Abstract
Nasopharyngeal carcinoma (NPC) is a malignant epithelial carcinoma of the head and neck region which mainly distributes in southern China and Southeast Asia and has a crucial association with the Epstein–Barr virus. Based on epidemiological data, both incidence and mortality of NPC have significantly declined in recent decades grounded on the improvement of living standard and medical level in an endemic region, in particular, with the clinical use of individualized chemotherapy and intensity-modulated radiotherapy (IMRT) which profoundly contributes to the cure rate of NPC patients. To tackle the challenges including local recurrence and distant metastasis in the current NPC treatment, we discussed the implication of using targeted therapy against critical molecules in various signal pathways, and how they synergize with chemoradiotherapy in the NPC treatment. Combination treatment including targeted therapy and IMRT or concurrent chemoradiotherapy is presumably to be future options, which may reduce radiation or chemotherapy toxicities and open new avenues for the improvement of the expected functional outcome for patients with advanced NPC.
Subject terms: Cancer, Oncology
Introduction
Nasopharyngeal carcinoma (NPC) is a malignant tumor derived from head and neck epithelial cells. In 2018, there were 129,000 new cases of NPC worldwide, accounting for 0.7% of global cancers, of which the mortality rate of male patients was three times than of females.1 The majority of NPC patients are geographically localized to Southeast Asia, while China is one of the countries that have the highest incidence and mortality rates.2 According to the World Health Organization, NPC is classified into various histological subtypes: keratinizing squamous cell carcinoma (KSCC), non-keratinizing differentiated carcinoma (NKDC), and non-keratinizing undifferentiated carcinoma (NKUC).3 In fact, non-keratinizing subtype closely associated with Epstein–Barr virus (EBV) infection comprises up to 95% of cases in endemic areas, such as southern China, while squamous cell cancers are common in the United States and Europe.4,5 In addition, patients with recurrence or metastasis often have a very poor prognosis due to distant metastasis.6,7
The genetic and epigenetic alterations of NPC have been unveiled by the constant genome-wide studies, which involve cytogenic, allelotyping, CGH, and array-based CGH analysis.8–11 Not only copy numbers losses of chromosome 1p, 3p, 9p, 9q, 11q, 13q, 14q, and 16q but also amplification of chromosome 1q, 3q, 8q, 12p, and 12q were detected in primary NPC by CGH.12–15 Promoter hypermethylation of RASSF1A at 3p21.3, homozygous deletions of CDKN2A at 9p21.3 and TGFBR2 at 3p24 have been regarded as triggers of tumorigenesis.10,16,17 The alterations of the somatic genome were reported when applying NGS technology on normal and tumor specimens, most of which are either EBV-positive or non-keratinizing NPC.18 As an important cause of NPC, EBV infection leads to the expression of various latent viral proteins, such as latent membrane proteins (LMP1, LMP2), BamH1-A fragment rightward reading frame 1 (BARF1) and nuclear antigen (EBNA1).19–21 At the same time, EBV infection also leads to the accumulation of a set of non-coding RNAs.22 Recently, Hong et al.23 found that circCRIM, a kind of circRNAs, promote NPC metastasis and epithelial–mesenchymal transition (EMT) through binding miR-422a to cancel its inhibition to FOXQ1. These viral and host’s genomic products affect the signal transductions and cellular mechanisms of normal nasopharyngeal epithelial cells and have major roles in the pathogenesis of NPC.24 Mutations and repair disorders caused by viral infection are important causes of malignant changes in the nasopharyngeal epithelium. As a main substitution type at NpCpG trinucleotides, the C>T transitions results of spontaneous deamination of 5-methylcytosine, followed by a corrupted DNA mismatch repair signature,25 while C>G and C>T mutations at TpCpN trinucleotides are linked to catalytic polypeptide-like-mediated signature and the apolipoprotein B mRNA-editing enzyme.26 What’s more, there are mismatch repair (MMR) gene mutations and a primary NPC subgroup with a hypermutation phenotype.25 C666-1 which is EBV-positive has its own characteristics of inactivating PMS2 mutation and hypermutation phenotype.
The epigenetic machinery of NPC cells could be altered to reprogram the epigenomes of virus and host cells through EBV-encoded proteins. LMP1 contributes to the expression of DNA methyltransferase and the interaction of EBNA3A and EBNA3C with co-repressor of transcription CtBP could modulate polycomb group protein, which could form higher-order chromatin structures to silence target genes.27,28 The promoter hypermethylation of RASSF1A, BLU, CDKN2A, and DLEC1 could be detected in NPC, which have roles in DNA damage response, stress response, cell proliferation during G1 and STAT3 signal pathway.29–31 What’s more, a variety of tumor-related genes are epigenetically modified, involving transcription factors, enzymes, mitotic checkpoint regulators, cadherins, non-coding RNAs. As the most significantly hypermethylated gene, HOPX is highly associated with early distant metastasis in NPC.32 The antiangiogenic effect and anti-cancer activity of metalloprotease (MMP)-19 are inhibited in NPC by allelic deletion and promoter hypermethylation.33 As a mitotic checkpoint regulator, promoter hypermethylation of CHFR could cancel the impediment to chromatin condensation.34 Sun et al.35 found aberrant methylation of CDH13 could be detected in 89.7% primary NPC tumors with methylation-specific PCR. Long non-coding RNA MEG3 is also silenced epigenetically, which can inhibit proliferation, colony formation, induce cell cycle arrest, and has tumor-suppressive properties in vivo and in vitro.36 Leong also found abnormal histone bivalent switch is linked to suppressing DNA damage repair gene, which indicates another kind of epigenetic modification.
Targeted therapy involves the design of specific drugs that bind specifically to oncogenic targets within tumor cells to inhibit the development of tumors. MicroRNAs inhibit transcription and translation by binding to the 3′-UTR of target mRNA and affect the expression of target proteins, which has an important role in the genesis and development of tumors.37,38 In addition, abnormal activation and silencing of signal pathways in tumor cells also have a crucial role in tumor activities.39–42 Imbalance of the phosphatidylinositol 3-kinase (PI3K)/Akt/mTOR signal pathway is associated with malignant transformation and apoptosis of tumor cells, and metastasis and radioresistance of tumor tissues,43 while abnormal activation of the VEGF pathway is associated with angiogenesis in tumor tissue.44 Upregulation of the Wnt/β-catenin pathway in tumors is closely related to radioresistance,45 activation of the Notch pathway is widely present in human tumors by regulating self-renewal of cells with inhibition of differentiation.46,47 Abnormal activation of the Mitogen-activated protein kinase (MAPK) pathway is associated with proliferation, migration, invasion, and angiogenesis of tumor cells.48,49
In recent years, NPC patients receiving chemoradiotherapy have a poor quality of life, along with severe side effects such as bone suppression.50 However, targeted therapy can accurately identify and treat NPC cells with low toxic and side effects, suggesting a broad prospect of targeted therapy in the clinical treatment of NPC.51 In this article, we reviewed crucial molecules in signal pathways and miRNAs/lncRNAs in NPC cells studied in recent five years, regarding their roles in the promotion or suppression of NPC and functions as potential therapeutic targets of this disease. In addition, we present future perspectives of biomarker-based treatments and clinical diagnoses in NPC.
Crucial signal pathways related to targeted therapy of NPC
Aberrant activation of signal pathways brings about a variety of human diseases. Abnormal transmembrane signal pathways, including prosurvival pathways (PI3K/Akt, NF-κB, MAPK, STAT3, Wnt/β-catenin) and proapoptosis pathways (p53, endoplasmic reticulum stress) in NPC cells, have been proved to be associated with the development, progression, and prognosis of NPC by influencing biological processes such as cell cycle, apoptosis, and DNA repair. They are of potential clinical significance for personalized treatment strategies for NPC. The order of descriptions below corresponds to the depth of the last five years of research.
PI3K/Akt pathway
PI3K phosphorylates phosphatidylinositol 4,5-bisphosphate (PIP2) and converts it to phosphatidylinositol 3,4,5-trisphosphate (PIP3), which is critical for activation of Akt.52 Phosphatase and tensin homolog (PTEN) is a phosphatase that dephosphorylates PIP3, and dephosphorylation of PIP3 can block PI3K/Akt signal pathway.53 mTOR is a serine/threonine kinase that one of the upstream regulators of mTOR is the PI3K/Akt signal pathway.54 In the PI3K/Akt pathway, infrequent mutations of activators or regulators (PIK3CA, PTEN, PIK3R1, AKT2, and mTOR) were observed.25 The 110α catalytic subunit of PI3K is encoded by the PIK3CA gene and PIK3CA amplification likely results in the activation of the PI3K/Akt pathway.55,56 The activation of the PI3K/Akt pathway is also related to EBV-encoded latent membrane proteins 1, 2A, 2B.57
NPC is highly associated with EBV infection and the major oncogenic proteins of EBV are LMP1 and LMP2A.58,59 LMP1 induces anti-TNF-related apoptosis-inducing ligand (TRAIL) activity in NPC cells by activating the PI3K/Akt pathway, thereby promoting the progression of NPC.60 DNA methyltransferase 1 (DNMT1) can mediate the downregulation of PTEN by LMP1 thereby activating Akt signal.61 Downregulation of DNMT1 can reduce the methylation level of the miR-152 gene and improve the expression of miR-152, leading to lower expression of DNMT1 mRNA and protein which inhibits the migration and invasion of tumor cells.62 On the other hand, Li et al.63 found that DNMT1 can promote EMT and metastasis of NPC by inhibiting the miR-142-3p/Zinc-finger E-box binding homeobox 2 (ZEB2) axis. LMP1 can induce lipid synthesis mediated by sterol regulatory element-binding protein 1 (SREBP1) through the mTOR signal pathway to promote cell proliferation and tumor invasion.64 LMP2A-mediated activation of the PI3K/Akt/mTOR/HIF-1α signal cascade can lead to vasculogenic mimicry (VM).65
Recent studies provide a basis for the selection of potential targets for targeted therapy of NPC.
Sodium butyrate (NaBu) may inhibit Akt/mTOR axis activity by promoting the degradation of EGFR in histone deacetylase 6 dependent way in NPC cells.66 Mitogen-activated protein kinase-activated protein kinase 2 (MK2) is a serine/threonine kinase.67 MiR-296-3p can block MK2-induced PI3K/Akt/c-Myc signal pathway by directly targeting and downregulating the expression of MK2 thereby inhibiting cell cycle and EMT as well as cisplatin resistance.68 Studies have demonstrated that miR-374a inhibits PI3K/Akt signal pathway, cell cycle, and EMT signal by directly targeting and downregulating Cyclin D1(CCND1), while CCND1 can activate the PI3K/Akt pathway to increase the expression of c-Jun to downregulate miR-374a.69 As one of the most upregulated lncRNAs, FAM225A could enhance the expression of integrin β3 (ITGB3) by functioning as a miR-590-3p and miR-1275 sponge, thus activating FAK/PI3K/Akt signal pathway related to proliferation and invasion in NPC.70 FOXO1 can inhibit the expression of myosin heavy chain 9 (MYH9) by inhibiting the PI3K/Akt/c-Myc pathway and activating p53/miR-133a-3p axis thereby inhibiting the stem cell characteristics, metastasizing and enhancing the sensitivity to cisplatin of NPC cells.71 MiR-9 inhibits the activation of the PI3K/Akt pathway by targeting and downregulating midkine (MDK).72,73 MiR-92a promotes NPC cell migration and invasion by targeting and downregulating PTEN causing the activation of the PI3K/Akt pathway.74 EBV-miR-BART7-3p, an EBV-encoded BART-microRNA highly expressed in NPC, activates the PI3K/Akt signal pathway, induces the expression of c-Myc and c-Jun, and promotes the growth, proliferation, and tumorigenesis of NPC cells.75 For the downregulation of fibroblast growth factor receptor 2 (FGFR2) can enhance the activation of the caspase pathway caused by cisplatin.76 Fibroblast growth factor 2 (FGF2) is the upstream molecule of the PI3K/Akt signal pathway so that FGF2/FGFR2 has become a crucial target in the targeted therapy of NPC as well.77 MiR-16 can directly target and inhibit FGF2, resulting in the inhibition of both PI3K/Akt and MAPK signal pathways, causing the inhibition of proliferation, migration, and invasion of NPC cells.77 Collagen type I alpha 1 (COL1A1) can regulate the radioresistance of tumor cells through the PI3K/Akt pathway.78 MiR-29a can induce radiosensitivity in NPC cells by directly targeting and downregulating COL1A1.79 RNA-binding motif protein 3 (RBM3) inhibits cancer cells apoptosis by activating the PI3K/Akt/Bcl-2 signal pathway thereby enhancing radiation tolerance.80 Ionizing radiation (IR) can increase the expression of phosphatase 1 nuclear-targeting subunit (PNUTS) in NPC cells, which induces EMT by activating the PI3K/Akt signal pathway.81 Annexin A1 inhibits the autophagy pathway of NPC cells by increasing Akt phosphorylation level and membrane transport to activate the PI3K/Akt pathway thereby upregulating Sequestosome-1 (SQSTM1) and Snail, inducing EMT in NPC cells and promoting NPC cell migration, invasion, and metastasis.82 Besides, IL-8 can regulate NPC metastasis by means of activating Akt signaling and inducing EMT of NPC cells.83,84 Downregulation of cyclin-dependent kinase inhibitor 3 (CDKN3) decreases the phosphorylation of Akt and inhibits the increase in the size and weight of transplanted tumors.85 C-Src in NPC cells promotes the EMT process to improve the metastatic ability of cancer cells by activating the PI3K/Akt pathway.86 The cell membrane alteration also makes an important impact in metastasis. Flotillin-2 (Flot-2), a key component of lipid rafts, is found to be a high sensitivity biomarker for lymph node metastasis in NPC.87 Silencing Flot-2 expression in 5-8F cells suppressed metastasis and proliferation as a result of inhibiting NF-κB and PI3K/Akt3 signal pathways.88 Besides, the important role of Flot-2 in the progression of NPC might be partially linked to its interaction with PLC-δ3 (PLCD3).89 In addition, as a type I transmembrane glycoprotein, the role of epithelial cell adhesion molecule (EpCAM) in different cancers is distinct which might depend on the cell type and microenvironment. In head and neck squamous cell carcinomas (HNSCCs), the extracellular domain of EpCAM (EpEX) has a role of a ligand of EGFR that induces EGFR-dependent proliferation but counteracts EGF-induced EMT.90 On the contrary, the overexpression of EpCAM could promote EMT and stemness and metastasis through PTEN/AKT/mTOR signal pathway in NPC cells.91 Li et al. found that EphA2 is associated with the formation of NPC as a tumor promoter. In particular, the phosphorylation of EphA2 at serine 897 site act as a predominant role in the clinical metastasis of NPC. pS897 EphA2 activates PI3K through the regulatory subunit p85 of PI3K, which may promote NPC invasion, metastasis, and cancer stem cell characteristics.92
Leucine zipper tumor suppressor 2 (LZTS2) can inhibit the activation of PI3K/Akt signal pathway causing the inhibition of tumorigenesis and radioresistance in NPC.93 LMP1 can increase miR-155 expression and miR-155–UBQLN1 axis can affect the proliferation, cell cycle, and EMT progression of NPC cells by activating PI3K/Akt pathway.94 MiR-18a can activate mTOR by targeting and downregulating suppressor of morphogenesis in genitalia 1 (SMG1), which is an antagonist of mTOR in NPC. Nuclear factor-kappa B (NF-κB) activation and LMP1 expression can induce miR-18a expression in NPC cells.95
In summary, in addition to directly targeted inhibition of PI3K, Akt, and mTOR, targeted inhibition of HIF-1α, MK2, CCND1, lncRNA FAM225A, MYH9, MDK, miR-92a, miR-18a, EBV-miR-BART7-3p, FGF2, COL1A1, RBM3, PNUTS, Annexin A1, IL-8, CDKN3, c-Src, Flot-2, EpCAM, OCT4, BEX3, and targeted activation of LZTS2, UBQLN1, SMG1 may become potential therapeutic strategies that affecting the PI3K/Akt pathway in NPC.
p53 pathway
TP53 was consistently regarded as one of the significantly mutated genes in NPC through whole-exome sequencing (WES)/whole-genome sequencing studies (WGS).26 As a tumor suppressor gene, its mutation is related to cancer progression and treatment resistance.96 The level of p53 protein in cells is tightly controlled by its negative regulator, the E3 ubiquitin-protein ligase murine double minute 2 (MDM2).97 Nutlin-3 competitively inhibits MDM2 and activates the p53 pathway, thereby increasing the sensitivity of NPC cells to cisplatin.98 MDM2 inhibitor RG7388 can activate the p53 pathway, increase the expression of p21 protein and caspase family protein that mediate cell cycle arrest, ultimately leading to cell cycle arrest, cell proliferation inhibition, and apoptosis induction.99
Other recent studies have provided evidence for the selection of p53-related targets to NPC treatment. Shi et al. found that cycloxygenase-2 (COX-2) may suppress chemotherapy-induced senescence by inhibiting the activation of p53. This study provided an experimental basis for anti-tumor therapy by targeting COX-2.100 FOXO1 suppresses the expression of MYH9 by inhibiting the PI3K/Akt/c-Myc/p53/miR-133a-3p pathway, thereby inhibiting the stem cell characteristics, metastasis and increasing cisplatin sensitivity of NPC cells.71 B-cell-specific Moloney murine leukemia virus insertion site 1 (Bmi-1) can improve the proliferation, migration, and invasion ability of NPC cells by inhibiting the p16INK4a-p14ARF-p53 pathway. Targeted silencing of Bmi-1 may have potential clinical significance in the treatment of NPC.101 As a tumor suppressor gene, Pin2 telomeric repeat factor 1-interacting telomerase inhibitor 1 (PinX1) inhibits cell proliferation, migration, and invasion by regulating p53/miR-200b-mediated transcriptional inhibition of Snail1, Twist1, and Zeb1, thereby inhibiting EMT of CD133(+) cancer stem cells (CSCs) in NPC.102 Furthermore, Zhao et al.103 found that cisplatin treatment can induce the upregulation of miR-125a and miR-125b expression, and these miRNAs can target p53 mRNA and reduce p53 protein-induced apoptosis, which may be one of the causes of cisplatin resistance in NPC cells.
For the p53 pathway, targeted inhibition of MDM2, COX-2, MYH9, Bmi-1, miR-125a, and miR-125b may become potential therapeutic strategies in NPC.
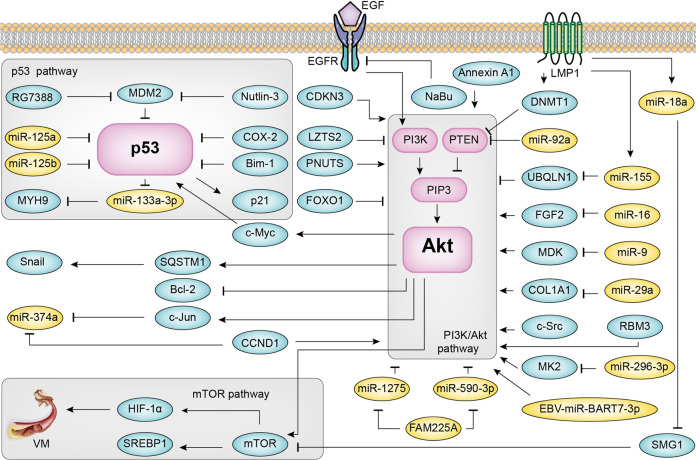
A summary of the PI3K/Akt signal pathway, p53 signal pathway, and mTOR signal pathway in NPC is shown in Fig. 1.
Fig. 1.
PI3K/Akt signal pathway, p53 signal pathway, and mTOR signal pathway in NPC. LMP1 latent membrane protein 1, LMP2A latent membrane protein 2A, PIP2 phosphatidylinositol 4,5-bisphosphate, PIP3 phosphatidylinositol 3,4,5-trisphosphate, PTEN phosphatase, and tensin homolog, PI3K phosphoinositide 3-kinase, DNMT1 DNA methyltransferase 1, SREBP1 sterol regulatory element-binding protein 1, VM vasculogenic mimicry, NaBu sodium butyrate, MK2 mitogen-activated protein kinase-activated protein kinase 2, CCND1 cyclin D1, MYH9 myosin heavy chain 9, ITGB3 integrin β3, MDK midkine, FGF2 fibroblast growth factor 2, COL1A1 collagen type I alpha 1, RBM3 RNA-binding motif protein 3, PNUTS phosphatase 1 nuclear-targeting subunit, CDKN3 cyclin-dependent kinase inhibitor 3, SQSTM1 Sequestosome-1, LZTS2 leucine zipper tumor suppressor 2, UBQLN1 ubiquilin1, SMG1 suppressor of morphogenesis in genitalia 1, MDM2 murine double minute 2, COX-2 cycloxygenase-2, Bmi-1 B-cell-specific Moloney murine leukemia virus insertion site 1, EMT epithelial–mesenchymal transformation. Among them, LMP1, mTOR, PI3K, HIF-1α, miR-92a, Annexin A1, CDKN3, OCT4, c-Src, and COX-2 can be used as prognostic markers of NPC. The preclinical studies of NPC show that HIF-1α, COX-2 has a good research value in targeted therapy. EGFR inhibitor, VEGF inhibitor, VEGFR inhibitor, and Akt inhibitor show positive effects and have less and tolerable adverse reactions in phase II clinical trials of NPC
NF-κB pathway
NF-κB is a key multipotent dimer transcription factor.104 Studies have shown that the activation of the NF-κB pathway is closely related to persistent infection of EBV, the formation of immortal nasopharyngeal epithelial cells and immunosuppressive environment, cancer stem cells generation, and metabolic reprogramming.105 Through the WES, several NF-κB signaling negative regulators NFKBIA, CYLD, and TNFAIP3 were found multiple loss-of-function mutations. The loss-of-function mutations in NFKBIA lead to protein truncation and result in the altered NF-κB activity, which contributes to NPC tumorigenesis.26
LMP1 is believed to activate the NF-κB signal pathway.106 In EBV-associated NPC cells, LMP1-activated NF-κB binds to the promoter region of the miR-203 gene and inhibits miR-203 expression, Cadherin 6 (CDH6) as a direct target of miR-203 upregulates in turn induced EMT and promotes metastasis. Furthermore, EBV-negative NPC cells can induce the EMT potential through the uptake of exo-LMP1.107 The NF-κB inhibitor aspirin can reverse EMT, reduce the release of exo-LMP1, promote the expression of miR-203, and inhibit the metastasis of NPC cells in nude mice.108 Provirus integration site for Moloney murine leukemia virus 1 (Pim1) is a serine/threonine kinase. LMP1-activated NF-κB signal pathway can promote the expression of downstream Pim1, thus promoting cell proliferation. Quercetagetin, an inhibitor of Pim1, can significantly inhibit the proliferation activity of NPC cells that express LMP1.109
In the view of the key role of inhibitor of NF-κB kinase (IKK) in the activation of the NF-κB pathway, IKK inhibitor is considered as one of the strategies of targeted therapy for cancer.110 The natural flavonoid glycoside vitexin can inhibit the activity of IKK thereby inhibiting the activation of the NF-κB signal pathway and inducing NPC cell apoptosis.111 BST2, also known as CD317 or HM1.24, is found to be highly expressed in cisplatin-resistant NPC cells. It can activate the NF-κB signal pathway and increase the expression of downstream anti-apoptotic proteins. BST2 overexpression is associated with a low survival rate in patients with NPC. Therefore, BST2 could be used as a prognostic marker and therapeutic target for NPC.112
Decreased expression of various components that inhibit the NF-κB pathway in NPC cells is one of the reasons for the abnormal activation of the NF-κB pathway. SIRT6, a kind of deacetylase, is downregulated in NPC cells. Lei et al. found that overexpression of SIRT6 might inhibit the expression of NF-κB by means other than acetylation and promoted apoptosis of NPC cells.113 In addition, knockout of NEAT1, a cancer-related long non-coding RNA, can inhibit the proliferation of NPC cells and promote apoptosis via promoting the activity of the miR-124/NF-κB axis.114 Deleted in liver cancer-1 (DLC-1) is a member of the GTPase-activating protein (GAP) family that is able to inhibit multiple tumor processes.115 Huang et al.116 demonstrated that DLC-1 could induce mitochondrial apoptosis and inhibit EMT and related processes by inhibiting the activation of the EGFR/Akt/NF-κB axis. Tumor necrosis factor-alpha-induced protein 3 (TNFAIP3), which has the function of the ubiquitin-editing enzyme, can inhibit the upstream signal transduction of the NF-κB signal pathway.117 Relative studies have shown that miR-19b-3p and miR-125b can directly suppress TNFAIP3 expression, thereby activating the NF-κB signal pathway, promote the proliferation of NPC cells, and inhibit the apoptosis of NPC cells.118,119 Ras-like estrogen-regulated growth inhibitor (RERG) is regarded as a potential tumor suppressor gene, expressed in a variety of normal tissues.120,121 Zhao et al. found that RERG was silenced by DNA hypermethylation in NPC cells. The extracellular-signal-regulated kinases (ERK)/NF-κB pathway is suppressed after RERG demethylation activation, which results in downregulating the expression of MMPs and pro-angiogenic cytokines, reducing the proliferation, migration, invasion, colony formation, and angiogenesis of NPC cells.122 Being a key active subunit of the NF-κB pathway, p65 is closely involved in the deregulation of the NF-κB pathway.123 Li et al.124 found that Epigallocatechin-3-gallate (EGCG) could inhibit NF-κB p65 activity, thus suppressing cancer progression, which is relevant to CSCs and EMT.
The NF-κB pathway can also be combined with immunotherapy. Huang et al.125 found that treating drug-resistant NPC cells with sunitinib could promote the expression of nature killer group 2 member D ligands (NKG2DLs) on the cell membrane by activating the NF-κB signal pathway, thereby enhancing NK cell-mediated cytotoxicity.
To sum up, the targeted inhibition of p65, LMP1, IKK, CDH6, Pim1, BST2, NEAT1, and the targeted activation of SIRT6, DLC-1, TNFAIP3, RERG, NKG2DLs in the targeted therapy of NPC could be a potential therapeutic strategy through the NF-κB pathway.
MAPK pathway
MAPK is a member of the serine/threonine kinases family. There are three main subfamilies of MAPK: the ERK, the c-Jun N-terminal (JNK) or stress-activated protein kinases (SAPK), and MAPK14 (P38-α).126 The cascade activation of MAPK is an important pathway for the survival, proliferation, and drug resistance of cancer cells.127 In the MAPK pathway, recurrent mutations of its activators or regulators (FGFR2, FGFR3, BRAF1, NF1, and ERBB3) were detected in NPC samples.25 Hotspot mutations of KRAS, HRAS, and NRAS genes, promoter hypermethylation of RASAL, and DAB2 genes are also found.29,128
As an upstream kinase of the p38/MAPK pathway, the overexpression of mitogen-activated protein kinase kinase 6 (MAP2K6) is related to the radioresistance and poor prognosis of patients with NPC.129 In the MAPK/ERK pathway, PAK1 can phosphorylate Raf1 at Ser338 and MEK1 at Ser298, thereby activating the MAPK pathway.130,131 Franck et al. found that the macrocyclic lactone antibiotic ivermectin (IVM) could act as a PAK1 inhibitor to block the phosphorylation process of Raf1 and MEK1, resulting in cytotoxicity to NPC cells.132 After the MAPK pathway activation, it can phosphorylate and activate MAP kinase interacting serine-threonine kinase 1 (MNK1) which has been proved to be overexpressed in many kinds of cancers.133,134 Zhang et al.135 designed an MNK1 inhibitor compound 12dj that could inhibit the phosphorylation of downstream eukaryotic initiation factor 4E (eIF4E), thus producing cytotoxicity against NPC cells which is possibly related to the apoptotic cell death subroutine. BLU, a tumor suppressor gene, is found to disrupt cell cycle progression and result in the suppression of tumor growth, which is related to downregulated ERK signaling and the corresponding downstream effector cyclins D1 and B1.136
MiR-483-5p directly decreases death-associated protein kinase 1 (DAPK1) protein expression, increases colony formation of NPC cells, reduces radiation-induced apoptosis and DNA damage, via activating the ERK signal pathway.137 On the contrary, miR-124 can inhibit the occurrence of NPC through the MALAT1/ERK/MAPK axis.138 In addition, Peng et al.139 found that the suppression of proliferation, invasion, and metastasis of NPC by miR-124 is achieved by regulation of Homo sapiens forkhead box Q1 (Foxq1). Peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (PIN1), as an important signal regulator, is associated with EBV infection.140 Xu et al.141 found that PIN1 was overexpressed in EBV-associated NPC cells and PIN1 inhibitors Juglone could eliminate the PIN1 effect of activating the MAPK/JNK pathway, reducing the downstream protein cyclin D1 expression and enhancing the activity of caspase 3, finally inhibiting proliferation. PDZ binding kinase (PBK) is a kind of MAPK kinase (MAPKK) that is able to participate in many cellular functions through phosphorylating P38, JNK, and ERK.142–144 Wang et al.145 applied the PBK inhibitor HI-TOPK-032 to NPC cells and found that inhibiting PBK induced the oxidative stress by activating JNK/P38 signals, resulting in the accumulation of reactive oxygen species (ROS) and cell apoptosis.
To sum up, the targeted inhibition of MAP2K6, PAK1, MNK1, FGF2, PIN1, PBK, and the targeted activation of DAPK1, BLU, miR-124 in the targeted therapy of NPC could be a potential therapeutic strategy through the MAPK pathway.
STAT3 pathway
Signal transducer and activator of transcription 3 (STAT3), a transcription factor encoded by the STAT3 gene, is a member of the STAT protein family.146 STAT3 is phosphorylated by Janus kinase (JAK) to have the role of activator of transcription and mediate a series of signal cascade reactions.
In vivo, miRNA is involved in the regulation of the STAT3 pathway. Recently a study showed that miR-29a can inhibit the 3′-UTR of STAT3 mRNA, reduce the level of STAT3, phosphorylated STAT3 and Bcl-2, inhibit cell proliferation, and enhance the level of apoptosis and drug sensitivity.147 Li et al.148 found that sulforaphane can upregulate the level of miR-124-3p in NPC cells, inhibit the 3′-UTR of STAT3 mRNA, enhance cell apoptosis, and inhibit cell proliferation. In addition, miR-124-3p was found to be upregulated in UCA1 gene knockout NPC cells and inhibition of the proliferation, invasion, and migration of NPC cells by miR-124-3p was achieved by inhibiting the expression of integrin β1 (ITGB1).149
EBV has previously been proposed to be particularly relevant to the onset of NPC. A quintessential example should be cited that is LMP1, which may contribute to the development of NPC through the STAT3 signal pathway. Ding et al.109 revealed that LMP1 can promote the activation of STAT3, protein kinase C (PKC), NF-κB, and AP1 in EBV-associated NPC cell NPC cells, thus activating Pim1 and promoting the proliferation of NPC cells.
He et al.150 showed that the downregulation of Raf kinase inhibitory protein (RKIP) can activate the signal transduction of the STAT3 pathway, enhance the migration and invasion ability of NPC cells in vitro, besides it can also enhance the metastasis and EMT in vivo. Furthermore, Huang et al.151 found that miR-181a can enhance radioresistance by inhibiting RKIP.
Eph receptors, a member of the receptor tyrosine kinase family (RTKs), participate in the regulation of the STAT3 signal pathway. Eph2 is often overexpressed in human malignant tumors, accompanied by the absence of Ephrin-A1, which can promote tumor invasion and metastasis, induce EMT, and maintain the cancer stem cell characteristics.152
JAK also has an essential role in the regulation of the STAT3 signal pathway. It is reported that IL-6 can activate lncRNA DANCR through the STAT3 pathway, forming a positive feedback loop, enhancing the invasion and proliferation ability of NPC cells in vitro.153 Liu et al.154 indicated that ovatodiolide could significantly inhibit the JAK2/STAT3 signal pathway, upregulate the level of Bax and Slug and decrease the level of Bcl-xL, c-Myc, and cyclin D1, which significantly reduces the cancer stem cell characteristics of NPC cells together with survival, proliferation, invasion, migration, and EMT inhibited, and promote the apoptosis of NPC cells.
For STAT3 pathways, except for directly targeting STAT3 for NPC treatment, targeted inhibition of LMP1, AP1, LncRNA DANCR, and targeted activation of miR-29a, miR-124-3p, and RKIP may become potential treatment strategies for NPC.
Wnt/β-catenin pathway
Wnt/β-catenin signal pathway disorder is closely related to the occurrence and development of cancers.155 As a class of secreted glycoproteins, Wnt can bind to the receptors on the cell membrane and regulate the content of β-catenin in cells. β-catenin combines with T cell factor (TCF)/lymphoid enhancing factor (LEF) family in the nucleus, regulating the expression of the downstream genes.156 The promoter region of Wnt inhibitory factor 1 and SOX1 have been reported to be frequently hypermethylated in NPC which is in connection with the Wnt/β-catenin pathway activation.157,158
β-catenin is a key molecule in the Wnt/β-catenin signal pathway.159 Li et al.160 found that β-catenin could promote the expression of manganese superoxide dismutase (MnSOD), thereby reducing the level of ROS and increasing the resistance of anoikis in NPC cells. A small nuclear protein Chibby is able to inhibit β-catenin transcriptional activation through binding to its carboxyl terminus and decrease β-catenin content in the nucleus by cooperating with 14-3-3 adaptor proteins to transport it out of the nucleus, thereby inhibiting cell proliferation.161 MiR-34c directly suppresses β-catenin expression, thereby inhibiting proliferation, EMT, and radioresistance of NPC cells.162 Calpain small subunit 1 (Capn4), a small regulatory subunit of the Calpain family, has been shown to be highly expressed in a variety of cancers.163–165 MiR-124 can target Capn4 and then suppress the expression of β-catenin, cyclin D1, and c-Myc, leading to the inhibition of proliferation, invasion, and migration of NPC cells.166
Glycogen synthase kinase 3β (GSK3β), adenomatosis polyposis coli (APC), Axin and casein kinase Iα (CKIα) forms degradation complex to combine with β-catenin. GSK3β phosphorylates the Ser/Thr residues at the N-terminal of β-catenin, leading to the degradation of β-catenin.167 Huang et al.168 found that miR‑150 directly inhibited GSK3β expression at the protein level, resulting in the abnormal accumulation of β-catenin, leading to radiotherapy resistance of NPC cells. CREB binding protein (CBP), which co-activates and acetylates β-catenin with a promoter-specific pattern, is highly expressed in NPC cells.169,170 A small-molecule Wnt modulator ICG-001 can bind to CBP, thereby suppressing Wnt/β-catenin signal pathway and resulting in the reduction of the CSC population.171 MiR-506 could inhibit tumor growth and metastasis in NPC by downregulating LIM Homeobox 2 (LHX2), through the inactivation of the Wnt/β-catenin pathway.172 Furthermore, Forkhead box O3a (FOXO3a) silencing could induce radioresistance and EMT in NPC cells through activation of the Wnt/β-catenin pathway.173
To sum up, the targeted inhibition of β-catenin, Capn4, CBP, LHX2, FOXO3a, and the targeted activation of GSK3β in the targeted therapy of NPC could be a potential therapeutic strategy through the Wnt/β-catenin pathway.
EGFR pathway
EGFR, also known as HER1 or ErbB1, is the first member that has been discovered in the ErbB family of tyrosine kinase receptor, which can bind with EGF, transforming growth factor-alpha (TGF-α), amphiregulin (AR), heparin-binding EGF-like growth factor (HB-EGF), and betacellulin (BTC); thus, signal cascade reaction and gene transcription are initiated in the cell. Downstream signal cascades of EGFR including RAS/RAF/MEK/MAPK/ERK, PI3K/Akt, PKC, Src, and JAK/STAT pathways, are crucial for cell proliferation, angiogenesis, apoptosis inhibition, cell motility, metastasis, adhesion, and gene expression.174
EGFR overexpression is common in NPC cells. Gu et al.175 found that the combination treatment of cetuximab and cisplatin for NPC cells can downregulate the levels of EGFR, phosphorylated EGFR, and phosphorylated Akt, upregulate the levels of Bax and caspase 3, and inhibit cell growth by increasing cisplatin-induced apoptosis, which indicated that the activation of EGFR/Akt pathway in NPC cells can inhibit the level of apoptosis, causing cisplatin resistance. In addition, serine protease inhibitor Kazal-type 6 (SPINK6) can promote cancer metastasis by binding and activating EGFR in NPC.176
In the treatment of NPC, targeted therapy for EGFR is still rarely approved for clinical use. It has been found that the progression-free survival (PFS) and overall survival (OS) of patients administered with nimotuzumab (NTZ) and intensity-modulated radiotherapy (IMRT) were significantly prolonged comparing with patients without adjuvant chemotherapy, and patients treated with cetuximab (CTX) and concurrent chemoradiotherapy (CCRT) had a significant improvement in OS, PFS and distant metastasis-free survival comparing with patients without cetuximab, but there is no significant difference in OS between anti-EGFR therapy using CTX/NTZ combined with palliative chemotherapy (PCT) and single PCT treatment.177–180
For EGFR pathways, apart from directly targeting EGFR for NPC treatment, targeting DLC-1, as well as a combination of EGFR targeting inhibitors with chemoradiotherapy may be potential therapeutic strategies for NPC.
VEGF pathway
Notably, VEGF not only has an important role in leukemia and lymphoma but also is highly expressed in various solid malignant tumors, which is involved in the progress of malignant tumor diseases. The overexpression of VEGF in tumor tissue is closely related to the increase in angiogenesis, proliferation, and metastasis.181 Neuropilin-1 (NRP-1) is a VEGF receptor, which is co-expressed with VEGF in many tumor cells. It has been reported that NRP-1 can promote tumor growth.182 Using shRNA silencing NRP-1, Sun et al.183 discovered a vital inhibitory effect on the proliferation of CNE-2Z cells in vitro. Fu et al.184 found that lncRNA HOX transcript antisense intergenic RNA (Hotair) was significantly upregulated in NPC cells and clinical specimens, which can directly enhance the VEGF transcription activity, or indirectly enhance the VEGFA transcription activity and angiopoietin 2 (Ang2) activity through GRP78, mediating angiogenesis and tumor growth in NPC. Contrarily, miR-495 can directly target the 3′-UTR of GRP78, leading to the radiosensitivity of NPC.185
However, in the practical application, the clinical effect of conventional methods is limited as a result of the severe side effects. Li et al.186 studied the combination of bevacizumab and radiotherapy and chemotherapy and found that this combination treatment had a higher disease relief rate and a lower incidence of side effects, which can be used for further clinical experimental research.
Endoplasmic reticulum stress
Endoplasmic reticulum (ER) is directly linked to the synthesis and folding of membrane and secretory proteins. When cells suffer from physiological stress and pathological stress, the balance between demand for protein folding and ER processing ability can be broken, thus ER stress occurs. In the occurrence of ER stress, a series of signal transduction pathways in cells will be activated, which are collectively referred to as unfolded protein response (UPR).187
ER stress is involved in the treatment of tumors. Different chemotherapy drugs can have different effects through the UPR signal pathway, as for etoposide, activation of the UPR signal pathway can increase the cell resistance,188 while it may enhance cisplatin sensitivity and induce apoptosis.189
It was also reported that the combination treatment of lenvatinib and iodine-131 increased the expression of ATF-6, IER1 RERK, CHOP, JNK, p38, and caspase 3 in NPC cells, indicating that the treatment-induced apoptosis of NPC cells by upregulating ER stress.190 Recently, Pan et al. found that the use of a curcumin compound (B63) can promote cell apoptosis, inhibit cell proliferation, and arrest the cell at the G2/M stage. The level of CHOP, ATF-4, and XBP-1 protein was significantly upregulated, suggesting that the activation of ER stress pathway may have a significant role in the anti-tumor effect of B63.191 Lin et al.192 revealed that Tetrandrine (TET) treatment of NPC cells increased apoptosis, upregulated the expression level of calpain 1, calpain 2, caspase 12, IRE-1α, IRE-1 β, GADD153, Glucose-regulated protein 78 (GRP78), ATF-6α, and ATF-6, indicating that TET induced cell apoptosis through ER stress.
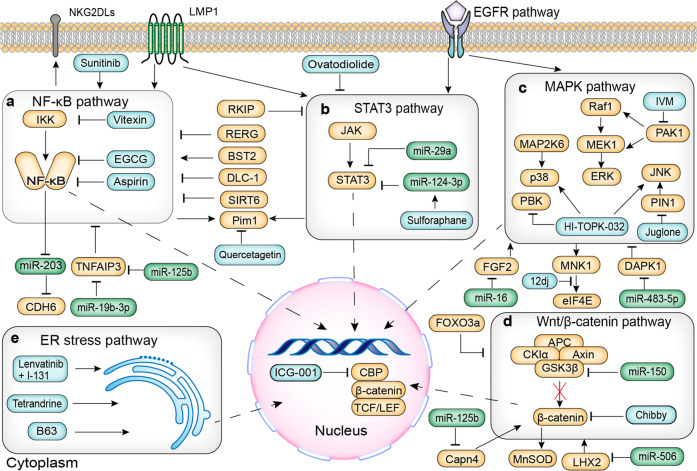
Signal pathways in NPC, including the NF-κB pathway, MAPK pathway, STAT3 pathway, Wnt/β-catenin pathway and ER stress pathway can regulate their downstream genes’ expression, thereby influencing the biological behaviors of NPC cells. In each pathway, some potential targets and corresponding drugs mentioned in this review are shown in Fig. 2.
Fig. 2.
NF-κB pathway, MAPK pathway, STAT3 pathway, Wnt/β-catenin pathway, and ER stress pathway in NPC. a NF-κB pathway. b The STAT3 pathway. c MAPK pathway. d Wnt/β-catenin pathway. e ER stress pathway. The orange rounded rectangles indicate target molecules. The green rounded rectangles indicate microRNAs. The blue rounded rectangles indicate potential drugs. NF-κB nuclear factor kappa B, IKK inhibitor of NF-κB kinase, EGCG epigallocatechin-3-gallate, CDH6 cadherin 6, TNFAIP3 tumor necrosis factor-alpha-induced protein 3, RERG Ras-like estrogen-regulated growth inhibitor, DLC-1 deleted in liver cancer-1, Pim1 provirus integration site for Moloney murine leukemia virus 1, NKG2DLs nature killer group 2 member D ligands, STAT3 signal transducer and activator of transcription 3, JAK Janus kinase, RKIP Raf kinase inhibitory protein, EGFR epidermal growth factor receptor, LMP1 latent membrane protein 1, MAPK mitogen-activated protein kinase, PAK1 p21-activated kinase 1, IVM ivermectin, ERK extracellular-signal-regulated kinases, JNK c-Jun N-terminal kinases, MAP2K6 mitogen-activated protein kinase kinase 6, PBK PDZ binding kinase, PIN1 peptidyl-prolyl cis-trans isomerase NIMA-interacting 1, MNK1 MAP kinase interacting serine/threonine kinase 1, eIF4E eukaryotic initiation factor 4E, FGF2 fiber cell growth factor 2, DAPK1 death-associated protein kinase 1, TCF T cell factor, LEF lymphoid enhancing factor, CBP CREB binding protein, GSK3β glycogen synthase kinase 3β, APC adenomatosis polyposis coli, CKIα casein kinase Iα, MnSOD manganese superoxide dismutase, LHX2 LIM Homeobox 2, FOXO3a Forkhead box O3a, Capn4 Calpain small subunit 1, ER endoplasmic reticulum
Some other signal pathways related to the targeted therapy of NPC
Zhao et al.193 found that the Notch signal pathway may have a new function of conferring radioresistance on CNE-1 and CNE-2 cells, which is mediated by miR-20a-5p and neuronal PAS domain protein 2 (NPAS2). MiR-20a-5p can promote the invasion, metastasis, and radioresistance of NPC cells by inhibiting GTPases Rab27B, an important role in the development and metastasis of tumors.194,195 As a suppressor and promoter in various tumors, TGF-β not only has inhibitive roles in tumorigenesis but also induces EMT and tumor migration.196 The expression of E-cadherin, N-cadherin, twist, and snail can be regulated by the TGF-β pathway activated by annexin A2, which mediates the EMT process of NPC TW01 cells.197 Wang et al.198 found that berberine can reduce the activation of the TGF-β signal pathway induced by specificity protein 1 (Sp1) in CNE-2 cells, thus enhancing radiosensitivity. Nicotine negatively regulates miR-296-3p which directly targets the Ras/Braf/Erk/Mek/c-Myc pathway mediated by oncogenic protein MK2, promoting cytoplasmic transposition of c-Myc and the chemotherapy resistance, cell cycle progression, and EMT process of NPC.68 HIF-1 signal pathway is mainly regulated by the stability and activity of HIF-1α, and the overexpression of HIF-1α can lead to poor prognosis of NPC.199 Chen et al.200 constructed a kind of nanoparticle that can load HIF-1α siRNA, which has an inhibitive effect on tumor growth in CNE-2 tumor models. AMPK/mTOR/HIF-1 pathway can regulate the angiogenesis and glycolysis of NPC, and the microRNA-BART1-5P encoded by EBV acts on the α1 catalytic subunit of AMPK to regulate tumor metabolism and angiogenesis.201 The aberrant regulation of store-operated Ca2+ entry (SOCE) is highly associated with the process of NPC. The Ca2+ channel blocker skf96365 can inhibit the colony formation and increase the cell death rate by interfering with the Ca2+ signal induced by EGF, and induce the apoptosis and cell cycle arrest of G2/M and S-phase in CNE-2 and HONE-1 cells through caspase pathway.202 NaBu can promote SOCE in 5-8F and 6-10B cells to increase Ca2+ inflow and induce apoptosis in NPC cells.203 In addition, the overexpression of WW domain-containing oxidoreductase (WWOX) gene can also promote apoptosis by accumulating the cleavage of Caspase 3.204
Non-coding RNA related to targeted therapy of NPC
Long non-coding RNA (lncRNA) and microRNA (miRNA) are highly associated with various tumors. In the past 5 years, the mechanism of lncRNA and miRNA in the progression, radioresistance, drug resistance, and angiogenesis of NPC has been studied.184,205–207 The role of lncRNAs and miRNAs in different NPC cell lines and the corresponding mechanisms have been, respectively, listed in Tables 1 and 2.
Table 1.
Potential long non-coding RNA targets and related molecular mechanisms in NPC
| LncRNA | Cell lines | Roles | Effects on NPC cells | Corresponding signal pathway | References |
|---|---|---|---|---|---|
| ANRIL | 5-8F, CNE-1, CNE-2 and HONE-1 | Oncogene |
↑Proliferation ↓Apoptosis ↓Radiosensitivity |
↑ANRIL/↓miR-125a | 205 |
| XIST | CNE-1, CNE-2 | Oncogene |
↑Proliferation ↓Radiosensitivity |
↑XIST/↓miR-29c | 206 |
| NEAT1 | HK-1, CNE-1, CNE-2 subclone S18 and SUNE-1 subclone 5-8F | Oncogene |
↑Proliferation ↑Cisplatin resistance |
↑NEAT1/↓let-7a-5p/↓RSF-1 Ras/MAPK signal pathway |
207 |
| Hotair | CNE-1, CNE-2 | Oncogene |
↑Proliferation ↑Angiogenesis |
↑Hotair/↑VEGFA or ↑ GRP78/↑Ang2 | 184 |
| CASC2 | SUNE-1, SUNE-2, 6-10B | Tumor suppressor gene |
↓Proliferation ↑Apoptosis |
↓CASC2/↑miR-18a-5p/↓RBBP8 axis | 208 |
| CASC9 | CNE-1 | Oncogene |
↑Proliferation ↑Glycolysis Biomarker of poor prognosis |
HIF-1 signal pathway | 218 |
| FAM225A | CNE-1, CNE-2, HONE-1, SUNE-1, HNE-1, 5-8F, 6-10B, C666-1 and HK-1 | Oncogene |
↑Proliferation ↑Invasion |
miR-590-3p, miR-1275/↑ITGB3/FAK/PI3K/Akt pathway | 70 |
| UCA1 | 5-8F, CNE-2 | Oncogene |
Tumor promotor ↑Proliferation ↑Invasion ↑Migration |
↑UCA1/↓miR-145/↑ADAM 17 | 219 |
| LINC00460 | 5-8F | Oncogene |
↑Metastasis ↑Invasion ↑EMT |
↑LINC00460/↓miR-30a-3p/↑Rap1A | 220 |
| ANCR | CNE-1, CNE-2, SUNE-1, C666-1, HONE-1 and HNE-1 | Oncogene |
↑Proliferation ↑Radioresistance |
↑ANCR/↓PTEN | 226 |
| MALATA1 | 5-8F, CNE-2 | Oncogene |
↑Radioresistance ↑Activity of cancer stem cells |
MALAT1/miR-1/slug axis | 227 |
| PVT1 | 5-8F, CNE-2 | Oncogene |
↑Radioresistance ↓Apoptosis Biomarker of poor prognosis |
ATM–p53 pathway Caspase pathway |
228 |
“↑” means upregulation, “↓” means downregulation, EMT epithelial–mesenchymal transition, ANRIL CDKN2B antisense RNA 1, XIST X inactive-specific transcript, Rsf-1 remodeling and spacing factor 1, VEGFA vascular endothelial growth factor A, GRP78 glucose-regulated protein 78, Ang2 angiogenin 2, CASC2 cancer susceptibility candidate 2, RBBP8 retinoblastoma binding protein 8, HIF-1 hypoxia induced factor 1, ITGB3 integrin β3, UCA1 urothelial carcinoma-associated 1, Rap1A Ras-related protein 1A, ANCR, antidifferentiation non-coding RNA, PTEN phosphatase and tensin homolog, MALAT1 metastasis-associated lung adenocarcinoma transcript 1
Table 2.
Functions and mechanism of miRNAs in NPC cells
| MiRNA | Cell lines | Roles | Functions | Mechanism | References |
|---|---|---|---|---|---|
| miR-26b | CNE-2, HNE-1 | Tumor suppressor gene | ↑Cisplatin sensitivity | FOXD3/↑miR-26b /↓JAG1 | 225 |
| miR-7 | CNE-1, CNE-2 | Tumor suppressor gene | ↓Proliferation, ↓invasion | miR-7/↓Skp2/p57↑ | 210 |
| miR-16 | CNE-1, CNE-2 | Tumor suppressor gene | ↓Proliferation, ↓invasion, ↓migration | miR-16/↓FGF2/↓PI3K/Akt pathway | 77 |
| miR-1 | 5-8F, CNE-2 | Tumor suppressor gene | ↑Radiosensitivity | MALAT1/↓miR-1/↑slug | 227 |
| miR-124 | 6-10B | Tumor suppressor gene | ↓Migration, ↓proliferation, ↓EMT |
miR-124/↓MALAT1/ERK/MAPK axis; NEAT1/↓miR-124/ NF-κB axis; miR-124/↓Capn4/↓ cyclin D1 and c-Myc; miR-124/↓Foxq1 |
138,139,114,167 |
| miR-148b | CNE-2, C666-1 | Tumor suppressor gene | ↓Proliferation, ↓migration, ↓invasion | miR-148b/↓MTA2 | 314 |
| miR-149 | 6‐10B, 5‐8F | Oncogene | ↑Proliferation, ↑invasion, ↑migration | miR-149/↓PKP3 | 222 |
| miR-150 | CNE-2, HONE-1 | Tumor suppressor gene | ↓Proliferation | miR-150/↓CDK2, CCND1, CCND2, CCNE2 | 215 |
| miR-181a | CNE-2-IR, CNE-2 | Oncogene | ↑Radioresistance | miR-181a/↓RKIP | 151 |
| miR-212 | 6-10B, CNE-2 | Tumor suppressor gene | ↓Metastasis, ↓invasion | miR-212/↓SOX4 | 211 |
| miR-324-3p | 5-8F | Tumor suppressor gene | ↓Proliferation, ↓Invasion, ↓metastasis | miR-324-3p /↓GLI3 | 209 |
| miR-504 | CNE-2-IR, HK-1-IR | Oncogene | ↑Radioresistance | miR-504/↓NRF1 | 231 |
| miR‑18a‑5p | NPC cells | Oncogene | ↑Proliferation | ↓CASC2/↑miR-18a-5p/↓RBBP8 | 208 |
| miR‑495 | 5-8F, 5-8F-IR | Tumor suppressor gene | ↑Radiosensitivity | miR-495/↓GRP78 | 185 |
| miR-138-5p | HONE-1, HK-1 | Tumor suppressor gene | ↑Radiosensitivity | miR-138-5p /↓EIF4EBP1/ ↑eIF4E | 229 |
| miR-29a |
CNE-2R, CNE-2, |
Tumor suppressor gene | ↑Radiosensitivity | miR-29a-3p /↓COL1A1 | 79 |
| miR-20a-5p | CNE-1, CNE-2 | Oncogene | ↑Radioresistance, ↑migration, ↑invasion | miR-20a-5p /↓Rab27B | 195 |
| miR-29c | HNE-1, CNE-2 | Tumor suppressor gene | ↓Proliferation | miR-29c/↓HBP1/↓cyclin D1 | 216 |
| miR-19b-3p | CNE-1, CNE-2 | Oncogene | ↑Radioresistance | miR-19b-3p /↓TNFAIP3/NF-κB axis | 118 |
| miR-142-3p |
CNE-2, SUNE-1 |
Tumor suppressor gene | ↓Metastasis | miR-142-3p /↓ZEB2 | 63 |
| miR-124-3p |
SUNE-1, C666-1 |
Tumor suppressor gene | ↓Proliferation, ↓migration, ↓invasion | miR-124-3p /↓ITGB1 | 149 |
| miR-152 | CNE-2 | Tumor suppressor gene | ↓Invasion, ↓migration | miR-152/↓DNMT1 | 62 |
| miR-101 | CNE-2, 5-8F | Tumor suppressor gene | ↓Metastasis, ↓invasion, ↓angiogenesis | miR-101/↓ITGA3 | 214 |
| miR-483-5p | CNE-1, 5-8F | Oncogene | ↑Radioresistance | miR-483-5p /↓DAPK1 | 137 |
| miR-432 | CNE-2, 5-8F | Tumor suppressor gene | ↓Invasion, ↓metastasis | miR-432/↓E2F3 | 212 |
| miR-185-3p, miR-324-3p | CNE-2 | Tumor suppressor gene | ↓Proliferation | miR-185-3p, miR-324-3p /↓SMAD7 | 217 |
| miR-92a | 5-8F, 6-10B | Oncogene | ↑Metastasis, ↑invasion | miR-92a/↓PTEN/Akt pathway | 74 |
| miR-506 | CNE-2, 5-8F | Tumor suppressor gene | ↓Proliferation, ↓migration, ↓invasion | miR-506/↓LHX2/↓TCF4, ↓Wnt/β-catenin pathway | 172 |
| miR-378 | 5-8F, 6-10B | Oncogene | ↑Proliferation, ↑migration, ↑invasion | miR-378/↓TOB2 | 315 |
| miR-9 | 5-8F, CNE-1 | Tumor suppressor gene | ↓Angiogenesis | miR-9/↓MDK/↓PDK/Akt pathway | 72 |
“↑” means promoting, “↓” means inhibiting, JAG1 Jagged1, Skp2 S-phase kinase-associated protein 2, FGF2 fibroblast growth factor 2, MALAT1 metastasis-associated with lung adenocarcinoma transcript 1, MTA2 metastasis-associated gene 2, PKP3 Plakophilin3, CCND1 cyclin D1, CCND2 cyclin D2, CDK2 cyclin-dependent kinase 2, CCNE2 cyclin E2, RKIP Raf kinase inhibitory protein, SOX4 SRY-box transcription factor 4, GLI3 Homo sapiens GLI family zinc-finger 3, NRF1 nuclear respiratory factor 1, RBBP8 RB binding protein 8, GRP78 glucose-regulated protein 78, EIF4EBP1 eukaryotic initiation factor 4E binding protein 1, eIF4E eukaryotic initiation factor 4E, COL1A1 collagen type I alpha 1 chain, Rab27B member RAS oncogene family, HBP1 HMG-box transcription factor 1, TNFAIP3 TNF alpha-induced protein 3, ZEB2 Zinc-finger E-box binding homeobox 2, ITGB1 integrin beta-1, DNMT1 DNA methyltransferase 1, ITGA3 integrin subunit alpha 3, DAPK1 death-associated protein kinase 1, E2F3 E2F transcription factor 3, SMAD7 SMAD family member 7, PTEN Phosphatase and tensin homolog, LHX2 LIM Homeobox 2, TCF4 transcription factor 4, TOB2 transducer of ERBB2
The anti-cancer effect
Recent studies have found that some microRNAs and lncRNAs in tumor tissues are downregulated and show negative regulation of pathological activities of NPC.
lncRNA cancer susceptibility candidate 2 (CASC2) could inhibit proliferation, induce apoptosis through inhibiting the activation of miR-18a-5p/RB binding protein 8 (RBBP8) axis.208
MiR-324-3p can inhibit the invasion of tumor cells through its suppression of Homo sapiens GLI family zinc-finger 3 (GLI3) gene expression.209 High expressions of miR-7 inhibit the proliferation and invasion of NPC cells by downregulating the expression of S-phase kinase-associated protein 2 (Skp2) which reduces the ubiquitination degradation of its targets such as p21, p57, and E-cadherin.210 MiR-212 directly targets and inhibits the expression of SOX4, a transcription factor at its downstream target, thus inhibiting the migration and invasion of NPC cells.211 In addition, miR-432 inhibits the expression of E2F transcription factor 3 (E2F3) by binding to the 3′-UTR of E2F3, leading the inhibition of the invasion and migration of NPC cells.212 MiR-148b inhibits proliferation, invasion, and metastasis of NPC cells by inhibiting metastasis-related gene 2 (MTA2).213
MiR-101 suppresses the level of integrin subunit alpha 3 (ITGA3), leading to inhibition of metastasis and angiogenesis of the tumor.214 MiR-150 was found to block cell cycle and inhibit the proliferation of NPC cells by inhibiting the expression of cyclin-related genes such as CCND1, cyclin D2 (CCND2), cyclin-dependent kinase 2 (CDK2), and cyclin E2 (CCNE2).215 Arresting cell at G1/S-phase and inhibiting the proliferation of NPC cells by miR-29c can be achieved by reduction of the transcription factor HMG-box transcription factor 1 (HBP1), causing the downregulation of cyclin D1 and cyclin D3.216
MiR-185-3p and miR-324-3p regulate the growth and apoptosis of NPC, which can be partially achieved by targeting the 3′-UTR of SMAD7.217
Promotion of cancer
Conversely, some miRNAs and lncRNAs are upregulated in cancer tissues and facilitate pathological activities related to NPC, including inhibition of apoptosis, promotion of tumor cell proliferation, invasion, and metastasis.
LncRNA ANRIL, the expression of which is upregulated in NPC tissues compared to the normal nasopharyngeal epithelium, could promote proliferation and inhibit apoptosis in NPC via sponging miR-125a.205 As a member of the CASC family, lncRNA CASC9 could activate HIF-1α, thus facilitating the tumorigenesis and glycolysis of NPC cells.218 The expression of oncogene ADAM 17 could be increased after lncRNA urothelial carcinoma-associated 1 (UCA1) sponges miR-145 and UCA1 in NPC is regarded as a tumor promoter.219 LINC00460 is highly associated with the EMT in NPC cells via binding miR-30a-3p to regulate the expression of Ras-related protein 1A (Rap1A).220 What’s more, patients whose infiltrating lymphocytes are characterized by high expression of lncRNA AFAP1-AS1 incline to distant metastasis and poor prognosis, especially with positive PD1.221 N,N′‐dinitrosopiperazine (DNP) can promote proliferation, invasion, and metastasis of NPC by enhancing the expression of miR-149 which suppresses the level of PKP3.222 It is mostly believed that RBBP8 is involved in the repair of DNA double-strand breaks in cancer.223
Drug resistance
Combined chemotherapy is one of the main methods to treat patients with NPC, but in recent years, it has been found that the therapeutic effects of anti-cancer drugs are not satisfactory, the main reason for which is that NPC cells have developed resistance to anti-cancer drugs.
Triptonide, as a molecule monomer extracted from Chinese herbal medicine, can interfere with the lnc-THOR-IGF2BP1 signal and inhibit the proliferation of NPC cells in vitro and in vivo.224 Forkhead box protein D3 (FOXD3) can promote the expression of miR-26b, which inhibits the JAG1/Notch axis, inducing the sensitivity of NPC cells to cisplatin (CDDP).225
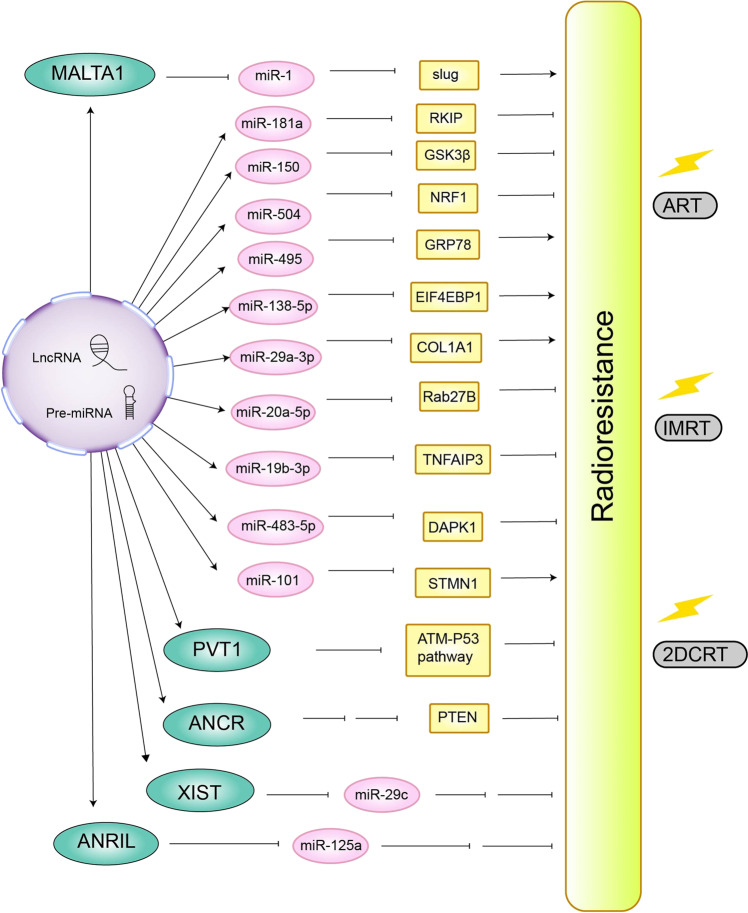
Radioresistance
The radioresistance of NPC is one of the main reasons for the low efficacy of radiotherapy. It is widely believed that some miRNAs are upregulated or downregulated in radiation-resistant NPC cells and can reduce or enhance the sensitivity of tumor cells to radiation. How non-coding RNAs induce or inhibit the radioresistance of NPC has been shown in Fig. 3.
Fig. 3.
Mechanism of non-coding RNA on radioresistance of NPC. JAG1 Jagged1, Skp2 S-phase kinase-associated protein 2, FGF2 fibroblast growth factor 2, MALAT1 metastasis-associated with lung adenocarcinoma transcript 1, MTA2 metastasis-associated gene 2, PKP3 Plakophilin3, CCND1 cyclin D1, CCND2 cyclin D2, CDK2 cyclin-dependent kinase 2, CCNE2 cyclin E2, RKIP Raf kinase inhibitory protein, SOX4 SRY-box transcription factor 4, GLI3 Homo sapiens GLI family zinc-finger 3, NRF1 nuclear respiratory factor 1, RBBP8 RB binding protein 8, GRP78 glucose-regulated protein 78, EIF4EBP1 eukaryotic initiation factor 4E binding protein 1, COL1A1 collagen type I alpha 1 chain, Rab27B member RAS oncogene family, HBP1 HMG-box transcription factor 1, TNFAIP3 TNF alpha-induced protein 3, ZEB2 zinc-finger E-box binding homeobox 2, ITGB1 integrin β1, DNMT1 DNA methyltransferase 1, ITGA3 integrin subunit alpha 3, DAPK1 death-associated protein kinase 1, E2F3 E2F transcription factor 3, SMAD7 SMAD family member 7, PTEN phosphatase and tensin homolog, ANRIL CDKN2B antisense RNA 1, XIST X inactive-specific transcript, ANCR antidifferentiation non-coding RNA, 2DCRT two-dimensional radiotherapy, IMRT intensity-modulated radiotherapy, ART adaptive radiotherapy
The knockdown of lncRNA X inactive-specific transcript (XIST) could upregulate miR-29c, resulting in the inhibition of DNA damage repair and an increase of the radiosensitivity of NPC cells.206 Antidifferentiation non-coding RNA (ANCR) could regulate PTEN expression epigenetically to promote radioresistance.226 Besides, lncRNA MALAT1 modulates cancer stem cell activity of NPC and induces radioresistance via regulating the miR-1/slug axis.227 LncRNA NEAT1 downregulates remodeling and spacing factor 1 (Rsf-1) expression to activate the Ras-MAPK pathway to mediate NPC resistance to cisplatin through direct interaction with let-7a-5p.114,207 Downregulated expression of lncRNA PVT1 can also induce apoptosis of NPC cells through the DNA damage repair pathway after radiotherapy, thus being regarded as a prognostic indicator.228
By reducing the level of eukaryotic initiation factor 4E binding protein 1 (EIF4EBP1), miR-138-5p increases eIF4E, enhancing the autophagy of NPC cells induced by radiotherapy.229 MiR-101 enhances radiation-induced autophagy and radiation sensitivity of tumor cells by targeting Stathmin 1 (STMN1).230 By inhibiting nuclear respiratory factor 1 (NRF1), miR-504 interferes with mitochondrial-mediated oxidation reaction and enhances radioresistance.231
Clinical significance
Clinical trials
Failure of NPC treatment mainly includes distant metastasis, recurrence, radiation resistance, and drug tolerance. Targeted therapy blocks signal transmission by targeting specific molecules related to tumor progression in and out of NPC cells, thus inhibiting the occurrence and development of NPC. At present, most of the clinical trials of targeted therapy against NPC are clinical phase I or II trials, which show that different targeted drugs can delay the process of NPC to different degrees and prolong the life of patients.
At present, clinical trials on targeted therapy for NPC are not abundant, which are mainly targeting EGFR and VEGF/VEGFR. Drugs that target EGFR include gefitinib, nimotuzumab, cetuximab, h-R3, and so on while drugs targeting VEGF/VEGFR mainly include axitinib, aflibercept, bevacizumab, sorafenib, sunitinib.
In phase II clinical trial, gefitinib is well-tolerated by subjects along with a poor response rate, making it less suitable for clinical treatment.232 In contrast, nimotuzumab in combination with 5-fluorouracil is significantly effective and well-tolerated by subjects in the treatment of recurrent and metastatic NPC.233 In stage N3 NPC, induction chemotherapy and sequential nimotuzumab plus CCRT achieved a positive survival benefit with tolerable toxicity.234 Compared with helical tomotherapy (HT) combined with cetuximab followed by adjuvant chemotherapy (ACT) with docetaxel, HT combined with cetuximab followed by ACT with cisplatin is an effective treatment for locally advanced disease (LANC), which has a high survival rate and few side effects.235 In a phase II trial, cetuximab-radiotherapy has better therapeutic effects but shows more acute adverse effects than cisplatin-chemoradiotherapy.236 h-R3 can enhance the radiosensitivity of locally advanced NPC with good safety, but the long-term efficacy is not effective.237
In patients with NPC, the use of bevacizumab can show a better effect compared with corticosteroids.238 Adding bevacizumab to chemoradiation is an effective and feasible treatment, suggesting that bevacizumab may delay the progression of subclinical disease.239 Axitinib has good control of disease progression and safety in patients with severe pre-treated NPC.240 Aflibercept plus docetaxel has achieved preliminary efficacy in Chinese patients with NPC, and this treatment deserves further trials.241
Mk-2206 is an inhibitor of Akt, which has limited activity in the heavily pre-treated group of patients in a multicenter phase II clinical trial.242 Further studies are needed to select appropriate Akt inhibitors to treat NPC.
Famitinib, a tyrosine kinase inhibitor whose targets include VEGFR, platelet-derived growth factor receptor (PDGFR), and stem cell factor receptor (SCFR), has an encouraging anti-cancer profile and tolerability for patients with NPC along with chemoradiation. And it is necessary to expand the sample size to further confirm the efficacy.243 In NPC patients receiving high-dose radiation therapy, the incidence of upper respiratory tract bleeding will become higher after the use of sunitinib.244 Sorafenib has a certain anti-tumor effect and is well-tolerated by the subjects.245 The outcome of the phase II clinical trial has verified sorafenib combined with cisplatin and 5-FU is feasible and tolerable in patients with recurrent or metastatic NPC.246
Combination of endostar with gemcitabine–cisplatin chemotherapy can have good control of cancer progression and improve the prognosis of patients with NPC.247 Besides, endostar combined with IMRT has lower acute toxicity along with similar effects compared with IMRT.248
In clinical trials, the effect of targeted drugs alone is not good, whose PFS is generally less than one year, while targeted drugs combined with chemotherapy or radiotherapy can significantly delay the progress of the tumor, with a great improvement of PFS and OS.
In addition, there are some problems when studying clinical trials in targeted therapy of NPC:
The quantity of patients is small, which may cause the inaccuracy of the results.
Almost all the targets that occurred in clinical trials of NPC are VEGFR or EGFR and other new drugs targeting miRNAs or other key molecules can be developed.
More phase III clinical trials are needed after the drug has passed phase I and phase II clinical trials.
We summarize the current clinical trials related to targeted therapy for NPC, which are presented in Table 3.
Table 3.
Present clinical trials about targeted therapy in NPC
| Drug | Mechanism/target | Trial phase | Treatment schedule | Patients number | Patients characteristics | PFS | OS | References |
|---|---|---|---|---|---|---|---|---|
| Gefitinib | EGFR | II | Single drug | 19 | Recurrent metastatic NPC | – | 16 months | 232 |
| Nimotuzumab | EGFR | II | Combined with cisplatin and 5-fluorouracil | 39 | Recurrent metastatic NPC | 7.0 months | 16.3 months | 233 |
| Nimotuzumab | EGFR | II | Induction chemotherapy, sequential Nimotuzumab plus concurrent chemoradiotherapy. | 45 | N3M0 | 79.5% (3 years) | 85.6 (3 years) | 234 |
| Cetuximab | EGFR | II | Concurrent HT with cetuximab, followed by chemotherapy (docetaxel and cisplatin) | 43 | 33 Stage III and 10 Stage IV | 79.1% (2 years), 72% (3 years) | 93.0% (2 years), 85.7% (3 years) | 235 |
| Cetuximab | EGFR | II | Cetuximab-radiotherapy | 21 | Stage III–IVb | 95.2% (3 years) | 100% (3 years) | 236 |
| h-R3 | EGFR | II | Radiotherapy combined with h-R3 | 35 | Stage III–IVb | – | – | 237 |
| Bevacizumab | VEGF | II | 44 | – | – | 90.9% (2 years) | 238 | |
| Bevacizumab | VEGF | II | Bevacizumab, corticosteroid-controlled | 112 | – | – | – | 239 |
| Axitinib | VEGFR | II | Single drug | 40 | Recurrent or metastatic NPC | 5.0 months | 10.4 months | 240 |
| Aflibercept | VEGF | I | Aflibercept plus docetaxel | 16 | – | – | – | 241 |
| Mk-2206 | Akt | II | Single drug | 21 | Recurrent or metastatic NPC | 3.5 months | 10 months | 242 |
| Famitinib | VEGFR, PDGFR (platelet-derived growth factor receptor), SCFR (stem cell factor receptor) | I | Single drug | 20 | Stage III or IVa-b NPC | 75% (3 years) | – | 243 |
| Sunitinib | multi-kinase inhibitor | II | Single drug | 14 | Previously received high-dose radiation | 3.5 months | 10.5 months | 244 |
| Sorafenib | multi-kinase inhibitor | II | Single drug | 28 | – | 3.9% (6 months) | 4.2 months | 245 |
| Sorafenib | multi-kinase inhibitor | II | Single drug | 54 | Recurrent or metastatic NPC | 7.2 months | 11.8 months | 246 |
| Endostar | VEGF, VEGFR, PDGFR | II | Combination of gemcitabine | 30 | – | 19.4 months | 90.2% (1 year) | 247 |
| Endostar | VEGF, VEGFR, PDGFR | – | Intensity-modulated radiotherapy combined with endostar | 23 | Stage III-IVa | 100% (2 years) | 100% (2 years) | 248 |
“–” means not clear, PFS progression-free survival, OS overall survival
Biomarkers and preclinical researches
PKB, mTOR, and PI3K in NPC tissues are highly upregulated and have higher positive rates than in normal nasopharyngeal tissues; Cox regression analysis reveals expressions of PI3K, PKB and mTOR are the major risk factors for the prognosis of NPC.249 High expression of LMP1 is strongly associated with NPC patients’ survival, which indicates LMP1 may be potential prognostic biomarkers.250,251 In a study of NPC epithelial tissue, high expression of HIF-1α is found to be a new independent biomarker for predicting poor prognosis in NPC patients.252 It is found that the serum BMI-1 antibody in patients is significantly higher than in normal persons, suggesting that BMI-1 antibody may be a potential biomarker of NPC and has diagnostic and prognostic value.253 CDH6 is overexpressed in the LMP1-positive NPC tissues, which can promote EMT and metastasis of NPC, which may be a therapeutic target of NPC.107 Multivariable Cox regression analysis shows that BST2 expression can serve as independent prognostic factors and high BST2 expression can predict poor prognosis in patients with locally advanced NPC treated with platinum-based chemoradiotherapy.254 The expression of NRP-1 is highly upregulated in the NPC tissues and the multivariate analysis indicates that the overexpression of NRP-1 is an independent prognostic factor for NPC patients.255 Multivariate Cox regression indicates that the elevated MAP2K6 is independently associated with poor prognosis in NPC patients.129 Phosphorylated MNK1 has a significantly higher expression in NPC tissues compared to the nasopharyngeal epithelium and may be independent prognostic factors of NPC.256 The concentration of DAPK1 methylation in serum is significantly higher compared with the normal group and may become a diagnostic biomarker for early NPC.257
Clinical analysis shows that the high expression of miR-92a is associated with adverse clinicopathological features such as lymph node metastasis and distant metastasis in advanced tumors, and miR-92a is a good biomarker for predicting the prognosis of NPC patients.74 Similarly, clinical parameter researches reveal that elevated miR-18a levels are associated with advanced stages of NPC, lymph node metastasis, human herpesvirus IV infection, and high NPC mortality.258 MiR-124-3p significantly elevates after treatment and decreases at recurrence or metastasis compared with pretreatment, which reveals miR-124-3p may serve as the prognostic biomarker in NPC.259 The expression of miR-185-3p and miR-324-3p is significantly decreased after RT in radioresistant, and combined low miR-185-3p and miR-324-3p may be vital markers for prediction of low response to RT/CRT.217 Expression of lncRNA Hotair in NPC tissues is higher than in nasopharyngeal tissues and the multivariate analysis reveals that Hotair is a potential biomarker for prognosis of NPC.260 LncRNA ANRIL is overexpressed in NPC tissues, which is related to the clinical stage and can serve as an independent predictor for NPC patients.261
In addition, Annexin A1, CDKN3, OCT4, c-Src, COX-2, TNFAIP3, RERG, PBK, STAT3, DANCR, miR-29a, β-catenin, c-Myc, and Capn4 can be used as prognostic markers in NPC. Annexin A1 is a potential biomarker for predicting response to RT of NPC and predicting NPC differentiation and prognosis.262,263 High expression of CDKN3 is an independent negative prognostic factor in NPC.264 OCT4 is significantly associated with EMT and can be used as an independent prognostic factor in NPC.265 Elevated serum c-Src levels are associated with poor prognosis in NPC patients.86 In NPC patients, aberrant expression of COX-2 is associated with recurrence and poor prognosis.100 Downregulation of TNFAIP3 is associated with distant metastasis and worse patient prognosis.266 The methylation rates of RERG can serve as novel biomarkers for early detection and screening of NPC.267 High-level PBK in NPC is significantly associated with poor prognosis.145 STAT3 is associated with a relatively good prognosis in NPC patients.268 LncRNA DANCR can be used as a biomarker for poor prognosis.269 MiR-29a can promote metastasis and invasion of NPC cells, and it would be an ideal prognostic marker.270 Positive expression of β-catenin and c-Myc is negatively correlated with the survival rate of NPC patients, demonstrating they can be used as important prognostic biomarkers.271 Capn4 can promote invasion and metastasis of NPC, which suggests that Capn4 may be an independent prognostic factor in NPC.272
The lack of preclinical models is an important reason that hinders the development of targeted therapies for NPC, and we summarize some meaningful preclinical studies.
PBK can promote the growth of NPC in nude mice and HI-TOPK-032, the specific inhibitor for PBK/TOPK, can significantly reduce the volume and weight of NPC in nude mice without obvious signs of toxicity.145 In Wong et al.’s273 research, the tumor weight of mice treated with the PI3K-mTOR dual inhibitor PF-0469150210 is significantly reduced when compared with the control group. Besides, the PF-04691502 has minimal effect on the animal’s body weight with no gross toxicity observed throughout the treatment.
Brevilin A can inhibit PI3K/Akt/mTOR and STAT3 signaling pathways in vitro and Brevilin A treatment led to no significant weight loss in treated mice. These contribute to the preclinical development of Brevilin A as a chemotherapeutic for NPC.274 Evofosfamide is a hypoxia-activated prodrug that selectively targets hypoxic regions in solid tumors. Since HIF-1α is overexpressed in NPC tissues, the results provide preclinical evidence that Evofosfamide is used as a single drug in combination with DDP to target the selective anoxic fraction of NPC.275 COX-2 can promote the occurrence and recurrence of NPC, and the cellular senescence of fibroblasts in COX-2 knockout mice is significantly increased, suggesting that COX-2 may be a potential indicator to predict NPC recurrence and treatment resistance as well as a target for targeted therapy of NPC.100 The expression of EGFR correlates with β-catenin in NPC patient specimens, and β-catenin is responsible for regulating CSC characteristics of EGFR/Akt activation. The results suggest that targeting β-catenin is a reasonable clinical treatment for NPC with high EGFR or Akt expression.276
Discussion
The models for NPC research can be divided into two categories: in vitro models and in vivo models. The former includes the previous two-dimensional models and the current potential of the three-dimensional (3D) models.277 Two-dimensional models are effortless to build and maintained at a low cost.278 However, the lack of crosstalk with fibroblasts, immune cells and endothelial cells indicates that the tumor microenvironment in vivo cannot be entirely simulated, which is not convenient for drug penetration and drug resistance evaluation.277,279,280 The construction of 3D tumor spheroid models for NPC could be accomplished by EB virus-positive C666-1 cells, and also EB virus negative CNE-1 and CNE-2, HONE-1, and SUNE-1.124,171,273,281 Researchers can utilize different matrix to reconstruct tumor microenvironment, which guarantees drug sensitivity, the alterations of signaling pathways and gene expression in tumor cells.277 Benefiting from its simulation of body condition, they ensure the reliability and validity of the experimental results of the targeted drug candidates. However, the study used lapatinib, a tyrosine kinase inhibitor against EGFR, on HONE-1 spheroids exhibited that the drug did not diffuse effectively to core cells of mass.282 Organoids are a group of cells that undergo organ differentiation and directional self-organization of adult stem cells or pluripotent embryonic stem cells in vitro.283 The organoids from patients are called patient-derived organoids (PDO) models, which have the characteristics of high simulation, short culture period, and stable passage.284 It is considered as the most ideal preclinical model at present. Tumor organoids are obtained by using tumor cells harvested from patients to culture masses in vitro, which retains the genetic background and reproduces the microenvironment. PDO models are promising substitutes for patients, which can simulate the treatment response from the aspects of pathology, gene, cell and tumor microenvironment.285 Organoids can also be used as the model of NPC stem cells. The increased expression of tumor stem cell markers in organoids can be considered as the concentration and enrichment of tumor stem cells so that organoids behave similarly to patients on tumor recurrence and treatment resistance. Organoids have advantages in the study of intercellular interaction and immune microenvironment for it can stably carry the EB virus for a long time and mimic intercellular communication involving in exosomes.286 The test results of the breast cancer organoids for the HER-2 targeted drug gefitinib were consistent with the patients’ conditions, indicating that the organ model had similar properties to cancer in vivo.287
The construction of in vivo models could be divided into spontaneous models, induced models, transplantation models, and transgenic models.288–292 Spontaneous models are rarely obtained and utilized.288 Induction conforms to the characteristics of tumor dynamics and is often used to screen carcinogens but seldom used in targeted therapy for NPC.289 Transplantation models include subcutaneous xenotransplantation, orthotopic xenotransplantation, and patient-derived tumor xenografts (PDX).293,294 The first two tumors have different injection sites and in terms of the xenograft models, the tumor was in a mouse microenvironment rather than a human one. PDX models maintain the heterogeneity of tumor tissues, thus enabling phase I efficacy evaluation results to be more than 87% similar to clinical results.295,296 Several NPC PDXs are available for research in the past, including C18, C17, and C15.297 However, they passaged so long in nude mice that they may have altered the biological characteristics of original tumors. Thus, novel NPC PDXs models need to be established, normalized and unified to ensure the reliability of experimental results. Hsu et al.298 constructed a novel kind of PDX model to study the effect of anti-cancer drugs and treated a patient with liver metastasis of NPC with the same drugs and they confirmed that Palbociclib, a cyclin-dependent kinase inhibitor, had an anti-cancer effect, which helps to show the reliability of the application of PDX models in targeted therapy.
The products of EBV, lncRNAs, and miRNAs formulate a model of the regulatory network of metastasis in NPC.299 However, CSCs and EMT are closely related to recurrence and early metastasis in NPC. In NPC cells, some stem cell markers such as ALDH1, CD44, CD133, and Bim-1 have been confirmed. CSCs have biological characteristics including high self-renewal ability, pluripotent marker expression, and resistance to drug and radiation. Some signal pathways are important for the self-renewal and maintenance of stem cells.300 Nowadays, EMT activation is thought to be associated with the generation of CSCs.301 After activation of EMT, tumor epithelial cells transform into mesenchymal cells, with the loss of cell polarity and cell–cell adhesion and the gain of migratory and invasive property.302 Recent study showed that different mechanisms of EMT participate in cancer metastasis which includes cytoskeletal reorganization, altered expression of cell adhesion molecules, degradation of the basement membrane, and continuous autocrine growth factor signaling to evade apoptosis or anoikis.303 Serglycin has a vital role in enhancing NPC metastasis via enhancing EMT, cellular migration, and cellular invasiveness.304 Besides, IL-6 is able to reduce cell adherence toward laminin and stimulates the expression of MMP-2 and MMP-9, leading to metastasis of NPC.305–307 It is hoped that the emergence of targeted therapies against CSCs and EMT might bring about clinical benefits. However, continued study is still imperative in order to attain the goal of understanding the molecular expression profile together with the characteristics of signal pathways in CSCs.
The In-depth researches on targeted therapy of NPC are conducive to the clinical treatment of NPC. The PI3K/Akt pathway, which has an important role in NPC, can be activated by the EGF signal, and there are currently targeted drugs such as Cetuximab that target EGFR.236 Inhibitors of components in the PI3K/Akt pathway have been used to treat other cancers, and further studies are needed to determine whether they are appropriate for the treatment of NPC. P53 is an important tumor suppressor gene. There have been many studies on targeted therapy of p53. The main therapeutic methods are to restore the function of p53 and to interfere with the p53–MDM2 axis.308 By reviewing recent studies on PI3K/Akt pathway and p53 pathway in NPC, we have summarized some potential targets that can affect the PI3K/Akt pathway and p53 pathway, which will be conducive to the selection of targeted therapeutic targets for NPC in future basic studies. Meanwhile, the targeted drugs used to treat NPC in clinical trials mainly consist of EGFR inhibitor (Cetuximab, Nimotuzumab), VEGF/VEGFR inhibitor (Bevacizumab, Endostar). Most targeted drugs are still in the level of basic experiments, their clear mechanisms of action need a further investigation. However, compared with traditional treatment, the molecular targeted therapy brings less side effects, which can improve the prognosis of patients and increase the tolerance of treatment. Owing to the fact that the Notch signal pathway could be involved in the radioresistance of NPC, whether it has other roles in the progression and prognosis of NPC should be further studied. Radioresistance is the main cause of poor prognosis of advanced-stage NPC, thus molecular targets that reduce radioresistance and increase radiosensitivity should be thoroughly studied, and related drugs should be combined with radiotherapy to test efficacy and safety.
On the one hand, lncRNAs could modulate the related miRNA and downstream genes axis so that they have dual roles in NPC. On the other hand, the research and development of drugs targeting lncRNAs for the treatment of NPC are still rare and studies will be needed to develop new strategies based on lncRNAs in the future. MiRNAs have recently been found to be highly or lowly expressed in tumor cells, and some miRNAs have been shown to promote or inhibit the processes of NPC cells in vitro and in vivo. Future NPC treatment can inhibit the proliferation, metastasis, EMT or angiogenesis of tumor cells by inhibiting the relevant miRNAs. Some miRNAs can increase the sensitivity of tumor cells to anti-cancer drugs and can be used in combination with targeted therapeutic drugs to improve the efficacy, while other miRNAs can reduce the radioresistance of NPC cells and can be considered in combination with local IMRT. However, to carry out the above possible therapeutic methods, it is also necessary to continuously study the functions of molecules including proteins, DNA, and RNA on the cytoplasm and membrane of tumor cells and normal cells, gradually complete the relationship network in the tumor and perform cellular and animal experiments on potential targets. In addition, miRNAs have an important role in the maintenance of the tumor microenvironment and communication between tumor cells, and it can be explored to understand what the specific mechanism of miRNA involvement is, which in turn provides a theoretical basis for possible targeted therapy.
In addition to further study in NPC treatment, effective population screening may improve the detection rate of early-stage NPC, which is conducive to the early treatment of NPC. By now, the detection of early-stage NPC is mainly through EBA IgA antibody (EA-IgA), anti-EBV capsid antigen (VCA-IgA), anti-EBV nuclear antigen 1 (EBNA1-IgA), while the extensive application is restricted by the low sensitivity and specificity.309 Encouragingly, recent studies have found that plasma EBV DNA detection displays a better outcome on early-stage NPC detection.310,311 Besides, with the profound study of vaccine technology and the growing understanding of EBV immunology, an increasing number of vaccine candidates against EBV have been developed.312,313 Clearly, thorough studies are needed to provide more insight into early-stage NPC screening and NPC vaccines, which have a huge application foreground in the prevention and treatment of NPC in the future.
Funding
The present study was supported by the National Natural Science Foundation of China (grant nos. 81773179 and 81272972 (C.R.), and grant no. 81472355 (X.J.)), the Provincial Natural Science Foundation of Hunan (grant nos. 2020JJ4771, 2016JJ2172 (W.L.)), the National Basic Research Program of China (2010CB833605 (C.R.)), the Program for New Century Excellent Talents in University (NCET-10-0790 (C.R.)), the Hunan Provincial Science and Technology Department (grant nos. 2016JC2049 (C.R.), 2014FJ6006 (X.J.)), and the Undergraduate Training Programs for Innovation and Entrepreneurship (UTPIE, S2020105330083 (Y.K.)).
Author contributions
Y.K., W.H., H.X., and C.R. contributed to design the study. Y.K., W.H., J.Q., Q.G., and J.H. drafted and critically revised the manuscript. H.X., X.J., L.W., and C.R. discussed and revised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Yuanbo Kang, Weihan He
Contributor Information
Caiping Ren, Email: rencaiping@csu.edu.cn.
Lei Wang, Email: leiwang@csu.edu.cn.
References
- 1.Bray F, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Chen YP, et al. Nasopharyngeal carcinoma. Lancet. 2019;394:64–80. doi: 10.1016/S0140-6736(19)30956-0. [DOI] [PubMed] [Google Scholar]
- 3.Wang HY, et al. A new prognostic histopathologic classification of nasopharyngeal carcinoma. Chin. J. Cancer. 2016;35:41. doi: 10.1186/s40880-016-0103-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamran SC, Riaz N, Lee N. Nasopharyngeal carcinoma. Surg. Oncol. Clin. N. Am. 2015;24:547–561. doi: 10.1016/j.soc.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Young LS, Dawson CW. Epstein-Barr virus and nasopharyngeal carcinoma. Chin. J. Cancer. 2014;33:581–590. doi: 10.5732/cjc.014.10208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kong F-F, et al. Effectiveness and toxicities of intensity-modulated radiation therapy for patients with T4 nasopharyngeal carcinoma. PLoS ONE. 2014;9:e91362. doi: 10.1371/journal.pone.0091362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng SH, et al. Prognostic features and treatment outcome in locoregionally advanced nasopharyngeal carcinoma following concurrent chemotherapy and radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 1998;41:755–762. doi: 10.1016/S0360-3016(98)00092-3. [DOI] [PubMed] [Google Scholar]
- 8.Huang DP, Ho JH, Chan WK, Lau WH, Lui M. Cytogenetics of undifferentiated nasopharyngeal carcinoma xenografts from southern Chinese. Int. J. Cancer. 1989;43:936–939. doi: 10.1002/ijc.2910430535. [DOI] [PubMed] [Google Scholar]
- 9.Hui AB, et al. Array-based comparative genomic hybridization analysis identified cyclin D1 as a target oncogene at 11q13.3 in nasopharyngeal carcinoma. Cancer Res. 2005;65:8125–8133. doi: 10.1158/0008-5472.CAN-05-0648. [DOI] [PubMed] [Google Scholar]
- 10.Lo KW, Chung GT, To KF. Deciphering the molecular genetic basis of NPC through molecular, cytogenetic, and epigenetic approaches. Semin. Cancer Biol. 2012;22:79–86. doi: 10.1016/j.semcancer.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 11.Lo KW, et al. High resolution allelotype of microdissected primary nasopharyngeal carcinoma. Cancer Res. 2000;60:3348–3353. [PubMed] [Google Scholar]
- 12.Wong N, et al. Molecular cytogenetic characterization of nasopharyngeal carcinoma cell lines and xenografts by comparative genomic hybridization and spectral karyotyping. Cancer Genet. Cytogenet. 2003;140:124–132. doi: 10.1016/S0165-4608(02)00657-X. [DOI] [PubMed] [Google Scholar]
- 13.Hui AB, et al. Detection of recurrent chromosomal gains and losses in primary nasopharyngeal carcinoma by comparative genomic hybridisation. Int. J. Cancer. 1999;82:498–503. doi: 10.1002/(SICI)1097-0215(19990812)82:4<498::AID-IJC5>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 14.Chen YJ, et al. Chromosomal aberrations in nasopharyngeal carcinoma analyzed by comparative genomic hybridization. Genes Chromosomes Cancer. 1999;25:169–175. doi: 10.1002/(SICI)1098-2264(199906)25:2<169::AID-GCC13>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 15.Fang Y, et al. Analysis of genetic alterations in primary nasopharyngeal carcinoma by comparative genomic hybridization. Genes Chromosomes Cancer. 2001;30:254–260. doi: 10.1002/1098-2264(2000)9999:9999<::AID-GCC1086>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 16.Lin W, et al. Establishment and characterization of new tumor xenografts and cancer cell lines from EBV-positive nasopharyngeal carcinoma. Nat. Commun. 2018;9:4663. doi: 10.1038/s41467-018-06889-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lo KW, et al. High frequency of promoter hypermethylation of RASSF1A in nasopharyngeal carcinoma. Cancer Res. 2001;61:3877–3881. [PubMed] [Google Scholar]
- 18.Lin DC, et al. The genomic landscape of nasopharyngeal carcinoma. Nat. Genet. 2014;46:866–871. doi: 10.1038/ng.3006. [DOI] [PubMed] [Google Scholar]
- 19.Dawson CW, Port RJ, Young LS. The role of the EBV-encoded latent membrane proteins LMP1 and LMP2 in the pathogenesis of nasopharyngeal carcinoma (NPC) Semin. Cancer Biol. 2012;22:144–153. doi: 10.1016/j.semcancer.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Frappier L. Role of EBNA1 in NPC tumourigenesis. Semin. Cancer Biol. 2012;22:154–161. doi: 10.1016/j.semcancer.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Takada K. Role of EBER and BARF1 in nasopharyngeal carcinoma (NPC) tumorigenesis. Semin Cancer Biol. 2012;22:162–165. doi: 10.1016/j.semcancer.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Cosmopoulos K, et al. Comprehensive profiling of Epstein-Barr virus microRNAs in nasopharyngeal carcinoma. J. Virol. 2009;83:2357–2367. doi: 10.1128/JVI.02104-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong X, et al. Circular RNA CRIM1 functions as a ceRNA to promote nasopharyngeal carcinoma metastasis and docetaxel chemoresistance through upregulating FOXQ1. Mol. Cancer. 2020;19:33. doi: 10.1186/s12943-020-01149-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Young LS, Yap LF, Murray PG. Epstein-Barr virus: more than 50 years old and still providing surprises. Nat. Rev. Cancer. 2016;16:789–802. doi: 10.1038/nrc.2016.92. [DOI] [PubMed] [Google Scholar]
- 25.Li YY, et al. Exome and genome sequencing of nasopharynx cancer identifies NF-kappaB pathway activating mutations. Nat. Commun. 2017;8:14121. doi: 10.1038/ncomms14121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng H, et al. Whole-exome sequencing identifies multiple loss-of-function mutations of NF-kappaB pathway regulators in nasopharyngeal carcinoma. Proc. Natl Acad. Sci. USA. 2016;113:11283–11288. doi: 10.1073/pnas.1607606113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsai CN, Tsai CL, Tse KP, Chang HY, Chang YS. The Epstein-Barr virus oncogene product, latent membrane protein 1, induces the downregulation of E-cadherin gene expression via activation of DNA methyltransferases. Proc. Natl Acad. Sci. USA. 2002;99:10084–10089. doi: 10.1073/pnas.152059399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skalska L, White RE, Franz M, Ruhmann M, Allday MJ. Epigenetic repression of p16(INK4A) by latent Epstein-Barr virus requires the interaction of EBNA3A and EBNA3C with CtBP. PLoS Pathog. 2010;6:e1000951. doi: 10.1371/journal.ppat.1000951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kwong J, et al. Promoter hypermethylation of multiple genes in nasopharyngeal carcinoma. Clin. Cancer Res. 2002;8:131–137. [PubMed] [Google Scholar]
- 30.Qiu GH, et al. The candidate tumor suppressor gene BLU, located at the commonly deleted region 3p21.3, is an E2F-regulated, stress-responsive gene and inactivated by both epigenetic and genetic mechanisms in nasopharyngeal carcinoma. Oncogene. 2004;23:4793–4806. doi: 10.1038/sj.onc.1207632. [DOI] [PubMed] [Google Scholar]
- 31.Li L, et al. Epigenomic characterization of a p53-regulated 3p22.2 tumor suppressor that inhibits STAT3 phosphorylation via protein docking and is frequently methylated in esophageal and other carcinomas. Theranostics. 2018;8:61–77. doi: 10.7150/thno.20893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ren X, et al. HOPX hypermethylation promotes metastasis via activating SNAIL transcription in nasopharyngeal carcinoma. Nat. Commun. 2017;8:14053. doi: 10.1038/ncomms14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chan KC, et al. Catalytic activity of Matrix metalloproteinase-19 is essential for tumor suppressor and anti-angiogenic activities in nasopharyngeal carcinoma. Int. J. Cancer. 2011;129:1826–1837. doi: 10.1002/ijc.25855. [DOI] [PubMed] [Google Scholar]
- 34.Cheung HW, et al. Epigenetic inactivation of CHFR in nasopharyngeal carcinoma through promoter methylation. Mol. Carcinog. 2005;43:237–245. doi: 10.1002/mc.20106. [DOI] [PubMed] [Google Scholar]
- 35.Sun D, et al. Aberrant methylation of CDH13 gene in nasopharyngeal carcinoma could serve as a potential diagnostic biomarker. Oral. Oncol. 2007;43:82–87. doi: 10.1016/j.oraloncology.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 36.Chak WP, et al. Downregulation of long non-coding RNA MEG3 in nasopharyngeal carcinoma. Mol. Carcinog. 2017;56:1041–1054. doi: 10.1002/mc.22569. [DOI] [PubMed] [Google Scholar]
- 37.Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-Y. [DOI] [PubMed] [Google Scholar]
- 38.Wightman B, Ha I, Ruvkun G. Posttranscriptional regulation of the heterochronic gene lin-14 by lin-4 mediates temporal pattern formation in C. elegans. Cell. 1993;75:855–862. doi: 10.1016/0092-8674(93)90530-4. [DOI] [PubMed] [Google Scholar]
- 39.Chang L, et al. Acquisition of epithelial-mesenchymal transition and cancer stem cell phenotypes is associated with activation of the PI3K/Akt/mTOR pathway in prostate cancer radioresistance. Cell Death Dis. 2013;4:e875. doi: 10.1038/cddis.2013.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh-Gupta V, et al. Radiation-induced HIF-1alpha cell survival pathway is inhibited by soy isoflavones in prostate cancer cells. Int. J. Cancer. 2009;124:1675–1684. doi: 10.1002/ijc.24015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hsieh AC, et al. The translational landscape of mTOR signalling steers cancer initiation and metastasis. Nature. 2012;485:55–61. doi: 10.1038/nature10912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dowling RJ, et al. mTORC1-mediated cell proliferation, but not cell growth, controlled by the 4E-BPs. Science. 2010;328:1172–1176. doi: 10.1126/science.1187532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ni J, et al. Cancer stem cells in prostate cancer chemoresistance. Curr. Cancer Drug Targets. 2014;14:225–240. doi: 10.2174/1568009614666140328152459. [DOI] [PubMed] [Google Scholar]
- 44.Kim KJ, et al. Inhibition of vascular endothelial growth factor-induced angiogenesis suppresses tumour growth in vivo. Nature. 1993;362:841–844. doi: 10.1038/362841a0. [DOI] [PubMed] [Google Scholar]
- 45.Chen MS, et al. Wnt/beta-catenin mediates radiation resistance of Sca1+ progenitors in an immortalized mammary gland cell line. J. Cell Sci. 2007;120:468–477. doi: 10.1242/jcs.03348. [DOI] [PubMed] [Google Scholar]
- 46.Stier S, Cheng T, Dombkowski D, Carlesso N, Scadden DT. Notch1 activation increases hematopoietic stem cell self-renewal in vivo and favors lymphoid over myeloid lineage outcome. Blood. 2002;99:2369–2378. doi: 10.1182/blood.V99.7.2369. [DOI] [PubMed] [Google Scholar]
- 47.Duncan AW, et al. Integration of Notch and Wnt signaling in hematopoietic stem cell maintenance. Nat. Immunol. 2005;6:314–322. doi: 10.1038/ni1164. [DOI] [PubMed] [Google Scholar]
- 48.De Luca A, Maiello MR, D'Alessio A, Pergameno M, Normanno N. The RAS/RAF/MEK/ERK and the PI3K/AKT signalling pathways: role in cancer pathogenesis and implications for therapeutic approaches. Expert Opin. Ther. Targets. 2012;16(Suppl 2):S17–S27. doi: 10.1517/14728222.2011.639361. [DOI] [PubMed] [Google Scholar]
- 49.Deschênes-Simard X, et al. Tumor suppressor activity of the ERK/MAPK pathway by promoting selective protein degradation. Genes Dev. 2013;27:900–915. doi: 10.1101/gad.203984.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caponigro F, Longo F, Ionna F, Perri F. Treatment approaches to nasopharyngeal carcinoma: a review. Anti-Cancer drugs. 2010;21:471–477. doi: 10.1097/CAD.0b013e328337160e. [DOI] [PubMed] [Google Scholar]
- 51.Colli LM, et al. Landscape of combination immunotherapy and targeted therapy to improve cancer management. Cancer Res. 2017;77:3666–3671. doi: 10.1158/0008-5472.CAN-16-3338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Engelman JA, Luo J, Cantley LC. The evolution of phosphatidylinositol 3-kinases as regulators of growth and metabolism. Nat. Rev. Genet. 2006;7:606–619. doi: 10.1038/nrg1879. [DOI] [PubMed] [Google Scholar]
- 53.Maehama T, Dixon JE. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J. Biol. Chem. 1998;273:13375–13378. doi: 10.1074/jbc.273.22.13375. [DOI] [PubMed] [Google Scholar]
- 54.Kim YC, Guan K-L. mTOR: a pharmacologic target for autophagy regulation. J. Clin. Invest. 2015;125:25–32. doi: 10.1172/JCI73939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gustin JP, Cosgrove DP, Park BH. The PIK3CA gene as a mutated target for cancer therapy. Curr. Cancer Drug Targets. 2008;8:733–740. doi: 10.2174/156800908786733504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Or YY, Hui AB, To KF, Lam CN, Lo KW. PIK3CA mutations in nasopharyngeal carcinoma. Int J. Cancer. 2006;118:1065–1067. doi: 10.1002/ijc.21444. [DOI] [PubMed] [Google Scholar]
- 57.Bruce JP, Yip K, Bratman SV, Ito E, Liu FF. Nasopharyngeal cancer: molecular landscape. J. Clin. Oncol. 2015;33:3346–3355. doi: 10.1200/JCO.2015.60.7846. [DOI] [PubMed] [Google Scholar]
- 58.Horikawa T, et al. Epstein-Barr virus latent membrane protein 1 induces Snail and epithelial-mesenchymal transition in metastatic nasopharyngeal carcinoma. Br. J. Cancer. 2011;104:1160–1167. doi: 10.1038/bjc.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Siler CA, Raab-Traub N. Rhesus lymphocryptovirus latent membrane protein 2A activates beta-catenin signaling and inhibits differentiation in epithelial cells. Virology. 2008;377:273–279. doi: 10.1016/j.virol.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 60.Li SS, Yang S, Yin DH, Li P. Inhibition of PI3K-Akt pathway reverses LMP1 induced TRAIL resistance in nasopharyngeal carcinoma cell. J. Clin. Otorhinolaryngol. Head. Neck Surg. 2016;30:744–747. doi: 10.13201/j.issn.1001-1781.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 61.Luo X, et al. DNMT1 mediates metabolic reprogramming induced by Epstein-Barr virus latent membrane protein 1 and reversed by grifolin in nasopharyngeal carcinoma. Cell Death Dis. 2018;9:619. doi: 10.1038/s41419-018-0662-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lu ZW, et al. MiR-152 functioning as a tumor suppressor that interacts with DNMT1 in nasopharyngeal carcinoma. OncoTargets Ther. 2018;11:1733–1741. doi: 10.2147/OTT.S154464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li Y, et al. EZH2-DNMT1-mediated epigenetic silencing of miR-142-3p promotes metastasis through targeting ZEB2 in nasopharyngeal carcinoma. Cell Death Differ. 2019;26:1089–1106. doi: 10.1038/s41418-018-0208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lo AK, et al. Activation of sterol regulatory element-binding protein 1 (SREBP1)-mediated lipogenesis by the Epstein-Barr virus-encoded latent membrane protein 1 (LMP1) promotes cell proliferation and progression of nasopharyngeal carcinoma. J. Pathol. 2018;246:180–190. doi: 10.1002/path.5130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Xiang T, et al. Vasculogenic mimicry formation in EBV-associated epithelial malignancies. Nat. Commun. 2018;9:5009. doi: 10.1038/s41467-018-07308-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 66.Huang W, et al. Sodium butyrate induces autophagic apoptosis of nasopharyngeal carcinoma cells by inhibiting AKT/mTOR signaling. Biochem. Biophys. Res. Commun. 2019;514:64–70. doi: 10.1016/j.bbrc.2019.04.111. [DOI] [PubMed] [Google Scholar]
- 67.Johansen C, et al. MK2 regulates the early stages of skin tumor promotion. Carcinogenesis. 2009;30:2100–2108. doi: 10.1093/carcin/bgp238. [DOI] [PubMed] [Google Scholar]
- 68.Deng X, et al. miR-296-3p negatively regulated by nicotine stimulates cytoplasmic translocation of c-Myc via MK2 to suppress chemotherapy resistance. Mol. Ther. 2018;26:1066–1081. doi: 10.1016/j.ymthe.2018.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhen Y, et al. miR-374a-CCND1-pPI3K/AKT-c-JUN feedback loop modulated by PDCD4 suppresses cell growth, metastasis, and sensitizes nasopharyngeal carcinoma to cisplatin. Oncogene. 2017;36:275–285. doi: 10.1038/onc.2016.201. [DOI] [PubMed] [Google Scholar]
- 70.Zheng ZQ, et al. Long noncoding RNA FAM225A promotes nasopharyngeal carcinoma tumorigenesis and metastasis by acting as ceRNA to sponge miR-590-3p/miR-1275 and upregulate ITGB3. Cancer Res. 2019;79:4612–4626. doi: 10.1158/0008-5472.CAN-19-0799. [DOI] [PubMed] [Google Scholar]
- 71.Li Y, et al. Chemical compound cinobufotalin potently induces FOXO1-stimulated cisplatin sensitivity by antagonizing its binding partner MYH9. Signal Transduct. Target. Ther. 2019;4:48. doi: 10.1038/s41392-019-0084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lu J, et al. Exosomal miR-9 inhibits angiogenesis by targeting MDK and regulating PDK/AKT pathway in nasopharyngeal carcinoma. J. Exp. Clin. cancer Res. 2018;37:147. doi: 10.1186/s13046-018-0814-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xu Y, et al. Midkine positively regulates the proliferation of human gastric cancer cells. Cancer Lett. 2009;279:137–144. doi: 10.1016/j.canlet.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 74.Zhang H, Cao H, Xu D, Zhu K. MicroRNA-92a promotes metastasis of nasopharyngeal carcinoma by targeting the PTEN/AKT pathway. OncoTargets Ther. 2016;9:3579–3588. doi: 10.2147/OTT.S105470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cai L, et al. Gold nano-particles (AuNPs) carrying anti-EBV-miR-BART7-3p inhibit growth of EBV-positive nasopharyngeal carcinoma. Oncotarget. 2015;6:7838–7850. doi: 10.18632/oncotarget.3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pu L, Su L, Kang X. The efficacy of cisplatin on nasopharyngeal carcinoma cells may be increased via the downregulation of fibroblast growth factor receptor 2. Int. J. Mol. Med. 2019;44:57–66. doi: 10.3892/ijmm.2019.4193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.He Q, et al. miR-16 targets fibroblast growth factor 2 to inhibit NPC cell proliferation and invasion via PI3K/AKT and MAPK signaling pathways. Oncotarget. 2016;7:3047–3058. doi: 10.18632/oncotarget.6504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liu S, Liao G, Li G. Regulatory effects of COL1A1 on apoptosis induced by radiation in cervical cancer cells. Cancer Cell Int. 2017;17:73. doi: 10.1186/s12935-017-0443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guo Y, Zhai J, Zhang J, Ni C, Zhou H. Improved radiotherapy sensitivity of nasopharyngeal carcinoma cells by miR-29-3p targeting COL1A1 3'-UTR. Med. Sci. Monit. 2019;25:3161–3169. doi: 10.12659/MSM.915624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ma R, et al. RNA binding motif protein 3 (RBM3) drives radioresistance in nasopharyngeal carcinoma by reducing apoptosis via the PI3K/AKT/Bcl-2 signaling pathway. Am. J. Transl. Res. 2018;10:4130–4140. [PMC free article] [PubMed] [Google Scholar]
- 81.Yu D, et al. PNUTS mediates ionizing radiation-induced CNE-2 nasopharyngeal carcinoma cell migration, invasion, and epithelial-mesenchymal transition via the PI3K/AKT signaling pathway. OncoTargets Ther. 2019;12:1205–1214. doi: 10.2147/OTT.S188571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhu JF, et al. Annexin A1-suppressed autophagy promotes nasopharyngeal carcinoma cell invasion and metastasis by PI3K/AKT signaling activation. Cell Death Dis. 2018;9:1154. doi: 10.1038/s41419-018-1204-7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 83.Li XJ, et al. As an independent unfavorable prognostic factor, IL-8 promotes metastasis of nasopharyngeal carcinoma through induction of epithelial-mesenchymal transition and activation of AKT signaling. Carcinogenesis. 2012;33:1302–1309. doi: 10.1093/carcin/bgs181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang RL, et al. IL-8 suppresses E-cadherin expression in nasopharyngeal carcinoma cells by enhancing E-cadherin promoter DNA methylation. Int. J. Oncol. 2016;48:207–214. doi: 10.3892/ijo.2015.3226. [DOI] [PubMed] [Google Scholar]
- 85.Wang H, Chen H, Zhou H, Yu W, Lu Z. Cyclin-dependent kinase inhibitor 3 promotes cancer cell proliferation and tumorigenesis in nasopharyngeal carcinoma by targeting p27. Oncol. Res. 2017;25:1431–1440. doi: 10.3727/096504017X14835311718295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ke L, et al. c-Src activation promotes nasopharyngeal carcinoma metastasis by inducing the epithelial-mesenchymal transition via PI3K/Akt signaling pathway: a new and promising target for NPC. Oncotarget. 2016;7:28340–28355. doi: 10.18632/oncotarget.8634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wen Q, et al. Increased expression of flotillin-2 protein as a novel biomarker for lymph node metastasis in nasopharyngeal carcinoma. PLoS ONE. 2014;9:e101676. doi: 10.1371/journal.pone.0101676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu J, et al. Flotillin-2 promotes metastasis of nasopharyngeal carcinoma by activating NF-κB and PI3K/Akt3 signaling pathways. Sci. Rep. 2015;5:11614. doi: 10.1038/srep11614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu W, et al. PLCD3, a flotillin2-interacting protein, is involved in proliferation, migration and invasion of nasopharyngeal carcinoma cells. Oncol. Rep. 2018;39:45–52. doi: 10.3892/or.2017.6080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pan M, et al. EpCAM ectodomain EpEX is a ligand of EGFR that counteracts EGF-mediated epithelial-mesenchymal transition through modulation of phospho-ERK1/2 in head and neck cancers. PLoS Biol. 2018;16:e2006624. doi: 10.1371/journal.pbio.2006624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang M-H, et al. Epithelial cell adhesion molecule overexpression regulates epithelial-mesenchymal transition, stemness and metastasis of nasopharyngeal carcinoma cells via the PTEN/AKT/mTOR pathway. Cell Death Dis. 2018;9:2. doi: 10.1038/s41419-017-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Li JY, et al. S897 phosphorylation of EphA2 is indispensable for EphA2-dependent nasopharyngeal carcinoma cell invasion, metastasis and stem properties. Cancer Lett. 2019;444:162–174. doi: 10.1016/j.canlet.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 93.Xu S, et al. LZTS2 inhibits PI3K/AKT activation and radioresistance in nasopharyngeal carcinoma by interacting with p85. Cancer Lett. 2018;420:38–48. doi: 10.1016/j.canlet.2018.01.067. [DOI] [PubMed] [Google Scholar]
- 94.Yang F, Liu Q, Hu CM. Epstein-Barr virus-encoded LMP1 increases miR-155 expression, which promotes radioresistance of nasopharyngeal carcinoma via suppressing UBQLN1. Eur. Rev. Med. Pharmacol. Sci. 2015;19:4507–4515. [PubMed] [Google Scholar]
- 95.Mai S, et al. MicroRNA-18a promotes cancer progression through SMG1 suppression and mTOR pathway activation in nasopharyngeal carcinoma. Cell Death Dis. 2019;10:819. doi: 10.1038/s41419-019-2060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tsang CM, Lui VWY, Bruce JP, Pugh TJ, Lo KW. Translational genomics of nasopharyngeal cancer. Semin Cancer Biol. 2020;61:84–100. doi: 10.1016/j.semcancer.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 97.Huang L, et al. The p53 inhibitors MDM2/MDMX complex is required for control of p53 activity in vivo. Proc. Natl Acad. Sci. USA. 2011;108:12001–12006. doi: 10.1073/pnas.1102309108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Voon YL, et al. Nutlin-3 sensitizes nasopharyngeal carcinoma cells to cisplatin-induced cytotoxicity. Oncol. Rep. 2015;34:1692–1700. doi: 10.3892/or.2015.4177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fan X, et al. MDM2 inhibitor RG7388 potently inhibits tumors by activating p53 pathway in nasopharyngeal carcinoma. Cancer Biol. Ther. 2019;20:1328–1336. doi: 10.1080/15384047.2019.1638677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shi C, et al. High COX-2 expression contributes to a poor prognosis through the inhibition of chemotherapy-induced senescence in nasopharyngeal carcinoma. Int. J. Oncol. 2018;53:1138–1148. doi: 10.3892/ijo.2018.4462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Xu X, et al. Downregulation of Bmi-1 is associated with suppressed tumorigenesis and induced apoptosis in CD44(+) nasopharyngeal carcinoma cancer stem-like cells. Oncol. Rep. 2016;35:923–931. doi: 10.3892/or.2015.4414. [DOI] [PubMed] [Google Scholar]
- 102.Yu C, et al. Pin2 telomeric repeat factor 1-interacting telomerase inhibitor 1 (PinX1) inhibits nasopharyngeal cancer cell stemness: implication for cancer progression and therapeutic targeting. J. Exp. Clin. Cancer Res. 2020;39:31. doi: 10.1186/s13046-020-1530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chen JJ, Liu SX, Chen MZ, Zhao ZY. HasmiR125a and 125b are induced by treatment with cisplatin in nasopharyngeal carcinoma and inhibit apoptosis in a p53 dependent manner by targeting p53 mRNA. Mol. Med. Rep. 2015;12:3569–3574. doi: 10.3892/mmr.2015.3863. [DOI] [PubMed] [Google Scholar]
- 104.Hayden MS, Ghosh S. NF-kappaB, the first quarter-century: remarkable progress and outstanding questions. Genes Dev. 2012;26:203–234. doi: 10.1101/gad.183434.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yi M, et al. Rediscovery of NF-kappaB signaling in nasopharyngeal carcinoma: How genetic defects of NF-kappaB pathway interplay with EBV in driving oncogenesis? J. Cell Physiol. 2018;233:5537–5549. doi: 10.1002/jcp.26410. [DOI] [PubMed] [Google Scholar]
- 106.Shair KH, et al. EBV latent membrane protein 1 activates Akt, NFkappaB, and Stat3 in B cell lymphomas. PLoS Pathog. 2007;3:e166. doi: 10.1371/journal.ppat.0030166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zuo LL, et al. Cadherin 6 is activated by Epstein-Barr virus LMP1 to mediate EMT and metastasis as an interplay node of multiple pathways in nasopharyngeal carcinoma. Oncogenesis. 2017;6:402–402. doi: 10.1038/s41389-017-0005-7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 108.Zuo L, et al. Targeting exosomal EBV-LMP1 transfer and miR-203 expression via the NF-kappaB pathway: the therapeutic role of aspirin in NPC. Mol. Ther. Nucleic Acids. 2019;17:175–184. doi: 10.1016/j.omtn.2019.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ding RR, et al. Epstein-Barr virus-encoded LMP1 regulated Pim1 kinase expression promotes nasopharyngeal carcinoma cells proliferation. OncoTargets Ther. 2019;12:1137–1146. doi: 10.2147/OTT.S190274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Paul, A., Edwards, J., Pepper, C. & Mackay, S. Inhibitory-kappaB Kinase (IKK) alpha and nuclear factor-kappaB (NFkappaB)-inducing kinase (NIK) as anti-cancer drug targets. Cells. 7, 176 (2018). [DOI] [PMC free article] [PubMed]
- 111.Wang W, Cheng H, Gu X, Yin X. The natural flavonoid glycoside vitexin displays preclinical antitumor activity by suppressing NF-kappaB signaling in nasopharyngeal carcinoma. OncoTargets Ther. 2019;12:4461–4468. doi: 10.2147/OTT.S210077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kuang CM, et al. BST2 confers cisplatin resistance via NF-kappaB signaling in nasopharyngeal cancer. Cell Death Dis. 2017;8:e2874. doi: 10.1038/cddis.2017.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ouyang L, et al. SIRT6 overexpression induces apoptosis of nasopharyngeal carcinoma by inhibiting NF-kappaB signaling. OncoTargets Ther. 2018;11:7613–7624. doi: 10.2147/OTT.S179866. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 114.Cheng N, Guo Y. Long noncoding RNA NEAT1 promotes nasopharyngeal carcinoma progression through regulation of miR-124/NF-kappaB pathway. OncoTargets Ther. 2017;10:5843–5853. doi: 10.2147/OTT.S151800. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 115.Durkin ME, et al. DLC-1:a Rho GTPase-activating protein and tumour suppressor. J. Cell. Mol. Med. 2007;11:1185–1207. doi: 10.1111/j.1582-4934.2007.00098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Huang W, et al. DLC-1 induces mitochondrial apoptosis and epithelial mesenchymal transition arrest in nasopharyngeal carcinoma by targeting EGFR/Akt/NF-kappaB pathway. Med. Oncol. 2015;32:115. doi: 10.1007/s12032-015-0564-4. [DOI] [PubMed] [Google Scholar]
- 117.Wertz IE, et al. De-ubiquitination and ubiquitin ligase domains of A20 downregulate NF-kappaB signalling. Nature. 2004;430:694–699. doi: 10.1038/nature02794. [DOI] [PubMed] [Google Scholar]
- 118.Huang T, et al. MicroRNA-19b-3p regulates nasopharyngeal carcinoma radiosensitivity by targeting TNFAIP3/NF-kappaB axis. J. Exp. Clin. Cancer Res. 2016;35:188. doi: 10.1186/s13046-016-0465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zheng Z, et al. MiR-125b regulates proliferation and apoptosis of nasopharyngeal carcinoma by targeting A20/NF-kappaB signaling pathway. Cell Death Dis. 2017;8:e2855. doi: 10.1038/cddis.2017.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Finlin BS, et al. RERG is a novel ras-related, estrogen-regulated and growth-inhibitory gene in breast cancer. J. Biol. Chem. 2001;276:42259–42267. doi: 10.1074/jbc.M105888200. [DOI] [PubMed] [Google Scholar]
- 121.Key MD, Andres DA, Der CJ, Repasky GA. Characterization of RERG: an estrogen-regulated tumor suppressor gene. Methods Enzymol. 2006;407:513–527. doi: 10.1016/S0076-6879(05)07041-2. [DOI] [PubMed] [Google Scholar]
- 122.Zhao W, et al. RERG suppresses cell proliferation, migration and angiogenesis through ERK/NF-kappaB signaling pathway in nasopharyngeal carcinoma. J. Exp. Clin. Cancer Res. 2017;36:88. doi: 10.1186/s13046-017-0554-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hayden MS, Ghosh S. Shared principles in NF-kappaB signaling. Cell. 2008;132:344–362. doi: 10.1016/j.cell.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 124.Li, Y. J. et al. Epigallocatechin-3-gallate inhibits nasopharyngeal cancer stem cell self-renewal and migration and reverses the epithelial-mesenchymal transition via NF-kappaB p65 inactivation. Tumour Biol.36, 2747–2761 (2015). [DOI] [PubMed]
- 125.Huang YX, et al. Sunitinib induces NK-kappaB-dependent NKG2D ligand expression in nasopharyngeal carcinoma and hepatoma cells. J. Immunother. 2017;40:164–174. doi: 10.1097/CJI.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 126.Slattery ML, et al. The MAPK-signaling pathway in colorectal cancer: dysregulated genes and their association with microRNAs. Cancer Inform. 2018;17:1176935118766522. doi: 10.1177/1176935118766522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Burotto M, Chiou VL, Lee JM, Kohn EC. The MAPK pathway across different malignancies: a new perspective. Cancer. 2014;120:3446–3456. doi: 10.1002/cncr.28864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang L, et al. Genomic analysis of nasopharyngeal carcinoma reveals TME-based subtypes. Mol. Cancer Res. 2017;15:1722–1732. doi: 10.1158/1541-7786.MCR-17-0134. [DOI] [PubMed] [Google Scholar]
- 129.Li Z, Li N, Shen L. MAP2K6 is associated with radiation resistance and adverse prognosis for locally advanced nasopharyngeal carcinoma patients. Cancer Manag. Res. 2018;10:6905–6912. doi: 10.2147/CMAR.S184689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.King AJ, et al. The protein kinase Pak3 positively regulates Raf-1 activity through phosphorylation of serine 338. Nature. 1998;396:180–183. doi: 10.1038/24184. [DOI] [PubMed] [Google Scholar]
- 131.Frost JA, et al. Cross-cascade activation of ERKs and ternary complex factors by Rho family proteins. EMBO J. 1997;16:6426–6438. doi: 10.1093/emboj/16.21.6426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gallardo F, Mariame B, Gence R, Tilkin-Mariame AF. Macrocyclic lactones inhibit nasopharyngeal carcinoma cells proliferation through PAK1 inhibition and reduce in vivo tumor growth. Drug Des. Dev. Ther. 2018;12:2805–2814. doi: 10.2147/DDDT.S172538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bramham CR, Jensen KB, Proud CG. Tuning specific translation in cancer metastasis and synaptic memory: control at the MNK-eIF4E axis. Trends Biochem. Sci. 2016;41:847–858. doi: 10.1016/j.tibs.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 134.Silva RL, Wendel HG. MNK, EIF4E and targeting translation for therapy. Cell Cycle. 2008;7:553–555. doi: 10.4161/cc.7.5.5486. [DOI] [PubMed] [Google Scholar]
- 135.Zhang M, et al. Design, synthesis and biological evaluation of 4-aniline-thieno[2,3-d]pyrimidine derivatives as MNK1 inhibitors against renal cell carcinoma and nasopharyngeal carcinoma. Bioorg. Med. Chem. 2019;27:2268–2279. doi: 10.1016/j.bmc.2019.04.022. [DOI] [PubMed] [Google Scholar]
- 136.Zhang X, et al. Tumor suppressor BLU exerts growth inhibition by blocking ERK signaling and disrupting cell cycle progression through RAS pathway interference. Int. J. Clin. Exp. Pathol. 2018;11:158–168. [PMC free article] [PubMed] [Google Scholar]
- 137.Tian Y, et al. miR-483-5p decreases the radiosensitivity of nasopharyngeal carcinoma cells by targeting DAPK1. Lab. Invest. 2019;99:602–611. doi: 10.1038/s41374-018-0169-6. [DOI] [PubMed] [Google Scholar]
- 138.Du M, et al. TGF-? regulates the ERK/MAPK pathway independent of the SMAD pathway by repressing miRNA-124 to increase MALAT1 expression in nasopharyngeal carcinoma. Biomed. Pharmacother. 2018;99:688–696. doi: 10.1016/j.biopha.2018.01.120. [DOI] [PubMed] [Google Scholar]
- 139.Peng XH, et al. MiR-124 suppresses tumor growth and metastasis by targeting Foxq1 in nasopharyngeal carcinoma. Mol. Cancer. 2014;13:186. doi: 10.1186/1476-4598-13-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Narita Y, et al. Pin1 interacts with the Epstein-Barr virus DNA polymerase catalytic subunit and regulates viral DNA replication. J. Virol. 2013;87:2120–2127. doi: 10.1128/JVI.02634-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xu M, et al. Overexpression of PIN1 enhances cancer growth and aggressiveness with cyclin D1 induction in EBV-associated nasopharyngeal carcinoma. PLoS ONE. 2016;11:e0156833. doi: 10.1371/journal.pone.0156833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ayllon V, O'Connor R. PBK/TOPK promotes tumour cell proliferation through p38 MAPK activity and regulation of the DNA damage response. Oncogene. 2007;26:3451–3461. doi: 10.1038/sj.onc.1210142. [DOI] [PubMed] [Google Scholar]
- 143.Zhu F, et al. Bidirectional signals transduced by TOPK-ERK interaction increase tumorigenesis of HCT116 colorectal cancer cells. Gastroenterology. 2007;133:219–231. doi: 10.1053/j.gastro.2007.04.048. [DOI] [PubMed] [Google Scholar]
- 144.Oh SM, et al. T-lymphokine-activated killer cell-originated protein kinase functions as a positive regulator of c-Jun-NH2-kinase 1 signaling and H-Ras-induced cell transformation. Cancer Res. 2007;67:5186–5194. doi: 10.1158/0008-5472.CAN-06-4506. [DOI] [PubMed] [Google Scholar]
- 145.Wang MY, et al. PDZ binding kinase (PBK) is a theranostic target for nasopharyngeal carcinoma: driving tumor growth via ROS signaling and correlating with patient survival. Oncotarget. 2016;7:26604–26616. doi: 10.18632/oncotarget.8445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Akira S, et al. Molecular cloning of APRF, a novel IFN-stimulated gene factor 3 p91-related transcription factor involved in the gp130-mediated signaling pathway. Cell. 1994;77:63–71. doi: 10.1016/0092-8674(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 147.Gao J, et al. Targeted regulationof STAT3 by miR-29a in mediating Taxol resistance of nasopharyngeal carcinoma cell line CNE-1. Cancer Biomark. 2018;22:641–648. doi: 10.3233/CBM-170964. [DOI] [PubMed] [Google Scholar]
- 148.Li X, et al. Sulforaphane promotes apoptosis, and inhibits proliferation and self-renewal of nasopharyngeal cancer cells by targeting STAT signal through miRNA-124-3p. Biomed. Pharmacother. 2018;103:473–481. doi: 10.1016/j.biopha.2018.03.121. [DOI] [PubMed] [Google Scholar]
- 149.Liu C, Zhang H, Liu H. Long noncoding RNA UCA1 accelerates nasopharyngeal carcinoma cell progression by modulating miR-124-3p/ITGB1 axis. OncoTargets Ther. 2019;12:8455–8466. doi: 10.2147/OTT.S215819. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 150.He QY, et al. Reduction of RKIP expression promotes nasopharyngeal carcinoma invasion and metastasis by activating Stat3 signaling. Oncotarget. 2015;6:16422–16436. doi: 10.18632/oncotarget.3847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Huang W, et al. miR-181a upregulation promotes radioresistance of nasopharyngeal carcinoma by targeting RKIP. OncoTargets Ther. 2019;12:10873–10884. doi: 10.2147/OTT.S228800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Miao H, Wang B. EphA receptor signaling-complexity and emerging themes. Semin. Cell Dev. Biol. 2012;23:16–25. doi: 10.1016/j.semcdb.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhang X, Yang J, Bian Z, Shi D, Cao Z. Long noncoding RNA DANCR promotes nasopharyngeal carcinoma progression by interacting with STAT3, enhancing IL-6/JAK1/STAT3 signaling. Biomed. Pharmacother. 2019;113:108713. doi: 10.1016/j.biopha.2019.108713. [DOI] [PubMed] [Google Scholar]
- 154.Liu SC, et al. Ovatodiolide suppresses nasopharyngeal cancer by targeting stem cell-like population, inducing apoptosis, inhibiting EMT and dysregulating JAK/STAT signaling pathway. Phytomedicine. 2019;56:269–278. doi: 10.1016/j.phymed.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 155.Clevers H, Nusse R. Wnt/beta-catenin signaling and disease. Cell. 2012;149:1192–1205. doi: 10.1016/j.cell.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 156.Reya T, Clevers H. Wnt signalling in stem cells and cancer. Nature. 2005;434:843–850. doi: 10.1038/nature03319. [DOI] [PubMed] [Google Scholar]
- 157.Guan Z, et al. SOX1 down-regulates beta-catenin and reverses malignant phenotype in nasopharyngeal carcinoma. Mol. Cancer. 2014;13:257. doi: 10.1186/1476-4598-13-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chan SL, et al. The tumor suppressor Wnt inhibitory factor 1 is frequently methylated in nasopharyngeal and esophageal carcinomas. Lab. Invest. 2007;87:644–650. doi: 10.1038/labinvest.3700547. [DOI] [PubMed] [Google Scholar]
- 159.Cui C, Zhou X, Zhang W, Qu Y, Ke X. Is beta-catenin a druggable target for cancer therapy? Trends Biochem. Sci. 2018;43:623–634. doi: 10.1016/j.tibs.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 160.Li S, et al. Manganese superoxide dismutase mediates anoikis resistance and tumor metastasis in nasopharyngeal carcinoma. Oncotarget. 2016;7:32408–32420. doi: 10.18632/oncotarget.8717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cai CF, et al. Anti-oncogenic activity of Chibby in the development of human nasopharyngeal carcinoma. Oncol. Lett. 2018;15:5849–5858. doi: 10.3892/ol.2018.8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wan FZ, et al. Exosomes overexpressing miR-34c inhibit malignant behavior and reverse the radioresistance of nasopharyngeal carcinoma. J. Transl. Med. 2020;18:12. doi: 10.1186/s12967-019-02203-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhuang Q, et al. Capn4 mRNA level is correlated with tumour progression and clinical outcome in clear cell renal cell carcinoma. J. Int. Med. Res. 2014;42:282–291. doi: 10.1177/0300060513505524. [DOI] [PubMed] [Google Scholar]
- 164.Bai DS, et al. Capn4 overexpression underlies tumor invasion and metastasis after liver transplantation for hepatocellular carcinoma. Hepatology. 2009;49:460–470. doi: 10.1002/hep.22638. [DOI] [PubMed] [Google Scholar]
- 165.Zheng PC, et al. Capn4 is a marker of poor clinical outcomes and promotes nasopharyngeal carcinoma metastasis via nuclear factor-kappaB-induced matrix metalloproteinase 2 expression. Cancer Sci. 2014;105:630–638. doi: 10.1111/cas.12416. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 166.Hu H, Wang G, Li C. miR-124 suppresses proliferation and invasion of nasopharyngeal carcinoma cells through the Wnt/beta-catenin signaling pathway by targeting Capn4. OncoTargets Ther. 2017;10:2711–2720. doi: 10.2147/OTT.S135563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Niehrs C. The complex world of WNT receptor signalling. Nat. Rev. Mol. Cell Biol. 2012;13:767–779. doi: 10.1038/nrm3470. [DOI] [PubMed] [Google Scholar]
- 168.Huang Y, et al. miR-150 contributes to the radioresistance in nasopharyngeal carcinoma cells by targeting glycogen synthase kinase-3beta. J. Cancer Res. Ther. 2018;14:111–118. doi: 10.4103/jcrt.JCRT_682_17. [DOI] [PubMed] [Google Scholar]
- 169.Teo JL, Kahn M. The Wnt signaling pathway in cellular proliferation and differentiation: A tale of two coactivators. Adv. Drug Deliv. Rev. 2010;62:1149–1155. doi: 10.1016/j.addr.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 170.Zeng ZY, et al. Gene expression profiling of nasopharyngeal carcinoma reveals the abnormally regulated Wnt signaling pathway. Hum. Pathol. 2007;38:120–133. doi: 10.1016/j.humpath.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 171.Chan KC, et al. Therapeutic targeting of CBP/beta-catenin signaling reduces cancer stem-like population and synergistically suppresses growth of EBV-positive nasopharyngeal carcinoma cells with cisplatin. Sci. Rep. 2015;5:9979. doi: 10.1038/srep09979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Liang TS, et al. MicroRNA-506 inhibits tumor growth and metastasis in nasopharyngeal carcinoma through the inactivation of the Wnt/beta-catenin signaling pathway by down-regulating LHX2. J. Exp. Clin. Cancer Res. 2019;38:97. doi: 10.1186/s13046-019-1023-4. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 173.Luo M, et al. FOXO3a knockdown promotes radioresistance in nasopharyngeal carcinoma by inducing epithelial-mesenchymal transition and the Wnt/beta-catenin signaling pathway. Cancer Lett. 2019;455:26–35. doi: 10.1016/j.canlet.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 174.Xu MJ, Johnson DE, Grandis JR. EGFR-targeted therapies in the post-genomic era. Cancer Metastasis Rev. 2017;36:463–473. doi: 10.1007/s10555-017-9687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Gu J, et al. Cetuximab and cisplatin show different combination effect in nasopharyngeal carcinoma cells lines via inactivation of EGFR/AKT signaling pathway. Biochem. Res. Int. 2016;2016:7016907. doi: 10.1155/2016/7016907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Zheng LS, et al. SPINK6 promotes metastasis of nasopharyngeal carcinoma via binding and activation of epithelial growth factor receptor. Cancer Res. 2017;77:579–589. doi: 10.1158/0008-5472.CAN-16-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Huang J, et al. Intensity-modulated radiotherapy plus nimotuzumab with or without concurrent chemotherapy for patients with locally advanced nasopharyngeal carcinoma. OncoTargets Ther. 2017;10:5835–5841. doi: 10.2147/OTT.S151554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zhai RP, et al. Experience with combination of nimotuzumab and intensity-modulated radiotherapy in patients with locoregionally advanced nasopharyngeal carcinoma. OncoTargets Ther. 2015;8:3383–3390. doi: 10.2147/OTT.S93238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shen J, Sun C, Zhou M, Zhang Z. Combination treatment with cetuximab in advanced nasopharyngeal carcinoma patients: a meta-analysis. OncoTargets Ther. 2019;12:2477–2494. doi: 10.2147/OTT.S193039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sun XS, et al. Palliative chemotherapy with or without anti-EGFR therapy for de novo metastatic nasopharyngeal carcinoma: a propensity score-matching study. Drug Des. Dev. Ther. 2019;13:3207–3216. doi: 10.2147/DDDT.S215190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Harmey, J. H. VEGF and Cancer. Landes Bioscience/Eurekah.com (Kluwer Academic/Plenum Publishers, New York, N.Y., 2004).
- 182.Yue B, et al. Knockdown of neuropilin-1 suppresses invasion, angiogenesis, and increases the chemosensitivity to doxorubicin in osteosarcoma cells - an in vitro study. Eur. Rev. Med. Pharmacol. Sci. 2014;18:1735–1741. [PubMed] [Google Scholar]
- 183.Sun J, et al. Construction and identification of small hairpin RNA plasmids targeting neuropilin-1 gene and their inhibitory effect on human nasopharyngeal carcinoma CNE-2Z cell proliferation in vitro and in vivo. Eur. Arch. Oto-Rhino-Laryngol. 2016;273:2541–2547. doi: 10.1007/s00405-015-3873-5. [DOI] [PubMed] [Google Scholar]
- 184.Fu WM, et al. Long noncoding RNA hotair mediated angiogenesis in nasopharyngeal carcinoma by direct and indirect signaling pathways. Oncotarget. 2016;7:4712–4723. doi: 10.18632/oncotarget.6731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Feng X, Lv W, Wang S, He Q. miR495 enhances the efficacy of radiotherapy by targeting GRP78 to regulate EMT in nasopharyngeal carcinoma cells. Oncol. Rep. 2018;40:1223–1232. doi: 10.3892/or.2018.6538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Li J, et al. Bevacizumab plus cisplatin and helical tomotherapy in treatment of locally advanced nasopharyngeal carcinoma. OncoTargets Ther. 2015;8:1315–1319. doi: 10.2147/OTT.S80159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Lin JH, Walter P, Yen TS. Endoplasmic reticulum stress in disease pathogenesis. Annu Rev. Pathol. 2008;3:399–425. doi: 10.1146/annurev.pathmechdis.3.121806.151434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Gray MD, Mann M, Nitiss JL, Hendershot LM. Activation of the unfolded protein response is necessary and sufficient for reducing topoisomerase IIalpha protein levels and decreasing sensitivity to topoisomerase-targeted drugs. Mol. Pharmacol. 2005;68:1699–1707. doi: 10.1124/mol.105.014753. [DOI] [PubMed] [Google Scholar]
- 189.Obeng EA, et al. Proteasome inhibitors induce a terminal unfolded protein response in multiple myeloma cells. Blood. 2006;107:4907–4916. doi: 10.1182/blood-2005-08-3531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Wang G, et al. Combined effects of Lenvatinib and iodine-131 on cell apoptosis in nasopharyngeal carcinoma through inducing endoplasmic reticulum stress. Exp. Ther. Med. 2018;16:3325–3332. doi: 10.3892/etm.2018.6652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Pan Y, et al. A novel curcuminoid exhibits enhanced antitumor activity in nasopharyngeal carcinoma. Int. J. Oncol. 2016;48:2175–2183. doi: 10.3892/ijo.2016.3425. [DOI] [PubMed] [Google Scholar]
- 192.Lin, Y. J. et al. Tetrandrine induces apoptosis of human nasopharyngeal carcinoma NPC-TW 076 cells through reactive oxygen species accompanied by an endoplasmic reticulum stress signaling pathway. Molecules21, 1353 (2016). [DOI] [PMC free article] [PubMed]
- 193.Zhao F, et al. MiR-20a-5p promotes radio-resistance by targeting NPAS2 in nasopharyngeal cancer cells. Oncotarget. 2017;8:105873–105881. doi: 10.18632/oncotarget.22411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ostenfeld MS, et al. Cellular disposal of miR23b by RAB27-dependent exosome release is linked to acquisition of metastatic properties. Cancer Res. 2014;74:5758–5771. doi: 10.1158/0008-5472.CAN-13-3512. [DOI] [PubMed] [Google Scholar]
- 195.Huang D, et al. MiR-20a-5p promotes radio-resistance by targeting Rab27B in nasopharyngeal cancer cells. Cancer Cell Int. 2017;17:32. doi: 10.1186/s12935-017-0389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Colak S, Ten Dijke P. Targeting TGF-beta signaling in cancer. Trends Cancer. 2017;3:56–71. doi: 10.1016/j.trecan.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 197.Chen CY, et al. Targeting annexin A2 reduces tumorigenesis and therapeutic resistance of nasopharyngeal carcinoma. Oncotarget. 2015;6:26946–26959. doi: 10.18632/oncotarget.4521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Wang J, et al. Berberine sensitizes nasopharyngeal carcinoma cells to radiation through inhibition of Sp1 and EMT. Oncol. Rep. 2017;37:2425–2432. doi: 10.3892/or.2017.5499. [DOI] [PubMed] [Google Scholar]
- 199.Rankin EB, Giaccia AJ. The role of hypoxia-inducible factors in tumorigenesis. Cell Death Differ. 2008;15:678–685. doi: 10.1038/cdd.2008.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Chen Y, et al. Nanoformulation of d-alpha-tocopheryl polyethylene glycol 1000 succinate-b-poly(epsilon-caprolactone-ran-glycolide) diblock copolymer for siRNA targeting HIF-1alpha for nasopharyngeal carcinoma therapy. Int. J. Nanomed. 2015;10:1375–1386. doi: 10.2217/nnm.15.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lyu X, et al. EBV-miR-BART1-5P activates AMPK/mTOR/HIF1 pathway via a PTEN independent manner to promote glycolysis and angiogenesis in nasopharyngeal carcinoma. PLoS Pathog. 2018;14:e1007484. doi: 10.1371/journal.ppat.1007484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhang J, et al. SKF95365 induces apoptosis and cell-cycle arrest by disturbing oncogenic Ca(2+) signaling in nasopharyngeal carcinoma cells. OncoTargets Ther. 2015;8:3123–3133. doi: 10.2147/OTT.S92005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Huang W, et al. Inhibition of store-operated Ca(2+) entry counteracts the apoptosis of nasopharyngeal carcinoma cells induced by sodium butyrate. Oncol. Lett. 2017;13:921–929. doi: 10.3892/ol.2016.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Mo L, et al. WWOX suppresses proliferation and induces apoptosis via G2 arrest and caspase 3 pathway in nasopharyngeal carcinoma cells. Int. J. Clin. Exp. Pathol. 2017;10:11526–11535. [PMC free article] [PubMed] [Google Scholar]
- 205.Hu X, Jiang H, Jiang X. Downregulation of lncRNA ANRIL inhibits proliferation, induces apoptosis, and enhances radiosensitivity in nasopharyngeal carcinoma cells through regulating miR-125a. Cancer Biol. Ther. 2017;18:331–338. doi: 10.1080/15384047.2017.1310348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Han Q, et al. Downregulation of lncRNA X inactive specific transcript (XIST) suppresses cell proliferation and enhances radiosensitivity by upregulating mir-29c in nasopharyngeal carcinoma cells. Med. Sci. Monit. 2017;23:4798–4807. doi: 10.12659/MSM.905370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Liu F, Tai Y, Ma J. LncRNA NEAT1/let-7a-5p axis regulates the cisplatin resistance in nasopharyngeal carcinoma by targeting Rsf-1 and modulating the Ras-MAPK pathway. Cancer Biol. Ther. 2018;19:534–542. doi: 10.1080/15384047.2018.1450119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Miao WJ, et al. lncRNA CASC2/miR18a5p axis regulates the malignant potential of nasopharyngeal carcinoma by targeting RBBP8. Oncol. Rep. 2019;41:1797–1806. doi: 10.3892/or.2018.6941. [DOI] [PubMed] [Google Scholar]
- 209.Zhang HQ, et al. The expression of microRNA-324-3p as a tumor suppressor in nasopharyngeal carcinoma and its clinical significance. OncoTargets Ther. 2017;10:4935–4943. doi: 10.2147/OTT.S144223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Feng S, et al. Curcumin exerts its antitumor activity through regulation of miR-7/Skp2/p21 in nasopharyngeal carcinoma cells. OncoTargets Ther. 2017;10:2377–2388. doi: 10.2147/OTT.S130055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Jiang C, et al. MicroRNA-212 inhibits the metastasis of nasopharyngeal carcinoma by targeting SOX4. Oncol. Rep. 2017;38:82–88. doi: 10.3892/or.2017.5641. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 212.Wang T, et al. MicroRNA-432 suppresses invasion and migration via E2F3 in nasopharyngeal carcinoma. OncoTargets Ther. 2019;12:11271–11280. doi: 10.2147/OTT.S233435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Wu M, et al. Upregulation of metastasis-associated gene 2 promotes cell proliferation and invasion in nasopharyngeal carcinoma. OncoTargets Ther. 2016;9:1647–1656. doi: 10.2147/OTT.S96518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Tang XR, et al. MicroRNA-101 inhibits invasion and angiogenesis through targeting ITGA3 and its systemic delivery inhibits lung metastasis in nasopharyngeal carcinoma. Cell death Dis. 2017;8:e2566. doi: 10.1038/cddis.2016.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Li, X. et al. miR150 inhibits proliferation and tumorigenicity via retarding G1/S phase transition in nasopharyngeal carcinoma. Int. J. Oncol.10.3892/ijo.2017.3909 (2017). [DOI] [PMC free article] [PubMed]
- 216.He S, et al. HMG-box transcription factor 1: a positive regulator of the G1/S transition through the Cyclin-CDK-CDKI molecular network in nasopharyngeal carcinoma. Cell Death Dis. 2018;9:100. doi: 10.1038/s41419-017-0175-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Xu J, Ai Q, Cao H, Liu Q. MiR-185-3p and miR-324-3p predict radiosensitivity of nasopharyngeal carcinoma and modulate cancer cell growth and apoptosis by targeting SMAD7. Med. Sci. Monit. 2015;21:2828–2836. doi: 10.12659/MSM.895660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Su X, Li G, Liu W. The long noncoding RNA cancer susceptibility candidate 9 promotes nasopharyngeal carcinogenesis via stabilizing HIF1alpha. DNA Cell Biol. 2017;36:394–400. doi: 10.1089/dna.2016.3615. [DOI] [PubMed] [Google Scholar]
- 219.Wu J, et al. Long noncoding RNA UCA1 promotes the proliferation, invasion, and migration of nasopharyngeal carcinoma cells via modulation of miR-145. OncoTargets Ther. 2018;11:7483–7492. doi: 10.2147/OTT.S182290. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 220.Yiu, S. P. T. et al. Autophagy-dependent reactivation of epstein-barr virus lytic cycle and combinatorial effects of autophagy-dependent and independent lytic inducers in nasopharyngeal carcinoma. Cancers. 11, 1871 (2019). [DOI] [PMC free article] [PubMed]
- 221.Tang Y, et al. Co-expression of AFAP1-AS1 and PD-1 predicts poor prognosis in nasopharyngeal carcinoma. Oncotarget. 2017;8:39001–39011. doi: 10.18632/oncotarget.16545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Li Y, et al. Dinitrosopiperazine-decreased PKP3 through upregulating miR-149 participates in nasopharyngeal carcinoma metastasis. Mol. Carcinog. 2018;57:1763–1779. doi: 10.1002/mc.22895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Limbo O, et al. Ctp1 is a cell-cycle-regulated protein that functions with Mre11 complex to control double-strand break repair by homologous recombination. Mol. Cell. 2007;28:134–146. doi: 10.1016/j.molcel.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Wang SS, et al. Triptonide inhibits human nasopharyngeal carcinoma cell growth via disrupting Lnc-RNA THOR-IGF2BP1 signaling. Cancer Lett. 2019;443:13–24. doi: 10.1016/j.canlet.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 225.Shi L, Yin W, Zhang Z, Shi G. Down-regulation of miR-26b induces cisplatin resistance in nasopharyngeal carcinoma by repressing JAG1. FEBS Open Biol. 2016;6:1211–1219. doi: 10.1002/2211-5463.12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ma X, et al. LncRNA ANCR promotes proliferation and radiation resistance of nasopharyngeal carcinoma by inhibiting PTEN expression. OncoTargets Ther. 2018;11:8399–8408. doi: 10.2147/OTT.S182573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Jin C, Yan B, Lu Q, Lin Y, Ma L. The role of MALAT1/miR-1/slug axis on radioresistance in nasopharyngeal carcinoma. Tumour Biol. 2016;37:4025–4033. doi: 10.1007/s13277-015-4227-z. [DOI] [PubMed] [Google Scholar]
- 228.He Y, et al. Long non-coding RNA PVT1 predicts poor prognosis and induces radioresistance by regulating DNA repair and cell apoptosis in nasopharyngeal carcinoma. Cell Death Dis. 2018;9:235. doi: 10.1038/s41419-018-0265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gao W, et al. MicroRNA-138-5p controls sensitivity of nasopharyngeal carcinoma to radiation by targeting EIF4EBP1. Oncol. Rep. 2017;37:913–920. doi: 10.3892/or.2017.5354. [DOI] [PubMed] [Google Scholar]
- 230.Sun Q, et al. MiR-101 sensitizes human nasopharyngeal carcinoma cells to radiation by targeting stathmin 1. Mol. Med. Rep. 2015;11:3330–3336. doi: 10.3892/mmr.2015.3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Zhao L, et al. miR-504 mediated down-regulation of nuclear respiratory factor 1 leads to radio-resistance in nasopharyngeal carcinoma. Oncotarget. 2015;6:15995–16018. doi: 10.18632/oncotarget.4138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Chua DT, et al. Phase II study of gefitinib for the treatment of recurrent and metastatic nasopharyngeal carcinoma. Head. Neck. 2008;30:863–867. doi: 10.1002/hed.20792. [DOI] [PubMed] [Google Scholar]
- 233.Zhao C, et al. Anti-epidermal growth factor receptor (EGFR) monoclonal antibody combined with cisplatin and 5-fluorouracil in patients with metastatic nasopharyngeal carcinoma after radical radiotherapy: a multicentre, open-label, phase II clinical trial. Ann. Oncol. 2019;30:637–643. doi: 10.1093/annonc/mdz020. [DOI] [PubMed] [Google Scholar]
- 234.Zhang S, et al. An open-label, single-arm phase II clinical study of induction chemotherapy and sequential Nimotuzumab combined with concurrent chemoradiotherapy in N3M0 stage nasopharyngeal carcinoma. J. Buon. 2018;23:1656–1661. [PubMed] [Google Scholar]
- 235.Zhang X, et al. A phase II clinical trial of concurrent helical tomotherapy plus cetuximab followed by adjuvant chemotherapy with cisplatin and docetaxel for locally advanced nasopharyngeal carcinoma. Int. J. Biol. Sci. 2016;12:446–453. doi: 10.7150/ijbs.12937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Xu T, et al. Weekly cetuximab concurrent with IMRT aggravated radiation-induced oral mucositis in locally advanced nasopharyngeal carcinoma: results of a randomized phase II study. Oral. Oncol. 2015;51:875–879. doi: 10.1016/j.oraloncology.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 237.Wu RR, et al. Phase II clinical trial of h-R3 combined with radiotherapy in locally advanced nasopharyngeal carcinoma. J. Buon. 2014;19:930–936. [PubMed] [Google Scholar]
- 238.Lee NY, et al. Addition of bevacizumab to standard chemoradiation for locoregionally advanced nasopharyngeal carcinoma (RTOG 0615): a phase 2 multi-institutional trial. Lancet Oncol. 2012;13:172–180. doi: 10.1016/S1470-2045(11)70303-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Xu Y, et al. Bevacizumab monotherapy reduces radiation-induced brain necrosis in nasopharyngeal carcinoma patients: a randomized controlled trial. Int. J. Radiat. Oncol. Biol. Phys. 2018;101:1087–1095. doi: 10.1016/j.ijrobp.2018.04.068. [DOI] [PubMed] [Google Scholar]
- 240.Hui EP, et al. Efficacy, safety, and pharmacokinetics of axitinib in nasopharyngeal carcinoma: a preclinical and phase II correlative study. Clin. Cancer Res. 2018;24:1030–1037. doi: 10.1158/1078-0432.CCR-17-1667. [DOI] [PubMed] [Google Scholar]
- 241.Huang Y, et al. Phase I dose-escalation study of aflibercept plus docetaxel in nasopharyngeal carcinoma and other solid tumors. Future Oncol. 2014;10:2579–2591. doi: 10.2217/fon.14.206. [DOI] [PubMed] [Google Scholar]
- 242.Ma BB, et al. Multicenter phase II study of the AKT inhibitor MK-2206 in recurrent or metastatic nasopharyngeal carcinoma from patients in the mayo phase II consortium and the cancer therapeutics research group (MC1079) Invest. New Drugs. 2015;33:985–991. doi: 10.1007/s10637-015-0264-0. [DOI] [PubMed] [Google Scholar]
- 243.Chen Q, et al. Famitinib in combination with concurrent chemoradiotherapy in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 1, open-label, dose-escalation Study. Cancer Commun. 2018;38:66. doi: 10.1186/s40880-018-0330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Hui EP, et al. Hemorrhagic complications in a phase II study of sunitinib in patients of nasopharyngeal carcinoma who has previously received high-dose radiation. Ann. Oncol. 2011;22:1280–1287. doi: 10.1093/annonc/mdq629. [DOI] [PubMed] [Google Scholar]
- 245.Elser C, et al. Phase II trial of sorafenib in patients with recurrent or metastatic squamous cell carcinoma of the head and neck or nasopharyngeal carcinoma. J. Clin. Oncol. 2007;25:3766–3773. doi: 10.1200/JCO.2006.10.2871. [DOI] [PubMed] [Google Scholar]
- 246.Xue C, et al. Phase II study of sorafenib in combination with cisplatin and 5-fluorouracil to treat recurrent or metastatic nasopharyngeal carcinoma. Ann. Oncol. 2013;24:1055–1061. doi: 10.1093/annonc/mds581. [DOI] [PubMed] [Google Scholar]
- 247.Jin T, Li B, Chen XZ. A phase II trial of Endostar combined with gemcitabine and cisplatin chemotherapy in patients with metastatic nasopharyngeal carcinoma ( NCT01612286) Oncol. Res. 2013;21:317–323. doi: 10.3727/096504014X13983417587401. [DOI] [PubMed] [Google Scholar]
- 248.Kang M, Wang F, Liao X, Zhou P, Wang R. Intensity-modulated radiotherapy combined with endostar has similar efficacy but weaker acute adverse reactions than IMRT combined with chemotherapy in the treatment of locally advanced nasopharyngeal carcinoma. Medicine. 2018;97:e11118. doi: 10.1097/MD.0000000000011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Yu JH, Chen L, Yu JY, Luo HQ, Wang L. PI3K-PKB-mTOR hyperactivation in relation to nasopharyngeal carcinoma progression and prognosis. J. Cell Biochem. 2019;120:10186–10194. doi: 10.1002/jcb.28303. [DOI] [PubMed] [Google Scholar]
- 250.Chen J, et al. Epstein-Barr virus encoded latent membrane protein 1 regulates mTOR signaling pathway genes which predict poor prognosis of nasopharyngeal carcinoma. J. Transl. Med. 2010;8:30–30. doi: 10.1186/1479-5876-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Chen Y-P, et al. Effect of latent membrane protein 1 expression on overall survival in Epstein-Barr virus-associated cancers: a literature-based meta-analysis. Oncotarget. 2015;6:29311–29323. doi: 10.18632/oncotarget.4906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Feng J, et al. Elevated HSP90 associates with expression of HIF-1α and p-AKT and is predictive of poor prognosis in nasopharyngeal carcinoma. Histopathology. 2019;75:202–212. doi: 10.1111/his.13862. [DOI] [PubMed] [Google Scholar]
- 253.Tong Y-Q, et al. BMI-1 autoantibody in serum as a new potential biomarker of nasopharyngeal carcinoma. Cancer Biol. Ther. 2008;7:340–344. doi: 10.4161/cbt.7.3.5422. [DOI] [PubMed] [Google Scholar]
- 254.Kuang C-M, et al. BST2 confers cisplatin resistance via NF-κB signaling in nasopharyngeal cancer. Cell Death Dis. 2017;8:e2874–e2874. doi: 10.1038/cddis.2017.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Xu Y, et al. Prognostic implication of neuropilin-1 upregulation in human nasopharyngeal carcinoma. Diagn. Pathol. 2013;8:155. doi: 10.1186/1746-1596-8-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Zheng J, et al. Phosphorylated Mnk1 and eIF4E are associated with lymph node metastasis and poor prognosis of nasopharyngeal carcinoma. PLoS ONE. 2014;9:e89220–e89220. doi: 10.1371/journal.pone.0089220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Tian F, et al. Promoter hypermethylation of tumor suppressor genes in serum as potential biomarker for the diagnosis of nasopharyngeal carcinoma. Cancer Epidemiol. 2013;37:708–713. doi: 10.1016/j.canep.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 258.Luo Z, et al. miR-18a promotes malignant progression by impairing microRNA biogenesis in nasopharyngeal carcinoma. Carcinogenesis. 2013;34:415–425. doi: 10.1093/carcin/bgs329. [DOI] [PubMed] [Google Scholar]
- 259.Xu X, et al. Dynamic changes in plasma MicroRNAs have potential predictive values in monitoring recurrence and metastasis of nasopharyngeal carcinoma. Biomed. Res. Int. 2018;2018:7329195. doi: 10.1155/2018/7329195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Nie Y, et al. Long non-coding RNA HOTAIR is an independent prognostic marker for nasopharyngeal carcinoma progression and survival. Cancer Sci. 2013;104:458–464. doi: 10.1111/cas.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Zou ZW, et al. LncRNA ANRIL is up-regulated in nasopharyngeal carcinoma and promotes the cancer progression via increasing proliferation, reprograming cell glucose metabolism and inducing side-population stem-like cancer cells. Oncotarget. 2016;7:61741–61754. doi: 10.18632/oncotarget.11437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Cheng A-L, et al. Identification of novel nasopharyngeal carcinoma biomarkers by laser capture microdissection and proteomic analysis. Clin. Cancer Res. 2008;14:435–445. doi: 10.1158/1078-0432.CCR-07-1215. [DOI] [PubMed] [Google Scholar]
- 263.Zeng G-Q, et al. Annexin A1: a new biomarker for predicting nasopharyngeal carcinoma response to radiotherapy. Med. Hypotheses. 2013;81:68–70. doi: 10.1016/j.mehy.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 264.Chang S-L, et al. CDKN3 expression is an independent prognostic factor and associated with advanced tumor stage in nasopharyngeal carcinoma. Int J. Med Sci. 2018;15:992–998. doi: 10.7150/ijms.25065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Luo W, et al. Embryonic stem cells markers SOX2, OCT4 and Nanog expression and their correlations with epithelial-mesenchymal transition in nasopharyngeal carcinoma. PLoS ONE. 2013;8:e56324. doi: 10.1371/journal.pone.0056324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Huang T, et al. TNFAIP3 inhibits migration and invasion in nasopharyngeal carcinoma by suppressing epithelial mesenchymal transition. Neoplasma. 2017;64:389–394. doi: 10.4149/neo_2017_309. [DOI] [PubMed] [Google Scholar]
- 267.Xu, Y. et al. Combination of RERG and ZNF671 methylation rates in ccfDNA: a novel biomarker for screening of nasopharyngeal carcinoma. Cancer Sci.10.1111/cas.14431 (2020). [DOI] [PMC free article] [PubMed]
- 268.Hsiao JR, et al. Constitutive activation of STAT3 and STAT5 is present in the majority of nasopharyngeal carcinoma and correlates with better prognosis. Br. J. Cancer. 2003;89:344–349. doi: 10.1038/sj.bjc.6601003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Wen X, et al. Long non-coding RNA DANCR stabilizes HIF-1α and promotes metastasis by interacting with NF90/NF45 complex in nasopharyngeal carcinoma. Theranostics. 2018;8:5676–5689. doi: 10.7150/thno.28538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Qiu F, et al. miR-29a/b enhances cell migration and invasion in nasopharyngeal carcinoma progression by regulating SPARC and COL3A1 gene expression. PLoS ONE. 2015;10:e0120969. doi: 10.1371/journal.pone.0120969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Pang Q, Hu W, Zhang X, Pang M. Wnt/β-catenin signaling pathway-related proteins (DKK-3, β-catenin, and c-MYC) are involved in prognosis of nasopharyngeal carcinoma. Cancer Biother. Radiopharm. 2019;34:436–443. doi: 10.1089/cbr.2019.2771. [DOI] [PubMed] [Google Scholar]
- 272.Zheng P-C, et al. Capn4 is a marker of poor clinical outcomes and promotes nasopharyngeal carcinoma metastasis via nuclear factor-κB-induced matrix metalloproteinase 2 expression. Cancer Sci. 2014;105:630–638. doi: 10.1111/cas.12416. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 273.Wong CH, et al. Preclinical evaluation of the PI3K-mTOR dual inhibitor PF-04691502 as a novel therapeutic drug in nasopharyngeal carcinoma. Invest. New Drugs. 2013;31:1399–1408. doi: 10.1007/s10637-013-0007-z. [DOI] [PubMed] [Google Scholar]
- 274.Liu R, et al. Brevilin A induces cell cycle arrest and apoptosis in nasopharyngeal carcinoma. Front. Pharmacol. 2019;10:594. doi: 10.3389/fphar.2019.00594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Huang Y, et al. Efficacy of the hypoxia-activated prodrug evofosfamide (TH-302) in nasopharyngeal carcinoma in vitro and in vivo. Cancer Commun. 2018;38:15. doi: 10.1186/s40880-018-0285-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Ma L, et al. Cancer stem-like cell properties are regulated by EGFR/AKT/β-catenin signaling and preferentially inhibited by gefitinib in nasopharyngeal carcinoma. FEBS J. 2013;280:2027–2041. doi: 10.1111/febs.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Siva Sankar P, et al. Modeling nasopharyngeal carcinoma in three dimensions. Oncol. Lett. 2017;13:2034–2044. doi: 10.3892/ol.2017.5697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Beaumont KA, Mohana-Kumaran N, Haass NK. Modeling melanoma in vitro and in vivo. Healthcare. 2013;2:27–46. doi: 10.3390/healthcare2010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Loessner D, et al. Bioengineered 3D platform to explore cell-ECM interactions and drug resistance of epithelial ovarian cancer cells. Biomaterials. 2010;31:8494–8506. doi: 10.1016/j.biomaterials.2010.07.064. [DOI] [PubMed] [Google Scholar]
- 280.Goodman TT, Ng CP, Pun SH. 3-D tissue culture systems for the evaluation and optimization of nanoparticle-based drug carriers. Bioconjug. Chem. 2008;19:1951–1959. doi: 10.1021/bc800233a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Wang WJ, et al. MYC regulation of CHK1 and CHK2 promotes radioresistance in a stem cell-like population of nasopharyngeal carcinoma cells. Cancer Res. 2013;73:1219–1231. doi: 10.1158/0008-5472.CAN-12-1408. [DOI] [PubMed] [Google Scholar]
- 282.Lui VW, et al. Anti-invasion, anti-proliferation and anoikis-sensitization activities of lapatinib in nasopharyngeal carcinoma cells. Invest. New Drugs. 2011;29:1241–1252. doi: 10.1007/s10637-010-9470-y. [DOI] [PubMed] [Google Scholar]
- 283.Li M, Izpisua Belmonte JC. Organoids—preclinical models of human disease. N. Engl. J. Med. 2019;380:569–579. doi: 10.1056/NEJMra1806175. [DOI] [PubMed] [Google Scholar]
- 284.Drost J, Clevers H. Organoids in cancer research. Nat. Rev. Cancer. 2018;18:407–418. doi: 10.1038/s41568-018-0007-6. [DOI] [PubMed] [Google Scholar]
- 285.He, J. et al. Organoid technology for tissue engineering. J. Mol. Cell Biol. 10.1093/jmcb/mjaa012 (2020). [DOI] [PMC free article] [PubMed]
- 286.Wang XW, et al. Establishment and application of nasopharyngeal carcinoma organoid disease model. Acta. Acad. Med. Mil. Tert. 2020;42:1371–1379. [Google Scholar]
- 287.Sachs N, et al. A living biobank of breast cancer organoids captures disease heterogeneity. Cell. 2018;172:373–386. doi: 10.1016/j.cell.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 288.Dorn CR, Priester WA. Epidemiologic analysis of oral and pharyngeal cancer in dogs, cats, horses, and cattle. J. Am. Vet. Med. Assoc. 1976;169:1202–1206. [PubMed] [Google Scholar]
- 289.Lin MC, Lin YC, Chen ST, Young TH, Lou PJ. Therapeutic vaccine targeting Epstein-Barr virus latent protein, LMP1, suppresses LMP1-expressing tumor growth and metastasis in vivo. BMC Cancer. 2017;17:18. doi: 10.1186/s12885-016-3027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Yip YL, et al. Establishment of a nasopharyngeal carcinoma cell line capable of undergoing lytic Epstein-Barr virus reactivation. Lab. Invest. 2018;98:1093–1104. doi: 10.1038/s41374-018-0034-7. [DOI] [PubMed] [Google Scholar]
- 291.Cai L, et al. Epstein-Barr virus-encoded microRNA BART1 induces tumour metastasis by regulating PTEN-dependent pathways in nasopharyngeal carcinoma. Nat. Commun. 2015;6:7353. doi: 10.1038/ncomms8353. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 292.Wei J, et al. Blockage of LMP1-modulated store-operated Ca(2+) entry reduces metastatic potential in nasopharyngeal carcinoma cell. Cancer Lett. 2015;360:234–244. doi: 10.1016/j.canlet.2015.02.032. [DOI] [PubMed] [Google Scholar]
- 293.de Jong M, Essers J, van Weerden WM. Imaging preclinical tumour models: improving translational power. Nat. Rev. Cancer. 2014;14:481–493. doi: 10.1038/nrc3751. [DOI] [PubMed] [Google Scholar]
- 294.Hoffman RM. Patient-derived orthotopic xenografts: better mimic of metastasis than subcutaneous xenografts. Nat. Rev. Cancer. 2015;15:451–452. doi: 10.1038/nrc3972. [DOI] [PubMed] [Google Scholar]
- 295.Richmond A, Su Y. Mouse xenograft models vs GEM models for human cancer therapeutics. Dis. Model Mech. 2008;1:78–82. doi: 10.1242/dmm.000976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Merlino G, et al. Meeting report: the future of preclinical mouse models in melanoma treatment is now. Pigment Cell Melanoma Res. 2013;26:E8–E14. doi: 10.1111/pcmr.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Busson P, et al. Establishment and characterization of three transplantable EBV-containing nasopharyngeal carcinomas. Int. J. Cancer. 1988;42:599–606. doi: 10.1002/ijc.2910420422. [DOI] [PubMed] [Google Scholar]
- 298.Hsu CL, et al. Integrated genomic analyses in PDX model reveal a cyclin-dependent kinase inhibitor Palbociclib as a novel candidate drug for nasopharyngeal carcinoma. J. Exp. Clin. Cancer Res. 2018;37:233. doi: 10.1186/s13046-018-0873-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Zhao C-X, et al. The regulatory network of nasopharyngeal carcinoma metastasis with a focus on EBV, lncRNAs and miRNAs. Am. J. Cancer Res. 2018;8:2185–2209. [PMC free article] [PubMed] [Google Scholar]
- 300.Wei P, et al. Cancer stem-like cell: a novel target for nasopharyngeal carcinoma therapy. Stem Cell Res. Ther. 2014;5:44. doi: 10.1186/scrt433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Ye X, Weinberg RA. Epithelial-mesenchymal plasticity: a central regulator of cancer progression. Trends Cell Biol. 2015;25:675–686. doi: 10.1016/j.tcb.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 303.Ribatti D, Tamma R, Annese T. Epithelial-mesenchymal transition in cancer: a historical overview. Transl. Oncol. 2020;13:100773. doi: 10.1016/j.tranon.2020.100773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Li X-J, et al. Serglycin is a theranostic target in nasopharyngeal carcinoma that promotes metastasis. Cancer Res. 2011;71:3162–3172. doi: 10.1158/0008-5472.CAN-10-3557. [DOI] [PubMed] [Google Scholar]
- 305.Chew MM, Gan SY, Khoo AS, Tan EL. Interleukins, laminin and Epstein - Barr virus latent membrane protein 1 (EBV LMP1) promote metastatic phenotype in nasopharyngeal carcinoma. BMC Cancer. 2010;10:574. doi: 10.1186/1471-2407-10-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Sun W, et al. Interleukin-6 promotes the migration and invasion of nasopharyngeal carcinoma cell lines and upregulates the expression of MMP-2 and MMP-9. Int. J. Oncol. 2014;44:1551–1560. doi: 10.3892/ijo.2014.2323. [DOI] [PubMed] [Google Scholar]
- 307.Zergoun AA, et al. IL-6/NOS2 inflammatory signals regulate MMP-9 and MMP-2 activity and disease outcome in nasopharyngeal carcinoma patients. Tumour Biol. 2016;37:3505–3514. doi: 10.1007/s13277-015-4186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Stegh AH. Targeting the p53 signaling pathway in cancer therapy—the promises, challenges and perils. Expert Opin. Ther. Targets. 2012;16:67–83. doi: 10.1517/14728222.2011.643299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Yu KJ, et al. Prognostic utility of anti-EBV antibody testing for defining NPC risk among individuals from high-risk NPC families. Clin. Cancer Res. 2011;17:1906–1914. doi: 10.1158/1078-0432.CCR-10-1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Guo R, et al. Proposed modifications and incorporation of plasma Epstein-Barr virus DNA improve the TNM staging system for Epstein-Barr virus-related nasopharyngeal carcinoma. Cancer. 2019;125:79–89. doi: 10.1002/cncr.31741. [DOI] [PubMed] [Google Scholar]
- 311.Chan KCA, et al. Analysis of plasma Epstein-Barr virus DNA to screen for nasopharyngeal cancer. N. Engl. J. Med. 2017;377:513–522. doi: 10.1056/NEJMoa1701717. [DOI] [PubMed] [Google Scholar]
- 312.Ge Y, et al. In vitro evaluation of the therapeutic effectiveness of EBV-LMP2 recombinant adenovirus vaccine in nasopharyngeal carcinoma. Biomed. Pharmacother. 2020;121:109626. doi: 10.1016/j.biopha.2019.109626. [DOI] [PubMed] [Google Scholar]
- 313.Chia WK, et al. A phase II study evaluating the safety and efficacy of an adenovirus-DeltaLMP1-LMP2 transduced dendritic cell vaccine in patients with advanced metastatic nasopharyngeal carcinoma. Ann. Oncol. 2012;23:997–1005. doi: 10.1093/annonc/mdr341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Wu M, et al. MicroRNA-148b suppresses proliferation, migration, and invasion of nasopharyngeal carcinoma cells by targeting metastasis-associated gene 2. OncoTargets Ther. 2017;10:2815–2822. doi: 10.2147/OTT.S135664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Yu BL, et al. MicroRNA-378 functions as an onco-miR in nasopharyngeal carcinoma by repressing TOB2 expression. Int. J. Oncol. 2014;44:1215–1222. doi: 10.3892/ijo.2014.2283. [DOI] [PubMed] [Google Scholar]