Abstract
Tuberculosis (TB) in humans is primarily caused by Mycobacterium tuberculosis (M. tuberculosis), with millions of infections and hundreds of thousands of deaths worldwide. It creates a substantial economic burden on the community. Unlike M. tuberculosis, Mycobacterium bovis infects cattle and causes bovine TB, also known as zoonotic TB. People can contract zoonotic TB after consumption of unpasteurized dairy products, handling the sick animals, and via occupational exposures. The association between the zoonotic TB in humans and cattle is not well known in Nepal. The study examined the associated risk factors, including exposure to infected cattle, that contribute to TB's development in human beings in Nepal.
The study consists of human and animal subjects. Firstly, a retrospective matched case-control study was conducted at the National Tuberculosis Center (NTC), Bhaktapur, Nepal. A total of 290 people (equal numbers of TB cases and control subjects) were interviewed to obtain information on socio-demographic, behavioral, and occupational risks, including the history of cattle related exposures. Secondly, a cross-sectional study was performed among the cattle owned by the TB-confirmed patients. Comparative tuberculin skin test, rapid antibody test, and ELISA were used in parallel to detect M. bovis infection in cattle.
The risk factors for the development of TB in humans were smokers (OR = 4.6, 95% CI: 2.1–10.0, p < 0.001), previous history of TB (OR = 7.9, 95% CI: 3.0–20.6, p < 0.001) and history of cattle exposures (OR = 3.9, 95% CI: 2.1–7.4, p = 0.001). Out of 123 cattle sampled, 12 cattle (9.76%, 95% CI: 5.37–16.76, p < 0.0001) were positive by the tuberculin test, 46 (37.4%, 95% CI: 28.97–46.62, p = 0.007) were tested positive by the rapid test, and 7 (5.7%, 95% CI: 2.52–11.80, p < 0.0001) by ELISA test. The inter-test agreement between the tuberculin and ELISA was very strong (κ = 0.72, 95% CI: 0.48–0.95, p < 0.01).
This study indicates that exposure to infected cattle and socio-demographic risk factors can contribute to the development of TB in human beings.
Keywords: Bovine tuberculosis, Cattle, Human, Risk factors
1. Introduction
Tuberculosis (TB) in humans is mainly caused by Mycobacterium tuberculosis, a member of the Mycobacterium tuberculosis complex (MTBC) bacteria, which has a global importance [1,2]. It is estimated that approximately 10 million people fall ill with TB worldwide annually, and the disease is one of the top ten lethal diseases in the human population [3]. The annual economic burden of TB is estimated at over $12 billion [4].
In Nepal, TB remains a major public health problem. Approximately 117,000 people lived with TB in 2019. The prevalence and incidence of TB in Nepal was estimated as 416 per 100,000 population and 245 per 100,000 person-years, respectively [5]. As per the Global TB report 2019, as many as 7000 people die annually from TB in Nepal. Numerous studies identified sociodemographic, environmental, and behavioral risk factors such as age, sex, occupations, indoor air pollutions, smoking, and alcohol consumption [[6], [7], [8], [9], [10], [11], [12]] as being associated with the development of TB in humans.
Additionally, cattle-related exposures could be a potential risk factor associated with TB in human beings [[13], [14], [15]]. When the cattle become infected with M. bovis, another member of the MTB complex, develops TB known as Bovine tuberculosis (bovine TB). The bovine TB, also known as zoonotic TB, transmitted to human beings mainly through the consumption of unprocessed dairy products, occupational exposure to livestock, and less commonly through the ingestion of untreated meat products [16]. The overall proportion of zoonotic TB infections among humans globally has been underestimated in developing countries like Nepal, due to the lack of information among public health officials [[17], [18], [19], [20], [21]]. Zoonotic TB accounted for an estimated 147,000 new human cases and 12,500 deaths globally in 2016 [22]. It was estimated that between 0.4% and 10% of TB cases in Africa are zoonotic [23,24].
There are few studies on bovine TB in animal health, information on the disease in humans in Nepal is almost absent. For instance, Jha et al. [25] isolated M. bovis strains in Kathmandu and Kaski from limited cattle and buffalos' samples in 2007. A cross-sectional study conducted by Pandey et al. [26] in Chitwan reported the prevalence of bovine TB was up to 15% in 100 cattle sampled. However, due to the lack of a coordinated national surveillance program on bovine TB in human health and animal health services, the exact prevalence of bovine TB is unknown either in human or animal populations. More importantly, there is no provision of differentiating the TB in humans, either that is caused by M. tuberculosis or M. bovis (personal communication with the director of National TB Center, Nepal) [27]. It is a challenging issue because the physician develops almost the same treatment plans for both types of TB, even though, M. bovis is naturally resistant to pyrazinamide, one of the four medications used in the standard first-line anti-tuberculosis treatment regimen. It is a big gap behind the patient's effective treatment and timely recovery [28].
A multisector collaboration among the World Health Organization (WHO), World Organization for Animal Health (OIE), Food and Agriculture Organization (FAO) and the International Union Against Tuberculosis and Lung Disease (The Union) had launched a road map of zoonotic tuberculosis in 2017 [22]. The road map focuses on the priorities of increasing the scientific evidence by collecting complete and accurate data, reduce the transmission of zoonotic TB at the animal and human interface that ensure the food safety through collaborative engagements [29]. In 2014, WHO launched the End TB strategy and it is expected that the world would be free of TB by 2035 [30].
This research attempts to explore potential sociodemographic, behavioral, and environmental risk factors such as age, gender, level of education, occupations, smoking habits, and animal-associated risk factors such as exposure with diseased cattle, consumption of raw dairy products related to TB in humans. It also attempts to link the bovine TB in cattle with TB in people by estimating the prevalence of bovine TB in cattle owned by the TB patients in Kathmandu Valley (consisting of Kathmandu, Bhaktapur, Lalitpur) and Kavre district. Our study can be an example of a One Health approach linking zoonotic disease with public health and finding common ground for the solutions.
2. Methods
2.1. Study site
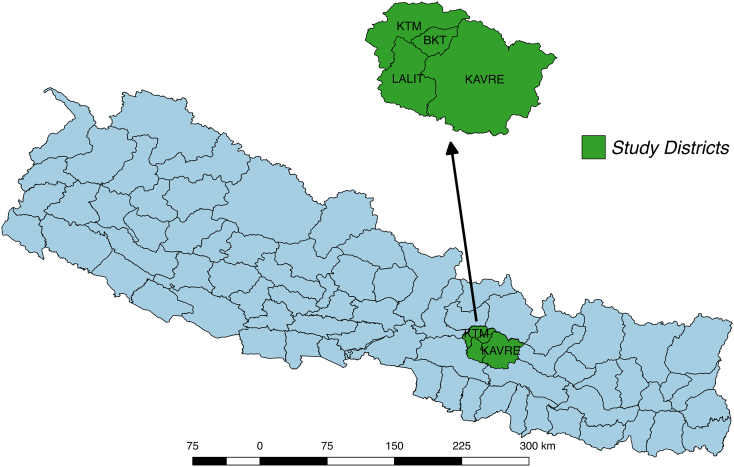
The study was conducted at the National Tuberculosis Center (NTC), Bhaktapur district and cattle farms of Kathmandu valley (Kathmandu, Bhaktapur and Lalitpur) and Kavre district of Nepal (Fig. 1). The Kathmandu valley was selected as the study site because it constituted more than 2.5 million people and contained Nepal's capital city [31]. Kavre is an adjacent district to Kathmandu with many livestock, such as cattle and buffaloes [32].
Fig. 1.
A map of Nepal with districts selected for the study.
2.2. Study design
The study is based on the One Health approach that has mainly the following components: i) the human subjects and their socio-demographic information, ii) animal subjects, and their farm management system. The human part involves a retrospective case-control study, and the cattle component consists of a cross-sectional study nested within the human element. In the case-control study, the cases were TB patients receiving or had received treatment at the National Tuberculosis Center (NTC) during January 2018 and December 2019. Since NTC receives the TB referral cases from all over the country, the cases represent the general population. The controls selected were relatives of non-TB patients matched with on average of 15-year band, and residing to the same local unit within the district with the cases [7,12]. The respondents were not matched with sex as it may be the potential risk factors and may confound other variables. The non-TB patients were confirmed negative to TB at the National Tuberculosis Center, Bhaktapur, Nepal.
The demographic, socio-economic, behavioral, and occupational information of all the respondents was collected using paper-based questionnaires at NTC. The survey was initially designed in English and later translated to Nepali (S1 file). It was pretested with a small group of suspected TB patients at Kalimati Chest Hospital, Kathmandu. The response rate and clarity of the questions were assessed to refine the survey questions. A sample of 5–10 responses were obtained, coded, and analyzed. Items that did not provide useful data were discarded, and the questionnaire was revised to give a final structure. However, no physical samples were collected from TB patients.
2.2.1. Sampling and sample size calculation for human subjects
The sample size was calculated using online epidemiological software (Open Epi 3.01) based on 80% power of detecting a difference, the hypothetical proportion of controls with exposure at 40%, and keeping equal ratio (1:1) of case and controls. It produced 290 samples with 145 cases and 145 control subjects altogether.
2.2.2. Selection of the risk factors
The risk factors were categorized under the broad categories of demographic (ethnicities, joint or nuclear family, family size, urban or rural residence, type of district located), socioeconomic status (occupations, education level), and behavioral health-related factors (habit of alcohol consumption, previous TB history, raw dairy products consumptions) [7,15,33]. The variables such as having cattle at home, contact with neighbor's cows, work at the cattle farm, and consumption of unpasteurized dairy products were highly associated. These variables were merged to a single risk factor mentioned as “joint cattle exposure status.”
2.2.3. Animal component and sampling process
We visited the houses of every human case interviewed at the NTC, to assess the cattle exposures around their area. Simultaneously, we performed skin testing and blood collection form the cattle owned by them. If we did not see any cows at their homes, we selected the nearest cattle farms from their homes. We consider 500 m as the cut off for “one village management unit” where people generally walk freely and reach house of one another within this area. We tried to choose one cattle farm on average for one village management unit such that altogether it produced at least 145 cattle farms. But some of the cases and control residence overlapped within 500-meter distance; and some of the farm owners were not at home, resulting in only 123 cattle farm selection. In total, we were able to perform skin testing and blood collection on 123 cattle.
2.2.4. Single intradermal comparative tuberculin test (SICTT)
This method required avian and bovine TB antigens in separate vials of 2000 IU each. Two injection sites on the neck of cattle, at a distance of twelve cm from another, were prepared by clipping and cleaning the skin. 0.2 ml of bovine and avian tuberculin were injected intradermally with the help of a registered veterinarian. The Vernier caliper was used to measure the initial thickness of cattle's skin at the tuberculin injection site. And at the same time, 10 ml of blood was collected from the animals for further blood-based assay. The tuberculin injections sites were read after 72 h to measure the increase in skin thickness at injections locations. Any increase in skin thickness between the avian and the bovine tuberculin ≥4 mm was considered positive, < 4 mm to >2 mm was deemed inconclusive, and ≤ 2 mm was considered negative [34,35].
2.2.5. Laboratory testing of samples
The Whole blood samples collected from each cattle were transported to Central Veterinary Laboratory (CVL), Kathmandu, by maintaining a cold chain for further laboratory testing. Firstly, sera were separated from the whole blood and tested against the bovine TB with a commercially available rapid test kit supplied from Bionote, Inc. (Animal Genetics, Inc., Korea). The result was interpreted after 20 min. Next, the serum samples, including the positives at rapid test, were subjected to M. bovis antibody ELISA (IDEXX Laboratories, Inc. The Netherlands) at CVL to detect bovine TB antibodies in them.
2.2.6. Ethical approval
Ethical statements for human and animal subjects were approved by the Nepal Health Research Council (NHRC), Nepal (Ref. No 703/2018), and Nepal Veterinary Council (NVC) Ref. No 246/2018, respectively. Written consent of each human patient and the cattle owner were obtained before the interview. Two experienced veterinarians handled the animals for the skin test and blood collection.
2.2.7. Statistical analysis
The data collected from the questionnaire were recorded in a spreadsheet and cleaned for the final analysis. The descriptive analysis was performed using R Studio Version 1.2.52019. Subsequently, the data were analyzed using the conditional logistic regression by clogit function in STATA 14.2.
Initially, a descriptive study of the sociodemographic factors such as age, sex, education level, occupation, ethnicity, family type, and habit of dairy product consumption was performed (Table 1). The potential confounding effects of the variables such as age, sex, BCG vaccination history, smoking, and alcohol consumption habits were checked with the changes in the point estimates of the variables that remain in the model [36,37]. Any changes in the coefficient with >20% were included in the final model.
Table 1.
Socio-demographic and behavioral distribution of the humans with and without TB disease at Kathmandu valley and Kavre district in Nepal.
| Determinants | Total (N = 290) |
Cases (n = 145) |
Controls (n = 145) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age category (Mean age = 37.27 years) | |||
| 1–15 | 11 (3.8) | 6 (4.1) | 5 (3.4) |
| 16–30 | s127 (43.8) | 70 (48.3) | 57(39.3) |
| 31–45 | 64 (22.1) | 25 (17.2) | 39 (26.9) |
| 46–60 | 53 (18.3) | 21 (14.5) | 32 (22.1) |
| 61–75 | 26 (9.0) | 18 (12.4) | 8 (5.5) |
| >75 | 9 (3.1) | 5 (3.4) | 4 (2.8) |
| Sex | |||
| Female | 129 (44.5) | 61 (42.1) | 68 (46.9) |
| Male | 161 (55.5) | 84 (57.9) | 77 (53.1) |
| Education level | |||
| Illiterate | 74 (25.5) | 38 (26.2) | 36 (24.8) |
| Literate (without formal education) | 36 (12.4) | 16 (11.0) | 20 (13.8) |
| Primary level | 59 (20.3) | 32 (22.1) | 27 (18.6) |
| Secondary level | 54 (18.6) | 23 (15.9) | 31 (21.4) |
| Higher Secondary (+2) | 31 (10.7) | 14 (9.7) | 17 (11.7) |
| University | 36 (12.4) | 22 (15.2) | 14 (9.7) |
| Occupation | |||
| Housewives | 65 (22.4) | 19 (13.1) | 46 (31.7) |
| Farmer | 43 (14.8) | 21(14.5) | 22 (15.2) |
| Business | 22 (7.6) | 11 (7.6) | 11 (7.6) |
| Student | 54 (18.6) | 35 (24.1) | 19 (13.1) |
| Others (drivers, labors, service people) | 106 (36.6) | 59 (40.7) | 47 (32.4) |
| Ethnicity | |||
| Janajati | 203(70.0) | 98 (67.6) | 105 (72.4) |
| Bhramin | 39 (13.4) | 17 (11.7) | 22 (15.2) |
| Chettri | 29 (10.0) | 18 (12.4) | 11 (7.6) |
| Dalit | 12 (4.1) | 7 (4.8) | 5 (3.4) |
| Others | 7 (2.4) | 5 (3.4) | 2 (1.4) |
| Residence | |||
| Rural | 90 (31.0) | 41(28.3) | 49 (33.8) |
| Urban | 200 (69.0) | 104 (71.7) | 96 (66.2) |
| BCG vaccination history | |||
| Yes | 111(38.3) | 59 (40.7) | 52 (35.9) |
| No | 72 (24.8) | 37 (22.5) | 35 (24.1) |
| Don't remember | 107 (36.9) | 49 (33.8) | 58 (40.0) |
| Family type | |||
| Joint | 132 (45.5) | 61(42.1) | 71 (49.0) |
| Nuclear | 158 (54.5) | 84 (57.9) | 74 (51.0) |
| Family size | |||
| 1–3 | 62 (21.4) | 36 (24.8) | 26 (17.9) |
| 4–6 | 162 (55.9) | 79 (54.5) | 83 (57.2) |
| 7–9 | 66 (22.8) | 30 (20.7) | 36 (24.8) |
| Smoking habit before | |||
| Yes | 75 (25.9) | 52 (35.9) | 23 (15.9) |
| No | 215 (74.1) | 93 (64.1) | 122 (84.1) |
| Alcohol consumption habit before | |||
| Yes | 86 (29.7) | 48 (33.1) | 38 (26.2) |
| No | 204 (70.3) | 97 (66.9) | 107 (73.8) |
| Previous TB History | |||
| Yes | 46 (15.9) | 39 (26.9) | 7 (4.8) |
| No | 244 (84.1) | 106 (73.1) | 138 (95.2) |
| Contact with cattle or unpasteurized dairy product consumption | |||
| Yes | 156 (53.8) | 93(64.1) | 63 (43.4) |
| No | 134 (46.2) | 52(35.9) | 82 (56.6) |
| Locations | |||
| Kathmandu | 113 (39.0) | 61 (42.1) | 52 (35.9) |
| Bhaktapur | 96 (33.1) | 49 (33.8) | 47 (32.4) |
| Lalitpur | 44 (15.2) | 21 (14.5) | 23 (15.9) |
| Kavre | 37 (12.8) | 14 (9.7) | 23 (15.9) |
Next, the univariable conditional logistic regression analysis was performed to compare the cases and controls separately to the outcome. The Chi-square tests were used to identify associations between variables. The associated variables with p-values ≤0.2 at univariable analysis including the potential confounders, were selected for the final multivariable conditional logistic regression model.
For the cattle data, the study was performed with variables related to animal characteristics and their relations to estimated prevalence against the parallel testing of tuberculin, rapid test, and ELISA. The inter-test agreements among the tuberculin, rapid diagnostic test, and indirect ELISA were calculated by Kappa statistic [36,38].
3. Results
The descriptive analysis showed that the mean age of people interviewed was 37.27 (95% CI: 35.3, 39.3) years. The proportion of female and male subjects in the study was 0.44 (129/290) and 0.56 (161/190). The percent of cases selected in females and males, were 42.1% (61/145) and 57.93% (84/145).
Of the total TB case interviewed, 26.2% (38/145) were the illiterate people, 11.0% (16/145) of the people were literate without a formal education, and 69.2% (91/145) of the people were educated with at least primary level education (Table no 1). Among the different occupation brackets, students (35/145; 24.1%), farmers (21/145; 14.5%) and housewives (19/145;13.1%) had a higher proportion of TB than other professions. TB patients interviewed belonged to major ethnic communities such as Janajati (98/145; 67.59%), Chettri (18/145;12.41%), Bhramin (17/145; 11.72%), Dalit (7/145; 4.8%) and others (5/145; 3.4%). Most of the cases (104/145; 71.72%) were from urban settings such as big cities of the Kathmandu valley, and the remaining cases were from the rural area of Kavre district (41/145;28.3%). Although, 40.69% (59/145) of the cases mentioned that they had their BCG vaccination, the remaining of cases either did not have or could not remember their vaccination status. More than half of the cases (9/145,54.5%) mentioned, that they had 4 to 6 members their family.
Some, 35.9% (52/145) of the cases had a smoking habit, while 33.10% (48/145) of them had habit of alcohol consumption. Of the total cases, 26.9% (39/145) mentioned that they had previously contracted TB. Interestingly, 64.1% (93/145) of the cases had a recent history of cattle-related exposures, such as handling the sick cattle and consuming unpasteurized dairy products.
The initial screening of variables identified, such as age, sex, occupations, and habit of drinking alcohol as the confounders, and they were retained in the final multivariable model, even though they were not significant at the univariable conditional logistic regression analysis.
Final multivariable conditional logistic regression analysis indicated that people with smoking habits (OR = 4.6, 95% CI: 2.1, 10.0, p < 0.001) had four-fold odds of developing TB than people who did not smoke. People who had previous TB history were almost eight times (OR = 7.9, 95% CI: 3.0, 20.6, p < 0.001) at risk of contracting TB than those with no prior TB history. Importantly, the people who had prior repeated contact with the sick cattle and consumption of unpasteurized dairy products had higher odds (OR = 3.9, 95% CI: 2.1, 7.4, p < 0.001) of developing TB compared to those who had no history of cattle exposure (Table 2).
Table 2.
Results of multivariable analysis of the socio-economic and behavioral habit tested for association with development of TB among humans at Kathmandu valley and Kavre district in Nepal.
| Determinants | Case (n = 145) | Control (n = 145) | adjusted OR | 95% CI | P value |
|---|---|---|---|---|---|
| Smoking habit | |||||
| Yes | 52 | 23 | 4.6 | (2.1, 10.0) | <0.001* |
| No | 93 | 122 | |||
| Previous TB history | |||||
| Yes | 39 | 7 | 7.9 | (3.0, 20.6) | <0.001* |
| No | 106 | 138 | |||
| Contact with sick cattle or consumption of raw dairy products | |||||
| Yes | 93 | 63 | 3.9 | (2.1, 7.4) | <0.001* |
| No | 52 | 82 |
Of 123 cattle, tested against bovine TB by the comparative tuberculin test, 12 (9.76%, 95% CI: 5.37–16.76, p < 0.0001) of the cattle were deemed positive or reactive (Table 3). The distribution of the positive case based on various animal characteristics are depicted as following (Table 3).
Table 3.
Cattle characteristics and bovine TB status according to tuberculin testing at Kathmandu valley and Kavre district in Nepal.
| Determinants | Classification of TB status by tuberculin test |
|||
|---|---|---|---|---|
| Positive (n = 12), (≥ 4 mm) | Inconclusive (n = 11), (>2 mm and < 4 mm) | Negative (n = 100), (<2 mm) | Total no cattle tested (N = 123) | |
| Age category | ||||
| 1_3 | 3 | 3 | 29 | 35 |
| 4_6 | 5 | 6 | 42 | 53 |
| 7_9 | 4 | 2 | 29 | 35 |
| Herd_size | ||||
| <5 | 2 | 5 | 37 | 44 |
| 5_10 | 6 | 2 | 26 | 34 |
| 11_15 | 0 | 2 | 15 | 17 |
| >15 | 4 | 2 | 22 | 28 |
| Body condition | ||||
| Good | 2 | 1 | 10 | 13 |
| Medium | 6 | 6 | 69 | 81 |
| Poor | 4 | 4 | 21 | 29 |
| Husbandry practice | ||||
| Intensive or stall fed | 10 | 9 | 84 | 103 |
| Semi-intensive or mixed | 2 | 2 | 16 | 20 |
| 1Breed | ||||
| Holstein cross | 2 | 1 | 23 | 26 |
| Jersey cross | 8 | 6 | 62 | 76 |
| Local | 2 | 4 | 15 | 21 |
| Coughing history | ||||
| Yes | 7 | 5 | 31 | 43 |
| No | 5 | 6 | 69 | 80 |
| Animal Origin | ||||
| Home breed | 4 | 4 | 30 | 38 |
| Imported | 8 | 7 | 70 | 85 |
| Grand Total | 12 | 11 | 100 | 123 |
Out of total 123 cattle serum samples, tested by rapid test methods and ELISA, 46 (37.4%, 95% CI: 28.97–46.62, p = 0.007) and 7 (5.7%, 95% CI: 2.52–11.80, p < 0.0001) of the samples showed positive results respectively (Table 4). The detail animal characteristics and production systems with the seropositive cattle were mentioned as follows (Table 4).
Table 4.
Cattle characteristics and bovine TB status according to Rapid test and ELISA Test at Kathmandu valley and Kavre district in Nepal.
| Determinants |
Classification status by rapid test |
Classification status by ELISA test |
|---|---|---|
| Total Cattle Tested (N) = 123 | Positive = 46 (37.4%) | Positive = 7 (5.7%) |
| Age category (years) | ||
| 1_3 | 8 (6.5) | 1 (0.81) |
| 4_6 | 21 (17.07) | 2 (1.63) |
| 7_9 | 17 (13.82) | 4 (3.25) |
| Herd size | ||
| <5 | 18 (14.63) | 1 (0.81) |
| 5_10 | 16 (13.01) | 2 (2.44) |
| 11_15 | 4 (3.25) | 0 (0) |
| >15 | 8 (6.59) | 3 (2.44) |
| Body condition | ||
| Good | 9 (7.32) | 2 (1.63) |
| Medium | 24 (19.51) | 3 (2.44) |
| Poor | 13 (10.57) | 2 (1.63) |
| Husbandry practice | ||
| Intensive | 38 (30.89) | 6 (4.88) |
| Semi intensive | 8 (6.51) | 1 (0.81) |
| Breed | ||
| Holstein cross | 9 (7.32) | 1 (0.81) |
| Jersey cross | 29 (23.58) | 5 (4.1) |
| Local | 8 (6.50) | 1 (0.81) |
| Coughing history | ||
| Yes | 17 (13.82) | 5(4.15) |
| No | 29 (23.58) | 2 (1.62) |
| Animal Origin | ||
| Imported | 36 (29.27) | 1 (0.81) |
| Home breed | 10 (8.13) | 6 (4.88) |
3.1. Inter-test Agreement among tuberculin test, rapid test and indirect ELISA
There is a fair kappa agreement between the two tests: the tuberculin test and rapid test (κ = 0.32, 95%CI: 16–0.45, p < 0.001). While, there is only a slight kappa agreement between the rapid test and ELISA (κ = 0.18, 95%CI: 0.06–0.31, p = 0.003). However, there is a substantial agreement between the tuberculin tests and ELISA test (κ = 0.72, 95% CI: 0.48–0.95, p < 0.01), which indicates substantial agreement between these two tests [36,38].
4. Discussion
The people who used to smoke had four-fold odds of developing TB compared to those who never smoked. This finding was supported by many systematic reviews, meta-analysis, and the original research articles. [11,[39], [40], [41], [42]].
The people who had previous TB history, were significantly eight times more likely to develop TB again in life compared to those who had no prior history of TB. The finding was consistent with the study by Kapoor et al. [43] and Marahatta [42], who mentioned that people with previous TB had chances of recurrent episodes.
More importantly, those who had either a history of exposure to sick cattle or consumption of raw dairy products or cattle-rearing at their homes were four folds more likely to develop TB than those who had no history of cattle exposures. Case-control studies in Ethiopia by Fetene et al. [13] and Mengistu et al. [14] found a strong positive association (OR = 3.23, P < 0.001,) and (OR = 8.32, 95% CI; 2.82–24.60) between exposure to bovine TB and TB disease in humans respectively.
The findings support a meta-analysis of Muller et al. [17] who suggested that more than 2% of human TB cases worldwide could be attributed to zoonotic tuberculosis, with higher levels in developing countries. In Asia, around 94% of the people live in countries where bovine TB control programs in cattle and buffalo are almost absent [19]. Our study outcome is in line with several other studies that mentioned that consumption of unpasteurized dairy products and people involved in infected cattle rearing could be one of the most important risk factors for humans to develop bovine TB (zoonotic TB) [21,44,45].
Finally, our study depicts as high as 9.8, and 5.7 percentage of cattle tested positive by tuberculin tests and ELISA, respectively of the cattle owned by the family of TB infected persons. Also, there is good agreement between the tuberculin and ELISA but poor agreement with the rapid tests. If we could incorporate more standard diagnostic tests such as gamma interferon assay for the disease diagnosis, it would improve the tests' overall sensitivity. This seropositivity indicated an association of cattle exposure and the development of TB in human beings in Kathmandu valley and Kavre, Nepal. So, there might be a substantial contribution of M. bovis in Nepal's total proportion of human TB.
5. Limitation of study
There is no provision of differentiating M. bovis and M. tuberculosis in the National Tuberculosis Center (NTC) at routine culturing because the method of culture for M. bovis is different from that of M. tuberculosis. We could not provide the molecular evidence of the shared strain of M. bovis infection between humans and cattle. For this, NTC and CVL should establish the culture and molecular detection methods of M. bovis in human and animal samples, respectively. We tried to minimize the information bias in selecting controls by collecting enough information on the exposure status; however, some recall bias might occur there.
6. Conclusion
In addition to the socio-demographic, environmental, and behavioral risk factors, the exposure to infected cattle and consumption of unprocessed dairy products leads to the contribution of the development of TB in human beings. An effective control program of bovine TB in livestock populations could curtail the number of TB cases in Nepal. Maintaining the bovine TB free cattle herds would ensure people's good health and accentuates cattle products' trade outside the country. A joint program needs to be implemented among animal, human, and environmental sectors through One Health approach to reduce the TB burden of Nepal.
7. Recommendations
Nepal is one of the members of OIE, WHO, and FAO. An integrated surveillance plan for bovine TB should be initiated among animal, human, and environmental sectors based on the One Health aspects. The inter-collaborative programs should be launched to estimate the true prevalence of zoonotic TB in animals and actual proportions in human TB patients. The government should fund the studies of bovine Tuberculosis both in animal and human health. Nepal government approved the One Health Strategy Framework in 2019, and it should be implemented for the control of bovine Tuberculosis in Nepal. Since cattle owning is related to the religious and cultural practice of many people here, the bovine TB management could be a challenging job. A group of anthropologists, social workers, and veterinarians should jointly address the related cultural issues and advocate removing infected cattle from the herds. Moreover, we suggest a robust plan for prospective research on bovine or zoonotic TB work in Nepal.
Funding resources
The study was partially funded by Nepal Academy of Science and Technology (NAST), Lalitpur after the first author (TRG) was selected through a nation-wide, competitive individual research grant 2018, Lalitpur, Nepal.
Declaration of Competeing Interest
The authors declare no competing interest.
Acknowledgments
Acknowledgement
We want to acknowledge all families who agreed to participate in the TB study, and the farmers who willingly allowed research on their animals. Again, we want to recognize Mr. Dinesh Joshi, Dr. Rabina Ghimire, Dr. Suresh Burlakoti, Dr. Urmila Pokhrel who helped us in the sample collections and tuberculin testing. We are grateful to Dr. Francsico Olea Popelka, Dr. Laura Rosen, and Dr. Catherine Davis of Colorado State University, USA, for their contributions in the preliminary reviewing of this article. We want to thank Dr. Bhim Singh Tikari, former director of Nepal Tuberculosis Center, and all lab staff of NTC who helped us making the availability of lab reports during the study period.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.onehlt.2020.100156.
Appendix A. Supplementary materials
(S1):Questionnaire used for interviewing human subjects.
Appendix B. Research data (R1)
The data for this article can be accessed through the GitHub repository at: https://github.com/tulsiramgompo/human_tb_and_cattle_tb.
References
- 1.Briken V., Miller J.L. Living on the edge: inhibition of host cell apoptosis by Mycobacterium tuberculosis. Future Microbiol. 2008;3:415–422. doi: 10.2217/17460913.3.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schöning J.M., Cerny N., Prohaska S., Wittenbrink M.M., Smith N.H., Bloemberg G. Surveillance of bovine tuberculosis and risk estimation of a future reservoir formation in wildlife in Switzerland and Liechtenstein. Gordon SV, editor. PLoS One. 2013;8 doi: 10.1371/journal.pone.0054253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global tuberculosis report WHO. 2019. https://www.who.int/tb/publications/global_report/en/ Available:
- 4.McLaren Z.M., Milliken A.A., Meyer A.J., Sharp A.R. Does directly observed therapy improve tuberculosis treatment? More evidence is needed to guide tuberculosis policy. BMC Infect. Dis. 2016;16:537. doi: 10.1186/s12879-016-1862-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National TB Prevalence Survey National Tuberculosis Control Centre. 2018/2019. https://nepalntp.gov.np/wp-content/uploads/2020/03/TBPS-Summary-Report_English_Final_21-March-2020_compressed.pdf Available.
- 6.Lienhardt C., Fielding K., Sillah J., Bah B., Gustafson P., Warndorff D. Investigation of the risk factors for tuberculosis: a case–control study in three countries in West Africa. Int. J. Epidemiol. 2005;34:914–923. doi: 10.1093/ije/dyi100. [DOI] [PubMed] [Google Scholar]
- 7.Shetty N., Shemko M., Vaz M., D’Souza G. An epidemiological evaluation of risk factors for tuberculosis in South India: a matched case control study. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2006;10:80–86. [PubMed] [Google Scholar]
- 8.Lönnroth K., Jaramillo E., Williams B.G., Dye C., Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc. Sci. Med. 2009;68:2240–2246. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 9.Nava-Aguilera E., Andersson N., Harris E., Mitchell S., Hamel C., Shea B. Risk factors associated with recent transmission of tuberculosis: systematic review and meta-analysis. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2009;13:17–26. [PubMed] [Google Scholar]
- 10.Pokhrel A.K., Bates M.N., Verma S.C., Joshi H.S., Sreeramareddy C.T., Smith K.R. Tuberculosis and indoor biomass and kerosene use in Nepal: a case–control study. Environ. Health Perspect. 2010;118:558–564. doi: 10.1289/ehp.0901032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Narasimhan P., Wood J., MacIntyre C.R., Mathai D. Risk factors for tuberculosis. Pulm Med. 2013;2013:1–11. doi: 10.1155/2013/828939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murakami R., Matsuo N., Ueda K., Nakazawa M. Epidemiological and spatial factors for tuberculosis: a matched case-control study in Nagata, Japan. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2019;23:181–186. doi: 10.5588/ijtld.18.0369. [DOI] [PubMed] [Google Scholar]
- 13.Fetene T., Kebede N., Alem G. Tuberculosis infection in animal and human populations in three districts of Western Gojam, Ethiopia: tuberculosis infection in animal and human populations in three districts. Zoonoses Public Health. 2011;58:47–53. doi: 10.1111/j.1863-2378.2009.01265.x. [DOI] [PubMed] [Google Scholar]
- 14.Mengistu A., Enquselassi F., Aseffa A., Beyen D. Bovine tuberculosis (BTB) as a risk factor for developing tuberculosis in humans in the rural community of Ethiopia: a case-control study. Ethiop. Med. J. 2015;53:1–8. [PubMed] [Google Scholar]
- 15.Meisner J., Curtis K., Graham T.W., Apamaku M.B., Manhart L.E., Rabinowitz P.M. Cattle-associated risk factors for human tuberculosis in rural livestock-keeping communities, Uganda. Zoonoses Public Health. 2019;66:73–82. doi: 10.1111/zph.12530. [DOI] [PubMed] [Google Scholar]
- 16.Ayele W.Y., Neill S.D., Zinsstag J., Weiss M.G., Pavlik I. Bovine tuberculosis: an old disease but a new threat to Africa. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2004;8:924–937. [PubMed] [Google Scholar]
- 17.Müller B., Dürr S., Alonso S., Hattendorf J., Laisse C.J.M., Parsons S.D.C. Zoonotic Mycobacterium bovis –induced tuberculosis in humans. Emerg. Infect. Dis. 2013;19:899–908. doi: 10.3201/eid1906.120543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thoen C.O., Steele J.H., Kaneene J.B. Zoonotic Tuberculosis: Mycobacterium Bovis and Other Pathogenic Mycobacteria. 2014. http://public.eblib.com/choice/publicfullrecord.aspx?p=4035671 Available:
- 19.Cosivi O. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries. Emerg. Infect. Dis. 1998;4:59–70. doi: 10.3201/eid0401.980108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pérez-Lago L., Navarro Y., García-de-Viedma D. Current knowledge and pending challenges in zoonosis caused by Mycobacterium bovis: a review. Res. Vet. Sci. 2014;97:S94–S100. doi: 10.1016/j.rvsc.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Olea-Popelka F.J., Costello E., White P., McGrath G., Collins J.D., O’Keeffe J. Risk factors for disclosure of additional tuberculous cattle in attested-clear herds that had one animal with a confirmed lesion of tuberculosis at slaughter during 2003 in Ireland. Prev Vet Med. 2008;85:81–91. doi: 10.1016/j.prevetmed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Zoonotic Tuberculosis. WHO, OIE, FAO; 2017. https://www.who.int/tb/areas-of-work/zoonotic-tb/ZoonoticTBfactsheet2017.pdf?ua=1 Available: [Google Scholar]
- 23.Firdessa R., Tschopp R., Wubete A., Sombo M., Hailu E., Erenso G. High prevalence of bovine tuberculosis in dairy cattle in Central Ethiopia: implications for the dairy industry and public health. Langsley G, editor. PLoS One. 2012;7 doi: 10.1371/journal.pone.0052851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Michel A.L. Implications of tuberculosis in African wildlife and livestock. Ann. N. Y. Acad. Sci. 2002;969:251–255. doi: 10.1111/j.1749-6632.2002.tb04387.x. [DOI] [PubMed] [Google Scholar]
- 25.Jha V.C., Morita Y., Dhakal M., Besnet B., Sato T., Nagai A. Isolation of Mycobacterium spp. from milking buffaloes and cattle in Nepal. J. Vet. Med. Sci. 2007;69:819–825. doi: 10.1292/jvms.69.819. [DOI] [PubMed] [Google Scholar]
- 26.Pandey G., Dhakal S., Sadaula A., Kc G., Subedi S., Pandey K. Status of tuberculosis in bovine animals raised by tuberculosis infected patients in Western Chitwan, Nepal. Int J Infect Microbiol. 2013;1:49–53. doi: 10.3126/ijim.v1i2.7407. [DOI] [Google Scholar]
- 27.National Tuberculosis Program Nepal. Bhaktapur, Nepal: National Tuberculosis Control Center 2018. https://nepalntp.gov.np/wp-content/uploads/2020/04/NTP-Annual-Report-2075-76-2018-19.pdf Available:
- 28.Olea-Popelka F., Muwonge A., Perera A., Dean A.S., Mumford E., Erlacher-Vindel E. Zoonotic tuberculosis in human beings caused by Mycobacterium bovis —a call for action. Lancet Infect. Dis. 2017;17:e21–e25. doi: 10.1016/S1473-3099(16)30139-6. [DOI] [PubMed] [Google Scholar]
- 29.Dean A.S., Forcella S., Olea-Popelka F., Idrissi A.E., Glaziou P., Benyahia A. A roadmap for zoonotic tuberculosis: a one health approach to ending tuberculosis. Lancet Infect. Dis. 2018;18:137–138. doi: 10.1016/S1473-3099(18)30013-6. [DOI] [PubMed] [Google Scholar]
- 30.The End Tb Strategy. WHO; 2015. https://www.who.int/tb/End_TB_brochure.pdf?ua=1 Available: [Google Scholar]
- 31.City Population. NEPAL: Kathmandu Valley. 2017. https://www.citypopulation.de/php/nepal-kathmanduvalley.php Available:
- 32.Ministry of Agriculture and Livestock Development Livestock Statistics of Nepal. Nepal. 2017. https://nepalindata.com/resource/livestock-statistics-of-nepal-2017--/ Available:
- 33.Nuru A., Mamo G., Zewude A., Mulat Y., Yitayew G., Admasu A. Preliminary investigation of the transmission of tuberculosis between farmers and their cattle in smallholder farms in northwestern Ethiopia: a cross-sectional study. BMC Res Notes. 2017;10 doi: 10.1186/s13104-016-2349-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.European Commission Report of the Scientific Committee on Animal Health and Animal Welfare. EUROPEAN COMMISSION HEALTH & CONSUMER PROTECTION DIRECTORATE-GENERAL. 1999. https://ec.europa.eu/food/sites/food/files/safety/docs/sci-com_scah_out33_en.pdf Report No.: Sanco/B3/R10/1999. Available:
- 35.Terrestrial Animal Health Code. Paris: World Organisation for Animal Health (OIE) 2019. https://www.oie.int/index.php?id=169&L=0&htmfile=chapitre_bovine_tuberculosis.htm Available:
- 36.Dahoo I., Martin W., Stryhn H. VER Inc; Charlottetown, CA: 2014. Veterinary Epidemiologic Research. 2. Ed., 3. Print. [Google Scholar]
- 37.Hosmer D.W., Lemeshow S. John Wiley & Sons; New York; Toronto: 2005. Applied Logistic Regression. Available: [DOI] [Google Scholar]
- 38.Falzon L.C., Traoré S., Kallo V., Assamoi J.-B., Bonfoh B., Schelling E. Evaluation of the fluorescence polarization assay as a rapid on-spot test for ruminant brucellosis in Côte d’Ivoire. Front Vet Sci. 2019;6:287. doi: 10.3389/fvets.2019.00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.den Boon S., Verver S., Marais B.J., Enarson D.A., Lombard C.J., Bateman E.D. Association between passive smoking and infection with Mycobacterium tuberculosis in children. PEDIATRICS. 2007;119:734–739. doi: 10.1542/peds.2006-1796. [DOI] [PubMed] [Google Scholar]
- 40.Bates M.N. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Arch. Intern. Med. 2007;167:335. doi: 10.1001/archinte.167.4.335. [DOI] [PubMed] [Google Scholar]
- 41.Slama K., Chiang C.-Y., Enarson D.A., Hassmiller K., Fanning A., Gupta P. Tobacco and tuberculosis: a qualitative systematic review and meta-analysis. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2007;11:1049–1061. [PubMed] [Google Scholar]
- 42.Marahatta S.B. Prevalance of tuberculosis and risk factors Assoicated with multidrug resistant tuberculosis in Central Nepal. Int. J. Epidemiol. 2015;44:i106. doi: 10.1093/ije/dyv096.059. [DOI] [Google Scholar]
- 43.Kapoor A.K., Deepani V., Dhall M., Kapoor S. Pattern of socio-economic and health aspects among TB patients and controls. Indian J. Tuberc. 2016;63:230–235. doi: 10.1016/j.ijtb.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 44.Srivastava K., Chauhan D.S., Gupta P., Singh H.B., Sharma V.D., Yadav V.S. Isolation of Mycobacterium bovis & M. tuberculosis from cattle of some farms in north India--possible relevance in human health. Indian J. Med. Res. 2008;128:26–31. [PubMed] [Google Scholar]
- 45.Dabade G., Kale A., Athani B.R., Sankri V., Pawar S.L., Megeri S.N. A study on zoonotic tuberculosis in selected rural areas of Bagalkot and Belgaum districts of Karnataka state. J Clin Tuberc Mycobact Dis. 2017;9:30–35. doi: 10.1016/j.jctube.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(S1):Questionnaire used for interviewing human subjects.