Abstract
Age-related macular degeneration (AMD) and glaucoma are degenerative conditions of the retina and a significant cause of irreversible blindness in developed countries. Alzheimer’s disease (AD), the most common dementia of the elderly, is often associated with AMD and glaucoma. The cardinal features of AD include extracellular accumulation of amyloid β (Aβ) and intracellular deposits of hyper-phosphorylated tau (p-tau). Neuroinflammation and brain iron dyshomeostasis accompany Aβ and p-tau deposits and, together, lead to progressive neuronal death and dementia. The accumulation of Aβ and iron in drusen, the hallmark of AMD, and Aβ and p-tau in retinal ganglion cells (RGC), the main retinal cell type implicated in glaucoma, and accompanying inflammation suggest overlapping pathology. Visual abnormalities are prominent in AD and are believed to develop before cognitive decline. Some are caused by degeneration of the visual cortex, while others are due to RGC loss or AMD-associated retinal degeneration. Here, we review recent information on Aβ, p-tau, chronic inflammation, and iron dyshomeostasis as common pathogenic mechanisms linking the three degenerative conditions, and iron chelation as a common therapeutic option for these disorders. Additionally discussed is the role of prion protein, infamous for prion disorders, in Aβ-mediated toxicity and, paradoxically, in neuroprotection.
Keywords: glaucoma, iron, oxidative stress, inflammation, Alzheimer’s disease, reactive oxygen species, age related macular degeneration, drusen, prion protein, retinal degeneration
1. Introduction
Alzheimer’s disease (AD) is characterized by the gradual and progressive loss of memory and cognitive functions due to a loss of neurons in the hippocampus and, progressively, in other regions of the brain. The principal cause of neurotoxicity is the extracellular accumulation of amyloid β (Aβ), a product of abnormal processing of the amyloid precursor protein (APP), and the intracellular accumulation of tau, a microtubule stabilizing protein, as neurofibrillary tangles (NFTs) [1,2]. Inflammation and oxidative stress due to brain iron dyshomeostasis are other prominent features of AD brain pathology [3,4,5]. Whether these are triggered by Aβ and tau deposits or are a consequence of these changes remains unclear. The diagnosis of AD is mostly clinical, though biomarkers in the cerebrospinal fluid (CSF) provide corroborative evidence. The most reliable and frequently used biomarkers are elevated levels of Aβ1−42, the most toxic form of Aβ, total tau (t-tau), and hyper-phosphorylated tau (p-tau) in the CSF [6]. Vision-related changes are common in AD [7] and are summarized in Table 1. Some of the visual defects are due to degeneration of the visual cortex, while others are attributed to retinal degeneration associated with glaucoma and age-related macular degeneration (AMD) [8,9]. Thinning of the retinal nerve fiber layer (RNFL) due to the selective death of retinal ganglion cells (RGCs) has emerged as a potential diagnostic test for AD [10,11], prompting visualization of the retina by optical coherence tomography (OCT) and functional analysis with electroretinography (ERG). Though promising, these tests lack sufficient specificity and sensitivity for broad clinical applications [12,13,14,15].
Table 1.
Ocular symptoms associated with Alzheimer’s disease (AD).
| Tissue | Symptoms | Contradictory Findings |
|---|---|---|
| Clinical Manifestations | ||
| Visual Dysfunction | Impaired contrast sensitivity [16,17,18,19,20], color vision [16,17,19,20], visual acuity [17,19], and visual integration [17]. Macular thinning [16,17], visuospatial deficits [18,19,20], visuomotor impairment [21,22,23,24], visual field loss [25] | |
| Cornea | Increased corneal sensitivity [26], corneal thinning [27,28] | |
| Retina | Reduced retinal nerve fiber layer thickness in superior and inferior quadrants [13,16,29,30], retinal astrogliosis [31], reduction of retinal ganglion cells [13,32] most notably in fovea [32] | |
| Pupil | Increased pupil diameter during cognitive effort [33], slowed pupillary responses to light and target detection task [34], exaggerated pupil response with dilute tropicamide [35,36], smaller baseline pupil size [37] | |
| Lens | Equatorial supranuclear cataracts [38,39] | Opacity not related to Alzheimer’s disease [40,41] |
| Optic Nerve | Axonal degeneration [42,43], thinner lamina cribrosa [28] | No axonal damage [44] |
| Intraocular pressure | Increased intraocular pressure in Alzheimer’s disease patients [45,46] | |
| Pathological Changes | ||
| Cornea | Fibroblasts, epithelium express amyloid precursor protein and amyloid β [47], A disintegrin and metalloproteinase domain-containing protein ADAM-10 and beta-site amyloid precursor protein cleaving enzyme 1 increased in fibroblasts [47], decreased microvilli and altered morphology in corneal epithelia [27], several-fold increase in amyloid precursor protein expression, amyloid β deposition, and increased apoptosis in corneal epithelia [27] | |
| Retina | Reduced oxygen metabolism [48,49], amyloid β plaques [50,51], accumulation of phospho-tau [52,53], amyloid β deposition in retinal microvasculature and pericytes [54], compromised blood-retinal barrier [54], retinal vasculature abnormalities [55,56], increased retinal vascular amyloid β40 and amyloid β42, decreased vascular platelet-derived growth factor receptor β, and decreased vascular low-density lipoprotein -1 [54] | |
| Lens | Increased amyloid β aggregation in lens [38,57], presenilin expression in lens [58] | No aggregation of amyloid β [40,41] |
| Aqueous Humor | Increased levels of amyloid β [59,60] | |
| Vitreous Humor | Presence of Alzheimer’s disease -associated proteins [59,61] | |
| Choroid | Thinning of choroid [62,63] | |
| Optic Nerve | Tau deposition [20] | |
Glaucomatous RGC death is typically associated with elevated intraocular pressure (IOP), the pressure exerted by the aqueous humor (AH) in the anterior segment of the eye [64,65]. Normally, AH is secreted by the ciliary epithelium and drains into venous circulation by the conventional pathway along the trabecular meshwork (TM) cells and Schlemm’s canal, and the unconventional uveoscleral pathway [66]. Elevated IOP can occur due to the alteration of extracellular matrix (ECM) proteins in the TM which become less-responsive to elevated pressure as in open-angle glaucoma, where access to the drainage pathway is blocked as in closed-angle glaucoma, or where the cause of RGC death is not clear as in normal-tension glaucoma [67,68]. It is believed that chronic elevation of IOP leads to the accumulation of Aβ and p-tau in RGCs, resulting in their loss. This leads to thinning of the RNFL and optic nerve atrophy, ultimately leading to permanent blindness because of the failure to transmit visual stimuli to the brain [7,8]. However, it is difficult to distinguish whether visual defects due to RGC cell loss appear earlier than those due to neuronal loss in the occipital cortex, information critical for the early diagnosis of AD. A recent meta-analysis of 25 studies with 887 cases of AD, 216 cases of mild cognitive impairment, and 864 healthy controls showed a positive correlation between reduced RNFL thickness and confirmed cases of AD, linking RGC death to AD brain pathology [69]. Follow-up studies either confirmed or failed to reproduce some of these observations, leaving the matter unsettled. However, the presence of AD-associated RGC death with normal or low IOP suggests a complex pathology that requires further exploration [7,8,9,11,64,70,71].
Retinal degeneration associated with AMD shares several features with AD, including extracellular deposits of Aβ, chronic inflammation, and oxidative stress, the latter partly attributed to the accumulation of iron [72,73,74,75,76]. AMD is typically associated with the accumulation of drusen between the retinal pigment epithelial (RPE) cell layer that forms the outer blood-retinal barrier and the Bruch’s membrane (BM), resulting in dysfunction of the barrier and death of photoreceptor cells. Among the various denatured proteins that comprise drusen, Aβ is prominent, suggesting a link with AD [77]. In addition, inflammation, the accumulation of iron, and oxidative stress play a central role in disease progression [74]. In a recent study of ~800 cases of AD, a significant positive correlation was noted with the established diagnosis of AMD and recent diagnosis of glaucoma [78], linking the three conditions.
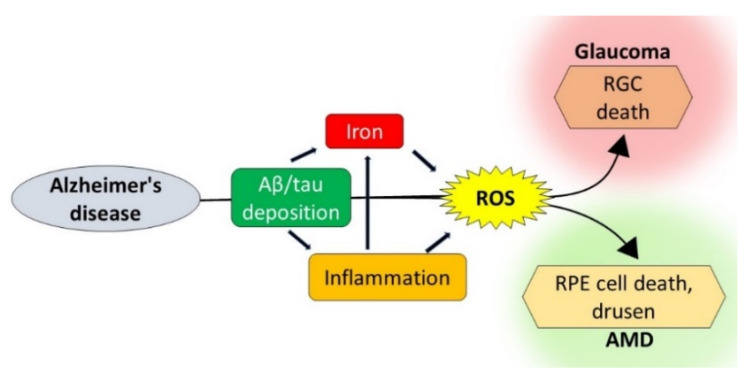
Whether these disparate conditions of the brain and the eye share pathogenic pathways remains unclear. The identification of common toxic stimuli could provide an anatomically accessible site for the early diagnosis of AD and the much-needed window for therapeutic management. Here, we review recent information on the pathological processes that are common to AD, glaucoma, and AMD, with emphasis on Aβ, p-tau, chronic inflammation-mediated iron dyshomeostasis, and iron-mediated reactive oxygen species (ROS) (Figure 1). In addition, the role of prion protein (PrPC) as a mediator of Aβ toxicity and, paradoxically, as an antioxidant is reviewed.
Figure 1.
Pathogenic pathways shared by Alzheimer’s disease (AD), AMD, and glaucoma: AD-associated amyloid β (Aβ) and tau deposits lead to inflammation and iron accumulation, increasing ROS. Aβ, hyper-phosphorylated tau (p-tau), inflammation, and ROS together lead to RGC death typical of glaucoma and retinal pigment epithelial (RPE) dysfunction associated with AMD. ROS: reactive oxygen species, RGC: retinal ganglion cells, and AMD: age-related macular degeneration.
2. Methods
This review is based on the appraisal of existing evidence from multiple systematic reviews linking AD, AMD, and glaucoma. A comprehensive search using the National Library of Medicine, MEDLINE, and Google scholar from 2015 to August 2020, including in vivo, in vitro, and clinical studies, was used to collect and critically appraise the relevant studies.
2.1. Aβ and Tau as Mediators of Retinal and Neuronal Degeneration
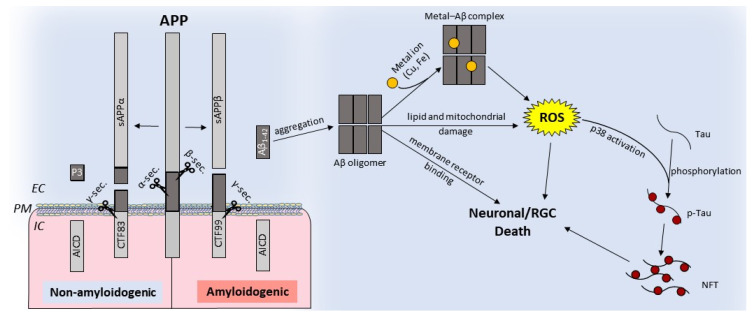
The retina and several other cell types in the eye express amyloid precursor protein (APP), a type I transmembrane glycoprotein, and other proteins implicated in AD. As in the brain, APP undergoes post-translational processing by two mutually exclusive pathways: nonamyloidogenic, and amyloidogenic. The nonamyloidogenic pathway involves the cleavage of APP by α-secretase followed by γ-secretase, and precludes the formation of Aβ. This cleavage occurs at the plasma membrane and is mediated by proteases belonging to the A-disintegrin and metalloprotease (ADAM) family. The resulting amino-terminal fragment APPα is released in the extracellular milieu, and the C-terminal fragment CTF83 is released intracellularly. Subsequent cleavage of CTF83 by γ-secretase releases the APP intracellular domain (AICD) and P3. Processing by the amyloidogenic pathway involves consecutive cleavage of APP by β-secretase and γ-secretase. Cleavage by β-secretase releases soluble APPβ and an intracellular fragment, CTF99. Subsequent cleavage of CTF99 by γ-secretase results in the generation of AICD and Aβ fragments of different lengths. Of these, Aβ1−42 is most toxic and accumulates in AD brains as extracellular plaques [1,2,79] (Figure 2). Aβ aggregates bind redox-active metals such as iron and copper, the sources of ROS, and cause mitochondrial damage, leading to neuronal toxicity. Aβ aggregates also cause the hyperphosphorylation and aggregation of tau, compounding the toxicity (Figure 2).
Figure 2.
Schematic representation of nonamyloidogenic and amyloidogenic processing of the amyloid precursor protein (APP): nonamyloidogenic processing of APP is mediated by α-secretase followed by γ-secretase, releasing soluble APPα and intracellular fragments AICD and P3. Amyloidogenic processing involves cleavage by β-secretase followed by γ-secretase, which releases toxic Aβ1−42 [79,80]. Aβ can oligomerize and form cytotoxic metal-Aβ complexes that generate ROS, disrupt the lipid bilayer, compromise mitochondrial function, or initiate aberrant signaling cascades. Activation of p38 by ROS phosphorylates tau results in NFTs. IC: intracellular, EC: extracellular, NFTs: neurofibrillary tangles, and PM: plasma membrane.
Similar processing of APP occurs in the retina and other cell types in the eye. Soluble APPα, APPβ, and pathogenic Aβ are present in the vitreous and aqueous humor (VH and AH) to varying amounts as in the cerebrospinal fluid (CSF) [61], and pathological deposits of Aβ are prominent in drusen in AMD, and the cause of RGC death and thinning of the RNFL associated with glaucomatous degeneration [81]. These observations are more consistent and prominent in mice models of AD that have been instrumental in gaining insight into the role of Aβ in AD-associated retinal degeneration. The 3xTG-AD, APP-PS1ΔE9, and APPswe/PS1ΔE9 mice that developed Aβ deposits in the brain also show aggregates of Aβ in the retina and thinning of the RNFL [82,83,84]. Colocalization of Aβ deposits with apoptotic RGCs and axonal degeneration have been reported in several animal models of AD [85,86]. In a rat model of glaucoma, the levels of Aβ1−42 in the retina increased with elevated IOP, exposure to light, and ageing, resulting in the apoptotic death of RGCs [87]. These observations were reproduced by intravitreal injection of Aβ1−42 [88], and RGCs rescued with agents that reduced Aβ1−42 levels or genetic variants that promote nonamyloidogenic processing of APP, indicating a causal relationship.
Deposits of Aβ are not restricted to RGCs. Aβ deposits are present in all layers of the retina, including the ganglion cell layer, nerve fiber layer, photoreceptor layer, and the inner plexiform layer where they promote phosphorylation and accumulation of tau as amorphous deposits and NFTs in the retinal layers and RGCs [81,89,90]. In mice models overexpressing mutant tau, there is a direct correlation between p-tau, Aβ deposits, and RGC death [53]. Interestingly, elevated IOP increases the accumulation of tau and RGC death, and downregulation of tau by short interfering RNA rescues RGCs, confirming tau as the underlying cause [87]. Due to its role in stabilizing microtubules, tau phosphorylation and aggregation interferes with anterograde axonal transport and inhibits mitochondrial transport, resulting in loss of energy and generation of ROS [91]. Additionally, Aβ deposits sequester redox-active metals such as iron and induce toxicity by iron-catalyzed ROS, which causes additional Aβ generation and aggregation, creating a positive feed-forward loop [4,5,92,93]. Moreover, Aβ deposits and intracellular NFTs initiate a cascade of events that activate retinal astrocytes and microglia with the secretion of inflammatory cytokines, including interleukin−1β (IL-1β), IL-6, and tumor necrosis factor α (TNFα) [94,95], which, along with Aβ-generated ROS, create a toxic microenvironment leading to RGC death and thinning of the RNFL.
The triggers that shift the physiological, non-amyloidogenic processing of APP to the amyloidogenic generation of Aβ are not clear, except for the inherited forms of AD. It is also unclear whether the processing of APP in the brain and the eye is altered to the same extent, and the efficiency of Aβ clearance mechanisms in the brain and the eye. In sporadic AD, which forms the bulk of AD cases, the deposition of Aβ and p-tau in RGCs is not a consistent observation [50,52,90]. It is therefore unclear whether the visual symptoms summarized in Table 1 are a direct consequence of degeneration of the visual cortex or result from dysfunction or death of RGCs that receive and transmit the visual stimuli.
The role of Aβ in the pathogenesis of AMD is less clear. Although Aβ deposits have been detected in drusen [93,96,97], the mechanism by which amyloidogenic processing takes precedent over the non-amyloidogenic processing of APP by retinal pigment epithelial (RPE) cells is unclear. It is likely that, during normal ageing, the production and secretion of Aβ1−42 by RPE cells increases, which accumulates at the interface of RPE cells and outer segments of the photoreceptors tips and in the subretinal space, where it is engulfed by the microglia [98]. In support of this hypothesis, the overexpression of Aβ in RPE cells induces AMD-like pathology [99] that is exacerbated by bloated microglia that accumulate Aβ deposits and other cellular debris. Together, these changes initiate an inflammatory response and deposition of drusen typical of AMD. A recent meta-analysis of 21 studies showed a significant association between AD and AMD [100], reinforcing the pathogenic role of Aβ in AMD.
Thus, AD and AMD share extracellular Aβ deposits and inflammation as common underlying pathogenic mechanisms. The glaucomatous degeneration of RGCs, in addition, is associated with p-tau. Whether these features suggest a link between the three disorders or are coincidental observations associated with ageing is unclear at present. The association of RNFL thinning with AD, however, suggests a causal relationship. Further exploration is necessary to resolve these questions.
2.2. Iron Dyshomeostasis and Reactive Oxygen Species
In addition to deposits of Aβ and p-tau, inflammation is a prominent feature of AD brains [3,101,102]. The chronic activation of resident microglia due to the incomplete degradation of phagocytosed Aβ and neuronal debris releases pro- and anti-inflammatory cytokines, exacerbating the underlying pathology by initiating a cascade of events. Among these, iron dyshomeostasis takes central stage due to its potential to generate ROS and associated toxicity [103]. Although a consistent feature of AD brains, the mechanism of iron accumulation has remained controversial. Recent evidence suggests the cytokine-mediated upregulation of brain hepcidin, the master regulator of iron homeostasis, as the underlying cause [104].
Hepcidin is a peptide hormone secreted mainly by the liver. It maintains systemic iron within a narrow range since iron is essential for vital catalytic reactions, but excess can be highly toxic because of the ease with which it cycles between redox states [105]. This is achieved by modulating the expression of ferroportin (Fpn), the only known iron export protein. Increased iron saturation of serum transferrin upregulates the secretion of liver hepcidin, which binds Fpn on the plasma membrane of cells and causes its internalization and degradation [106]. This decreases both iron uptake from the intestine and release from iron stores, reducing the circulating iron. The opposite scenario takes effect when iron levels are low [107]. Although the brain and the eye are protected from fluctuations in circulating iron by the blood-brain and blood-retinal barriers, respectively, several cell types in the brain, retina, and anterior segment of the eye express hepcidin, suggesting additional regulation of iron exchange locally. In the brain, hepcidin is expressed in the cortex, hippocampus, cerebellum, thalamus, and medulla oblongata [108,109,110]. In the eye, the synthesis and expression of hepcidin is noted in several cell types in the retina and the anterior segment [111,112,113].
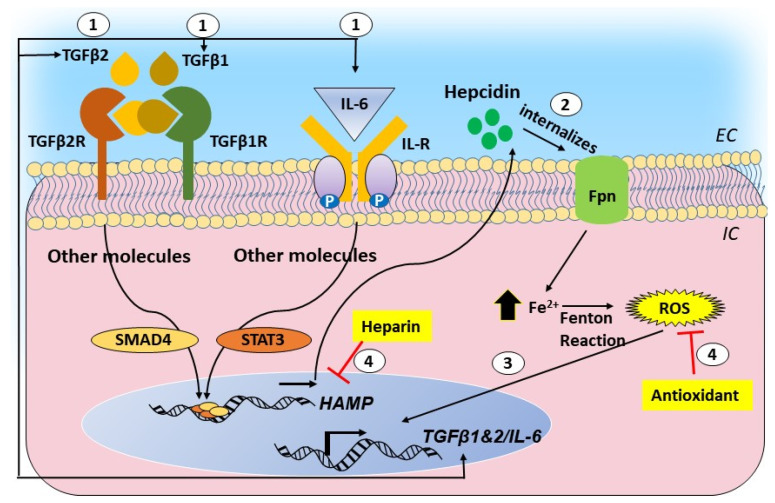
Though helpful in maintaining a stringent control of iron, hepcidin is also upregulated by inflammatory cytokines IL-6, IL-1β, and transforming growth factor (TGF) β1 and β2 (Figure 3). The inflammatory signal supersedes the signal from iron, and is the cause of the anemia of chronic inflammation, where iron is sequestered within liver cells and additional uptake is blocked despite low-circulating iron [114]. This raises the possibility of the upregulation of local hepcidin in the brain and the retina of AD cases, which is invariably accompanied by chronic inflammation. The consequent downregulation of Fpn is likely to increase the intracellular iron, creating a toxic environment by increasing ROS. Levels of hepcidin and redox-active iron are increased in AD brain tissue, supporting the above assumption [108]. Unlike systemic circulation, where excess iron is sequestered by the liver to protect vital organs, the brain and the retina lack such protection. The high metabolic rate of the brain and constant exposure of the retina to light provide an optimal milieu for reducing stored, relative stable ferric iron to its redox-active ferrous form, rendering these organs highly susceptible to iron-mediated toxicity by ROS.
Figure 3.
Graphical representation of the cytokine-hepcidin-iron feed-forward loop and its disruption by hepcidin antagonists and antioxidants: (1) transforming growth factor beta 1 and 2 (TGF-β1 and 2) and interleukin (IL)-6 upregulate hepcidin through the SMAD and signal transducer and activator of transcription (STAT)-mediated pathways. (2) Hepcidin causes the downregulation of ferroportin and intracellular accumulation of iron. (3) Iron-catalyzed ROS promotes the transcriptional activation of TGF-β1 and 2 and IL-6, creating a self-sustained feed-forward loop. (4) Hepcidin antagonists and antioxidants disrupt this loop.
As in AD, inflammation accompanies glaucomatous degeneration and AMD, and the release of various cytokines from activated microglia is likely to upregulate hepcidin, leading to an accumulation of iron. Oxidative stress is prominent in glaucoma [115,116,117], and is exacerbated by the release of TGFβ1 and IL-6, cytokines known to trigger the upregulation of hepcidin. In a recent report, the upregulation of hepcidin in TM cells by TGFβ2 initiated a positive feed-forward loop between TGFβ2, hepcidin, and iron fueled by ROS. Disruption of this loop with hepcidin antagonists and antioxidants reduced the iron accumulation and ROS, suggesting a prominent role of ROS in primary open-angle glaucoma [111,118] (Figure 3). In addition, significant protection of RGCs is achieved by chelating iron, reinforcing the toxic role of iron in glaucomatous degeneration [119].
The toxic role of iron is better understood in AMD, where intravenous iron and hereditary diseases associated with systemic iron overload, such as aceruloplasminemia, pantothene kinase deficiency, and Friedrich’s ataxia, show AMD-like retinal degeneration. Mice lacking ceruloplasmin and hephaestin, ferroxidases necessary for iron export, reproduce several features of AMD, and levels of transferrin, an iron uptake protein, are elevated in the retina and AH of AMD cases [118,120,121,122]. Elevated serum iron is also associated with retinal degeneration with AMD-like pathology, indicating a direct role of iron in retinal degeneration.
2.3. Clinically Relevant Therapeutic Options
Various anti-Aβ therapies have been tried for AD, AMD, and AD-associated glaucomatous degeneration, and have been discussed in excellent reviews [123]. Here, we describe recent developments in therapeutic options that reduce iron-catalyzed ROS and oxidative stress by iron chelators, hepcidin antagonists, and Fpn-stabilizing agents.
Partial success in ameliorating the symptoms of AD, glaucoma, and AMD with iron chelators re-enforces the central role of iron-mediated ROS in AD pathogenesis [124,125]. For example, iron chelators have been used to ameliorate the symptoms of AD with partial success [126]. Recently, deferiprone (DFP), a potent iron chelator, has been shown to rescue RGCs and glaucomatous degeneration in a mouse model of glaucoma [127,128]. In Abca4−/− mice, a widely used model of retinal degeneration, deferiprone reduced the oxidation-driven degradation of vital bisretinoids such as A2E [129]. In mice lacking ceruloplamin and hepaestin, which accumulate iron in the retina, salicylaldehyde isonicotinoyl hydrazine (SIH), a potent iron chelator, rescued the phenotype. SIH also provided efficient protection against H2O2-induced cytotoxicity in an in vitro model of AMD relative to other iron chelators such as deferoxamine, which had visual side effects.
Hepcidin antagonists are another class of small molecular weight compounds that reduce hepcidin-mediated accumulation of iron. These are likely to prove more beneficial in reducing the iron accumulation associated with chronic inflammation [130]. Some of the hepcidin antagonists are anti-inflammatory compounds, such as IL-1 receptor inhibitors, anti-IL-6 monoclonal antibody, and TNF-α blockers [131,132]. These agents, in addition to reducing the hepcidin-mediated accumulation of iron, are likely to reduce inflammation as well, adding to their therapeutic potential. In an in vitro model of glaucoma, the cytokine-mediated upregulation of hepcidin was disrupted with heparin, a hepcidin antagonist, and N-acetyl L carnosine (NAC), an antioxidant [111], suggesting that such agents are useful in decreasing the iron-catalyzed ROS and may prove useful in rescuing neurons and RGCs from ROS-mediated toxicity and death. Inflammatory changes accompany glaucomatous degeneration [131], and the use of anti-inflammatory compounds, including nonsteroidal anti-inflammatory drugs (NSAID) such as pranoprofen, have been useful in decreasing the IOP and rescue RGCs [133]. Several such compounds are undergoing clinical trials for systemic disorders of iron overload [134], and could be modified for use in the brain and the eye.
2.4. The Paradoxical Role of Prion Protein
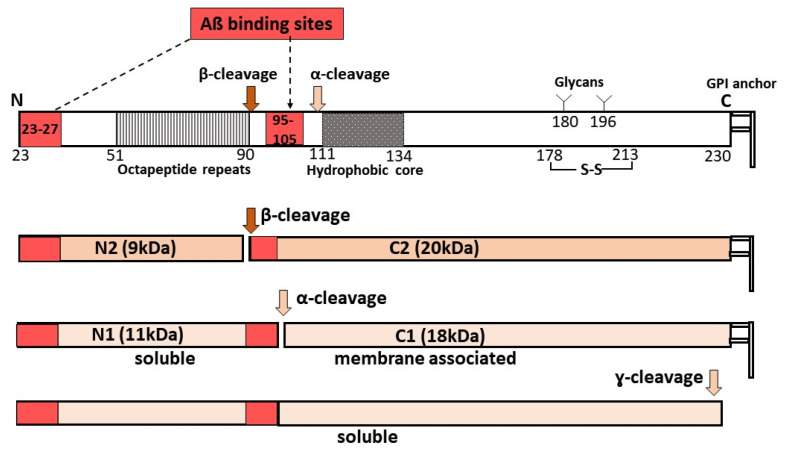
The prion protein (PrPC) is a ubiquitously expressed protein mainly known for its role as the substrate for PrP-scrapie (PrPSc), the principal pathogenic agent responsible for all prion disorders [135,136]. Besides its pathological role, several physiological functions are attributed to PrPC, including protection from oxidative stress, iron uptake, and in regulating the levels of TNFα-cleaving enzyme (TACE) [137,138,139,140,141]. The significance of PrPC in the pathogenesis of AD stems from its role as a receptor for Aβ oligomers [142,143]. Aβ1−42 specifically binds PrPC with high affinity in a saturable and reversible manner, and mediates biologically relevant downstream intracellular signaling events including the loss of synaptic function, impaired memory and cognition, and other functional deficits associated with AD [144,145]. Two binding sites of Aβ have been identified on PrPC: residues 95−105 and residues 23−27 [143] (Figure 4). Deletion of 95−105 residues or blocking this site with antibodies interferes with the Aβ-PrPC interaction, rescuing the toxicity of Aβ. Additionally, the binding of Aβ oligomers to PrP activates the tyrosine kinase Fyn pathway, leading to synaptic dysfunction and loss [146].
Figure 4.
Processing of prion protein (PrPC) and Aβ binding: PrPC undergoes α-, β-, or γ-cleavage, releasing extracellular N-terminal fragments N1 (α-cleavage), N2 (β-cleavage), or soluble PrPC. Full-length PrPC has two Aβ binding sites. N2 has one, and N1 and soluble PrPC have two Aβ binding sites that could sequester soluble Aβ. The truncated C2 and C1 are attached to the plasma membrane, and the presence of one Aβ-binding site on C2 is likely to transmit the toxic signal of Aβ.
It is interesting to note that, under steady-state conditions, ~65−80% of PrPC on neuronal cells undergoes physiological cleavage at residues 111/112, releasing the N-terminal soluble fragment N1 in the extracellular milieu and C-terminal fragment C1 attached to the plasma membrane. This is also referred to as α-cleavage and occurs in an endocytic compartment during the recycling of PrPC from the plasma membrane. This cleavage is mediated by ADAM17 [147]. Since C1 lacks the primary Aβ-binding site, this cleavage is believed to protect the neurons from Aβ-induced toxicity. The released N1 fragment, on the other hand, is likely to bind and sequester Aβ in the extracellular milieu and protect the cells from toxicity. However, in the retina, ~90% of PrPC is cleaved around residue 90, leaving the primary Aβ-binding site intact on the C-terminal fragment or C2. The released N-terminal fragment N2 contains the secondary Aβ-binding site spanning residues 23−27. Also called the β-cleavage of PrPC, this event is mediated mainly by oxidative stress and is believed to protect the cells from free radical damage [148] (Figure 4). It is likely that the presence of β-cleaved PrPC in retinal cells and other cell types in the eye is due to the constant exposure to light, a source of oxidative stress, or reduced expression of ADAM17. This enzyme is also responsible for the α-cleavage of APP that precludes its amyloidogenic processing [149]. The relative paucity of Aβ deposits in confirmed cases of AD makes it unlikely that the preferred β-cleavage of PrPC is due to the lack of ADAM17. Further exploration is necessary to resolve this question. Nevertheless, the genetic deletion of PrPC reduces Aβ binding by ~50%, implicating PrPC in Aβ-mediated toxicity [150]. It is likely that additional cell-surface proteins participate in this process, or distinct oligomeric species of Aβ bind PrPC.
Paradoxically, PrPC protects the retina from light-induced oxidative damage and stabilizes ECM proteins by interacting with β1 integrin [151,152]. The down-regulation of PrPC activates the Ras homolog gene family member A (RhoA)-associated coiled-coil containing kinase (ROCK) pathway, resulting in the overactivation of ROCK and signaling through the LIMK-cofilin pathway [153,154]. The net result is a shift from cell-cell interactions to cell-substrate interactions. In the eye, this results in increased stiffness of the ECM, resistance to aqueous outflow, and elevated IOP, resulting in RGC death. In the brain, PrPC protects the cells from free radicals, with the result that mice lacking PrPC are more susceptible to intracellular ROS [155]. It is likely that chelation of redox-active metals such as copper and iron by the N-terminal octapeptide repeats provide protection from metal-catalyzed ROS [156,157,158,159]. At the same time, this region is involved in copper and iron transport [141,160,161], suggesting that PrPC maintains an adequate intracellular concentration of these metals by shedding off the octapeptide repeat region, a hypothesis that requires further testing.
3. Conclusions
In this review, common pathogenic mechanisms and differences between AD and age-related and glaucomatous degeneration are highlighted, with emphasis on Aβ, p-tau, and inflammation-mediated iron dyshomeostasis as the common underlying cause. In AD, the incomplete degradation of Aβ and p-tau by microglial cells is likely to trigger the release of cytokines, which upregulate local hepcidin and iron accumulation in the brain. In glaucomatous degeneration, inflammation initiated by Aβ and p-tau deposits due to amyloidogenic processing of APP in the retina and RGCs is likely to increase cytokine levels, upregulating retinal hepcidin and the accumulation of iron. The elevation of IOP has a similar effect, blurring the distinction between AD-associated glaucoma and RGC death due to elevated IOP. AMD is associated with inflammation, the accumulation of iron, and Aβ deposits in drusen, suggesting a strong correlation with AD. However, both AD and AMD are diseases of advanced age, and it is difficult to attribute these changes to AD per se. The increased synthesis of hepcidin due to inflammation is common among the three conditions and offers an untapped opportunity to reduce iron-catalyzed ROS with hepcidin antagonists. Iron chelators have proved beneficial in treating AD, AMD, and glaucoma. Hepcidin antagonists are likely to be more effective if delivered locally in the brain or the eye in optimal amounts. Several such compounds are undergoing clinical trials for systemic disorders of iron accumulation, and could be modified for use in the brain and the eye.
PrPC, though apparently disconnected, is involved in all three disorders. First, it links neuronal and RGC death by serving as a mediator of Aβ toxicity. Second, PrPC transports iron across biological membranes, contributing to the accumulation of iron. Third, the unusual processing of PrPC in the retina at the β-site suggests that PrPC offers protection from increased oxidative stress probably from constant exposure to light. Paradoxically, the absence of PrPC increases the IOP by altering the characteristics of the ECM, which is likely to promote the accumulation and oligomerization of p-tau in RGCs. Additional studies are required to clarify the specific role of PrPC in the eye.
Abbreviations
| AD | Alzheimer’s Disease |
| ADAM | A-disintegrin and metalloprotease |
| AH | Aqueous Humor |
| AMD | Age related macular degeneration |
| APP | Amyloid Precursor Protein |
| Aβ | Amyloid β |
| CSF | Cerebrospinal Fluid |
| DFP | Deferiprone |
| ECM | Extracellular Matrix |
| ERG | Electroretinography |
| Fpn | Ferroportin |
| IL | Interleukin |
| IOP | Intraocular Pressure |
| NFT | Neurofibrillary Tangles |
| NOS | Nitric Oxide Synthase |
| OCT | Optical Coherence Tomography |
| PrPC | Prion Protein |
| PrPSc | Prion Protein Scrapie isoform |
| p-tau | phosphorylated tau |
| RGC | Retinal Ganglion Cells |
| RhoA | Ras homolog gene family member A |
| RNFL | Retinal Nerve Fiber Layer |
| ROCK | Rho-associated protein kinase |
| ROS | Reactive oxygen species |
| SIH | Salicylaldehyde Isonicotinoyl Hydrazine |
| TACE | Tumor Necrosis Factor α cleaving enzyme |
| TGFβ2 | Transforming growth factor beta-2 |
| TM | Trabecular meshwork |
| TNFα | Tumor Necrosis Factor α |
| t-tau | Total tau |
| VH | Vitreous Humor |
Author Contributions
A.A. and N.S.: conceived the idea, did literature search, and wrote the manuscript; A.A.: modified and edited the figures; S.C.: prepared figures and revised the manuscript; A.E.K., A.S.W., and N.R.: prepared the figures and edited the manuscript; and V.B., D.M., and R.A.: edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
NIH (R01NS 092:145 to NS).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Kent S.A., Spires-Jones T.L., Durrant C.S. The physiological roles of tau and Abeta: Implications for Alzheimer’s disease pathology and therapeutics. Acta Neuropathol. 2020;140:1–31. doi: 10.1007/s00401-020-02196-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajmohan R., Reddy P.H. Amyloid-β and Phosphorylated Tau Accumulations Cause Abnormalities at Synapses of Alzheimer’s disease Neurons. J. Alzheimers Dis. 2017;57:975–999. doi: 10.3233/JAD-160612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kinney J.W., Bemiller S.M., Murtishaw A.S., Leisgang A.M., Salazar A.M., Lamb B.T. Inflammation as a central mechanism in Alzheimer’s disease. Alzheimers Dement. 2018;4:575–590. doi: 10.1016/j.trci.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheignon C., Tomas M., Bonnefont-Rousselot D., Faller P., Hureau C., Collin F. Oxidative stress and the amyloid β peptide in Alzheimer’s disease. Redox. Biol. 2018;14:450–464. doi: 10.1016/j.redox.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collin F., Cheignon C., Hureau C. Oxidative stress as a biomarker for Alzheimer’s disease. Future Med. 2018;12:201–203. doi: 10.2217/bmm-2017-0456. [DOI] [PubMed] [Google Scholar]
- 6.Ibarra R., Radanovic M., Pais M.V., Talib L.L., Forlenza O.V. AD-related CSF biomarkers across distinct levels of cognitive impairment: Correlations with global cognitive state. J. Geriatr. Psychiatry Neurol. 2020:891988720944237. doi: 10.1177/0891988720944237. [DOI] [PubMed] [Google Scholar]
- 7.Cerquera-Jaramillo M.A., Nava-Mesa M.O., Gonzalez-Reyes R.E., Tellez-Conti C., de-la-Torre A. Visual features in Alzheimer’s fisease: From basic mechanisms to clinical overview. Neural. Plast. 2018;2018:2941783. doi: 10.1155/2018/2941783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asanad S., Ross-Cisneros F.N., Nassisi M., Barron E., Karanjia R., Sadun A.A. The retina in Alzheimer’s disease: Histomorphometric analysis of an ophthalmologic biomarker. Investig. Ophthalmol. Vis. Sci. 2019;60:1491–1500. doi: 10.1167/iovs.18-25966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta V., Gupta V.B., Chitranshi N., Gangoda S., Vander Wall R., Abbasi M., Golzan M., Dheer Y., Shah T., Avolio A., et al. One protein, multiple pathologies: Multifaceted involvement of amyloid β in neurodegenerative disorders of the brain and retina. Cell. Mol. Life Sci. 2016;73:4279–4297. doi: 10.1007/s00018-016-2295-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones-Odeh E., Hammond C.J. How strong is the relationship between glaucoma, the retinal nerve fibre layer, and neurodegenerative diseases such as Alzheimer’s disease and multiple sclerosis? Eye. 2015;29:1270–1284. doi: 10.1038/eye.2015.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sivak J.M. The aging eye: Common degenerative mechanisms between the Alzheimer’s brain and retinal disease. Invest. Ophthalmol. Vis. Sci. 2013;54:871–880. doi: 10.1167/iovs.12-10827. [DOI] [PubMed] [Google Scholar]
- 12.Tsokolas G., Tsaousis K.T., Diakonis V.F., Matsou A., Tyradellis S. Optical coherence tomography angiography in neurodegenerative diseases: A review. Eye Brain. 2020;12:73–87. doi: 10.2147/EB.S193026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marziani E., Pomati S., Ramolfo P., Cigada M., Giani A., Mariani C., Staurenghi G. Evaluation of retinal nerve fiber layer and ganglion cell layer thickness in Alzheimer’s disease using spectral-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2013;54:5953–5958. doi: 10.1167/iovs.13-12046. [DOI] [PubMed] [Google Scholar]
- 14.Ngolab J., Honma P., Rissman R.A. Reflections on the Utility of the Retina as a Biomarker for Alzheimer’s disease: A Literature Review. Neurol. Ther. 2019;8:57–72. doi: 10.1007/s40120-019-00173-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liao H., Zhu Z., Peng Y. Potential utility of retinal imaging for Alzheimer’s disease: A review. Front. Aging Neurosci. 2018;10:188. doi: 10.3389/fnagi.2018.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polo V., Rodrigo M.J., Garcia-Martin E., Otin S., Larrosa J.M., Fuertes M.I., Bambo M.P., Pablo L.E., Satue M. Visual dysfunction and its correlation with retinal changes in patients with Alzheimer’s disease. Eye. 2017;31:1034–1041. doi: 10.1038/eye.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salobrar-García E., de Hoz R., Ramírez A.I., López-Cuenca I., Rojas P., Vazirani R., Amarante C., Yubero R., Gil P., Pinazo-Durán M.D., et al. Changes in visual function and retinal structure in the progression of Alzheimer’s disease. PLoS ONE. 2019;14:1–23. doi: 10.1371/journal.pone.0220535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilmore G.C., Levy J.A. Spatial contrast sensitivity in Alzheimer’s disease: A comparison of two methods. Optom. Vis. Sci. 1991;68:790–794. doi: 10.1097/00006324-199110000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Cronin-Golomb A. Vision in Alzheimer’s disease. Gerontologist. 1995;35:370–376. doi: 10.1093/geront/35.3.370. [DOI] [PubMed] [Google Scholar]
- 20.Rizzo M., Anderson S.W., Dawson J., Nawrot M. Vision and cognition in Alzheimer’s disease. Neuropsychologia. 2000;38:1157–1169. doi: 10.1016/S0028-3932(00)00023-3. [DOI] [PubMed] [Google Scholar]
- 21.De Boer C., van der Steen J., Mattace-Raso F., Boon A.J.W., Pel J.J.M. The effect of neurodegeneration on visuomotor behavior in Alzheimer’s disease and Parkinson’s disease. Motor. Control. 2016;20:1–20. doi: 10.1123/mc.2014-0015. [DOI] [PubMed] [Google Scholar]
- 22.De Boer C., Mattace-Raso F., van der Steen J., Pel J.J.M. Mini-mental state examination subscores indicate visuomotor deficits in Alzheimer’s disease patients: A cross-sectional study in a Dutch population. Geraitr. Gerontol. Int. 2014;14:880–885. doi: 10.1111/ggi.12183. [DOI] [PubMed] [Google Scholar]
- 23.Mollica M.A., Navarra J., Fernández-Prieto I., Olives J., Tort A., Valech N., Coll-Padrós N., Molinuevo J.L., Rami L. Subtle visuomotor difficulties in preclinical Alzheimer’s disease. J. Neuropsychol. 2017;11:56–73. doi: 10.1111/jnp.12079. [DOI] [PubMed] [Google Scholar]
- 24.Tippett W.J., Sergio L.E. Visuomotor integration is impaired in early stage Alzheimer’s disease. Brain Res. 2006;1102:92–102. doi: 10.1016/j.brainres.2006.04.049. [DOI] [PubMed] [Google Scholar]
- 25.Lee A.G., Martin C.O. Neuro-ophthalmic findings in the visual variant of Alzheimer’s disease. Ophthalmology. 2004;111:376. doi: 10.1016/S0161-6420(03)00732-2. [DOI] [PubMed] [Google Scholar]
- 26.Örnek N., Dağ E., Örnek K. Corneal sensitivity and tear function in neurodegenerative diseases. Curr. Eye Res. 2015;40:423–428. doi: 10.3109/02713683.2014.930154. [DOI] [PubMed] [Google Scholar]
- 27.Dong Z., Luo A., Gan Y., Li J. Amyloid β deposition could cause corneal epithelial cell degeneration associated with increasing apoptosis in APPswePS1 transgenic mice. Curr. Eye Res. 2018;43:1326–1333. doi: 10.1080/02713683.2018.1501070. [DOI] [PubMed] [Google Scholar]
- 28.Eun Ji L., Tae-Woo K., Dae Seung L., Hyunjoong K., Young Ho P., Jungeun K., Joon Woo L., SangYun K. Increased CSF tau level is correlated with decreased lamina cribrosa thickness. Alzheimer Res. Ther. 2016;8:1–9. doi: 10.1186/s13195-015-0169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu D., Zhang L., Li Z., Zhang X., Wu Y., Yang H., Min B., Zhang X., Ma D., Lu Y. Thinner changes of the retinal nerve fiber layer in patients with mild cognitive impairment and Alzheimer’s disease. BMC Neurol. 2015;15:14. doi: 10.1186/s12883-015-0268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berisha F., Feke G.T., Trempe C.L., McMeel J.W., Schepens C.L. Retinal abnormalities in early Alzheimer’s disease. Investig. Ophthalmol. Vis. Sci. 2007;48:2285–2289. doi: 10.1167/iovs.06-1029. [DOI] [PubMed] [Google Scholar]
- 31.Blanks J.C., Porrello K.V., Torigoe Y., Hinton D.R., Blanks R.H.I., Schmidt S.Y. Retinal pathology in Alzheimer’s disease. II. Regional neuron loss and glial changes in GCL. Neurobiol. Aging. 1996;17:385–395. doi: 10.1016/0197-4580(96)00009-7. [DOI] [PubMed] [Google Scholar]
- 32.Blanks J.C., Torigoe Y., Blanks R.H.I., Hinton D.R. Retinal pathology in Alzheimer’s disease. I. Ganglion cell loss in foveal/parafoveal retina. Neurobiol. Aging. 1996;17:377–384. doi: 10.1016/0197-4580(96)00010-3. [DOI] [PubMed] [Google Scholar]
- 33.Kremen W.S., Panizzon M.S., Elman J.A., Granholm E.L., Andreassen O.A., Dale A.M., Gillespie N.A., Gustavson D.E., Logue M.W., Lyons M.J., et al. Pupillary dilation responses as a midlife indicator of risk for Alzheimer’s disease: Association with Alzheimer’s disease polygenic risk. Neurobiol. Aging. 2019;83:114–121. doi: 10.1016/j.neurobiolaging.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dragan M.C., Leonard T.K., Lozano A.M., McAndrews M.P., Ng K., Ryan J.D., Tang-Wai D.F., Wynn J.S., Hoffman K.L. Pupillary responses and memory-guided visual search reveal age-related and Alzheimer’s-related memory decline. Behav. Brain Res. 2017;322:351–361. doi: 10.1016/j.bbr.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 35.Scinto L.F.M. ApoE allelic variability influences pupil response to cholinergic challenge and cognitive impairment. Genes Brain Behav. 2007;6:209–215. doi: 10.1111/j.1601-183X.2006.00247.x. [DOI] [PubMed] [Google Scholar]
- 36.Iijima A., Haida M., Ishikawa N., Ueno A., Minamitani H., Shinohara Y. Re-evaluation of tropicamide in the pupillary response test for Alzheimer’s disease. Neurobiol. Aging. 2003;24:789. doi: 10.1016/S0197-4580(02)00235-X. [DOI] [PubMed] [Google Scholar]
- 37.Kawasaki A., Ouanes S., Crippa S.V., Popp J., Lee C. Early-stage Alzheimer’s disease does not alter pupil responses to colored light stimuli. J. Alzheimer Dis. 2020;75:1273–1282. doi: 10.3233/JAD-200120. [DOI] [PubMed] [Google Scholar]
- 38.Melov S., Wolf N., Strozyk D., Doctrow S.R., Bush A.I. Mice transgenic for Alzheimer disease β-amyloid develop lens cataracts that are rescued by antioxidant treatment. Free Radic. Biol. Med. 2005;38:258–261. doi: 10.1016/j.freeradbiomed.2004.10.023. [DOI] [PubMed] [Google Scholar]
- 39.Kerbage C., Sadowsky C., Jennings D., Cagle G., Hartung P. Alzheimer’s disease diagnosis by detecting exogenous fluorescent signal of ligand bound to β amyloid in the lens of human eye: An exploratory study. Front. Neurol. 2013;4:62. doi: 10.3389/fneur.2013.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ho C.Y., Troncoso J.C., Knox D., Stark W., Eberhart C.G. β-amyloid, phospho-tau and α-synuclein deposits similar to those in the brain are not identified in the eyes of Alzheimer’s and Parkinson’s disease patients. Brain Pathol. 2014;24:25–32. doi: 10.1111/bpa.12070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michael R., Otto C., Lenferink A., Gelpi E., Montenegro G.A., Rosandić J., Tresserra F., Barraquer R.I., Vrensen G.F.J.M. Absence of amyloid-β in lenses of Alzheimer patients: A confocal Raman microspectroscopic study. Exp. Eye Res. 2014;119:44–53. doi: 10.1016/j.exer.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 42.Sadun A.A., Bassi C.J. Optic nerve damage in Alzheimer’s disease. Ophthalmology. 1990;97:9–17. doi: 10.1016/S0161-6420(90)32621-0. [DOI] [PubMed] [Google Scholar]
- 43.Nishioka C., Liang H.F., Barsamian B., Sun S.W. Amyloid-β induced retrograde axonal degeneration in a mouse tauopathy model. NeuroImage. 2019;189:180–191. doi: 10.1016/j.neuroimage.2019.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun S.W., Nishioka C., Labib W., Liang H.F. Axonal terminals exposed to amyloid-β may not lead to pre-synaptic axonal damage. J. Alzheimer Dis. 2015;45:1139–1148. doi: 10.3233/JAD-142154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bayer A.U., Keller O.N., Ferrari F., Maag K.P. Association of glaucoma with neurodegenerative diseases with apoptotic cell death: Alzheimer’s disease and Parkinson’s disease. Am. J. Ophthalmol. 2002;133:135. doi: 10.1016/S0002-9394(01)01196-5. [DOI] [PubMed] [Google Scholar]
- 46.Wostyn P., Audenaert K., de Deyn P.P. Alzheimer’s disease-related changes in diseases characterized by elevation of intracranial or intraocular pressure. Clin. Neurol. Neurosurg. 2008;110:101–109. doi: 10.1016/j.clineuro.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 47.Choi S.I., Lee B., Woo J.H., Jeong J.B., Jun I., Kim E.K. APP processing and metabolism in corneal fibroblasts and epithelium as a potential biomarker for Alzheimer’s disease. Exp. Eye Res. 2019;182:167–174. doi: 10.1016/j.exer.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 48.Einarsdottir A.B., Hardarson S.H., Kristjansdottir J.V., Bragason D.T., Snaedal J., Stefánsson E. Retinal oximetry imaging in Alzheimer’s disease. J. Alzheimer Dis. 2016;49:79–83. doi: 10.3233/JAD-150457. [DOI] [PubMed] [Google Scholar]
- 49.Olafsdottir O.B., Saevarsdottir H.S., Hardarson S.H., Hannesdottir K.H., Traustadottir V.D., Karlsson R.A., Einarsdottir A.B., Jonsdottir K.D., Stefansson E., Snaedal J. Retinal oxygen metabolism in patients with mild cognitive impairment. Alzheimer Dement. Diagn. Assess. Disease Monit. 2018;10:340–345. doi: 10.1016/j.dadm.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koronyo Y., Biggs D., Barron E., Boyer D.S., Pearlman J.A., Au W.J., Kile S.J., Blanco A., Fuchs D.T., Ashfaq A., et al. Retinal amyloid pathology and proof-of-concept imaging trial in Alzheimer’s disease. JCI Insight. 2017;2:e93621. doi: 10.1172/jci.insight.93621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Koronyo Y., Salumbides B.C., Black K.L., Koronyo-Hamaoui M. Alzheimer’s disease in the retina: Imaging retinal aβ plaques for early diagnosis and therapy assessment. Neurodegener. Dis. 2012;10:285–293. doi: 10.1159/000335154. [DOI] [PubMed] [Google Scholar]
- 52.Den Haan J., Morrema T.H.J., Verbraak F.D., de Boer J.F., Scheltens P., Rozemuller A.J., Bergen A.A.B., Bouwman F.H., Hoozemans J.J. Amyloid-β and phosphorylated tau in post-mortem Alzheimer’s disease retinas. Acta Neuropathol. Commun. 2018;6:147. doi: 10.1186/s40478-018-0650-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chiasseu M., Alarcon-Martinez L., Belforte N., Quintero H., Dotigny F., Destroismaisons L., Vande Velde C., Panayi F., Louis C., Di Polo A. Tau accumulation in the retina promotes early neuronal dysfunction and precedes brain pathology in a mouse model of Alzheimer’s disease. Mol. Neurodegener. 2017;12:58. doi: 10.1186/s13024-017-0199-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shi H., Koronyo Y., Rentsendorj A., Regis G.C., Sheyn J., Fuchs D.T., Kramerov A.A., Ljubimov A.V., Dumitrascu O.M., Rodriguez A.R. Identification of early pericyte loss and vascular amyloidosis in Alzheimer’s disease retina. Acta Neuropathol. 2020;139:813–836. doi: 10.1007/s00401-020-02134-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Frost S., Kanagasingam Y., Sohrabi H., Vignarajan J., Bourgeat P., Salvado O., Villemagne V., Rowe C.C., Macaulay S.L., Szoeke C. Retinal vascular biomarkers for early detection and monitoring of Alzheimer’s disease. Transl. Psychiatry. 2013;3:e233. doi: 10.1038/tp.2012.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheung C.Y.L., Ong Y.T., Ikram M.K., Ong S.Y., Li X., Hilal S., Catindig J.A.S., Venketasubramanian N., Yap P., Seow D. Microvascular network alterations in the retina of patients with Alzheimer’s disease. Alzheimer Dement. 2014;10:135–142. doi: 10.1016/j.jalz.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 57.Liu S., Zhu S. Correlation between Alzheimer disease and cataract [Zhonghua yan ke za Zhi] Chin. J. Ophthalmol. 2017;53:314–316. doi: 10.3760/cma.j.issn.0412-4081.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 58.Frederikse P.H., Zigler S.J., Jr. Presenilin expression in the ocular lens. Curr. Eye Res. 1998;17:947–952. doi: 10.1076/ceyr.17.9.947.5135. [DOI] [PubMed] [Google Scholar]
- 59.Prakasam A., Anusuyadevi M., Ablonczy Z., Greig N.H., Fauq A., Rao K.J., Pappolla M.A., Sambamurti K. Differential accumulation of secreted AβPP metabolites in ocular fluids. J. Alzheimer Dis. 2010;20:1243–1253. doi: 10.3233/JAD-2010-100210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kwak D.E., Ko T., Koh H.S., Ji Y.W., Shin J., Kim K., Kim H.Y., Lee H.K., Kim Y. Alterations of aqueous humor Aβ levels in Aβ-infused and transgenic mouse models of Alzheimer disease. PLoS ONE. 2020;15:e0227618. doi: 10.1371/journal.pone.0227618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wright L.M., Stein T.D., Jun G., Chung J., McConnell K., Fiorello M., Siegel N., Ness S., Xia W., Turner K.L., et al. Association of cognitive function with amyloid-β and tau proteins in the vitreous humor. J. Alzheimers Dis. 2019;68:1429–1438. doi: 10.3233/JAD-181104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cunha J.P., Proença R., Dias-Santos A., Melancia D., Almeida R., Águas H., Santos B.O., Alves M., Ferreira J., Papoila A.L., et al. Choroidal thinning: Alzheimer’s disease and aging. Alzheimer Dement. Diagn. Assess. Dis. Monitor. 2017;8:11–17. doi: 10.1016/j.dadm.2017.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Trebbastoni A., Marcelli M., Mallone F., D’Antonio F., Imbriano L., Campanelli A., de Lena C., Gharbiya M. Attenuation of choroidal thickness in patients with Alzheimer disease. Alzheimer Dis. Assoc. Disord. 2017;31:128–134. doi: 10.1097/WAD.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 64.Mancino R., Martucci A., Cesareo M., Giannini C., Corasaniti M.T., Bagetta G., Nucci C. Glaucoma and Alzheimer Disease: One age-related neurodegenerative disease of the brain. Curr. Neuropharmacol. 2018;16:971–977. doi: 10.2174/1570159X16666171206144045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mirzaei M., Gupta V.B., Chick J.M., Greco T.M., Wu Y., Chitranshi N., Wall R.V., Hone E., Deng L., Dheer Y., et al. Age-related neurodegenerative disease associated pathways identified in retinal and vitreous proteome from human glaucoma eyes. Sci. Rep. 2017;7:12685. doi: 10.1038/s41598-017-12858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Goel M., Picciani R.G., Lee R.K., Bhattacharya S.K. Aqueous humor dynamics: A review. Open Ophthalmol. J. 2010;4:52. doi: 10.2174/1874364101004010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weinreb R.N., Aung T., Medeiros F.A. The pathophysiology and treatment of glaucoma: A review. JAMA. 2014;311:1901–1911. doi: 10.1001/jama.2014.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Davis B.M., Crawley L., Pahlitzsch M., Javaid F., Cordeiro M.F. Glaucoma: The retina and beyond. Acta Neuropathol. 2016;132:807–826. doi: 10.1007/s00401-016-1609-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Den Haan J., Verbraak F.D., Visser P.J., Bouwman F.H. Retinal thickness in Alzheimer’s disease: A systematic review and meta-analysis. Alzheimers Dement. 2017;6:162–170. doi: 10.1016/j.dadm.2016.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wostyn P., van Dam D., de Deyn P.P. Alzheimer’s disease and glaucoma: Look-alike neurodegenerative diseases. Alzheimers Dement. 2019;15:600–601. doi: 10.1016/j.jalz.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 71.Ishikawa M., Yoshitomi T., Covey D.F., Zorumski C.F., Izumi Y. Neurosteroids and oxysterols as potential therapeutic agents for glaucoma and Alzheimer’s disease. Neuropsychiatry. 2018;8:344–359. doi: 10.4172/Neuropsychiatry.1000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liu Y., Wei W., Baazaoui N., Liu F., Iqbal K. Inhibition of AMD-like pathology with a neurotrophic compound in aged rats and 3xTg-AD mice. Front. Aging. Neurosci. 2019;11:309. doi: 10.3389/fnagi.2019.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hadziahmetovic M., Song Y., Wolkow N., Iacovelli J., Kautz L., Roth M.P., Dunaief J.L. Bmp6 regulates retinal iron homeostasis and has altered expression in age-related macular degeneration. Am. J. Pathol. 2011;179:335–348. doi: 10.1016/j.ajpath.2011.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lynn S.A., Keeling E., Munday R., Gabha G., Griffiths H., Lotery A.J., Ratnayaka J.A. The complexities underlying age-related macular degeneration: Could amyloid β play an important role? Neural. Regen. Res. 2017;12:538–548. doi: 10.4103/1673-5374.205083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Madeira M.H., Boia R., Santos P.F., Ambrosio A.F., Santiago A.R. Contribution of microglia-mediated neuroinflammation to retinal degenerative diseases. Mediators Inflamm. 2015;2015:673090. doi: 10.1155/2015/673090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Masuzzo A., Dinet V., Cavanagh C., Mascarelli F., Krantic S. Amyloidosis in retinal neurodegenerative diseases. Front. Neurol. 2016;7:127. doi: 10.3389/fneur.2016.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bergen A.A., Arya S., Koster C., Pilgrim M.G., Wiatrek-Moumoulidis D., van der Spek P.J., Hauck S.M., Boon C.J.F., Emri E., Stewart A.J., et al. On the origin of proteins in human drusen: The meet, greet and stick hypothesis. Prog. Retin. Eye Res. 2019;70:55–84. doi: 10.1016/j.preteyeres.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 78.Lee C.S., Larson E.B., Gibbons L.E., Lee A.Y., McCurry S.M., Bowen J.D., McCormick W.C., Crane P.K. Associations between recent and established ophthalmic conditions and risk of Alzheimer’s disease. Alzheimers Dement. 2019;15:34–41. doi: 10.1016/j.jalz.2018.06.2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Haass C., Kaether C., Thinakaran G., Sisodia S. Trafficking and proteolytic processing of APP. Cold Spring. Harb. Perspect. Med. 2012;2:a006270. doi: 10.1101/cshperspect.a006270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mockett B.G., Richter M., Abraham W.C., Muller U.C. Therapeutic potential of secreted amyloid precursor protein APPsalpha. Front. Mol. Neurosci. 2017;10:30. doi: 10.3389/fnmol.2017.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hart N.J., Koronyo Y., Black K.L., Koronyo-Hamaoui M. Ocular indicators of Alzheimer’s: Exploring disease in the retina. Acta Neuropathol. 2016;132:767–787. doi: 10.1007/s00401-016-1613-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gupta V.K., Chitranshi N., Gupta V.B., Golzan M., Dheer Y., Wall R.V., Georgevsky D., King A.E., Vickers J.C., Chung R., et al. Amyloid β accumulation and inner retinal degenerative changes in Alzheimer’s disease transgenic mouse. Neurosci. Lett. 2016;623:52–56. doi: 10.1016/j.neulet.2016.04.059. [DOI] [PubMed] [Google Scholar]
- 83.Joly S., Lamoureux S., Pernet V. Nonamyloidogenic processing of amyloid β precursor protein is associated with retinal function improvement in aging male APPswe/PS1DeltaE9 mice. Neurobiol. Aging. 2017;53:181–191. doi: 10.1016/j.neurobiolaging.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 84.Edwards M.M., Rodriguez J.J., Gutierrez-Lanza R., Yates J., Verkhratsky A., Lutty G.A. Retinal macroglia changes in a triple transgenic mouse model of Alzheimer’s disease. Exp. Eye Res. 2014;127:252–260. doi: 10.1016/j.exer.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guo L., Salt T.E., Luong V., Wood N., Cheung W., Maass A., Ferrari G., Russo-Marie F., Sillito A.M., Cheetham M.E. Targeting amyloid-β in glaucoma treatment. Proc. Natl. Acad. Sci. USA. 2007;104:13444–13449. doi: 10.1073/pnas.0703707104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chiu K., Chan T.F., Wu A., Leung I.Y.P., So K.F., Chang R.C.C. Neurodegeneration of the retina in mouse models of Alzheimer’s disease: What can we learn from the retina? Age. 2012;34:633–649. doi: 10.1007/s11357-011-9260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chiasseu M., Cueva Vargas J.L., Destroismaisons L., Vande Velde C., Leclerc N., Di Polo A. Tau Accumulation, Altered Phosphorylation, and Missorting Promote Neurodegeneration in Glaucoma. J. Neurosci. 2016;36:5785–5798. doi: 10.1523/JNEUROSCI.3986-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Walsh D., Bresciani L., Saunders D., Manca M., Jen A., Gentleman S., Jen L. Amyloid β peptide causes chronic glial cell activation and neuro-degeneration after intravitreal injection. Neuropathol. Appl. Neurobiol. 2005;31:491–502. doi: 10.1111/j.1365-2990.2005.00666.x. [DOI] [PubMed] [Google Scholar]
- 89.Ho W.L., Leung Y., Tsang A.W.T., So K.F., Chiu K., Chang R.C.C. Tauopathy in the retina and optic nerve: Does it shadow pathological changes in the brain? Mol. Vis. 2012;18:2700. [PMC free article] [PubMed] [Google Scholar]
- 90.Shah T.M., Gupta S.M., Chatterjee P., Campbell M., Martins R.N. β-amyloid sequelae in the eye: A critical review on its diagnostic significance and clinical relevance in Alzheimer’s disease. Mol. Psychiatry. 2017;22:353–363. doi: 10.1038/mp.2016.251. [DOI] [PubMed] [Google Scholar]
- 91.Rhein V., Song X., Wiesner A., Ittner L.M., Baysang G., Meier F., Ozmen L., Bluethmann H., Drose S., Brandt U., et al. Amyloid-β and tau synergistically impair the oxidative phosphorylation system in triple transgenic Alzheimer’s disease mice. Proc. Natl. Acad. Sci. USA. 2009;106:20057–20062. doi: 10.1073/pnas.0905529106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Butterfield D.A., Boyd-Kimball D. Oxidative stress, amyloid-β peptide, and altered key molecular pathways in the pathogenesis and progression of Alzheimer’s Disease. J. Alzheimers Dis. 2018;62:1345–1367. doi: 10.3233/JAD-170543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Guo L.Y., Alekseev O., Li Y., Song Y., Dunaief J.L. Iron increases APP translation and amyloid-β production in the retina. Exp. Eye Res. 2014;129:31–37. doi: 10.1016/j.exer.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nilson A.N., English K.C., Gerson J.E., Barton Whittle T., Nicolas Crain C., Xue J., Sengupta U., Castillo-Carranza D.L., Zhang W., Gupta P., et al. Tau oligomers associate with inflammation in the brain and retina of tauopathy mice and in neurodegenerative diseases. J. Alzheimers Dis. 2017;55:1083–1099. doi: 10.3233/JAD-160912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fernández-Albarral J.A., Salobrar-García E., Martínez-Páramo R., Ramírez A.I., de Hoz R., Ramírez J.M., Salazar J.J. Retinal glial changes in Alzheimer’s disease–A review. J. Optom. 2019;12:198–207. doi: 10.1016/j.optom.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ohno-Matsui K. Parallel findings in age-related macular degeneration and Alzheimer’s disease. Prog. Retin. Eye Res. 2011;30:217–238. doi: 10.1016/j.preteyeres.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 97.Ong S.S., Proia A.D., Whitson H.E., Farsiu S., Doraiswamy P.M., Lad E.M. Ocular amyloid imaging at the crossroad of Alzheimer’s disease and age-related macular degeneration: Implications for diagnosis and therapy. J. Neurol. 2019;266:1566–1577. doi: 10.1007/s00415-018-9028-z. [DOI] [PubMed] [Google Scholar]
- 98.Zhao Y., Bhattacharjee S., Jones B.M., Hill J.M., Clement C., Sambamurti K., Dua P., Lukiw W.J. β-amyloid precursor protein (β APP) processing in Alzheimer’s disease (AD) and age-related macular degeneration (AMD) Mol. Neurobiol. 2015;52:533–544. doi: 10.1007/s12035-014-8886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Prasad T., Zhu P., Verma A., Chakrabarty P., Rosario A.M., Golde T.E., Li Q. Amyloid β peptides overexpression in retinal pigment epithelial cells via AAV-mediated gene transfer mimics AMD-like pathology in mice. Sci. Rep. 2017;7:3222. doi: 10.1038/s41598-017-03397-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rong S.S., Lee B.Y., Kuk A.K., Yu X.T., Li S.S., Li J., Guo Y., Yin Y. Comorbidity of dementia and age-related macular degeneration calls for clinical awareness: A meta-analysis. Br. J. Ophthalmol. 2019;103:1777–1783. doi: 10.1136/bjophthalmol-2018-313277. [DOI] [PubMed] [Google Scholar]
- 101.Onuska K.M. The dual role of microglia in the progression of Alzheimer’s disease. J. Neurosci. 2020;40:1608–1610. doi: 10.1523/JNEUROSCI.2594-19.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tejera D., Mercan D., Sanchez-Caro J.M., Hanan M., Greenberg D., Soreq H., Latz E., Golenbock D., Heneka M.T. Systemic inflammation impairs microglial Abeta clearance through NLRP3 inflammasome. EMBO J. 2019;38:e101064. doi: 10.15252/embj.2018101064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lane D.J.R., Ayton S., Bush A.I. Iron and Alzheimer’s disease: An update on emerging mechanisms. J. Alzheimers Dis. 2018;64:S379–S395. doi: 10.3233/JAD-179944. [DOI] [PubMed] [Google Scholar]
- 104.Vela D. Hepcidin, an emerging and important player in brain iron homeostasis. J. Transl. Med. 2018;16:25. doi: 10.1186/s12967-018-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shu W., Baumann B.H., Song Y., Liu Y., Wu X., Dunaief J.L. Ferrous but not ferric iron sulfate kills photoreceptors and induces photoreceptor-dependent RPE autofluorescence. Redox. Biol. 2020;34:101469. doi: 10.1016/j.redox.2020.101469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wang L., Liu X., You L.H., Ci Y.Z., Chang S., Yu P., Gao G., Chang Y.Z. Hepcidin and iron regulatory proteins coordinately regulate ferroportin 1 expression in the brain of mice. J. Cell. Physiol. 2019;234:7600–7607. doi: 10.1002/jcp.27522. [DOI] [PubMed] [Google Scholar]
- 107.Nemeth E., Tuttle M.S., Powelson J., Vaughn M.B., Donovan A., Ward D.M., Ganz T., Kaplan J. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306:2090–2093. doi: 10.1126/science.1104742. [DOI] [PubMed] [Google Scholar]
- 108.Qian Z.M., Ke Y. Hepcidin and its therapeutic potential in neurodegenerative disorders. Med. Res. Rev. 2020;40:633–653. doi: 10.1002/med.21631. [DOI] [PubMed] [Google Scholar]
- 109.You L.H., Yan C.Z., Zheng B.J., Ci Y.Z., Chang S.Y., Yu P., Gao G.F., Li H.Y., Dong T.Y., Chang Y.Z. Astrocyte hepcidin is a key factor in LPS-induced neuronal apoptosis. Cell. Death Dis. 2017;8:e2676. doi: 10.1038/cddis.2017.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hänninen M.M., Haapasalo J., Haapasalo H., Fleming R.E., Britton R.S., Bacon B.R., Parkkila S. Expression of iron-related genes in human brain and brain tumors. BMC Neurosci. 2009;10:36. doi: 10.1186/1471-2202-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ashok A., Chaudhary S., Kritikos A.E., Kang M.H., McDonald D., Rhee D.J., Singh N. TGFβ2-hepcidin feed-forward loop in the trabecular meshwork implicates iron in glaucomatous pathology. Investig. Ophthalmol. Vis. Sci. 2020;61:24. doi: 10.1167/iovs.61.3.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ashok A., Chaudhary S., McDonald D., Kritikos A., Bhargava D., Singh N. Local synthesis of hepcidin in the anterior segment of the eye: A novel observation with physiological and pathological implications. Exp. Eye Res. 2020;190:107890. doi: 10.1016/j.exer.2019.107890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gnana-Prakasam J.P., Martin P.M., Mysona B.A., Roon P., Smith S.B., Ganapathy V. Hepcidin expression in mouse retina and its regulation via lipopolysaccharide/Toll-like receptor-4 pathway independent of Hfe. Biochem. J. 2008;411:79–88. doi: 10.1042/BJ20071377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nemeth E., Rivera S., Gabayan V., Keller C., Taudorf S., Pedersen B.K., Ganz T. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J. Clin. Investig. 2004;113:1271–1276. doi: 10.1172/JCI200420945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Benoist d’Azy C., Pereira B., Chiambaretta F., Dutheil F. Oxidative and anti-oxidative stress markers in chronic glaucoma: A systematic review and meta-analysis. PLoS ONE. 2016;11:e0166915. doi: 10.1371/journal.pone.0166915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schwab C., Paar M., Fengler V.H., Lindner E., Haas A., Ivastinovic D., Seidel G., Weger M., Wedrich A., Oettl K. Vitreous albumin redox state in open-angle glaucoma patients and controls: A pilot study. Int. Ophthalmol. 2020;40:999–1006. doi: 10.1007/s10792-019-01268-5. [DOI] [PubMed] [Google Scholar]
- 117.Ung L., Pattamatta U., Carnt N., Wilkinson-Berka J.L., Liew G., White A.J.R. Oxidative stress and reactive oxygen species: A review of their role in ocular disease. Clin. Sci. 2017;131:2865–2883. doi: 10.1042/CS20171246. [DOI] [PubMed] [Google Scholar]
- 118.Song D., Kanu L.N., Li Y., Kelly K.L., Bhuyan R.K., Aleman T., Morgan J.I., Dunaief J.L. AMD-like retinopathy associated with intravenous iron. Exp. Eye Res. 2016;151:122–133. doi: 10.1016/j.exer.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shu W., Dunaief J.L. Potential treatment of retinal diseases with iron chelators. Pharmaceuticals. 2018;11:112. doi: 10.3390/ph11040112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Song D., Dunaief J.L. Retinal iron homeostasis in health and disease. Front. Aging Neurosci. 2013;5:24. doi: 10.3389/fnagi.2013.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jünemann A.G., Stopa P., Michalke B., Chaudhri A., Reulbach U., Huchzermeyer C., Schlötzer-Schrehardt U., Kruse F.E., Zrenner E., Rejdak R. Levels of aqueous humor trace elements in patients with non-exsudative age-related macular degeneration: A case-control study. PLoS ONE. 2013;8:e56734. doi: 10.1371/journal.pone.0056734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chowers I., Wong R., Dentchev T., Farkas R.H., Iacovelli J., Gunatilaka T.L., Medeiros N.E., Presley J.B., Campochiaro P.A., Curcio C.A. The iron carrier transferrin is upregulated in retinas from patients with age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2006;47:2135–2140. doi: 10.1167/iovs.05-1135. [DOI] [PubMed] [Google Scholar]
- 123.Ding J.D., Johnson L.V., Herrmann R., Farsiu S., Smith S.G., Groelle M., Mace B.E., Sullivan P., Jamison J.A., Kelly U., et al. Anti-amyloid therapy protects against retinal pigmented epithelium damage and vision loss in a model of age-related macular degeneration. Proc. Natl. Acad. Sci. USA. 2011;108:E279–E287. doi: 10.1073/pnas.1100901108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dekens D.W., De Deyn P.P., Sap F., Eisel U.L., Naudé P.J. Iron chelators inhibit amyloid-β-induced production of lipocalin 2 in cultured astrocytes. Neurochem. Int. 2020;132:104607. doi: 10.1016/j.neuint.2019.104607. [DOI] [PubMed] [Google Scholar]
- 125.Palanimuthu D., Wu Z., Jansson P.J., Braidy N., Bernhardt P.V., Richardson D.R., Kalinowski D.S. Novel chelators based on adamantane-derived semicarbazones and hydrazones that target multiple hallmarks of Alzheimer’s disease. Dalton Trans. 2018;47:7190–7205. doi: 10.1039/C8DT01099D. [DOI] [PubMed] [Google Scholar]
- 126.Nuñez M.T., Chana-Cuevas P. New perspectives in iron chelation therapy for the treatment of neurodegenerative diseases. Pharmaceuticals. 2018;11:109. doi: 10.3390/ph11040109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cui Q.N., Bargoud A.R., Ross A.G., Song Y., Dunaief J.L. Oral administration of the iron chelator deferiprone protects against loss of retinal ganglion cells in a mouse model of glaucoma. Exp. Eye Res. 2020;193:107961. doi: 10.1016/j.exer.2020.107961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhao L., Hadziahmetovic M., Wang C., Xu X., Song Y., Jinnah H.A., Wodzinska J., Iacovelli J., Wolkow N., Krajacic P., et al. Cp/Heph mutant mice have iron-induced neurodegeneration diminished by deferiprone. J. Neurochem. 2015;135:958–974. doi: 10.1111/jnc.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ueda K., Kim H.J., Zhao J., Song Y., Dunaief J.L. Iron promotes oxidative cell death caused by bisretinoids of retina. Proc. Natl. Acad. Sci. USA. 2018;115:4963–4968. doi: 10.1073/pnas.1722601115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Poli M., Asperti M., Ruzzenenti P., Naggi A., Arosio P. Non-anticoagulant heparins are hepcidin antagonists for the treatment of anemia. Molecules. 2017;22:598. doi: 10.3390/molecules22040598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Adornetto A., Russo R., Parisi V. Neuroinflammation as a target for glaucoma therapy. Neural. Regen. Res. 2019;14:391–394. doi: 10.4103/1673-5374.245465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Russo R., Varano G.P., Adornetto A., Nucci C., Corasaniti M.T., Bagetta G., Morrone L.A. Retinal ganglion cell death in glaucoma: Exploring the role of neuroinflammation. Eur. J. Pharmacol. 2016;787:134–142. doi: 10.1016/j.ejphar.2016.03.064. [DOI] [PubMed] [Google Scholar]
- 133.Zhu S., Wang D., Han J. Effect of a topical combination of latanoprost and pranoprofen on intraocular pressure and the ocular surface in open-angle glaucoma patients. J. Ophthalmol. 2018;2018:7474086. doi: 10.1155/2018/7474086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Katsarou A., Pantopoulos K. Hepcidin therapeutics. Pharmaceuticals. 2018;11:127. doi: 10.3390/ph11040127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Prusiner S.B. Prions. Proc. Natl. Acad. Sci. USA. 1998;95:13363–13383. doi: 10.1073/pnas.95.23.13363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Scheckel C., Aguzzi A. Prions, prionoids and protein misfolding disorders. Nat. Rev. Gen. 2018;19:405–418. doi: 10.1038/s41576-018-0011-4. [DOI] [PubMed] [Google Scholar]
- 137.Singh N. The role of iron in prion disease and other neurodegenerative diseases. PLoS Pathog. 2014;10:e1004335. doi: 10.1371/journal.ppat.1004335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Singh N., Singh A., Das D., Mohan M.L. Redox control of prion and disease pathogenesis. Antioxid. Redox Signal. 2010;12:1271–1294. doi: 10.1089/ars.2009.2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Castle A.R., Gill A.C. Physiological functions of the cellular prion protein. Front. Mol. Biosci. 2017;4:19. doi: 10.3389/fmolb.2017.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ezpeleta J., Boudet-Devaud F., Pietri M., Baudry A., Baudouin V., Alleaume-Butaux A., Dagoneau N., Kellermann O., Launay J.M., Schneider B. Protective role of cellular prion protein against TNFα-mediated inflammation through TACE α-secretase. Sci. Rep. 2017;7:7671. doi: 10.1038/s41598-017-08110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Asthana A., Baksi S., Ashok A., Karmakar S., Mammadova N., Kokemuller R., Greenlee M.H., Kong Q., Singh N. Prion protein facilitates retinal iron uptake and is cleaved at the β-site: Implications for retinal iron homeostasis in prion disorders. Sci. Rep. 2017;7:9600. doi: 10.1038/s41598-017-08821-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Purro S.A., Nicoll A.J., Collinge J. Prion protein as a toxic acceptor of amyloid-β oligomers. Biol. Psychiatry. 2018;83:358–368. doi: 10.1016/j.biopsych.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 143.Lauren J., Gimbel D.A., Nygaard H.B., Gilbert J.W., Strittmatter S.M. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-β oligomers. Nature. 2009;457:1128–1132. doi: 10.1038/nature07761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Brody A.H., Strittmatter S.M. Synaptotoxic signaling by amyloid β oligomers in Alzheimer’s disease through prion protein and mGluR5. Adv. Pharmacol. 2018;82:293–323. doi: 10.1016/bs.apha.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang Y., Zhao Y., Zhang L., Yu W., Wang Y., Chang W. Cellular prion protein as a receptor of toxic amyloid-β 42 oligomers is important for Alzheimer’s disease. Front. Cell. Neurosci. 2019;13:339. doi: 10.3389/fncel.2019.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Nygaard H.B., van Dyck C.H., Strittmatter S.M. Fyn kinase inhibition as a novel therapy for Alzheimer’s disease. Alzheimer Res. Ther. 2014;6:8. doi: 10.1186/alzrt238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Altmeppen H.C., Puig B., Dohler F., Thurm D.K., Falker C., Krasemann S., Glatzel M. Proteolytic processing of the prion protein in health and disease. Am. J. Neurodegener. Dis. 2012;1:15. [PMC free article] [PubMed] [Google Scholar]
- 148.Linsenmeier L., Altmeppen H.C., Wetzel S., Mohammadi B., Saftig P., Glatzel M. Diverse functions of the prion protein-Does proteolytic processing hold the key? Biochim. Biophys. Acta Mol. Cell. Res. 2017;1864:2128–2137. doi: 10.1016/j.bbamcr.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 149.Asai M., Hattori C., Szabó B., Sasagawa N., Maruyama K., Tanuma S.i., Ishiura S. Putative function of ADAM9, ADAM10, and ADAM17 as APP α-secretase. Biochem. Biophys. Res. Commun. 2003;301:231–235. doi: 10.1016/S0006-291X(02)02999-6. [DOI] [PubMed] [Google Scholar]
- 150.Renner M., Lacor P.N., Velasco P.T., Xu J., Contractor A., Klein W.L., Triller A. Deleterious effects of amyloid β oligomers acting as an extracellular scaffold for mGluR5. Neuron. 2010;66:739–754. doi: 10.1016/j.neuron.2010.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Frigg R., Wenzel A., Samardzija M., Oesch B., Wariwoda H., Navarini A.A., Seeliger M.W., Tanimoto N., Remé C., Grimm C. The prion protein is neuroprotective against retinal degeneration in vivo. Exp. Eye Res. 2006;2006 83:1350–1358. doi: 10.1016/j.exer.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 152.Loubet D., Dakowski C., Pietri M., Pradines E., Bernard S., Callebert J., Ardila-Osorio H., Mouillet-Richard S., Launay J.M., Kellermann O., et al. Neuritogenesis: The prion protein controls β 1 integrin signaling activity. FASEB J. 2012;26:678–690. doi: 10.1096/fj.11-185579. [DOI] [PubMed] [Google Scholar]
- 153.Alleaume-Butaux A., Nicot S., Pietri M., Baudry A., Dakowski C., Tixador P., Ardila-Osorio H., Haeberle A.M., Bailly Y., Peyrin J.M., et al. Double-edge sword of sustained ROCK activation in prion diseases through neuritogenesis defects and prion accumulation. PLoS Pathog. 2015;11:e1005073. doi: 10.1371/journal.ppat.1005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kim H.J., Choi H.S., Park J.H., Kim M.J., Lee H.G., Petersen R.B., Kim Y.S., Park J.B., Choi E.K. Regulation of RhoA activity by the cellular prion protein. Cell. Death Dis. 2017;8:e2668. doi: 10.1038/cddis.2017.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Bertuchi F.R., Bourgeon D.M., Landemberger M.C., Martins V.R., Cerchiaro G. PrPC displays an essential protective role from oxidative stress in an astrocyte cell line derived from PrPC knockout mice. Biochem. Biophys. Res. Commun. 2012;418:27–32. doi: 10.1016/j.bbrc.2011.12.098. [DOI] [PubMed] [Google Scholar]
- 156.Zeng F., Watt N.T., Walmsley A.R., Hooper N.M. Tethering the N-terminus of the prion protein compromises the cellular response to oxidative stress. J. Neurochem. 2003;84:480–490. doi: 10.1046/j.1471-4159.2003.01529.x. [DOI] [PubMed] [Google Scholar]
- 157.Zeng L., Zou W., Wang G. Cellular prion protein (PrPC) and its role in stress responses. Int. J. Clin. Exp. Med. 2015;8:8042. [PMC free article] [PubMed] [Google Scholar]
- 158.Dupiereux I., Falisse-Poirrier N., Zorzi W., Watt N.T., Thellin O., Zorzi D., Pierard O., Hooper N.M., Heinen E., Elmoualij B. Protective effect of prion protein via the N-terminal region in mediating a protective effect on paraquat-induced oxidative injury in neuronal cells. J. Neurosci. Res. 2008;86:653–659. doi: 10.1002/jnr.21506. [DOI] [PubMed] [Google Scholar]
- 159.Haigh C.L., Collins S.J. Endoproteolytic cleavage as a molecular switch regulating and diversifying prion protein function. Neural Regen. Res. 2016;11:238. doi: 10.4103/1673-5374.177726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Brown D.R., Clive C., Haswell S.J. Antioxidant activity related to copper binding of native prion protein. J. Neurochem. 2001;76:69–76. doi: 10.1046/j.1471-4159.2001.00009.x. [DOI] [PubMed] [Google Scholar]
- 161.Singh A., Haldar S., Horback K., Tom C., Zhou L., Meyerson H., Singh N. Prion protein regulates iron transport by functioning as a ferrireductase. J. Alzheimer Dis. 2013;35:541–552. doi: 10.3233/JAD-130218. [DOI] [PMC free article] [PubMed] [Google Scholar]