In the past few weeks, there has been a great deal of trepidation among the public about the impact of children returning to school on the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Children have greater difficulty adhering to physical distancing rules but are believed to transmit the virus less efficiently than adults.1 Rhinoviruses normally circulate year-round with seasonal peaks in spring and autumn and are transmitted in largely the same manner as SARS-CoV-2. Children are the main drivers of transmission of rhinovirus, with subsequent transmission to adults associated with exacerbations of airways disease and hospitalisations.2
In Southampton, UK, we tested adult medical patients admitted to hospital using point-of-care multiplexed PCR testing (using the QIAstat-Dx Respiratory SARS-CoV-2 Panel and the Biofire Respiratory Panel 2.1 plus) for a wide range of respiratory viruses, including SARS-CoV-2, from the height of the pandemic.3 We compared the rate of respiratory virus detection in 2020 with the same period in 2019 (when multiplex PCR testing for the same respiratory viruses was performed in the laboratory).
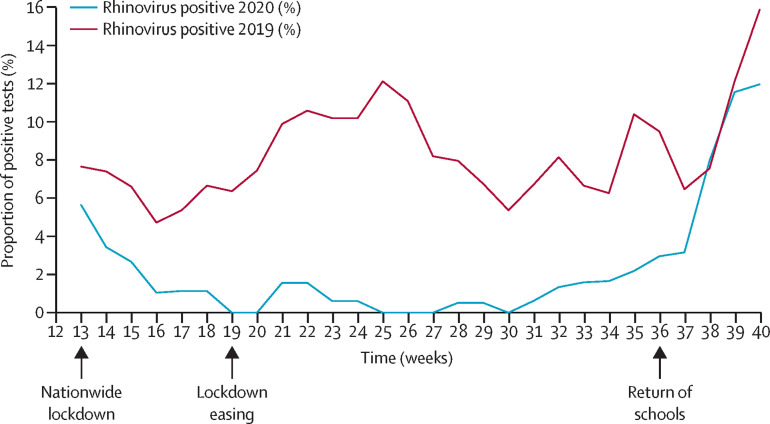
3898 adult patients were tested between March 23 and Sept 20, 2020, and 1898 adults during the same period in 2019. There was a drop in the rate of detection of all respiratory viruses including rhinovirus following the nationwide lockdown on March 23, 2020. Detection of rhinovirus remained low after the easing of national lockdown on the May 10, 2020, compared with the previous year. Around 2 weeks after the concurrent re-opening of state primary and secondary schools in early September, there was a sharp increase in the number of detections similar to that seen in 2019 (figure ).
Figure.
Proportion of tests positive for human rhinovirus
Data points are 2-week rolling average.
Schools are required by government to perform their own risk assessment and adapt a series of infection control measures to their own circumstances to minimise the risk of SARS-CoV-2 transmission. These include enhancing hand hygiene and minimising contact between individuals. The wearing of face coverings is not mandated for any school age children by the UK Government, but individual schools and colleges have discretion to require face coverings in communal indoor areas for secondary school children where distancing cannot be safely maintained.4
Our data support previous reports that children are a major reservoir for rhinovirus infection, and a key driver of transmission to adults. Furthermore, our data suggests that current physical distancing measures adopted by schools do not effectively prevent rhinovirus transmission. These findings might have important implications for circulation of both influenza and SARS-CoV-2 in the coming winter months. If current distancing measures in schools do not prevent rhinovirus transmission, it seems likely that the same will hold true for influenza, for which young children are also known to be key transmitters.5 The implications for SARS-CoV-2 are less clear, as young children appear to be less susceptible to infection than older children or adults, but once infected they have similar levels of detectable virus in the nasopharynx.6
Acknowledgments
TWC reports non-financial support from QIAGEN, during the conduct of the study, personal fees and non-financial support from BioMerieux and BioFire LLC, and personal fees from Synairgen, Roche, Cidara Therapeutics, Janssen, and Randox Laboratories, outside of the submitted work. SP, NJB, and ART declare no competing interests.
References
- 1.Lee B, Raszka WV. COVID-19 transmission and children: the child is not to blame. Pediatrics. 2020;146 doi: 10.1542/peds.2020-004879. [DOI] [PubMed] [Google Scholar]
- 2.Peltola V, Waris M, Österback R, Susi P, Ruuskanen O, Hyypiä T. Rhinovirus transmission within families with children: incidence of symptomatic and asymptomatic infections. J Infect Dis. 2008;197:382–389. doi: 10.1086/525542. [DOI] [PubMed] [Google Scholar]
- 3.Brendish NJ, Poole S, Naidu V V. Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): a prospective, interventional, non-randomised, controlled study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30454-9. published online Oct 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UK Government Coronavirus (COVID-19): education and childcare. Guidance for teachers, school leaders, carers, parents and students. https://www.gov.uk/coronavirus/education-and-childcare
- 5.Cauchemez S, Valleron AJ, Boëlle PY, Flahault A, Ferguson NM. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature. 2008;452:750–754. doi: 10.1038/nature06732. [DOI] [PubMed] [Google Scholar]
- 6.L'Huillier AG, Torriani G, Pigny F, Kaiser L, Eckerle I. Culture-competent SARS-CoV-2 in nasopharynx of symptomatic neonates, children, and adolescents. Emerg Infect Dis. 2020;26:2494–2497. doi: 10.3201/eid2610.202403. [DOI] [PMC free article] [PubMed] [Google Scholar]