Abstract
Objective
Individuals with post-traumatic stress disorder (PTSD) who experience additional traumas or stressful life events may undergo symptomatic worsening, but no data exist on whether exposure to the COVID-19 pandemic in a high infection area worsens mental health among older adults with chronic PTSD.
Methods
Seventy-six older adults (N = 46 with PTSD and N = 30 trauma-exposed comparison subjects [TE]) for whom prepandemic data were available were interviewed between April 1 and May 8, 2020 to quantify depressive (Hamilton Rating Scale for Depression [HRSD]) and PTSD symptom (Post-traumatic Stress Disorder Checklist [PCL-5]) levels. Group differences in baseline characteristics as well as pre-post pandemic symptom levels were examined, and participant characteristics were assessed as moderators of symptom change.
Results
Compared to TEs, individuals with PTSD more often reported living alone and experiencing a physical illness (χ2 = 5.1, df = 1, p = 0.02). PCL-5 scores among individuals with PTSD decreased during the COVID-19 pandemic by 7.1 points (t(69) = -3.5, p = 0.0008), whereas the TE group did not change significantly. Overall no significant differences in HRSD were found between groups, but a race or ethnicity variable was found to moderate HRSD symptom change. Non-black or Hispanic individuals with PTSD experienced significantly increased HRSD scores during the pandemic compared to black or Hispanic PTSD participants.
Conclusion
The findings are indicative of complexity in the responses of older individuals with PTSD to further stressful life events as well as possibly unique aspects to the COVID-19 pandemic as a stressor. Sources of resilience may exist based on experience with prior traumas as well as increasing age promoting more adaptive coping styles.
Key Words: COVID-19, post-traumatic stress disorder, loneliness, older adult
INTRODUCTION
After an index trauma, individuals with post-traumatic stress disorder (PTSD) are thought to be vulnerable to increased symptomatology following additional traumatic and stressful events. Compared to controls, older adult Holocaust survivors subjected to additional trauma experienced increased intrusive thoughts and hyperarousal symptoms related to the reactivation of traumatic memories.1 Traumatized refugees with pre-existing PTSD have been shown to experience an increase in symptoms and comorbid psychiatric disorders following an additional traumatic experience.2 Some data suggest that symptom-inciting events need not only be those meeting Diagnostic and Statistical Manual (DSM) criterion A3 for an additional trauma, but also may be non-traumatic but nonetheless stressful life events.4
It has been broadly anticipated that the spread of the novel coronavirus SARS-CoV-2 and its associated disease (designated COVID-19), as well as social distancing and stay-at-home orders instituted to mitigate spread of the pandemic, may be experienced by vulnerable individuals as a traumatic stressor.5 , 6 Past experience with disasters of various types (terrorist attacks, natural, and environmental) has been associated with increased depressive and anxiety (including PTSD) symptoms as well as substance misuse.7 In particular, individuals with mood and anxiety disorders may be at risk of recurrent or worsening symptoms resultant from diminished social engagement, loneliness, and prolonged exposure to social isolation.8 Additionally, the advent of 24 into 7 news cycles may serve to worsen the traumatic exposure, as recent studies suggest repeated media exposure to large-scale crises can lead to increased anxiety and heightened stress responses.9 , 10 Despite their intuitive appeal, these hypotheses remain untested, and mental health effects of the COVID-19 pandemic on vulnerable populations such as individuals with PTSD are unknown at this time.
Older individuals and those who are racial or ethnic minorities are at increased risk for adverse medical outcomes associated with COVID-19,11 , 12 but whether they also may be subject to increased mental health risks associated with the pandemic is unclear. On the one hand, natural disasters and public health crises can disrupt essential services for community-dwelling older adults, such as assistance from family caregivers, home-delivered meals, and personal care.13 More than a third of adults over 65 years old live alone,14 and the majority have multiple chronic medical conditions and/or sensory deficits (vision and hearing loss) that limit daily activities and may interfere with the ability to prepare for and respond to large-scale disruptions in their usual lives.15 It is feared that stay-at-home orders may cause older adults to lose their usual ways to connect with support networks, health providers, exercise and social activities, and volunteer and employment opportunities, thereby contributing to increased loneliness.16 On the other hand, following the 2004 hurricanes in Florida, older individuals had lower rates of PTSD, other anxiety disorders, and Major Depressive Disorder compared to younger adults.17 A survey of metropolitan New York City area residents in the aftermath of the September 11, 2001 terrorist attacks found that cumulative prevalence rates of PTSD and depression were lower (12.2% and 10.6%, respectively) in the cohort aged 55 and above compared to the 18–54 age groups (28.8% and 27.2%).18 Other studies suggest that even the clinical presentation of trauma-related distress appears less intense in older adults compared to younger populations.19
A typical methodologic challenge in assessing postdisaster change in mental health symptoms is a lack of measurements performed prior to the stressor, so whether postmeasurements indicate a change in baseline among the individuals studied is unknown. Since the fall of 2017, we have been conducting a study of brain aging among individuals with PTSD aged 50 and older as well as trauma-exposed healthy comparison subjects (TE). This study, being conducted in New York City, involves a comprehensive assessment of PTSD and TE participants in terms of mental health symptoms and current functioning, which provided an appealing population in whom to study change in mental health following the beginning of the COVID-19 pandemic. Therefore, we contacted currently enrolled individuals for participation in a telephone survey and queried willing individuals in regard to their exposure to the SARS-CoV-2 virus and social distancing policies, levels of depressive and PTSD symptoms, substance use, and degrees of social isolation and loneliness. Given the above risks posed by the COVID-19 pandemic, particularly to those who may be vulnerable on the basis of age, race, or ethnicity, we hypothesized that older adults with chronic PTSD would experience greater symptomatic increases and a higher degree of social isolation or loneliness compared to TEs.
METHODS
Study Design
Data were collected from participants in a larger ongoing study examining the influence of chronic PTSD on biological aging processes in older adults. All individuals completing the parent protocol by March 13, 2020 were eligible for participation in this study. Having previously given permission to be approached for future research studies, potential participants were contacted via telephone by study staff between April 1 and May 8, 2020. Those who indicated their interest in participation and signed informed consent were given a telephone or videoconference interview date at their convenience. All study procedures were approved by the New York State Institutional Review Board.
Subjects
For the ongoing study from which participants in this survey were recruited, PTSD patients were men and women aged ≥50 years old who were currently diagnosed with DSM5 PTSD using the Structured Clinical Interview for DSM-5. They additionally had PTSD duration at least 6 months, Post-traumatic Stress Disorder Checklist (PCL-5) score ≥33, Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) score ≥25, and were willing to and capable of providing informed consent and complying with study procedures. Individuals were excluded for past or current diagnosis with traumatic brain injury, bipolar disorder, psychotic disorder, or dementia, severe Alcohol or Cannabis Use Disorder or any other Substance Use Disorder except Nicotine, current treatment with mood stabilizers or antipsychotic medications, Mini Mental State Examination (MMSE) <25, acute, unstable, or severe medical disorder, and contraindication to magnetic resonance imaging (magnetic resonance imaging scan was a separate portion of study).
In addition, trauma-exposed healthy comparison subjects (TE) were recruited who were men and women aged ≥50 years old, exposed to trauma, and willing to and capable of providing informed consent and complying with study procedures. TE subjects were excluded based on personal history of traumatic brain injury, current or past DSM 5 disorder, or PTSD diagnosed in a first degree relative, current treatment with psychotherapy or psychotropic medications such as antidepressants, mood stabilizers, antipsychotic, or sedative or hypnotic medications, past or current diagnosis of dementia or MMSE <25, Hamilton Rating Scale for Depression (HRSD) >7, CAPS-5 ≥10, in addition to magnetic resonance imaging exclusion criteria.
All participants resided in the New York City metropolitan area within driving or public transportation distance to Columbia University Irving Medical Center.
Measurement of COVID-19 Impact
A semistructured interview was performed to quantify participants’ exposure to the COVID-19 pandemic. Respondents were queried as to their personal and familial medical exposure to the novel coronavirus (COVID diagnosis, hospitalization, mechanical ventilation), participation in New York State on PAUSE (e.g., need to self-quarantine, days since left house), consumption of media reports on the pandemic (television, smartphone, other online), access to healthcare resources (primary doctor, specialists, medication), and social support or engagement (members of household, time spent speaking with family or friends).
Clinical Assessments
Data were available from the parent protocol (i.e., pre-COVID-19 pandemic) on participant demographics (age, sex, gender, marital status, race or ethnicity, years of education, employment status, and income), chronic medical illness burden (Cumulative Illness Rating Scale-Geriatric [CIRS-G]), PTSD symptom severity (Post-traumatic Stress Disorder Checklist [PCL-5], and CAPS-5), trauma type (Life Events Checklist for DSM 5 [LEC-5]), general anxiety symptoms (Hamilton Anxiety Rating Scale), depressive symptoms (24-item HRSD) and Inventory of Depressive Symptoms—Self Report), and global functioning (Clinical Global Impressions [Clinical Global Impressions Severity and Improvement] and World Health Organization Disability Assessment Schedule 2.0). Cognition was assessed using the 30-item MMSE, and physical function was assessed via a measure of weekly kilocalories (kcal) derived from the 18-item Minnesota Leisure Time Physical Activity Questionnaire and the Short Physical Performance Battery (SPPB).
Repeat assessments performed remotely during the COVID-19 pandemic included the 24-item HRSD, PCL-5, Minnesota Leisure Time Physical Activity Questionnaire, and Drug/Alcohol Timeline Followback Assessment of recent substance use. Further assessments newly added at the time of the COVID-19 survey to quantify psychosocial effects of the pandemic were the UCLA Loneliness Scale, Perceived Stress Scale, Pittsburgh Sleep Quality Index, Duke Social Support Index, and GAD 7.
Data Analyses
Descriptive statistics for baseline clinical and demographic variables between PTSD and TE subjects were calculated using frequencies, means, and standard deviations. For skewed distributions, medians and interquartile range were computed. Group differences were examined using χ2 (and Fisher's exact tests, when appropriate) and independent samples t tests (and Mann-Whitney U tests for skewed distributions).
To examine the association of PTSD status (PTSD versus TE) on pandemic-related change in psychiatric symptoms (HRSD, PCL-5), physical activity, and substance use (alcohol, cannabis), generalized linear mixed models for each outcome were fit, with a random effect for time and an unstructured covariance structure to account for within-subject correlation. A linear link function was used for the psychiatric symptoms and physical activity outcomes, and a logistic link function for the substance use outcomes. All models included the effect of time (pre- versus postpandemic), group (PTSD versus TE), and group by time interaction, and adjusted for the covariates of age, race or ethnicity (black or Hispanic versus not black or Hispanic), cognitive status (MMSE total score), physical functioning (SPPB score), and medical comorbidity (CIRS-G score).
Additionally, we explored whether black or Hispanic race or ethnicity, older age, increased medical comorbidity (CIRS-G score), or decreased physical functioning (SPPB score) represented specific vulnerability factors for HRSD and PCL-5 worsening during the COVID-19 pandemic. The three-way interactions of group by time by moderator were tested for each of these four potential moderators. If the three-way interaction term was significant, contrasts were performed to compare pre-post change between PTSD and TE groups stratified by the moderator variables.
All tests were performed at two-tailed significance level of 5%.
RESULTS
Baseline Subject Characteristics Prior to the COVID-19 Pandemic
Seventy-six completers to date in the parent protocol (N = 46 PTSD, N = 30 TE) could be reached by telephone within the study time frame and agreed to participate. As shown in Table 1 , PTSD participants were significantly younger than TEs (62.5 ± 9.0 versus 67.4 ± 9.4 years of age; t = -2.3, df = 74, p = 0.025) and demonstrated significantly higher symptom severity as judged by rater-administered measures and self-reported PTSD, anxiety, and depressive symptoms. Despite being on average 5 years younger, PTSD subjects as compared to TEs had significantly higher disability scores on the World Health Organization Disability Assessment Schedule 2.0 (median(interquartile range) = 74 (63–90) versus 40 (37–49); U = 577.5, p <0.001). The sample overall was 53.9% male, 63.2% white, 30.3% black, and 13.1% Hispanic, with no significant differences on these demographic variables between groups.
TABLE 1.
Demographics and Pre-COVID-19 Clinical Characteristics of Sample
| PTSD (N = 46) |
TE (N = 30) |
Comparison |
|||
|---|---|---|---|---|---|
| Characteristic | N (%) | χ2 | df | p | |
| Male | 21 (45.7) | 20 (66.7) | 3.23 | 1 | 0.07 |
| Fisher's Exact Test | |||||
| Race | 0.69 | ||||
| Asian | 1 (2.2) | 0 | |||
| Black | 13 (28.3) | 10 (33.3) | |||
| >1 race | 1 (2.2) | 0 | |||
| Other | 3 (6.5) | 0 | |||
| White | 28 (60.9) | 20 (66.7) | |||
| Ethnicity | 0.078 | ||||
| Hispanic/Latino | 9 (19.6) | 1 (3.3) | |||
| Not Hispanic/Latino | 37 (80.4) | 29 (96.7) | |||
| LEC-5 trauma type | 0.15 | ||||
| Combat | 7 (15.2) | 1 (3.3) | |||
| Noncombat interpersonal | 27 (58.7) | 16 (53.3) | |||
| Noninterpersonal | 12 (26.1) | 13 (43.3) | |||
| Alcohol use (≥1 drink per week) | 16 (34.8) | 13 (43.3) | 0.478 | ||
| Cannabis use (≥once per week) | 6 (13.0) | 1 (3.3) | 0.234 | ||
| Mean ± SD | t | df | p | ||
| Age | 62.5 ± 9.0 | 67.4 ± 9.4 | −2.3 | 74 | 0.025 |
| Median (Interquartile Range) | U | p | |||
| Cumulative Illness Rating Scale-Geriatric (CIRS-G) | 4 (0–8) | 3 (1–4) | 1013.5 | 0.13 | |
| PTSD Checklist for DSM5 (PCL-5) | 42 (36–51) | 8 (0–15) | 477.5 | <0.001 | |
| Clinician-Administered PTSD Scale for DSM5 (CAPS-5) | 32.5 (27–41) | 1.5 (0–7) | 470.5 | <0.001 | |
| Hamilton Anxiety Rating Scale (HARS) | 16 (8–24) | 3.5 (0–6) | 679.5 | <0.001 | |
| Hamilton Rating Scale for Depression (HRSD) | 17 (8–24) | 2 (0–4) | 655.5 | <0.001 | |
| Inventory for Depressive Symptomatology-Self Report (IDS-SR)* | 33 (23–40) | 10 (4–15) | 535.5 | <0.001 | |
| Mini-Mental Status Examination (MMSE)* | 29 (28–30) | 29 (28–30) | 1195 | 0.660 | |
| World Health Organization Disability Assessment Schedule (WHODAS2.0) | 74 (63–90) | 40 (37–49) | 577.5 | <0.001 | |
| Short Physical Performance Battery (SPPB) | 10 (9–11) | 11 (10–12) | 1331.5 | 0.055 | |
| Minnesota Leisure Time Physical Activity Questionnaire (kcal/wk) | 1302.3 (469.5–2923.9) | 1713 (622.6–2790) | 1230.5 | 0.425 | |
For IDS-SR, the final N = 74 (one subject is missing from the PTSD group and 1 from the TE group).
U: Mann-Whitney U test statistic; PTSD: post-traumatic stress disorder; TE: trauma-exposed healthy comparison group.
Exposure to COVID-19 Infection and Social Distancing
As shown in Table 2 , significantly more PTSD subjects compared to TEs reported living alone (63.0% versus 36.7%; χ2 = 5.1, df = 1, p = 0.02). Both groups of participants reported spending approximately 2 hours per day watching television news reports, though there were indications PTSD subjects spent more time overall viewing smartphone, computer, or television screens (U = 961.5, p = 0.050). Respondents’ reported loneliness (UCLA Loneliness Scale) and Perceived Stress Scores did not differ significantly by group. Thirty out of 46 (65.2%) PTSD patients compared to 19/30 (63.3%) TEs had UCLA Loneliness Scale scores indicating the presence of significant loneliness (i.e., >25).
TABLE 2.
Social and Interpersonal Effects of Stay-at-Home Orders in New York
| PTSD (N = 46) |
TE (N = 30) |
Comparison |
|||
|---|---|---|---|---|---|
| Characteristic | N (%) | χ2 | df | p | |
| Became ill during pandemic | 17 (37.0) | 4 (13.3) | 5.1 | 1 | 0.02 |
| Formally diagnosed COVID | 0 | 1 (3.3) | Fisher's exact test | 0.39 | |
| Hospitalized | 1 (2.2) | 0 (0.0) | Fisher's exact test | 0.12 | |
| Reports able to access doctors | 36 (78.3) | 18 (60.0) | 2.9 | 1 | 0.09 |
| Living alone | 29 (63.0) | 11 (36.7) | 5.1 | 1 | 0.02 |
| Mean ± SD | t | df | p | ||
| UCLA Loneliness Scale | 20.6 ± 12.9 | 19.5 ± 13.0 | 0.34 | 62 | 0.74 |
| Perceived Stress Score | 18.0 ± 9.1 | 18.0 ± 10.8 | −0.01 | 55 | 0.99 |
| Duke Social Support | 26.8 ± 4.1 | 27.3 ± 3.8 | −0.62 | 66 | 0.54 |
| Median (Interquartile range) | U | p | |||
| No. days since left house | 1 (0–3) | 1 (0–3) | 1089.5 | 0.48 | |
| Hours per day watching newsa | 2 (1–4.5) | 2 (1–3) | 1043.0 | 0.29 | |
| Hours per day viewing screena | 4 (2–6) | 3 (1.5–4) | 961.5 | 0.05 | |
| Times per day speak with friends | 1 (1–2) | 2 (0.5–4) | 1241.5 | 0.36 | |
The final N = 75 (1 subject is missing from the PTSD group).
U: Mann-Whitney U test statistic; PTSD: post-traumatic stress disorder; TE: trauma-exposed healthy comparison group.
Significantly more PTSD subjects compared to TEs reported experiencing a physical illness during the pandemic (37.0% versus 13.3%; χ2 = 5.1, df = 1, p = 0.02), but only 1 subject was diagnosed with the novel coronavirus using the PCR diagnostic test. A large majority of all respondents (71.1%, not different by group) reported maintaining access to their doctors and healthcare professionals as needed during the pandemic.
Pandemic-Related Change in Psychiatric Symptoms, Physical Activity, and Substance Use
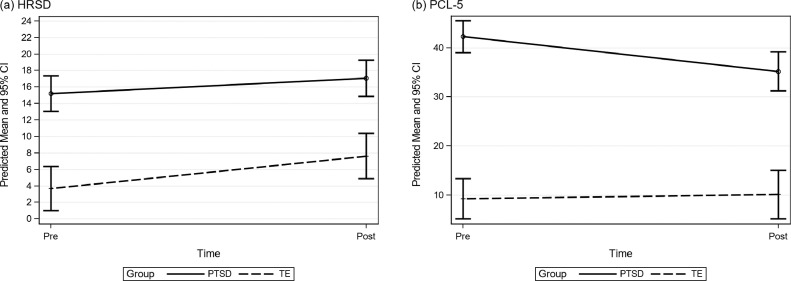
There was a significant group difference in the change in PCL-5 scores (group*treatment interaction F(1,69) = 6.14, p = 0.016), but the change was in the opposite direction originally hypothesized. Figure 1 b shows that in the PTSD group, average PCL-5 scores significantly decreased by 7.1 points (t(69) = -3.5, p = 0.0008), whereas in the TE group, PCL-5 scores remained low and did not change significantly during the pandemic (estimated mean change = 0.83, t(69) = 0.34, p = 0.74). None of the adjusted covariates were significant.
FIGURE 1.
Model-estimated means and 95% confidence intervals of (a) HRSD and (b) PCL-5 change pre- and post-COVID, adjusting for age, cognitive status, physical functioning, and medical comorbidity.
As shown in Figure 1a and Table 3 , both the PTSD and TE groups experienced a modest increase in HRSD scores during the pandemic, with the increase among TE subjects being statistically significant (estimated mean change = +3.9, t(69) = 2.29, p = 0.025). Contrary to our hypotheses, there were no significant group (PTSD versus TE) differences in the change in HRSD scores from prior to the pandemic to their reassessment during the COVID-19 pandemic (F(1,69) = 0.88, p = 0.352). None of the adjusted covariates were significant.
TABLE 3.
Adjusted Means and Standard Errors From Longitudinal Multiple Linear Regression Models, Adjusting for the Covariates of Age, Cognitive Status, Physical Functioning, and Medical Comorbidity for the Outcomes of Depressive and Post-traumatic Stress Disorder (PTSD) Symptoms
| HRSD | Adjusted Mean (SE) |
Within-Group Change |
Differential Change |
|||||
|---|---|---|---|---|---|---|---|---|
| Group | Pre | During | Change Score | t Value | p | Adj M (SE) | t Value | p |
| PTSD | 15.21 (1.09) | 17.08 (1.12) | 1.87 (1.38) | 1.35 | 0.181 | −2.06 (2.20) | −0.94 | 0.352 |
| TE | 3.68 (1.37) | 7.62 (1.40) | 3.93 (1.71) | 2.29 | 0.025 | |||
| PCL-5 | Adjusted Mean (SE) |
Within-Group Change |
Differential Change |
|||||
|---|---|---|---|---|---|---|---|---|
| Group | Pre | During | Change Score | t Value | p | Adj M (SE) | t Value | p |
| PTSD | 42.27 (1.65) | 35.2 (2.02) | −7.07 (2.00) | −3.53 | 0.0008 | 7.90 (3.19) | −2.48 | 0.016 |
| TE | 9.29 (2.09) | 10.13 (2.53) | 0.83 (2.48) | 0.34 | 0.7379 | |||
There were no significant group (PTSD versus TE) differences in the change in physical activity levels (F(1,69) = 0.09, p = 0.76), dichotomized alcohol use (0 versus ≥1 drink weekly; F(1,69) = 1.15, p = 0.29), or dichotomized cannabis use (0 versus ≥1 use weekly; F(1,69) = 1.0, p = 0.32) scores from prepandemic to their reassessment during the COVID-19 pandemic, while adjusting for covariates.
Moderator Analyses of Group Effects on Psychiatric Symptoms
Moderator analyses revealed a significant three-way interaction of group by time by race or ethnicity (F(1,68) = 5.29, p = 0.0245) for HRSD scores. Contrasts showed that the adjusted average HRSD scores significantly increased by 4.8 points (t(68) = 2.66, p = 0.0097) among non-black or Hispanic PTSD subjects. This change was significantly different (t(68) = -2.42, p = 0.018) compared to black or Hispanic PTSD subjects, whose HRSD scores decreased on average 1.7 points (t(68) = -0.84, p = 0.40). HRSD scores increased by 6.2 points (t(68) = 2.25, p = 0.027) in black or Hispanic TE subjects, which was not significantly different compared to the increase of 2.6 points (t(68) = 1.26, p = 0.21) experienced by non-black or Hispanic TE subjects.
Results did not support disproportionate worsening in HRSD scores between older compared to younger subjects or based on higher or lower degrees of medical comorbidity or physical functioning. No significant moderators were found of the group effect on PCL-5 change scores.
DISCUSSION
As they entered the COVID-19 pandemic, this racially and ethnically diverse sample of older adults with chronic PTSD experienced high levels of depressive and anxiety symptoms compared to TEs. Moreover, PTSD participants were more socially isolated (nearly twice as likely to be living alone), experienced more physical illness during the reporting period, and had somewhat greater exposure to pandemic media coverage in terms of electronic screen viewing time. Despite these risk factors for adverse mental health consequences secondary to COVID-19 and the fact that significantly more PTSD participants actually became ill during the time period covered by this study, PTSD symptoms actually significantly declined among PTSD participants relative to TEs. Interestingly, while there were no overall group differences on HRSD change during the pandemic, PTSD subjects who were not racial or ethnic minorities experienced increased depressive symptoms compared to black or Hispanic PTSD participants.
These results raise interesting questions regarding to what extent the COVID-19 pandemic may function as a traumatic stressor capable of amplifying or retriggering symptoms among individuals exposed to a different trauma type earlier in their lives. Though national and international healthcare organizations,20 in addition to the popular media21 have warned of a “tsunami” of mental health problems resultant from COVID-19 and associated stay-at-home policies, it remains to be seen whether this will be the case. An alternative perspective that is consistent with the present findings is that catastrophic events have different, less severe, pathologic implications when they occur on a global scale to all citizens as compared to when they occur to specific individuals or groups. As individuals with mental health symptoms due to trauma often have cognitions relating to their specific propensity to attract catastrophic events,22 feeling part of a dominant group process in which danger exists for everyone may serve to normalize and assuage such patients’ painful sense of difference from others. In such a way, making assumptions about the mental health impact of global events may result in missed opportunities to understand human resilience.
Relatedly, rather than assuming (as we in fact hypothesized) that a diagnosis of PTSD would confer vulnerability, it may be asked whether a prior history of trauma or PTSD actually may provide protection against the development or worsening of depressive and anxiety symptoms during COVID-19. One might speculate that past traumatic experiences could help individuals contextualize and deal with negative events, particularly when those events are unrelated to the specific traumas that they earlier experienced. Whereas prior to the pandemic individuals with PTSD may have believed (or been informed by others) that their hypervigilant stance was abnormal and discordant with societal norms, during the pandemic such a position might be considered understandable and adaptive. Importantly, findings from this study did not provide evidence that stay-at-home orders facilitated avoidance behavior on the part of PTSD patients, making them less likely to encounter triggers and therefore report fewer symptoms. We found suggestive evidence that PTSD patients may have had greater exposure to the pandemic via spending more electronic screen time than TEs.
Despite increasing age being a risk factor for worse medical outcomes due to COVID-19, we did not find similar evidence for worse mental health outcomes among older compared to younger individuals. These data are consistent with large recent surveys that have reported no large increases in loneliness associated with stay-at-home orders during the COVID-19 pandemic.23 It is possible that resilience may be conferred on the basis of maturational changes in emotion processing, as older adults with PTSD may benefit from greater wisdom and more adaptive coping styles.24 Compared to younger adults, older individuals have fewer negative emotional experiences, are less likely to report unhappiness, and feel a greater sense of well-being.25 As the life course progresses, negative affect decreases,26 positive affect increases or remains stable,27 and the incidence and prevalence of depression and anxiety disorders are generally reduced.28 In support of this interpretation, we recently reported that 73 community-dwelling elders with pre-existing Major Depressive Disorder showed similar resilience during the first 2 months of the COVID-19 pandemic.29 While these recently depressed individuals had concerns about the future, their level of symptomatology had not increased substantially compared to before the pandemic began.
Available evidence points to substantial health disparities in the impact of the COVID-19 pandemic in the United States, including higher rates of SARS-CoV-2 infections and death among African American and Hispanic individuals.30 , 31 Thus, we had anticipated that racial or ethnic minority status might be an additional source of vulnerability among PTSD patients, placing them at high risk for psychiatric symptom increases during the pandemic. This hypothesis was not supported by the moderator analyses conducted here, as black or Hispanic race and ethnicity appeared to confer resilience against depressive symptom increases among PTSD participants while being a risk factor for increased depressive symptoms in TEs. We note that some evidence suggests that greater community and religious support among African Americans may be a protective factor against depression compared to non-Hispanic whites.32 However, these findings must be interpreted with caution given the small size of our sample and the fact that we did not comprehensively assess these potentially protective variables.
Although this study benefits from important strengths, most notably including its characterization of a high-risk population and measurement of mental health status before and during the COVID-19 pandemic, there are significant limitations to consider. First, since this survey was conducted approximately 2 months into the COVID-19 experience in New York, an alternative interpretation is that these data were collected too early to capture a later-occurring rise in psychiatric symptomatology. It has been observed in disaster psychiatry that in the immediate aftermath of a crisis there can occur a “honeymoon” period during which communities come together and individuals experience enhanced well-being.33 Consistent with this alternative possibility is the separate, multicity evaluation of depressed older adults’ experiences during the COVID-19 pandemic mentioned above, where we found a similar resilience to stress among respondents and a stability of depressive symptoms.29 Relatedly, given the acuity of stressors facing respondents during the survey time period, the methods attempted to minimize the burden of participating in the study survey. As a result, the data collected were narrowly focused on symptom levels and social support to the exclusion of other interesting questions, such as the adverse economic impacts on participants by COVID-19, specific changes PTSD participants may have experienced in their mental health treatment, and positive alterations that may have influenced the resilience observed in older adults.
Second, the individuals surveyed in this study were not selected on the basis of random sampling of a population, but rather were participants in an ongoing study of PTSD and aging, which may have introduced a bias in the results. The requirement of a threshold PTSD symptom severity score at study entry specifically may have resulted in regression to the mean that contributed to the decline in PCL-5 scores noted among PTSD participants. Additionally, the sample size was relatively small, and social desirability factors may have influenced respondents’ answers to some questions, such as those regarding alcohol consumption. Given the exploratory nature of this survey, a number of comparisons and therefore statistical tests were performed, leading to the possibility of Type I error influencing the study results. Finally, while respondents with PTSD attributed the physical illnesses they reported to COVID-19 infection, at the time of this survey diagnostic testing was limited to individuals having a level of illness requiring hospitalization, so almost no subjects were formally tested for the novel coronavirus using the PCR diagnostic test.
In summary, results from this study raise intriguing questions about the response of older adults with PTSD to the stress associated with the COVID-19 pandemic and the stay-at-home orders imposed by New York state. Rather than it being the case that the pandemic per se is associated with increased symptomatology among this population, results from this study suggest that the specific characteristics and scale of the stressor (i.e., population-wide versus impacting selected groups or individuals) may influence its impact on individuals with PTSD. More research on older adults with PTSD is needed to determine how adaptive maturational changes in emotion processing as well as deleterious aging-associated processes such as cognitive decline influence older adults’ responses to further stressors.
AUTHORS’ CONTRIBUTIONS
Bret Rutherford designed the study, obtained funding, interpreted the data, and prepared this manuscript for publication. Ying Liu and Jean Choi played significant roles in the data analysis. Steven Roose, Rachel Yehuda, Janine Flory, Yuval Neria, and Patrick Brown made contributions to the conception of the study, acquisition of the data, and interpretation of the data. Marika Chrisanthopoulos, Chloe Salzman, Carlen Zhu, and Carolina Montes-Garcia played key roles in the data acquisition. All authors participated in drafting this manuscript, gave final approval of this version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
DISCLOSURE
Dr. Rutherford had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Rutherford, Liu, Brown, Yehuda, Flory, Neria, and Roose; Ms. Chrisanthopoulos, Salzman, Zhu, and Montes-Garcia; and Ms. Choi have no disclosures or conflicts of interest to report. This paper has not been previously presented.
This study was supported by funding from National Institute of Mental Health (NIMH) R01 MH111596 (Rutherford).
References
- 1.Fossion P, Leys C, Kempenaers C. Beware of multiple traumas in PTSD assessment: the role of reactivation mechanism in intrusive and hyper-arousal symptoms. Aging Ment Health. 2015;19:258–263. doi: 10.1080/13607863.2014.924901. [DOI] [PubMed] [Google Scholar]
- 2.Kinzie JD, Boehnlein JK, Riley C. The effects of september 11 on traumatized refugees: reactivation of posttraumatic stress disorder. J Nerv Ment Dis. 2002;190:437–441. doi: 10.1097/00005053-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . 5th ed. American Psychiatric Association; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 4.Schock K, Bottche M, Rosner R. Impact of new traumatic or stressful life events on pre-existing PTSD in traumatized refugees: results of a longitudinal study. Eur J Psychotraumatol. 2016:7. doi: 10.3402/ejpt.v7.32106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html. Accessed on November 1, 2020
- 6.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 7.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38:467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39:355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holman EA, Garfin DR, Lubens P. Media exposure to collective trauma, mental health, and functioning: does it matter what you see? Clin Psychol Sci. 2020;8:111–124. [Google Scholar]
- 11.Verity R, Okell LC, Dorigatti I. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hooper MW, Napoles AM, Perez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shih RA, Acosta JD, Chen EK. Improving disaster resilience among older adults: insights from public health departments and aging-in-place efforts. Rand Health Q. 2018;8:3. [PMC free article] [PubMed] [Google Scholar]
- 14.Komisar HL, Feder J, Kasper JD. Unmet long-term care needs: an analysis of Medicare-Medicaid dual eligibles. Inquiry. 2005;42:171–182. doi: 10.5034/inquiryjrnl_42.2.171. [DOI] [PubMed] [Google Scholar]
- 15.Aldrich N, Benson WF. Disaster preparedness and the chronic disease needs of vulnerable older adults. Prev Chronic Dis. 2008;5:A27. [PMC free article] [PubMed] [Google Scholar]
- 16.Berg-Weger M, Morley JE. Loneliness and social isolation in older adults during the Covid-19 pandemic: implications for gerontological social work. J Nutr Health Aging. 2020;24:456–458. doi: 10.1007/s12603-020-1366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Acierno R, Ruggiero KJ, Kilpatrick DG. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. Am J Geriatr Psychiatry. 2006;14:1051–1059. doi: 10.1097/01.JGP.0000221327.97904.b0. [DOI] [PubMed] [Google Scholar]
- 18.Neria Y, DiGrande L, Adams BG. Posttraumatic stress disorder following the September 11, 2001 terrorist attacks. Am Psychol. 2011;66:429–446. doi: 10.1037/a0024791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fontana A, Rosenheck R. Traumatic war stressors and psychiatric symptoms among World War II, Korean, and Vietnam War veterans. Psychol Aging. 1994;9:27–33. doi: 10.1037//0882-7974.9.1.27. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization (WHO).https://www.who.int/news-room/detail/14-05-2020-substantial-investment-needed-to-avert-mental-health-crisis. Accessed November 1, 2020
- 21.Roxby P: “Psychiatrists fear ‘tsunami’ of mental illness after lockdown,” BBC News online.https://www.bbc.com/news/health-52676981. Accessed November 1, 2020.
- 22.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- 23.Luchetti M, Lee JH, Aschwanden D. The trajectory of loneliness in response to COVID-19. Am Psychol. 2020;75:897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bangen KJ, Meeks TW, Jeste DV. Defining and assessing wisdom: a review of the literature. Am J Geriatr Psychiatry. 2013;21:1254–1266. doi: 10.1016/j.jagp.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carstensen LL, Pasupathi M, Mayr U. Emotional experience in everyday life across the adult life span. J Personal Soc Psychol. 2000;79:644–655. [PubMed] [Google Scholar]
- 26.Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: a theory of socioemotional selectivity. Am Psychol. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 27.Kryla-Lighthall N, Mather M. The role of cognitive control in older adults’ emotional well-being. In: Berngtson V, Gans D, Putney N, Silverstein M., editors. Handbook of Theories of Aging. 2nd ed. Springer Publishing; New York: 2009. pp. 323–344. [Google Scholar]
- 28.Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30:11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- 29.Hamm ME, Brown PJ, Karp JF. Experiences of American older adults with pre-existing depression during the COVID-19 pandemic: a multi-city, mixed-methods study. Am J Geriatr Psychiatry. 2020;28:934–942. doi: 10.1016/j.jagp.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 31.Moore JT, Ricaldi JN, Rose CE. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5–18, 2020—22 states, February–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1122–1126. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woodward AT, Taylor RJ, Abelson JM. Major depressive disorder among older African Americans, Caribbean African Americans, and non-Hispanic whites: secondary analysis of the National Survey of American Life. Depress Anxiety. 2013;30:589–597. doi: 10.1002/da.22041. [DOI] [PubMed] [Google Scholar]
- 33.Zunin LM, Myers D. 2nd ed. Center for Mental Health Services; Washington, DC: 2000. Training Manual for Human Service Workers in Major Disasters. [Google Scholar]