Abstract
Introduction:
The present study examined the underlying role of anxiety sensitivity in the association between effortful control and anxiety and depressive symptoms in a sample of clinically anxious children. It was hypothesized that effortful control would exert an indirect effect through anxiety sensitivity in relation to child anxiety and depressive symptoms.
Method:
Clinically anxious children (N = 105; Mage = 10.09 years, SD = 1.22; 56.7% female; 61% ethnic minority) and their mothers completed a diagnostic interview and a battery of questionnaires that included self- and mother-ratings of child effortful control, anxiety sensitivity, and anxiety and depressive symptoms.
Results:
The indirect effect of effortful control via anxiety sensitivity on child anxiety and depressive symptoms was significant across child- and mother-completed measures.
Discussion:
Among clinically anxious youth, greater effortful control was related to lower anxiety sensitivity, which was related to lower anxiety and depressive symptoms. Future work should evaluate whether targeting effortful control leads to clinically meaningful reductions in anxiety sensitivity and child anxiety and depressive symptoms.
Keywords: effortful control, anxiety sensitivity, anxiety, depression, children
1. Introduction
Anxiety and depressive disorders in children are highly prevalent and represent a significant social and public health concern (Costello, Egger, Copeland, Erkanli, & Angold, 2011; Merikangas et al., 2010). Rates of comorbidity are also high; 10–15% of youth with a primary anxiety disorder also meet criteria for a depressive disorder (Axelson & Birmaher, 2001; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Cummings, Caporino, & Kendall, 2014) and 25–50% of youth with depressive disorders have a concurrent anxiety disorder (Axelson & Birmaher, 2001). The presence of comorbid depressive symptoms among youth with an anxiety disorder is associated with greater functional impairment, including lower family functioning, more severe anxiety, and lower ratings of global functioning (O’Neil, Podell, Benjamin, & Kendall, 2010). Comorbid anxiety and depression are related to higher rates of treatment resistance than either disorder alone, increased suicide attempts, marked impairment, less favorable treatment response, and greater utilization of mental health services (Birmaher et al., 1996; Garber & Weersing, 2010). These findings underscore a need for increased understanding of risk and protective mechanisms associated with greater symptom severity among clinically anxious youth with depressive symptomology (Kendall et al., 2016).
Effortful control, a temperamental trait defined as the ability to utilize executive functions to inhibit an impulsive reaction in favor of an adaptive response (Lonigan & Vasey, 2009; Rothbart & Bates, 2006), is one clinically-relevant factor that is associated with anxiety and depressive symptoms among youth. Effortful control is comprised of three components (Muris & Ollendick, 2005): attentional control, which reflects the capacity to focus attention as well as to shift attention when desired (Muris, van der Pennen, Sigmond, & Mayer, 2008); inhibitory control, which refers to the ability to monitor and control conscious thought as well as to inhibit or delay a prepotent response (Carlson & Moses, 2001); and activation control, which refers to the capacity to perform an action when there is a strong tendency to avoid it (Snyder et al., 2015).
Greater effortful control (and its subcomponents) have been associated with lower psychopathology in clinical and community samples (Raines et al., 2019; White, McDermott, Degnan, Henderson, & Fox, 2011). Conversely, deficits in effortful control are positively associated with mental health difficulties (Eisenberg, Hofer, & Vaughan, 2007; Niditch & Varela, 2018), including anxiety and depression (e.g., Lonigan & Vasey, 2009; Muris & Ollendick, 2005; Niditch & Varela, 2018). In a longitudinal investigation of effortful control and depression in middle childhood, children who were rated lower (vs. higher) on effortful control at baseline showed a significant increase in depressive symptoms over time (Kotelnikova, Mackrell, Jordan, & Hayden, 2015). Scheper and colleagues (2017) found that clinic-referred children ages 3–7 years exhibited less effortful control than healthy controls, and that effortful control was negatively associated with internalizing problems (Scheper et al., 2017). A separate investigation reported that lower effortful control was associated with greater child anxiety symptoms, and that effortful control in the preschool years mediated the relation between infant behavioral inhibition and anxiety symptoms in early childhood (Niditch & Varela, 2018). Lower effortful control was also related to greater threat perceptions, which in turn, were related to more severe anxiety among clinically anxious children (Raines et al., 2019). Collectively, these findings align with theory suggesting that children’s ability to regulate ‘top-down’ attentional capacities, generally, and effortful control, specifically, is inversely related to anxious psychopathology (Muris & Ollendick, 2005).
Although it is not fully understood exactly why greater effortful control is associated with lower anxiety psychopathology, one possibility supported by theory is that the enhanced attentional capacities stemming from greater effortful control (Eysenck, Derakshan, Santos, & Calvo, 2007) may allow anxious children to ‘slow down’ and interpret internal experiences (e.g., somatic sensations) more objectively. More specifically, clinically anxious children with greater effortful control may be better equipped to accurately interpret interoceptive perturbation, which in turn, may contribute to lower anxiety and depressive symptoms (Waszczuk, Brown, Eley, & Lester, 2015). Unfortunately, despite theoretical support, whether clinically anxious children’s interpretations of interoceptive stimuli are indeed a putative mechanism linking low effortful control and anxiety and depressive symptoms has yet to be examined.
One transdiagnostic mechanism that may underlie the association between effortful control and both anxiety and depressive symptoms is anxiety sensitivity, defined as the fear of anxiety-related sensations due to the belief that these sensations signal catastrophic consequences (Chorpita & Lilienfeld, 1999; Silverman, Fleisig, Rabian, & Peterson, 1991). For example, a child experiencing high levels of anxiety sensitivity may interpret an anxiety-related increase in his heart rate as a serious medical concern, which may amplify preexisting levels of anxiety (Reiss, 1991), Although originally conceptualized as a risk factor for anxiety disorders, extensive work has reported significant associations between anxiety sensitivity and anxiety (e.g., Capron, Allan, Ialongo, Leen-Feldner, & Schmidt, 2015; Lambert et al., 2004; Varela, Weems, Berman, Hensley, & de Bernal, 2007) and depressive symptoms (e.g., Grant, Beck, & Davila, 2007; Tull & Gratz, 2008; Viana & Rabian, 2009; Weems, Hammond-Laurence, Silverman, & Ferguson, 1997). Yet, the underlying role of anxiety sensitivity in the associations between effortful control and both anxiety and depressive symptoms in youth has not been examined.
The present investigation examined the indirect of effect of effortful control, through anxiety sensitivity, on child anxiety and depressive symptoms in a sample of children with anxiety disorders. We hypothesized that effortful control would be inversely related to anxiety sensitivity and child anxiety and depressive symptoms (Muris & Ollendick, 2005). We also hypothesized that anxiety sensitivity would partially explain the association between effortful control and child anxiety and depressive symptoms. Specifically, we expected that effortful control would be negatively associated with anxiety sensitivity, which in turn, would be positively associated with anxiety and depressive symptoms (i.e., an indirect association between effortful control and anxiety and depressive symptoms).
2. Method
2.1. Participants
The present study involved secondary analysis of data from a federally-funded clinical trial (NCT02095340) investigating the role of maternal interpretation biases on child anxiety and related responses. Families were included if (a) the child was between the ages of 8-12 years and had a primary anxiety disorder (by either mother or child report), (b) the mother reported levels of anxiety within the clinical range during clinical interview or on the Depression, Anxiety, and Stress Scales (DASS; Lovibond & Lovibond, 1995), and (c) the child currently lived with the mother. Children were excluded based on the following reasons: (a) physical disability impairing ability to use a computer, (b) borderline or extremely low intellectual functioning, (c) below average reading comprehension, (d) concurrent primary diagnosis of any non-anxiety disorder, (e) currently receiving psychological or pharmacological treatment for anxiety, (f) danger to self/others, and (g) non-English speaking child/parent. Because the original trial involved evaluating the effect of a computerized intervention targeting maternal cognitions, mothers were excluded if they were currently involved in cognitive behavioral therapy for anxiety (which explicitly targets cognitions) and/or if they had changes in their pharmacological treatment (for anxiety) in within 12 weeks prior to enrollment. The original study focused on mothers as 69-75% of caregivers are women, and female caregivers spend as much as 50% more time providing care to their children than male caregivers (U.S. Census Bureau, 2015). Moreover, given their higher likelihood of exhibiting interpretation biases, the original study focused on clinically anxious mother in particular.
The final sample was comprised of 105 children with anxiety disorders between 8 to 12 years of age (N = 105; M = 10.07 years, SD = 1.22; 57% female) and their clinically anxious mothers (M = 39.35 years, SD = 7.05; range = 26 – 61 years; 67% married). In terms of race and ethnicity, mothers identified as follows: 51.4% White, 29.5% Hispanic, 14.3% African American, 2.9% mixed ethnicity, and 1.9% Asian American. Children identified as follows: 39.0% White, 28.6% Hispanic, 16.2% mixed ethnicity, 14.3% African American, and 1.9% Asian American. Twenty-three percent of families reported an annual household of < $40,000, 16% between $40,000-$69,999, 22% between $70,000-$99,999, 36% over $100,000, and 2.9% did not report their income. Three percent of mothers had less than a high school education, 6.7% had a high school diploma or GED, 17.3% had some college education, 5.4% had a 2-year college degree, 34.6% had a 4-year college degree, 3.8% had completed some graduate level courses, 13.5% had a master degree, and 5.8% had a doctoral or professional degree. Fifty percent of mothers worked full time.
Children met Diagnostic and Statistical Manual of Mental Disorders (5th ed.; American Psychiatric Association, 2013) criteria for at least one anxiety disorder diagnosis based on results from semi-structured interviews conducted (separately) with both the child and the mother. generalized anxiety disorder was the most common anxiety disorder (46.7%), followed by social anxiety disorder (27.6%), specific phobias (16.2%), separation anxiety disorder (7.6%), and other anxiety disorders (1.9%). Most of the sample (69.5%) had comorbid diagnoses, the most common being specific phobias (14.3%), attention deficit/hyperactivity disorder (12.4%), generalized anxiety disorder (8.6%), oppositional defiant disorder (7.6%), current major depressive disorder (7.6%), separation anxiety disorder (5.7%), and social anxiety disorder (5.7%).
2.2. Procedure
All procedures were approved by the Institutional Review Board. Families were recruited to participate in a larger, two-session study on mother and child anxiety through local advertisements, child-oriented events, and flyers. To ensure that an adequate number of participants had high anxiety, recruitment materials specifically encouraged families experiencing difficulties with child anxiety to participate. Interested mothers initially contacted or were contacted by study personnel via telephone or email. A description of the study was provided and a brief screen was conducted to assess for child exclusionary criteria. An initial three-hour session was scheduled with eligible families. Data from the second session were not utilized in the present investigation.
Upon arrival for the first session, informed consent from mothers and informed assent from children were obtained. After eligibility was confirmed, clinical interviews were conducted with mothers and children (separately) by graduate students under the direct supervision of a doctoral-level clinician. After the clinical interview, mothers and children completed (separately) a battery of questionnaires. Upon completion of the second session, the mother and child were fully debriefed. Information regarding the results of the diagnostic evaluation, recommended evidence-based treatments, and contact information of local mental health providers were made available to families. Families received $50 per session for their participation, and children were also able to choose a small toy after each session.
2.3. Measures
2.3.1. MINI International Neuropsychiatric Interview for Children and Adolescents (MINI-Kid; Sheehan, 1998).
The MINI-Kid is a structured diagnostic interview for children from 6 to 17 years old based on DSM-5 psychiatric disorders. Twenty-four DSM-5 diagnoses are assessed with discrete modules. If module’s initial screening item(s) is endorsed, the assessor proceeds through additional questions to determine diagnostic criteria. Separate child and parent (about the child) interviews were conducted. Mother and child interviews were conducted separately, in adjacent rooms. MINI-KID interviews were conducted by either a board-certified and licensed clinical child and adolescent psychologist, or an advanced graduate student under supervision. Graduate student assessors were trained to use the MINI-KID by observing videotaped samples of interviews conducted by the principal investigator; assessors were required to meet perfect inter-rater reliability with the PI on three interviews before conducting two independent interviews while being shadowed by the PI (i.e., live supervision). All MINI-KID interviews were videotaped and all diagnoses were reviewed during supervision sessions with assessors. Fifteen percent of videotaped interviews were reviewed for interrater reliability; as in past work using fully structured interview formats (Zvolensky et al., 2019), no instances of diagnostic disagreement were found. The child’s final primary diagnosis was based on the clinical interview with the mother; if the mother did not report a primary diagnosis, but the child did, then the child’s final primary diagnosis was the self-reported diagnosis. Nearly half (48.6%) of children received a primary anxiety disorder diagnoses based on diagnostic agreement across both mother and child interviews; the remaining children received a primary anxiety disorder diagnosis based on the interview with the mother (40%) or the child (11.4%).
2.3.2. Child Anxiety Sensitivity Index, Child and Parent Report (CASI and CASI-P; Silverman et al., 1991).
The CASI is an 18-item self-report questionnaire that assesses the fear of anxiety-related sensations in children and adolescents. Participants are asked to rate the extent to which they experience fearful reactions to normal anxiety responses on a 3-point scale (1 = none, 2 = some, 3 = a lot). Sample items include “It scares me when I am nauseous” and “When I can’t keep my mind on my schoolwork, I worry that I might be going crazy.” A total score is computed by summing the responses to all items with a possible range of scores from 18 to 54. Silverman et al. (1991) reported an alpha coefficient and test-retest reliability estimates of 0.87 and 0.76, respectively, in a nonclinical sample, and 0.87 and 0.79, respectively, in a clinical sample. In this study, the internal consistency of the CASI was excellent (α = 0.90).
The parent version of the CASI (CASI-P; Weems, Taylor, Marks, & Varela, 2010), was used to assess parental report of their child’s anxiety sensitivity. The CASI-P format and items are identical to the CASI, except that the item stems are changed from “I” to “my child” (e.g., “It scares my child when she/he feels shaky”). This strategy has been used in past research on reports of childhood fears and trait anxiety (see Pina et al. 2001) and facilitates the development of non-arbitrary metrics (see Blanton & Jaccard 2006) by utilizing the same metric as used with the CASI (i.e., levels reported by the child can be directly compared with those reported by the parent). In this study, the internal consistency of the CASI-P was excellent (α = 0.88).
2.3.3. Early Adolescent Temperament Questionnaire, Revised Short Form, Child and Parent Report (EATQ-RS; Ellis & Rothbart, 2001).
The EATQ-RS is a 65-item, child-completed questionnaire designed to assess temperament traits in late childhood through late adolescence. It contains 11 temperament subscales (activation control, activity level, affiliation, attention, fear, frustration, high intensity pleasure, inhibitory control, perceptual sensitivity, pleasure sensitivity, and shyness) and two behavioral scales (aggression and depressive mood). Items are rated on a 5-point Likert scale, ranging from 1 (almost never true) to 5 (almost always true). The inhibitory control subscale, reflecting the capacity to plan and to suppress inappropriate responses (e.g., “when someone tells me to stop doing something, it is easy for me to stop”); attentional control subscale, reflecting the capacity to focus attention as well as to shift attention when desired (e.g., “I pay close attention when someone tells me how to do something”); and activation control subscale, reflecting the ability to begin and complete tasks when there is a strong tendency to avoid it (e.g., “If I have a hard assignment to do, I get started right away”) were averaged to create an effortful control total score, which is consistent with previous work (α = .72; Morris & Age, 2009).
Parents completed The Early Adolescent Temperament Questionnaire – Revised Parent Report (EATQ-P), a 62-item questionnaire designed to assess temperament traits in late childhood through adolescence. Items are rated on a 5-point Likert scale identical to that of the self-report form (EATQ-P). The inhibitory control, attentional control, and activation control subscales were averaged to create an effortful control total score (α = 0.87).
2.3.4. Revised Child Anxiety and Depression Scale, Child and Parent Report (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000).
The RCADS is a self-report measure based on the Spence Children’s Anxiety Scale (Spence, 1998) and designed to assess DSM-IV-TR (American Psychiatric Association, 2000) separation anxiety disorder, social anxiety disorder, panic disorder, obsessive compulsive disorder, generalized anxiety disorder, and major depressive disorder symptoms in children. The child is asked to respond to 47 questions on a Likert scale (0 = never to 3 = always) regarding the extent to which he/she agrees with statements indicative of anxiety (e.g., “I worry that bad things will happen to me”) and depression (e.g., “nothing is much fun anymore”). Studies show that the RCADS has good internal consistency in both clinical and community samples of youth (Chorpita et al., 2000), adequate convergent validity with established measures of anxiety and depression, and with the diagnostic syndromes it was purported to assess (Chorpita, Moffitt, & Gray, 2005). The RCADS total anxiety score (RCADS-A; α = 0.94) and total depression score (RCADS-D; α =0 .84) were used in the current study as an index of anxiety and depressive symptom severity.
The parent version of the RCADS (i.e., RCADS-P; Chorpita et al., 2000) was identical to the child version, except that items/descriptions are rephrased from the parents’ perspective. Sample items include “my child is scared to take a test,” “my child feels worthless,” and “when my child has a problem, his/her stomach feels funny.” The RCADS-P total anxiety score (RCADS-P-A; α = 0.90) and total depression score (RCADS-P-D; α = 0.83) were used in the current study as an index of anxiety and depressive symptom severity.
2.4. Data Analytic Plan
First, variables’ distributions were examined to evaluate patterns of skewness and kurtosis. The data was also examined for the presence of potential univariate and/or multivariate outliers. Second, correlational analyses were used to examine associations among study variables and to identify possible sociodemographic covariates. Third, the PROCESS macro for SPSS (Hayes, 2018) was used to examine the indirect of effortful control through anxiety sensitivity on child anxiety and depressive symptoms (see Figure 1).
Figure 1.
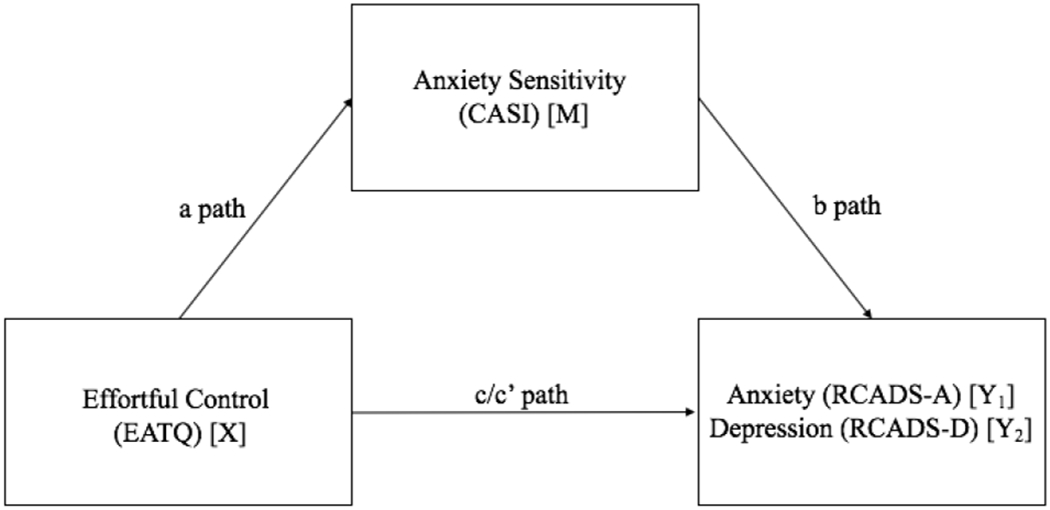
Theoretical Model: Child anxiety sensitivity as a potential mediator between effortful control and anxiety and depressive symptom severity. A significant indirect effect (a*b) suggests potential mediation.
A total of four separate models were tested: two models with child-completed measures (predicting anxiety and depressive symptoms, respectively) and two models with mother-completed measures (predicting anxiety and depressive symptoms, respectively). Significant indirect effects were determined by examining the 95% bootstrapped confidence intervals (10,000 re-samples) for the indirect effect in each regression. A bootstrap-confidence interval that does not include zero provides evidence of a significant indirect effect (Preacher & Hayes, 2008). Additionally, following recent recommendations (Wen & Fan, 2015), the ratio of the indirect effect to the total effect (i.e., PM, or mediation ratio; Ditlevsen, Christensen, Lynch, Damsgaard, & Keiding, 2005) was reported as a measure of effect size for significant indirect effects. Finally, to test for model specificity, reverese models (reversing the independent variable and mediating variable) were also conducted.
3. Results
3.1. Preliminary analyses
Means, standard deviations, and correlations among all study variables are presented in Table 1. All variables demonstrated acceptable levels of skewness and kurtosis. Child and parent ratings of child effortful control were positively associated. Child ratings of effortful control were negatively associated with child ratings of anxiety sensitivity, anxiety, and depressive symptoms. Similarly, parent ratings of child effortful control were negatively associated with parent ratings of child anxiety sensitivity, anxiety, and depressive symptoms. Child ratings of anxiety sensitivity, anxiety, and depressive symptoms were positively associated. Parent ratings of child anxiety sensitivity, anxiety, and depressive symptoms were also positively associated. Given the lack of cross-informant associations among the dependent variables (with the exception of child and parent ratings of child depression symptoms, which were positively correlated; see Table 1), within-informant (vs. cross-informant) mediation analyses were conducted, resulting in four mediation models.1
Table 1.
Correlations and descriptive statistics (N = 105)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | ||||||||||
| 2. Gender | .13 | -- | |||||||||
| 3. Ethnicity | .05 | .12 | -- | ||||||||
| 4. Effortful Control-C | .12 | −.00 | .12 | -- | |||||||
| 5. Effortful Control-P | .15 | .03 | −.00 | .38** | -- | ||||||
| 6. Anxiety Sensitivity-C | −.11 | .16 | .05 | −.45** | .01 | -- | |||||
| 7. Anxiety Sensitivity-P | .16 | .03 | .12 | −.10 | −.30* | .13 | -- | ||||
| 8. Anxiety-C | −.05 | .15 | −.03 | −.51** | −.01 | .80** | .14 | -- | |||
| 9. Depression-C | −.14 | .15 | .06 | −.50** | −.13 | .63** | .10 | .73** | -- | ||
| 10. Anxiety-P | −.07 | .19 | .19 | −.01 | −.34** | .14 | .62** | .13 | .14 | -- | |
| 11. Depression-P | .06 | .12 | .06 | −.15 | −.46** | .04 | .35** | .05 | .29* | .46** | -- |
| Mean | 10.07 | 1.57 | -- | 3.50 | 3.07 | 28.07 | 30.64 | 29.05 | 6.25 | 31.20 | 5.99 |
| SD | 1.22 | .50 | .55 | .65 | 7.29 | 6.81 | 18.63 | 4.94 | 14.10 | 4.41 | |
| Minimum | 8 | -- | 2.07 | 1.61 | 18 | 19 | 2 | 0 | 1 | 0 | |
| Maximum | 12 | -- | 5.00 | 4.70 | 49 | 49 | 91 | 23 | 77 | 22 | |
Note.
Effortful Control = Early Adolescent Temperament Questionnaire – effortful control subscale; Anxiety Sensitivity = Childhood Anxiety Sensitivity Index (C = child report, P = parent report); Anxiety and Depression = Revised Children’s Anxiety and Depression Scale (A = anxiety total raw score, D = depression total raw score; C = child report, P = parent report). Gender: male =1 and female = 2.
p < .01
p < .001
3.2. Mediation Analyses: Tests of indirect effects
3.2.1. Child-reported Anxiety.
Results of indirect effects tests are presented in Table 2. The total effect model predicting RCADS-A was significant and accounted for 25.8% of variance (b = 17.14, SE = 2.86, p ≤ 0.001). There was a significant positive indirect effect of effortful control on RCADS-A via CASI (completely standardized point estimate = −0.32, SE = 0.06, BC 95% CI [−0.43, −0.21]). The ratio of the indirect effect to the total effect of effortful control on RCADS-A was 0.63 (PM = 0.63, SE = 0.10; BC 95% CI [0.44, 0.85]). The comparison model (reversing X and M) also yielded a significant indirect effect (completely standardized point estimate = 0.08, SE = 0.03, BC 95% CI [0.03, 0.17]).
Table 2.
Mediation Analyses (N = 105)
| Y | Model | β | SE | t | p | CI(l) | CI (u) |
|---|---|---|---|---|---|---|---|
| 1 | EFFORTFUL CONTROL-C → ANXIETY SENSITIVITY-C (a) | −5.88 | 1.17 | −5.05 | .000 | −8.19 | −3.57 |
| ANXIETY SENSITIVITY-C → ANXIETY-C (b) | 1.82 | 0.16 | 11.19 | .000 | 1.50 | 2.15 | |
| EFFORTFUL CONTROL-C → ANXIETY-C (c) | −17.14 | 2.86 | −5.98 | .000 | −22.82 | −11.46 | |
| EFFORTFUL CONTROL-C → ANXIETY-C (c’) | −6.41 | 2.15 | −2.98 | .004 | −10.68 | −2.14 | |
| EFFORTFUL CONTROL-C → ANXIETY SENSITIVITY- C → ANXIETY-C (ab) | −10.73 | 2.40 | -15.74 | -6.38 | |||
| 2 | EFFORTFUL CONTROL-C → ANXIETY SENSITIVITY-C (a) | −5.88 | 1.17 | −5.05 | .000 | −8.19 | −3.57 |
| ANXIETY SENSITIVITY-C → DEPRESSION-C (b) | 0.35 | .06 | 6.33 | .000 | 0.24 | 0.46 | |
| EFFORTFUL CONTROL-C → DEPRESSION-C (c) | −4.47 | 0 .76 | −5.86 | .000 | −5.98 | −2.96 | |
| EFFORTFUL CONTROL-C → DEPRESSION-C (c’) | −2.43 | 0.73 | −3.34 | .001 | −3.87 | −0.99 | |
| EFFORTFUL CONTROL-C → ANXIETY SENSITIVITY-C → DEPRESSION-C (ab) | −2.04 | 0.58 | −3.41 | −1.09 | |||
| 3 | EFFORTFUL CONTROL-P → ANXIETY SENSITIVITY-P (a) | −2.89 | 0.90 | −3.21 | .002 | −4.67 | −1.11 |
| ANXIETY SENSITIVITY-P → ANXIETY-P (b) | 1.17 | 0.17 | 7.09 | .000 | 0.84 | 1.50 | |
| EFFORTFUL CONTROL-P → ANXIETY-P (c) | −6.82 | 1.83 | −3.72 | .000 | −10.45 | −3.18 | |
| EFFORTFUL CONTROL-P → ANXIETY-P (c’) | −3.43 | 1.58 | −2.17 | .032 | −6.57 | −0.30 | |
| EFFORTFUL CONTROL-P → ANXIETY SENSITIVITY-P → ANXIETY-P (ab) | −3.38 | 1.18 | −6.06 | −1.40 | |||
| 4 | EFFORTFUL CONTROL-P → ANXIETY SENSITIVITY-P (a) | −2.89 | 0.90 | −3.21 | .002 | −4.67 | −1.11 |
| ANXIETY SENSITIVITY-P → DEPRESSION-P (b) | 0.15 | 0.06 | 2.61 | .010 | 0.04 | 0.27 | |
| EFFORTFUL CONTROL-P → DEPRESSION-P (c) | −2.82 | 0.54 | −5.18 | .000 | −3.89 | −1.74 | |
| EFFORTFUL CONTROL-P → DEPRESSION-P (c’) | −2.38 | 0.55 | −4.29 | .000 | −3.48 | −1.28 | |
| EFFORTFUL CONTROL-P → ANXIETY SENSITIVITY-P → DEPRESSION-P (ab) | 0.44 | 0.25 | −1.09 | −0.08 | |||
Note. a = Effect of X on M; b = Effect of M on Y; c = Total effect of X on Y; c’ = Direct effect of X on Y controlling for M. ab = indirect effect of X on Y through M. The standard error and 95% CI for a*b are obtained by bootstrap with 10,000 re-samples. CI (lower) = lower bound of a 95% confidence interval; CI (upper) = upper bound; → = affects. Effortful Control (−C and −P) are the predictors, Anxiety Sensitivity (−C and −P) are the explanatory variables, and Anxiety and Depression (−C and −P) are the outcomes.
3.2.2. Child-reported Depression.
The total effect model predicting RCADS-D was significant and accounted for 25% of variance (b = −4.47, SE = 0.76, p = ≤ 0.001). There was a significant positive indirect effect of effortful control on RCADS-D via CASI (completely standardized point estimate = −0.23, SE = 0.05, BC 95% CI [−0.35, −0.13]). The ratio of the indirect effect of CASI scores to the total effect of effortful control on RCADS-D was 0.46 (PM = 0.46, SE = 0.11; BC 95% CI [0.26, 0.72]). The comparison model (reversing X and M) also yielded a significant indirect effect (completely standardized point estimate = 0.12, SE = 0.04, BC 95% CI [0.05, 0.21].
3.2.3. Parent-reported Anxiety.
Results of indirect effects tests are presented in Table 2. The total effect model predicting RCADS-P-A was significant and accounted for 11.8% of variance (b = −6.82, SE = 1.83, p = ≤ 0.001). There was a significant positive indirect effect of effortful control on RCADS-P-A via CASI-P (completely standardized point estimate = −0.17, SE = 0.06, BC 95% CI [−0.30, −0.07]). The ratio of the indirect effect of CASI-P scores to the total effect of effortful control on RCADS-P-A was 0.51 (PM =0 .51, SE = 0.19; BC 95% CI [0.22, 0.97]). The comparison model (reversing X and M) also yielded a significant indirect effect (completely standardized point estimate =0 .05, SE = 0.03, BC 95% CI [0.01, 0.12]).
3.2.4. Parent-reported Depression.
The total effect model predicting RCADS-P-D was significant and accounted for 20.7% of variance (b = −2.82, SE = 0.54, p = ≤ 0 .001). There was a significant positive indirect effect of effortful control on RCADS-P-D via CASI-P (completely standardized point estimate = −0.07, SE =0 .04, BC 95% CI [−0.17, −0.01]). The ratio of the indirect effect of CASI-P scores to the total effect of effortful control on RCADS-P-D was 0.15 (PM = 0.15, SE = 0.10; BC 95% CI [0.02, 0.43]). The comparison model (reversing X and M) also yielded a significant indirect effect (completely standardized point estimate = 0.12, SE = 0.05, BC 95% CI [0.04, 0.23].
4. Discussion
The present investigation examined the indirect effect of effortful control, through anxiety sensitivity, on anxiety and depressive symptoms in a sample of children with anxiety disorders. Consistent with past work (Muris et al., 2008) and in support of the first hypothesis, greater effortful control was associated with lower anxiety sensitivity, anxiety, and depressive symptoms. These findings suggest that better effortful control may allow clinically anxious children to resist interpreting bodily sensations in a fearful manner, which, in theory, may lower anxiety and depressive symptoms (Gorlin & Teachman, 2015; Salemink & Wiers, 2012; Scheper et al., 2017).
In support of the second hypothesis, effortful control exerted a significant indirect effect through anxiety sensitivity on anxiety and depressive symptoms, accounting for 12-25% and 21-26% of the variance, respectively. These findings are consistent with research underscoring the influence of cognitive-affective factors on relations between temperamental regulatory abilities and anxiety and depressive symptoms (Gramszlo, Geronimi, Arellano, & Woodruff-Borden, 2018; Kotelnikova et al., 2015; Raines et al., 2019). Specifically, higher levels of effortful control may allow children to shift attention from, or inhibit, inaccurate thoughts about the dangers of anxiety-related sensations, which in turn, may lower emotional distress. Notably, effect sizes across the anxiety and depression models lend further support to the role of anxiety sensitivity in anxiety and depressive disorders (Muris, Schmidt, Merckelbach, & Schouten, 2001; Weems et al., 1997), and underscore the transdiagnostic applicability of the theorized model.
Although not the focus of the present investigation, two additional findings warrant mention. First, although the pattern of results held across child self-ratings and parent ratings of child functioning, respectively, child self-ratings of effortful control did not correlate with parental reports of child symptoms (and vice versa). Cross-informant mediational models, as alluded to earlier, were not significant either.1 Discrepancies in child and parent reports of child psychopathology are exceedingly common in general (De Los Reyes et al., 2015) and in childhood anxiety specifically (Grills & Ollendick, 2003), and may be due to a number of factors, such as child age, parenting practices, maternal psychopathology, and child willingness to disclose symptoms (De Los Reyes & Kazdin, 2005). For example, younger children may not be aware of their difficulties, may struggle to report them on questionnaires, or may not share anxious and/or depressed feelings with their parents. In addition, parents may not observe their children in certain contexts (e.g., school, socially), which limits their ability to report their child’s anxiety and/or depressive symptoms (De Los Reyes et al., 2015). Nevertheless, the possibility that the significance of our within-informant models was, in part, influenced by within-informant shared method variance cannot be ruled out.
Second, although the effect sizes were considerably smaller, reverse models (i.e., reversing the independent and mediating variables) were also significant. As such, it is possible that the relations between effortful control and anxiety sensitivity are bidirectional, wherein fear of interoceptive sensations disrupts the child’s effortful control abilities. However, effortful control and its developmental precursors (e.g., infant orienting/regulation; Bridgett et al., 2011) emerge early in development (Bridgett et al., 2011; Kochanska & Knaack, 2003; Posner & Rothbart, 2003; Rothbart & Bates, 1998), prior to the development of higher-order cognitions (e.g., anxiety sensitivity). Thus, while bidirectional associations cannot be ruled out, developmental theory and findings provide stronger support for the hypothesized models.
The present study has several limitations. First, the cross-sectional design precludes determining the exact direction of the association among variables. A longitudinal design would be better suited to address questions regarding the temporal sequence among the assessed constructs and would therefore provide a more robust evaluation of the hypothesized model. Second, mothers also had clinically significant levels of anxiety, which may have impacted parent report of child symptoms and contributed to informant discrepancies. For instance, a study examining the interaction between child age and maternal anxiety on informant discrepancies found that 1) when maternal anxiety is high and the child is older, maternal report of anxiety is relatively higher than the child’s and 2) when maternal anxiety is high and the child is younger, child report of anxiety is relatively higher (Niditch & Varela, 2011). A larger sample size may allow examination of child age as a potential moderator of effortful control-anxiety/depression associations. Third, cross-informant agreement for child internalizing symptoms is notoriously low (De Los Reyes & Kazdin, 2005; Grills & Ollendick, 2003). Moreover, within-informant shared method variance may have contributed to statistical significance of the within-informant models. Nevertheless, that the purported model was significant among child- and parent-reported measures, respectively, provides a greater degree of confidence in our findings. Fourth, given that the present investigation focused exclusively on mothers, it is unknown whether a similar pattern of findings would be obtained with fathers. Research has found that mother and father reports of child symptoms may differ due to several factors, including gender socialization, the setting in which the parent observes and interacts with the child, and/or the amount of time spent with the child (Jansen, Bodden, Muris, van Doorn, & Granic, 2017). Indeed, in a study examining correspondence between mother and father reports of child anxiety, Jansen and colleagues (2017) found greater agreement between mother (vs. father) and child reports of child anxiety. Future research should therefore examine differences in our hypothesized model as a function of parental report and moderators that may impact these effects (e.g., child gender). Finally, effortful control was only assessed through child- and parent-report. Given the relative paucity of behavioral assessments of effortful control (c.f., Lengua, Bush, Long, Kovacs, & Trancik, 2008; Lengua, Honorado, & Bush, 2007), future work would benefit from examining relations between both self-reported and behaviorally-indexed effortful control. Notably, if children believe that they have poor effortful control abilities, but display average effortful control skills in a behavioral task, this would point to the perception (vs. actual ability) of poor effortful control as a driving force in their emotional functioning.
Despite these limitations, there are clinical implications stemming from this work. Findings suggest the clinical utility of targeting effortful control in anxiety treatments. Indeed, effortful control has been found to be a malleable construct (Diamond, Barnett, Thomas, & Munro, 2007). Therefore, children with low effortful control may be targeted for interventions to improve this executive ability. Specifically, increasing ‘top down’ control may decrease anxiety sensitivity by improving the regulation/interpretation of ‘bottom-up’ sensations. Likewise, the findings suggest that there may be value in targeting anxiety sensitivity in children with effortful control deficits. Several studies have found support for brief interventions targeting anxiety sensitivity (Schmidt, Norr, Allan, Raines, & Capron, 2017), yet this construct is rarely specifically targeted in clinical work with children (c.f. Sherman, Braun, & Ehrenreich-May, 2019). Future studies with children should evaluate whether targeting anxiety sensitivity specifically results in improved outcomes, particularly among children with low effortful control.
Overall, the present investigation found support for anxiety sensitivity as a possible mechanism underlying the relation between effortful control and child anxiety and depressive symptoms in sample of children with anxiety disorders. Results suggest that children’s effortful control may reduce the likelihood of catastrophic interpretations of anxiety symptoms, which in turn, could lower anxiety and depressive symptoms. Interventions targeting effortful control may foster improved outcomes.
Acknowledgments
This work was supported by the National Institute of Mental Health [R21-MH101309-01A1; NCT02095340]. The views articulated in this article are those of the authors and do not necessarily reflect the views of the National Institutes of Health or National Institute of Mental Health. The authors report no conflict of interest.
Footnotes
Cross-informant models, wherein (1) child self-ratings of effortful control (X) and anxiety sensitivity (M) predicted parent ratings of child anxiety/depression (Y) and (2) parent ratings of child effortful control and anxiety sensitivity predicted child self-ratings of anxiety/depression were not significant.
References
- American Psychiatric Association. (2000) Diagnostic and Statistical Manual of Mental Disorders (4th, text revision ed.). Washington, DC. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: Author. [Google Scholar]
- Axelson DA, & Birmaher B (2001). Relation between anxiety and depressive disorders in childhood and adolescence. Depression and Anxiety, 14(2), 67–78. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, … Nelson B (1996). Childhood and adolescent depression: a review of the past 10 years. Part I. Journal of the American Academy of Child & Adolescent Psychiatry, 35(11), 1427–1439. [DOI] [PubMed] [Google Scholar]
- Bridgett DJ, Gartstein MA, Putnam SP, Lance KO, Iddins E, Waits R, … Lee L (2011). Emerging effortful control in toddlerhood: The role of infant orienting/regulation, maternal effortful control, and maternal time spent in caregiving activities. Infant Behavior and Development, 34(1), 189–199. [DOI] [PubMed] [Google Scholar]
- Capron DW, Allan NP, Ialongo NS, Leen-Feldner E, & Schmidt NB (2015). The depression distress amplification model in adolescents: A longitudinal examination of anxiety sensitivity cognitive concerns, depression and suicidal ideation. Journal of Adolescence, 41, 17–24. doi: 10.1016/j.adolescence.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson SM, & Moses LJ (2001). Individual differences in inhibitory control and children’s theory of mind. Child Development, 72(4), 1032–1053. doi: 10.1111/1467-8624.00333 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, & Lilienfeld SO (1999). Clinical assessment of anxiety sensitivity in children and adolescents: Where do we go from here? Psychological Assessment, 11(2), 212–224. doi:Doi 10.1037/1040-3590.11.2.212 [DOI] [Google Scholar]
- Chorpita BF, Moffitt CE, & Gray J (2005). Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behaviour Research and Therapy, 43(3), 309–322. doi: 10.1016/j.brat.2004.02.004 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. doi: 10.1016/S0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, Copeland W, Erkanli A, & Angold A (2011). Thedevelopmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity In Field AP & Silverman WK (Eds.), Anxiety Disorders in Children and Adolescents (2 ed., pp. 56–75). Cambridge: Cambridge University Press. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, & Angold A (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60(8), 837–844. doi:DOI 10.1001/archpsyc.60.8.837 [DOI] [PubMed] [Google Scholar]
- Cummings CM, Caporino NE, & Kendall PC (2014). Comorbidity of Anxiety and Depression in Children and Adolescents: 20 Years After. Psychological bulletin, 140(3), 816–845. doi: 10.1037/a0034733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DAG, Burgers DE, & Rabinowitz J (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological bulletin, 141(4), 858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, & Kazdin AE (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological bulletin, 131(4), 483–509. Retrieved from <Go to ISI>://WOS:000230851400001 [DOI] [PubMed] [Google Scholar]
- Diamond A, Barnett WS, Thomas J, & Munro S (2007). Preschool program improves cognitive control. Science (New York, NY), 318(5855), 1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditlevsen S, Christensen U, Lynch J, Damsgaard MT, & Keiding N (2005). The mediation proportion: a structural equation approach for estimating the proportion of exposure effect on outcome explained by an intermediate variable. Epidemiology, 16(1), 114–120. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Hofer C, & Vaughan J (2007). Effortful control and its socioemotional consequences In Gross JJ (Ed.), Handbook of emotion regulation (Vol. 2, pp. 287–288). [Google Scholar]
- Ellis LK, & Rothbart MK (2001). Revision of the Early Adolescent Temperament Questionnaire. Paper presented at the biennial meeting of the Society for Research in Child Development, Minneapolis, MN. [Google Scholar]
- Eysenck MW, Derakshan N, Santos R, & Calvo MG (2007). Anxiety and cognitive performance: attentional control theory. Emotion, 7(2), 336. [DOI] [PubMed] [Google Scholar]
- Garber J, & Weersing VR (2010). Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology: Science and Practice, 17(4), 293–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gramszlo C, Geronimi EMC, Arellano B, & Woodruff-Borden J (2018). Testing a Cognitive Pathway Between Temperament and Childhood Anxiety. Journal of Child and Family Studies, 27(2), 580–590. [Google Scholar]
- Grant DM, Beck JG, & Davila J (2007). Does anxiety sensitivity predict symptoms of panic, depression, and social anxiety? Behaviour Research and Therapy, 45(9), 2247–2255. doi: 10.1016/j.brat.2007.02.008 [DOI] [PubMed] [Google Scholar]
- Grills AE, & Ollendick TH (2003). Multiple informant agreement and the anxiety disorders interview schedule for parents and children. J Am Acad Child Adolesc Psychiatry, 42(1), 30–40. doi: 10.1097/00004583-200301000-00008 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (Second Edition ed.): Guilford Publications. [Google Scholar]
- Jansen M, Bodden DHM, Muris P, van Doorn M, & Granic I (2017). Measuring anxiety in children: the importance of separate mother and father reports. Child & youth care forum, 46(5), 643–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Cummings CM, Villabø MA, Narayanan MK, Treadwell K, Birmaher B, … Walkup J (2016). Mediators of change in the Child/Adolescent Anxiety Multimodal Treatment Study. Journal of Consulting and Clinical Psychology, 84(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, & Knaack A (2003). Effortful control as a personality characteristic of young children: Antecedents, correlates, and consequences. Journal of Personality, 71(6), 1087–1112. doi: 10.1111/1467-6494.7106008 [DOI] [PubMed] [Google Scholar]
- Kotelnikova Y, Mackrell SVM, Jordan PL, & Hayden EP (2015). Longitudinal associations between reactive and regulatory temperament traits and depressive symptoms in middle childhood. Journal of Clinical Child & Adolescent Psychology, 44(5), 775–786. [DOI] [PubMed] [Google Scholar]
- Lambert SF, McCreary BT, Preston JL, Schmidt NB, Joiner TE, & Ialongo NS (2004). Anxiety sensitivity in African-American adolescents: Evidence of symptom specificity of anxiety sensitivity components. Journal of the American Academy of Child and Adolescent Psychiatry, 43(7), 887–895. doi: 10.1097/01.chi.0000128799.99225.88 [DOI] [PubMed] [Google Scholar]
- Lengua LJ, Bush NR, Long AC, Kovacs EA, & Trancik AM (2008). Effortful control as a moderator of the relation between contextual risk factors and growth in adjustment problems. Development and Psychopathology, 20(2), 509–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ, Honorado E, & Bush NR (2007). Contextual risk and parenting as predictors of effortful control and social competence in preschool children. Journal of Applied Developmental Psychology, 28(1), 40–55. doi: 10.1016/j.appdev.2006.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonigan CJ, & Vasey MW (2009). Negative affectivity, effortful control, and attention to threat-relevant stimuli. Journal of Abnormal Child Psychology, 37(3), 387–399. doi: 10.1007/s10802-008-9284-y [DOI] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. doi: 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui LH, … Swendsen J (2010). Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49(10), 980–989. doi:DOI 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, & Age TR (2009). Adjustment among youth in military families: The protective roles of effortful control and maternal social support. Journal of Applied Developmental Psychology, 30(6), 695–707. [Google Scholar]
- Muris P, & Ollendick TH (2005). The role of temperament in the etiology of child psychopathology. Clinical Child and Family Psychology Review, 8(4), 271–289. doi: 10.1007/s10567-005-8809-y [DOI] [PubMed] [Google Scholar]
- Muris P, Schmidt H, Merckelbach H, & Schouten E (2001). Anxiety sensitivity in adolescents: factor structure and relationships to trait anxiety and symptoms of anxiety disorders and depression. Behaviour Research and Therapy, 39(1), 89–100. [DOI] [PubMed] [Google Scholar]
- Muris P, van der Pennen E, Sigmond R, & Mayer B (2008). Symptoms of anxiety, depression, and aggression in non-clinical children: Relationships with self-report and performance-based measures of attention and effortful control. Child Psychiatry and Human Development, 39(4), 455–467. doi: 10.1007/s10578-008-0101-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niditch LA, & Varela RE (2011). Mother–child disagreement in reports of child anxiety: Effects of child age and maternal anxiety. Journal of Anxiety Disorders, 25(3), 450–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niditch LA, & Varela RE (2018). A longitudinal study of inhibited temperament, effortful control, gender, and anxiety in early childhood. Child & Youth Care Forum. doi: 10.1007/s10566-018-9447-0 [DOI] [Google Scholar]
- O’Neil KA, Podell JL, Benjamin CL, & Kendall PC (2010). Comorbid Depressive Disorders in Anxiety-disordered Youth: Demographic, Clinical, and Family Characteristics. Child Psychiatry & Human Development, 41(3), 330–341. doi: 10.1007/s10578-009-0170-9 [DOI] [PubMed] [Google Scholar]
- Posner MI, & Rothbart MK (2003). Developing mechanisms of self-regulation In Hertzig ME & Farber EA (Eds.), Annual progress in child psychiatry and child development: 2000–2001. (pp. 21–42). New York, NY, US: Brunner-Routledge. [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Raines EM, Viana AG, Trent ES, Woodward EC, Candelari AE, Zvolensky MJ, & Storch EA (2019). Effortful Control, Interpretation Biases, and Child Anxiety Symptom Severity in a Sample of Children with Anxiety Disorders. Journal of Anxiety Disorders, 102136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S (1991). Expectancy Model of Fear, Anxiety, and Panic. Clinical Psychology Review, 11(2), 141–153. doi:Doi 10.1016/0272-7358(91)90092-9 [DOI] [Google Scholar]
- Rothbart MK, & Bates JE (1998). Temperament In Eisenberg N (Ed.), Handbook of child psychology: Social, emotional, and personality development. (pp. 105–176). Hoboken, NJ, US: John Wiley & Sons Inc. [Google Scholar]
- Rothbart MK, & Bates JE (2006). Temperament In Eisenberg N, Damon W, & Lerner RM (Eds.), Handbook of child psychology: Vol. 3, Social, emotional, and personality development (6th ed.). (pp. 99–166). Hoboken, NJ, US: John Wiley & Sons Inc. [Google Scholar]
- Scheper FY, Majdandžić M, van de Ven PM, Jansen LMC, Doreleijers TAH, Schuengel C, & de Vries ALC (2017). Temperament traits and psychopathology in young clinically referred children compared to a general population sample. Child Psychiatry and Human Development, 48(6), 841–850. doi: 10.1007/s10578-016-0708-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, & Capron DW (2017). A Randomized Clinical Trial Targeting Anxiety Sensitivity for Patients With Suicidal Ideation. Journal of Consulting and Clinical Psychology, 85(6), 596–610. doi: 10.1037/ccp0000195 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Fleisig W, Rabian B, & Peterson RA (1991). Childhood Anxiety Sensitivity Index. Journal of Clinical Child Psychology, 20(2), 162–168. doi:DOI 10.1207/s15374424jccp2002_7 [DOI] [PubMed] [Google Scholar]
- Snyder HR, Gulley LD, Bijttebier P, Hartman CA, Oldehinkel AJ, Mezulis A, … Hankin BL (2015). Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology, 109(6), 1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence SH (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36(5), 545–566. doi: 10.1016/S0005-7967(98)00034-5 [DOI] [PubMed] [Google Scholar]
- Tull MT, & Gratz KL (2008). Further examination of the relationship between anxiety sensitivity and depression: The mediating role of experiential avoidance and difficulties engaging in goal-directed behavior when distressed. Journal of Anxiety Disorders, 22(2), 199–210. doi: 10.1016/j.janxdis.2007.03.005 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2015). Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2015: 2015 Population Estimates. [Google Scholar]
- Varela RE, Weems CF, Berman SL, Hensley L, & de Bernal MCR (2007). Internalizing symptoms in Latinos: The role of anxiety sensitivity. Journal of Youth and Adolescence, 36(4), 429–440. doi: 10.1007/s10964-007-9168-4 [DOI] [Google Scholar]
- Viana AG, & Rabian B (2009). Fears of cognitive dyscontrol and publicly observable anxiety symptoms: Depression predictors in moderate-to-high worriers. Journal of Anxiety Disorders, 23(8), 1126–1131. doi: 10.1016/j.janxdis.2009.07.017 [DOI] [PubMed] [Google Scholar]
- Waszczuk MA, Brown HM, Eley TC, & Lester KJ (2015). Attentional control theory in childhood: enhanced attentional capture by non-emotional and emotional distractors in anxiety and depression. Plos One, 10(11), e0141535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weems CF, Hammond-Laurence K, Silverman WK, & Ferguson C (1997). The relation between anxiety sensitivity and depression in children and adolescents referred for anxiety. Behaviour Research and Therapy, 35(10), 961–966. doi:Doi 10.1016/S0005-7967(97)00049-1 [DOI] [PubMed] [Google Scholar]
- Weems CF, Taylor LK, Marks AB, & Varela RE (2010). Anxiety sensitivity in childhood and adolescence: Parent reports and factors that influence associations with child reports. Cognitive Therapy and Research, 34(4), 303–315. [Google Scholar]
- Wen Z, & Fan X (2015). Monotonicity of effect sizes: Questioning kappa-squared as mediation effect size measure. Psychological Methods, 20(2), 193. [DOI] [PubMed] [Google Scholar]
- White LK, McDermott JM, Degnan KA, Henderson HA, & Fox NA (2011). Behavioral inhibition and anxiety: The moderating roles of inhibitory control and attention shifting. Journal of Abnormal Child Psychology, 39(5), 735–747. doi: 10.1007/s10802-011-9490-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Rogers AH, Bakhshaie J, Viana AG, Walker R, Mayorga NA, … Ruiz AC (2019). Perceived racial discrimination, anxiety sensitivity, and mental health among Latinos in a federally qualified health center. Stigma and Health. [DOI] [PubMed] [Google Scholar]


