent 1999;1:255–65. [PubMed] [Google Scholar]
- [5].Zarone F, Sorrentino R, Apicella D, et al. Evaluation of the biomechanical behavior of maxillary central incisors restored by means of endocrowns compared to a natural tooth: a 3D static linear finite elements analysis. Dent Mater 2006;22:1035–44. [DOI] [PubMed] [Google Scholar]
- [6].Bankoglu Gungor M, Turhan Bal B, Yilmaz H, et al. Fracture strength of CAD/CAM fabricated lithium disilicate and resin nano ceramic restorations used for endodontically treated teeth. Dent Mater J 2017;36:135–41. [DOI] [PubMed] [Google Scholar]
- [7].Ramirez-Sebastia A, Bortolotto T, Cattani-Lorente M, et al. Adhesive restoration of anterior endodontically treated teeth: influence of post length on fracture strength. Clin Oral Investig 2014;18:545–54. [DOI] [PubMed] [Google Scholar]
- [8].Ortega VL, Pegoraro LF, Conti PC, et al. Evaluation of fracture resistance of endodontically treated maxillary premolars, restored with ceromer or heat-pressed ceramic inlays and fixed with dual-resin cements. J Oral Rehabil 2004;31:393–7. [DOI] [PubMed] [Google Scholar]
- [9].Staderini E, Guglielmi F, Cornelis MA, et al. Three-dimensional prediction of roots position through cone-beam computed tomography scans-digital model superimposition: a novel method. Orthod Craniofac Res 2019;22:16–23. [DOI] [PubMed] [Google Scholar]
- [10].Biacchi GR, Basting RT. Comparison of fracture strength of endocrowns and glass fiber post-retained conventional crowns. Oper Dent 2012;37:130–6. [DOI] [PubMed] [Google Scholar]
- [11].Dejak B, Mlotkowski A. 3D-Finite element analysis of molars restored with endocrowns and posts during masticatory simulation. Dent Mater 2013;29:e309–17. [DOI] [PubMed] [Google Scholar]
- [12].Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, et al. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res 2000;79:1519–24. [DOI] [PubMed] [Google Scholar]
- [13].Staderini E, Meuli S, Gallenzi P. Orthodontic treatment of class three malocclusion using clear aligners: a case report. J Oral Biol Craniofac Res 2019;9:360–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Vilela ABF, Soares PBF, Almeida GA, et al. Three-dimensional finite element stress analysis of teeth adjacent to a traumatized incisor. Dent Traumatol 2019;35:128–34. [DOI] [PubMed] [Google Scholar]
- [15].Rodrigues MP, Soares PBF, Valdivia A, et al. Patient-specific finite element analysis of fiber post and ferrule design. J Endod 2017;43:1539–44. [DOI] [PubMed] [Google Scholar]
- [16].Verri FR, Okumura MHT, Lemos CAA, et al. Three-dimensional finite element analysis of glass fiber and cast metal posts with different alloys for reconstruction of teeth without ferrule. J Med Eng Technol 2017;41:644–51. [DOI] [PubMed] [Google Scholar]
- [17].Bergman B, Lundquist P, Sjogren U, et al. Restorative and endodontic results after treatment with cast posts and cores. J Prosthet Dent 1989;61:10–5. [DOI] [PubMed] [Google Scholar]
- [18].Einhorn M, DuVall N, Wajdowicz M, et al. Preparation ferrule design effect on endocrown failure resistance. J Prosthodont 2017;28:e237–42. [DOI] [PubMed] [Google Scholar]
- [19].Santos-Filho PC, Verissimo C, Soares PV, et al. Influence of ferrule, post system, and length on biomechanical behavior of endodontically treated anterior teeth. J Endod 2014;40:119–23. [DOI] [PubMed] [Google Scholar]
- [20].Santos-Filho PC, Verissimo C, Raposo LH, et al. Influence of ferrule, post system, and length on stress distribution of weakened root-filled teeth. J Endod 2014;40:1874–8. [DOI] [PubMed] [Google Scholar]
- [21].Verissimo C, Simamoto Junior PC, Soares CJ, et al. Effect of the crown, post, and remaining coronal dentin on the biomechanical behavior of endodontically treated maxillary central incisors. J Prosthet Dent 2014;111:234–46. [DOI] [PubMed] [Google Scholar]
- [22].Soares CJ, Rodrigues MP, Faria ESAL, et al. How biomechanics can affect the endodontic treated teeth and their restorative procedures? Braz Oral Res 2018;32: suppl 1: e76. [DOI] [PubMed] [Google Scholar]
- [23].Fokkinga WA, Kreulen CM, Bronkhorst EM, et al. Composite resin core-crown reconstructions: an up to 17-year follow-up of a controlled clinical trial. Int J Prosthodont 2008;21:109–15. [PubMed] [Google Scholar]
- [24].Sedrez-Porto JA, Rosa WLdOd, da Silva AF, et al. Endocrown restorations: a systematic review and meta-analysis. J Dent 2016;52:8–14. [DOI] [PubMed] [Google Scholar]
- [25].Guo J, Wang XY, Li XS, et al. Influence of different designs of marginal preparation on stress distribution in the mandibular premolar restored with endocrown. Nan Fang Yi Ke Da Xue Xue Bao 2016;36:200–4. [PubMed] [Google Scholar]
- [26].Upadhyaya V, Bhargava A, Parkash H, et al. A finite element study of teeth restored with post and core: effect of design, material, and ferrule. Dent Res J (Isfahan) 2016;13:233–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Zhen M, Wei YP, Hu WJ, et al. Finite element analysis of the maxillary central incisor with traditional and modified crown lengthening surgery and post-core restoration in management of crown-root fracture. Zhonghua Kou Qiang Yi Xue Za Zhi 2016;51:362–7. [DOI] [PubMed] [Google Scholar]
- [28].Hayes A, Duvall N, Wajdowicz M, et al. Effect of endocrown pulp chamber extension depth on molar fracture resistance. Oper Dent 2017;42:327–34. [DOI] [PubMed] [Google Scholar]


