Abstract
In the United States (US), chronic disease risk factors are highly prevalent among Asian immigrant communities, who also exhibit low health screening rates. Perceived neighborhood social cohesion (NSC) has been associated with preventive healthcare use in the general US population, although it remains unexplored among Asian Americans (AAs). The aim of this study is to evaluate the association between NSC and preventive screening for hypertension, high cholesterol, diabetes, and depression among East, South and Southeast Asian American (EAA, SAA, SEAA) communities in New York City (NYC) using cross-sectional, locally collected data from 2013 to 2016. NSC was assessed using a 4-question scale to create an additive score between 4 and 16 and was analyzed both as a continuous and categorial variable (High, Medium, and Low tertiles). Recent screening was defined as a check-up within the last year for each of the included health conditions. A one-unit increase in NSC score was associated with increased odds of recent screening for high cholesterol in EAAs (AOR = 1.09, 95%CI:1.00–1.20); for high cholesterol, diabetes, and depression in SAAs (AOR = 1.08, 95%CI:1.00–1.20; AOR = 1.07, 95%CI:1.00–1.15; AOR = 1.15, 95%CI:1.06–1.25); and with high cholesterol among SEAAs (AOR = 1.12, 95%CI:1.00–1.25). Overall, NSC was an important facilitator for preventive screening behaviors for specific conditions in different groups, though was consistently associated with screening for high cholesterol in our sample. Enhancing NSC through family and community-based programming may be one strategy to encourage screening for preventive behaviors, though more research is needed to elucidate a precise mechanism.
Keywords: Social cohesion, Neighborhood environment, Social support, Hypertension, Type 2 diabetes, Cholesterol, Depression, Asian immigrants, Screening
Highlights
-
•
Recent cholesterol screening consistently associated with neighborhood social cohesion (NSC).
-
•
Association between NSC and recent screening varied by Asian American subgroup.
-
•
Both one-unit and tertile increases in NSC were associated with screening behaviors.
-
•
Recent depression screening was particularly low in the study sample.
1. Background
Asian Americans (AAs) are the fastest growing ethnic population in the United States (US) (Pew Research Center, 2012). Chronic diseases such as type 2 diabetes and cardiovascular disease (CVD) are highly prevalent across certain AA communities (Ye et al., 2009). Factors contributing to this chronic disease burden among AA communities may include lifestyle contributors (diet, exercise, sleep, and stress) as well as barriers to accessing healthcare (including language and cultural barriers, and lack of health insurance) (Ye et al., 2009; Kim and Keefe, 2010; Appel et al., 2011). Healthcare utilization rates among AAs are also low; only 55.3% of foreign-born AA adults noted having contact with a doctor in the last 12 months (Ye et al., 2012), significantly lower than the 62.5% proportion observed among US-born AAs as well as the 84.3% US average (Ye et al., 2012; Centers for Disease Control and Prevention, 2018). Moreover, recent studies suggest that declines in CVD mortality observed in the broader US population in the past decade have not been as great in AA populations, indicating that current activities may not be reaching these groups (Hastings et al., 2015; Jose et al., 2014). Similarly, there is growing evidence of various health-related disparities between different AA subgroups, such as the greater heart disease mortality burden observed among Asian Indian and Filipino American men (Jose et al., 2014). These findings highlight the importance of disaggregated analysis in AA health research to address different burdens and health dynamics experienced within these different subgroups.
Secondary prevention of chronic diseases through preventive healthcare use is an important component of reducing disease incidence and progression. Despite recommendations by the US Preventive Services Task Force for routine screenings of hypertension, type 2 diabetes, cholesterol, and depression, low screening rates among AAs remain a major obstacle in the prevention of chronic disease (Collins et al., 2002; Contreras, 1999; Tung et al., 2017; U.S. Preventive Services Task Force, n.d.). AAs are the least likely ethnic group to receive recommended diabetes screening (34% lower adjusted odds than non-Hispanic whites) (Tung et al., 2017). Likewise, in a nationwide survey, AAs were less likely than the population average to report having their blood pressure checked (74% vs. 83%) and more likely to have never had cholesterol checked (19% vs 16%) (Collins et al., 2002).
The need for early screening for CVD risk factors among AAs is compounded by the fact that new screening guidelines identify certain ethnicities, like South Asian Americans (SAAs), at increased risk for developing CVD (American Health Association News, 2019). Likewise, although depression prevalence estimates differ across the AA community, the underutilization of mental health services and barriers in depression screening are significant concerns, which may contribute to issues of underdiagnosis (Kim et al., 2015; Office of the Surgeon General, et al., 2001; Augsberger et al., 2015; Misra et al., 2020). Interventions to increase preventive screening have usually targeted individual-level risk factors or healthcare settings, such as increasing access to health insurance, improving awareness and providing navigation for health services, or changing provider behavior to enhance patient screening (Park et al., 2018; Ursua et al., 2014; Ngoc Nguyen et al., 2008).
Growing evidence has highlighted the role community- or neighborhood-level factors, such as perceived neighborhood social cohesion (NSC), as barriers or facilitators to preventive healthcare use or improvement of health outcomes among AAs (Dong and Bergren, 2017; Lagisetty et al., 2016; Yi et al., 2016). NSC is defined as the perceived degree of connectedness among neighbors, and their willingness to intervene for the common good (Sampson et al., 1997). The role of NSC in individual screening behaviors can be understood through the socio-ecological model, which posits that individual-level health behaviors are catalyzed by layers of high-order factors (e.g. interpersonal networks) which interact with each other and collectively shape an individual's unique health experience (McLaren and Hawe, 2005). Past studies have analyzed the variable either as a continuous measure, providing insights on the effect of incremental increases in NSC on health outcomes, or as a categorical measure using tertiles in order to better analyze key differences between “high” and “low” NSC (Kim and Kawachi, 2017; Lagisetty et al., 2016). To understand the specific mechanisms of the association between increased NSC and higher uptake of preventive health services, Kim and Kawachi (2017) have hypothesized four casual pathways: 1) increased diffusion of information about preventive services; 2) social and psychological support; 3) collective ability to advocate for resources; and 4) maintenance of healthy norms through informal social control (Kim and Kawachi, 2017). However, the relationship between NSC and preventive healthcare use has not been explored among AAs, a community with many unique neighborhood dynamics (Kim and Kawachi, 2017). For example, many AAs live in ethnic enclaves, such as Chinatown in New York City (NYC), which are neighborhoods comprised of members of similar national origin or ethnicity (Walton, 2015). Given the importance of informal and formal community support systems in AA communities and evidence linking neighborhood factors with certain types of healthcare utilization, higher NSC may correspond with preventive healthcare use in this community as observed in other US populations (Supplemental File 1) (Weng, 2016; Kim and Kawachi, 2017; Chang and Chan, 2015).
NSC has been studied with a select number of health conditions and behaviors among AAs. While no association between NSC and physical activity has been observed among AAs in national data, higher NSC has been associated with reduced hypertension and physical activity among select SAA subgroups (Yi et al., 2016; Lagisetty et al., 2016; Yi et al., 2020). Its comparative protective effect on different AA immigrant sub-populations remains largely unknown, and its association with other non-communicable conditions such as high cholesterol is unexplored (Lagisetty et al., 2016). Thus, the aim of this study is to evaluate the association between NSC with guideline concordant screening for diabetes, hypertension, high cholesterol, and depression among Asian immigrant populations in NYC.
2. Methods
The NYU Center for the Study of Asian American Health's Community Health Resources and Needs Assessment (CHRNA) was a cross-sectional survey administered between 2013 and 2016 in 15 NYC AA communities. Surveys were conducted at community-based social services agencies, faith-based organizations, or during community events (such as festivals, informational events, and health fairs) and included validated questions on participant demographics, healthcare access, health status, and various disease risk factors. Community-based convenience sampling was conducted to recruit self-identifying AA participants aged 18–85 years living in the NYC metropolitan area in partnership with AA-serving community organizations, and surveys were administered in the participant's preferred language. Data collection was approved by the NYU Grossman School of Medicine Institutional Review Board. Survey methods have been previously described (Jung et al., 2017).
For the purpose of the study, AAs were defined as participants who self-identified as being from one of three Asian ethnic subgroups based on country of origin: East Asian Americans (EAAs), South Asian Americans (SAAs), and South East Asian Americans (SEAAs). EAA included Chinese, Korean, Japanese, Tibetan – Himalayan ethnicities, SAA included Asian Indian, Bangladeshi, Pakistani, Sri Lankan, Nepali - Himalayan, Indo-Caribbean ethnicities, and SEAA included Filipino, Vietnamese, Cambodian, Indonesian, Thai ethnicities. Socio-demographic variables included sex, age, percentage of time lived in US, self-reported English fluency, self-rated health, education, income, and discrimination. Discrimination was measured by the nine-item Everyday Discrimination Scale (range 0–45), with higher scores indicating greater perceived discrimination (Williams et al., 1997).
NSC was assessed using a modified four-item scale developed by Sampson et al. (1997).) Participants were provided four statements and asked how true each was in the context of their own neighborhoods (scale of 1 to 4): 1) People in this neighborhood can be trusted; 2) People in this neighborhood generally get along with each other; 3) I have neighbors who would help me if I had an emergency; and 4) People in my neighborhood look out for each other. Scores for each NSC statement were added into an overall NSC score between 4 and 16 (a higher score indicating stronger perceived neighborhood social cohesion). For both perceived discrimination and NSC, mean scores were used to fill in missing data (“don't know” or “skipped”) when the participant answered ≥75% of the scale questions (Downey and King, 1998). Scores were analyzed both as a continuous variable and as a categorical variable (High, Medium, and Low using sample-based tertiles). Past usage to analyze NSC trends in other AA populations demonstrated validity of the instrument, and although reliability of the tool in one study among AAs was relatively low (α = 0.65), the tool evidenced strong reliability in our study (α = 0.87) (Hong et al., 2014; Lagisetty et al., 2016).
NSC score tertiles across the entire study sample were identified as: low (4.0–11.9), medium (12.0–14.9), and high (15.0–16.0) thresholds were calculated such that approximately 33.3% of the participants would fall into each level of perceived NSC. Overall descriptive statistics were first analyzed and then stratified by NSC tertiles; ANOVA and chi square tests were used to assess group differences. Multivariable complete-case regression analyses were conducted to assess odds ratios (ORs) of recent screening by one-unit increases and tertiles of NSC. Given prior evidence suggesting a complex relationship between social cohesion and discrimination in neighborhood social processes, models were first adjusted solely for discrimination, and then further adjusted for sex, age, percentage of time lived in the US, self-reported English proficiency, and education (based on literature and preliminary bivariate analysis) (Saleem et al., 2018). Participants with missing data on any of the covariates (n = 219 in full sample) or screening behaviors data (n = 89 in full sample) were excluded in each regression analysis. Significance for both the continuous and tertile-based analyses was set at an OR 95% confidence interval which excluded the 1.00 null hypothesis value. All analyses were performed using R Version 4.0.0 (R Core Team, 2020).
Preventive healthcare use was assessed through recent screening behaviors for four conditions; participants were asked how recently, if ever, a check-up or screening was received for: 1) cholesterol, 2) diabetes, 3) blood pressure, and 4) depression or other mental health related problems. Answer choices included: in the past 12 months, 1 to 2 years ago, 2 to 3 years ago, 3 or more years ago, never, and don't know/not sure. Given the study aim of assessing recent health screenings, responses for each question were synthesized into a binary variable for analysis: recent (in the past 12 months), >one year/don't know/not sure (all other answers).
3. Results
Of the 1684 participants of EAA (n = 504), SAA (n = 710), or SEAA (n = 470) descent surveyed, 290 were excluded due to missing data on NSC. A total of 1394 participants remained for the final analysis, including 401 EAA, 630 SAA, and 360 SEAA participants. Table 1 provides a summary of descriptive results of socio-demographic variables across NSC tertiles.
Table 1.
Demographic characteristics of study population, n = 1394.
| Total (n = 1394) |
Low NSC [4.0–11.9] (n = 359) |
Medium NSC [12.0–14.9] (n = 522) |
High NSC [15.0–16.0] (n = 513) |
|
|---|---|---|---|---|
| Age, mean ± SD | 46.0 ± 16.5 | 43.6 ± 16.5 | 44.0 ± 16.6 | 49.7 ± 15.8 |
| Percent of time in US, mean ± SD | 0.41 ± 0.28 | 0.45 ± 0.31 | 0.44 ± 0.29 | 0.36 ± 0.24 |
| Discrimination, mean ± SD | 5.94 ± 8.01 | 9.46 ± 9.28 | 6.20 ± 7.46 | 3.29 ± 6.54 |
| Asian American subgroup, n (%) | ||||
| East Asian | 401 (28.8) | 98 (27.3) | 145 (27.8) | 158 (30.8) |
| South Asian | 630 (45.2) | 129 (33.4) | 218 (41.8) | 292 (56.9) |
| Southeast Asian | 363 (26.0) | 141 (39.3) | 159 (30.5) | 63 (12.3) |
| Sex, n (%) | ||||
| Male | 593 (42.6) | 160 (44.6) | 232 (44.5) | 201 (39.2) |
| Female | 800 (57.4) | 216 (55.7) | 320 (54.7) | 323 (60.4) |
| English fluency, n (%) | ||||
| Very well | 461 (33.2) | 125 (35.2) | 208 (40.0) | 128 (25.0) |
| Well | 477 (34.3) | 107 (29.9) | 183 (35.2) | 187 (36.5) |
| Not well/not at all | 452 (32.5) | 126 (35.2) | 129 (24.8) | 197 (38.5) |
| Education, n (%) | ||||
| College graduate | 554 (40.3) | 139 (39.5) | 230 (45.5) | 185 (36.5) |
| High school/some college | 464 (33.7) | 124 (35.2) | 186 (36.0) | 154 (30.4) |
| Less than high school | 358 (26.0) | 89 (25.3) | 101 (19.5) | 168 (33.1) |
| Income, n (%) | ||||
| >$55,000 | 326 (23.4) | 64 (17.8) | 156 (29.9) | 106 (20.7) |
| $25,000–$55,000 | 355 (25.5) | 111 (30.9) | 130 (24.9) | 114 (22.2) |
| <$25,000 | 413 (29.6) | 105 (29.2) | 134 (25.7) | 174 (33.9) |
| Missing/Don't know/decline to state | 300 (21.5) | 79 (22.0) | 102 (19.5) | 119 (23.2) |
| Self-reported health status, n (%) | ||||
| Excellent/very good | 503 (36.2) | 111 (31.1) | 218 (41.9) | 174 (34.1) |
| Good | 489 (35.2) | 138 (38.7) | 176 (33.8) | 175 (34.2) |
| Fair/poor | 396 (28.5) | 108 (30.3) | 126 (24.2) | 162 (31.7) |
The average age of participants was 46.0 years. Fifty-seven percent of participants were female, 40.3% were college graduates, 29.6% had an annual income below $25,000, and 36.2% reported excellent or very good health. The average NSC score across the study population was 12.88 out of 16, with statistically different group averages of 13.04 among EAA, 13.48 among SAA, and 11.68 among SEAA participants. Analysis of association between individual covariates and NSC while adjusted for all other covariates identified the following significant determinants (data not shown): age was positively associated with NSC, while SEAA subgroup and discrimination were negatively associated. Compared to the full sample, EAA participants on average were slightly older (mean: 56.2, SD:17.36) and had significantly lower English proficiency (50.8% speaking English not well/not at all), while SEAA participants reported significantly greater perceived discrimination (mean: 8.23, SD:8.15).
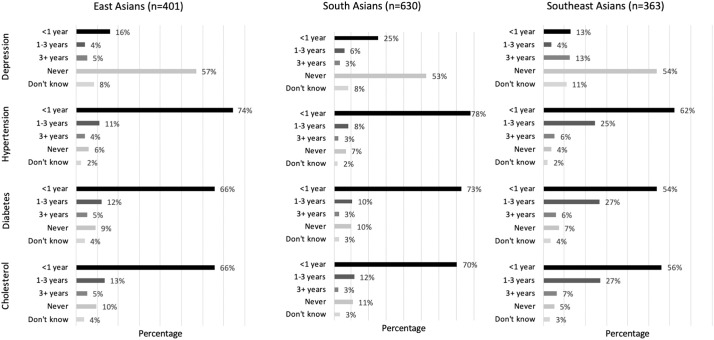
Across the study population, a majority of participants reported recent screening for the chronic disease conditions under study, with the exception of depression (Fig. 1 ). In the total sample, during the past year, 72.9% of participants had screened for hypertension, 65.9% had screened for diabetes, 65.4% had screened for high cholesterol, and 19.4% had screened for depression.
Fig. 1.
Summary of recent screening behaviors of chronic disease conditions in study population^, n = 1394.
^ Percentages may not add to 100% as participants with missing data on recent screening behaviors not displayed.
After adjusting for covariates, in the total sample, a one-unit increase in NSC was associated with increased odds of recent checkup for all examined chronic disease screenings (Table 2 ). However, analysis stratified by AA subgroup identified that the magnitude of association between NCS and preventive screening varied by screening type and statistical significance varied by AA subgroup. A one-unit increase in NSC was associated with increased odds of cholesterol screening for all subgroups, with an increased odds of depression and diabetes screening only among SAAs (AOR = 1.15, 95%CI = 1.06–1.25; AOR = 1.07, 95%CI = 1.00–1.15).
Table 2.
Multivariable regression models of one-unit increase in Neighborhood Social Cohesion score and recent check-up (within the last year) for different chronic diseases, n = 1394.
| Model | Preventative behavior (recent check-up) | Total sample, n = 1394 OR (95%CI) |
East Asian3, n = 401 OR (95%CI) |
South Asian4, n = 630 OR (95%CI) |
Southeast Asian5, n = 360 OR (95%CI) |
|---|---|---|---|---|---|
| Unadjusted | Cholesterol | 1.13 (1.09–1.18) | 1.11 (1.03–1.20) | 1.11 (1.04–1.17) | 1.14 (1.05–1.23) |
| Diabetes/blood sugar | 1.12 (1.08–1.17) | 1.10 (1.02–1.18) | 1.09 (1.03–1.16) | 1.11 (1.03–1.20) | |
| Blood pressure | 1.13 (1.09–1.18) | 1.13 (1.04–1.22) | 1.09 (1.02–1.16) | 1.11 (1.03–1.20) | |
| Depression | 1.13 (1.08–1.19) | 1.12 (1.01–1.24) | 1.13 (1.05–1.21) | 1.05 (0.94–1.18) | |
| Adjusted for Discriminaton.1 | Cholesterol | 1.12 (1.08–1.17) | 1.11 (1.02–1.21) | 1.10 (1.03–1.17) | 1.13 (1.04–1.23) |
| Diabetes/blood sugar | 1.11 (1.07–1.16) | 1.09 (1.00–1.18) | 1.09 (1.03–1.17) | 1.11 (1.02–1.21) | |
| Blood pressure | 1.12 (1.08–1.18) | 1.12 (1.03–1.22) | 1.08 (1.01–1.16) | 1.13 (1.04–1.24) | |
| Depression | 1.15 (1.09–1.22) | 1.12 (0.99–1.25) | 1.18 (1.09–1.28) | 1.02 (0.95–1.16) | |
| Adjusted for Discrimination.1 + All2 | Cholesterol | 1.10 (1.05–1.15) | 1.09 (1.00–1.20) | 1.08 (1.01–1.16) | 1.12 (1.00–1.25) |
| Diabetes/blood sugar | 1.09 (1.04–1.15) | 1.06 (0.97–1.17) | 1.07 (1.00–1.15) | 1.09 (0.97–1.22) | |
| Blood pressure | 1.10 (1.04–1.15) | 1.09 (0.99–1.21) | 1.07 (0.99–1.15) | 1.07 (0.96–1.20) | |
| Depression | 1.12 (1.05–1.18) | 1.07 (0.95–1.22) | 1.15 (1.06–1.25) | 0.98 (0.86–1.13) |
Discrimination: The everyday discrimination scale (Williams et al., 1997).
Sex, age, percent of time lived in US, English fluency, education.
East Asian: Chinese, Korean, Japanese, Tibetan – Himalayan.
South Asian: Asian Indian, Bangladeshi, Pakistani, Sri Lankan, Nepali – Himalayan, Indo-Caribbean.
Southeast Asian: Filipino, Vietnamese, Cambodian, Indonesian, Thai.
Although higher tertiles of NSC were associated with recent screening for each of the four conditions in the total population, most of these associations were not significant when stratified by AA subgroup (Table 3 ). Compared to those in the lowest NSC tertile, SEAA participants in the highest NSC tertile were more likely to report high cholesterol screening (AOR = 3.13, 95%CI:1.24–7.90), while a higher likelihood of depression screening was observed among EAA participants in the medium NSC tertile (AOR = 3.05, 95%CI:1.13–8.23) and SAA participants in the highest NSC tertile NSC (AOR = 2.42, 95%CI: 1.33–4.41).
Table 3.
Adjusted1 Multivariable regression models of Neighborhood Social Cohesion score tertiles and recent check-up (within the last year) for different chronic diseases, n = 1508.
| Preventative behavior (recent check-up) | Neighborhood social Cohesion2 | Total sample, n = 1394 OR (95%CI) |
East Asian3, n = 401 OR (95%CI) |
South Asian4, n = 630 OR (95%CI) |
Southeast Asian5, n = 360 OR (95%CI) |
|---|---|---|---|---|---|
| Cholesterol | Low | Ref | Ref | Ref | Ref |
| Medium | 1.20 (0.87–1.67) | 1.26 (0.66–2.42) | 0.83 (0.48–1.44) | 1.51 (0.79–2.89) | |
| High | 1.95 (1.36–2.80) | 1.66 (0.85–3.23) | 1.57 (0.90–2.76) | 3.13 (1.24–7.90) | |
| Diabetes/blood sugar | Low | Ref | Ref | Ref | Ref |
| Medium | 1.19 (0.86–1.66) | 1.26 (0.65–2.45) | 0.80 (0.46–1.40) | 1.43 (0.75–2.73) | |
| High | 1.95 (1.36–2.81) | 1.38 (0.70–2.72) | 1.60 (0.90–2.85) | 2.32 (0.96–5.60) | |
| Blood pressure | Low | Ref | Ref | Ref | Ref |
| Medium | 1.25 (0.89–1.77) | 1.10 (0.54–2.24) | 0.83 (0.46–1.50) | 1.51 (0.80–2.87) | |
| High | 1.86 (1.26–2.74) | 1.58 (0.75–3.31) | 1.26 (0.69–2.32) | 2.20 (0.89–5.41) | |
| Depression | Low | Ref | Ref | Ref | Ref |
| Medium | 1.53 (0.99–2.36) | 3.05 (1.13–8.23) | 1.17 (0.62–2.20) | 1.17 (0.51–2.66) | |
| High | 2.37 (1.54–3.65) | 2.30 (0.84–6.29) | 2.42 (1.33–4.41) | 1.35 (0.46–3.92) |
Discrimination, sex, age, percent of time lived in US, English fluency, education.
Low: 4.0–11.9, medium: 12.0–14.9, high: 15.0–16.0.
East Asian: Chinese, Korean, Japanese, Tibetan - Himalayan.
South Asian: Asian Indian, Bangladeshi, Pakistani, Sri Lankan, Nepali - Himalayan, Indo-Caribbean.
Southeast Asian: Filipino, Vietnamese, Cambodian, Indonesian, Thai.
4. Discussion
This study sought to evaluate the association between NSC and recent screening for diabetes, hypertension, high cholesterol, and depression among AA ethnic subgroups. Overall, higher NSC was associated with higher odds of recent screening for all chronic health conditions in the full sample, although findings varied by ethnic group. However, there were a number of key differences when NSC data was analyzed in one-unit increases versus in tertiles. These identified associations provide some support to the theorized mechanisms behind the relationship between NSC and preventive healthcare use established by Kim and Kawachi (2017). However, our findings also suggest that while the protective effect of some chronic disease prevention behaviors may be significant with marginal (one-unit) increases in NSC for some conditions, for others these effects may only be meaningful with significant (Low to High tertile) NSC increases.
Compared to the blood pressure and cholesterol screening prevalence among AAs observed by Collins et al., the proportion of participants who screened for hypertension in the last year was relatively consistent (72.9% vs. 74%), while a significantly greater percent of participants had recently screened for high cholesterol (65.4% vs. 49%) (Collins et al., 2002). With respect to diabetes, Tung et al. found that 47.1% of AA adults had received a recommended diabetes screening, while 65.9% of participants in the current study noted recently having been screened for diabetes (Tung et al., 2017). Although past studies have examined depression prevalence among AAs, there is a lack of prior research on prevalence of community-wide screening rates (Kim et al., 2015). However, the low rates of recent depression screening across the AA community support past research highlighting the low proportion of AAs mentioning depression symptoms to their doctors (2% vs. 13% national average) (Office of the Surgeon General, et al., 2001).
Trends in the NSC and cholesterol screening outcome was a significant finding in this study, suggesting interventions targeting social cohesion at the community level may be a potential way to bolster cholesterol screening rates in different AA communities. Given that past studies on NSC in AA settings have not studied cholesterol levels or cholesterol screening, the generalizability of these observations are unclear (Dong and Bergren, 2017; Lagisetty et al., 2016). However, one study among US adults and children noted lack of knowledge about cholesterol-CVD links was a salient barrier in screening – barriers which may be mitigated by improved social support and community knowledge that are potentially catalyzed by socially supportive neighborhood environments (Deskins et al., 2006). Thus one explanation for these findings that is that knowledge, resource, or social barriers among AAs related to cholesterol screening may be particularly addressable through neighborhood-level relationships and social cohesion.
A one-unit increase in NSC was associated with statistically significant increased odds of screening for diabetes among SAAs, but not other AA subgroups. The statistically significant association with diabetes screening did not remain when NSC was examined by tertiles. The observed association may be due to the high existing prevalence of type 2 diabetes among SAAs, thus SAAs may have access to more community level social or knowledge resources related to diabetes compared to other AA groups (Kim and Kawachi, 2017; Nguyen et al., 2015). However, past research has observed mixed or no associations in the relationship between NSC and diabetes among SAAs, or in the relationship between neighborhood factors and diabetes outcomes in general (Lagisetty et al., 2016; Smalls et al., 2015). Moreover, similar to SAAs, Filipino Americans display significantly higher rates of diabetes compared to other Asian subpopulations; however, due to the relatively small sample of Filipino American participants (n = 64, or 17.6% of the SEAA sample), it is unclear whether similar dynamics between NSC and diabetes screening are present in the community, or how this may have affected the overall SEAA trends (Choi et al., 2013). Nonetheless, it is important to consider that the nature of NSC and its impact on diabetes screening may be different from other health screenings and vary across communities, even when diabetes prevalence is high across certain communities.
The null association between hypertension screening and NSC in part supports some of the mixed findings observed in past studies on hypertension prevention behaviors. Lagisetty et al., for instance, similarly found no association between NSC and hypertension prevalence among SAAs (Lagisetty et al., 2016). Another study observed no association between increased NSC and odds of medication management of hypertension, although NSC was associated with the odds of measuring blood pressure at home (Schmitz et al., 2011). One possible reason for the observed null finding is the routine nature of blood pressure screenings during regular physical examinations (supported by the fact that 72.9% of participants had recently been screened for hypertension, the highest proportion among the studied health screenings), whereas screening for other chronic diseases may be less routine or aimed largely towards at-risk individuals (such as targeted diabetes screening for overweight or obese individuals). This higher baseline prevalence of hypertension screening may have limited the potential mediating effect that factors such as NSC had in further improving screening rates. Likewise, the cost and effort required for hypertension screening is minimal in comparison to diabetes or cholesterol screening, which often requires drawing blood or fasting on the part of the patient, and may be widely available in both clinical and non-clinical settings, such as pharmacies or faith-based organizations (Snella et al., 2006; Yi et al., 2019).
Recent depression screening was largely not found to be associated with NSC (except among SAAs). Mental health remains highly stigmatized in many AA settings, and the underutilization of mental health services in the community has been linked to a perceived lack of support at the familial and community level to seek medical attention for mental health concerns, as well as the structural deficiencies in culturally appropriate services (Augsberger et al., 2015). Such barriers may be limiting the potential of a socially cohesive environment to catalyze higher rates of depression screening in AA settings. However, the positive association between NSC and depression screening observed among SAA participants may suggest these interpersonal and community levels barriers to mental health screening support are not generalizable to all AA populations, and that improved NSC may still catalyze greater mental health screening in select groups.
The study has some limitations. First, the study relied on participant recall of specific screening behaviors, which is subject to recall bias. For instance, the PHQ depression screening instrument is being employed in routine entry paperwork in some healthcare practices, which may underestimate true depression screening rates if participants were not aware of these procedures (Savoy and O'Gurek, 2016). Further research using screening data from health care practices can help to support the validity of the current study's findings. Likewise, although the NSC tool displayed high internal reliability among study participants (α = 0.87), the original instrument was designed for a majority white US population, thus survey items may not completely reflect the unique nature of NSC among AAs (Sampson et al., 1997). A sensitivity analysis was conducted among participants with and without NSC data, which revealed that although accultration related factors such as English fluency and years lived in the US did not differ between the two groups, differences in percieved discrimination were observed. Similarly, other social and neighborhood level factors (such as the neighborhood built environment or social networks), as well as the underlying mechanisms between the relationship between NSC and preventive healthcare use were not examined in the current study.
While the study presents a diverse sample of different AA subgroups that are often not reflected in past research on AAs, the sample population was primarily low-income, first-generation Asian immigrants, which tend to exhibit disproportionately lower preventive healthcare use compared to US-born AAs and the general population (Ye et al., 2012; Centers for Disease Control and Prevention, 2018). In NYC, AAs are more likely to have no health insurance (10% AA average but as high 17% among Korean Americans vs. the 9% city average), which may also be a barrier to preventive healthcare use (New York City Department of Health and Mental Hygiene, 2018). Likewise, we were not able to adjust by income due to significant missing data. Further research may explore NSC trends in high-income or second-generation AA communities, which may display unique social or behavioral profiles relevant to NSC related dynamics (Ali et al., 2020).
The rapidly evolving COVID-19 pandemic in 2020 has shed further light on the need to critically consider the role of and dynamics between neighbors during health crises. Specifically, the impact many of the COVID-19 behavioral prevention measures (such as social distancing) on the understanding and experience of social cohesion in neighborhoods is deserving of critical examination, particularly on its subsequent impact on preventive healthcare use and other health behaviors, and thus a re-assessment of NSC trends post-COVID-19 is warranted.
5. Conclusion
Given the pressing chronic disease burden and low healthcare utilization concerns among AAs, coupled with the significance of the neighborhood environment and support systems in the community, the lens of NSC provides a uniquely powerful approach to better understand and address the needs of AAs. The associations observed between NSC and preventive healthcare use suggest that neighborhood level interventions to enhance community capacity and social support for preventive healthcare use may have the potential improve low chronic disease screening rates.
While low income or first generation AAs in settings such as NYC may face multiple barriers to preventive healthcare use, incorporating a community-based approach that enhances resource and knowledge capacity, builds on pre-existing community ties, and leverages networks of social support has the potential to strongly complement preventive screening interventions that focus on individual level factors. Given the variability in the trends observed across different AA subgroups, findings also emphasize the need to disaggregate AA health research (including disaggregating beyond the three categorizes used in this study) and target interventions based on the specific health trends in each subgroup. Likewise, this study provides crucial evidence needed to support further, in-depth, mixed method exploration on social and community level barriers and facilitators in preventive healthcare use in AA communities, and the specific mechanisms behind the role of NSC in facilitating higher screening rates.
Acknowledgments
This study is supported by the National Institutes of Health National Institute on Minority Health and Health Disparities grant U54MD000538; Centers for Disease Control and Prevention Grant U48DP001904; National Institutes of Health National Institute of Diabetes and Digestive Kidney Diseases Grants R18DK110740, R01DK11048, P30 DK111022; and National Institutes of Health National Center for Advancing Translational Science Grant UL1TR001445. The views expressed are those of the authors and do not necessarily represent the official position of the funding organizations.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2020.106298.
Appendix A. Supplementary data
Adapted diagram of theorized mechanisms of relationship between NSC and preventive healthcare use identified by Kim & Kawachi (2017)
References
- Ali Shahmir H., DiClemente Ralph J., Parekh Niyati. Changing the landscape of South Asian migrant health research by advancing second-generation immigrant health needs. Transl. Behav. Med. 2020;Online ahead of print:ibaa084. doi: 10.1093/tbm/ibaa084. [DOI] [PubMed] [Google Scholar]
- American Health Association News Ethnicity a 'risk-enhancing' factor under new cholesterol guidelines. American Heart Association Web site. 2019. https://www.heart.org/en/news/2019/01/11/ethnicity-a-risk-enhancing-factor-under-new-cholesterol-guidelines Accessed January 13, 2020.
- Appel H.B., Huang B., Ai A.L., Lin C.J. Physical, behavioral, and mental health issues in Asian American women: results from the National Latino Asian American Study. J. Women’s Health. 2011;20(11):1703–1711. doi: 10.1089/jwh.2010.2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augsberger A., Yeung A., Dougher M., Hahm H.C. Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Serv. Res. 2015;15:542. doi: 10.1186/s12913-015-1191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Ambulatory Care Use and Physician office visits. 2018. https://www.cdc.gov/nchs/fastats/physician-visits.htm Accessed May 7, 2020.
- Chang E., Chan K.S. Variations in Asian Americans: how neighborhood concordance is associated with health care access and utilization. Am. J. Public Health. 2015;105(1):66–68. doi: 10.2105/AJPH.2014.302275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S.E., Liu M., Palaniappan L.P., Wang E.J., Wong N.D. Gender and ethnic differences in the prevalence of type 2 diabetes among Asian subgroups in California. J. Diabetes Complicat. 2013;27(5):429–435. doi: 10.1016/j.jdiacomp.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins K.S., Hughes D.L., Doty M.M., Ives B.L., Edwards J.N., Tenney K. Diverse communities, common concerns: assessing health care quality for minority Americans. Commonwealth Fund New York Web site. 2002. https://www.commonwealthfund.org/publications/fund-reports/2002/mar/diverse-communities-common-concerns-assessing-health-care
- Contreras C.A. Addressing cardiovascular health in Asian Americans and Pacific islanders: a background report. Asian Am Pac Isl J Health. 1999;7(2):95–145. [PubMed] [Google Scholar]
- Deskins S., Harris C.V., Bradlyn A.S. Preventive Care in Appalachia: use of the theory of planned behavior to identify barriers to participation in cholesterol screenings among west Virginians. J. Rural. Health. 2006;22(4):367–374. doi: 10.1111/j.1748-0361.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- Dong X., Bergren S.M. The associations and correlations between self-reported health and neighborhood cohesion and disorder in a community-dwelling U.S. Chinese population. Gerontologist. 2017;57(4):679–695. doi: 10.1093/geront/gnw050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey R.G., King C.V. Missing data in Likert ratings: a comparison of replacement methods. J. Gen. Psychol. 1998 Apr 1;125(2):175–191. doi: 10.1080/00221309809595542. [DOI] [PubMed] [Google Scholar]
- Hastings K.G., Jose P.O., Kapphahn K.I. Leading causes of death among Asian American subgroups (2003−2011) PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong S., Zhang W., Walton E. Neighborhoods and mental health: exploring ethnic density, poverty, and social cohesion among Asian Americans and Latinos. Soc. Sci. Med. 2014;111:117–124. doi: 10.1016/j.socscimed.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose P.O., Frank A.T., Kapphahn K.I. Cardiovascular disease mortality in Asian Americans. J. Am. Coll. Cardiol. 2014;64(23):2486–2494. doi: 10.1016/j.jacc.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung M., Kwon S.C., Edens N., Northridge M.E., Trinh-Shevrin C., Yi S.S. Oral health care receipt and self-rated Oral health for diverse Asian American subgroups in New York City. Am. J. Public Health. 2017;107(S1):S94–S96. doi: 10.2105/AJPH.2017.303661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.S., Kawachi I. Perceived neighborhood social cohesion and preventive healthcare use. Am. J. Prev. Med. 2017;53(2):e35–e40. doi: 10.1016/j.amepre.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim W., Keefe R.H. Barriers to healthcare among Asian Americans. Soc Work Public Health. 2010;25(3–4):286–295. doi: 10.1080/19371910903240704. [DOI] [PubMed] [Google Scholar]
- Kim H.J., Park E., Storr C.L., Tran K., Juon H.-S. Depression among Asian-American adults in the community: systematic review and meta-analysis. PLoS One. 2015;10(6):e0127760. doi: 10.1371/journal.pone.0127760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagisetty P.A., Wen M., Choi H., Heisler M., Kanaya A.M., Kandula N.R. Neighborhood social cohesion and prevalence of hypertension and diabetes in a south Asian population. J. Immigr. Minor. Health. 2016;18(6):1309–1316. doi: 10.1007/s10903-015-0308-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L., Hawe P. Ecological perspectives in health research. J. Epidemiol. Community Health. 2005;59(1):6–14. doi: 10.1136/jech.2003.018044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra Supriya, Wyatt Laura C., Wong Jennifer A. Determinants of Depression Risk among Three Asian American Subgroups in New York City. Ethnicity & Disease. 2020;30(4):553–562. doi: 10.18865/ed.30.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene Health Disparities among Asian New Yorkers. 2018. https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief100.pdf Accessed May 7, 2020.
- Ngoc Nguyen T.-U., Tanjasiri S.P., Kagawa-Singer M., Tran J.H., Foo M.A. Community health navigators for breast- and cervical-cancer screening among Cambodian and Laotian women: intervention strategies and relationship-building processes. Health Promot. Pract. 2008;9(4):356–367. doi: 10.1177/1524839906290251. [DOI] [PubMed] [Google Scholar]
- Nguyen T.H., Nguyen T.-N., Fischer T., Ha W., Tran T.V. Type 2 diabetes among Asian Americans: prevalence and prevention. World J. Diabetes. 2015;6(4):543–547. doi: 10.4239/wjd.v6.i4.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General,, Center for Mental Health Services, National Institute of Mental Health . Mental Health Care for Asian Americans and Pacific Islanders. In: Substance Abuse and Mental Health Services Administration, editor. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Substance Abuse and Mental Health Services Administration; Rockville (MD): 2001. https://www.ncbi.nlm.nih.gov/books/NBK44245/ [PubMed] [Google Scholar]
- Park J.J., Humble S., Sommers B.D., Colditz G.A., Epstein A.M., Koh H.K. Health Insurance for Asian Americans, native Hawaiians, and Pacific islanders under the affordable care act. JAMA Intern. Med. 2018;178(8):1128–1129. doi: 10.1001/jamainternmed.2018.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center The Rise of Asian Americans. Pew Research Center Web site. 2012. https://www.pewsocialtrends.org/2012/06/19/the-rise-of-asian-americans/ Accessed January 14, 2020.
- R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2020. http://www.R-project.org/
- Saleem F.T., Busby D.R., Lambert S.F. Neighborhood social processes as moderators between racial discrimination and depressive symptoms for African American adolescents. J Community Psychol. 2018;46(6):747–761. [Google Scholar]
- Sampson R.J., Raudenbush S.W., Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Savoy M.L., O’Gurek D.T. Screening your adult patients for depression. Fam. Pract. Manag. 2016;23(2):16–20. [PubMed] [Google Scholar]
- Schmitz M.F., Giunta N., Parikh N.S., Chen K.K., Fahs M.C., Gallo W.T. The association between neighbourhood social cohesion and hypertension management strategies in older adults. Age Ageing. 2011;41(3):388–392. doi: 10.1093/ageing/afr163. [DOI] [PubMed] [Google Scholar]
- Smalls B.L., Gregory C.M., Zoller J.S., Egede L.E. Assessing the relationship between neighborhood factors and diabetes related health outcomes and self-care behaviors. BMC Health Serv. Res. 2015;15(1):445. doi: 10.1186/s12913-015-1086-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snella K.A., Canales A.E., Irons B.K. Pharmacy- and community-based screenings for diabetes and cardiovascular conditions in high-risk individuals. J. Am. Pharm. Assoc. 2006;46(3):370–377. doi: 10.1331/154434506777069598. [DOI] [PubMed] [Google Scholar]
- Tung E.L., Baig A.A., Huang E.S., Laiteerapong N., Chua K.-P. Racial and ethnic disparities in diabetes screening between Asian Americans and other adults: BRFSS 2012-2014. J. Gen. Intern. Med. 2017;32(4):423–429. doi: 10.1007/s11606-016-3913-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force Recommendation Topics. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics Accessed May 7, 2020.
- Ursua R.A., Aguilar D.E., Wyatt L.C. A community health worker intervention to improve management of hypertension among Filipino Americans in New York and New Jersey: a pilot study. Ethn. Dis. 2014;24(1):67–76. [PMC free article] [PubMed] [Google Scholar]
- Walton E. Making sense of Asian American ethnic neighborhoods: a typology and application to health. Sociol. Perspect. 2015;58(3):490–515. [Google Scholar]
- Weng S.S. Asset mapping for an Asian American community: informal and formal resources for community building. Psychosoc. Interv. 2016;25(1):55–62. [Google Scholar]
- Williams D.R., Yan Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J. Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Ye J., Rust G., Baltrus P., Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann. Epidemiol. 2009;19(10):718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye J., Mack D., Fry-Johnson Y., Parker K. Health care access and utilization among US-born and foreign-born Asian Americans. J. Immigr. Minor. Health. 2012;14(5):731–737. doi: 10.1007/s10903-011-9543-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi S.S., Trinh-Shevrin C., Yen I.H., Kwon S.C. Racial/ethnic differences in associations between neighborhood social cohesion and meeting physical activity guidelines, United States, 2013-2014. Prev. Chronic Dis. 2016;13 doi: 10.5888/pcd13.160261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi S.S., Wyatt L.C., Patel S. A faith-based intervention to reduce blood pressure in underserved metropolitan New York immigrant communities. Prev. Chronic Dis. 2019;16 doi: 10.5888/pcd16.180618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi S.S., Kanaya A.M., Wen M. Associations of neighborhood factors and activity behaviors: the mediators of atherosclerosis in south Asians living in America (MASALA) study. J. Immigr. Minor. Health. 2020 doi: 10.1007/s10903-020-01021-6. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Adapted diagram of theorized mechanisms of relationship between NSC and preventive healthcare use identified by Kim & Kawachi (2017)