Abstract
In June 2019 the first equine case of Hendra virus in the Hunter Valley, New South Wales, Australia was detected. An urgent human and animal health response took place, involving biosecurity measures, contact tracing, promotion of equine vaccinations and investigation of flying fox activity in the area.
No human or additional animal cases occurred. Equine vaccination uptake increased by over 30-fold in the surrounding region in the three months following the case. Black flying fox and grey-headed flying fox species were detected in the Valley. The incident prompted review of Hendra virus resources at local and national levels.
This event near the “horse capital of Australia”, is the southernmost known equine Hendra case. Management of the event was facilitated by interagency collaboration involving human and animal health experts. Ongoing One Health partnerships are essential for successful responses to future zoonotic events.
Keywords: Zoonosis, Equine, Henipaviruses, Hendra virus
Highlights
-
•
In June 2019 the southernmost known equine case of Hendra virus was detected in the Hunter Valley, Australia.
-
•
This signified an increase in potential equine and human populations at risk of infection.
-
•
Interagency collaboration between animal and human health experts is essential in managing Hendra virus spillover events.
1. Background
Hendra virus was first documented in 1994, when a mystery illness in a horse preceded the death of a well-known trainer and thirteen other stable horses in Hendra, a suburb of Brisbane, Australia. To date, there have been over 100 confirmed or probable equine cases, all of which died or were euthanised [1]. Seven known cases of Hendra virus infection have occurred in humans, four of which were fatal [2].
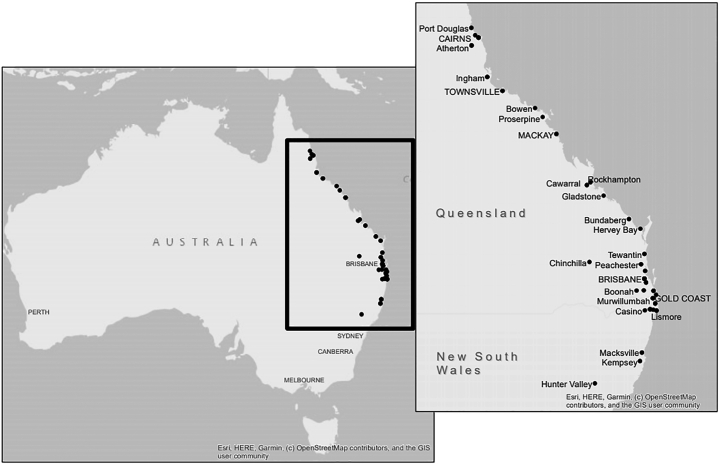
Hendra virus is a paramyxovirus, genus Henipavirus, for which Pteropus spp. fruit bats (flying foxes; family Pteropodidae) are the natural reservoir [3]. While spillover events of other Henipaviruses (e.g. Nipah virus) have occurred in Asia, Hendra virus spillover events have only been reported in eastern Australia [4]. Prior to 2019, all known events had occurred between Port Douglas in northern Queensland and Kempsey in northern New South Wales (NSW) [1] (Fig. A1).
Hendra virus appears endemic in Australian flying foxes [5]. While antibodies are detected across all four mainland species, black flying foxes and spectacled flying foxes are more commonly associated with Hendra virus excretion than other species [[6], [7], [8]]. Virus excretion can occur any time of the year, with a winter peak found particularly in northern NSW and southern Queensland [9].
Transmission to horses may occur through direct contact between horses and urine or excreta from infected flying foxes, or via contamination of horse feed, pasture and vegetation [10,11]. Equine infection can present with a range of clinical signs, but usually includes respiratory and/or neurological illness with rapid deterioration [12]. Horse-to-horse transmission has occurred in settings of close contact, such as stables, possibly involving fomites [2].
There have been no documented cases of bat-to-human transmission but horse-to-human transmission can occur when there is substantial direct exposure of secretions or tissue from an infected horse to a person's mucous membranes or non-intact skin [2]. Human infection ranges from self-limiting influenza-like illness to severe pneumonia and/or encephalitis. All human cases have had extensive close contact with an infected horse, such as performing endoscopy or post mortem examinations [2]. Two cases had close contact with a horse over the three days before its onset of symptoms, suggesting pre-clinical virus shedding may occur late in a horse's incubation period [13]. No infections have been documented in people with lower levels of exposure nor in those wearing appropriate personal protective equipment (PPE) and there is no evidence of human-to-human transmission to date [2].
In Australia and within NSW, Hendra virus is a notifiable disease in animals and humans under the Biosecurity (2015) and NSW Public Health Acts (2010) [14]. Horse-owners and veterinarians in Hendra virus regions are encouraged to minimise infection risk through equine vaccination and by distancing horses and feed from bat roosting sites. They must also utilise strict infection control and PPE when managing suspected or confirmed cases [15]. A safe and effective equine vaccine that requires annual boosters has been available since 2012 [16]. However concerns regarding cost, adverse events and a perception of minimal risk of infection have contributed to low vaccine uptake in some areas [17].
In Queensland, a monoclonal antibody therapy (m102.4) is available on compassionate grounds as post-exposure prophylaxis for human contacts with high levels of exposure to a Hendra-infected horse. Recent phase 1 trials found it to be safe and well-tolerated [18]. However, there is currently no specific proven treatment for humans or horses once infected, making routine prevention and swift control measures critical.
2. Event
On the morning of Friday, 7 June 2019, an unvaccinated mare from a property near Scone, NSW, Australia, was noted to be lethargic. Over the day, she became progressively ataxic, developed excessive salivation, noisy respiration and progressed to lateral recumbency. The mare was euthanised that night, less than 24 h from onset of signs.
Scone, situated in the Upper Hunter Valley region of NSW, is the “horse capital of Australia.” It is home to many equine thoroughbred properties and has the largest equine veterinary practice in the southern hemisphere. Because equine Hendra virus infection had never been recorded so far south, and the water troughs and hand-feeding location for the affected horse were not located under possible bat feeding sites, the owners logically assessed the risk of Hendra virus to be very low. Nevertheless, the mare's clinical signs concerned the astute on-site veterinarian. This reduced further unnecessary close contact between persons and the mare prior to and following euthanasia, and the case was reported for Hendra virus exclusion.
NSW Department of Primary Industries (NSW DPI) and Hunter Local Land Services (Hunter LLS) were notified via the Emergency Animal Disease Hotline on the morning of Sunday 9 June. That afternoon, a District Veterinarian collected blood and nasal, oral and rectal swabs from the deceased horse using appropriate PPE. Hendra virus RNA was detected in all samples by real time reverse transcription PCR (qRT-PCR) [19] on the evening of Tuesday 11 June (Elizabeth Macarthur Agricultural Institute [EMAI], NSW, confirmed by Australian Animal Health Laboratory [AAHL], Victoria).
3. Response
An urgent One Health coordinated response involving human and animal health investigations commenced upon laboratory confirmation of the Hendra virus infection.
On Wednesday 12 June, a site visit was conducted by Hunter LLS and a Biosecurity Direction was implemented to limit animal movement on and off the property. Twenty-eight horses and two dogs were subject to health monitoring for 21 days. Infection control training and supplies were provided to minimise subsequent risk and enable safe management of animals under quarantine.
Contact tracing and interviews with ten human contacts were conducted by Hunter New England Public Health Unit and presented to a national Expert Panel consisting of human and animal health representatives. All ten contacts were assessed as having low, negligible or nil risk of exposure and therefore post-exposure prophylaxis was not indicated [2]. Public health unit staff visited the property to verify information, offer education and provide support. Contacts were followed up daily for symptoms for 21 days following exposure.
Investigation of flying fox activities commenced on Friday 14 June by a team of bat ecologists, involving observations and sampling from the property and nearby roosts.
It was anticipated that the event would generate public concern therefore media releases and extensive public communications were led by NSW DPI and Hunter LLS representatives. Information sessions were arranged for equine practitioners and thoroughbred industry representatives in the region, involving presentations from a bat ecologist, a veterinary disease ecologist, and the vaccine manufacturer.
4. Outcomes and lessons learned
Fortunately, no human or additional domestic animal cases occurred during or after the recommended period of animal quarantine and observation of human and animal contacts. The Biosecurity Direction ended on 2 August 2019.
One person developed mild, self-limiting respiratory symptoms during their observation period. Respiratory virus PCR on a throat swab detected rhinovirus and enterovirus, and anti-Hendra virus IgM and IgG antibodies were not detected in blood (Queensland Health Forensic and Scientific Services), therefore Hendra virus infection was excluded. Given the season, there was a high chance of respiratory tract illness from common winter pathogens, potentially complicating the monitoring of contacts.
Investigation by bat ecologists found that both black flying fox and grey-headed flying fox species were present in the Upper Hunter Valley at the time. Scone is located within the long-term range of grey-headed flying foxes and the species had been observed roosting on the affected property at various times over several decades. While black flying foxes had been recorded in roosts in the Lower Hunter Valley and Singleton since the early 2000s, they were first observed in the Upper Hunter Valley in the months before the spillover occurred.
The emergence of Hendra virus in the Hunter Valley, NSW, Australia, resulted in a substantial increase in horse populations, and thus humans, considered at risk of Hendra virus spillover, and has had major implications for agricultural and veterinary practices in the region. Nearly all major stud farms in the Hunter Valley adopted a uniform policy whereby they would not accept mares to be served that were not vaccinated against Hendra virus [20]. A 30-fold increase in equine vaccination uptake was seen in the Scone region over the 90 days following the event compared with the 90 days prior. [Zoetis – data on file] By comparison, previous similar events in Casino, NSW in 2016 and Bundaberg, Queensland in 2014 triggered only 18% and 22% increases in vaccine uptake, respectively.
The people who were potentially exposed in this incident experienced considerable stress throughout the event. Despite exposures and risk of infection being assessed as low, the potential consequences of infection would be catastrophic. Comprehensive exposure interviews and involvement of veterinarians and clinicians with experience from previous Hendra virus events was essential for accurate risk assessment and management of contacts. Skilled risk communication and consistent advice is imperative, especially regarding rare diseases where much is still unknown.
A multi-agency after-action review identified shared learnings and the need for ongoing collaboration. The deliberations of the Expert Panel showed that a contact's level of risk could be more confidently determined if the human health experts had greater familiarity with equine husbandry and veterinary activities. Therefore, NSW DPI and Hunter LLS have committed to develop a photographic and video library of such activities. Review of national Hendra virus public health guidelines [2], investigation and risk assessment tools was undertaken by NSW Health and Queensland Health with animal expert advice. Logistical planning has begun for the administration of monoclonal antibody m102.4 in NSW if required in future events.
5. Conclusion
This was the southernmost known equine Hendra virus case to date and has had major implications for animal and human health practices in the region. Successful management of the event was facilitated by interagency collaboration involving human and animal health experts. Ongoing One Health partnership is essential for successful responses to zoonotic events.
Funding
AJP was supported by an ARC DECRA fellowship (DE190100710). Bat fieldwork was funded by the DARPA PREEMPT program Cooperative Agreement # D18AC00031.
Declaration of Competing Interest
De-identified data on vaccination rates were supplied by Zoetis Inc. The authors declare no conflicts of interest. The content of the information does not necessarily reflect the position or the policy of the U.S. government, and no official endorsement should be inferred.
Acknowledgements
The authors would like to acknowledge the affected property owners, and Dr. Tali White, Professor Geoffrey Playford, the Hendra Expert Panel Group, Dr. Margaret Young, Dr. Richard L'Estrange, Elizabeth Macarthur Agricultural Institute and Queensland Health Forensic & Scientific Services.
Map created using ArcGIS® software by Esri. ArcGIS® and ArcMap™ are the intellectual property of Esri and are used herein under license. Copyright © Esri. All rights reserved. For more information about Esri® software, please visit www.esri.com
Contributor Information
K.M. Williamson, Email: kirsten.williamson@health.nsw.gov.au.
BatOneHealth field team:
Appendix A. Appendix
Fig. A1.
Location of known events of Hendra virus spillover to horses in Australia from August 1994 to June 2019. (Black dots represent locations where confirmed Hendra spillover events have occurred; derived from Queensland Government: ‘Summary of Hendra virus incidents in horses.’ [1] Note: Some towns/cities have had more than one spillover event; please see reference for details.)
References
- 1.Queensland Government Summary of Hendra Virus Incidents in Horses. https://www.business.qld.gov.au/industries/service-industries-professionals/service-industries/veterinary-surgeons/guidelines-hendra/incident-summary Last updated 20/06/2019. Accessed on 27/04/2020. Accessible at.
- 2.Communicable Diseases Network Australia [Internet] Canberra, ACT: Australian Government Department of Health. Series of National Guidelines – Hendra Virus. Version 3.0. https://www1.health.gov.au/internet/main/publishing.nsf/Content/cdna-song-hendra.htm Updated 2016 Nov 09 [cited 2020 Apr 25]. Accessible at.
- 3.Mahalingam S., Herrero L.J., Playford E.G., Spann K., Herring B., Rolph M.S. Hendra virus: an emerging paramyxovirus in Australia. Lancet Infect. Dis. 2012;12(10):799–807. doi: 10.1016/S1473-3099(12)70158-5. (Epub 2012/08/28) [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Hendra Virus Disease – Outbreak Distribution Map. https://www.cdc.gov/vhf/hendra/outbreaks/distribution-map.html Updated 17 March 2014 [cited 2020 Apr 27] Accessible at.
- 5.Field H. The University of Queensland; Brisbane, Australia: 2004. The Ecology of Hendra Virus and Australian Bat Lyssavirus. (PhD Thesis) [Google Scholar]
- 6.Plowright R., Field H., Smith C., Divljan A., Palmer C., Tabor G., Daszak P., Foley J. Reproduction and nutritional stress are risk factors for Hendra virus infection in little red flying foxes (Pteropus scapulatus) Proc. R. Soc. B Biol. Sci. 2008;275(1636):861–869. doi: 10.1098/rspb.2007.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edson D., Field H., McMichael L., Vidgen M., Goldspink L., Broos A., Melville D., Kristoffersen J., Jong C., McLaughlin A., Davis R., Kung N., Jordan D., Kirkland P., Smith C. Routes of Hendra virus excretion in naturally-infected flying-foxes: implications for viral transmission and spillover risk. PLoS One. 2015;10(10) doi: 10.1371/journal.pone.0140670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldspink L., Edson D., Vidgen M., Bingham J., Field H., Smith C. Natural Hendra virus infection in flying-foxes - tissue tropism and risk factors. PLoS One. 2015;10(6) doi: 10.1371/journal.pone.0128835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Field H., Jordan D., Edson D., Morris S., Melville D., Parry-Jones K. Spatiotemporal aspects of Hendra virus infection in pteropid bats (flying-foxes) in eastern Australia. PLoS One. 2015;10(12) doi: 10.1371/journal.pone.0144055. (Epub 2015/12/02) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin G., Plowright R., Chen C., Kault D., Selleck P., Skerratt L. Hendra virus survival does not explain spillover patterns and implicates relatively direct transmission routes from flying foxes to horses. J. Gen. Virol. 2015;96(6) doi: 10.1099/vir.0.000073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin G., Webb R., Chen C., Plowright R., Skerratt L. Microclimates might limit indirect spillover of the bat borne zoonotic Hendra virus. Microb. Ecol. 2017;74(1):106 115. doi: 10.1007/s00248-017-0934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kung N.Y.-H. Overview of Hendra Virus Infection. MSD Veterinary Manual. Oct 2014. https://www.msdvetmanual.com/generalized-conditions/hendra-virus-infection/overview-of-hendra-virus-infection [cited 2020 Apr 27] Accessible at.
- 13.Playford E.G., McCall B., Smith G. Human Hendra virus encephalitis associated with equine outbreak, Australia, 2008. Emerg. Infect. Dis. 2010;16(2):219–223. doi: 10.3201/eid1602.090552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biosecurity Act . 2015. (Cth) Schedule 2, Part 1. [Google Scholar]
- 15.NSW Department of Primary Industries The General Biosecurity Duty. www.dpi.nsw.gov.au/biosecurity/managing-biosecurity/the-general-biosecurity-duty [cited 2020 Apr 26] Accessible at.
- 16.Queensland Agriculture and Environment Committee Hendra Virus EquiVac Vaccine and Its Use by Veterinary Surgeons in Queensland. https://www.parliament.qld.gov.au/Documents/TableOffice/TabledPapers/2016/5516T1889.pdf Report No. 24, 55th Parliament Agriculture and Environment Committee October 2016. Accessible at.
- 17.Manyweathers J., Field H., Longnecker N. “Why won't they just vaccinate?” Horse owner risk perception and uptake of the Hendra virus vaccine. BMC Vet. Res. 2017;13:103. doi: 10.1186/s12917-017-1006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Playford E.G., Munro T., Mahler S.M., Elliott S., Gerometta M. Safety, tolerability, pharmacokinetics, and immunogenicity of a human monoclonal antibody targeting the G glycoprotein of henipaviruses in healthy adults: a first-in-human, randomised, controlled, phase 1 study. Lancet Infect. Dis. 2020 April 01;20(4):445–454. doi: 10.1016/S1473-3099(19)30634-6. [DOI] [PubMed] [Google Scholar]
- 19.Kirkland P.D., Gabor M., Poe I., Neale K., Chaffey K., Finlaison D.S., Gu X., Hick P.M., Read A.J., Wright T., Middleton D. Hendra virus infection in dog, Australia 2013. Emerg. Infect. Dis. 2015 Dec;21(12):2182–2185. doi: 10.3201/eid2112.151324. http://wwwnc.cdc.gov/EID/article/21/12/15-1324-Techapp1.pdf technical appendix. Accessible at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Queensland Racing Integrity Commission Hunter Valley Breeders Take on the Hendra Virus Threat. https://qric.qld.gov.au/news/hunter-valley-breeders-take-on-the-hendra-virus-threat/ Published 12 July 2019 (cited 2020 Apr 24) Accessible at.