Abstract
Rabies is a global problem, but the burden is higher in less developed or developing countries of Asia and Africa. In Nepal, rabies is reported to kill around 500 animals and up to 32 human beings in recent years, with possible under-reporting of cases and deaths. As a prophylactic measure, around 30,000 livestock and 300,000 humans get vaccinated each year in Nepal. This review summarizes the past, present and future perspectives of rabies control and prevention in Nepal. The global strategic plan of World Health Organization (WHO) aims to bring human deaths from dog-transmitted rabies to zero by 2030. To achieve this goal of ‘Zero by 30’, the concerned governmental and non-governmental agencies in Nepal should work together using the One Health concept.
Keywords: Rabies, Nepal, One health, Dog, Epidemiology
Highlights
-
•
Rabies is caused by Lyssa virus that is responsible for deaths of 55,000 people annually across the world.
-
•
Dogs are responsible for 95% of rabies cases around the globe and 99% in endemic regions.
-
•
Asia has the highest burden of rabies and India alone accounts for around 35% of world rabies cases.
-
•
In Nepal, less than 35 people have died each year due to rabies.
-
•
One health approach is mandatory to end dog mediated rabies by the year 2030.
1. Introduction
Rabies is a fatal viral zoonosis caused by an RNA virus belonging to the family Rhabdoviridae of genus Lyssavirus [1,2]. This virus can infect all the animals of group Mammalia, but dogs have been considered as the major source of infection. 95% of the human cases of rabies are due to dog bites but the tally reaches 99% in the endemic regions [3,4]. However, a slight proportion of the disease in humans is also reported via wildlife such as foxes, wolves, jackals, mongoose, raccoons, skunks and bats, especially in developed countries that have successfully controlled domestic cases of rabies [5,6]. The rabies-infected animals transmit the virus to other animals and humans via saliva [7]. The infection is on the central nervous system, primarily brain and spinal cord resulting in encephalitis, thus leading to the highest documented case-fatality rate, nearing 100% [8]. Millions of the death reports have been on evidence since its introduction in 4000 BCE [9]. The incidence of rabies in the world is decreasing due to the development of pre- and post-prophylactic vaccines [10]. The disease has been eliminated in many countries due to strong control measures. Although many necessary measures are being undertaken to control and eradicate rabies, the virus is still prevailing worldwide and causing substantial health and economic burden in the developing countries, mainly in Africa and Asia [11].
The government of Nepal along with the concerned authorities and local bodies with the co-operation of various governmental and non-governmental organizations are working towards decreasing the rabies cases by mass vaccinations of dogs, animal birth control programs in various densely populated areas of the country and awareness generation campaigns. Despite these efforts, veterinary epidemiological center has reported 6 to 32 human deaths in the last five years in Nepal. Similarly, National Vaccine Production Laboratory has also been unable to meet its target goal of rabies vaccine production in the last five years as reported by the Animal Disease Investigation and Control Division. Also due to the geographical barriers, the people in hilly regions are less fortunate in terms of facilities like transportation, education, medicine, which leads to a lack of access to awareness campaigns and other rabies control-related programs. Owing to such limitations, it is likely that the actual rabies cases are under-represented in Nepal. This paper describes the current situation of the dog borne rabies in Nepal, associated campaigns and collaborations to minimize the risks and prospects of rabies control and prevention.
2. History, causative agent and transmission of rabies
Rabies, from the Latin word ‘rabere’ meaning “the rage,” has terrified mankind since antiquity [2,12]. The incidence in the world goes back more than two millennia. Rabies has also been mentioned in Mesopotamian laws of Eshnunna that is dated around 2200 BCE [13]. Likewise, Aristotle (384 BCE–322 BCE), a Greek Philosopher, has referenced rabies as ‘madness of the dog’ in ‘History of animals’. Considering the present time, an Italian physician Girolamo Fracastoro discovered rabies a fatal disease in the 16th century, calling it “an incurable wound” [14,15]. The incidence of rabies in the Asian subcontinent is assumed to be reported from the Vedic Period (1500-500 BCE) [16]. Similarly, Chinese and Indians described rabies as hydrophobia in 500 BCE and 100 BCE respectively [15]. Only at the start of the 19th-century rabies epizootics associated with the dogs were reported [17]. Zinke, in 1804 CE, proved the fact that the causative agent of rabies is associated with the saliva of rabid animals whereas Galtier experimented in rabbits to support this conclusion [15]. Similarly, it was in 1821, Magendie and Breschet concluded that the causative agent is identical for both humans and animals [18]. The first vaccine of rabies was discovered by Louis Pasteur after he successfully cured a rabid dog bitten boy, Joseph Meister, in July 1885 [2,19].
Rabies is caused by Lyssavirus belonging to the family Rhabdoviridae which are enveloped viruses having single-stranded, negative-sense RNA genome of approximately 12 kilobytes size [1,2,20]. The genus, Lyssa, comes from the Greek goddess Lyssa, the 11 spirits of madness, frenzy, and rage [2,21]. Meanwhile, rabies on itself is derived from Latin term rabere that implies madness and raving [2,22]. In Sanskrit, the word rabies is derived from an ancient word rabhas that implies ‘to create violence’ [23,24].
Dogs are responsible for the spread of rabies, which is true in 95% of the cases in regions like Asia and Africa [25]. Dogs alone are responsible for 99% of disease transmission in rabies endemic regions [3,4]. But in nature, the transmission and maintenance of rabies occur in two interrelated cycles: the urban cycle, which involves domesticated and stray dogs; and a sylvatic cycle, that involves wildlife like foxes, wolves, jackals, mongoose, raccoons, skunks and bats [26,27]. In South East Asian countries like Bangladesh, India, and Nepal, dogs are the major reservoir host whereas wolves (Canis lupus), jackals (Canis aureus) and foxes (Vulpes bengalensis) are described as the wildlife reservoirs [26]. Rabies is mainly transmitted through the bite of the rabid animals [22,28], but in rare instances, the lick by the rabid animals into an open wound may also transmit the virus [15,22]. Very rarely, the virus transmission by the organ transplant has also been reported [22,29,30]. The bodily fluids like tears and nervous tissues can also possibly transmit the disease but the virus is not reported in feces or blood [31]. Oral transmission of the disease, transmission through abrasions in the oral mucosa and transplacental transmission have also been experimentally recorded [32]. Transmission through the consumption of milk and cooked meat has not been reported to date but the consumption of milk and meat from rabid animals is discouraged [31]. Few cases of aerosol transmission of the disease have also been reported previously [33].
3. Global situation of rabies
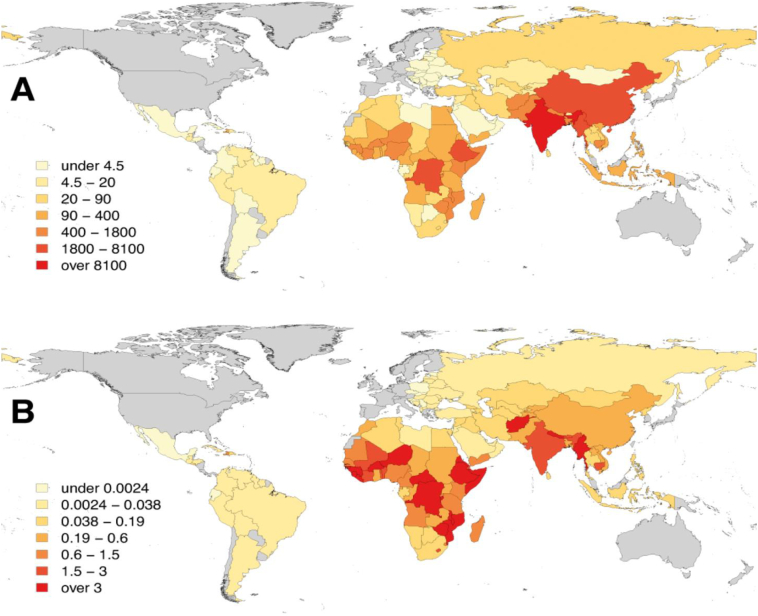
Around 59,000 human deaths are estimated every year across the world due to rabies, out of which 45% prevails in South Asian Association for Regional Cooperation (SAARC) countries [34] and the remaining deaths occur mainly in Africa, middle east and central Asia. Rabies is a major burden in Asia, mostly in the rural and underprivileged regions, with an estimated over 35,000 human deaths per year (Fig. 1) [3]. India alone accounts for nearly 60% of rabies deaths in Asia and 35% of deaths globally [3,35]. Likewise, over 20,000 deaths occur each year in Africa due to dog-mediated rabies [36].
Fig. 1.
Burden of rabies around the world in 2017. A: Number of deaths per year, B: Deaths per 100,000 population [3].
The other reports are from Central Asia and the middle east which indicate hundreds of deaths per year due to rabies [3]. Many European countries and countries in North and South America like Belize, Colombia, Costa Rica, Chile, Ecuador, Panama, Paraguay, and Uruguay have already eliminated rabies as a public health problem through compulsory vaccination of dogs and provision of good access to post-exposure prophylaxis for human beings [20]. European Union encountered nine cases from the year 2011 and the origin was from a visitor to endemic regions, the maximum number of cases was in the year 2014 with 3 rabies cases [[37], [38], [39]]. Dog-mediated rabies has been eliminated from Western Europe, Canada, the United States of America, Japan and some Latin American countries [22]. Australia and many Pacific island nations have always been free from dog-mediated rabies [3].
4. Situation of rabies in Asia
World Health Organization (WHO) has named eleven members in its South East Asia (SEA) region (Bangladesh, Bhutan, Democratic People's Republic of Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste) and among them, eight of the countries are endemic to rabies with more than 1 billion people being at risk of the disease (Table 1) [26]. Each year more than 3.8 million people in the SEA region receive post-exposure vaccines after being exposed to animals [3]. In India, more than 15,000 people die each year due to rabies infection [40] and there is one Indian death out of every five global deaths due to rabies [41]. The number of patients who receive the post-exposure vaccination each year in India is over 1 million [42].
Table 1.
Estimation of human rabies cases in South East Asian region (data as of 2011) [26].
| Countries | Estimated number of human rabies cases |
|---|---|
| India | 18,000–20,000 |
| Pakistan | 2000–5000 |
| Afghanistan | 2000–3000 |
| Bangladesh | 2000–2500 |
| Myanmar | 1000 |
| Indonesia | 150–300 |
| Nepal | <100 |
| Sri Lanka | <60 |
| Thailand | <25 |
| Bhutan | <10 |
In Thailand, the number of dog bites each year is around 400,000 and the human deaths are less than 25 in number [26]. Until mid-October 17 human deaths were reported in Thailand in 2018 [44]. About 54% (13,088/24332) dogs were found to be positive for the disease from the year 1987 to 1996 in Thailand [45]. In Vietnam, more than 350,000 people per year were bitten by dogs and cats, on average, while more than 80 human deaths have been reported yearly [46], whereas 362 cases of human rabies were reported from 2007 to 2010 [47]. A total of 809 fatal human rabies cases were reported in Chongqing, China from 2007 to 2016. Approximately 3200 human deaths were reported from rabies in the year 2006 in China. In 1998, 5 million people and 130 million dogs were given post-exposure prophylaxis in China [48]. Even though these countries have progressed with development, dog-meat eating behavior has likely increased the dog bite incidence. Although the transmission through meat ingestion is not recorded but the bites during handling of the dogs while slaughtering may be the cause.
In Bhutan, rabies was prevalent until 1990 but from the year 1996 to 2009, 814 rabies cases (cattle 55% and dog 39%) were reported [43]. Around 2000–2500 rabies cases were encountered in Bangladesh yearly with estimated dog bite of 300,000 [26] and around 50% of people did not get vaccinations and health care recommendations [49]. The reason may be due to a lack of understanding about the disease and severity. The Maldives has always been free of rabies because it is an island so the transmission of the virus through the oceans has been really difficult [34].
5. Situation of rabies in Nepal
Nepal is a landlocked country which is surrounded from the South, East, and West direction by India, the country carrying the heaviest rabies burden. Due to the open border, the eradication of the disease has been difficult. Nepal used to have a high rate of human rabies deaths per total population in the 1970s as compared to other countries across the globe [43]. This has been reduced in recent years but there are several cases which do not get reported. Rabies can be transmitted in humans by domesticated and stray dogs (urban cycle) as well as some wild animals like foxes, raccoons, and bats (sylvatic cycle). The incidence of the urban cycle of rabies transmission is considerably higher as compared to the sylvatic [26].
The first attempt to carry out a dog census in Nepal was carried out by National Zoonoses and Food Hygiene Research Center (NZFHRC) in 1998, where they estimated the number of dog populations in Nepal to be nearly 2 million which was 1 dog per 10 human population [50]. Similarly, in the country capital, Kathmandu, the number of stray dogs was estimated 170,000 in 1997 [51]. In a similar survey, the stray dog population was found to be more than 22,000 in 2012 (5.18 dogs per hector) showing a decreasing trend compared to 30,000 in 2006 but the number was still alarming [52]. In 2016, this number increased to around 30,000 indicating that the stray dog population was highly fluctuating [53]. Around 1700 stray dogs were present inside Pokhara valley [52,54]. The dog census in Lalitpur, sponsored by French non-profit organization in 1989, reported the dog population to be 10,375 [55], which was reduced to 2793 in the year 2015 [56]. Biratnagar metropolitan, then sub-metropolitan had an estimated 8000 dog population in 2008 which increased exponentially reaching 20,000 in 2014 [57]. Despite the progress made lately in terms of anti-rabies vaccination and population birth control, owing to the continuous efforts of educational and animal welfare organizations, the stray dogs' number is still considerable in Nepal.
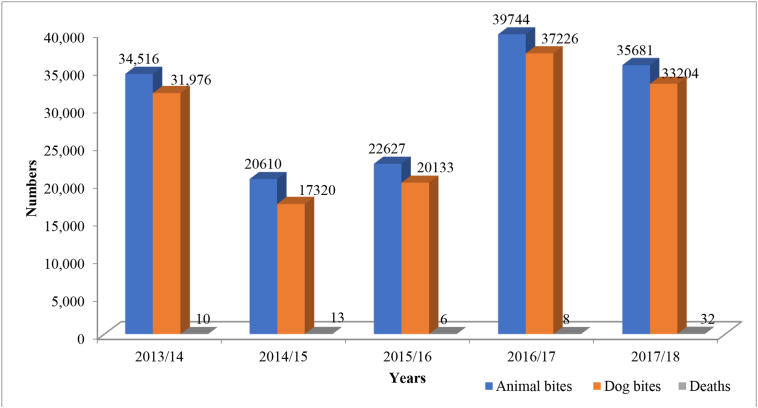
In the last five years, around 20,000 to 40,000 animal bites were reported in Nepal (Fig. 2). The highest number of animal bites was reported in year 2016/17 while the lowest (20,610) number of animal bites was reported in year 2014/15. Irrespective of the total number of animal bites, dogs were responsible for more than 90% of the bites each year. According to the reports from Sukraraj Tropical and Infectious Disease Hospital, 150 people visit the hospital each day to receive anti-rabies vaccination, out of which 30 visits are at night [63]. The statistics are appalling considering the efforts and finance invested every year to reduce the incidence. The urbanization in the major cities like Kathmandu, Pokhara, Bharatpur, Butwal, and Biratnagar has increased the number of stray dogs as it offers greater food opportunities for dogs which in turn increases the human-dog interactions. Children are more susceptible to dog bites because of their high acquaintance with newborn pups while pedestrians also become the victim of stray dog bites.
Fig. 2.
The number of animal bites, dog bites and human deaths due to rabies in different fiscal years (2013/14–2017/18) in Nepal [[58], [59], [60], [61], [62]].
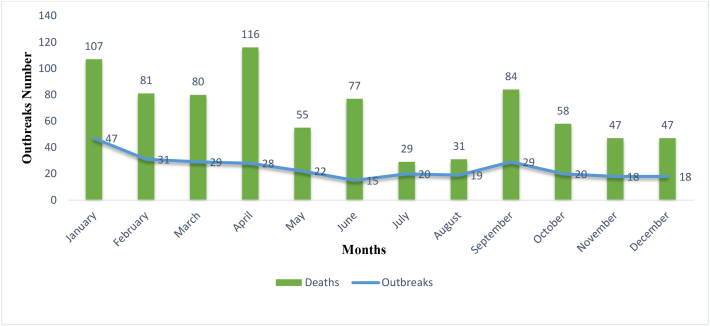
In four years (2014–2017), eight districts of Nepal (Kanchanpur, Dailekh, Jajarkot, Chitwan, Dhading, Ramechhap, Siraha, and Morang) had more than 10 rabies outbreaks. Similarly, 4 districts (Jhapa, Siraha, Sindhuli, and Surkhet) had more than 10 rabies outbreaks in the year 2018 [64]. The Year 2014 and 2017 had an equal number of 73 outbreaks. The cumulative data of 2014 to 2017 indicated that a large number of outbreaks occurred during the month of January (47), February (31), March (29) and September (29) while the highest number of animal deaths occurred during April (116), January (107), September (84) and February (81) (Fig. 3).
Fig. 3.
Month wise rabies outbreak and animal deaths from the year 2014–2017. The outbreaks and deaths of each month during four subsequent years are combined [64].
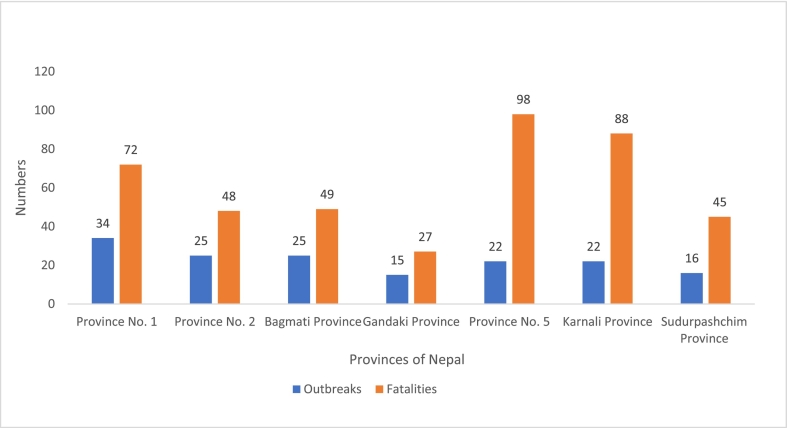
The year 2018 showed an abrupt increase in the rabies outbreak reaching to a total of 159 outbreaks (Fig. 4). As mentioned in the quarterly bulletin of Veterinary Epidemiology Centre, Province 5 had the highest number of animal deaths (98) followed by Karnali province (88) and province 1 (72) (Fig. 4). Province 5 is connected to the largest rabies bearing nation in the world, India, and shares an open border. Some districts under this province belong to the less fortunate areas in terms of medical and educational facilities which can also be a factor contributing to the high number of rabies associated animal deaths. In province 5, Rupandehi district, where lies the provincial capital and second-largest Nepal-India border has the maximum reported animal deaths due to rabies, followed by Kapilvastu (16 deaths) and Gulmi district (15 deaths). None of the infected cases in the country could be treated but vaccinations of 30,076 animals were conducted in the meantime. Similarly, 49, 48, 45 and 27 animal deaths were reported in Bagmati province, Gandaki province, Sudurpaschim province and Province 2 respectively (Fig. 4). Maximum deaths from outbreaks in 2018 occurred in Surkhet (48), Jhapa (30), and Siraha (26) districts of Nepal [65].
Fig. 4.
Animal rabies outbreaks and fatalities in different provinces of Nepal from January – December 2018 [65].
The risk of human rabies has been maximum in densely populated areas of Terai, inner Terai and mid-hills of Nepal [66]. On a monthly basis, the highest number of deaths were recorded in the winter seasons like January to April whereas the least from July to August. The breeding season plays an important role in the outbreaks. In Nepal, dogs breed majorly in the October. With the gestation period of two months, the pups are born in cold seasons like January to March which consequently increases the number of animal fatalities due to rabies. The densely populated Terai region offers better feeding opportunities for the stray dogs, which in turn helps in survival and procreation resulting in the increment of the stray dog population. Likewise, in the less developed areas of the hilly region surrounded by the dense forests, where animal domestication is the main sources of income, wild canines hunt the domesticated animals resulting in a large number of rabies outbreaks and animal deaths.
6. Programs undertaken for rabies control, prevention and elimination in Nepal
The treatment of 9 years old Joseph Meister, suffering from rabies, by French biologist Louis Pasteur in 1885 brought a revolution in the efficacious measure to control rabies [19,67]. Despite the fact rabies having 100% case fatality rate, the disease is entirely preventable by the application of pre- and post-prophylactic vaccinations [68,69]. The mass vaccinations of the dogs have resulted in massive declination of the disease in many countries of Europe. Rabies has been eradicated from several countries of Latin America and Europe, courtesy of the successful mass vaccinations during the past [20]. Rabies control program in Nepal has been first referenced by Bahmanyar [50]. Although the first committee for rabies elimination was established in 1979, the first program was undertaken after 4 years, in 1983, with the support of Department of Livestock Development and Animal Health. This led to the vaccination of over 22,000 pet dogs in Kathmandu valley and over 14,000 dogs in other districts of Nepal through different veterinary hospitals [70]. In Nepal, the first anti- rabies vaccine (ARV) production initiated in 1970 by Rabies Vaccine Production Laboratory (RVPL) [71] and the collections and distributions were handled by the regional laboratories. The vaccines were nerve tissue origin in the initial phases. The phenolized 5% and 5% beta propiolactone inactivated vaccines phased out in 2004 and 2006 respectively following the WHO recommendation [73]. RVPL in association with Japan International Cooperation Agency (JICA) released the first batch of cell culture ARV, NeJa Rab (trade name of the vaccine), for animal use in June 2006 [72]. National Vaccine Production Laboratory (NVPL), earlier known as RVPL, produced 120,000 doses of rabies vaccine in Nepal in the year 2019.
Various organizations in both the national and international levels have been actively participating in the dog mediated rabies elimination in Nepal. For example, NZFHRC, an organization actively working in the field of animal health since the 1980s, successfully vaccinated over 18,000 dogs and cats in 8 years from 2000 CE [74]. In 2007, with the support of WHO, a workshop was conducted with an aim to control rabies by 2012 and eliminate rabies by 2027 [50]. Alliance Group for Rabies control in Nepal was established in 2008 which included various institutions working in the field of disease control. Since its establishment, the alliance has been actively participating in the vaccination of over 10,000 community and stray dogs [75]. Sneha's care is an organization that has been actively working in the field of stray dogs' management, their treatment, health checkup, and sanitation. Due to their vaccination programs, the number of infected stray dogs have been greatly reduced in recent years. In the same way, Kathmandu Animal Treatment (KAT) Centre is significantly contributing to neutering dogs and also has been providing anti-rabies vaccination for dogs since 2004. KAT Centre has vaccinated over 37,000 street dogs against rabies to date and sterilized over 23,000 dogs [76]. Himalayan Animal Rescue Trust (HART) is another leading organization working in the field of dog health and management. They focus on dog population census, mass anti-rabies vaccination, sterilization, and public awareness generation. The other contributing organizations are, Animal Welfare Society, Animal Nepal, Institute of Agriculture and Animal Sciences (IAAS) and Agriculture and Forestry University (AFU). Various animal health camps for canine and free anti-rabies vaccination campaigns are organized by educational institutions including IAAS and AFU. IAAS, Paklihawa campus has also been providing free neutering services to decrease the number of stray dogs in Rupandehi district. Various veterinary hospitals at local levels under Nepal government have also been providing free rabies vaccinations for both stray and pet dogs. Global Alliance for Rabies Control has also been actively participating in the rabies control programs in Nepal. The organization also initiated the celebration of World Rabies Day in 2007. Free dog vaccination and awareness campaigns are held across the nation on September 28th each year to celebrate World Rabies day. World Organization for Animal Health (OIE) has been helping Nepal in this regard and had donated 200,000 vials of ARV in 2012 [50]. Rabies in Asia Foundation held a conference in 2008 focusing several measures to eliminate rabies from Nepal. Several new initiatives for rabies control from international agencies like WHO have also been started. WHO Regional Office for South East Asia, SAARC and Rabies in Asia Foundation have various initiatives that are currently in practice in Nepal.
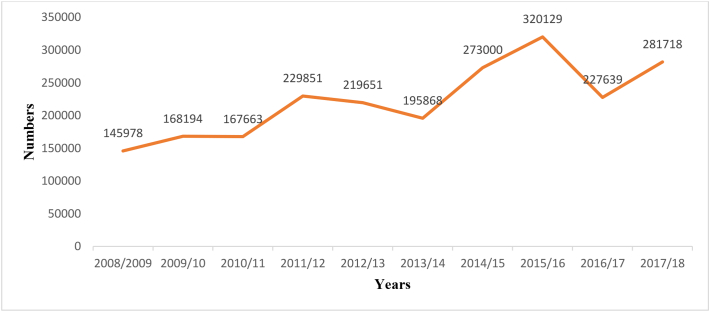
In humans, the uptake of anti-rabies vaccine ranged from around 150,000 to 320,000 from 2008/9 to 2017/18 (Fig. 5). In order to buy anti-rabies vaccines for the fiscal year 2018/19, Government of Nepal had allocated around 1 million USD. Nepal bought anti-rabies vaccines worth 70,000 USD in the previous fiscal year alone reported by the Epidemiology and Disease Control Division (EDCD) [77]. Despite investing the heavy sum of money, time, and efforts by the government and the stakeholders, the rabies cases have not yet decreased as expected. Kathmandu metropolitan city (KMC) had allocated a budget of around 35,000 USD to manage the stray dogs' population in the fiscal year 2015/16 and had the plan to eliminate all the stray dogs' populations in the upcoming 3 to 4 years [78]. The plan execution and the efforts turned out to be ineffective as more than 20,000 stray dogs still wandered the streets of the metropolitan city in the year 2019 [79] Different concerned authorities are contributing at their level to decrease the cases so that Nepal can achieve zero rabies cases by 2030.
Fig. 5.
Number of vials of anti-rabies vaccines consumed per year by humans in Nepal [[58], [59], [60], [61], [62]].
7. Future perspectives for rabies control, prevention and elimination from Nepal
Despite several attempts in the past decades to eliminate rabies, this disease still prevails in Nepal. The stray dog population is still large in major cities of the country; pet dogs are also abandoned once they lose the aesthetic value or after they acquire some diseases; contact between pet dogs and stray dogs occurs frequently increasing the chance of bite and virus transmission, and the rabid animals can be introduced through Indian side due to open borders. All these reasons contribute to the persistence of animal rabies in Nepal. There is also a lack of harmony and collaboration between various organizations working in rabies control [77]. The ongoing rabies control programs mostly focus on the urban and developed areas but the rural and less developed areas, which contribute to the significant number of animal bites and rabies cases in Nepal, are still neglected [50]. Moreover, there are limited number of laboratories, only in the major cities, for the proper diagnosis of the disease leading to inadequate reporting and ineffective surveillance of rabies from rural areas [43].
Vaccination is the key to decrease the number of rabies in animals and humans. NVPL produced 120,000 doses of vaccines in Nepal in the year 2019. Considering the number of streets and domesticated dogs in Nepal, domestic vaccine production should be increased. Likewise, Nepal fully depends upon the import of both pre- and post-exposure prophylaxis vaccines for human use, which are made available freely on several public hospitals of Nepal [34,50]. This may cost more than a million USD which is a significantly high amount for a nation of this stature and hence vaccine production through government laboratory within the country should be initiated for human use. Nepal is a part of ‘united against rabies collaboration’ formed by WHO, FAO, OIE and GARC in 2015, which has a goal to end dog-mediated rabies by 2030 worldwide: ‘Zero by 30’. To achieve this goal, the different governmental and non-governmental agencies should collaborate and work jointly so that available resources will be utilized rationally. Programs like mass dog vaccination campaigns should be launched under one umbrella. Rural areas, which in general lack education, transportation, and medical facilities, should also be prioritized by the agencies working in rabies control. The healthcare facilities in the rural areas should be equipped with the manpower and equipment required for the diagnosis and prevention of rabies in human as well as animal health sectors. In order to control the possible introduction of rabid animals from the open Indian border, proper quarantine is necessary. Adoption of stray dogs, together with birth control and rabies vaccination, should be encouraged among the public to solve the issue of street dogs. Stray dog population can also be controlled by the establishment of proper waste management facilities. Rabies is a common problem of animal and human health sectors. Therefore, short and long-term strategies of rabies control should be formulated following the One Health (OH) approach.
At present, the leading departments of human and animal health sectors, Department of Health Services (DHS) and Department of Livestock Services (DLS) have their sectoral priorities where OH approach has been overlooked or not properly implemented. Establishment of a separate OH organizational framework involving the representatives from the aforementioned departments can create a common platform for rabies surveillance, resource utilization, and development and implementation of effective rabies control programs [80]. Despite the initiation of various OH approaches in the past including development of tissue culture rabies vaccine for human use in 2010 by NVPL under the DLS [81]; World Bank funded ‘zoonoses control project’ (2012–2014) [82]; and establishment of OH hubs in the 75 districts of Nepal under One Health Network South Asia implemented by Massey University (2013) [83]; the outcomes did not match the expectations. This may be due to the lack of effective central policy for initiating and maintaining productive communication, surveillance efforts, resource mobilizations, innovative idea sharing, and collaborations among different sectors and stakeholders involved in rabies control within the country. The government of Nepal should involve both human and animal health sectors together in the rabies control plan that will effectively coordinate for collective disease diagnosis; production of vaccines; vaccination of animals and humans; awareness generation; and other preventive and therapeutic initiatives. Leading non-governmental organizations as well as state and local government bodies should also be actively linked to the OH hubs for effective rabies control program planning and execution. The goal of eliminating rabies by 2030 is only possible when all the concerned stakeholders work together under the umbrella of One Health.
8. Conclusion
Rabies is one of the major zoonotic threat in Nepal. Each year, several outbreaks and deaths associated with rabies are reported in the animal sector. Likewise, animal bites, more importantly, dog bites are reported in thousands of human individuals leading to the consumption of a large number of pre- and post-prophylactic measures. Hence, a joint effort to control rabies is necessary from animal and human health sectors under One Health approach. The governmental, as well as non-governmental agencies should work together and launch rabies control programs throughout the country. Only with the combined efforts of all of the stakeholders, the goal of achieving zero rabies by 2030 will be feasible in Nepal.
Authors contributions
Conceptualization, S.P., D.S., and K.K.; methodology and literature research S.P., D.S., U.P., S·S; writing-original draft preparation, S.P., D.S., S.D.; writing review and editing, S.P., D.S., K.K., S.D.; supervision S.D., and K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgements
We are grateful to Er. Sameer Pantha, Mr. Bickal Gautam, Mr. Sulav Dhakal, Mr. Keshav Kharel Mr. Santosh Subedi and two anonymous reviewers for their valuable suggestions and contribution in the completion of this article.
Contributor Information
Saurav Pantha, Email: sauravvet@gmail.com.
Deepak Subedi, Email: subedideepu26@gmail.com.
References
- 1.Rupprecht C.E., Barrett J., Briggs D., Cliquet F., Fooks A.R., Lumlertdach B., Meslin F.X., Müler T., Nel L.H., Schneider C., Tordo N., Wandeler A.I. Can rabies be eradicated? Dev. Biol. (Basel) 2008;131:95–121. [PubMed] [Google Scholar]
- 2.Hankins D.G., Rosekrans J.A. Overview, prevention, and treatment of rabies. Mayo Clin. Proc. 2004;79(5):671–676. doi: 10.4065/79.5.671. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Epidemiology and burden of disease http://www.who.int/rabies/epidemiology/en/ Available online.
- 4.Ma X., Blanton J.D., Millien M.F., Medley A.M., Etheart M.D., Fénelon N., Wallace R.M. Quantifying the risk of rabies in biting dogs in Haiti. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-57908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Neweshy Mahmoud S., Mayahi Nada Al, Mamari Wafa Al, Rashdi Zahra Al, Mawly Julanda H. Al. Animal rabies situation in Sultanate of Oman (2017–2019) Trop. Anim. Health Pro. 2020 doi: 10.1007/s11250-020-02328-0. [DOI] [PubMed] [Google Scholar]
- 6.Jimenez I., Spraker T. Anderson.; Bowen,R,; Gilbert, A. isolation of rabies virus from the salivary glands of wild and domestic carnivores during a skunk rabies epizootic. J. Wildl. Dis. 2019;55(2):473. doi: 10.7589/2018-05-127. [DOI] [PubMed] [Google Scholar]
- 7.Leung A.K.C., Davies H.D., Hon K.-L.E. Rabies: epidemiology, pathogenesis, and prophylaxis. Adv. Ther. 2007;24(6):1340–1347. doi: 10.1007/BF02877781. [DOI] [PubMed] [Google Scholar]
- 8.Fooks A.R., Banyard A.C., Horton D.L., Johnson N., McElhinney L.M., Jackson A.C. Current status of rabies and prospects for elimination. Lancet. 2014;384(9951):1389–1399. doi: 10.1016/S0140-6736(13)62707-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baiee Hasan Alwan. Epidemiology of Human Rabies Deaths in Babylon Province, Five Years Descriptive Epidemiologic Study. J. Glob. Pharma Technol. 2017 [Google Scholar]
- 10.Briggs D.J. The role of vaccination in rabies prevention. Curr. Opin. Virol. 2012;2(3):309–314. doi: 10.1016/j.coviro.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Hampson K., Coudeville L., Lembo T., Sambo M., Kieffer A., Attlan M., Barrat J., Blanton J.D., Briggs D.J., Cleaveland S., Costa P., Freuling C.M., Hiby E., Knopf L., Leanes F., Meslin F.-X., Metlin A., Miranda M.E., Müller T., Nel L.H., Recuenco S., Rupprecht C.E., Schumacher C., Taylor L., Antonio M., Vigilato N., Zinsstag J., Dushoff J. Global alliance for rabies control partners for rabies prevention. Correction: estimating the global burden of endemic canine rabies. PLoS Negl. Trop. Dis. 2015;9(5) doi: 10.1371/journal.pntd.0003786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatami H. History of rabies in traditional medicine’s resources and Iranian research studies: on the CccasiOn of the world rabies day (September 28, 2012) Int. J. Prev. Med. 2012;3(9):593–595. [PMC free article] [PubMed] [Google Scholar]
- 13.Tarantola A. Four thousand years of concepts relating to rabies in animals and humans, its prevention and its cure. Trop. Med. Infect. Dis. 2017;2:5. doi: 10.3390/tropicalmed2020005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brightman C. Rabies: an acute viral infection. Trends Urol. Mens Health. 2012;3(5):31–33. doi: 10.1002/tre.287. [DOI] [Google Scholar]
- 15.Rupprecht C.E., Hanlon C.A., Hemachudha T. Rabies re-examined. Lancet Infect. Dis. 2002;2(6):327–343. doi: 10.1016/S1473-3099(02)00287-6. [DOI] [PubMed] [Google Scholar]
- 16.Menezes R. Rabies in India. Can. Med. Assoc. J. 2008;178(5):564–566. doi: 10.1503/cmaj.071488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blanton J.D., Palmer D., Dyer J., Rupprecht C.E. Rabies surveillance in the United States during 2010. J. Am. Vet. Med. Assoc. 2011;239(6):773–783. doi: 10.2460/javma.239.6.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kammer A.R., Ertl H.C.J. Rabies vaccines: from the past to the 21st century. Hybrid. Hybridomics. 2002;21(2):123–127. doi: 10.1089/153685902317401726. [DOI] [PubMed] [Google Scholar]
- 19.Bourhy H., Dautry-Varsat A., Hotez P.J., Salomon J. Rabies. Still neglected after 125 years of vaccination. PLoS Negl. Trop. Dis. 2010;4:11. doi: 10.1371/journal.pntd.0000839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vigilato M.A.N., Clavijo A., Knobl T., Silva H.M.T., Cosivi O., Schneider M.C., Leanes L.F., Belotto A.J., Espinal M.A. Progress towards eliminating canine rabies: policies and perspectives from Latin America and the Caribbean. Philos. Trans. R. Soc. B Biol. Sci. 2013;368(1623):20120143. doi: 10.1098/rstb.2012.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Potegal M. 1st ed. Springer-Verlag; New York: 2010. Stemmler (Auth.), G.; Potegal, M.; Stemmler, G.; Spielberger (Eds.), C. International Handbook of Anger: Constituent and Concomitant Biological, Psychological, and Social Processes. [Google Scholar]
- 22.Ruiz M., Chávez C.B. Rabies in Latin America. Neurol. Res. 2010;32(3):272–277. doi: 10.1179/016164110X12645013284257. [DOI] [PubMed] [Google Scholar]
- 23.Kolhe R.P., Bhilegaonkar K.N., Surkar S.H., Agarwal R.K. An overview of epidemiology and control of rabies: global and Indian scenario. J. Vet. Pub. Hlth. 2012;10(2):73–84. [Google Scholar]
- 24.Why Rabies Still Kills http://therisingnepal.org.np/news/15481?fbclid=IwAR3M4J0PM4BHcyKzizR5FHyeRCfIs2vPdhc2nlV5ywWVeqypmYhSVwMDXOQ Available online.
- 25.Wunner W.H., Briggs D.J. Rabies in the 21st century. PLoS Negl. Trop. Dis. 2010;4(3) doi: 10.1371/journal.pntd.0000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gongal G., Wright A.E. Human rabies in the WHO Southeast Asia region: forward steps for elimination. Adv. Prev. Med. 2011;2011:1–5. doi: 10.4061/2011/383870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campos A.A.S., Santos dos R.N., Benavides J.A., Batista H.B. de C.R., Finoketti F., Wagner P.G.C., Zafalon-Silva B., Alievi M., Silva da F.B., Witt A., Tartarotti A., Silva da A. de C.R., Ferreira K.C.S., Frazzon A.P.G., Roehe P.M., Franco A.C. Rabies surveillance in wild mammals in south of Brazil. Transbound. Emerg. Dis. 2020;67(2):906–913. doi: 10.1111/tbed.13415. [DOI] [PubMed] [Google Scholar]
- 28.Nigg A.J., Walker P.L. Overview, prevention, and treatment of rabies. Pharmacotherapy. 2009;29(10):1182–1195. doi: 10.1592/phco.29.10.1182. [DOI] [PubMed] [Google Scholar]
- 29.CDC Questions and Answers - Human Rabies Due to Organ Transplantation. https://www.cdc.gov/rabies/resources/news/2013-03-15.html Available online.
- 30.Srinivasan A., Burton E.C., Kuehnert M.J., Rupprecht C., Sutker W.L., Ksiazek T.G., Paddock C.D., Guarner J., Shieh W.-J., Goldsmith C., Hanlon C.A., Zoretic J., Fischbach B., Niezgoda M., El-Feky W.H., Orciari L., Sanchez E.Q., Likos A., Klintmalm G.B., Cardo D., LeDuc J., Chamberland M.E., Jernigan D.B., Zaki S.R. Transmission of rabies virus from an organ donor to four transplant recipients. N. Engl. J. Med. 2005;352(11):1103–1111. doi: 10.1056/NEJMoa043018. [DOI] [PubMed] [Google Scholar]
- 31.Frequently Asked Questions about Rabies for the general public. https://www.who.int/rabies/Rabies_General_Public_FAQs_21Sep2018.pdf?ua=1html Available online.
- 32.Afshar A. A review of non-bite transmission of rabies virus infection. Br. Vet. J. 1979;135(2):142–148. doi: 10.1016/S0007-1935(17)32935-4. [DOI] [PubMed] [Google Scholar]
- 33.Johnson N., Phillpotts R., Fooks A.R. Airborne transmission of Lyssaviruses. J. Med. Microbiol. 2006;55(6):785–790. doi: 10.1099/jmm.0.46370-0. [DOI] [PubMed] [Google Scholar]
- 34.Pant G.R. Rabies Control Strategy in SAARC Member Countries. https://www.oie.int/doc/ged/D12940.pdf Available online.
- 35.Reddy G.B.M., Singh R., Singh K.P., Sharma A.K., Vineetha S., Saminathan M., Sajjanar B. Molecular epidemiological analysis of wild animal rabies isolates from India. Vet. World. 2019;12(3):352–357. doi: 10.14202/vetworld.2019.352-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahmad T., Musa T.H., Jin H. Rabies in Asian countries: where we are stand? Biomed. Res. Ther. 2018;5(10):2719–2720. doi: 10.15419/bmrat.v5i10.485. [DOI] [Google Scholar]
- 37.Annual Epidemiological Report for 2015. Rabies https://www.ecdc.europa.eu/sites/default/files/documents/AER_for_2015-rabies.pdf Available online.
- 38.Rabies Annual Epidemiological Report for 2018. https://www.ecdc.europa.eu/sites/default/files/documents/rabies-annual-epidemiological-report-2018.pdf Available online.
- 39.Annual Epidemiological Report for 2016. Rabies https://www.ecdc.europa.eu/sites/default/files/documents/rabies-annual-epidemiological-report-2016.pdf Available online.
- 40.Baxter J.M. One in a million, or one in thousand: what is the morbidity of rabies in India? J. Glob. Health. 2012;2(1) doi: 10.7189/jogh.02.010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahuja S., Tripathi K.K., Saha S.M., Saxena S.N. Epidemiology of rabies in India. In: Kuwert E., Mérieux C., Koprowski H., Bögel K., editors. Rabies in the Tropics. Springer; Berlin, Heidelberg: 1985. pp. 571–582. [DOI] [Google Scholar]
- 42.Knobel D.L., Cleaveland S., Coleman P.G., Fèvre E.M., Meltzer M.I., Miranda M.E.G., Shaw A., Zinsstag J., Meslin F.-X. Re-evaluating the burden of rabies in Africa and Asia. Bull. World Health Organ. 2005;83:360–368. doi: 10.1590/S0042-96862005000500012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yadav S. 2012. Animal Rabies in Nepal and Raccon Rabies in Albany County, New York. Thesis. [Google Scholar]
- 44.Rabies Death Toll Climbs to 17 this Year in Thailand. http://www.xinhuanet.com/english/2018-10/18/c_137542478.htm Available online.
- 45.Mitmoonpitak C., Tepsumethanon V., Wilde H. Rabies in Thailand. Epidemiol. Infect. 1998;120(2):165–169. doi: 10.1017/S0950268897008601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee H.S., Thiem V.D., Anh D.D., Duong T.N., Lee M., Grace D., Nguyen-Viet H. Geographical and temporal patterns of rabies post exposure prophylaxis (PEP) incidence in humans in the Mekong River Delta and southeast central coast regions in Vietnam from 2005 to 2015. PLoS One. 2018;13(4) doi: 10.1371/journal.pone.0194943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen A.K.T., Nguyen D.V., Ngo G.C., Nguyen T.T., Inoue S., Yamada A., Dinh X.K., Nguyen D.V., Phan T.X., Pham Q., Nguyen H.T., Nguyen H.T.H. Molecular epidemiology of rabies virus in Vietnam (2006–2009) Jpn. J. Infect. Dis. 2011;64:391–396. [PubMed] [Google Scholar]
- 48.Davlin S.L., VonVille H.M. Canine rabies vaccination and domestic dog population characteristics in the developing world: a systematic review. Vaccine. 2012;30(24):3492–3502. doi: 10.1016/j.vaccine.2012.03.069. [DOI] [PubMed] [Google Scholar]
- 49.Hossain M., Ahmed K., Bulbul T., Hossain S., Rahman A., Biswas M.N.U., Nishizono A. Human rabies in rural Bangladesh. Epidemiol. Infect. 2012;140(11):1964–1971. doi: 10.1017/S095026881100272X. [DOI] [PubMed] [Google Scholar]
- 50.Devleesschauwer B., Aryal A., Sharma B.K., Ale A., Declercq A., Depraz S., Gaire T.N., Gongal G., Karki S., Pandey B.D., Pun S.B., Duchateau L., Dorny P., Speybroeck N. Epidemiology, impact and control of rabies in Nepal: a systematic review. PLoS Negl. Trop. Dis. 2016;10(2) doi: 10.1371/journal.pntd.0004461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kato M., Yamamoto H., Inukai Y., Kira S. Survey of the stray dog population and the health education program on the prevention of dog bites and dog-acquired infections: a comparative study in Nepal and Okayama prefecture, Japan. Acta Med. Okayama. 2003;57(5):261–266. doi: 10.18926/AMO/32829. [DOI] [PubMed] [Google Scholar]
- 52.Kakati K. Street Dog Population Survey Kathmandu. 2012. https://animalnepal.files.wordpress.com/2013/09/dog-survey-kathmandu-valley-2012.pdf Available online.
- 53.Ojha A. Stray Dogs Call the Shots in City. https://kathmandupost.com/valley/2018/06/06/stray-dogs-call-the-shots-in-city Available online.
- 54.Acharya M., Dhakal S. Survey on street dog population in Pokhara Valley of Nepal. Bangladesh J. Vet. Med. 2015;13(1):65–70. doi: 10.3329/bjvm.v13i1.23722. [DOI] [Google Scholar]
- 55.Wandeler A.I., Matter H.C., Kappeler A., Budde A. The ecology of dogs and canine rabies: a selective review. Rev. sci. tech. Off. int. Epiz. 1993;12(1):51–71. doi: 10.20506/rst.12.1.663. [DOI] [PubMed] [Google Scholar]
- 56.Animal Nepal Launches Lalitpur Dog Population Survey Report. https://animalnepal.wordpress.com/2016/01/26/animal-nepal-launches-lalitpur-dog-population-survey-report/ Available online. (accessed 23 February 2020)
- 57.Jha A.K. Rising Number of Stray Dogs Haunts Public in Biratnagar. https://kathmandupost.com/national/2014/06/19/rising-number-of-stray-dogs-haunts-public-in-biratnagar Available online.
- 58.Department of Health Services Annual Report 2070/71. 2013/2014. https://dohs.gov.np/wp-content/uploads/2014/04/Annual_Report_2070_71.pdf Available online. (accessed 25 February 2020)
- 59.Department of Health Services Annual Report 2071/72. 2014/2015. https://dohs.gov.np/wp-content/uploads/2016/06/Annual_Report_FY_2071_72.pdf Available online. (accessed 25 February 2020)
- 60.Department of Health Services Annual Report 2072/73. 2015/2016. https://dohs.gov.np/wp-content/uploads/2017/06/DoHS_Annual_Report_2072_73.pdf Available online.
- 61.Department of Health Services 2016/2017. https://dohs.gov.np/wp-content/uploads/2018/04/Glimpse_FY_%202073-74.pdf Annual Report 2073/74. Available online.
- 62.Department of Health Services https://dohs.gov.np/wp-content/uploads/2019/07/DoHS-Annual-Report-FY-2074-75-date-22-Ashad-2076-for-web-1.pdf Annual Report 2074/75 (2017/2018) Available online.
- 63.Hospital receives 150 Dog Bite Cases Per Day. https://thehimalayantimes.com/kathmandu/hospital-receives-150-dog-bite-cases-per-day/ Available online.
- 64.Quarterly Animal Health E-Bulletin (Rabies specific) Jan-April 2018. http://epivet.gov.np/uploads/files/0936410132.PDF Available online.
- 65.Annual Epidemiological Bulletin January-December 2018; Veterinary Epidemiology Center (VES). Animal Disease Investigation and Control Division: Tripureshwor, Kathmandu, Nepal, 2018.
- 66.Shrestha J.M. Proceedings of the 9th National Veterinary Conference of Nepal Veterinary Association, Kathmandu, Nepal. 22–24 April 2010. Rabies epidemiology, economics and major challenges. [Google Scholar]
- 67.Rappuoli R. Inner workings: 1885, the first rabies vaccination in humans. Proc. Natl. Acad. Sci. 2014;111(34):12273. doi: 10.1073/pnas.1414226111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Taylor L.H., Nel L.H. Global epidemiology of canine rabies: past, present, and future prospects. Vet. Med. Res. Rep. 2015;6:361–371. doi: 10.2147/VMRR.S51147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chatterjee S., Riaz H. Rabies: Beware of the dog. BMJ. 2013;347(oct01 3):f5912. doi: 10.1136/bmj.f5912. [DOI] [PubMed] [Google Scholar]
- 70.Joshi D.D. Proceedings of the First National Seminar on Rabies, Kathmandu, 17–22 November 1985. 3rd Ed. National Zoonoses and Food Hygiene Research Centre; Kathmandu: 2001. Present situation on the control of human and canine rabies in Nepal. [Google Scholar]
- 71.Rabies Vaccine Production Laboratory. Trend of Rabies vaccine production http://www.rvpl.gov.np/content.php?id=223 Available online.
- 72.Rabies Vaccine Production Laboratory. Commercial batch of NeJa Rab vaccine http://www.rvpl.gov.np/content.php?id=222 Available online.
- 73.Pant G.R. Proceedings of the a Workshop on Snake Envenoming and Rabies. Nepal Health Research Council; 2009. Production and use of anti-rabies vaccine in Nepal; pp. 52–55. [Google Scholar]
- 74.Free Dog Rabies Vaccination in 24 Municipalities of Nepal. Zoonoses and Food Hygiene News. http://nzfhrc.org.np/wp-content/uploads/2016/08/V14N1.pdf Available online. (accessed 26 February 2020)
- 75.Enhancing Progress towards Rabies Elimination www.saohnet.org/wp-content/uploads/2019/12/Enhancing-Progress-towards-Rabies-Elimination-Zero-by-30-in-SAARC-Region_V3.5_20191122.pdf Available online: ‘Zero by 30’ in SAARC Regionhttps://
- 76.KAT Centre. Rabies Prevention https://katcentre.org.np/en/rabies-prevention Available online:
- 77.Poudel A. Nepal Has Pledged to End Rabies by 2030, but Dog-Bite Cases Are Rising Available Online. https://kathmandupost.com/national/2019/02/04/nepal-has-pledged-to-end-rabies-by-2030-but-dog-bite-cases-are-rising
- 78.Thapa G. A Dogged Drive against Stray Dogs of Capital Available Online. https://kathmandupost.com/valley/2016/01/14/a-dogged-drive-against-stray-dogs-of-capital
- 79.L Barbara. Kathmandu: Animal Nepal Rescues Stray Dogs Available Online. https://www.gonomad.com/5645-kathmandu-animal-nepal-rescues-stray-dogs
- 80.Acharya K.P., Karki S., Shrestha K., Kaphle K. One health approach in Nepal: scope, opportunities and challenges. One Health. 2019;8 doi: 10.1016/j.onehlt.2019.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pant G.R. Production of tissue culture rabies vaccine for human use in Nepal. Int. J. Infect. Dis. 2012;16:e311. doi: 10.1016/j.ijid.2012.05.1007. [DOI] [Google Scholar]
- 82.World Bank . World Bank Group; Washington, DC: 2014. Nepal - Zoonoses Control Project (English)http://documents.worldbank.org/curated/en/203131468059704553/Nepal-Zoonoses-Control-Project [Google Scholar]
- 83.McKenzie J.S., Dahal R., Kakkar M., Debnath N., Rahman M., Dorjee S.…Halimi A. One Health research and training and government support for One Health in South Asia. Infect. Ecol. Epidemiol. 2016;6(1):33842. doi: 10.3402/iee.v6.33842. [DOI] [PMC free article] [PubMed] [Google Scholar]