Graphical abstract
Keywords: PLSVC, Congenital heart disease, Contrast echocardiography, Cardiac MRI
Highlights
-
•
Adults with congenital heart disease have a high incidence of stroke.
-
•
Agitated saline administration via the left upper extremity was used to detect PLSVC.
-
•
Cardiac MRI was used to accurately diagnose PLSVC.
-
•
Bicuspid aortic valve can coexist in patients with PLSVC.
Introduction
Persistent left superior vena cava (PLSVC) is a congenital malformation caused by abnormal embryologic development of the left cardinal vein, resulting in a left superior vena cava that can connect to either atrium.1 A systemic right-to-left shunt occurs if the PLSVC drains into the left atrium.2,3 Although PLSVC often remains undetected, patients have a higher incidence of stroke compared with the general population.4 In addition, PLSVC is often associated with other congenital heart defects that can become clinically significant.5 Here, we present a case of PLSVC with a bicuspid aortic valve in a middle-aged adult who had recurrent strokes with previously negative workup.
Case Presentation
A 43-year-old Caucasian woman with a prior stroke presented to the emergency department with acute right upper and lower extremity weakness that began in the morning upon awakening from sleep. On presentation, she was afebrile. Her blood pressure was 109/87 mm Hg and her pulse was 87 beats/min. Physical examination was significant only for mild right-sided lower extremity weakness and a harsh crescendo-decrescendo systolic murmur at the right upper sternal border with radiation to the carotid arteries. Thus, transthoracic echocardiography (TTE) was ordered and neurology was consulted for stroke evaluation.
Of note, the patient had a stroke at 27 years of age, when she experienced acute left upper extremity weakness. Subsequent brain magnetic resonance imaging (MRI) identified a small infarct in the right frontal lobe. A comprehensive stroke workup was performed at that time, including TTE with agitated saline, which did not detect any intracardiac shunting. Thus, this stroke was ultimately classified as cryptogenic and attributed to earlier oral contraceptive use. She had no residual neurologic deficits. Except for the prior stroke, the patient had no other significant medical history. She was a nonsmoker and denied illicit drug use.
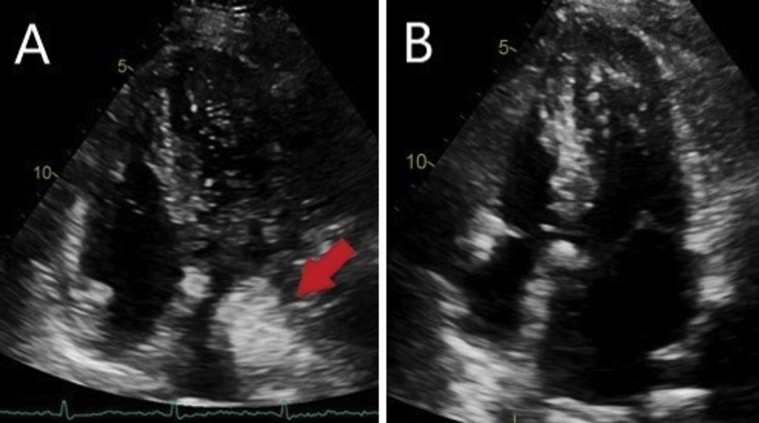
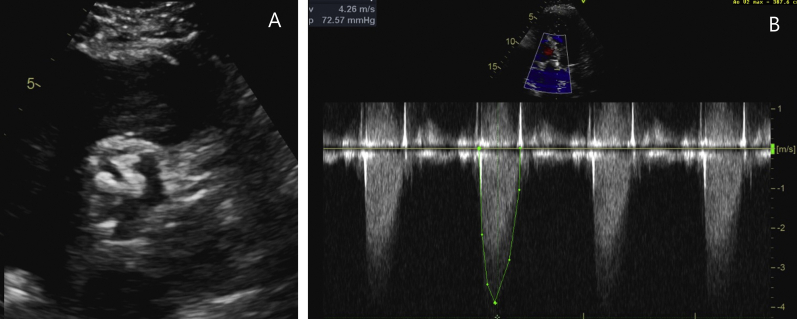
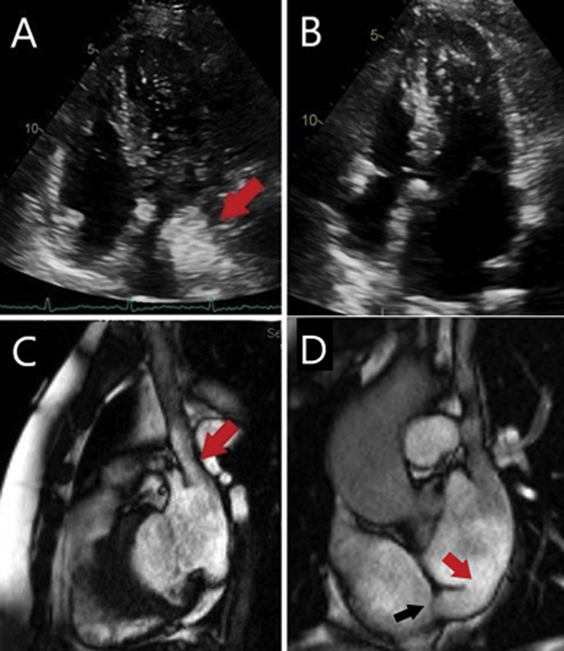
Initial investigation with computed tomography of the head did not show any large infarcts or hemorrhage, and computed tomographic angiography of the head and neck showed no significant intra- or extracranial stenoses. However, brain MRI showed an acute infarct in the posterior left insula and a subacute infarct in the posterior left frontal lobe. Additionally, brain MRI identified a chronic small infarct in the right frontal lobe. TTE with agitated saline injected through the left antecubital vein was performed. A large right-to-left shunt was visualized with immediate opacification of the left atrium (Figure 1A, Video 1 in Supplementary Data). This was suggestive of systemic venous drainage into the left atrium. Echocardiography also showed normal biventricular size and function (Figure 1B) and the presence of a calcified bicuspid aortic valve (Figure 2A, Video 2 in Supplementary Data) with moderate aortic stenosis (Figure 2B).
Figure 1.
Apical four-chamber views of agitated saline contrast study and noncontrast images. (A) Immediate opacification of the left atrium after agitated saline was administrated via the left antecubital vein (red arrow). (B) Normal-sized right atrium and right ventricle.
Figure 2.
TTE of bicuspid aortic valve and moderate aortic stenosis. (A) Parasternal short-axis view of bicuspid aortic valve with heavy calcification. (B) Continuous-wave Doppler showing moderate aortic stenosis with a peak velocity of 388 cm/sec and a mean gradient of 34 mm Hg.
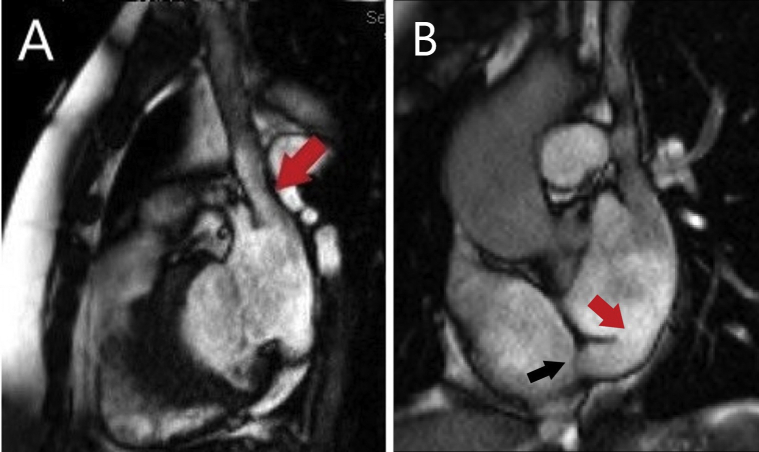
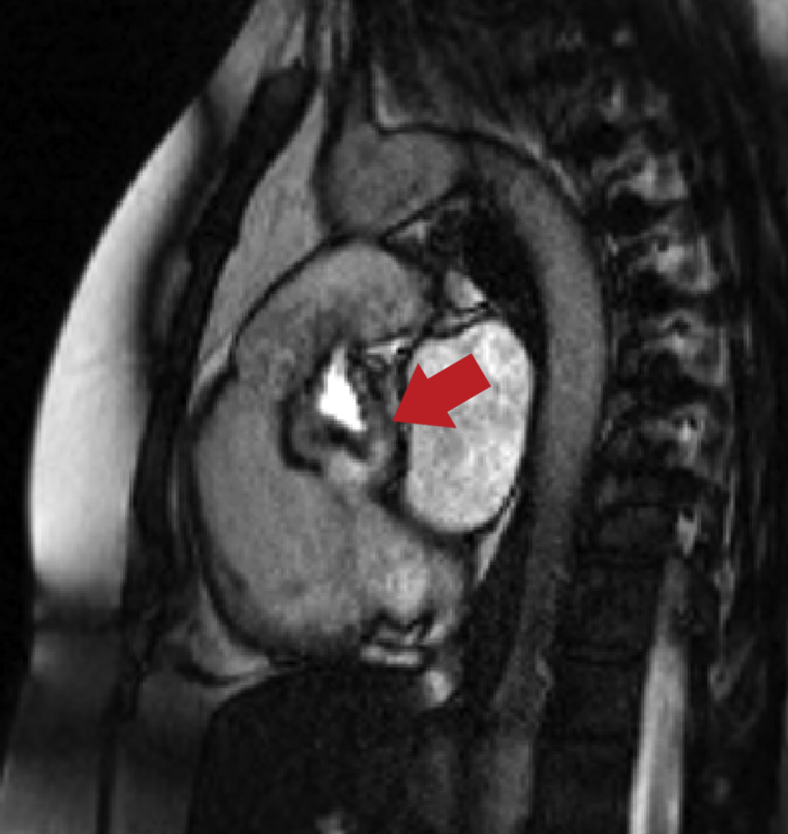
Subsequent cardiac MRI revealed a PLSVC draining into the left atrium (Figure 3A) and a completely unroofed coronary sinus (Figure 3B, red arrow, Video 3 in Supplementary Data). A Thebesian valve was also visualized in the right atrium at the orifice of the coronary sinus (Figure 3B, black arrow), which may have limited the flow into the right atrium, resulting in a normal-sized right atrium and right ventricle. A calcified Sievers type 1 bicuspid aortic valve with fusion of the right and left coronary cusps was also noted on cardiac MRI (Figure 4, Video 4 in Supplementary Data). No deep vein thromboses were detected on venous Doppler ultrasound of the upper and lower extremities. Cardiac telemetry during the hospitalization did not detect any arrhythmia for >48 hours. The patient had no further events during the hospitalization.
Figure 3.
Cardiac MRI depicting the presence of PLSVC and unroofed coronary sinus. (A) PLSVC draining into the left atrium (red arrow). (B) Basal short-axis view of a completely unroofed coronary sinus (red arrow) and a Thebesian valve (black arrow) visualized at the coronary sinus orifice in the right atrium.
Figure 4.
Cardiac MRI revealed a Sievers type 1 bicuspid aortic valve with heavy calcification during mid-systole (red arrow).
Given the concern for recurrent strokes in the presence of the aforementioned congenital defects, the patient was referred to cardiothoracic surgery. She underwent successful reconstruction of the coronary sinus, in which the surgeon connected the PLSVC orifice to the coronary sinus using a baffle made from bovine pericardial tissue, followed by atrial septum repair. During the operation, the native aortic valve was noted to be bicuspid with heavy calcification and was subsequently replaced with a mechanical prosthesis.
Discussion
Adults with congenital heart disease have been shown to have a high incidence of ischemic stroke, with incidence up to 9 to 12 times higher in patients <55 years of age compared with the general population.6 It has also been estimated that up to 10% of adults <65 years of age with congenital heart disease have experienced strokes.6 PLSVC is still the most common thoracic vein anomaly, affecting about 0.3% to 2.0% of the general population, and can coexist in 4% to 10% of patients with congenital heart defects.1 A large retrospective study of neonates identified that 3.6% and 10.6% of patients with PLSVC also possessed bicuspid aortic valves and secundum atrial septal defects, respectively.5 In addition, there is a significant association between PLSVC and unroofed coronary sinus defects. Previous reports have suggested that up to 75% to 83% of unroofed coronary sinus cases are associated with PLSVC.2,7, 8, 9, 10, 11, 12
A majority of PLSVC cases (80%–90%) involve the PLSVC draining to the right atrium through a dilated coronary sinus and are typically asymptomatic.1,2,5 However, when the PLSVC communicates with the left atrium, either directly or via the unroofed coronary sinus or pulmonary vein, a right-to-left shunt results.1, 2, 3, 4, 5,7, 8, 9, 10, 11, 12, 13 According to our literature review, all documented cases of stroke and thromboembolism in PLSVC have been attributed to right-to-left shunting, and the most common mechanism is through an unroofed coronary sinus into the left atrium.5,8,10, 11, 12 It is believed that stroke in the setting of PLSVC with left atrial drainage is likely caused by thromboembolism due to formation of thrombus occurring in the left superior vena cava or the left upper extremity veins and then subsequent paradoxical embolization via the right-to-left shunt.4,13, 14, 15
The diagnosis of PLSVC using TTE has been shown to depend on the correct administration of agitated saline into the left upper extremity peripheral vein.3,12 Saline injection via the right upper extremity vein may detect other anatomic mechanisms of intracardiac shunting, such as a patent foramen ovale, but would fail to detect the presence of an isolated PLSVC. Further imaging with cardiac MRI and/or multidetector cardiac computed tomography can better characterize the venous anomaly and its associated anatomic variants.8,9,11,12
Conclusion
PLSVC can present as a stroke and should be considered especially in patients <55 years of age with a new or recurrent stroke. To successfully diagnose the presence of PLSVC by TTE, agitated saline must be injected via the left upper extremity veins. We recommend that left-sided saline administration in contrast echocardiography should be a standard practice as part of the diagnostic workup for stroke in young to middle-aged patients, particularly with recurrent strokes.
Footnotes
Dr. Park is supported by grant T32HL076132 from the National Institutes of Health. Dr. Zhou is the site principal investigator of the ADAPTABLE trial and receives research funds from the Patient-Centered Outcomes Research Institute.
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2020.05.019.
Supplementary Data
Agitated saline contrast study. Apical four-chamber view revealed immediate opacification of the left atrium after agitated saline was administrated via the left antecubital vein.
TTE of the aortic valve. Parasternal short-axis view of the aortic valve demonstrated a heavily calcified bicuspid aortic valve with restricted excursion.
Cardiac MRI of the PLSVC and unroofed coronary sinus. PLSVC was shown draining into the left atrium with a completely unroofed coronary sinus. A Thebesian valve was visualized at the coronary sinus orifice in the right atrium.
Cardiac MRI of the bicuspid aortic valve. Right ventricular outflow view showed a stenotic Sievers type 1 bicuspid aortic valve with fusion of the right and left coronary cusps.
References
- 1.Buirski G., Jordan S.C., Joffe H.S., Wilde P. Superior vena caval abnormalities: their occurrence rate, associated cardiac abnormalities and angiographic classification in a paediatric population with congenital heart disease. Clin Radiol. 1986;37:131–138. doi: 10.1016/s0009-9260(86)80382-8. [DOI] [PubMed] [Google Scholar]
- 2.Tyrak K.W., Holda J., Holda M.K., Koziej M., Piatek K., Klimek-Piotrowska W. Persistent left superior vena cava. Cardiovasc J Afr. 2017;28:e1–e4. doi: 10.5830/CVJA-2016-084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta R., Pearson A. Diagnosis of persistent left superior vena cava draining directly into the left atrium. North Am J Med Sci. 2013;5:496–497. doi: 10.4103/1947-2714.117328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hutyra M., Skala T., Sanak D., Novotny J., Köcher M., Taborsky M. Persistent left superior vena cava connected through the left upper pulmonary vein to the left atrium: an unusual pathway for paradoxical embolization and a rare cause of recurrent transient ischaemic attack. Eur J Echocardiogr. 2010;11:e35. doi: 10.1093/ejechocard/jeq079. [DOI] [PubMed] [Google Scholar]
- 5.Chao Y.J., Chen M.R., Hung W.L., Yeh S.J., Lin S.M. Impact of persistent left superior vena cava detection in a normal neonatal population through echocardiography. Acta Cardiologica Sinica. 2019;45:600–605. doi: 10.6515/ACS.201911_35(6).20190704A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lanz J., Brophy J.M., Therrien J., Kaouache M., Guo L., Marelli A.J. Stroke in adults with congenital heart disease: incidence, cumulative risk, and predictors. Circulation. 2015;132:2385–2394. doi: 10.1161/CIRCULATIONAHA.115.011241. [DOI] [PubMed] [Google Scholar]
- 7.Ouchi K., Sakuma T., Kawai M., Fukuda K. Incidence and appearances of coronary sinus anomalies in adults on cardiac CT. Japanese J Radiol. 2016;34:684–690. doi: 10.1007/s11604-016-0574-y. [DOI] [PubMed] [Google Scholar]
- 8.Bonardi M., Valentini A., Camporotondo R. Unroofed coronary sinus and persistent left superior vena cava: a case report. J Ultrasound. 2012;15:179–182. doi: 10.1016/j.jus.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yousaf M., Malak S.F. Left atrial drainage of a persistent left superior vena cava. Radiol Case Rep. 2008;3:225. doi: 10.2484/rcr.v3i4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurtoglu E., Cakin O., Akcay S., Akturk E., Korkmaz H. Persistent left superior vena cava draining into the coronary sinus: a case report. Cardiol Res. 2011;2:249–252. doi: 10.4021/cr85w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Eshmawi A., Tang G.H., Pawale A., Anyanwu A.C., Adams D.H. Unroofed coronary sinus in an adult. J Card Surg. 2013;28:19–22. doi: 10.1111/jocs.12035. [DOI] [PubMed] [Google Scholar]
- 12.Xu B., Betancor J., Cremer P.C., Renapurkar R., Pettersson G.B., Asher C.R. Multimodality cardiovascular imaging of unroofed coronary sinus defects. JACC Cardiovasc Imaging. 2018;11:1027–1030. doi: 10.1016/j.jcmg.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Recto M.R., Sadlo H., Sobczyk W.L. Rare case of persistent left superior vena cava to left upper pulmonary vein: pathway for paradoxical embolization. J Invasive Cardiol. 2007;19:e313–e316. [PubMed] [Google Scholar]
- 14.Butera G., Salvia J., Carminati M. When side matters: contrast echocardiography with injection from the left antecubital vein to detect a persistent left superior vena cava draining to the left atrium in a patient with cerebral stroke. Circulation. 2012;125:e1. doi: 10.1161/CIRCULATIONAHA.110.013318. [DOI] [PubMed] [Google Scholar]
- 15.Saranteas T., Mandila C., Poularas J., Papanikolaou J., Patriankos A., Karakitsos D. Transesophageal echocardiography and vascular ultrasound in the diagnosis of catheter-related persistent left superior vena cava thrombosis. Eur J Echocardiogr. 2009;10:452–455. doi: 10.1093/ejechocard/jen334. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Agitated saline contrast study. Apical four-chamber view revealed immediate opacification of the left atrium after agitated saline was administrated via the left antecubital vein.
TTE of the aortic valve. Parasternal short-axis view of the aortic valve demonstrated a heavily calcified bicuspid aortic valve with restricted excursion.
Cardiac MRI of the PLSVC and unroofed coronary sinus. PLSVC was shown draining into the left atrium with a completely unroofed coronary sinus. A Thebesian valve was visualized at the coronary sinus orifice in the right atrium.
Cardiac MRI of the bicuspid aortic valve. Right ventricular outflow view showed a stenotic Sievers type 1 bicuspid aortic valve with fusion of the right and left coronary cusps.