Abstract
According to recent guidelines, 46% of U.S. adults have high blood pressure (i.e., hypertension). Traditionally addressed in clinical settings, only 54% of adults successfully manage their hypertension. Community–clinical partnerships that facilitate medication adherence and lifestyle changes are promising avenues to achieve population-level blood pressure control. We examined partnerships for blood pressure control in Washington State, their facilitators and barriers, and ways public health departments could foster partnerships. We conducted 41 semistructured interviews with clinic staff, community-based organization (CBO) staff, pharmacy staff, and community health workers (CHWs). The Centers for Disease Control and Prevention–adapted Himmelman Collaboration Continuum, which describes five levels of partnership intensity, guided our thematic analysis. We found variation across sectors in partnership frequency and intensity. Clinic and pharmacy staff reported fewer partnerships than CBO staff and CHWs, and mostly either low or very high intensity partnerships. CBO staff and CHWs described partnerships at each intensity level. Trust and having a shared mission facilitated partnerships. Competition, lack of time, limited awareness of resources, and lack of shared health records constituted barriers to partnership. Bringing potential partners together to discuss shared goals, increasing technological integration, and building awareness of resources may help bridge clinical and community silos and improve population-level blood pressure control.
Keywords: cardiovascular disease, chronic disease, community organization, health promotion, health research, lay health advisors/community health workers, medical care, partnerships/coalitions
INTRODUCTION
Current diagnostic criteria estimate that more than 103 million adults in the United States (46%) have hypertension (i.e., high blood pressure) (Benjamin et al., 2018). Contributing to more than 1,000 deaths per day, uncontrolled hypertension is a risk factor for heart attack, stroke, chronic heart failure, and kidney disease (Benjamin et al., 2018; Mozaffarian et al., 2014; Whelton et al., 2018) and costs the US $46 billion annually (Mozaffarian et al., 2014). Improving population-level blood pressure control is therefore a prime interest of public health practitioners, policymakers, and scholars (Alley, Asomugha, Conway, & Sanghavi, 2016; Carter, Bosworth, & Green, 2011).
Blood pressure control has traditionally been addressed by primary care providers, who prescribe medications and recommend lifestyle changes such as weight loss, smoking cessation, reduced alcohol consumption, physical activity, and improved diet (Fang, Ayala, & Loustalot, 2015; Hyman & Pavlik, 2000; Sloane & Ebell, 2007). However, only 54% of diagnosed patients are able to successfully manage their high blood pressure (Mozaffarian et al., 2014). Team-based care that includes physicians, nurses, pharmacists, and community health workers (CHWs) is an evidence-based strategy to improve hypertension outcomes (Carter et al., 2011; Coleman, Austin, Brach, & Wagner, 2009; Institute of Medicine Committee on Public Health Priorities to Reduce and Control Hypertension in the U.S. Population, 2010; Kravetz & Walsh, 2016; Margolius et al., 2012), but clinical interventions alone may not address all patient needs. A public health approach focused on fostering partnerships between clinical entities and community organizations (i.e., community–clinical linkages) could help patients who need additional support for managing their blood pressure by improving access to resources in their communities, where they spend most of their time (Brownstein et al., 2007; Centers for Disease Control and Prevention [CDC], 2014; Division for Heart Disease and Stroke Prevention, 2016; Payán et al., 2017; Thomas et al., 2014).
Recognizing the need for such an approach, the CDC has been promoting and supporting, through funding available for state departments of health, the development of community–clinical linkages for evidence-based chronic disease prevention and management. One such funding mechanism is the State and Local Public Health Actions to Prevent Obesity, Diabetes, and Heart Disease and Stroke Program (DP14–1422), an Affordable Care Act–funded program to prevent obesity, diabetes, heart disease, and stroke and reduce health disparities through community and health system interventions (CDC, 2018). One of the aims of the program was to develop partnerships between clinics, pharmacists, CHWs, and community organizations to prevent and manage chronic diseases, such as hypertension, especially among those who are most at risk (CDC, 2018). However, little is known about what existing clinical–community partnerships entail or about facilitators and barriers to their development and maintenance (Barnes & Curtis, 2009; Buckley et al., 2013; Fishleder et al., 2018; Payán et al., 2017; Porterfield et al., 2012; Valaitis et al., 2018).
Washington State Department of Health was one of 21 DP14–1422 Program grantees (Trust for America’s Health, 2016). Washington has similar rates of hypertension to the broader United States (30.4% compared to 31.4%, respectively) (United Health Foundation, 2019), but faces significant disparities between rural and urban areas, and among different racial/ethnic groups (CDC, 2017; Trust for America’s Health, 2016; Washington State Department of Health, 2018). Given the specific focus of DP14–1422 on facilitating community–clinical linkages, we developed this study primarily to describe current blood pressure control partnerships among clinics, pharmacists, CHWs, and community-based organizations (CBOs) in Washington State. Second, we aimed to identify factors that helped or hindered the formation of these partnerships and to highlight strategies that state or local public health departments could take to foster community–clinical linkages. Our results are informing ongoing efforts to support intersectoral partnerships for blood pressure control and other types of chronic disease prevention and management in Washington and may inform similar efforts in other states.
METHOD
We conducted semistructured qualitative interviews between December 2016 and July 2017, with participants from four professional sectors—clinic staff, pharmacists, CBO staff, and CHWs. The Consolidated Criteria for Reporting Qualitative Research (COREQ) guided our methodology and presentation of results (Tong, Sainsbury, & Craig, 2007). We received institutional review board approval for the study from the University of Washington Human Subjects Division.
Participants
We sought to recruit participants who worked as clinic staff, pharmacists, CHWs, or CBO staff in Washington State and who engaged in blood pressure control activities as part of their jobs. We recruited participants using snowball sampling (Marshall, 1996), first asking members of our professional networks to send a study recruitment email to potential participants within each sector, and then asking enrolled participants for their help in recruiting other eligible participants. Through this process, we identified 57 potential participants who expressed interest in the study and self-identified as meeting the eligibility criteria.
Data Collection
We developed interview guides tailored to each sector (Supplemental Appendix). These included standard demographic questions, open-ended questions about each organization’s activities related to blood pressure control, partnerships with other sectors to prevent and manage high blood pressure, facilitators and barriers to developing and maintaining partnerships, and ideas about how the Washington State Department of Health (Washington DOH) could support these partnerships. We piloted the guides with at least one representative from each sector and made changes based on their feedback.
A trained interviewer conducted 25- to 45-minute phone interviews in English. We interviewed 45 of 57 potential participants (78.9% participation rate). Twelve potential participants did not participate because we had met our quota (n = 6), they did not meet eligibility criteria (n = 3), they did not respond to follow-up requests (n = 2), or they felt their work did not focus enough on blood pressure control to be relevant in the study (n = 1). We provided a $50 incentive to participants. All interviews were audiorecorded and professionally transcribed verbatim.
Conceptual Framework
Our study was informed by the Himmelman Collaboration Continuum (Himmelman, 2002), a framework that describes networking, coordination, cooperation, and collaboration as increasingly stronger levels of inter-organizational partnership and identifies turf, time, and trust (the “3Ts”) as potential facilitators and barriers to partnership (Himmelman, 2002). The original framework was recently modified by the CDC to include a fifth level of partnership, merging (Division for Heart Disease and Stroke Prevention, 2016). We use this five-level classification in the present study and refer to it hereafter as the Collaboration Continuum.
Data Analysis
We used inductive and deductive thematic analysis (Miles & Huberman, 2013; Vaismoradi, Turunen, & Bondas, 2013) to identify types of partnership, facilitators and barriers to partnership, and strategies for overcoming barriers and supporting partnership development.
Two researchers read a sample of transcripts from each sector and developed an initial codebook that included several emergent codes as well as eight a priori codes based on the Collaboration Continuum: five partnership levels and three facilitators/barriers—time, trust, and turf. More detailed information about these concepts is presented in Table 1.
TABLE 1.
Description of Partnership Levels in the Collaboration Continuum (Division for Heart Disease and Stroke Prevention, 2016; Himmelman, 2002)
| Partnership Level (Level of Formality) | Activities | Primary Focus | Timea and Trustb | Shared Turfc | Shared Resources, Responsibilities, and Risks |
|---|---|---|---|---|---|
| Networking (informal) | Exchanging information | Exchanging information | Minimal | No | No |
| Coordination (formal) | Exchanging information and altering activities | Increasing accessibility to services and resources | Moderate | No | No or minimal |
| Cooperation (formal) | Exchanging information, altering activities, and sharing resources | Extensive sharing of resources, risks, responsibilities, and rewards | High | High | High |
| Collaboration (formal) | Exchanging information, altering activities, sharing resources, and enhancing each other’s capacity | Enhancing each other’s capacity for mutual benefit | Extensive | Extensive | Extensive |
| Merging/integration (formal) | Integrating information, activities, and resources to enhance each other’s capacity | Organizational restructuring to operate as one entity | Extensive | Full | Full |
Time refers to how much time an entity has to work on establishing, maintaining, and deepening partnerships.
Trust is the confidence one entity has in another to be reliable and do what is right.
Turf denotes an organization’s sphere of activity or influence.
Three researchers double-coded one transcript from each sector and discussed their coding until they reached consensus on code application. They considered the codebook complete when no new themes emerged and they agreed on code definitions. Two researchers then used Atlas.ti Version 7.5.18 (Scientific Software Development GmbH, 2017) to double-code sets of transcripts until they reached 80% intercoder agreement in each of the four organizational sectors (Miles & Huberman, 2013). They then divided the remaining transcripts for independent coding and checked four of their coding partner’s assigned transcripts (one transcript per sector) to ensure ongoing consistent coding. The researchers wrote analytic memos after coding each sector to help summarize main themes (Miles & Huberman, 2013).
We shared our findings with participants and gave them the opportunity to provide feedback (Tong et al., 2007). Participants did not indicate that any changes needed to be made in our interpretation of the findings. This process of member checking is used in qualitative research to help establish credibility of the study (Creswell & Miller, 2000).
RESULTS
Characteristics of Study Participants
We conducted 41 interviews with clinic staff (n = 10), CBO staff (n = 10), pharmacists (n = 10), and CHWs (n = 11). Interviews were one-on-one except one group interview with four community pharmacists working in a grocery store pharmacy and one group interview with two CBO staff, for a total of 45 participants. Participants were mostly White (n = 29) and female (n = 38) (Table 2). Clinic staff participants included seven physicians, two nurses, and one behavioral health specialist. The clinic staff came from regional hospital systems (n = 8), a small, free clinic (n = 1), and a federally qualified health center (n = 1). We interviewed nine pharmacists working in clinical settings in large, integrated hospital systems (n = 8), an educational institution (n = 1) (“clinical pharmacists”), and four community retail pharmacists working in a grocery store (“community pharmacists”). The CBO staff participants worked in public health-focused organizations (n = 5), other nonprofits (n = 3), and educational institutions (n = 2). The CHW participants worked in public health organizations (n = 5), low-income housing (n = 3), and other health-focused nonprofits (n = 3). Participants came from urban (n = 33) and rural (n = 8) settings across Western (n = 21), Southwest (n = 10), Central (n = 3), and Eastern Washington (n = 7).
TABLE 2.
Participant Demographic Characteristics, Washington State, December 2016–July 2017
| Demographic Characteristic | Clinic Staff | Pharmacists | CBO Staff | CHWs | Total |
|---|---|---|---|---|---|
| No. of interviews | 10 | 10 | 10 | 11 | 41 |
| No. of participants | 10 | 13 | 11 | 11 | 45 |
| Agea (years), M (SD) | 41.1 (12.2) | 35.9 (9.8) | 49.1 (14.3) | 58.4 (9.1) | 44.7 (14.1) |
| Genderb, n (%) | |||||
| Female | 7 (70.0) | 10 (76.9) | 11 (100.0) | 10 (90.9) | 38 (84.4) |
| Race or ethnicityc, n (%) | |||||
| Asian | 3 (30.0) | 3 (23.1) | 0 (0.0) | 0 (0.0) | 6 (13.3) |
| Black | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4 (36.4) | 4 (8.9) |
| Hispanic | 1 (10.0) | 0 (0.0) | 0 (0.0) | 1 (9.1) | 2 (4.4) |
| White | 6 (60.0) | 10 (76.9) | 9 (81.8) | 4 (36.4) | 29 (64.4) |
| Multiracial | 0 (0.0) | 0 (0.0) | 1 (9.1) | 1 (9.1) | 2 (4.4) |
| Educationd, n (%) | |||||
| High school | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (27.3) | 3 (6.7) |
| Bachelors | 1 (10.0) | 2 (15.4) | 6 (54.5) | 4 (36.4) | 13 (28.8) |
| Masters | 1 (10.0) | 0 (0.0) | 5 (45.5) | 1 (9.1) | 7 (15.6) |
| Doctoral or professional | 8 (80.0) | 11 (84.6) | 0 (0.0) | 0 (0.0) | 17 (37.8) |
| Missing education | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (27.3) | 3 (6.7) |
NOTE: CBO = community-based organization; CHWs = community health worker.
Missing age: Clinic staff 1, CBO staff 1, CHWs 3.
Missing gender: None.
Missing race or ethnicity: CBO staff 1, CHWs 1.
Missing education: CHWs 3.
Partnership Frequency and Levels Across Sectors
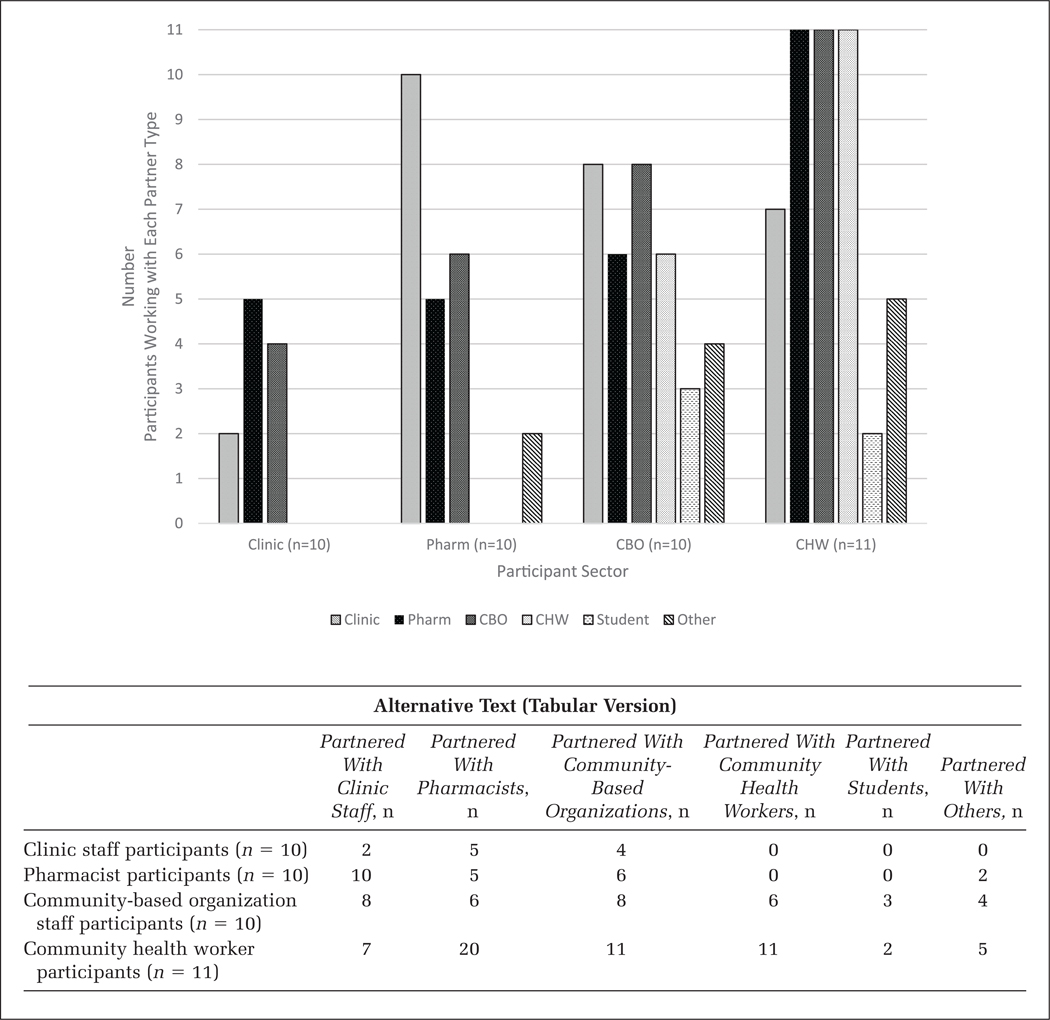
The number of partnerships that our participants reported varied substantially by sector (Figure 1). In addition to the four sectors from which we recruited, participants reported partnerships with health sciences students and their academic institutions (“Student”) and with organizations that have not traditionally played a role in delivering health services such as churches, low-income housing, laundromats, and barber shops (“Other”). Quotes that illustrate these partnerships are presented in Table 3, and examples from each sector are provided in Supplemental Table A1.
FIGURE 1. Partnership Frequency Distributions Among Organizations by Sector, Washington State, December 2016–July 2017.
NOTE: Clinic = clinics or clinic staff; Pharm = pharmacists; CBO = community-based organizations or their staff; CHW = community health worker; Student = students and their educational institutions; Other = organizations that have not traditionally played a role in delivering health services such as churches, low-income housing, laundromats, and barber shops. Interview participants from each sector identified the types of partners they were working with for blood pressure control. Clinic staff and pharmacists partnered with fewer partner types and less frequently than CBO staff and CHWs.
TABLE 3.
Levels of Collaboration, Facilitators and Barriers to Partnerships for Hypertension Management, Washington State, December 2016–July 2017
| Theme | Representative Quote |
|---|---|
| Collaboration Continuum level | |
| Networking | “It’s more of just sharing information [about our services] and gleaning [ways we can help] from the clinic.” (CBO partnering with a clinic) |
| Coordination | “We have a process where we work together to solve insurance reimbursement issues.” (Pharmacist partnering with clinic staff) |
| Cooperation | “It was resources from them that enabled us to purchase those blood pressure cuffs. We put them in the community health advocate kits so that the community members would have increased access to those cuffs, and so that they can do some monitoring and self-monitoring of their overall health.” (CBO staff partnering with a Public Health Organization and CHWs) |
| Collaboration | “They help provide the training, you know, and what to do with the readings that we got when we do the readings.” (CHW partnering with a CBO) |
| Merging | “Yes, I guess we have an integrated pharmacy residency here, but we actually have pharmacists here that predated that. We have pharmacists in all of the . . . outpatient clinics.” (Clinic staff partnering with pharmacists) |
| Collaboration Continuum barriers and facilitators | |
| Turf (barrier) | “Well, I mean, healthcare is a business, right? [. . .] There are a lot of clinics that wouldn’t want you to come in and tell them how to do stuff, because you’re basically their competition.” (CBO staff) |
| Turf (facilitator) | None |
| Time (barrier) | “I think that over the last few years with the Affordable Care Act and all of the changes that our medical providers have had to institute, they really have a full plate. I think that sometimes they just don’t want to have to think about something different to commit to.” (CBO staff) |
| Time (facilitator) | “The pharmacist is taking these lower acuity patients and opening up the doctor’s time to see the higher acuity patients that they get more reimbursement for and so it’s a very cost-effective system. [. . .] It’s a win-win.” (Pharmacist) |
| Trust (barrier) | “My role is new here. [. . .] I’ve been here a little over two years. I’ve had to establish myself—for one, gaining trust within the clinic. It’s not that they don’t trust pharmacists, but just kind of learning what can we do and how can we help with efforts with our patients. And then as things have kind of come on, they’ve recognized that wow, you can definitely help us with things.” (Pharmacist) |
| Trust (facilitator) | “Yes, if I don’t know a resource, I can call [name]. That’s my ‘reach out and touch you’ lady at the community advocate office in the health department. I can say, ‘I have a person that needs help with this. Do you have resources to help me?’ She will get into her bag of tricks and come up with something.” (CHW) |
| Emergent barriers and facilitators | |
| Electronic health records (EHR) (barrier) | “Well, electronic medical record changes are extremely, extremely expensive to make and very slow in coming. So even if we requested some kind of medical record change [. . .] it may happen months later, and there is a huge queue and a long list of people in various specialties that all have their wish list.” (Clinic staff) |
| Electronic health records (facilitator) | “We have a direct referral system in place [. . .] where we receive referrals directly from providers through their EHR. We have secure fax where we receive referrals to the program. I would say that those are probably the strongest relationships we have [between] the community and clinic.” (CBO staff) |
| Shared mission (barrier) | None |
| Shared mission (facilitator) | “Most of the organizations have the same—not the same, but their mission is on the same path. So then the more help that they can get [from other organizations and stakeholders] the better it is, and it lightens the load.” (CHW) |
| Awareness of community resources (barrier) | “I think that also in order for community partners to be involved, I think knowledge [is important], too. I don’t know what community organizations are doing to manage hypertension; what they’re doing to work with clinics or healthcare providers to do so.” (Clinic staff) |
| Awareness of community resources (facilitator) | “I feel like we have a good pulse on our community and so I feel like I do get those linkages a lot. I’m not sure that everybody would say that, but I don’t really have a problem. I feel like we make good connections and we could get in [i.e., partner with] other places.” (CBO staff) |
NOTE: CBO = community-based organization; CHWs = community health worker.
In comparison to all other sectors, clinic staff reported the fewest partnerships outside their sector to support blood pressure control (Figure 1). Clinic staff reported partnering with other clinics, pharmacists, and CBOs. Clinic staff mainly partnered at the extremes of the Collaboration Continuum: they had networking partnerships with pharmacists and CBOs (e.g., sharing information about community programming), coordination partnerships with pharmacists to resolve medication interactions and adherence issues, and merging partnerships with pharmacists integrated into care teams.
All pharmacists reported working with clinic staff and other pharmacists; many also reported partnering with CBOs. They engaged in networking and coordination often: they had networking partnerships with clinic staff in the form of informal patient information exchange (asking a question about a prescription or making a clarification), and coordination partnerships that included taking extra steps with clinics to mitigate insurance issues. Nine of the clinical pharmacists were integrated into care teams, an example of merging.
CBO staff and CHWs reported partnering with all sectors and at all levels of the Collaboration Continuum. For CBO staff, networking involved sharing flyers and brochures about their programs with clinics. They coordinated with CHWs and attended each other’s events and health fairs. Cooperation entailed sharing resources like blood pressure monitoring devices with other CBOs or CHWs. Collaboration included training CHWs on blood pressure measurement. For CHWs, networking occurred when they shared information about events they organized that pertained to blood pressure. An example of coordination was referring people with high blood pressure to clinics. Cooperation occurred through sharing resources with food banks. CHWs and public health organizations offered joint trainings and worked with nursing practicum students to run blood pressure screening events, examples of collaboration. Finally, CHWs were employed by CBOs to serve as liaisons between them and the community, an instance of merging.
Facilitators and Barriers to Partnership
Participants reported barriers for all three a priori themes of turf, time, and trust, but facilitators only for the themes of time and trust. We identified three additional emergent themes: electronic health records, shared mission, and awareness of community resources. We include representative quotes for each of these themes in Table 3.
Turf.
Participants from all sectors mentioned turf, or competition, as a barrier to partnerships for high blood pressure prevention and control. Clinic staff members, pharmacists, and CBO staff explained how primary care providers who were accustomed to having the authority to treat their patients as they saw fit, might view new treatment protocols as infringements on their turf. Despite acknowledging that pharmacists were being integrated more often into clinical settings than in the past and that they were sometimes leading evidence-based programs for chronic disease management, the community pharmacists still felt they may be stepping on other sectors’ “toes” when expanding into these new areas. CBO staff mentioned competition between community organizations and clinics that may be offering similar self-management programs. CHWs described being excluded from clinical systems because potential partners might prefer to work only with people in their own systems and keep things “in-house.”
Time.
Participants from all sectors mentioned lack of time as a barrier, acknowledging that they were very busy and could not devote the time needed to develop effective partnerships for blood pressure control across sectors. On the other hand, those who were engaged in partnerships noted that partnerships could save time. For instance, clinical pharmacists involved in team-based care mentioned how they were saving physicians’ time by using protocols to triage patients and providing care for less complicated cases.
Trust.
Many participants, notably pharmacists, CHWs, and CBO staff, mentioned trust as a factor affecting partnerships. Clinic and CBO staff mentioned that not all clinic staff trusted providers from CBO or CHW sectors unless they saw documentation of positive outcomes from patient involvement in community-based programming. Pharmacists that joined clinical teams felt they had to prove their worth and gain trust from clinic staff. Some CHWs reported that they did not feel trusted by community organizations or public health entities to measure community members’ blood pressure, although some had nursing degrees and years of health care experience. Some CHWs did not feel trusted by clinic staff because of their perception that clinics were resistant to partnering with them.
Electronic Health Records.
Participants stressed the importance of electronic health records (EHRs) for seamless referrals, communication, and for building trust and tracking outcomes. Clinic staff stated that the cost and time needed for incorporating additional providers and organizations into EHRs could hamper the development of new partnerships. CBO staff and CHWs noted that not being able to access EHRs in the field, where they were meeting with patients, was a barrier to partnering for appropriate care provision.
Shared Mission.
Most participants across sectors mentioned shared mission as a facilitator to partnership. A clinic staff member described working with pharmacists for the mutual goal of helping patients obtain their medications. A CBO staff member explained how mission alignment led to a new partnership with a housing provider. A CHW noted that it “lightened the load” to partner with organizations with similar goals and priorities.
Awareness of Community Resources.
All participants mentioned awareness of community resources as a facilitator, or lack thereof as a barrier, for partnership development. Some clinic staff members did not feel they had enough information about community resources for blood pressure control to make informed recommendations to patients about available community support.
Strategies
Participants suggested several strategies that the Washington DOH could implement to address barriers and foster partnership development. For example, they suggested that the Washington DOH could mitigate the barrier of turf by facilitating meetings between potential partners to help them understand their common goals, build trust, and raise awareness of each other’s resources. They also felt that if Washington DOH provided designated, adequate, and sufficiently flexible funding, this would allow them time to support clinical–community partnerships. Finally, participants requested assistance from Washington DOH in being able to access EHRs from community settings, sharing EHRs across software platforms, and community sector (e.g., CBOs, CHWs) inclusion in EHR reporting and referral systems.
DISCUSSION
This study examined partnerships for blood pressure control involving clinics, pharmacists, CBOs, and CHWs in Washington State. We identified facilitators and barriers to the development of partnerships, and strategies Washington DOH could implement to alleviate barriers.
We found variation across organizational sectors in frequency and intensity of partnerships, two measures related to efficiency and effectiveness of chronic disease management (Buckley et al., 2013). Clinic staff and pharmacists reported fewer partnerships than CBO staff and CHWs, and they reported mostly networking, coordination, and merging partnerships with other clinic staff or pharmacists. CBOs and CHWs described partnerships that occurred at each Collaboration Continuum level. These differences in intensity of partnership may be explained by a current emphasis on team-based care within clinical institutions in health care transformation efforts (Carter et al., 2011), perhaps leaving less capacity for engaging in partnerships outside of clinical systems. This represents a missed opportunity because community-based provider efforts to support patients’ blood pressure control outside clinic walls through lifestyle changes, self-monitoring, and medication adherence may be more effective if these efforts included strong support from clinical settings (Division for Heart Disease and Stroke Prevention, 2016).
This study contributes to the literature by examining partnerships across four very different sectors (clinic, pharmacy, CBOs, CHWs). Our results reinforce findings from previous literature about the importance of factors such as turf, time, trust, shared mission, awareness of community resources, and EHR technology for the development of clinical–community partnerships (Fishleder et al., 2018; Payán et al., 2017; Valaitis et al., 2018). However, our findings differ from previous research in a few notable ways. First, our study included a wider range of health care professions than other studies, including CBO staff and CHWs. Our study also expands on ideas for how EHR technology can support intersectoral partnerships. For example, Payán et al. (2017) highlight the need for more technological knowledge about EHR functionality and faster EHR updates to maintain progress throughout intersectoral program implementation. Fishleder et al. (2018) argue that improved infrastructure support for communication and referrals between clinical providers and community organizations could lead to higher efficiency, trust, and potentially increased patient adherence. Although these observations are echoed by our study’s participants, they also expressed the need for EHR access in community settings for easier referrals and outcomes tracking during events such as health fairs. Valaitis et al. (2018) examined primary care and public health partnerships and identified time, turf, EHR, and shared mission as factors influencing collaboration, similar to our findings, and noted that co-locating clinical and community organizations may facilitate communication, information exchange, and trust. However, our participants noted that trust remained a barrier even in the context of team-based care, suggesting that more work needs to be done to facilitate collaboration and integration across professional, as well as organizational, boundaries.
This study makes an additional important contribution to the literature by presenting strategies for overcoming barriers to partnership generated by study participants. First, creating opportunities for potential partners to come together and learn about each other’s programs and discuss shared mission and priorities could help improve trust and highlight the benefits of partnering. This may lead to an understanding that the work of clinical and community partners is complementary rather than competitive (Division for Heart Disease and Stroke Prevention, 2016). Such efforts are in place in Washington State and elsewhere in the form of Accountable Communities of Health, which address upstream social determinants of health through partnerships between clinical and community sectors, with the ultimate goal of improving health outcomes and reducing costs (Alley et al., 2016). Second, to facilitate partnership and continuity of care, participants stated the need for community partners to have the ability to use EHR systems for patient referral and tracking outcomes. While this solution has been proposed elsewhere in the literature (Association for the State and Territorial Health Officials, n.d.; Miller & West, 2007), its implementation may include a number of challenges. Privacy concerns may arise if, for example, CBO staff have access to patient medical records. However, these concerns could be addressed by providing HIPAA (Health Insurance Portability and Accountability Act) training to nonclinical staff and allowing them only limited access to patient EHRs (Miller & West, 2007). Current initiatives in this direction include the integration of chronic disease prevention program data by YMCAs into the AthenaNet EHR system to improve care coordination with clinical providers (Association for the State and Territorial Health Officials, n.d.).
This study’s novel use of the Collaboration Continuum, recently adopted by the CDC, allowed us to identify different levels of partnership intensity. Our study suggests that community–clinical linkages are not “one size fits all,” but can involve varying levels of intensity and resources that might be useful to practitioners as they explore intersectoral partnerships for chronic disease prevention and management. Community and clinical organizations that want to develop new partnerships may choose to start at the lower levels of the Collaboration Continuum, since networking and coordination require minimal or moderate levels of trust, time, and other resources. If these partnerships prove successful, they may eventually progress along the Continuum to higher levels such as collaboration and merging that require extensive resources and sharing of responsibilities and risks and may also be more likely to lead to substantial impact.
Our results have informed the design of a new initiative to improve partnerships for population-level blood pressure control in Washington State. Through funding from two CDC grants, Improving the Health of Americans through Prevention and Management of Diabetes and Heart Disease and Stroke (CDC-RFA-DP18–1815) and an Innovation Award for Heart Disease and Stroke (CDC-RFA-DP18–1817), Washington’s Reducing Cardiovascular Disease Initiative (RCDI) addresses cardiovascular disease through contracts with local health jurisdictions serving two different regions of the state. The structure of RCDI was designed based on our findings, and the initiative aims to meet the request for designated, adequate, and sufficiently flexible funding to support building and sustaining clinical–community partnerships. Launched in January 2019, RCDI focuses on increasing awareness of community resources, increasing use of electronic systems that connect CHWs and clinical staff, and increasing trust and reducing turf issues by funding multisector projects with common outcomes.
This study had several limitations. Because of the qualitative design, snowball sampling, sample size, and geographical boundaries, the characteristics of our participants may not be representative or generalizable to other states. Also, location of the study participants may have influenced the number and types of partnerships reported. For example, in a rural community that may have fewer resources, more partnerships may develop. We did not have enough variation in our sample to be able to compare rural and urban settings, but further research could elucidate these differences. Additionally, an underreporting of turf and trust barriers may have occurred due to social desirability bias (Krumpal, 2011). While outside the scope of this study, patient perspectives should be included in future studies given the importance of patient-centered research (Domecq et al., 2014). Including patient perspectives could help elucidate which intersectoral partnerships would be most helpful in facilitating patient access to services that lead to adoption of lifestyle changes necessary for managing blood pressure and medication adherence
CONCLUSION
Partnerships between clinical and community organizations have the potential to improve outcomes for people with high blood pressure by increasing access to community resources that support lifestyle changes, medication adherence, and self-monitoring. Programs through federal agencies such as the CDC aim to promote the development of such partnerships, but significant barriers remain, particularly in the form of limited time, lack of adequate technology, clinical staff’s lack of awareness of community resources, and perceptions of mistrust and competition. Bringing potential partners together to discuss shared priorities and build awareness and trust, creating the technological infrastructure needed for seamless referrals, and incentivizing partnerships through sustained funding may help bridge clinical and community silos and improve blood pressure control at the population level.
Supplementary Material
Acknowledgments
Authors’ Note: We gratefully acknowledge our study participants and colleagues who recruited participants. We also acknowledge our colleague, Caitlin Mason, PhD, for reviewing a draft of this article. Ethical approval for this research was obtained from the University of Washington Institutional Review Board on October 27, 2016 (Study No. 00000178). This research was supported by the Grant or Cooperative Agreement Number, DP005531, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the U.S. Department of Health and Human Services (HHS). Recruitment of clinicians was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000423. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This project was supported by the Health Resources and Services Administration (HRSA) of the HHS. The information or content and conclusions are those of the author and should not be construed as the official position or policy of nor should any endorsements be inferred by HRSA, HHS, or the U.S. Government.
Footnotes
SUPPLEMENTAL MATERIAL
Supplemental material for this article is available online at https://journals.sagepub.com/home/hpp.
REFERENCES
- Alley DE, Asomugha CN, Conway PH, & Sanghavi DM (2016). Accountable health communities—Addressing social needs through Medicare and Medicaid. New England Journal of Medicine, 374, 8–11. doi: 10.1056/nejmp1512532 [DOI] [PubMed] [Google Scholar]
- Association for the State and Territorial Health Officials. (n.d.). State learning collaborative to improve blood pressure control. Retrieved from http://www.astho.org/Million-Hearts/State-Learning-Collaborative-to-Improve-Blood-Pressure-Control/?terms=Facilitators+and+barriers+to+accelerating+SMBP+nationally
- Barnes PA, & Curtis AB (2009). A national examination of partnerships among local health departments and faith communities in the United States. Journal of Public Health Management and Practice, 15, 253–263. doi: 10.1097/01.phh.0000349740.19361.ac [DOI] [PubMed] [Google Scholar]
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, . . . Muntner P (2018). Correction to: Heart disease and stroke statistics—2018 update: A report from the American Heart Association. Circulation, 137, e493. doi: 10.1161/cir.0000000000000573 [DOI] [PubMed] [Google Scholar]
- Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L, Zhang X, & Satterfield D (2007). Effectiveness of community health workers in the care of people with hypertension. American Journal of Preventive Medicine, 32, 435–447. doi: 10.1016/j.amepre.2007.01.011 [DOI] [PubMed] [Google Scholar]
- Buckley DI, McGinnis P, Fagnan L, Mardon R, Johnson M, & Dymek C (2013). Clinical-community relationships evaluation roadmap. Retrieved from Agency for Healthcare Research and Quality website: https://www.ahrq.gov/professionals/prevention-chronic-care/resources/clinical-community-relationships-eval-roadmap/index.html
- Carter BL, Bosworth HB, & Green BB (2011). The hypertension team: The role of the pharmacist, nurse, and teamwork in hypertension therapy. Journal of Clinical Hypertension, 14, 51–65. doi: 10.1111/j.1751-7176.2011.00542.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014). Technical assistance guide: States implementing community health worker strategies. Retrieved from https://www.cdc.gov/dhdsp/programs/spha/docs/1305_ta_guide_chws.pdf
- Centers for Disease Control and Prevention. (2017). Hypertension prevalence and control among adults: United States , 2015–2016 (NCHS data briefs No. 289). Retrieved from https://www.cdc.gov/nchs/products/databriefs/db289.htm [PubMed]
- Centers for Disease Control and Prevention. (2018, February 28). State and local public health actions program. Retrieved from https://www.cdc.gov/dhdsp/programs/spha/
- Coleman K, Austin BT, Brach C, & Wagner EH (2009). Evidence on the chronic care model in the new millennium. Health Affairs, 28(1), 75–85. doi: 10.1377/hlthaff.28.1.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW, & Miller DL (2000). Determining validity in qualitative inquiry. Theory Into Practice, 39, 124–130. doi: 10.1207/s15430421tip3903_2 [DOI] [Google Scholar]
- Division for Heart Disease and Stroke Prevention. (2016). Community-clinical linkages for the prevention and control of chronic diseases: A practitioner’s guide. Retrieved from Centers for Disease Control and Prevention website: https://www.cdc.gov/dhdsp/pubs/docs/ccl-practitioners-guide.pdf
- Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, . . . Murad MH (2014). Patient engagement in research: A systematic review. BMC Health Services Research, 14, 2025–2047. doi: 10.1186/1472-6963-14-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J, Ayala C, & Loustalot F (2015). Primary care providers’ recommendations for hypertension prevention, DocStyles Survey, 2012. Journal of Primary Care & Community Health, 6, 170–176. doi: 10.1177/2150131915568997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishleder S, Petrescu-Prahova M, Harris JR, Steinman L, Kohn M, Bennett K, & Helfrich CD (2018). Bridging the gap after physical therapy: Clinical–community linkages with older adult physical activity programs. Innovation in Aging, 2(1). doi: 10.1093/geroni/igy006. Retrieved from https://academic.oup.com/innovateage/article/2/1/igy006/4965891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelman AT (2002). Collaboration for a change: Definitions, decision-making models, roles, and collaboration process guide. Retrieved from https://depts.washington.edu/ccph/pdf_files/4achange.pdf [Google Scholar]
- Hyman DJ, & Pavlik VN (2000). Self-reported hypertension treatment practices among primary care physicians. Archives of Internal Medicine, 160, 2281–2286. doi: 10.1001/archinte.160.15.2281 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Committee on Public Health Priorities to Reduce and Control Hypertension in the U.S. Population (2010). A population-based policy and systems change approach to prevent and control hypertension. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Kravetz JD, & Walsh RF (2016). Team-based hypertension management to improve blood pressure control. Journal of Primary Care & Community Health, 7, 272–275. doi: 10.1177/2150131916645580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumpal I (2011). Determinants of social desirability bias in sensitive surveys: A literature review. Quality & Quantity, 47, 2025–2047. doi: 10.1007/s11135-011-9640-9 [DOI] [Google Scholar]
- Margolius D, Bodenheimer T, Bennett H, Wong J, Ngo V, Padilla G, & Thom DH (2012). Health coaching to improve hypertension treatment in a low-income, minority population. Annals of Family Medicine, 10, 199–205. doi: 10.1370/afm.1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall MN (1996). Sampling for qualitative research. Family Practice, 13, 522–526. doi: 10.1093/fampra/13.6.522 [DOI] [PubMed] [Google Scholar]
- Miles MB, & Huberman AM (2013). Qualitative data analysis an expanded sourcebook (3rd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Miller RH, & West CE (2007). The value of electronic health records in community health centers: Policy implications. Health Affairs, 26, 206–214. doi: 10.1377/hlthaff.26.1.206 [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, . . . Turner MB (2014). Heart disease and stroke statistics-2015 update. Circulation, 131, e29–e322. doi: 10.1161/cir.0000000000000152 [DOI] [PubMed] [Google Scholar]
- Payán DD, Sloane DC, Illum J, Vargas RB, Lee D, Galloway-Gilliam L, & Lewis LB (2017). Catalyzing implementation of evidence-based interventions in safety net settings: A clinical–community partnership in South Los Angeles. Health Promotion Practice, 18, 586–597. doi: 10.1177/1524839917705418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porterfield DS, Hinnant LW, Kane H, Horne J, McAleer K, & Roussel A (2012). Linkages between clinical practices and community organizations for prevention: A literature review and environmental scan. American Journal of Public Health, 102(Suppl. 3), S375–S382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scientific Software Development GmbH. (2017). Atlas.ti Version 7.5.18. Berlin, Germany: Author. [Google Scholar]
- Sloane PD, & Ebell MH (2007). Introduction to common problems In Sloane PD, Slatt LM, Ebell MH, Jacques LB, & Smith MA (Eds.), Essentials of family medicine (5th ed., pp. 119–130). Hagerstown, MD: Lippincott Williams & Wilkins. [Google Scholar]
- Thomas KL, Shah BR, Elliot-Bynum S, Thomas KD, Damon K, Allen LaPointe NM, . . . Peterson ED (2014). Check it, change it: A community-based, multifaceted intervention to improve blood pressure control. Circulation: Cardiovascular Quality and Outcomes, 7, 828–834. doi: 10.1161/circout-comes.114.001039 [DOI] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, & Craig J (2007). Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19, 349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Trust for America’s Health. (2016). CDC State and Local Public Health Actions to Prevent Obesity, Diabetes, and Heart Disease and Stroke (DP14–1422PPHF14) fact sheet and community profiles. Retrieved from https://www.tfah.org/wp-content/uploads/2018/02/1422.pdf
- United Health Foundation. (2019). Explore high blood pressure in Washington: 2018 annual report. Retrieved from https://www.americashealthrankings.org/explore/annual/measure/Hypertension/state/WA
- Vaismoradi M, Turunen H, & Bondas T (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing & Health Sciences, 15, 398–405. doi: 10.1111/nhs.12048 [DOI] [PubMed] [Google Scholar]
- Valaitis R, Meagher-Stewart D, Martin-Misener R, Wong ST, MacDonald M, & O’Mara L (2018). Organizational factors influencing successful primary care and public health collaboration. BMC Health Services Research, 18(1). doi: 10.1186/s12913-018-3194-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington State Department of Health. (2018). 2018 Washington State Health Assessment. Retrieved from https://www.doh.wa.gov/Portals/1/Documents/1000/SHA-CoronaryHeartDiseaseandHypertension.pdf
- Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, . . . Wright JT (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Journal of the American College of Cardiology, 71, e127–e248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.