Abstract
More than 75% of emerging infectious diseases and 60% of known human infectious diseases are transmitted from animals. Among these zoonoses, rabies is of utmost public health significance due to its lethality. The multi-faceted nature of zoonotic disease complicates control and prevention and thus, a multi-sectoral One Health Approach could be a better strategy to cope with rabies. Up until now, rabies prevention and control programs are conducted utilizing mass vaccination of domestic and community dogs and cats, and mass awareness programs. However, the burden of rabies has not been reduced as these approaches have failed to include all stakeholders (human, animal, and environmental health sectors) in disease management programs. The aim of this review is to highlight why and how One Health Approach would be the most effective way to control rabies in low- and middle-income countries (LMICs) like Nepal.
Keywords: Zoonoses, Rabies, Prevention, One health
1. Introduction
Rabies is a viral zoonotic disease of mammals. Approximately, 55,000 people are reported to die of rabies every year throughout the world [1]. Among zoonotic diseases, rabies is neglected, even though it has huge public health significance. Despite being a preventable disease, impact of rabies is increasing day by day, which is a worrisome issue in developing and developed countries [2]. Rabies has two, sylvatic and non-sylvatic, cycles of transmission [3]. Thus, it requires a comprehensive, strategic, and targeted control and prevention approach with collaboration from human, animal, and environmental health disciplines at local, national, and global levels to a make more effectual control program.
Rabies is endemic to Nepal and it has been listed as one of the prioritized zoonotic diseases [4]. Approximately, 96% of reported human rabies cases in Nepal are due to dog bites, and the remaining 4% cases are due to interactions with other animals [3]. The human transmission vectors for rabies may vary around the world. For example, in US 70% of cases were associated with bats [1], and in Nepal 96% cases are due to dog bites [3]. In Nepal, different government and non-government agencies are involved in rabies control and prevention programs mostly through implementation of vaccination, and domestic and community dog and cat population management. Additionally, dog bite cases have been managed through post exposure prophylaxis (PEP), and awareness programs since the early 2000's [5,6]. However, rabies cases have not reduced as a result of these programs due to lack of multi-sectoral management approaches [6,7]. In this review, we propose a “One Health Approach” as the most effective way to control rabies in Nepal using successful lessons and strategies from other countries.
2. Global situation of rabies
Rabies is an endemic disease in nearly all land masses except in islands like Australia, and Antarctica where no cases of dog mediated rabies have been reported [8,9]. Many Asian countries, European countries, and North and South American countries have been declared rabies free [8,10] but rabies is still a problem in many Asian and African countries. Rabies is particularly highly prevalent in Bangladesh and India, and moderately prevalent in Nepal, Myanmar, Bhutan, Thailand, and Indonesia [8,9]. The prevalence of canine rabies in the countries of Asian subcontinent is reported to range from 0 to 55% of the global canine rabies cases [9].
3. Rabies in Nepal
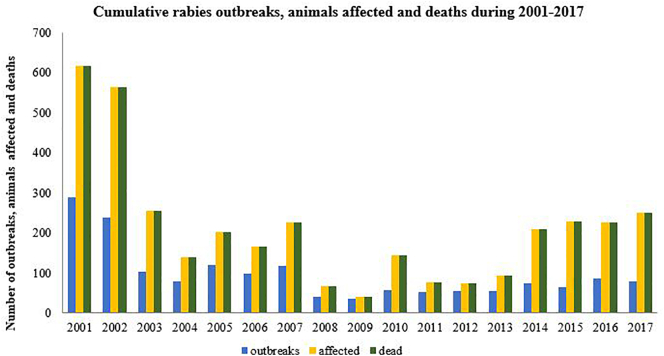
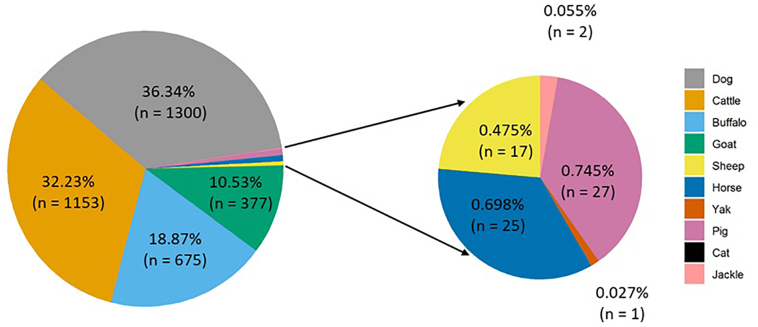
On an average one hundred livestock and 10–100 human deaths were reported each year in Nepal [3,11]. However, recent data from Veterinary Epidemiology Center (VEC) show that rabies cases in animals are on a rising trend with up to 300 deaths per year (Fig. 1), while up to 32 human deaths have been reported due to rabies in recent years [12]. Approximately, 1000 livestock and 35,000 humans receive rabies post-exposure prophylaxis [3]. The highest number of rabies cases were recorded in dogs followed by cattle, buffalo, and other animals with a few cases in wild animals like the Jackal (Fig. 2).
Fig. 1.
Cumulative rabies outbreaks, animals affected and deaths reported to Veterinary Epidemiology Center during 2001–2017.
Fig. 2.
Species wise cumulative rabies cases in animals during 2001–2017 (Source: Veterinary Epidemiology Center).
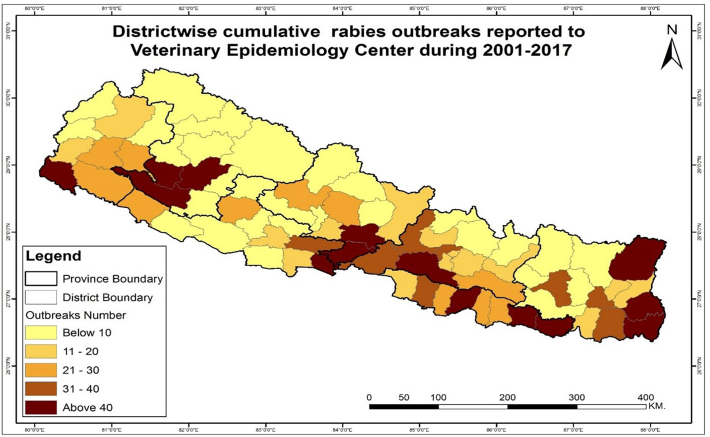
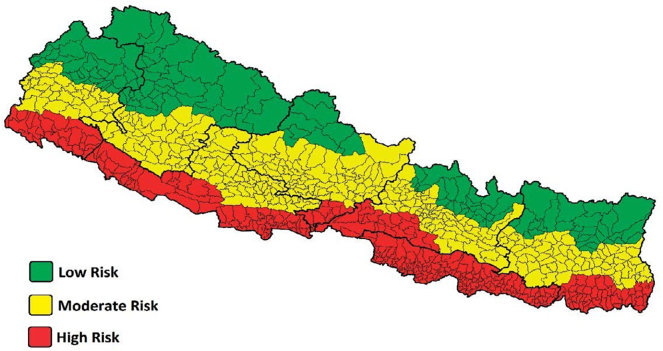
Approximately half of the Nepali population live in areas of high risk and an additional quarter live in areas of moderate risk of rabies [13]. Government data shows a decrease in rabies associated deaths despite increased cases of dog bites in recent years [3,[13], [14], [15]] with some degree of fluctuation [12] (Table 1). Dog bites stand as the predominant cause of human rabies infections while a small fraction are associated with cat and wild animals bites [3]. Moreover, cases of dog mediated rabies cases has been increasing in slum areas of major urban areas where waste disposal, hygiene and sanitation remains completely chaotic and scavenging dogs can have access to disposal area [16]. Communities where dogs are not managed as their pets and are unaware of their sanitation and hygiene, favor increase in the number of un-owned and community dog population. Geographically, in Nepal more cases of rabies are seen in plains areas compared to hilly or mountainous area [13,17] (Fig. 2; Fig. 3), which could be due to densely populated agricultural areas and wildlife population heterogeneity in those low-land Terai regions [3,17]. Based on the literature, Nepal's 20 plains districts are at a higher risk, 39 hilly districts are at a moderate risk, and the 16 mountainous districts are at a low risk of rabies [12] (Fig. 4).
Table 1.
Status of reported dog bites and rabies in Nepal.
| Year | Dog bites | Other animal bites | ARV vaccines consumed | Deaths |
|---|---|---|---|---|
| 2008/09 | 26,574 | 2,571 | 145,978 | 97 |
| 2009/10 | 25,662 | 2,145 | 168,194 | 89 |
| 2010/11 | 26,466 | 2,197 | 167,663 | 83 |
| 2011/12 | 31,313 | 2,211 | 229,851 | 76 |
| 2012/13 | 34,933 | 2,996 | 219,651 | 68 |
| 2013/14 | 31,976 | 2,540 | 195,868 | 10 |
| 2014/15 | 17,320 | 3,290 | 273,000 | 13 |
| 2015/16 | 20,133 | 2,494 | 320,139 | 6 |
| 2016/17 | 37,226 | 2,518 | 227,639 | 8 |
| 2017/18 | 33,204 | 2,477 | 281,718 | 32 |
(Source: Annual Technical Report, DOHS, 2012/13; 2017/18).
Fig. 3.
District wise cumulative rabies outbreaks in animal during 2001–2017 (N = 1641). (Source: Veterinary Epidemiology Center).
Fig. 4.
Rabies risk zones in Nepal (Adapted from DoHS 2017/18).
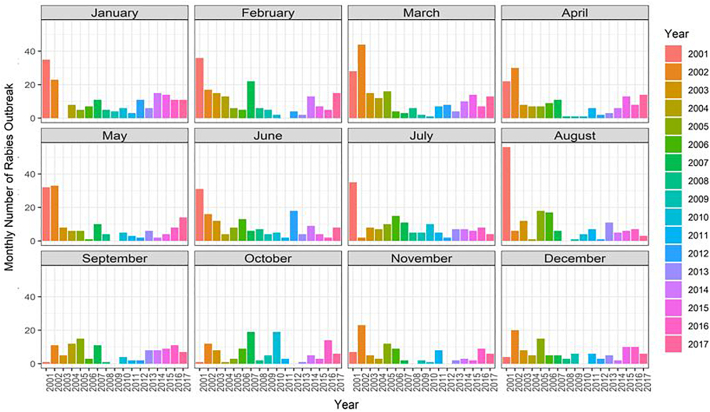
The highest number of recorded rabies cases in animals are in the months of March and October (Fig. 5). However, the number of cases in animals have been gradually decreasing in recent years (Fig. 5). This is probably due to anti-rabies vaccination in dogs.
Fig. 5.
Monthly number of rabies outbreaks in animals from 2001 to 2017 (N = 1641) (Source: Veterinary Epidemiology Center).
4. Ongoing rabies control programs and initiatives
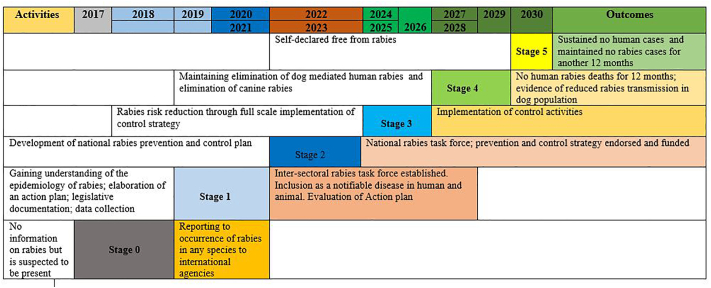
In 2019, the Epidemiology and Disease Control Division (EDCD) of Ministry of Health and Population of Nepal mandated for the control and prevention of rabies [7]. EDCD in coordination with public, non-governmental, and private partner organizations have been conducting many protective activities such as strategic vaccination in dogs and cats, raising public awareness, and capacity building among health professionals. Additionally, the Central Referral Veterinary Hospital, provinces, and municipalities have been conducting separate programs: mass rabies vaccination campaign together with dog and cat population management and public awareness under the Animal Disease Investigation and Control Division (ADICD) of Department of Livestock Services (DLS) [5]. Recent release of “National guidelines for rabies prophylaxis in Nepal 2019” guides health professionals on prevention and management of rabies and aims to achieve target ‘zero human death by 2030’ [7] along with a projected control plan involving sequence of actions and initiations [18,19] (Fig. 6).
Fig. 6.
Projected plan for rabies control in Nepal (Based on information obtained from the results of SARE assessment 2019 held in Kathmandu, Nepal).
An international workshop on rabies elimination in South Asian Association for Regional Cooperation (SAARC) countries held in 2019 in Nepal concluded with two goals; to develop and implement a national action plan and regional road maps for dog mediated rabies elimination in SAARC region and to make rabies a notifiable disease with high level of advocacy at national level garnering political commitments towards achieving the target ‘zero rabies by 2030’ [7,19,20]. Additionally, in January 2020, Government of Nepal (GoN) passed a “One Health Strategy 2020” aiming to foster the “One Health Approach” in all relevant sectors including zoonoses and antimicrobial resistance [21]. Based on assessment of the workshop for Stepwise Approach for Rabies Elimination (SARE), the Department of Livestock Services has been working to develop a comprehensive action plan to achieve dog mediated rabies elimination by 2030. As per the SARE assessment, Nepal is in the early stages of rabies control (stage in-between 0 and 1) and it would take another 12–13 years to eliminate rabies if the current situation remains persistent. However, with the capacity building and appropriate inter-sectoral collaboration, this target can be achieved by 2030. Currently, areas that require strengthening are surveillance, outbreak response and investigation, strategic mass dog vaccination, human vaccinations, expansion of free PEPs in all provinces, specimen referral, laboratory testing capacity, dog population management, advocacy and public awareness, professional education, and inter-sectoral collaboration [19,22].
Since 2007 EDCD has been implementing rabies control programs [3], and recently in 2019, it has launched national guideline for rabies PEP [7]. However, the guideline has been centered on humans PEP disregarding the importance of animal rabies [7,19,22]. The country is in process of developing a national action plan and has plans to undertake mass dog vaccination from 2023 onwards [22]. Although Nepal used to produce a 5% Beta-propiolactone (BPL) inactivated nerve tissue anti-rabies vaccine (ARV) for human use, it was phased out in 2006 [3]. Since then rabies vaccine is no longer being produced in the country for human use. Nepal produces a vaccine for use in livestock locally, but the supply is not enough to meet the national demand and additional doses of ARV vaccine is imported from abroad [3].
Recently, from May 2019 the Nepalese government has prioritized intradermal rabies vaccination program in human in order to minimize the cost of completion of full course of PEP vaccination [7]. Intradermal rabies vaccination requires only 1–2 doses of vaccines to complete the full course, while intramuscular vaccination requires four to five doses to complete the full course [23]. In contrast, requirement of sparing doses of rabies vaccine for human prophylaxis may not assure cost reduction as reported by Abbas et al. (2015) [24]. Furthermore, PEP to the public are limited to 54 different hospitals at subsidized fees, and rabies diagnostic facilities are limited to the Central Veterinary Laboratory [20] and the National Public Health Laboratory (NPHL) [7]. Nepal does not currently have rabies antibody detection and titration facilities to measure efficacy of post-vaccinal antibodies. Similarly, NGOs and INGOs working on rabies control and prevention are centered mostly in federal capital Kathmandu despite rabies cases outside the valley account for 94% of the total rabies burden in Nepal [3]. Thus, current rabies control strategies seem to be a fragmented approach by both government and NGO/INGO as mentioned by Acharya et al. 2019 [6].
One Health programs recognize that the health of humans are connected to the health of animals and our shared environment. Embracing a One Health approach focuses on outbreak management of rabies in both human and animals. Controlling animal-to-human transmission of rabies not only reduces the need of post exposure vaccine but also lowers budgetary load for rabies control in human. Also a One Health approach is known to be an economical method to control rabies for low income developing countries like Nepal [5,25]. To estimate the success metrics of this approach before deploying the program at a larger scale, a pilot project including both rural and city areas of different regions could be helpful.
Extension of availability of PEP rabies vaccine either by the GoN or through joint efforts of GoN, NGOs, INGOs and private sectors in all district hospitals would increase access and affordability to all citizens. Similarly, rabies diagnostic center in each regional laboratory would reduce the burden at the Central Reference Laboratory. Capable health professionals at the regional laboratories would ensure the quality and effectiveness of the monitoring program. Furthermore, coordination and communication of health professionals has a very important role in overall success of rabies control and prevention program [6,26,27]. Active surveillance of the disease in action would be helpful in figuring out the disease situation. Thus, an integrated approach along with coordination among each of these components i.e. human, animal, and environmental sectors, are equally important to execute a successful plan.
Focus on mass vaccination of animals and dog population management are key, but the latter should follow animal welfare guidelines. Inhumane killing and torturing of animals must be strictly prohibited via government initiatives [28], and if putting down animals is the only available options, in such case inhumane killing of animals should be replaced by a lawful euthanasia [29]. Similarly, pet ownership and public safety records can be made available with a legislative provision for mandatory registration. Population management of street or community dogs can also be done by animal birth control techniques such as spaying and castration [28]. Prior to these activities, an effective data collection and reporting system is required.
Success of the program depends mainly on public participation. Participation can be bolstered through a series of awareness campaigns. In addition, availability of basic infrastructures such as road, electricity, hospitals, and veterinary centers will dictate program implementation. The literacy and economic status of people may impact participation in post exposure vaccination, mass vaccination and animal birth controls programs [6,30]. Some critical, but not necessarily exclusive, factors to consider are socio-economic, environmental, animal, and human factors. Therefore, a “Multi-sectoral One Health Approach” could be a strong strategy to make justifiable progress towards rabies control and prevention.
A One Health approach has proven successful in several neighboring countries such as Bhutan, Bangladesh and Sri Lanka. Only seventeen cases of rabies have been reported from Bhutan between 2006 and 2016 [31,32]. Similarly, a One Health multi-sectoral approach was initially trialed in small rural communities and was later integrated to entire nation of Bangladesh with success. Bangladesh's approach was highly effective, reducing rabies deaths from 1500 in 2012 to 200 in 2015. Likewise, Sri Lanka reported that they were able to reduce rabies deaths to less than 50 in the year 2012 with the implementation of mass vaccination program in dogs. Most notably, India has recently completed a trial of this management approach in five different cities across the nation and has come to the conclusion that consideration of both human and animal component is critically important in this approach [33].
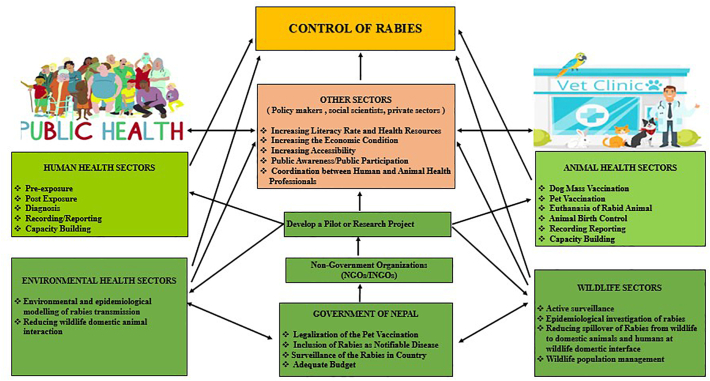
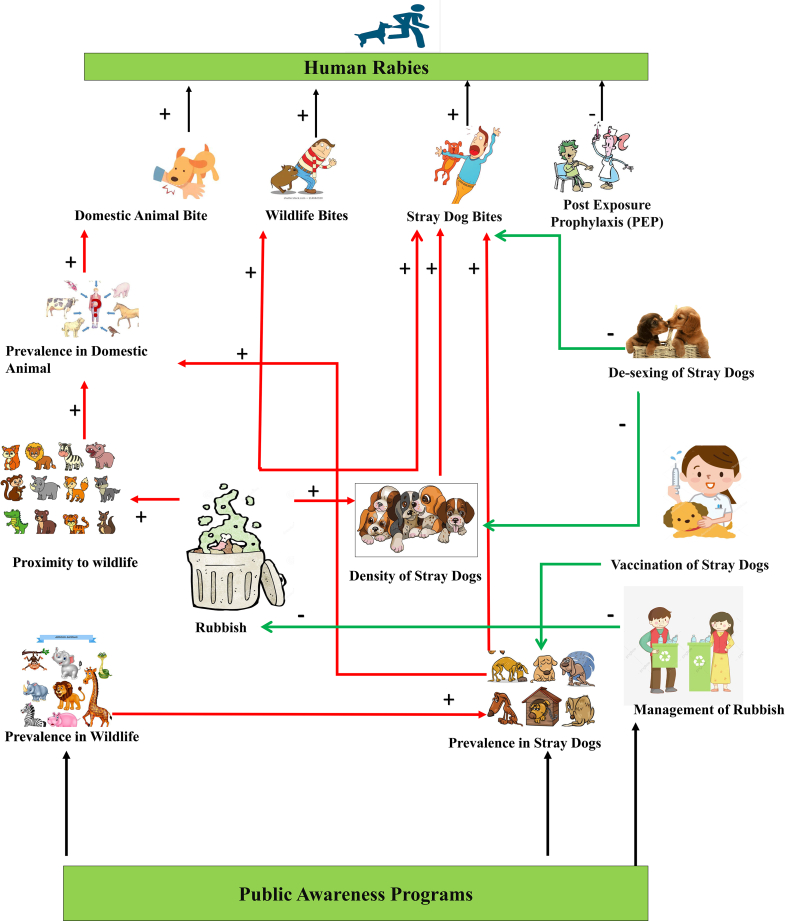
A One Health rabies management program is at its juvenile stage in Nepal [5,7]. A strong political commitment along with a rigid governmental action could be crucial in making it successful. Here is a conceptual framework on how to control or manage rabies using a One Health approach (Fig. 7; Fig. 8).
Fig. 7.
Conceptual framework on how to control rabies using One Health Approach.
Fig. 8.
Conceptual framework on how to control of human rabies. (The green lines are risk reduction options and the red lines are risk factors).
5. Way forward
Rabies can be prevented/managed efficiently by “One Health Approach” which involves inter-sectoral collaboration among animal, human, and environmental health. Considering specific national geopolitical situation, following measures could be helpful to make program successful in Nepal.
5.1. Systematic data collection and compilation
A One Health approach works best with a routine reporting system that enables evaluation of periodic progress, endemic and sporadic status of disease, and their socioeconomic impact. This information will be valuable in the creation of strategies or control programs at national level [34]. Symptoms of rabies are non-specific or common to nervous system illness, it is of no surprise that rabies cases can remain undocumented and becomes a more intense problem when registration facilities at tertiary care clinics and hospitals are unable to access clinical care and diagnostic confirmation databases [34]. Hence, a system that provides accurate information on dog population, suspected or confirmed cases of rabies, and total rabies infected population at a given area and time would be helpful in developing control roadmaps [34]. Equally, determination of human-dog population densities, data on vaccination in human and animals, comprehensive management and analysis of data are crucial for the effectiveness of rabies control programs.
5.2. Co-ordination and data sharing among animal, human and environmental health sectors
Lack of coordination and data sharing among concerned parties is a common issue in projects requiring multi-sectoral coordination. Collection, storage, and reporting of primary data in national and international databases will facilitate identification of problem areas leading to the creation management strategies. In many countries, rabies is not a common disease. Therefore, rabies data collection is limited only to formal monitoring systems in these countries. Monitoring of rabies in Nepal may be complicated due to operational difficulties in sample submission to laboratory and non-compliance to direct data reporting to line ministries. This will increase the likelihood of inaccurate and incomplete data generation.
5.3. Efficient and effective surveillance
Nepal's Animal Health Sector is mainly concerned with economically important diseases of livestock. Rabies is not on that list [6,35]. Including rabies under the diseases monitored by the Animal Health Sector would help in the collection of reliable data that can be used in strategic mass vaccination and population management. A functional surveillance system that generates primary data is vital to reach protective immune status of susceptible animal population and transmission, as suggested by Banyard and his colleagues [36]. Controlling rabies in wildlife, and wildlife-domestic animal interface could be vital to control rabies in Nepal, as humans, domestic animals and wildlife territories lie in close proximity. Thus, rabies surveillance and control programs requires extension to include wildlife so that any spillover of rabies from wildlife to domestic animals and humans could be checked effectively. One possible way to control wildlife rabies could be large scale oral vaccination campaigns with at least 70% coverage considering ecological and epidemiological features of rabies and wildlife species [37], which was successfully practiced in foxes in Europe [38], raccoons in Canada [39] and coyotes in Unites States [39]. The oral rabies vaccine (ORV) containing bait can be deposited throughout natural habitat: near buffer zone and inside national parks and wildlife reserves, community forests, and suburban regions. It may be helpful to reduce possible spillover of rabies from wildlife to livestock to humans and vice-versa.
5.4. Sufficiency and availability of post exposure prophylaxis (PEP)
PEP is the only means available for human rabies prevention after the dog bite. Obviously, rabies' burden will be higher when there is inaccessibility of PEP immediately after bite of a suspected rabid animal. In urban areas, pre-exposure prophylaxis (PrEP) and PEP is available in government and non-government hospitals [30]. However, in remote areas, PrEP and PEP are not easily available for many reasons. So far, health care facilities are mostly concentrated in urban centers making it difficult for the rural public to receive treatment when bitten [30]. To achieve zero human deaths from rabies by 2030, ensuring adequate availability of PEP is necessary. An integrated dog bite case management (IBCM) approach that involves rabies surveillance linking workers in public health and veterinary sectors to assess the risk of rabies among animal bite patients and biting animals [40,41], is another option to save more lives in short term. Long-term sustainable control of rabies is possible with strong interventions at local, national, and international level jointly.
5.5. Increasing vaccine coverage
Mass vaccination of dogs is a cost-effective means of controlling rabies. In Nepal, dog vaccination is neither practiced compulsorily nor in a routine basis [42]. According to the World Organization for Animal Health (OIE) and World Health Organization (WHO), vaccine coverage of 70% or more dog population can rapidly decrease the infection rabies rate. This will in turn directly diminishes human exposure. Investment in dog vaccination, especially mass vaccination, is advantageous in long term with higher cost-efficiency [43]. Hence, mass immunization of dog is one of the principle methods we suggest controlling rabies in both human and animal population. To increase the success of this approach, proper registration, confinement, and compulsory vaccination of domesticated and stray dogs is necessary. Follow up booster shots should also be pursued as dog that do not receive them with be incompletely immunized. In this case rabies infections are still possible after vaccination.
5.6. Increasing efficacy of vaccination
Vaccination is one of the most important measures of rabies control. Vaccines administered below the standard can fail to invoke immunity. The most common reasons of vaccine failure are inappropriate storage, transportation, and handling in addition to manufacturing defects. Thus, both vaccine quality and efficacy play equally pivotal roles in successful rabies control programs.
5.7. Increasing awareness
Public awareness programs targeting vulnerable communities will be key in the fight against any disease epidemic and rabies is not an exception. To some extent, Nepali communities are not aware of rabies. This might be due to several reasons including low literacy rate, socio-economic issues, and the failure of rabies to get a priority disease status. Nevertheless, knowledge on dog vaccination, PEP availability, and preventive measures against dog bites could be helpful to ameliorate the situation [44].
5.8. Strengthening laboratory capacity
Improvement in diagnostic capability is possible through well-equipped laboratories. For rabies, it is important to deploy preventive and control measures (vaccination program or a comprehensive package project) prior to exposure [45]. In this regard, locally available diagnostic services would be effective to achieve targeted vaccination coverage and assessment [46]. There are some sufficiently equipped laboratories meeting the standard stipulated by OIE in major cities in Nepal, but there is room for improvement to increase accessibility. To some extent, using rapid test kits for initial screening could lower the workload to these laboratories, but availability of the required laboratory facilities has no alternatives. When merely clinical signs and symptoms are the basis of disease diagnosis, poor accuracy is expected. With that said, it is not just an availability of reliable diagnosis, but also affordability of the service that are important for enhanced identification and reporting [47].
5.9. Research activities
Epidemiology field research on rabies might be helpful to identify associated risk factors, dominant mode of transmission, socio-economic implications, and locality-based disease dynamics. Thus, conducting this research could be a very good starting point for formulation of integrated multi-sectoral rabies management strategies.
Some key areas of research interventions and innovations are:
-
(1)
Development of tools to assess magnitude of rabies infections.
-
(2)
Accessibility of easy and economical diagnostic tests.
-
(3)
Studies focusing on promotion of “soft” population control measures such as dog population control, responsible dog ownership, and environmental aspects of rabies management.
-
(4)
Periodic data collection of basic population parameters of relevant animal species such as dog populations (size, turnover, accessibility, and ownership status) in different settings.
-
(5)
Public awareness campaigns to promote knowledge of PEP, first aid and animal bite management.
-
(6)
Raising awareness on the disease and responsible dog ownership with active mobilization of NGOs, community-based organizations, animal welfare societies, media, leaders, and other influential groups.
Authors' contributions
KPA and SP conceived the original paper, wrote the initial draft, and NA, SP, MU, and SL extensively revised and approved the final version of the manuscript.
Ethics approval and consent to participate
Not applicable.
Funding
No external funding was used in the preparation of this paper.
Declaration of Competing Interest
There are no competing interests.
Acknowledgements
Authors would like to thank Mr. Daya Sagar Subedi for GIS map; Niran Adhikari, Bhim Chaulagain and Richard Trevor Wilson for their feedback and inputs on the initial version of manuscript. In addition, authors are thankful to all helping hands for their direct and indirect help.
References
- 1.Pieracci E.G., Pearson C.M., Wallace R.M., Blanton J.D., Whitehouse E.R., Ma X., Stauffer K., Chipman R.B., Olson V. Vital signs: Trends in human rabies deaths and exposures — United States, 1938–2018. Morb. Mortal. Wkly Rep. 2019;68:524–528. doi: 10.15585/mmwr.mm6823e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasanov E., Zeynalova S., Geleishvili M., Maes E., Tongren E., Marshall E., Banyard A., McElhinney L.M., Whatmore A.M., Fooks A.R., Horton D.L. Assessing the impact of public education on a preventable zoonotic disease: rabies. Epidemiol. Infect. 2018;146:227–235. doi: 10.1017/S0950268817002850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devleesschauwer B., Aryal A., Sharma B.K., Ale A., Declercq A., Depraz S., Gaire T.N., Gongal G., Karki S., Pandey B.D., Pun S.B., Duchateau L., Dorny P., Speybroeck N. Epidemiology, impact and control of rabies in Nepal: a systematic review. PLoS Negl. Trop. Dis. 2016 doi: 10.1371/journal.pntd.0004461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah Y., Pandey K., Pant D.K., Poudel A., Dahal B., Panta K.P., Pandey B.D. Potential threat of rabies virus from bat bite in Nepal. Open Microbiol. J. 2019;12:419–421. doi: 10.2174/1874285801812010419. [DOI] [Google Scholar]
- 5.Acharya K.P., Karki S., Shrestha K., Kaphle K. 2019. One Health Approach in Nepal: Scope, Opportunities and Challenges, One Heal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Acharya K.P., Adhikari N., Tariq M. 2020. Fight against Rabies in Nepal: Immediate Need for Government Intervention, One Heal. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.EDCD National Guideline for Rabies Prophylaxis and Management in Nepal. 2019. http://www.edcd.gov.np/resources/download/national-guidelines-for-rabies-prophylaxis-and-management-in-nepal-new
- 8.Singh R., Singh K.P., Cherian S., Saminathan M., Kapoor S., Reddy G.B.M., Panda S., Dhama K. Rabies – epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: a comprehensive review. Vet. Q. 2017 doi: 10.1080/01652176.2017.1343516. [DOI] [PubMed] [Google Scholar]
- 9.Hampson K., Coudeville L., Lembo T., Sambo M., Kieffer A., Attlan M., Barrat J., Blanton J.D., Briggs D.J., Cleaveland S., Costa P., Freuling C.M., Hiby E., Knopf L., Leanes F., Meslin F.X., Metlin A., Miranda M.E., Müller T., Nel L.H., Recuenco S., Rupprecht C.E., Schumacher C., Taylor L., Vigilato M.A.N., Zinsstag J., Dushoff J. Estimating the global burden of endemic canine rabies. PLoS Negl. Trop. Dis. 2015 doi: 10.1371/journal.pntd.0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yousaf M.Z., Qasim M., Zia S., Khan M. Ur Rehman, Ashfaq U.A., Khan S. Rabies molecular virology, diagnosis, prevention and treatment. Virol. J. 2012 doi: 10.1186/1743-422x-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.VEC Quarterly Animal Health E-Bulletin (Rabies specific) Vet. Epidemiol. Cent. 2018:1–4. http://epivet.gov.np/uploads/files/0936410132.PDF [Google Scholar]
- 12.Department of Health Services . Vol. 75. 2019. Annual report 2075/75 (2017/18) pp. 1–476.https://dohs.gov.np/annual-report-2074-75/ [Google Scholar]
- 13.Department of Health Services Annual Report. Annu. Rep. 2017;4:1–354. doi: 10.1108/eb055690. [DOI] [Google Scholar]
- 14.Department of Health Services Annual Report 2072/73 (2015/2016) Annu. Rep. 2016;73:90. doi: 10.1039/C1DT90165F. [DOI] [Google Scholar]
- 15.Department of Health Services Ann. Rep. 2069/70 (2012/2013) 2013;70:1–480. https://dohs.gov.np/wp-content/uploads/2014/04/Annual_Report_2069_70.pdf [Google Scholar]
- 16.Muzzini E., Aparicio G., Muzzini A. Urban Growth and Spatial Transition in Nepal an Initial Assessment. 2013. https://documents.worldbank.org/en/publication/documents-reports/documentdetail/722941468291027381/urban-growth-and-spatial-transition-in-nepal-an-initial-assessment
- 17.Gongal G. The epidemiological trend of animal rabies in Nepal and future control strategy. APCRI. 2006;8 [Google Scholar]
- 18.Directorate of Animal Health . 2017. Proposed Rabies Control Strategy Draft. [Google Scholar]
- 19.SAARC . 2019. Rabies Elimination Workshop (SARE) Practical Workplan towards Approaching Rabies Elimination Nepal. [Google Scholar]
- 20.Pant G.R. Rabies Control Strategy in SAARC Member Countries, OIE. 2013. https://www.oie.int/doc/ged/D12940.pdf
- 21.Government of Nepal . 2020. Decision made by Cabinet of Ministers in Nepal including the One Health Strategy 2020. [Google Scholar]
- 22.W. SAARC OIE, Enhancing Progress towards Rabies Elimination ‘ Zero by 30 ’ in SAARC Region. 2019. https://www.saohnet.org/wp-content/uploads/2019/12/Enhancing-Progress-towards-Rabies-Elimination-Zero-by-30-in-SAARC-Region_V3.5_20191122.pdf
- 23.WHO WHO Recommends the Intradermal Route for Rabies Post-Exposure Prophylaxis. 2019. https://www.who.int/rabies/rabies_post_immunization/en/
- 24.Abbas S.S., Kakkar M. Rabies control in India: a need to close the gap between research and policy. Bull. World Health Organ. 2015;93:131–132. doi: 10.2471/BLT.14.140723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Upadhyaya M. 2016. Leadership in One Health Approach-Old Concept New Trend. [Google Scholar]
- 26.WHO . 2015. Rationale for Investing in the Global Elimination of Dog-Mediated Human Rabies. [DOI] [Google Scholar]
- 27.Richard F., ToddG S., JessieL D., Xianfu W., Michael N., CharlesE R. Current and future tools for global canine rabies elimination. Antivir. Res. 2013 doi: 10.1016/j.antiviral.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Acharya K.P., Acharya N., Wilson R.T. Animal welfare in Nepal. J. Appl. Anim. Welf. Sci. 2018 doi: 10.1080/10888705.2018.1519437. [DOI] [PubMed] [Google Scholar]
- 29.Neupane A. Activists Protest against Barbaric Behaviors on Animals (with Video) 2019. https://myrepublica.nagariknetwork.com/mycity/news/activists-protest-against-barbaric-behaviors-on-animals-with-video
- 30.Lechenne M., Mindekem R., Madjadinan S., Oussiguéré A., Moto D.D., Naissengar K., Zinsstag J. The importance of a participatory and integrated one health approach for rabies control: The case of N'Djaména. Chad, Trop. Med. Infect. Dis. 2017;2 doi: 10.3390/tropicalmed2030043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Global Alliance for Vaccines and Immunisation GAVI Countries Summary Bhutan. 2017. https://www.who.int/rabies/GAVI_country_summaries_June_2017.pdf
- 32.Tenzin T., Namgyal J., Letho S. Community-based survey during rabies outbreaks in Rangjung town, Trashigang, eastern Bhutan, 2016. BMC Infect. Dis. 2017 doi: 10.1186/s12879-017-2393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Rabies Control Programme . 2018. National Health Portal Of India. [Google Scholar]
- 34.Fahrion A.S., Mikhailov A., Giacinti J., Harries J., Fahrion A.S., Mikhailov A., Giacinti J., Harries J. 2016. Weekly epidemiological record Relevé épidémiologique hebdomadaire; pp. 13–20. [Google Scholar]
- 35.World Health Organization . WHO Regional Office for South-East Asia; New Delhi: 2012. Strategic Framework for Elimination of Human Rabies Transmitted by Dogs in the South-East Asia Region.https://apps.who.int/iris/bitstream/handle/10665/205920/B4891.pdf?sequence=1&isAllowed=y [Google Scholar]
- 36.Banyard A.C., Horton D.L., Freuling C., Müller T., Fooks A.R. Control and prevention of canine rabies: The need for building laboratory-based surveillance capacity. Antivir. Res. 2013 doi: 10.1016/j.antiviral.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Eisinger D., Thulke H.H. Spatial pattern formation facilitates eradication of infectious diseases. J. Appl. Ecol. 2008 doi: 10.1111/j.1365-2664.2007.01439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freuling C.M., Hampson K., Selhorst T., Schröder R., Meslin F.X., Mettenleiter T.C., Müller T. The elimination of fox rabies from Europe: determinants of success and lessons for the future. Philos. Trans. R. Soc. B Biol. Sci. 2013 doi: 10.1098/rstb.2012.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elmore S.A., Chipman R.B., Slate D., Huyvaert K.P., VerCauteren K.C., Gilbert A.T. Management and modeling approaches for controlling raccoon rabies: the road to elimination. PLoS Negl. Trop. Dis. 2017 doi: 10.1371/journal.pntd.0005249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Undurraga E.A., Meltzer M.I., Tran C.H., Atkins C.Y., Etheart M.D., Millien M.F., Adrien P., Wallace R.M. Cost-effectiveness evaluation of a novel integrated bite case management program for the control of human rabies, Haiti 2014-2015. Am. J. Trop. Med. Hyg. 2017 doi: 10.4269/ajtmh.16-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pieracci E. Glob; Alliance Rabies Control: 2018. Integrated Bite Case Management (IBCM)https://rabiesalliance.org/resource/emily-pieracciibcm-2018paracon-2018 [Google Scholar]
- 42.WHO FAO and OIE . 2014. Workshop on Relevant International Standards for Dog Rabies. [Google Scholar]
- 43.Zinsstag J., Dürr S., Penny M.A., Mindekem R., Roth F., Menendez Gonzalez S., Naissengar S., Hattendorf J. Transmission dynamics and economics of rabies control in dogs and humans in an African city. Proc. Natl. Acad. Sci. U. S. A. 2009 doi: 10.1073/pnas.0904740106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Balaram D., Taylor L.H., Doyle K.A.S., Davidson E., Nel L.H. World Rabies Day - a decade of raising awareness. Trop. Dis. Travel Med. Vaccines. 2016 doi: 10.1186/s40794-016-0035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aga A.M., Hurisa B. Current situation of rabies prevention and control in developing countries: Ethiopia perspective. J. Anc. Dis. Prev. Remedies. 2016;4:1–6. doi: 10.4172/2329-8731.1000128. [DOI] [Google Scholar]
- 46.Lembo T., Hampson K., Kaare M.T., Ernest E., Knobel D., Kazwala R.R., Haydon D.T., Cleaveland S. The feasibility of canine rabies elimination in Africa: dispelling doubts with data. PLoS Negl. Trop. Dis. 2010;4 doi: 10.1371/journal.pntd.0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hossain M., Ahmed K., Bulbul T., Hossain S., Rahman A., Biswas M.N.U., Nishizono A. Human rabies in rural Bangladesh. Epidemiol. Infect. 2012;140:1964–1971. doi: 10.1017/S095026881100272X. [DOI] [PubMed] [Google Scholar]