Abstract
COVID-19 pandemic is the more challenging public health emergency of the century, producing the collapse of health systems and unprecedented levels of morbidity and mortality around the world, especially in low resource settings. Patients with chronic diseases are the most affected, not only due to the high susceptibility to SARS-CoV-2 infection but also due to the decrease in opportunities for timely care. In this dark landscape, telemedicine, before limited to very specific scenarios, has become one of our main tools to manage cancer patients, particularly in Latin America where COVID-19 has had a strong impact on the public health. Telemedicine can provide rapid access to specialized cancer care in a scenario complicated, reducing the exposure of patients and healthcare personnel to the SARS-CoV-2. In this review, we would like to share our experience and our workflow using telemedicine at Oncosalud-AUNA, a private clinic in Peru.
Keywords: COVID-19, Cancer, Telehealth, Telemedicine, SARS-CoV-2, Patient management
1. Introduction
The new coronavirus disease (COVID-19) was first reported in Wuhan (China) on December 31, 2019. Since then daily cases have increased rapidly worldwide, so as to be labeled as pandemic by the World Health Organization (WHO) (World Health Organization, 2020a). Currently, the COVID-19 has infected more than 24 million people and has caused 827,246 deaths (August 28th, 2020). South America has become the new center of the pandemic, where Peru is one of the countries with the highest number of cases and deaths in the world, despite having imposed one of the earliest and strictest lockdowns to stop the spread of the coronavirus (World Health Organization, 2020b).
As a response measure in the health area in Peru, many hospitals have chosen to cancel outpatient appointments, but have sought ways to maintain ongoing care such as through telemedicine (remote medical service). Telemedicine has demonstrated since its application in different areas that it increases the quality of life, and decreases costs and patient visits without compromising communication between the physician and patient; but above all, in this current situation, it contributes to the decrease in transmission of COVID-19 (Russo et al., 2016).
AUNA, a network of private hospitals and medical centers located in various regions of Peru, has taken special care in the use of telemedicine in cancer patients during this pandemic because they are part of the population with more risk of getting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and having a worse prognosis since their own disease and anti-cancer therapy causes an immunosuppressive state (Blimark et al., 2015; Hijano et al., 2018).
Based on our experience at AUNA, our aim in this review is to show the importance of telemedicine in cancer patients during the COVID-19 pandemic.
2. Current situation of COVID-19 in Peru
The first case of COVID-19 in Peru was reported on March 6th, 2020; and on March 11th, the country entered an emergency state. One day later, the quarantine was established and it was prolonged until June 30th, 2020. The basic reproductive number (R0) estimated in Peru was 2.973 in the first 20 days of the pandemic (Torres-Roman et al., 2020).
Despite the early and strict measures given by the government (Peru was the first country in Latin America in declaring a general lockdown), socio-economic reality led to high contagion rates. Currently, Peru is one of the countries with more positive cases for COVID-19 with 639,435 patients and 28,607 deaths reported by the Ministry of Health of Peru (by August 29th, 2020) (Instituto Nacional de Salud y Centro Nacional de Epidemiología, 2020). Nowadays, there is a saturation of the health system complicated by high rates of contagion and mortality in the health personnel, where the Peruvian Medical College reports 3602 physicians infected with COVID-19 and 153 physician deaths due to this disease (Colegio Médico del Perú, 2020).
The complex situation of the Peruvian health system conducted to delaying of the diagnosis and treatment of hundreds of thousands of patients with several pathologies, including cancer, due to the healthcare being limited to medical emergencies in the first months of the pandemic. On the other hand, fear of patients becoming infected led to avoiding their visit to hospitals by another reason than COVID-19, causing excess of deaths in more than 65,000 Peruvians between March and August (Instituto Nacional de Salud y Centro Nacional de Epidemiología, 2020).
In the oncology area, services have been gradually and partially opened to prevent patients from getting SARS-CoV-2 but without affecting their care. To fulfill this objective, we are following international guidelines: We maximize remote outpatient follow-up and treatment, hypofractionate treatments whenever possible, delay possible treatments and procedures in relation to risk/benefit, switch to subcutaneous or oral therapies rather than intravenous ones when possible, and evaluate patients to detect SARS-CoV-2 infection even if suspicion is minimal. Furthermore, in the area of research, new clinical trials have been postponed, while some ongoing clinical trials have had to be discontinued or we have had to become more flexible in the protocols (Al-Shamsi et al., 2020; Moujaess et al., 2020; Arrieta et al., 2020; World Health Organization, 2020c; Auna, 2020).
3. Cancer patients are at higher risk of SARS-CoV-2 infection
Cancer patients are more susceptible to respiratory pathogens and severe pneumonia than the general population, as they are immunosuppressed due to their disease itself and anti-cancer therapy. Furthermore, they may also have an increased immune response to infection secondary due to immunomodulatory drugs (Blimark et al., 2015; Hijano et al., 2018).
Several studies suggest that cancer patients may have an increased risk of getting SARS-CoV-2 and develop severe complications, thus also having a higher mortality rate compared to the general population (Zhang et al., 2020; Epidemiology Working Group for NCIP Epidemic Response, 2020; Joint Mission, 2020; Lee et al., 2020; Kuderer et al., 2020). In addition, these patients have an increased risk of interactions of the drugs used to treat COVID-19 (drugs that do not have sufficient scientific support and that must be used with caution) with anticancer treatments, which makes their management more difficult. For example, combination checkpoint therapy (anti-PD-1/PD-L1 or anti- CTLA4) is associated with higher rate for immune-related toxicities (e.g. pneumonitis) which can potentially adversely impact outcome of COVID-19 infection (Jafari et al., 2020; Bersanelli, 2020).
In a retrospective study that included 28 cancer patients with COVID-19 attended in three Wuhan hospitals as of February 26, 2020, it was shown that 53.6 % of patients developed severe events, 21.4 % entered the intensive care unit, and 28.6 % of the patients died. The risk factors involved in developing severe events were receiving anti-cancer therapy within 14 days prior to the diagnosis of COVID-19 (HR = 4.079, 95 % CI 1.086–15.322, p = 0.037) and having patchy lung consolidation on computed tomography on admission (HR = 5.438, 95 % CI 1.498–19.748, P = 0.010). Likewise, depending on the type of cancer, it was observed that lung cancer developed a more severe and faster COVID-19 disease (Zhang et al., 2020).
The Chinese Center for Disease Control and Prevention described the epidemiological characteristics of 72,314 cases of COVID-19 in China up to of February 11, 2020. Of the 44,672 confirmed cases, 107 (0.5 %) were cancer patients. They reported a total of 1023 deaths within confirmed cases, of which 6 (1.5 %) of them had cancer; therefore, the crude mortality rate of these patients (5.6 %) was higher than the general population (2.3 %) (Epidemiology Working Group for NCIP Epidemic Response, 2020). Similarly, a WHO-China Joint Mission report on COVID-19 published on February 28, 2020, identified that there is higher mortality among cancer patients (7.6 %) compared to patients without comorbidity (1.4 %) (Joint Mission, 2020).
In contrast, a prospective observational study that included 800 cancer patients and positives for COVID-19 using RT-PCR during the period from March 18 to April 26, 2020, found no evidence that cancer treatment given within 4 weeks before confirmed COVID-19 has been contributed significantly to worsening the disease or increasing the risk of mortality. Mortality by COVID-19 in cancer patients seems to have been caused by their age, gender, and comorbidities (Lee et al., 2020).
Likewise, in a cohort study that included data from 928 patients with active or previous cancer and COVID-19 from the USA, Canada, and Spain from the COVID-19 and Cancer Consortium (CCC19) database for those who were added baseline data between March 17 and April 16, 2020; reported that 121 (13 %) patients died within 30 days after the diagnosis of COVID-19. Factors associated with its mortality were increasing age, male sex, former smoker, active cancer, comorbidities, Eastern Cooperative Oncology Group (ECOG) performance status ≥2, and treatment with hydroxychloroquine plus azithromycin versus treatment with neither. Ethnicity, obesity, cancer type, type of anti-cancer therapy, and any surgery in the 4 weeks before COVID-19 diagnosis were not associated with mortality (Kuderer et al., 2020).
Recent studies have shown that human angiotensin converting enzyme II (ACE2) and the type II transmembrane serine protease (TMPRSS2) are key proteins for the entry of SARS-Cov-2 into cells (Hoffmann et al., 2020). Dai et al. (2020) found through gene expression profiling analysis that liver hepatocellular carcinoma has a high expression of ACE2, which would increase its risk of SARS-CoV-2 infection, but was related to a good prognosis. Likewise, Fu et al. (Jiewen et al., 2020) also found a high expression of ACE2 in liver cancer as well as kidney cancer correlated with increased survival rate, indicating that ACE2 is a prognostic marker in both.
On the other hand, a meta-analysis that included 205 cancer patients (from 6 studies) with COVID-19 found that individuals with lung and colorectal cancer are more susceptible to SARS-CoV-2 infection (Wang and Huang, 2020). These cancers were the most frequent in the study (24.7 % and 20.5 %, respectively) and their expression of the mRNA of ACE2 and TMPRSS2 was higher than other types of cancer. However, more studies are needed to associate ACE2 and TMPRSS2 expression levels with susceptibility, progression, and severity of the disease caused by SARS-CoV-2, as it depends on various factors such as age, sex, ethnicity, medication, and comorbidity (Bourgonje et al., 2020).
Although these results are still preliminary and require validation with larger cohorts, they suggest that cancer patients are a significant at-risk population of getting SARS-CoV-2 and develop severe complications (Table 1 ). In addition, it must be taken into account that the risk of these patients of getting SARS-CoV-2 increases due to the fact that they are mostly older than 60 years, with one or more comorbidities, and they are frequently exposed through their visits to the hospital to receive their therapies, monitoring, or preventive and supportive care.
Table 1.
Impact of COVID-19 in cancer patients.
| Authors | Country | Period of study | Study design | Total of cancer patients with COVID-19 | Conclusions |
|---|---|---|---|---|---|
| Zhang et al. | China | February 26, 2020 | Retrospective | 28 | Cancer patients developed severe events and have poor outcomes from the SARS-CoV-2 infection. |
| Zhonghua et al. | China | February 11, 2020 | Retrospective | 107 | The mortality rate from COVID-19 is higher in cancer patients than in the general population. |
| WHO-China Joint Mission | China | February 28, 2020 | Retrospective | Not reported | The mortality rate from COVID-19 of cancer patients is higher than patients without comorbidities. |
| Lee et al. | United Kingdom | March 18 to April 26, 2020 | Prospective observational | 800 | Mortality by COVID-19 in cancer patients seems to have been caused by their age, gender, and comorbidities. |
| Kuderer et al. | USA, Canada and Spain | March 17 and April 16, 2020 | Retrospective | 928 | Factors associated with mortality in cancer patients with COVID-19 were increasing age, male sex, former smoker, active cancer, comorbidities, ECOG ≥ 2, and treatment with hydroxychloroquine plus azithromycin. |
Abbreviations: ECOG, Eastern Cooperative Oncology Group.
4. Role of telemedicine during the COVID-19 pandemic
Before the COVID-19 pandemic, telemedicine had already proven to be an option in the care of patients with high satisfaction rates for both patients and health personnel (Kruse et al., 2017; Powell et al., 2017). Generally, telemedicine was used to improve access to remote or less accessible areas for medical care, while in oncology it enabled the provision of remote clinical oncology services using interactive telecommunication tools (Sirintrapun and Lopez, 2018).
In the context of the pandemic, telemedicine has become a viable and safe alternative that increases access to patient care, avoids delays in treatment, decreases the risk of exposure to SARS-CoV-2 infection of patients as well as healthcare providers, and at the same time reduces the demand for personal protective equipment (PPE) which is limited during present times (Shirke et al., 2020; Elkaddoum et al., 2020). In oncology, it allows monitoring of chemotherapy adverse events, palliative management, evaluation of disease symptoms, and emotional support. Some healthcare providers have implemented telehealth as part of ongoing healthcare for cancer patients. Some applications of telemedicine in oncology are teleconsultation, telepathology, tele-education, tele-tumor board (multidisciplinary case discussions). Even an important part in the beginning of treatment, such as discussion of the treatment plan with patients, has been carried out virtually and to the satisfaction of the patient and the treating physicians (Al-Shamsi et al., 2020).
On the other hand, telehealth accelerates the training of oncologists. In a study carried out in two Peruvian hospitals, radiation oncologists, medical physicists, and radiation therapists were trained in stereotactic body radiation therapy and stereotactic radiosurgery by 15 specialists from nine American institutions. The participants had an improvement in their knowledge and a significant increase in their skills (Li et al., 2020).
Once the patients begins the active management of their disease, follow-up visits to the treatment started, management of their comorbidities, palliative consultations, resolution of questions, evaluation by subspecialties and second opinions, requesting laboratory tests or images can be made through telehealth. In-person care is reserved for cases that require a physical examination in person, or as part of the planning of continuous patient care. It is important to highlight that telemedicine also presents challenges such as limited access to telemedicine platforms, insufficient internet access, limited resolution of images, lack of training in technological tools, difficulties for physical examination of the patient, theoretical education with little hospital training, and reimbursement agreements with the payer or managers of insurance funds (Sirintrapun and Lopez, 2018; Shirke et al., 2020; Wahezi et al., 2020; Rallis and Tejerina, 2020).
5. Teleconsultation workflow in AUNA during the COVID-19 pandemic
The medical services that we were able to carry out through telehealth involve clinical visits, palliative care, nurse visits, pharmacy, and multidisciplinary services (Table 2 ). We describe below the workflow for teleconsultation.
Table 2.
Services provided in Oncosalud-AUNA through a telemedicine platform.
| Service category | Details |
|---|---|
| Clinical Visits | Follow up visits |
| Clinical trial visits | |
| Survivorship follow-up visits | |
| Prevention and diagnosis visits | |
| Psychological support | |
| Nutritional support | |
| Palliative care | Palliative consultations |
| Nurse visits | Patient education |
| Pharmacy | Drugs delivery |
| Multidisciplinary approach | Tumor Board |
In general terms, the teleconsultation workflow at AUNA is as follows:
5.1. Preparing for a teleconsultation
Contact patients days before their appointment to confirm it. Patients should receive instructions before the teleconsultation on how to use the virtual platform, how to handle the problems, the scope of the teleconsultation, and the standard questionnaires on the important points to ask or resolve with the doctor during the consultation. In addition, patients must consent to virtual medical care and must be informed of their rights and duties during the teleconsultation.
5.2. Day of consult
The environment from which the patient receives the teleconsultation must be away from annoying noises, with adequate lighting. Ideally, patients should be sitting in a comfortable chair. The equipment that the patient needs to access the teleconsultation can be a computer, laptop, tablet, or phone with high camera resolution and a stable Wi-Fi signal. If possible, there should be a second person at the teleconsultation. Patients should be encouraged to have a family or friend present during the visit so they can help with certain tasks if necessary.
5.3. The following consult
After the teleconsultation, a coordinated system for scheduling the appointment for the application of intravenous treatments is carried out; the patient receives the date and time of the application of his treatment through an email. The oral medication is then brought through a delivery system to his home. Laboratory tests are taken at home especially for patients with vulnerability criteria such as age over 70 years, difficulties with walking or patients on immunosuppressive treatment. It is very important to transmit any follow-up orders for testing, meds, and others; and send results of the consultation.
Some general considerations that must be taken into account are the duration of the teleconsultation, which must be equivalent to a traditional visit; the information transmitted by the oncologist must be delivered in a clear, honest and empathetic way; patients must have time to resolve their doubts and ask questions, and the oncologist must validate that the patient understood the information adequately.
Available technologies should be considered to measure the patient's vital functions, such as measuring pulse, blood pressure, temperature, and oxygen saturation; however, the unavailability of these resources should not be a definitive barrier that does not allow the possibility of teleconsultation.
A large number of patients in oncology can be followed or monitored by teleconsultation, but we suggest that patients who require a physical examination, especially if they have been recently diagnosed or a change in therapy due to disease progression is planned should have a traditional medical visit.
6. Patients satisfaction with telemedicine in Oncosalud-AUNA
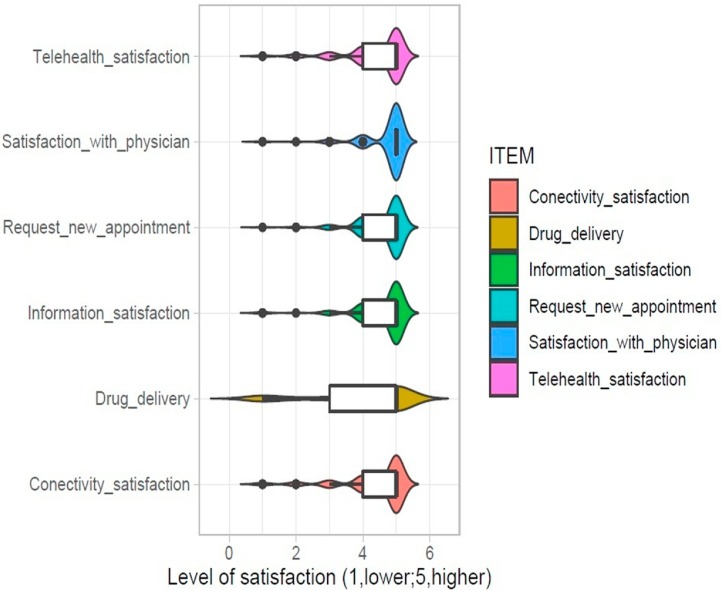
As part of our quality policies, we conducted a survey to know the satisfaction with telemedicine in patients who attended to Oncosalud-AUNA. Variables evaluated included satisfaction with the telehealth, satisfaction with the physician, the process of request new appointments, satisfaction with the information provided, satisfaction with the drug delivery, and satisfaction with the connectivity. We analyzed 273 patients surveyed between April and May 2020.
In general, there was a high level of satisfaction in all evaluated variables, where higher satisfaction was obtained from the interaction with the physicians. These surveys also show to us that the drug delivery (conducted by an external provider) is an important process to improve to achieve a better experience with the service provided (Fig. 1 ).
Fig. 1.
Results of a survey of patient’s satisfaction with telemedicine in 273 participants attended at Oncosalud-AUNA. The level of satisfaction was measured with a Likert-type questionnaire.
7. Conclusions
Despite the fact that the benefits of telemedicine have already been demonstrated for many years, this pandemic has forced us to adapt to it at an impressive speed, becoming it the "front line" of the battle against COVID -19. Telemedicine reduces the burden on hospitals, which are mainly dealing with COVID-19 cases; furthermore, it protects patients, health staff, and reduces the impact of lack of medical resources.
It has been a great challenge for the health area, since they have had to rapidly develop virtual care skills, such as performing physical exams without contact, and without losing empathy towards the patient or compromising the quality of their care. Our initial results in cancer patients as well as other studies demonstrate its effectiveness, satisfaction, and value in promoting social distancing. The current circumstances have accelerated the use of telemedicine reflecting that this method is the present, especially during periods of outbreaks of infectious diseases.
Unfortunately, our experience does not reflect the current situation of the public health system in Peru who attends patients with scarce or null internet connectivity, or with very limited access to electronic devices with the appropriate software. These patients are now unprotected and dealing with a collapsed health system and a falling economy. The Peruvian government should consider telemedicine a priority and make more efforts to expand its access to all patients.
Funding
This work was financially supported by AUNA.
CRediT authorship contribution statement
Paola Montenegro: Conceptualization, Writing - original draft, Supervision. Luis Pinillos: Data curation, Writing - review & editing. Frank Young: Data curation, Writing - review & editing. Alfredo Aguilar: Data curation, Writing - review & editing. Indira Tirado-Hurtado: Conceptualization, Writing - original draft. Joseph A. Pinto: Conceptualization, Writing - original draft. Carlos Vallejos: Data curation, Writing - review & editing.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgments
Authors would like to thanks to Dr. Denisse Bretel for her invaluable input and critical review of this manuscript.
Biographies
Paola Montenegro, MD: Oncologist specializing in gastrointestinal cancer, molecular biology, and genetic counseling. She is the current Deputy Medical Director of Oncosalud-AUNA.
Luis Pinillos, MD: Oncologist specializing in radiology. He was the General Director of the Instituto Nacional de Enfermedades Neoplásicas in 1985 and Minister of Health in 1988.
Frank Young, MD: Oncologist with a specialty in abdominal surgery, with a master's degree in administration and public management. He is the current Medical Director of Oncosalud-AUNA.
Alfredo Aguilar, MD: Oncologist with a Master's in Public Health. He is currently the Scientific and Academic Director of AUNA.
Indira Tirado-Hurtado, BSc: Biologist with a specialty in human genetics. She is currently a researcher at the Basic and Translational Research Unit – AUNA.
Joseph A. Pinto, MSc: Biologist specializing in genetics and molecular biology of cancer. Currently, he is the coordinator of the Basic and Translational Research Unit – AUNA.
Carlos Vallejos, MD: He is the founder of Oncosalud-AUNA and the Peruvian Society of Medical Oncology. He was the General Director of the Instituto Nacional de Enfermedades Neoplásicas and the institutional head of this institute. In addition, he was Minister of Health in 2006.
References
- Al-Shamsi H.O., Alhazzani W., Alhuraiji A., Coomes E.A., Chemaly R.F., Almuhanna M. A Practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) Pandemic: an international collaborative group. Oncologist. 2020;(25):e936–945. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrieta O., Cardona A.F., Lara-Mejía L., Heredia D., Barrón F., Zatarain-Barrón Z.L. Recommendations for detection, prioritization, and treatment of thoracic oncology patients during the COVID‐19 pandemic: the THOCOoP cooperative group. Crit. Rev. Oncol. Hematol. 2020;153 doi: 10.1016/j.critrevonc.2020.103033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auna . 2020. Guías de Práctica Clínica- auna.https://sites.google.com/auna.pe/gydp/documentos-auna/gu%C3%ADas-de-pr%C3%A1ctica-cl%C3%ADnica?authuser=0 [Google Scholar]
- Bersanelli M. Controversies about COVID-19 and anticancer treatment with immune checkpoint inhibitors. Immunotherapy n.d.;0. 10.2217/imt-2020-0067. [DOI] [PMC free article] [PubMed]
- Blimark C., Holmberg E., Mellqvist U.-H., Landgren O., Björkholm M., Hultcrantz M. Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients. Haematologica. 2015;100:107–113. doi: 10.3324/haematol.2014.107714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgonje A.R., Abdulle A.E., Timens W., Hillebrands J.-L., Navis G.J., Gordijn S.J. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19) J. Pathol. 2020 doi: 10.1002/path.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colegio Médico del Perú . 2020. Médicos con Covid-19 Positivo (Autoreporte). Col Méd Perú - Cons Nac.https://www.cmp.org.pe/medicos-con-covid-19-positivo-autoreporte/ (accessed July 31, 2020) [Google Scholar]
- Dai Y.-J., Hu F., Li H., Huang H.-Y., Wang D.-W., Liang Y. A profiling analysis on the receptor ACE2 expression reveals the potential risk of different type of cancers vulnerable to SARS-CoV-2 infection. Ann. Transl. Med. 2020;8 doi: 10.21037/atm.2020.03.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkaddoum R., Haddad F.G., Eid R., Kourie H.R. Telemedicine for cancer patients during COVID-19 pandemic: between threats and opportunities. Future Oncol n.d. 10.2217/fon-2020-0324. [DOI] [PMC free article] [PubMed]
- Epidemiology Working Group for NCIP Epidemic Response . Vol. 41. 2020. pp. 145–151. (Chinese Center for Disease Control and Prevention. [The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) in China]). Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi. [DOI] [Google Scholar]
- Hijano D.R., Maron G., Hayden R.T. Respiratory viral infections in patients with Cancer or undergoing hematopoietic cell transplant. Front. Microbiol. 2018;9 doi: 10.3389/fmicb.2018.03097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Salud y Centro Nacional de Epidemiología . 2020. Prevención y Control de Enfermedades-MINSA. Covid 19 en el Perú - Ministerio de Salud. Sala Situacional.https://covid19.minsa.gob.pe/sala_situacional.asp [Google Scholar]
- Jafari A., Dadkhahfar S., Perseh S. Considerations for interactions of drugs used for the treatment of COVID-19 with anti-cancer treatments. Crit. Rev. Oncol. Hematol. 2020;151 doi: 10.1016/j.critrevonc.2020.102982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiewen F., Baixu Z., Lianmei Z., Kyathegowdanadoddi S.B., C W, Xiaoyan L. Expressions and significances of the angiotensin-converting enzyme 2 gene, the receptor of SARS-CoV-2 for COVID-19. Mol. Biol. Rep. 2020;47:4383–4392. doi: 10.1007/s11033-020-05478-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint Mission . 2020. Report of the WHO-China Joint Mission on Coronavirus Disease19 (COVID-19) [Google Scholar]
- Kruse Cs, Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuderer N.M., Choueiri T.K., Shah D.P., Shyr Y., Rubinstein S.M., Rivera D.R. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet Lond Engl. 2020;395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee L.Y.W., Cazier J.B., Starkey T., Turnbull C.D., Kerr R., Middleton G. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395:1919–1926. doi: 10.1016/S0140-6736(20)31173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Sarria G.R., Hermansen M., Hao J., Martinez D., Garcia B. Impact of a SBRT/SRS longitudinal telehealth training pilot course in Latin America. Crit. Rev. Oncol. Hematol. 2020;154 doi: 10.1016/j.critrevonc.2020.103072. [DOI] [PubMed] [Google Scholar]
- Moujaess E., Kourie H.R., Ghosn M. Cancer patients and research during COVID-19 pandemic: a systematic review of current evidence. Crit. Rev. Oncol. Hematol. 2020;150 doi: 10.1016/j.critrevonc.2020.102972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell Re, Henstenburg Jm, Cooper G., Hollander Je, Rising Kl. Patient perceptions of telehealth primary care video visits. Ann. Fam. Med. 2017;15:225–229. doi: 10.1370/afm.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rallis K.S., Tejerina A.M.A. Tele-oncology in the COVID-19 Era: Are Medical Students Left Behind? Trends Cancer. 2020;0 doi: 10.1016/j.trecan.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo J.E., McCool R.R., Davies L. VA telemedicine: an analysis of cost and time savings. Telemed J E-Health Off J Am Telemed Assoc. 2016;22:209–215. doi: 10.1089/tmj.2015.0055. [DOI] [PubMed] [Google Scholar]
- Shirke M.M., Shaikh S.A., Harky A. Implications of telemedicine in oncology during the COVID-19 pandemic. Acta Biomed. 2020;91 doi: 10.23750/abm.v91i3.9849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirintrapun S.J., Lopez A.M. Telemedicine in Cancer care. Am. Soc. Clin. Oncol. Educ. Book Am. Soc. Clin. Oncol. Annu. Meet. 2018;38:540–545. doi: 10.1200/EDBK_200141. [DOI] [PubMed] [Google Scholar]
- Torres-Roman J.S., Kobiak I.C., Valcarcel B., Diaz-Velez C., La Vecchia C. The reproductive number R0 of COVID-19 in Peru: an opportunity for effective changes. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahezi S., Duarte R.A., Yerra S., Thomas M.A., Pujar B., Sehgal N. Telemedicine during COVID-19 and beyond: a practical guide and best practices multidisciplinary approach for the orthopedic and neurologic pain physical examination. Pain Physician. 2020;23:S205–38. [PubMed] [Google Scholar]
- Wang B., Huang Y. Which type of cancer patients are more susceptible to the SARS-COX-2: evidence from a meta-analysis and bioinformatics analysis. Crit. Rev. Oncol. Hematol. 2020;153 doi: 10.1016/j.critrevonc.2020.103032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Pandemic 2020.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (COVID-19) Situation Reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Accessed July 31, 2020) [Google Scholar]
- World Health Organization. Coronavirus disease (2019-COVID-19) technical guidance: Patient management n.d. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/patient-management (accessed September 25, 2020).
- Zhang L., Zhu F., Xie L., Wang C., Wang J., Chen R. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 2020 doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]