Graphical abstract
Keywords: Renal cell carcinoma, Transesophageal echocardiography, Secondary cardiac tumor
Highlights
-
•
RCC is the most common type of renal cancer.
-
•
RCC is capable of passing through the renal vein into the IVC.
-
•
Surgical resection requiring cardiopulmonary bypass is currently the only curative treatment.
-
•
Metastatic RCC tumor spread into the heart is a poor long-term prognostic factor.
Introduction
Renal cell carcinoma (RCC), the most common form of kidney cancer, is known to be an aggressive disease and accounts for 3% of all adult malignancies.1,2 Predisposing risk factors include obesity, smoking, hypertension, polycystic kidney disease, and male sex, with a peak incidence in the sixth and seventh decades of life. The typical presentation of hematuria, abdominal mass, and flank pain is rare and is usually associated with advanced disease.3 More than 70% of patients diagnosed with RCC are diagnosed incidentally using modern imaging technologies such as computed tomography (CT) that are often ordered to investigate nonspecific symptoms.4 As many as 25% of patients have metastatic disease at the time of diagnosis. RCC is known to spread into the inferior vena cava (IVC) in up to 15% of cases. Less common is spread of tumor thrombus burden into the right atrium of the heart, which occurs in <1% of cases.3 Even less common is RCC tumor spread across the tricuspid valve into the right ventricle.5, 6, 7 We present the case of a patient who was found incidentally to have RCC on CT with spread into the IVC. Transesophageal echocardiography was ordered to further evaluate tumor burden and revealed tumor thrombus combination extending into the right atrium, across the tricuspid valve, and into the right ventricle.
Case Presentation
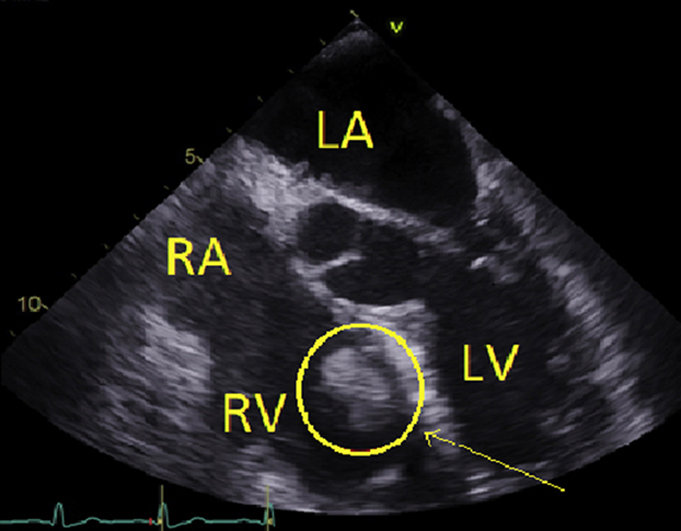
A 77-year-old Caucasian man with a history of tobacco use presented for evaluation after a syncopal episode at home. After the syncopal episode, the patient reported back and flank pain. While in the emergency department, he was sent for CT of the abdomen and pelvis, which revealed a large infiltrating heterogeneous left renal mass measuring 10.2 × 8.4 cm. The tumor was noted to involve the left renal vein and IVC. Transesophageal echocardiography was ordered for further evaluation of the tumor to better determine the extent into the heart and for surgical planning. Transesophageal echocardiography revealed a large, ropelike echodensity with exaggerated undulating motion extending from the IVC to the right atrium across the tricuspid valve and into the right ventricle (Figure 1, Figure 2, Figure 3). The left ventricular ejection fraction was noted to be 60% to 65%. Findings were consistent with probably metastatic propagation of renal carcinoma, possibly with added thrombus burden. No right ventricular strain was noted. Cardiothoracic, urologic, and general surgery services were consulted. The diagnosis was metastatic RCC. It was decided that the left kidney along with the tumor metastasis should be surgically resected. The patient was given an intravenous infusion of unfractionated heparin up until the time of surgery.
Figure 1.

Four-chamber view on transesophageal echocardiography. Tumor is noted within the right ventricle (circle). LA, Left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Figure 2.
Four-chamber view on transesophageal echocardiography. Tumor is noted within the right atrium (circle). LA, Left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Figure 3.

Bicaval view showing tumor entering from the IVC into the right atrium. Tumor is indicated by arrows. IVC, Inferior vena cava; LA, left atrium; RA, right atrium; SVC, superior vena cava.
Full laparotomy was performed with the left kidney mobilized for left radical nephrectomy. Full sternotomy was next performed, followed by cardiopulmonary bypass. After cardiac arrest was achieved, the right atrium was incised, and a large amount of tumor thrombus burden was seen tracking from the right atrium across the tricuspid valve into the right ventricle. This tumor was subsequently removed. A large amount of tumor thrombus was next removed from the IVC. The IVC was then opened at the junction of the left renal vein, with all tumor removed from the distal IVC and the left renal vein. The left kidney was finally removed, along with associated tumor. The chest and abdomen were closed.
After surgery, the patient was successfully extubated and admitted to surgery service. Specimens from the left kidney along with tumor thrombus from the IVC and right atrium were sent to pathology for further evaluation. Transthoracic echocardiography was ordered after surgery. The ejection fraction was noted to be 50% to 55%. The tricuspid valve was noted to open well, with only trace tricuspid regurgitation. The right atrium and the IVC were not well visualized. Right ventricular systolic pressure was estimated to be 36 mm Hg above right atrial pressure. Right atrial pressure could not be estimated. All surgical specimens showed disease consistent with clear cell renal carcinoma with rhabdoid differentiation (Figure 4), consistent with International Society of Urological Pathology grade 4 disease. Renal vein margin was positive for carcinoma. Angiolymphatic invasion was present as well. The patient had a prolonged hospital course complicated by left abdominal abscess and eventually intermittent hemodialysis. The patient did improve, no longer required hemodialysis, and was discharged home to follow with oncology as an outpatient for evaluation of immunotherapies. Considering that his presentation was related to renal cell cancer that was successfully resected, and the patient's being under early postoperative context, he was not prescribed a long-term oral anticoagulant. The patient has been following up with hematology and oncology as an outpatient at another facility and receiving further care.
Figure 4.

Right atrium clot with renal cell carcinoma. Histologic sections show metastatic carcinoma (big arrow) in blood clot (small arrow). 100x/ H&E stain.
Discussion
Primary cardiac tumors are extremely rare, with an incidence of approximately 0.02% on autopsy.8 However, secondary tumors are much more common.7 Metastatic tumors can make their way to the heart through the caval system or by direct invasion. Often symptoms due to a cardiac malignancy (primary or secondary) do not present until late stages of the disease. In addition to syncope and dyspnea, thromboembolic events and sudden cardiac death can be serious events related to cardiac tumors.9 Echocardiography is an essential tool for evaluating intracardiac masses, including tumors, endocarditis, and thrombi.8
RCC is most commonly diagnosed incidentally, as the classical triad of hematuria, flank pain, and abdominal mass is seen only in advanced stages. Cardiac metastasis is an uncommon site for RCC. Symptoms of right-sided cardiac involvement include dyspnea, syncope, right-sided murmurs, profound edema, ascites, and other signs of right-sided congestive symptoms.3 RCC is staged on the basis of tumor-node-metastasis staging set forth by the American Joint Committee on Cancer. Staging can be performed using CT or magnetic resonance imaging, but CT is most commonly used for staging.10
There is a correlation between long-term survival and stage of disease. The 5-year survival rate of stage I RCC is reported to be 66%, and the stage IV survival rate is as low as 11%.7 Surgical resection with cardiopulmonary bypass and deep hypothermal circulatory arrest is the current treatment for patients with tumor thrombus burden within the heart.5 Resection of tumor requires median sternotomy and cardiac arrest with cardiopulmonary bypass with cannulation of the ascending aorta, superior vena cava, and IVC. Right atriotomy is then performed for intracardiac tumor removal.11 RCC is resistant to conventional chemotherapy. Surgical resection and cytokine-based therapies were initially the mainstay of treatment for patients diagnosed with RCC. However, the development of tyrosine kinase receptor inhibitors is offering hope as a viable treatment option for treatment of patients with RCC.5 The long-term prognosis is poor for those who have been diagnosed with metastatic RCC, with life usually limited to months despite treatment with surgery and immunotherapy.1,2,12
The benefit of anticoagulation therapy in these patients in unclear. It is recommended that patients who have pure thrombus in addition to thrombus/tumor combination should undergo anticoagulation. Placement of an IVC filter is not recommended, as it significantly complicates any surgical resection.13 Anticoagulation in the postoperative period after any extensive retroperitoneal surgery should be avoided, as patients are at very high risk for bleeding.14 There are no guidelines available with regard to anticoagulation after the risk for postoperative bleeding has passed.
Conclusion
RCC usually presents with atypical symptoms rather than the triad of hematuria, flank pain, and abdominal mass. It is also known for metastasizing to the heart through the IVC.3 Expansion into the right ventricle is extremely uncommon.5, 6, 7 Cardiac tumor associated with RCC is associated with poor long-term prognosis.6
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
References
- 1.Shah S., Vinod P., Khayata M., Lane J.L., Hegde V., Raina R. Atrial metastasis of renal cell carcinoma: a rare presentation. Cardiol Res. 2018;9:183–185. doi: 10.14740/cr690w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reports C., Sountoulides P., Metaxa L., Cindolo L. Atypical presentations and rare metastatic sites of renal cell carcinoma : a review of case reports. J Med Case Rep. 2011;5:429. doi: 10.1186/1752-1947-5-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oltean M., Matuz R., Sitar-taut A., Mihailov A., Rednic N., Tantau A. Renal cell carcinoma with extensive tumor thrombus into the inferior vena cava and right atrium in a 70-year-old man. Am J Mens Health. 2019;13 doi: 10.1177/1557988319846404. 1557988319846404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen D.Y.T., Uzzo R.G. Evaluation and management of the renal mass. Med Clin North Am. 2011;95:179–189. doi: 10.1016/j.mcna.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Miura S., Yamada A., Iba Y., Maruyama R., Hatta E., Kurimoto Y. Surgical treatment of isolated right ventricular metastasis from renal cell carcinoma. Surg Case Reports. 2019;5:3–6. doi: 10.1186/s40792-019-0733-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noguchi K., Hori D., Nomura Y., Tanaka H. Renal cell carcinoma with tumor–thrombus extension into the right ventricle. Ann Vasc Dis. 2012;5:376–380. doi: 10.3400/avd.cr.11.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eddicks S., Kivelitz D., Breitwieser C., Knebel F., Theres H., Baumman G. Right ventricular metastasis caused by a renal cell carcinoma (Grawitz tumor): case report. J Am Soc Echocardiogr. 2006;19:1073.e11–1073.e15. doi: 10.1016/j.echo.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Reynen K. Frequency of primary tumors of the heart. Am J Cardiol. 1996;77:107. doi: 10.1016/s0002-9149(97)89149-7. [DOI] [PubMed] [Google Scholar]
- 9.Özer N., Deniz A., Pişkinpaşa S., Kilickap S., Kepez A., Hazirolan T. Renal cell carcinoma extending from superior vena cava into right atrium. J Am Soc Echocardiogr. 2007;20:538.e7–538.e8. doi: 10.1016/j.echo.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Dunnick N.R. Renal cell carcinoma: staging and surveillance. Abdom Radiol. 2016;41:1079–1085. doi: 10.1007/s00261-016-0692-0. [DOI] [PubMed] [Google Scholar]
- 11.Ishida N., Takemura H., Shimabukuro K., Matsuno Y. Complete resection of asymptomatic solitary right atrial metastasis from renal cell carcinoma without inferior vena cava involvement. J Thorac Cardiovasc Surg. 2011;142:e142–e144. doi: 10.1016/j.jtcvs.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Ljungberg B., Bensalah K., Bex A., Canfield S., Giles R., Hora M. EAU guidelines on renal cell carcinoma. https://uroweb.org/wp-content/uploads/10-Renal-Cell-Carcinoma_LR.pdf Available at: [DOI] [PubMed]
- 13.Quencer K.B., Friedman T., Sheth R., Oklu R. Tumor thrombus: incidence, imaging, prognosis and treatment. Cardiovasc Diagn Ther. 2017;7(suppl 3):S165–S177. doi: 10.21037/cdt.2017.09.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schimmer C., Hillig F., Riedmiller H., Elert O. Surgical treatment of renal cell carcinoma with intravascular extension. Interact Cardiovasc Thorac Surg. 2004;3:395–397. doi: 10.1016/j.icvts.2004.02.014. [DOI] [PubMed] [Google Scholar]



