Abstract
Patients with cystic fibrosis (CF) have increased life span because of improved care over last 50 years. With increasing survival, predisposition of cancer may become evident. We have observed increase risk of gastrointestinal tract cancer, testicular cancer and lymphoid leukemia. Lung cancer in patients with CF is rare. Our patient developed chronic respiratory failure due to CF related bronchiectasis. Patient had progressive disease despite optimum treatment, requiring lung transplantation. Pathology of explant lung showed focus of invasive adenocarcinoma of lung origin. Patient had no evidence of lung carcinoma recurrence in one year. To our knowledge this is the fourth reported lung cancer case in a patient with CF.
Keywords: Cystic fibrosis, Lung carcinoma, Lung transplant
1. Introduction
Lung carcinoma, usually of the non–small-cell type, is one of the most common malignancies with increasing incidence worldwide [1,2]. It remains the leading cause of mortality from cancer in the United States [3]. The presence of lung cancer in the explanted lung either known or incidentally found at surgery presents an intriguing clinical problem [4]. Smoking especially more than 60 pack-years is significant risk factor for developing lung cancer [5]. Post-transplant, de novo lung carcinoma occurs predominantly in single lung transplantation, arises in most cases in the native lung as a consequence of tobacco exposure and other carcinogenic conditions, such as pulmonary fibrosis [6]. Cystic Fibrosis (CF), the most common genetic disorder in Caucasians, considered being low risk to have primary lung cancer. Previous studies observed a decrease in respiratory tract cancer of borderline significance [[7], [8], [9]].
2. Case report
A 58 year-old-man was diagnosed with CF during childhood with gastrointestinal involvement, later confirmed with sweat chloride test and genetic study. Patient's history is significant for recurrent spontaneous pneumothorax on right side treated with chest tube insertion at the age of 55 years. After the second episode of pneumothorax on same side about one week later, patient received mechanical pleurodesis and right upper lobe wedge resection. Post-surgery, patient had aggressive decline in exercise. Despite aggressive chest physiotherapy with oscillatory vest to enhance airway secretion clearance, bronchodilators, Dornase Alfa to reduce viscosity of secretions and inhaled antibiotics patient's clinical condition continued to decline. Further, patient's course was complicated by frequent lower respiratory tract infections with Pseudomonas aeruginosa and Staphylococcus aureus. Patient did not have a history of smoking or other forms of tobacco use. Patient's overall condition continued to decline over the next few years with worsening dyspnea. His need for supplemental oxygen was increased with activities of daily living.
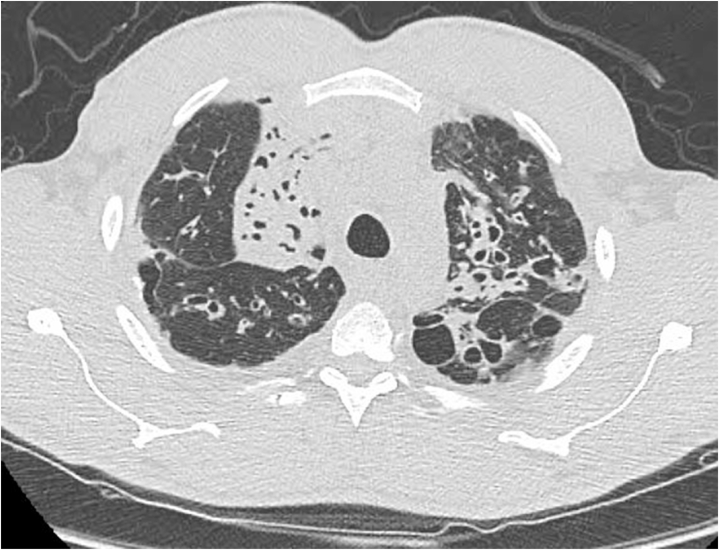
Patient was referred for lung transplantation. His computed tomography (CT) scan of chest showed diffuse bilateral upper lobe predominant bronchiectasis with areas of bronchial wall thickening and mucous plugging in peripheral airways (Fig. 1). There was no evidence of pulmonary artery hypertension on echocardiography and right heart catheterization. Colonoscopy showed diverticulosis and inflammatory polyp in the ascending colon. His CT scan of abdomen showed evidence of fatty infiltration of pancreas. After an evaluation patient was deemed to be an appropriate candidate for lung transplantation. Patient underwent bilateral lung transplantation without major complications. He received induction immunosuppression with Basiliximab. His immunosuppression was maintained per institutional protocol with Tacrolimus (FK506), Mycophenolate Mofetil (Cellcept) and Prednisone. He also received appropriate infection prophylaxis post-transplant as per institutional protocol with Valganciclovir, Voriconazole and Sulfamethoxazole/Trimethoprim.
Fig. 1.
CT scan of chest showed upper lobe predominant bronchiectasis.
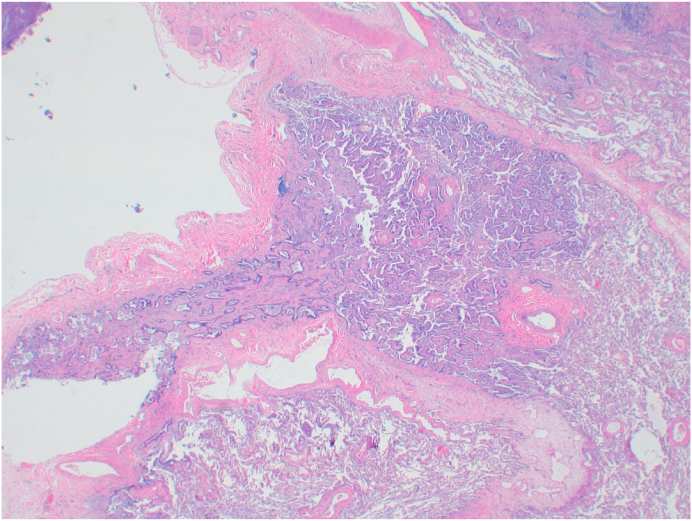
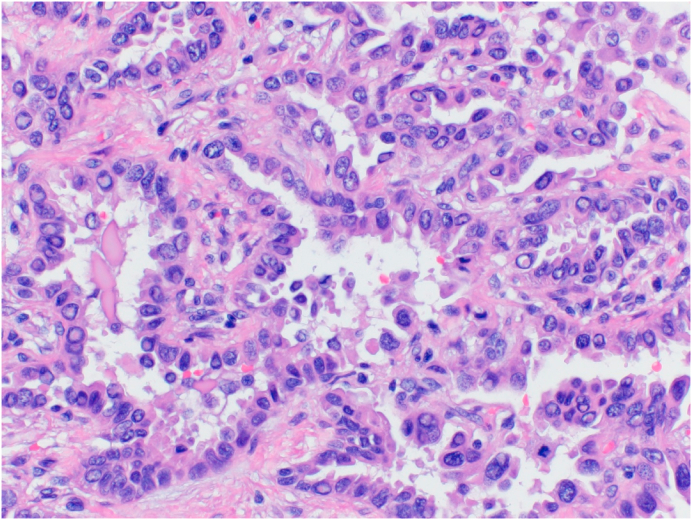
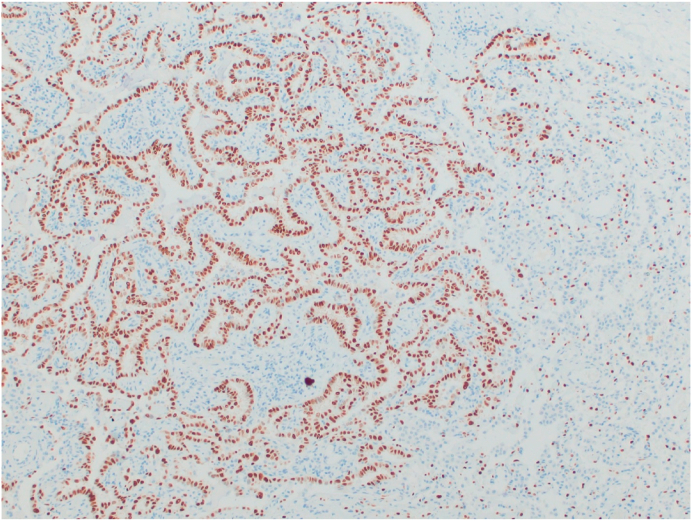
Explanted lung pathology showed widespread bronchiectasis and obstruction of airways by mucus throughout the lungs consistent with bronchiectasis. To our surprise, an eight-millimeter focus of invasive adenocarcinoma was noted on hematoxylin and eosin stains (Fig. 2). The carcinoma was papillary subtype predominant with minor components of acinar and lepidic subtype. There was no evidence of lympho-vascular and visceral pleural invasion. There was no evidence of a terminal bar or cilia to suggest markedly reactive bronchiolar metaplasia. At high power, there were malignant nuclear features including nuclear pseudo inclusions. There were multiple lymph nodes along with explant lung that did not show any evidence of carcinoma. The adenocarcinoma was in an area relatively spared of the marked inflammation surrounding the airways (Fig. 3). Bronchial and vascular surgical margins were free from invasive carcinoma. The malignant cells showed expression of cytokeratin 7, Thyroid transcription factor-1 (TTF-1) (Fig. 4) and Napsin A. A negative immunohistochemical staining for cytokeratin 20 and CDX2, a highly sensitive and specific marker of adenocarcinoma of intestinal origin, supported the diagnosis of adenocarcinoma of lung origin.
Fig. 2.
Hematoxylin and eosin stain in low power view showed an abrupt change from normal lung parenchyma (right side of images) to area with complex papillary architecture, enlarged hyperchromatic atypical nuclei and septal thickening.
Fig. 3.
High power view showed malignant nuclear features including nuclear pseudo inclusions.
Fig. 4.
Immunohistochemical staining for TTF-1 suggested primary lung carcinoma.
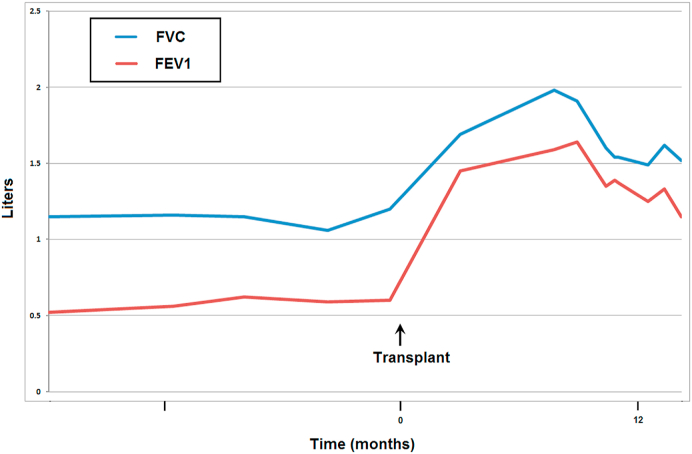
During post-transplant, patient developed mild degree of acute cellular rejection at two months after lung transplant noted on surveillance biopsy of lung, this was treated with high dose of prednisone per protocol. De novo donor specific antibodies (DSA) were noted about two month after lung transplant. The patient was treated with monthly infusion of intravenous immunoglobulin and Rituximab. Patient did not have any recurrence of DSA since the initial treatment. Periodic screening for lung carcinoma after lung transplant was performed every 3 months with CT scan of chest and positron emission tomography (PET) scan. The screening studies did not reveal any evidence of recurrence of lung carcinoma up to one year after lung transplantation. Over the year the patient had significant improvement in lung function and exercise tolerance (Fig. 5). After recovering from surgery, at three months after transplantation patient returned to full time work without any limitations to activity.
Fig. 5.
Pulmonary Function Test before and after lung transplant surgery showed significant improvement in function.
3. Discussion
Over last five decades, long-term survival rate for CF patients has significantly improved. In United States, the study based on large comprehensive database maintained by cystic fibrosis foundation (CFF) consisting of 3.5 million patient-years revealed that the overall cancer risk was similar to background risk (standardized incidence ratio [SIR] = 1.1, 95% confidence interval [CI] = 1.0 to 1.3). Further, increased risk of digestive tract cancer including biliary tract cancer (SIR = 3.5, 95% CI = 2.6 to 4.7), testicular cancer and lymphoid leukemia were observed. Analysis of the European data yielded findings similar to those of the United States [9]. There was a decrease (statistically non-significant) in lung cancer observed (SIR = 0.4, 95% CI 0.1 to 1.1). CF patients are significantly younger and less likely to smoke including second hand smoke exposure (23.4%). Cystic fibrosis transmembrane conductance regulator (CFTR) mutations have been proposed, however the role of CFTR in lung cancer remains controversial [10]. Evidently the pronounced inflammation does not predispose to the development of lung cancer [8]. There are only three lung cancers reported in CFF, Canadian Cystic Fibrosis Foundation Registry and European Cystic Fibrosis Organizations among 30 years [[7], [8], [9]]. Our patient is the fourth CF patient reported to have lung carcinoma. The United States Preventive Services Task Force (USPSTF) recommended annual screening for lung cancer with low dose CT for high-risk patients more than 55 years and a 30 pack-years smoking history [11]. There are no specific recommendations of lung cancer screening in CF patients.
Lung cancer after lung transplantation can be diagnosed as a result of three scenarios: transmission from the donor to the recipient, as a finding in the explanted lung and during follow up for lung transplant. Recipient risk factors for lung cancer are mainly associated with occupational and environmental exposure, tobacco being the leading cause, but also exposure to asbestos and silica. Chronic lung diseases like idiopathic pulmonary fibrosis and emphysema are also risks factors for lung cancer independent of smoking history. Donor risk factors include advanced age and history of smoking [12,13]. Lung transplant recipient for CF related bronchiectasis were substantially younger, less likely to smoke and more frequently received a bilateral lung transplant. Among lung transplant recipient lung cancer was the most common cancer in non-CF recipients, but risk was not increased in CF recipient [14].
Survival of patients with lung cancer in a lung transplant recipient primarily depends on the time of diagnosis, stage and the possibility of receiving active treatments. Management of immunosuppressant in these patients still lacks established recommendation [15,16]. There are different strategies that have been proposed. One of these strategies proposes a change to a regimen with an antiproliferative effect, such as Cellcept to an M-TOR inhibitor (Everolimus or Sirolimus). From the time of cancer diagnosis, survival is of 33% at one year and falls to 17% at two years [14]. Our patient has had no evidence of clinical-radiological recurrence of lung cancer during one-year follow up.
In conclusion, lung cancer in patients with CF is extremely rare. To our knowledge this is fourth reported case of lung carcinoma in a patient with CF. A vigilant screening for malignancy should be performed for the patients who undergo lung transplant evaluation. We also recommend an aggressive evaluation for recurrence of carcinoma after lung transplantation in case of incidental finding of lung carcinoma on explanted lung.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101242.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Chien C.R., Chen T.H. A Bayesian model for age, period, and cohort effects on mortality trends for lung cancer, in association with gender-specific incidence and case-fatality rates. J. Thorac. Oncol. 2009;4:167–171. doi: 10.1097/JTO.0b013e318194fabc. [DOI] [PubMed] [Google Scholar]
- 2.Subramanian J., Madadi A.R., Dandona M., Williams K., Morgensztern D., Govindan R. Review of ongoing clinical trials in non-small cell lung cancer: a status report for 2009 from the ClinicalTrials.gov website. J. Thorac. Oncol. 2010;5:1116–1119. doi: 10.1097/JTO.0b013e3181e76159. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A., Siegel R., Xu J., Ward E. Cancer statistics. Ca - Cancer J. Clin. 2010;60:277–300. doi: 10.3322/caac.20073. 2010. [DOI] [PubMed] [Google Scholar]
- 4.Mathew J., Kratzke R. Lung cancer and lung transplantation: a Review. J. Thorac. Oncol. 2009;4:753–760. doi: 10.1097/JTO.0b013e31819afdd9. [DOI] [PubMed] [Google Scholar]
- 5.Dickson R.P., Davis R.D., Rea J.B., Palmer S.M. High frequency of bronchogenic carcinoma after single-lung transplantation. J. Heart Lung Transplant. 2006;25:1297–1301. doi: 10.1016/j.healun.2006.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Picard C., Grenet D., Copie-Bergman C., Martin N., Longchampt E., Zemoura L., Stern M. Small-cell lung carcinoma of recipient origin after bilateral lung transplantation for cystic fibrosis. J. Heart Lung Transplant. 2006;25(8):981–984. doi: 10.1016/j.healun.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Neglia J.P., FitzSimmons S.C., Maisonneuve P. The risk of cancer among patients with cystic fibrosis. N. Engl. J. Med. 1995;332(8):494–499. doi: 10.1056/NEJM199502233320803. [DOI] [PubMed] [Google Scholar]
- 8.Maisonneuve P., FitzSimmons S.C., Neglia J.P., Campbell P.W., III, Lowenfels A.B. Cancer risk in nontransplanted and transplanted cystic fibrosis patients: a 10-year study. J. Natl. Cancer Inst. 2003;95(5):381–387. doi: 10.1093/jnci/95.5.381. [DOI] [PubMed] [Google Scholar]
- 9.Maisonneuve Patrick, Marshall Bruce C., Knapp Emily A., Lowenfels Albert B. Cancer risk in cystic fibrosis: a 20-year nationwide study from the United States. J. Natl. Cancer Inst. 2013;105:122–129. doi: 10.1093/jnci/djs481. [DOI] [PubMed] [Google Scholar]
- 10.Jin Li, Zhang Jie Ting, Jiang Xiaoh ua, Shi Xiaosh un, Shen Jianfei, Feng Fenglan, Chen Jing yi, Liu Guihong, He Ping, Jiang Juhong, Tsang Lai Ling, Wang Yan, Rosell Rafael, Jiang Long, He Jianxing, Chang Chan Hsiao. The cystic fibrosis transmembrane conductance regulator as a biomarker in non-small cell lung cancer. Int. J. Oncol. 2015;46:2107–2115. doi: 10.3892/ijo.2015.2921. [DOI] [PubMed] [Google Scholar]
- 11.Moyer V.A., U.S. Preventive Services Task Force Screening for lung cancer: U. S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2014;160(5):330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 12.Mathew J., Kratzke R. Lung cancer and lung transplantation. J. Thorac. Oncol. 2009;4:753–760. doi: 10.1097/JTO.0b013e31819afdd9. [DOI] [PubMed] [Google Scholar]
- 13.Callejo D., Torrente M., Parejo C., Laporta R., Ussetti P., Porvencio M. Lung cancer in lung transplantation: incidence and outcome. Postgrad. Med. 2017;4:134868. doi: 10.1136/postgradmedj-2017-134868. [DOI] [PubMed] [Google Scholar]
- 14.Fink A., Yanik E., Marshall B., Wilschanski M., Lynch C., Austin A., Copeland G., Sfaeian M., Engels E. Cancer risk among lung transplant recipients with cystic fibrosis. J. Cyst. Fibros. 2017;16:91–97. doi: 10.1016/j.jcf.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olland A.B., Falcoz P.E., Santelmo N. Primary lung cancer in lung transplant recipients. Ann. Thorac. Surg. 2014;98:362–371. doi: 10.1016/j.athoracsur.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Abrahams N.A., Meziane M., Ramalingam P., Mehta A., DeCamp M., Farver C.F. Incidence of primary neoplasms in explanted lungs: long- term follow-up from 214 lung transplant patients. Transplant. Proc. 2004;36:2808–2811. doi: 10.1016/j.transproceed.2004.10.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.