Abstract
Importance
Adequate sampling of the nasopharynx is crucial to performing accurate SARS-CoV-2 (COVID) testing. Formalized education of nasal anatomy may improve provider testing technique and reduce false-negative test results.
Objective
To assess the effect of nasal anatomy education on medical providers' comfort level and knowledge base in performing accurate SARS-CoV-2 (COVID) testing.
Study design
Pre-post survey.
Settings
Tertiary care academic hospital.
Participants
17 nurses performing COVID testing were enrolled.
Intervention
An educational session on COVID nasopharyngeal testing technique and nasal anatomy was presented by an otolaryngologist.
Main outcomes and measures
A pre-session survey assessed providers' prior nasal testing training and COVID testing challenges. Provider comfort level with COVID testing was surveyed pre-and post-session. A 6-question nasal anatomy test was administered pre- and post-session.
Results
16 out of 17 nurses performed fewer than 10 COVID tests prior to the educational session (94%). Reported challenges with COVID testing included patient discomfort (79.6%), inability to pass the test swab (23.5%) and nasal bleeding (11.8%). The number of providers comfortable with independently performing COVID testing increased from pre- to post-session (5 and 14, p = 0.013). The average number of correct responses to the 6-question nasal anatomy test increased following the session (3.2 ± 1.2 to 5.1 ± 1.1, p = 0.003). Specifically, the number of providers able to localize the nasopharynx increased from 8 providers pre-session to 14 providers post-session (p = 0.04).
Conclusion
Early implementation of nasal anatomy and nasopharyngeal swab technique education can help improve provider comfort and knowledge in performing accurate COVID testing.
Keywords: COVID, COVID testing, Education, Nasal anatomy
1. Introduction
The emergence of severe acute respiratory syndrome-related coronavirus-2 (SARS-CoV-2) has led to the widespread development of coronavirus disease 2019 (COVID-19) worldwide [1,2]. Clinical manifestations of COVID-19 are often nonspecific, including fever, fatigue, cough, anosmia, and shortness of breath, and a subset of patients are completely asymptomatic throughout their disease course [1]. However, severe cases of COVID-19 can rapidly progress to acute respiratory distress syndrome (ARDS), respiratory failure, and death. Accurate diagnostic testing is crucial to identify both symptomatic patients and asymptomatic carriers to ensure adequate treatment and isolation measures, thus preventing further disease transmission.
Currently, COVID-19 is diagnosed using real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) tests that specifically detect SARS-CoV-2 [2]. Clinical specimens are commonly obtained from areas with the highest viral load, including the lower respiratory tract (e.g. sputum, bronchoalveolar lavage) and upper respiratory tract (nasopharyngeal, nasal cavity, and oropharyngeal samples) [[1], [2], [3], [4], [5], [6], [7], [8], [9]]. While lower respiratory tract specimens carry higher viral loads and yield higher test sensitivity, risk of aerosolization and transmission to healthcare workers during specimen retrieval limits their clinical use [3,4,10]. Currently, the Centers for Disease Control (CDC) recommend upper respiratory tract sampling, with nasopharyngeal specimens as the preferred choice for initial diagnostic testing [1]. The viral load and rate of SARS-CoV-2 detection is highest in samples from the nasopharynx, as compared with those from the oropharynx, nasal cavity or nasal washings [[6], [7], [8], [9]].
Diagnostic accuracy of SARS-CoV-2 testing (COVID testing) relies on accurate sampling technique with adequate specimen retrieval [[11], [12], [13], [14]]. Various sources have provided written and video instruction regarding nasopharyngeal swab technique: insertion of swab through the nares until resistance is felt, rotation of swab for a few seconds to absorb secretions, and slow removal of the swab [1,15]. Given that the nasopharynx is a structure posterior to the nasal cavity, it cannot be easily visualized externally by the testing provider. Challenges to providers who are not well-versed in nasal anatomy include poor understanding of nasopharynx location relative to the nasal cavity, inability to pass the swab through either nare, and subsequent patient and provider discomfort with COVID testing. This study aims to assess the effect of nasal anatomy and nasopharyngeal swab technique teaching by an otolaryngologist on provider comfort level and knowledge base for COVID testing.
2. Methods
After Institutional Board Review exemption was attained, surgical nursing coordinators recruited nursing staff to participate in an educational session reviewing nasal anatomy and technique pertaining to COVID testing. Inclusion criteria for this study included nursing providers who were required to perform COVID testing at this institution, and who were able to attend the educational session in its entirety. Providers who were unable to attend the educational session or who could not complete both the pre- and post-session surveys were excluded from the study.
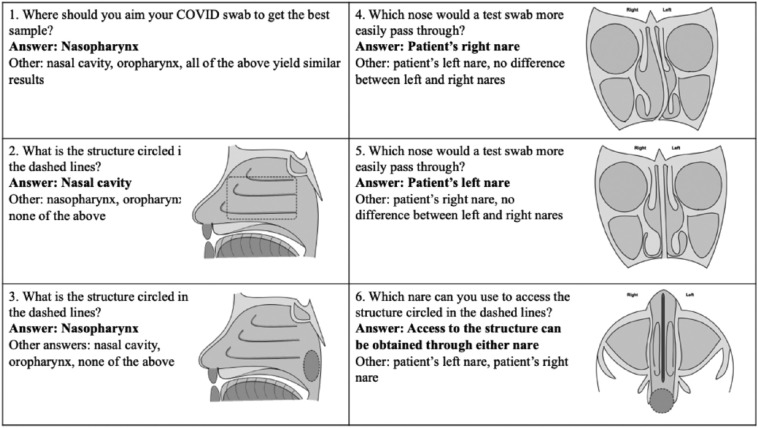
Seventeen providers were enrolled in this study, consisting of surgical pre-operative nurses and labor and delivery nurses who were required to perform COVID testing in their respective units. A pre-session survey was conducted evaluating the total number of COVID tests performed by each provider, prior nasal testing experience, and prior nasal anatomy teaching received. Provider-reported challenges with COVID testing and provider comfort level with performing and teaching COVID testing were assessed. A 6-question nasal anatomy test was then administered to evaluate the provider's knowledge base of COVID testing (Fig. 1 ). Questions included where a COVID test swab should be aimed, location of the nasal cavity and nasopharynx, and which sided nare a swab would more easily pass through when septal deviation or inferior turbinate hypertrophy was present.
Fig. 1.
Provider nasal anatomy test.
The 6-question test administered before and after the educational session to evaluate the provider's knowledge base of nasal anatomy related to COVID testing.
A 20-min educational session was provided by an otolaryngologist reviewing CDC guidelines for COVID testing, showing a video of proper nasopharyngeal swabbing technique, highlighting nasal anatomy as it pertains to COVID testing (Supplemental document), and supervising hands-on practice of COVID testing on a mannequin [1,15]. Emphasis was placed on targeting the nasopharynx, identifying the posterior location of the nasopharynx and how it may be accessed via either nare, and understanding that the presence of septal deviation or inferior turbinate hypertrophy may limit test swab passage. Following the presentation, the providers completed a post-session survey evaluating their comfort level with performing and teaching COVID testing, and repeated the 6-question nasal anatomy test.
Non-parametric paired McNemar tests were used to compare pre- and post-session provider comfort levels in performing and teaching COVID testing. McNemar tests were also used to compare the number of providers accurately answering each of the 6 nasal anatomy test questions pre- and post-session. Non-parametric paired Wilcoxon signed-rank test was used to compare the number of correct answers to the 6-question nasal anatomy test pre- and post-session. P-values of <0.05 were considered statistically significant.
3. Results
16 out of 17 nurses performed fewer than 10 COVID tests prior to the educational session (94%). Three providers (17.7%) reported having prior nasal anatomy training. Nine providers (52.9%) had prior experience performing another type of nasal testing, including MRSA (23.5%), influenza (35.5%), and nasal culture (5.9%). Reported challenges with COVID testing included patient discomfort (79.6%), inability to pass the test swab (23.5%) and nasal bleeding (11.8%) (Table 1 ).
Table 1.
Baseline characteristics of the study participants.
| Baseline characteristics (N = 17) | Number of providers (%) |
|---|---|
| <10 COVID tests performed | 16 (94.1%) |
| Prior nasal anatomy training | 3 (17.7%) |
| Other nasal testing performed | 9 (52.9%) |
| MRSA | 4 (23.5%) |
| Influenza | 6 (35.3%) |
| Nasal culture | 1 (5.9%) |
| COVID testing challenges | |
| Unable to pass swab | 4 (23.5%) |
| Patient discomfort | 12 (79.6%) |
| Nasal bleeding | 2 (11.8%) |
Five providers felt comfortable performing COVID testing independently prior to the educational session (29.4%), while the remainder either felt uncomfortable performing COVID testing (41.2%) or felt comfortable only with supervision (29.4%). Following the educational session, 14 providers felt comfortable performing COVID testing independently (73.7%), while 3 providers felt comfortable only with supervision (17.6%) (Table 2 ). The increase in the number of providers feeling comfortable performing COVID testing independently from pre- to post-session was statistically significant (5 and 14, respectively, p = 0.013). Additionally, all 14 of the providers who were comfortable performing COVID testing independently post-session also felt comfortable teaching proper COVID testing technique to fellow providers.
Table 2.
Provider comfort level performing and testing COVID testing pre- and post-educational session.
| Uncomfortable | Comfortable with supervision | Comfortable independently performing test | Comfortable teaching testing | |
|---|---|---|---|---|
| Pre-session | 7 | 5 | 5 | 5 |
| Post-session | 0 | 3 | 14 | 14 |
| p = 0.013 | p = 0.013 |
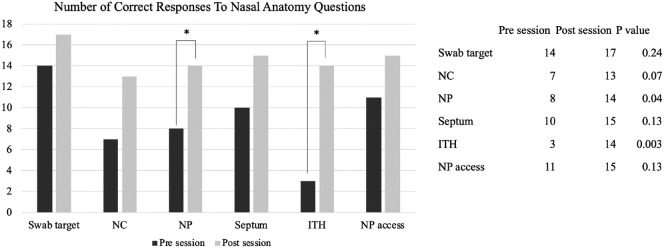
The average number of correct responses to the 6-question knowledge base test increased following the educational session, from 3.2 ± 1.2 to 5.1 ± 1.1, p = 0.003. The number of providers who chose the correct response also increased for each question post-session. Specifically, there was a statistically significant increase in the number of providers from pre- to post-session who were able to identify the location of the nasopharynx (8 and 14, respectively, p = 0.04) and the optimal nare to pass a swab through with asymmetric inferior turbinate hypertrophy (3 and 14, respectively, p = 0.003) (Fig. 2 ).
Fig. 2.
Number of providers who correctly answered nasal anatomy test questions
The number of providers who correctly answered each individual nasal anatomy question increased following the educational session, with statistical significance achieved for identification of the nasopharynx and which nare to swab in the presence of inferior turbinate hypertrophy.
4. Discussion
Diagnostic specimens for COVID testing are retrieved from areas with high viral loads, specifically the upper and lower respiratory tracts. Lower respiratory tract specimens, such as bronchoalveolar lavage and sputum, contain greater viral loads and yield higher test sensitivity than upper respiratory tract specimens [3,4]. However, an expert consensus by the Chinese Interventional Respiratory Medicine Group emphasizes that bronchoscopy should not be used routinely to diagnose COVID-19, due to risk of virus aerosolization and transmission to health care workers [10]. Concurrently, the CDC recommends upper respiratory tract sampling, with nasopharyngeal specimens as the preferred choice for initial diagnostic testing [1]. Similar to other respiratory viruses, SARS-CoV-2 is most readily detected in the nasopharynx due to higher viral load, as compared with the nasal cavity, nasal washings, or oropharynx [1,2,[5], [6], [7], [8], [9],[16], [17], [18]].
Nasopharyngeal COVID testing sensitivity relies on adequate specimen acquisition, safe specimen storage, and accurate rRT-PCR testing. Reported sensitivity of nasopharyngeal swab testing ranges from 38% to 78%, although the exact rate is still unknown [16,19]. Multiple studies have attempted to identify causes of false negative COVID test results, which are classified as pre-analytical and analytical vulnerabilities to testing [[11], [12], [13], [14],19,20]. Pre-analytical challenges with COVID testing include poor nasopharyngeal specimen collection technique, inadequate quantity of specimen obtained, and specimen storage issues, while analytical issues include testing outside of the diagnostic window, use of inadequately validated assays, instrument malfunctioning, and misinterpretation of expression profiles [11,13]. One particular study by Li et al. evaluating over 3000 COVID tests done in Wuhan, China reported that one of the most likely causes of false negative testing is inadequate specimen acquisition [13]. Specifically, the authors posit that testing providers were often learning on the job, and a lack of training led to inconsistent specimen acquisition and variable test sensitivity [13].
This study aimed to assess the effect of a formalized nasal anatomy and technique training session on medical providers' comfort level and knowledge base in performing accurate COVID testing. Almost all of the providers enrolled in this study had completed fewer than 10 COVID tests, and only half had performed any sort of nasal testing in the past. While the CDC has encouraged adopting the influenza testing technique for nasopharyngeal specimen retrieval, only 36% of those enrolled in this study had any experience performing influenza testing [1]. The inexperience with nasopharyngeal testing seen in our study population is not uncommon in the current resource-strained healthcare setting, as medical providers of various backgrounds are being tasked with COVID testing.
Prior to the educational session, only 5 of the 17 providers in this study felt comfortable independently performing a COVID test. Most providers acknowledged the nasopharynx as the optimal target for COVID swab testing, although only half correctly identified the nasopharynx on a sagittal image. Many providers were also unable to identify which nare to swab to avoid nasal obstruction (i.e. deviated septum, inferior turbinate hypertrophy), and some did not recognize that the nasopharynx could be accessed via either nare. This study found that after a 20-minute educational session provided by an otolaryngologist discussing proper nasopharyngeal swabbing technique and pertinent nasal anatomy, significantly more providers felt comfortable independently performing and teaching COVID testing. Almost all providers were able to locate the nasopharynx, and most were able to identify the correct nare to swab in the presence of nasal obstruction. These providers' improved knowledge base should theoretically address their reported COVID testing challenges. Patient discomfort and nasal bleeding from nasopharyngeal swabbing often result from trauma to the nasal septum, and identification of septal deviation may help providers avoid septal trauma with COVID testing. Knowledge that the nasopharynx can be accessed through either nare may also help providers troubleshoot unilateral nasal obstruction by passing a test swab through the contralateral nose.
Limitations to this study include small sample size and a single-institution experience. The nurses referred for this educational session were either pre-operative surgical nurses or labor and delivery nurses, most of whom were not routinely performing nasal testing. As a more diverse group of medical providers are being tasked with COVID testing during the COVID-19 pandemic, it is even more imperative to provide adequate training to ensure testing accuracy. Given their patient populations, most of the nurses enrolled in this study had performed fewer than 10 COVID tests prior to the educational session. This study strongly supports the early implementation of nasal anatomy and technique training to increase provider comfort and knowledge prior to high volume COVID testing. Future directions include implementation of a formal nasal anatomy and technique training session at other institutions and generalizing the findings of this study. Additional studies may assess the impact of a nasal anatomy and technique educational session on the rate of false negative COVID test results.
5. Conclusion
The nasopharynx carries a high viral load of SARS-CoV-2 that makes it an optimal target for diagnostic testing. Many testing providers may not understand the nasal anatomy or proper technique for attaining adequate nasopharyngeal specimen, thus leading to a high false-negative COVID testing rate. Early implementation of nasal anatomy education and nasopharyngeal swab technique training by the otolaryngologist can help improve medical provider comfort and knowledge base in performing more accurate COVID testing.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no conflicts of interest to report.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amjoto.2020.102777.
Appendix A. Supplementary data
Document describing the pertinent details of the nasopharyngeal swab educational session provided by the otolaryngologist. This includes a review of CDC guidelines for COVID testing and details from a video highlighting proper nasopharyngeal swabbing technique.
References
- 1.Centers for Disease Control Interim guidelines for collecting, handling, and testing clinical specimens from persons for coronavirus disease 2019 (COVID-19) 2020. https://www.cdc.gov/coronavirus/2019-nCoV/lab/guidelines-clinical-specimens.html
- 2.World Health Organization Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases. 2020, March 7. https://www.who.int/publications-detail/laboratory-testing-for-2019-novel-coronavirus-in-suspected-human-cases-20200117
- 3.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G. Detection of SARS-CoV-2 in different types of clinical specimens. Jama. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu F., Yan L., Wang N., Yang S., Wang L., Tang Y. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020;71(15):793–798. doi: 10.1093/cid/ciaa345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hong K.H., Lee S.W., Kim T.S., Huh H.J., Lee J., Kim S.Y. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann Lab Med. 2020;40(5):351–360. doi: 10.3343/alm.2020.40.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel R., Babady E., Theel E.S., Storch G.A., Pinsky B.A., George K.S. 2020. Report from the American Society for Microbiology COVID-19 international summit, 23 March 2020: value of diagnostic testing for SARS–CoV-2/COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. New England Journal of Medicine. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng M.P., Papenburg J., Desjardins M. Original: diagnostic testing for severe acute respiratory syndrome–related. N Engl J Med. 2020;382:727–733. doi: 10.7326/M20-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Y., Yang M., Shen C., Wang F., Yuan J., Li J. February 17, 2020. Laboratory diagnosis and monitoring the viral shedding of 2019-nCoV infections. medRxiv. DOI, 10(2020.02), 11-20021493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thoracic S. Expert consensus for bronchoscopy during the epidemic of 2019 novel coronavirus infection (Trial version) Zhonghua jie he he hu xi za zhi = Zhonghua jiehe he huxi zazhi = Chinese journal of tuberculosis and respiratory diseases. 2020;43(3):199. doi: 10.3760/cma.j.issn.1001-0939.2020.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Lippi G., Simundic A.M., Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19) Clinical Chemistry and Laboratory Medicine (CCLM) 2020;1 doi: 10.1515/cclm-2020-0285. [ahead-of-print] [DOI] [PubMed] [Google Scholar]
- 12.Tang Y.W., Schmitz J.E., Persing D.H., Stratton C.W. Laboratory diagnosis of COVID-19: current issues and challenges. J Clin Microbiol. 2020;58(6) doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li J., Ye G., Chen L., Wang J., Li Y. Analysis and countermeasures of false negative results of new coronavirus (2019-nCoV) nucleic acid test. Chinese J Lab Med. 2020:43. [Google Scholar]
- 14.Pan Y., Long L., Zhang D., Yuan T., Cui S., Yang P. Potential false-negative nucleic acid testing results for severe acute respiratory syndrome coronavirus 2 from thermal inactivation of samples with low viral loads. Clin Chem. 2020;66(6):794–801. doi: 10.1093/clinchem/hvaa091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marty F.M., Chen K., Verrill K.A. How to obtain a nasopharyngeal swab specimen. N Engl J Med. 2020;382(22):e76. doi: 10.1056/NEJMvcm2010260. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y.G., Yun S.G., Kim M.Y., Park K., Cho C.H., Yoon S.Y. Comparison between saliva and nasopharyngeal swab specimens for detection of respiratory viruses by multiplex reverse transcription-PCR. J Clin Microbiol. 2017;55(1):226–233. doi: 10.1128/JCM.01704-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L., Chen Q.Y., Li Y.Y., Wang Y.F., Yang Z.F., Zhong N.S. Comparison among nasopharyngeal swab, nasal wash, and oropharyngeal swab for respiratory virus detection in adults with acute pharyngitis. BMC Infect Dis. 2013;13(1):281. doi: 10.1186/1471-2334-13-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munywoki P.K., Hamid F., Mutunga M., Welch S., Cane P., Nokes D.J. Improved detection of respiratory viruses in pediatric outpatients with acute respiratory illness by real-time PCR using nasopharyngeal flocked swabs. J Clin Microbiol. 2011;49(9):3365–3367. doi: 10.1128/JCM.02231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu R., Han H., Liu F., Lv Z., Wu K., Liu Y. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin Chim Acta. 2020;505:172–175. doi: 10.1016/j.cca.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winichakoon P., Chaiwarith R., Liwsrisakun C., Salee P., Goonna A., Limsukon A. Negative nasopharyngeal and oropharyngeal swabs do not rule out COVID-19. J Clin Microbiol. 2020;58(5) doi: 10.1128/JCM.00297-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Document describing the pertinent details of the nasopharyngeal swab educational session provided by the otolaryngologist. This includes a review of CDC guidelines for COVID testing and details from a video highlighting proper nasopharyngeal swabbing technique.