SUMMARY:
Neurologic findings are being increasingly recognized in coronavirus disease 2019. We present a patient with a unique involvement of the corpus callosum that we relate to the cytokine storm seen in patients with Severe Acute Respiratory Syndrome coronavirus 2 infection. As the infection is increasingly seen around the world, recognition of these unique patterns may facilitate early identification of the progression of this disease and potentially facilitate appropriate management.
Since December 2019, coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) has spread across the globe, infecting hundreds of thousands of patients. This virus, while known for causing severe respiratory illness, has been reported to affect multiple organ systems, including the central nervous system. Approximately 36% of patients with COVID-19 develop neurologic symptoms such as headache, altered mental status, and paresthesia.1 Also of note, these neurologic symptoms may be the first signs of illness and appear to affect more severely infected patients.2 We discuss an adult patient managed in the intensive care unit with unusual imaging findings centered in the corpus callosum and discuss the potential pathophysiology, including the relation to the cytokine storm.
Case Description
A 66-year-old woman with a medical history of pulmonary sarcoidosis, coronary artery disease, type 2 diabetes, hypertension, and hyperlipidemia presented to the emergency department with a 2-day history of fevers, chills, and severe headache with associated blurry vision, which progressed to severe shortness of breath and chest pain. On admission, the patient's labs were remarkable for hyperglycemia, mild normocytic anemia, acute kidney injury, lymphopenia (0.4 bil/L), and elevated C-reactive protein (130 mg/L) and ferritin (630 mg/mL) levels. The patient subsequently tested positive for SARS-CoV-2 from a nasopharyngeal swab and was started on azithromycin and hydroxychloroquine. Eight days after symptom onset, the patient had a rapid decline with increasing respiratory distress requiring intubation and transfer to the intensive care unit. At transfer, D-dimer (1782 ng/mL) and fibrinogen (606 mg/dL) levels were elevated. These markers peaked several days later: D-dimer > 10,000 ng/mL and fibrinogen > 1000 mg/dL. She was also placed on intravenous heparin (therapeutic dosing), given the elevated levels of D-dimer. During the patient's intensive care unit stay, she required hemodialysis for her acute kidney injury, which was thought secondary to the COVID-19 infection. After reduction in sedation on hospital day 19, right-sided weakness was noted and a noncontrast head CT was obtained. This scan demonstrated hypodensities within the left parietotemporal region, as well as a more unusual hypodensity within the corpus callosum (Fig 1).
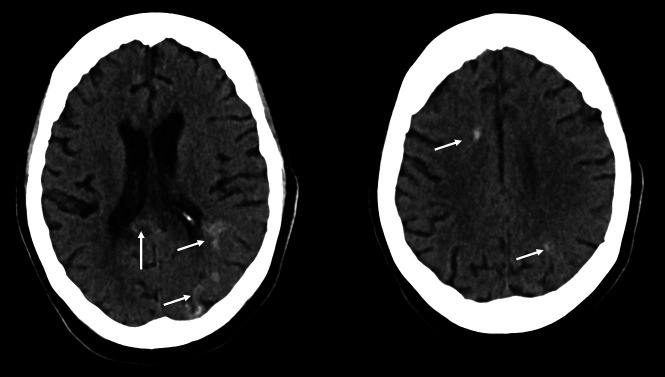
FIG 1.
Initial noncontrast head CT images demonstrate hypodensities in the left posterior parietal (black arrows) and peritrigonal regions as well as the corpus collosum (white arrows). No evidence of hemorrhage, mass effect, or midline shift is seen at this time.
Despite an overall improvement in the patient's respiratory status, extubation was delayed secondary to decreased mentation. On hospital day 27, an electroencephalography was performed, which demonstrated a triphasic morphology, most consistent with toxic encephalopathy with no evidence of epileptiform discharges. At that time, the patient was lethargic and aphasic with a poor prognosis for functional neurologic recovery. Subsequent noncontrast head CTs demonstrated areas of hemorrhage within the regions of hypodensity seen on the initial scan (Fig 2). The IV heparin was discontinued. The patient's mental status slowly improved with spontaneous eye opening/tracking and movement of the left extremities, though she remained aphasic. Secondary to improved mental status, the patient was eventually extubated.
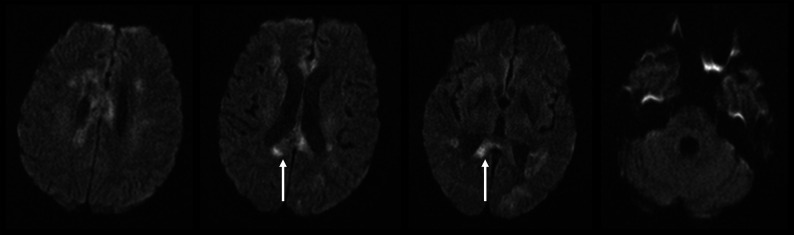
FIG 2.
Subsequent head CT demonstrates hemorrhage (white arrows) within the previously seen hypodensities. The posterior corpus collosum is involved.
Brain MR imaging obtained on hospital day 36 demonstrated multiple areas of diffusion restriction within the corpus callosum, corona radiata, and centrum semiovale, with associated T2-FLAIR hyperintensities. Multiple areas of microhemorrhage were also detected (Figs 3 and 4). The thalami, brain stem, and cerebellum were spared. At the time of this writing, the patient is receiving continued inpatient treatment.
FIG 3.
Multiple diffusion-weighted images demonstrate restriction centered in the corpus collosum (white arrows), with some additional areas in the adjacent deep white matter including the centrum semiovale. In addition, there is faint diffusion restriction in the left occipital and temporal lobes, possibly representing subacute strokes. The thalami, brain stem, and cerebellum are spared.
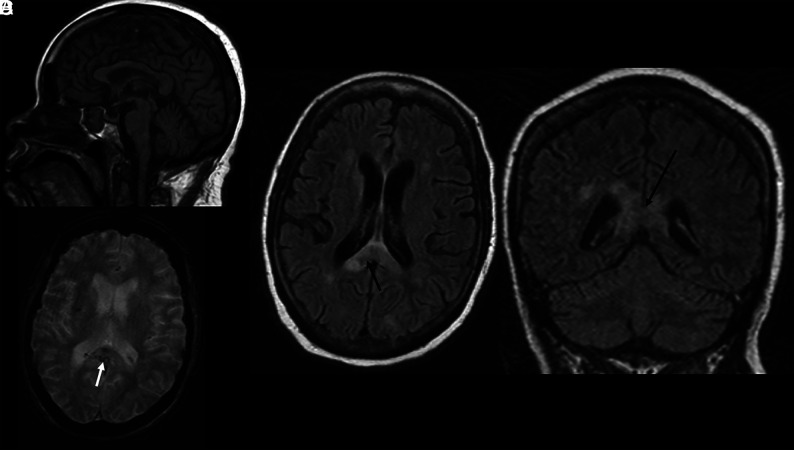
FIG 4.
A, Sagittal T1. Hypointense signal within the corpus collosum, most prominent in the splenium. B, Axial T2* sequence. Multiple punctate hypointensities compatible with hemorrhages are present within the corpus collosum (white arrow) and optic radiations, which are not shown. Axial (C) and coronal (D) T2 FLAIR. Increased T2 signal is seen with the corpus callosum (black arrows).
DISCUSSION
There appear to be multiple mechanisms for SARS-CoV-2 to cause neurologic damage, including direct neuronal injury, hypoxic damage from unresolved respiratory distress, autoimmune injury from the induced cytokine storm with resultant blood-brain barrier breakdown, vasculitis, and acute ischemic injury from a hypercoagulable state.1-5 A recent case report described acute necrotizing encephalopathy,4 a condition well-described in children from a multitude of causes.4,5 In these cases, the predominant findings are located in the thalami, with additional less common locations being the brain stem, cerebral white matter, and cerebellum.4 In contrast, our patient demonstrated extensive diffusion restriction within the corpus callosum (most severe in the splenium) without involvement of the thalami, brain stem, or cerebellum.
One entity that has a similar appearance is a condition called cytotoxic lesions of the corpus callosum (CLOCC).6 These have been described with several pathologies, including drug-associated conditions, trauma, malignancy, metabolic disorders, and, most importantly, infection, including several viruses such as adenovirus, H1N1 influenza, Epstein-Barr, and rotavirus.6 When cytokine release and inflammation are present in sufficient levels within the brain, astrocytes are stimulated to release glutamate as well as block the reuptake of this neurotransmitter.6-8 The greatly increased amount of glutamate within the extracellular space leads to excitotoxic action on multiple glutamate receptors, sodium-potassium pumps, and aquaporins, resulting in an influx of water trapped within the cells.6,9-11 These effects manifest on imaging as diffusion restriction, as seen in our patient.6
It is believed that the corpus callosum is vulnerable to cytokine-induced injury due to the high density of cytokine, glutamate, and other receptors present within this region of the brain, particularly the splenium.6,12-17 These previously described mechanisms combined with our patient's extremely elevated markers for acute-phase reactants, suggest initial autoimmune injury from a cytokine storm. With other infectious diseases, the involvement of the corpus callosum is typically transitory; however, in the setting of COVID-19, this has yet to be determined.6,16 The patient also had ischemic changes in other parts of the brain, and an alternative consideration is a stroke of the corpus callosum. However, the redundant blood supply to the corpus callosum, including the anterior communicating artery, the pericallosal artery, and the posterior pericallosal artery, makes strokes of the corpus callosum rare.18 The subsequent hemorrhage in these areas is likely multifactorial, with evolution of necrosis from a cytokine storm being a possible contributing factor. While the use of therapeutic-dose heparin was initially shown to improve patient mortality,19 this medication could also have played a role.
CONCLUSIONS
There is currently limited literature on the neuroimaging findings in COVID-19. To our knowledge, involvement of the corpus callosum related to the cytokine storm has not yet been described with this infection. While as of yet, the transitory nature of this complication is unknown, the authors believe that with continued surveillance, this question is likely to be answered. As management is directed to the cytokine storm, knowledge of this imaging pattern could be invaluable.
ABBREVIATIONS:
- COVID-19
coronavirus disease 2019
- SARS-Cov-2
Severe Acute Respiratory Syndrome coronavirus 2
Footnotes
Disclosures: Anant Krishnan—UNRELATED: Expert Testimony: Various.
References
- 1. Wu Y, Xu X, Chen Z, et al. . Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18–22 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-COV-2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92;552–55 10.1002/jmv.25728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen T, Wu D, Chen H, et al. . Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368:m1091 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Poyiadji N, Shahin G, Noujaim D, et al. . COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology 2020. March 31. [Epub ahead of print] 10.1148/radiol.2020201187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rossi A. Imaging of acute disseminated encephalomyelitis. Neuroimaging Clin N Am 2008;18:149–61 10.1016/j.nic.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 6. Starkey J, Kobayashi N, Numaguchi Y, et al. . Cytotoxic lesions of the corpus callosum that show restricted diffusion: mechanisms, causes, and manifestations. Radiographics 2017;37:562–76 10.1148/rg.2017160085 [DOI] [PubMed] [Google Scholar]
- 7. Miller AH, Haroon E, Raison CL, et al. . Cytokine targets in the brain: impact on neurotransmitter and neurocircuits. Depress Anxiety 2013;30:297–306 10.1002/da.22084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Phelps C, Korneva E, et al. . Neuroimmune biology. Cytokines and the Brain. Vol 6 Elsevier; 2008:295–98 [Google Scholar]
- 9. Leonoudakis D, Braithwaite SP, Beattie MS, et al. . TNFa-induced AMPA-receptor trafficking in CNS neurons: relevance to excitotoxicity? Neuron Glia Biol 2004;1:263–73 10.1017/S1740925X05000608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Prow NA, Irani DN. The inflammatory cytokine, interleukin-1 beta, mediates loss of astroglial glutamate transport and drives excitotoxic motor neuron injury in the spinal cord during acute viral encephalomyelitis. J Neurochem 2008;105:1276–86 10.1111/j.1471-4159.2008.05230.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Matute C, Alberdi E, Domercq M, et al. . Excitotoxic damage to white matter. J Anat 2007;210:693–702 10.1111/j.1469-7580.2007.00733.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hassel B, Boldingh KA, Narvesen C, et al. . Glutamate transport, glutamate synthetase and phosphate-activated glutaminase in rat CNS white matter: a quantitative study. J Neurochem 2003;87:230–37 10.1046/j.1471-4159.2003.01984.x [DOI] [PubMed] [Google Scholar]
- 13. Domercq M, Matute C. Expression of glutamate transporters in adult bovine corpus callosum. Brain Res Mol Brain Res 1999;67:296–302 10.1016/S0169-328X(99)00072-8 [DOI] [PubMed] [Google Scholar]
- 14. Goursaud S, Kozlova EN, Maloteaux J-M, et al. . Cultured astrocytes derived from corpus callosum or cortical grey matter show distinct glutamate handling properties. J Neurochem 2009;108:1442–52 10.1111/j.1471-4159.2009.05889.x [DOI] [PubMed] [Google Scholar]
- 15. Moritani T, Smoker WR, Sato Y, et al. . Diffusion-weighted imaging of acute excitotoxic brain injury. AJNR Am J Neuroradiology 2005;26:216–28 [PMC free article] [PubMed] [Google Scholar]
- 16. Takayama H, Kobayashi M, Sugishita M, et al. . Diffusion-weighted imaging demonstrates transient cytotoxic edema involving the corpus callosum in a patient with diffuse brain injury. Clin Neurol Neurosurg 2000;102:135–39 10.1016/S0303-8467(00)00079-2 [DOI] [PubMed] [Google Scholar]
- 17. Kimura EN, Okamoto S, Uchida Y, et al. . A reversible lesion of the corpus callosum splenium with adult influenza-associated encephalitis/encephalopathy: a case report. J Med Case Rep 2008;2:220 10.1186/1752-1947-2-220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yang LI, Huang YN, Cui ZT. Clinical features of acute corpus callosum infarction patients. Int J Clin Exp Pathol 2014;7:5160–64 [PMC free article] [PubMed] [Google Scholar]
- 19. Tang N, Bai H, Chen X, et al. . Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020;18:1094–99 10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]