Abstract
In response to loosened telehealth regulations and local restrictions on elective procedures during the coronavirus disease 2019 (COVID-19) pandemic, telemedicine use has dramatically increased. The goal of this study was to analyze patterns in telemedicine use among podiatric physicians during the COVID-19 crisis on a national level. Anonymous responses to a survey of practice metrics as well as subjective impressions of telemedicine efficacy were collected from 246 respondents, representing >1% of practicing podiatrists in the United States. Linear regression was performed to identify variables associated with COVID-19 prevalence and variables associated with higher self-reported likelihood of offering telemedicine visits post-COVID-19. Physicians in areas of lower COVID-19 prevalence were found to dispense durable medical equipment more frequently in-office and conduct more post-op telemedicine visits, with fewer visits for infections and trauma. Podiatrists in these regions also rated telemedicine more effective for medical and musculoskeletal pathologies. Additionally, fewer of their practices had modified office hours, and more of them advertised telemedicine services. Physicians more likely to offer telemedicine post-COVID-19 had significantly higher new patient volume and increased acuity of cases, with patient admission to the hospital after telemedicine visits. These physicians ranked the effectiveness of telemedicine more highly for every pathology surveyed. Of note, American College of Foot and Ankle Surgeons region and years in clinical practice were not statistically associated with likelihood of offering telemedicine visits post-COVID-19. This study represents the first systematic national assessment of telemedicine use in podiatry and highlights clinically relevant changes in practice and perception of telemedicine in response to the COVID-19 pandemic.
Keywords: coronavirus, pandemic, podiatric medicine, podiatric surgery, telehealth, telemedicine
Telemedicine has given patients an efficient and accessible means of extension for patient-physician interactions. One of the earliest reported uses of telehealth involves an article from 1879 discussing the use of telecommunications for patient-physicians in order to avoid unnecessary in-office visitation (1). The World Health Organization declared a national state of emergency concerning the coronavirus disease 2019 (COVID-19) outbreak on March 11, 2020. As of June 2020, there are 2.1 million cases with 116,862 associated deaths in the nation and 8.2 million cases with 445,535 deaths globally (2,3). The novel coronavirus pandemic drastically changed medical priorities for healthcare organizations on a global scale. These changes include careful surveillance of symptomatic and asymptomatic individuals, increasing coronavirus testing numbers and maintaining social distancing with strict public health quarantine, all disrupting typical routine care for physicians and surgeons. Unless the clinical encounter was considered emergent, healthcare visits and nonemergent surgeries were suspended in the United States.
During the coronavirus pandemic response, the United States government loosened telehealth regulations and provided funding to expand telehealth services and reduce the risk of viral spread (4). The use of telemedicine by healthcare institutions dramatically increased (5,6). A multitude of disciplines adapted rapidly to implement telemedicine with the intention of preventing virus exposure and reducing the burden on the healthcare system (7, 8, 9, 10, 11, 12, 13, 14, 15). Recently, there has been a significant amount of sharing of expertise throughout the literature to improve application of telehealth with better outcomes. The orthopedic department at Johns Hopkins University described their experience with rapidly integrating a program by applying important factors: patient triage, technologic resources, credentialing, billing, and coding (16). Furthermore, 50% of the typical clinic volume was reached via online, synchronous, 2-way audiovisual communication, while the remaining 50% were either postponed or treated with an asynchronous method of communication (16).
The diabetic patient population is a delicate one requiring close monitoring with routine wound care and surgical interventions and, if neglected, is at a higher risk of infection, amputation, and increased mortality (17, 18, 19). According to retrospective studies from Wuhan, China, a large proportion of patients infected with COVID-19 present with comorbidities including cardiovascular and cerebrovascular ones, and diabetes, and these studies suggest an increased mortality risk for these patients (20,21). Studies have proposed strategies for optimal podiatric care: Roger et al suggested a Pandemic Diabetic Foot Triage System in a “new pandemic standard of care” determining location for site of care based on the diabetic foot conditions and urgency of the situation (17). New paradigm shifts in the management of diabetic foot wounds have been described in the literature thus far, including physician-to-patient and physician-to-home nursing in order to perform proper wound care practices (22).
Literature suggests the useful application of telehealth during previous disease outbreaks, including the Ebola virus, Severe Acute Respiratory Syndrome, H1N1 influenza, H7N9, and the Middle-East respiratory syndrome Coronavirus (23). This paradigm shift in medical management and clinical practice can be expected to have relevance in future emerging infectious disease pandemics. The goal of this epidemiological study was to analyze the use of telemedicine among podiatric physicians during the peak of the COVID-19 crisis on a national level. In addition, we evaluated trends in certain regions of the nation with high vs low prevalence, with the intent of considering how the recent crisis may impact the future of telemedicine in podiatric practices. We suspect that the landscape of clinical medicine will change dramatically post-COVID-19, where telemedicine will have a lasting impact on all disciplines. We hope to contribute applicable data associated with an accelerated introduction of telemedicine for practical and fruitful continued use of podiatric medicine and surgery in the future.
Materials and Methods
Podiatrists who utilized telemedicine during the COVID-19 pandemic were surveyed about their practice characteristics, volume, and experiences with telemedicine (Fig. S1). The survey questionnaire was designed by the study team and publicized by the authors’ social media accounts and email newsletters from the American College of Foot and Ankle Surgeons (ACFAS) and New York State Podiatric Medical Association (NYSPMA) throughout the data collection period of May 8-June 9, 2020. Our study was administered using a cloud-based software platform, Survey Monkey. This observational study was conducted in accordance with the Declaration of Helsinki.
The questionnaire was primarily written by the senior author who had prior experience with telemedicine, and was reviewed by a committee consisting of multiple members of the ACFAS, the NYSPMA, and a public health graduate students, before the survey was administered. The construct of this survey aimed to assess clinical practice characteristics of podiatric foot and ankle surgeons in the United States in relation to their use of telemedicine before and after COVID-19, as well as subjective impressions of telemedicine efficacy. The questionnaire was formatted as a self-administered online survey for ease of distribution to large sample of clinical practices across the entire United States. The survey was administered as a combination of open-ended questions, multiple choice with write-in option, and Likert scales. Multiple-choice or write-in options were used to collect clinical practice characteristics, in order to capture a large range of possible responses, due to the predicted heterogeneity of the sample population. Each multiple-choice option and high frequency write-in responses were then converted into binary variables (e.g., used zoom for telemedicine), and numeric write-in options were treated as continuous variables (e.g., number of years in clinical practice). Likert scales were used to assess subjective ranking of telemedicine efficacy.
The prevalence of COVID-19 cases was determined for each of the 9 ACFAS regions. The reported cases and deaths from March 31 to April 7, 2020 are listed for the US jurisdictions by the Center for Disease Control and Prevention Morbidity and Mortality Weekly report (24). The total resident population for each ACFAS region was calculated according to population data provided by the US Census Bureau 2019, and the number of reported COVID-19 cases as of April 7, 2020 was divided by the population data (25).
Anonymous survey responses were collected and analyzed to capture the impact COVID-19 had on a wide variety of practice metrics and physicians' experiences with telemedicine. A total of 246 respondents were identified, and when reporting individual variables, those respondents who did not answer a question were excluded from that item's analysis. Outliers were defined as any data point with measured response value more than 1.5 interquartile ranges below the first quartile or above the third quartile for each of the numerical responses and where noted were excluded from figures for improved readability.
All survey response variables were reported using n (%) for categorical data and mean ± standard deviation for numerical data. Linear regression analysis was performed to identify variables statistically associated with COVID-19 prevalence and variables associated with self-reported likelihood of offering telemedicine visits post-COVID-19.
Variables reflecting age and geographical location were not included in the regression with COVID-19 prevalence because they are not mutable characteristics. To analyze likelihood of offering telemedicine visits post-COVID-19, reported importance of telemedicine post-COVID-19 was excluded as a tautological variable. In addition to the 61 survey variables, 3 additional constructed variables were created and included in the linear regression modeling: fold change in patient case load, proportion of office time lost due to COVID-19, and COVID-19 prevalence (state level). Each predictor variable was tested against the corresponding response variable by linear regression, and the p values of regression coefficients were computed by Student's t test and corrected for multiple testing by the Benjamini-Hochberg method. Variables were considered statistically significant in their association with COVID-19 prevalence or likelihood of offering telemedicine visits post-COVID-19 at p value ≤.05.
Results
Survey Responses
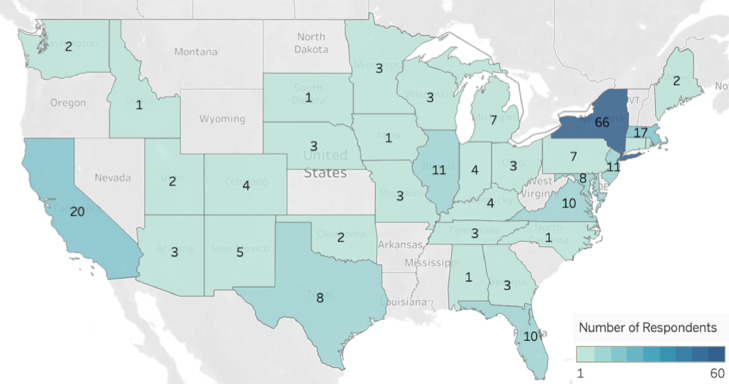
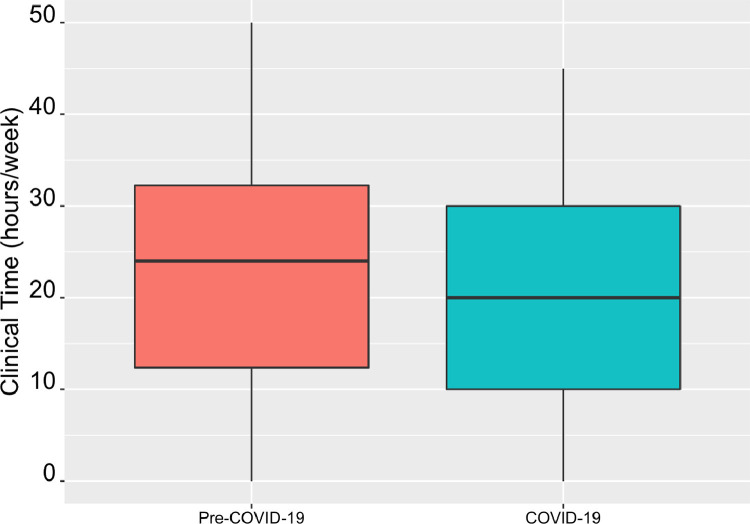
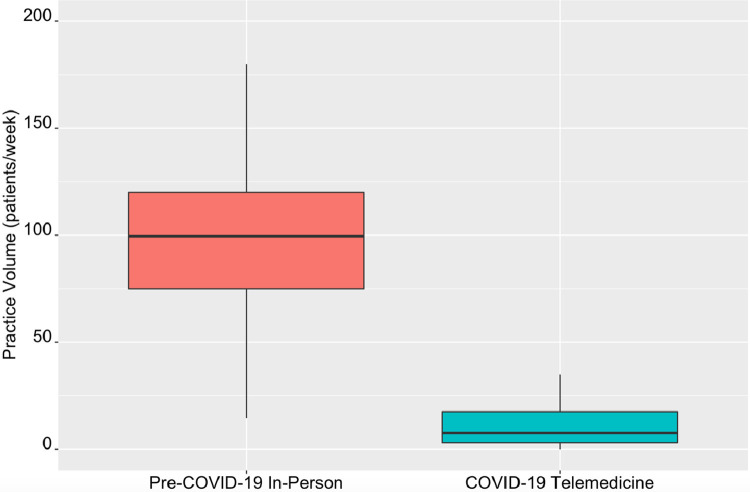
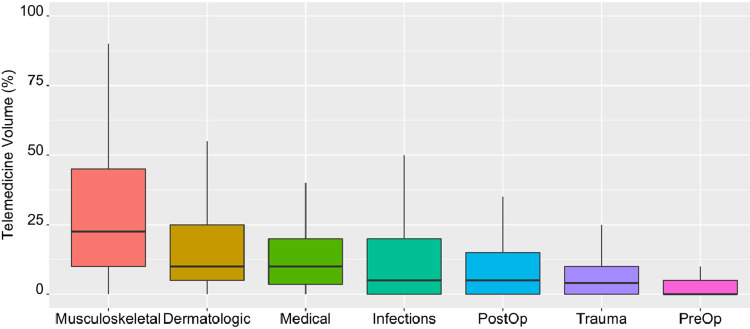
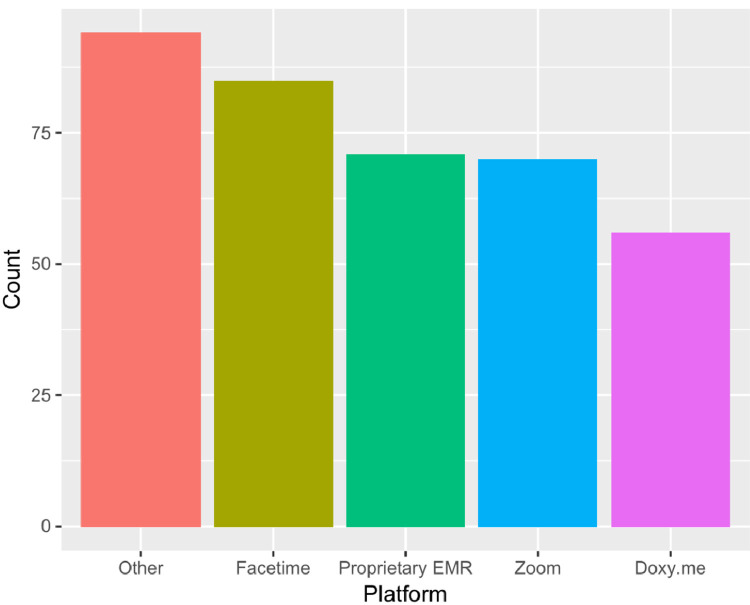
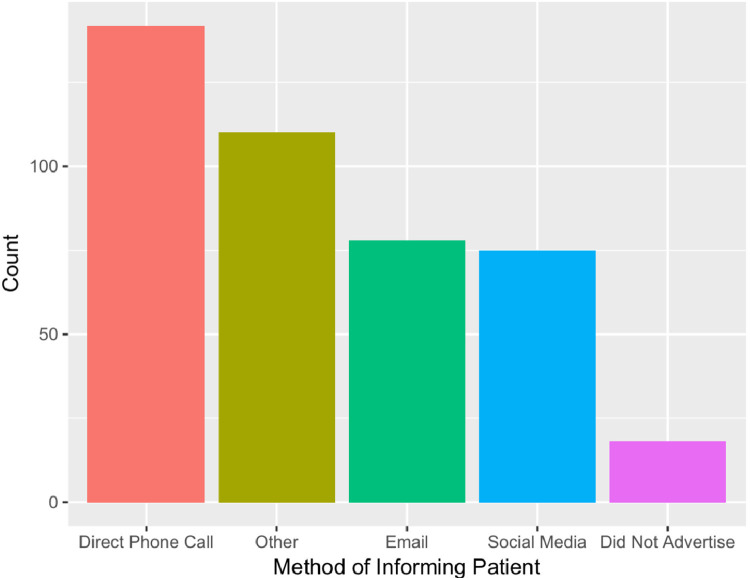
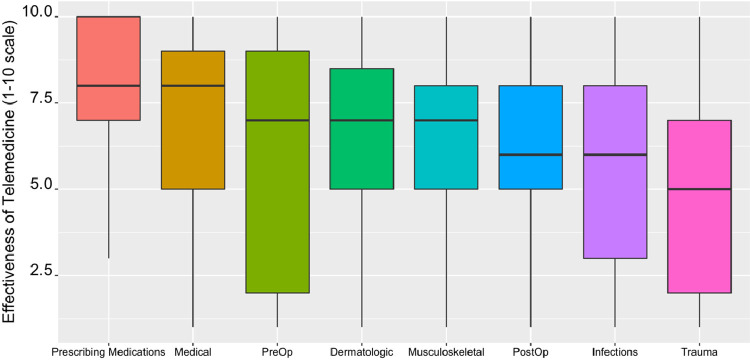
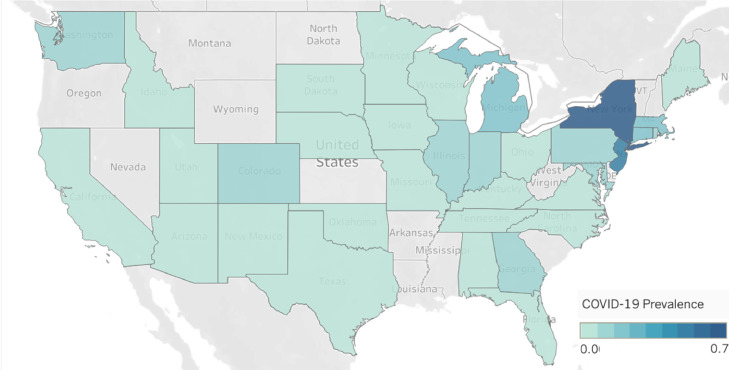
Responses to the survey were first analyzed according to practice characteristics and volume as shown in Table 1 . The majority of respondents were from the Northeast and Mid-Atlantic ACFAS regions, but all ACFAS regions were represented in the sample (Fig. 1 ). During COVID-19, the average in-person office time decreased by 9% (Fig. 2 ) and the COVID-19 telemedicine practice volume decreased 86% on average from pre-COVID-19 in-person office volume (Fig. 3 ). Respondents were also characterized according to their objective experiences with telemedicine (Table 2 ). Overall, the most frequently reported percentage of telemedicine cases were musculoskeletal (27%), and the lowest percentage (4%) were pre-op consultations (Fig. 4 ). The most frequently used video platforms were Facetime, proprietary hospital/electronic medical record platform, and Zoom (Fig. 5 ). The most frequent telemedicine advertising method was direct telephone call to patients, then email and social media (Fig. 6 ). Factors related to respondents’ subjective impressions of telemedicine were also profiled (Table 3 ). Telemedicine was rated most effective for prescribing medications (8/10), medical issues (7/10), and dermatologic conditions (7/10), and least effective on average for trauma (5/10) (Fig. 7 ). The estimated COVID-19 prevalence by state during the survey period was annotated and is shown in Supplemental Table S1. Fig. 8 is a heatmap of the estimated prevalence of COVID-19 by state, such that the estimated prevalence of COVID-19 was highest in New York using reported data from April 7, at 0.71% (26,27).
Table 1.
Practice characteristics and volume
| Practice Characteristics and Volume | All Respondents |
|---|---|
| n (%) or Average ± SD | |
| ACFAS region | |
| Northeast | 91 (38%) |
| Midatlantic | 24 (10%) |
| Pacific | 22 (9%) |
| Midwest | 21 (9%) |
| Big West | 19 (8%) |
| Tristate | 18 (8%) |
| Great Lakes | 18 (8%) |
| Southeast | 13 (5%) |
| Gulf States | 11 (5%) |
| Years in clinical practice | 19 ± 11 |
| Used telemedicine before COVID-19 | 13 (6%) |
| Office open during COVID-19 | 215 (90%) |
| Modified office hours | 187 (84%) |
| Normal in-person office time (h/wk) | 23 ± 12 |
| Time open during COVID-19 (h/wk) | 21 ± 12 |
| Distributed durable medical equipment | 172 (72%) |
| Dispensed in-person at office | 74 (31%) |
| Patients ordered online or at store | 67 (28%) |
| Drop shipped from a vendor or office | 31 (13%) |
| Jan and Feb in-person (pts/wk) | 108 ± 85 |
| Mar and Apr telemedicine (pts/wk) | 15 ± 21 |
| Telemedicine new patients (pts/wk) | 3 ± 5 |
Characteristics are expressed as n (%) or as the mean ± SD. For each variable, responses NA values were excluded from the analysis.
Fig. 1.
Heatmap of survey respondents. Geographic location of survey respondents by state.
Fig. 2.
Box plot of office hours. Comparison of in-person office time (h/wk) before and during COVID-19. Please note data were collected only from respondents whose office was open during COVID-19. Paired Student's t test: p value = .007.
Fig. 3.
Box plot of practice volume. Comparison of Jan and Feb in-person volume and Mar and Apr telemedicine volume (pts/wk). Paired Student's t test: p value <10−15.
Table 2.
Telemedicine: objective experience
| Telemedicine: Objective Experience | All Respondents |
|---|---|
| n (%) or Average ± SD | |
| Pathologies assessed via telemedicine (%) | |
| Musculoskeletal issues or tendinitis | 27 ± 23 |
| Dermatologic issues | 19 ± 22 |
| Medical issues | 16 ± 18 |
| Infections | 14 ± 19 |
| Post-op care | 11 ± 16 |
| Trauma | 9 ± 13 |
| Pre-op surgical discussions | 4 ± 9 |
| Video platform used | 221 (92%) |
| Facetime | 85 (36%) |
| Proprietary EMR or hospital platform | 71 (30%) |
| Zoom | 70 (29%) |
| Doxy.me | 56 (23%) |
| Other platform | 47 (20%) |
| 19 (8%) | |
| Skype | 14 (6%) |
| GoogleHangouts | 11 (5%) |
| Informed patients about telemedicine | 221 (92%) |
| Direct telephone call | 142 (59%) |
| 78 (33%) | |
| Social media | 75 (31%) |
| Other | 56 (23%) |
| Answering machine message | 34 (14%) |
| Text | 30 (13%) |
| Physical mailer | 12 (5%) |
| Length of telemedicine appointment (min) | 14 ± 6 |
| Coordinated with a visiting nurse service | 60 (25%) |
| Mar and Apr admitted telemedicine patient | 59 (25%) |
Characteristics are expressed as n (%) or as the mean ± SD. For each variable, responses NA values were excluded from the analysis.
Fig. 4.
Box plot of pathologies assessed via telemedicine (%): Distribution of reported percentage of total telemedicine volume for each pathology.
Fig. 5.
Histogram of video platform used. Other includes WhatsApp, telephone, Skype, GoogleHangouts, and other platforms with <20 respondents.
Fig. 6.
Histogram of telemedicine advertising method. Other includes answering machine, text message, physical mailer, and other platforms with <50 respondents.
Table 3.
Telemedicine: subjective impression
| Telemedicine: Subjective Impression | All Respondents |
|---|---|
| n (%) or Average ± SD | |
| Effectiveness of telemedicine by pathology* | |
| Prescribing medications | 8 ± 2 |
| Medical issues | 7 ± 2 |
| Dermatologic issues | 7 ± 2 |
| Musculoskeletal issues or tendinitis | 6 ± 2 |
| Post-op care | 6 ± 3 |
| Pre-op surgical discussions | 6 ± 3 |
| Infections | 6 ± 3 |
| Trauma | 5 ± 3 |
| Likelihood of offering telemedicine visits post-COVID-19* | 6 ± 3 |
| Importance of telemedicine visits post-COVID-19* | 6 ± 3 |
| % telemedicine visits that prevented hospital admission | 19 ± 30 |
| Able to triage emergencies via telemedicine effectively | 61 (52%) |
Characteristics are expressed as n (%) or as the mean ± SD. For each variable, responses NA values were excluded from the analysis.
*Question was asked using a 10-point Likert scale, ranging from 1 (lowest) to 10 (highest).
Fig. 7.
Box plot of effectiveness of telemedicine by pathology. Question was asked using a 10-point Likert scale, ranging from 1 (lowest) to 10 (highest).
Fig. 8.
Heatmap of COVID-19 prevalence. Geographic location of COVID-19 prevalence by state. Only states with survey respondents were included in the heatmap.
Factors Associated With COVID-19 Prevalence
In linear regression analysis, high COVID-19 prevalence was significantly associated with several characteristics of the physician's practice, objective experience with telemedicine, and subjective impression of telemedicine (Table 4 ). In areas of high COVID-19 prevalence, practices had significantly increased frequency of modified office hours, a higher percentage of infections and trauma cases. Practices in these areas also less frequently informed patients about telemedicine, reported increased frequency of completely closed offices, and used Facetime as their telemedicine platform at a higher rate. In areas of low COVID-19 prevalence, practices were statistically more likely to dispense durable medical equipment in-office, had a higher percentage of post-op telemedicine visits, rated telemedicine more effective for medical and musculoskeletal pathologies, and had longer hours open during COVID-19.
Table 4.
Factors associated with coronavirus disease 2019 prevalence
| Correlation Coefficient | p Value | |
|---|---|---|
| Modified office hours | .23 | .009 |
| Dispensed DME at office | -.23 | .009 |
| % Telemedicine visits | ||
| Infections | .22 | .009 |
| Trauma | .23 | .009 |
| Post-op | -.17 | .04 |
| Did not inform patients about telemedicine | .20 | .02 |
| Effectiveness of telemedicine* | ||
| Medical | -.21 | .02 |
| Musculoskeletal | -.19 | .03 |
| Completely closed | .18 | .03 |
| Hours open COVID-19 | -.19 | .03 |
| Video platform- Facetime | .17 | .04 |
Abbreviations: COVID-19, coronavirus disease 2019; DME, durable medical equipment; Post-op, postoperative.The relationship strength of the variables was determined via Pearson correlation coefficient and the statistical significance was determined using Student's t test. Positive correlation coefficient indicates association with high COVID-19 prevalence. Only significant variables (p value ≤ .05) were reported.
Question was asked using a 10-point Likert scale, ranging from 1 (lowest) to 10 (highest).
Factors Associated With Likelihood of Offering Telemedicine Visits Post-COVID-19
In linear regression analysis, higher self-reported likelihood of continued telemedicine use post-COVID-19 was significantly associated with physicians’ subjective impression and objective experience of telemedicine (Table 5 ). Physicians who responded that they were more likely to offer telemedicine post-COVID-19 had significantly higher numbers of weekly new telemedicine appointments and had a higher frequency of admitting at least one patient to the hospital after a telemedicine visit. Additionally, for every pathology surveyed, physicians who were more likely to offer telemedicine post-COVID-19 ranked telemedicine as being more effective for that pathology. Interestingly, there was no statistically significant association between self-reported likelihood of continued telemedicine use and characteristics of the physician's practice such as ACFAS region and years in clinical practice.
Table 5.
What factors are associated with continued use of telemedicine
| Correlation Coefficient | p Value | |
|---|---|---|
| Admit patient post telemedicine visit | .26 | .0003 |
| Weekly new telemedicine | .21 | .006 |
| Effectiveness of telemedicine* | ||
| Medical | .51 | 10−13 |
| Musculoskeletal | .50 | 10−13 |
| Trauma | .51 | 10−11 |
| Prescribing medications | .46 | 10−11 |
| Pre-operative | .41 | 10−9 |
| Post-operative | .41 | 10−7 |
| Infections | .37 | 10−7 |
| Dermatologic | .37 | 10−7 |
| Triage emergencies | .26 | .03 |
The relationship strength of the variables was determined via Pearson correlation coefficient and the statistical significance was determined using Student's t test. Only significant variables (p value ≤ .05) were reported.
Question was asked using a 10-point Likert scale, ranging from 1 (lowest) to 10 (highest).
Discussion
This study represents the first systematic assessment of telemedicine use in podiatric clinics across the country and highlights changes in practice in response to the unprecedented COVID-19 pandemic. Our 246 respondents represent >1% of practicing podiatrists in the United States. Although we had higher response rates from New York than other states, our survey data included responses from all 9 ACFAS regions. We have characterized the volume of telemedicine usage and breakdown of pathologies treated, as well as physician's subjective assessments of telemedicine efficacy. This analysis has revealed that podiatrists rated telemedicine most effective for prescribing medications, medical issues, and dermatologic issues and reports the most popular telemedicine platforms and advertising mechanisms.
The prevalence of COVID-19 is shifting across the United States, and current telemedicine practices should subsequently prepare for a shift in their usage of telemedicine. Physicians in areas of high COVID-19 prevalence such as the Northeast and Tristate regions should prepare for a shift in their current telemedicine practice when prevalence of COVID-19 decreases in their area. Their practices are predicted to include more durable medical equipment dispensed in office, a higher percentage of post-op telemedicine visits, and longer hours open. Physicians in regions with lower COVID-19 prevalence also rate telemedicine more effective for medical and musculoskeletal pathologies. Additionally, their practices will have a decreased frequency of modified office hours, decreased percentage of telemedicine appointments for infections and trauma, and will need to advertise telemedicine services more. Conversely, if physicians expect to have increased COVID-19 prevalence in their region, they should anticipate shifts in their telemedicine practices that are the reverse of the above. It is possible that these variables may have more to do with respondents' geographical area than COVID-19 prevalence, since COVID-19 disproportionately affected the Northeast and Tristate regions in this timeframe, and this should be noted as a limitation of this observational study.
Cronbach's alpha was not systematically assessed for the variables in this survey as they were not intended to query the same dimensionality. While certain variables assessed related concepts, such as telemedicine efficacy for different treatment indications, the aim of the study was not to intentionally test the same concept with multiple questions. Inter-rater reliability could also not be assessed for these data because there was only a single respondent from each clinical practice. Therefore, no two raters reported data from the same observation. Similarly, assessing intra-rater reliability with longitudinal observation is limited in this study as re-assessing the same respondents at a different point in time may change the responses as a result of a change in their clinical practice rather than unreliability of the test. The survey represents only a single cross section of respondents at a specific point in time rather than a longitudinal study. The survey administered in this study is entirely novel and aims to assess telemedicine use and impression of telemedicine among physicians. To our knowledge, there is no prior questionnaire with validity assessment targeted at the same research question. The clinical practice aspects of the questionnaire collect data that is directly observable such as practice location and patient volume, which we rely on respondents to report accurately from internal data. The subjective element of the survey targeted at unobservable attributes uses the 10 point Likert scale to assess impression of telemedicine efficacy. The 10 point Likert scale has been extensively applied across surveys for a wide variety of research questions and has been used to assess subjective impression of treatment efficacy (26,27).
Limitations of our study included voluntary recruitment of respondents, which may lead to a degree of nonresponse bias. The study was also limited in assuming accuracy of self-reported data due to virtual self-administration of the questionnaire. This study design was used to sample clinical practices across the entire United States, with outreach efforts by ACFAS and NYSPMA to reach a diverse pool of potential respondents. Despite the limitations of our investigation, we believe that the results of this study could be useful to help facilitate future integration of telemedicine in podiatric foot and ankle surgeon practices.
In conclusion, COVID-19 pushed the overwhelming majority (94%) of survey respondents into using telemedicine for the first time. We characterized the distinguishing features of physicians who self-reported a high likelihood of offering telemedicine visits post-COVID-19 in an attempt to identify modifiable factors or perceptions that could influence new adopters to continue offering it as a service. Physicians who are more likely to offer telemedicine post-COVID-19 had significantly higher new patient volume and increased acuity of cases, as they were more likely to have admitted at least one patient after a telemedicine visit. Physicians who were more likely to offer telemedicine post-COVID-19 ranked the effectiveness of telemedicine more highly for every pathology surveyed. Of note, COVID-19 prevalence, ACFAS region, and years in clinical practice were not statistically associated with the likelihood of offering telemedicine visits post-COVID-19, arguing against a regional or generational gap in receptiveness to offering telemedicine visits. These findings could be considered when creating trainings and recommendations to physicians who want to have a better experience with telemedicine, or to identify who is most likely to have a positive experience with telemedicine if they incorporate it into their practice.
Acknowledgments
The authors would like to thank ACFAS and NYSPMA for their assistance in reviewing the questionnaire before the survey was administered, and advertising the surveys via email. The authors would also like to thank Sam Powers, a public health graduate student at George Washington University, for his help in constructing and reviewing the questionnaire before it was administered.
Footnotes
Financial Disclosure: None reported.
Conflict of Interest: None reported.
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1053/j.jfas.2020.08.003.
Appendix. Supplementary Materials
Supplemental Table S1 Estimated Prevalence of COVID-19 by state. Data taken from the Center for Disease Control and the United States Census Bureau.
Supplemental Fig. S1 Survey Form distributed to study participants.
References
- 1.Nesbitt T. National Academies Press (US); Washington, DC: 2012. The Evolution of Telehealth: Where Have We Been and Where Are We Going? The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Board on Health Care Services; Institute of Medicine; p. 3.https://www.ncbi.nlm.nih.gov/books/NBK207141 Available at: Accessed June 24, 2020. [PubMed] [Google Scholar]
- 2.Coronavirus Disease 2019 (COVID-19). Cases in the U.S. Centers for Disease Control and Prevention web site. 2018. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates. Accessed June 18, 2020.
- 3.Coronavirus Disease 2019 (COVID-19) situation reports. World Health Organization web site. 2018. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed June 18, 2020.
- 4.OCR announces notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. U.S. Department of Health and Human Services web site. 2020. Available at: www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed June 18, 2020.
- 5.Contreras CM, Metzger GA, Beane JD, Dedhia PH, Ejaz A, Pawlik TM. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24:1692–1697. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elkbuli A, Ehrlich H, McKenney M. The effective use of telemedicine to save lives and maintain structure in a healthcare system: current response to COVID-19. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.04.003. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. BMJ. 2020;368:m1182. doi: 10.1136/bmj.m1182. [DOI] [PubMed] [Google Scholar]
- 8.Boehm K, Ziewers S, Brandt MP, Sparwasser P, Haack M, Willems F, Thomas A, Dotzauer R, Höfner T, Tsaur I, Haferkamp A, Borgmann H. Telemedicine online visits in urology during the COVID-19 pandemic-potential, risk factors, and patients' perspective. Eur Urol. 2020;78:16–20. [DOI] [PMC free article] [PubMed]
- 9.Liu S, Yang L, Zhang C, Xiang Y-T, Liu Z, Hu S, Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanthanna H, Strand NH, Provenzano DA, Lobo CA, Eldabe S, Bhatia A, Wegener J, Curtis K, Cohen SP, Narouze S. Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia. 2020;75:935–944. doi: 10.1111/anae.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garg SK, Rodbard D, Hirsch IB, Forlenza GP. Managing new-onset type 1 diabetes during the COVID-19 pandemic: challenges and opportunities. Diabetes Technol Ther. 2020;22:431–439. doi: 10.1089/dia.2020.0161. [DOI] [PubMed] [Google Scholar]
- 12.Jakhar D, Kaul S, Kaur I. WhatsApp messenger as a teledermatology tool during coronavirus disease (COVID-19): from bedside to phone-side. Clin Exp Dermatol. 2020;45:739–740. doi: 10.1111/ced.14227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markus HS, Brainin M. COVID-19 and stroke—a global World Stroke Organization perspective. Int J Stroke. 2020;15:361–364. doi: 10.1177/1747493020923472. [DOI] [PubMed] [Google Scholar]
- 14.Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: telemedicine in a Covid-19 era. Am J Ophthalmol. 2020;216:237–242. doi: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hakim AA, Kellish AS, Atabek U, Spitz FR, Hong YK. Implications for the use of telehealth in surgical patients during the COVID-19 pandemic. Am J Surg. 2020;220:48–49. doi: 10.1016/j.amjsurg.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogers LC, Lavery LA, Joseph WS, Armstrong DG. All feet on deck-the role of podiatry during the COVID-19 pandemic: preventing hospitalizations in an overburdened healthcare system, reducing amputation and death in people with diabetes. J Am Podiatr Med Assoc. 2020 doi: 10.7547/20-051. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Song K, Chambers AR. StatPearls [Internet] StatPearls Publishing; Treasure Island, FL: 2020. Diabetic foot care.https://www.ncbi.nlm.nih.gov/books/NBK553110 Available at: Accessed June 24, 2020. [Google Scholar]
- 19.Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, Mills JL, Ricco J-B, Suresh KR, Murad MH, Aboyans V, Aksoy M, Alexandrescu VA, Armstrong D, Azuma N, Belch J, Bergoeing M, Bjorck M, Chakfé N, Cheng S, Dawson J, Debus ES, Dueck A, Duval S, Eckstein HH, Ferraresi R, Gambhir R, Gargiulo M, Geraghty P, Goode S, Gray B, Guo W, Gupta PC, Hinchliffe R, Jetty P, Komori K, Lavery L, Liang W, Lookstein R, Menard M, Misra S, Miyata T, Moneta G, Munoa Prado JA, Munoz A, Paolini JE, Patel M, Pomposelli F, Powell R, Robless P, Rogers L, Schanzer A, Schneider P, Taylor S, De Ceniga MV, Veller M, Vermassen F, Wang J, Wang S; GVG Writing Group for the Joint Guidelines of the Society for Vascular Surgery (SVS), European Society for Vascular Surgery (ESVS), and World Federation of Vascular Societies (WFVS). Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg. 2019;69:3S–125S.e40. [DOI] [PMC free article] [PubMed]
- 20.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020;395:1038]. [DOI] [PMC free article] [PubMed]
- 22.Shin L, Bowling FL, Armstrong DG, Boulton AJM. Saving the diabetic foot during the COVID-19 pandemic: a tale of two cities. Diabetes Care. 2020;43:1704–1709. doi: 10.2337/dc20-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohannessian R. Telemedicine: potential applications in epidemic situations [Télémédecine: applications potentielles en situations épidémiques]. European Research in Telemedicine/La Recherche Européenne en Télémédecine. 2015;4:95-98.
- 24.Morbidity and Mortality Weekly Reports (MMWR). Centers for Disease Control and Prevention. 2020. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e4.htm. Accessed June 9, 2020.
- 25.National Population Totals: 2010-2019. United States Census Bureau. 2020. Available at: https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-total.html. Accessed June 9, 2020.
- 26.Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Clifasefi S, Garner M, Douglass A, Larimer ME, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Subst Abus. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bolognese JA, Schnitzer TJ, Ehrich EW. Response relationship of VAS and Likert scales in osteoarthritis efficacy measurement. Osteoarthritis Cartilage. 2003;11:499–507. doi: 10.1016/s1063-4584(03)00082-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table S1 Estimated Prevalence of COVID-19 by state. Data taken from the Center for Disease Control and the United States Census Bureau.
Supplemental Fig. S1 Survey Form distributed to study participants.