Abstract
Acceptance-based approaches have demonstrated promise for improving outcomes in behavioral treatments for obesity, but few studies have examined processes of change in these treatments. It is critical to identify mechanisms of action in treatment to further optimize this approach, refine theory, and inform future research. This study examined change in several domain-specific and general measures of psychological flexibility in a randomized controlled trial of an acceptance-based behavioral weight loss treatment. The relationships between change in these measures and weight loss outcomes were also examined. Adults (N = 283) were randomized to receive 12 months of acceptance-based (ABT) or non-acceptance-based (non-ABT) behavioral treatment and completed measures of general and weight control-specific psychological flexibility at months 0, 6, and 12. Participants in ABT demonstrated greater increases in psychological flexibility related to eating and physical activity experiences during treatment compared to participants in non-ABT, and changes in these processes were correlated with better weight loss. Parallel mediation analyses further revealed that psychological flexibility related to eating and physical activity experiences partially mediated the relationship between treatment condition and 12-month weight loss. Participants across conditions also experienced small increases in general psychological flexibility, but general psychological flexibility was not meaningfully related to weight loss outcomes. These findings indicate that domain-specific (versus general) psychological flexibility may be most impacted by ABT and most relevant to weight loss outcomes. Results also provide partial support for the theoretical model of ABT for weight management.
Keywords: acceptance-based behavioral treatment, psychological flexibility, obesity, lifestyle modification, weight loss
Obesity is a significant public health concern, as a majority of American adults have body mass indexes (BMIs) in the overweight or obese range (Flegal, Kruszon-Moran, Carroll, Fryar, & Ogden, 2016; National Center for Health Statistics, 2017) and obesity increases risk for numerous adverse health conditions (Kopelman, 2007). Many adults can achieve clinically meaningful weight loss (≥5%) through comprehensive behavioral treatment (Jensen et al., 2014). However, there is room to improve the short-term efficacy of treatment and weight regain afLillister treatment remains common, suggesting that innovative treatment approaches that can improve outcomes are needed (Dombrowski, Knittle, Avenell, Araujo-Soares, & Sniehotta, 2014). Acceptance-based behavioral treatment (ABT) is a relatively new approach for weight management that teaches individuals novel strategies for responding to the significant self-regulatory and motivational challenges of long-term weight control (Forman & Butryn, 2015; Forman, Butryn, Manasse, & Bradley, 2015; Lillis & Kendra, 2014). Several studies have shown that ABT can produce clinically meaningful weight loss. However, few studies have examined hypothesized mechanisms of action in ABT, and these studies have yielded inconsistent results. In order to inform the optimization of ABT for obesity, it is critical to further examine the processes by which this treatment approach operates and to identify measures that best capture change in key processes.
The theoretical model underlying ABT for weight control is rooted in Acceptance and Commitment Therapy (ACT), which is a third-wave therapy focused on fostering psychological flexibility, or the ability to engage in adaptive, values-consistent action regardless of one’s momentary internal experiences (urges, feelings, thoughts, physical sensations) (Hayes, Strosahl, & Wilson, 1999). Individuals are taught to become more psychologically accepting of their internal experiences through adopting an open, non-judgmental stance towards their thoughts, feelings, and urges, and through acknowledging that discomfort is a sometimes-unavoidable aspect of the human experience. Individuals’ values are also clarified and individuals are encouraged to use their values, rather than their momentary experiences, as a guide for behavior (i.e., whether to persist in or change a certain behavior). Various acceptance, values, and mindfulness-focused exercises and techniques are used to build these skills and increase psychological flexibility (Hayes et al., 1999).
Several studies have examined the efficacy of treatments that incorporate ACT-based skills with foundational weight control strategies (herein referred to as ABT), with results supporting the benefit of ABT for weight management. For example, one recent randomized controlled trial found that ABT produced superior weight loss compared to standard behavioral treatment at the end of a 12-month program (Forman et al., 2016), while a different randomized controlled trial found that ABT resulted in superior weight loss maintenance compared to standard behavioral treatment (Lillis et al., 2016). Two additional randomized controlled trials did not reveal a benefit of ABT over standard behavioral treatment for the total study population (Butryn et al., 2017; Forman et al., 2013, but did find ABT resulted in greater weight loss for certain subgroups (i.e., individuals who may be more susceptible to food cues (Forman et al., 2013) and African American individuals (Butryn et al., 2017)).
It is important to understand how ABT enhances outcomes in behavioral weight loss treatment in order to further improve its efficacy. A limited number of studies have examined purported processes of change in ABT. In Forman and colleagues’ (2016) trial in which ABT produced superior weight loss, greater psychological flexibility toward food-related urges and greater autonomous motivation partially mediated weight loss outcomes (Forman et al., 2016). However, psychological flexibility toward food-related urges mediated weight loss only among participants high in emotional eating in another trial (Forman et al., 2013). In Lillis and colleagues’ (2017) trial in which ABT produced superior weight loss maintenance, the only measure on which participants in ABT improved more than individuals in standard behavioral treatment was a measure of values consistent behavior. Interestingly, though, change on this measure did not mediate the effect of treatment on weight loss (Lillis, Thomas, Niemeier, & Wing, 2017).
Findings concerning ABT’s mechanisms of action may have differed in past studies partly due to differences in the measures used to assess process variables. Several measures of psychological flexibility have been developed. The Acceptance and Action Questionnaire (Hayes, Luoma, Bond, Masuda, & Lillis, 2006) and its later iterations (e.g., Bond et al., 2011) are widely used measures of general psychological flexibility (i.e., individuals’ psychological acceptance of internal experiences and ability to engage in values-consistent action overall, versus in regard to a certain concern or domain). Several measures of psychological flexibility specific to experiences related to weight, eating, and physical activity have also been developed (Butryn et al., 2015; Juarascio, Forman, Timko, Butryn, & Goodwin, 2011; Lillis & Hayes, 2007; Palmeira, Cunha, Pinto-Gouveia, Carvalho, & Lillis, 2016). Although both Lillis and colleagues (2017) and Forman and colleagues (2013, 2016) assessed psychological flexibility using measures specific to weight control—with the Acceptance and Action Questionnaire for Weight-Related Difficulties (Lillis & Hayes, 2008) and the Food Acceptance and Awareness Questionnaire (Juarascio, Forman, Timko, Butryn, & Goodwin, 2011), respectively—it has yet to be determined whether general or domain-specific measures best capture changes in psychological flexibility during ABT and are most strongly related to treatment outcomes. On the one hand, it is possible that general psychological flexibility measures are most predictive of weight loss, as participants who increase their overall psychological flexibility may be best able to apply ABT skills to the wide range of experiences that can impact weight control. Increases on general measures of psychological flexibility may also reflect greater mastery of ABT strategies. On the other hand, increased psychological flexibility toward the experiences most directly tied to eating and physical activity (e.g., urges to eat, urges to skip or stop exercising) may be sufficiently powerful for improving weight outcomes. Clarifying how general and domain-specific psychological flexibility relates to weight loss during ABT can inform further treatment development, help refine the theory of ABT for weight management, and inform measure selection in future studies.
The present study examined change in several measures of psychological flexibility and its relationship with weight outcomes in a randomized controlled trial in which participants received ABT or one of two behavioral treatments (combined for analyses) that did not contain acceptance-based skills (non-ABT; CITATION REMOVED FOR BLINDING). There were three aims. First, we examined the effect of condition (ABT versus non-ABT) on change in general and domain-specific measures of psychological flexibility during the 12-month treatment program. Although a main effect of condition on weight loss was not observed in the parent study (CITATION REMOVED FOR BLINDING), we remained interested in whether ABT enhanced psychological flexibility to a greater extent than non-ABT, given the specialized acceptance-based skills that participants in ABT were taught. Second, we examined the relationships between change in psychological flexibility and weight loss from both months 0 to 6 and months 0 to 12 among all participants, including those who did not receive ABT. We elected to assess these relationships among all participants because past research indicates that participants in standard behavioral treatment may experience gains in acceptance-related constructs (e.g., Lillis et al., 2017), and improvements in psychological flexibility should theoretically relate to greater weight loss regardless of how participants become more flexible (i.e., through learning specialized skills in ABT or through other processes non-specific to ABT). Third, for any process variables for which condition effects were observed in Aim 1, we conducted mediational analyses to assess the indirect effect of treatment condition on weight loss through these psychological flexibility measure(s). Modern bootstrapping-based mediational analyses can provide valuable information about hypothesized mechanisms of action in treatment even when significant differences in an outcome variable are not observed in a particular trial, as was the case with the parent study (Hayes, 2017; CITATION REMOVED FOR BLINDING). Across these aims, we were interested in the pattern of findings for general versus domain-specific psychological flexibility measures.
Methods
Participants.
Adults (N = 283) with BMIs in the overweight or obese range were recruited from the community for a study comparing the effect of three different behavioral treatments on weight loss and weight loss maintenance. Participants were recruited using radio advertisements, postcards, newspapers, and local websites. Eligibility required a BMI between 27.0 and 45.0 kg/m2, age 18 to 70 years, ability to safely engage in physical activity, and completion of prerandomization procedures (i.e., two screening/assessment visits and a 7-day food diary). Participants were excluded if they were pregnant, breastfeeding, or intended to become pregnant in the next two years; had a medical or psychiatric condition that would preclude their ability to follow and/or benefit from the program; had recently changed the dose of a medication that could meaningfully impact weight; were participating in or intended to participate in another weight loss program; or had a spouse or first-degree family member who was enrolled in the program. The parent study was approved by the host institution’s Institutional Review Board and all participants provided written informed consent to participate.
Design.
Eligible participants were randomized to one of three group-based treatment conditions: standard behavioral treatment (non-ABT), behavioral treatment augmented with specialized skills for addressing the obesogenic environment (non-ABT), or behavioral treatment with environment and acceptance-based skills (ABT). Both non-ABT conditions were combined for condition analyses in the present study. All groups met for 26, 75-minute sessions over 12 months. Group frequency decreased from weekly (months 1-4), to biweekly (months 5-6), to monthly (months 7-12). Each session began with a check-in on participants’ progress in the previous week(s), introduced or reviewed content or skills for weight control, and ended by assigning home practice for the following week(s). Groups were led by a clinician with a master’s or doctorate degree in clinical psychology and previous experience with behavioral weight loss, as well as a co-leader who was a more junior psychology trainee. Each group was composed of 10–14 participants and met in a research clinic on a university campus. Participants completed self-report measures and their weight was measured by research staff at months 0 (baseline), 6 (mid-treatment), and 12 (end-of-treatment).
Intervention Components.
Additional details about the treatment approaches can be found in the main outcomes paper (CITATION REMOVED FOR BLINDING).
Shared Components.
All treatment conditions contained foundational behavioral recommendations for weight loss/maintenance. Participants were instructed to follow a standard balanced deficit diet (1200–1800 kcals/day depending on starting weight); to self-monitor their calories, physical activity, and weight; and to gradually increase their weekly physical activity to 250 minutes of moderate-to-vigorous intensity activity performed in bouts of at least 10 minutes. Participants in all conditions were also taught basic skills to promote adherence to these goals, such as how to accurately determine portion sizes and strategies for restaurant eating.
Non-ABT Conditions.
Participants in the non-ABT conditions did not receive instruction in acceptance-based concepts or skills. Instead, in one of the non-ABT conditions, the intervention was standard behavioral treatment adapted from the Look AHEAD (The Look AHEAD Research Group, 2006) and Diabetes Prevention Program (The Diabetes Prevention Program Research Group, 1999) protocols. Treatment in this non-ABT condition focused on strategies such as identifying and planning for high-risk situations, managing stress, eliciting social support for weight control, and problem-solving. In the other non-ABT condition, many of these same elements were present, but there was particular emphasis placed on how environmental factors (e.g., availability and visibility of foods) can influence weight control and on specific skills for modifying the obesogenic environment.
ABT Condition.
The ABT condition also taught core behavioral and environmental strategies but in an abbreviated fashion to allow time for discussions and exercises promoting acquisition of acceptance-based skills for weight control. Participants were taught to increase awareness of their internal experiences (e.g., urges), to notice the influence of these experiences on behavior, and to adopt an accepting stance toward their internal experiences related to weight control. Additionally, activities and discussions sought to clarify participants’ values, to explore how these values related to weight control, and to increase the salience of participants’ values in their daily lives. Willingness was discussed as a key skill for choosing to take action toward one’s values (particularly those connected to health and weight control), even when doing so would require experiencing distress or less preferred internal states. Together, these skills sought to foster psychological flexibility that would enable participants to better adhere to weight control recommendations.
Measures.
Weight and Height.
Weight was measured at each assessment and session in light street clothes using a Seca® scale accurate to 0.1 kg. Height was measured with the built-in stadiometer at baseline to determine BMI. Percent weight loss at 12 months was computed such that positive values indicate greater weight loss.
Demographics.
Participants self-reported their age, gender, race, and ethnicity at baseline.
General Psychological Flexibility.
The Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011) was used to measure overall psychological flexibility. Participants were asked to rate each of 7 items (e.g., “I worry about not being able to control my worries and feelings”) from 1 (never true) to 7 (always true), and responses were summed to create a total score. In the present study, responses were reverse-scored so that higher total scores indicate greater psychological flexibility (to match the directionality of the two domain-specific flexibility measures). The AAQ-II has demonstrated good psychometric properties (Bond et al., 2011). In the present study, Cronbach’s α = .91.
Food-related Psychological Flexibility.
The Food Acceptance and Awareness Questionnaire (FAAQ; Juarascio et al., 2011) was used to measure participants’ openness to experiencing and flexibility in responding to food cravings and urges to eat. Participants were asked to respond to 7 items (e.g., “It’s OK to experience cravings and urges to overeat, because I don’t have to listen to them”) using a scale ranging from 1 (never true) to 7 (always true). Responses were summed to create a total score, with higher scores indicating greater psychological flexibility toward food-related experiences. The FAAQ has demonstrated adequate psychometric properties (Juarascio et al., 2011) and in the present study α = .74.
Physical Activity-related Psychological Flexibility.
The Physical Activity Acceptance Questionnaire (PAAQ; Butryn et al., 2015) was used to measure participants’ openness to experiencing and flexibility in responding to thoughts, feelings, and physical sensations that they may experience when deciding to exercise or while exercising. Participants were asked to rate each of 10 items (e.g., “It is okay to experience discomfort (e.g., fatigue, boredom, sweating) while I am exercising”) from 1 (never true) to 7 (always true). Responses were summed to create a total score, with higher scores indicating greater psychological flexibility toward physical activity internal experiences. In the present study, the first cohort of participants (n = 65) completed a now-outdated version of the measure at baseline that contained only 8 items. For these participants, scores on these 8 items were prorated to a 10-item summary score; follow-up analyses indicated no significant differences between these prorated scores and baseline scores for participants using the full 10-item version (p = .83). All participants completed the 10-item measure at months 6 and 12. The PAAQ has demonstrated adequate psychometric properties (Butryn et al., 2015) and in the present study α = .81.
Statistical Analyses.
Analyses were conducted using IBM SPSS Statistics software version 24. Differences between conditions in baseline characteristics and 12-month weight loss were examined using one-way ANOVA and X2. Baseline BMI, race, and age were all independently associated with 12-month weight loss. All models were run controlling for and not controlling for these covariates. Because the pattern of results was similar across these models, results from models without covariates are reported for ease of interpretation.
Change in each process measure over time and the effect of treatment condition on change in process measures were examined using linear mixed effects models (Aim 1). The dependent variable in each model was the process variable of interest (AAQ-II, FAAQ, or PAAQ). Condition (ABT versus non-ABT), assessment time point (0, 6, or 12 months), and the condition by assessment time point interaction were entered as fixed effects. We considered several covariance structures and selected the one that demonstrated the best overall fit, which was a variance components covariance structure. Assessment time point, subject, and the intercept were considered for inclusion as random effects in the models. Model fit indices (Bayesian information criterion value) indicated that fit was superior when subject and the intercept were included as random effects. The mixed effects models handled missing data by including all available data from participants.
Bivariate correlations were used to examine how change in process measures from months 0 to 6 and months 0 to 12 related to percent weight loss during the same time period (Aim 2). If participants were missing process measure data at month 6 (14% of participants for AAQ-II, 14% of participants for FAAQ, and 15% of participants for PAAQ) or month 12 (24% of participants for AAQ-II, 23% of participants for FAAQ, and 25% of participants for PAAQ), their last observed value from month 6 or 0 for that process measure was used. A small number of participants (n = 3) were missing baseline data for a process measure but had later process measure data available. In these cases, participants’ most recent observed value from month 6 or 12 was carried backward to baseline. Missing data were primarily due to attrition, as well as incomplete assessment data. If participants were missing 12-month weight data (18% of participants), an imputation method used in numerous prior studies (Wadden et al., 2006; Wing, Tate, Gorin, Raynor, & Fava, 2006) that assumes 0.30 kg (0.66 pounds) of weight gain per month following discontinued session attendance was used to estimate 12-month weight loss.
If condition differentially affected change in any process variables over time, parallel mediational models were performed with 6-month values of the process variable(s) as the mediator, treatment condition (ABT versus non-ABT) as the independent variable, baseline values of the process variables(s) as covariates, and 12-month weight loss as the dependent variable (Aim 3). Mediation was conducted using Preacher and Hayes’ (2008) bootstrapping method and the PROCESS script for SPSS (Hayes, 2012). Parameter estimates were based on 5,000 resamples and 95% bias-corrected confidence intervals were computed to determine the statistical significance of indirect effects. The indirect effect was estimated by first regressing 6-month process measure values on condition, while controlling for baseline process measure values. Percent weight loss at 12 months was subsequently regressed on 6-month process measure values, while controlling for condition and baseline process measure values. The indirect effect was then estimated as the product of the mean bootstrapped estimates of those regression coefficients. As with aim 2 analyses, the last observed value (i.e., baseline) for each process measure was used to account for any missing process measure data at 6 months. Of note, the same pattern of results was observed for Aims 2 and 3 when using completers only data.
Results
Baseline Characteristics, Weight Loss, and Bivariate Correlations for Psychological Flexibility Measures.
Table 1 displays sample characteristics and values on psychological flexibility measures at baseline. There were no significant baseline differences among participants assigned to non-ABT and ABT. Across all participants, mean percent weight loss at 12 months was 8.78% (SD = 6.42%). Percent weight loss did not differ significantly between ABT (M = 9.73%, SD = 7.54) and non-ABT (M = 9.16%, SD = 8.20), F(1, 281) = 0.34, p = .56. At baseline, AAQ-II scores were positively correlated with both FAAQ scores, r(279) = 0.16, p = .008, and PAAQ scores, r(280) = 0.16, p = .009. FAAQ and PAAQ scores were also positively correlated, r(277) = 0.33, p < .001.
Table 1.
Sample characteristics and baseline values of process variables
| Treatment Condition | ||
|---|---|---|
| Non-ABT (n = 181) | ABT (n = 102) | |
| BMI (kg/m2) | 35.17 (5.17) | 35.23 (4.64) |
| Age (years) | 53.33 (9.80) | 53.23 (9.43) |
| AAQ-II | 40.20 (7.38) | 40.79 (7.69) |
| FAAQ | 38.96 (8.24) | 39.35 (7.66) |
| PAAQ | 42.21 (10.38) | 41.64 (10.67) |
| Gender (n, %) | ||
| Male | 42 (23.2%) | 18 (17.6%) |
| Female | 139 (76.8%) | 84 (82.4%) |
| Race (n, %) | ||
| Caucasian/White | 122 (67.4%) | 64 (62.7%) |
| African American/Black | 51 (28.2%) | 32 (31.4%) |
| Other or more than one race | 8 (4.4%) | 6 (5.9%) |
| Ethnicity (n, %) | ||
| Hispanic/Latino | 11 (6.1%) | 12 (11.8%) |
| Non-Hispanic/Latino | 170 (93.9%) | 89 (87.3%) |
Note. Values are mean and standard deviations unless specified otherwise. Percentages may not add up to 100% due to missing data. Non-ABT represents the two treatment conditions that did not include acceptance-based skills, and ABT represents the treatment condition with these skills.
Aim 1: Change in Process Variables by Condition Over Time
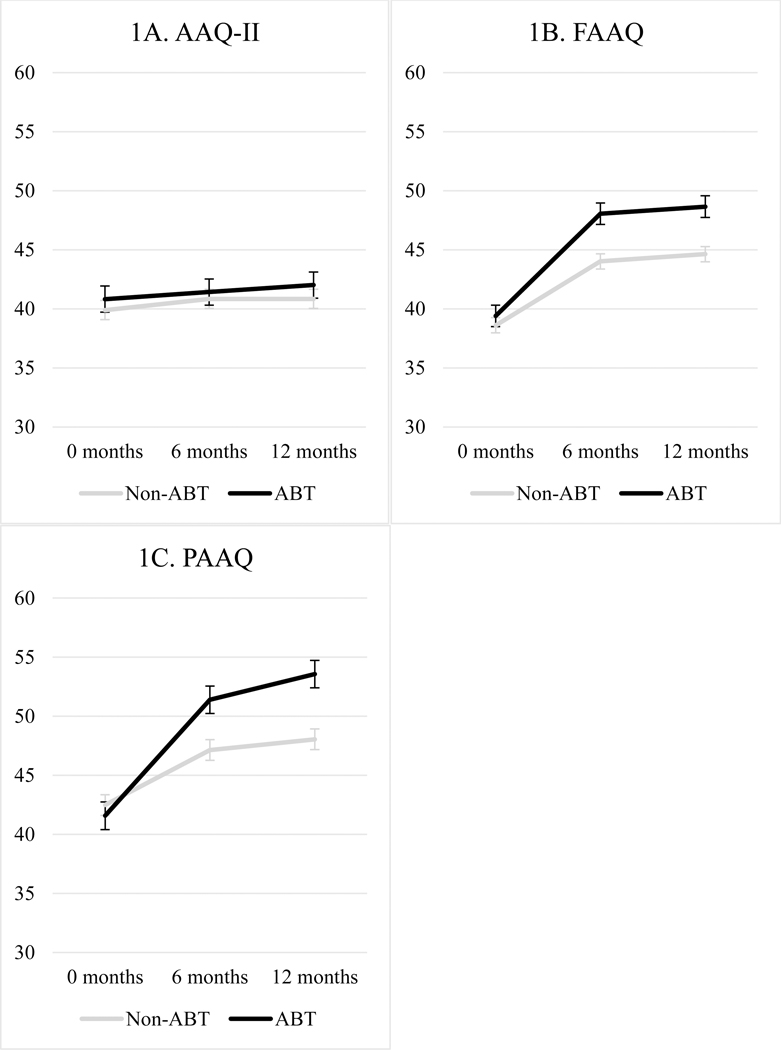
Figure 1 displays results for aim 1. Results from linear mixed model analyses revealed a significant main effect of time on AAQ-II scores (F = 3.77, p = .02), indicating that participants in ABT and non-ABT experienced increases in AAQ-II scores over time. Participants in ABT did not experience greater increases in AAQ-II scores than participants in non-ABT, as evidenced by a non-significant interaction between condition and assessment time point (F = 0.26, p = .78; see Figure 1A). Results from linear mixed model analyses revealed a significant interaction between assessment time point and condition on both FAAQ (F = 5.16, p = .006) and PAAQ scores (F = 10.36, p < .001; see Figures 1B and 1C). These interactions indicated that ABT (versus non-ABT) resulted in higher scores on both the FAAQ and PAAQ at 6 months (FAAQ: t = 2.78, p = .006; PAAQ: t = 3.51, p < .001) and 12 months (FAAQ: t = 2.70, p = .007; PAAQ: t = 4.17, p < .001) relative to baseline. Follow-up mixed model analyses among only non-ABT participants revealed that participants in non-ABT experienced significant increases in FAAQ (F = 44.83, p < .001) and PAAQ (F = 13.18, p < .001) scores over assessment time point, though the significant treatment condition by assessment interaction indicates that increases were less pronounced than those observed among participants in ABT.
Figure 1.
Change in process variables by condition across treatment. Note. Plotted values depict predicted values and error bars display 95% confidence internals from the mixed effects models.
Aim 2: Correlations between Change in Process Variables and Weight Loss
As shown in Table 2, change in AAQ-II scores from months 0 to 6 and from months 0 to 12 was not meaningfully related to percent weight loss during the same time periods. Greater increases in both FAAQ and PAAQ scores were related to greater percent weight loss during both time periods.
Table 2.
Relationships between change in process variables and weight loss
| Process Measure | n | Correlation between Change on Measure and Percent Weight Loss from 0 to 6 Months | Correlation between Change on Measure and Percent Weight Loss from 0 to 12 Months |
|---|---|---|---|
| AAQ-II | 282 | −0.001 | 0.07 |
| FAAQ | 279 | 0.37*** | 0.38*** |
| PAAQ | 280 | 0.40*** | 0.36*** |
Note.
p < .05,
p < .01,
p < .001.
The number of participants for each analysis differs slightly due to a small number of participants missing data for each process measure across all three time points.
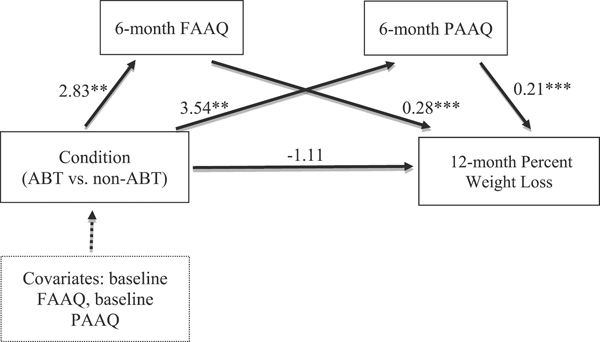
Aim 3: Mediation
Given the condition differences in FAAQ and PAAQ scores over time, a parallel mediation analysis was conducted to examine the indirect effect of treatment condition on 12-month weight loss through 6-month FAAQ and PAAQ scores. The indirect effect of treatment condition on weight loss through FAAQ was estimated as 0.78 (SE = 0.33, 95% CI: 0.23, 1.55), indicating that 12-month percent weight loss among participants in ABT was, on average, 0.78 units greater (i.e., mean percent weight loss was almost 1% more) than that of participants in non-ABT as a result of the indirect effect through psychological flexibility toward food experiences (Hayes, 2017). The indirect effect of treatment condition on weight loss through PAAQ was estimated as 0.75 (SE = 0.34, 95% CI: 0.22, 1.54), equating to greater percent weight loss of 0.75 units among participants in ABT versus non-ABT through psychological flexibility toward physical activity experiences. The total indirect effect was estimated as 1.52 (SE = 0.50, 95% CI: 0.58, 2.56). As illustrated in Figure 2, ABT (versus non-ABT) predicted greater 6-month FAAQ and PAAQ scores (significant a path), and greater 6-month FAAQ and PAAQ scores predicted greater weight loss (significant b path). The total effect (c path) of condition on 12-month weight loss was estimated at 0.42 (SE = 1.00) and was not significant (95% CI: −1.54, 2.37).
Figure 2.
Parallel mediation model for FAAQ and PAAQ , Note. ABT = acceptance-based behavioral treatment, FAAQ = food-related psychological flexibility, PAAQ = physical activity-related psychological flexibility
The partially standardized indirect effect (MacKinnon, 2008) of treatment condition on 12-month weight loss through 6-month FAAQ was 0.10 (95% CI: 0.03, 0.20), indicating that participants in ABT had, on average, 0.10 standard deviations greater weight loss than participants in non-ABT as a result of the indirect effect through FAAQ. The partially standardized indirect effect of treatment condition on 12-month weight loss through 6-month PAAQ was 0.09 (95% CI: 0.03, 0.19), indicating that participants in ABT had, on average, 0.09 standard deviations greater weight loss at 12 months than participants in non-ABT as a result of the indirect effect through PAAQ.
Discussion
Acceptance-based behavioral treatment is a promising new approach for improving weight loss outcomes. Despite growing evidence supporting the efficacy of ABT, the current research literature is limited by inadequate understanding of how to best measure and enhance mechanisms of change in ABT. This study aimed to address these limitations by examining changes in general and domain-specific psychological flexibility during a randomized trial of ABT, whether changes in psychological flexibility correlated with weight loss outcomes, and whether psychological flexibility mediated the relationship between treatment condition and weight loss.
Participants in both ABT and non-ABT demonstrated modest increases in general psychological flexibility during treatment that did not differ by treatment condition. By contrast, participants in ABT and non-ABT demonstrated improvements in food and physical activity-related psychological flexibility, and these increases were significantly larger among participants in AB. It is interesting to note that participants in both ABT and non-ABT increased on all measures of psychological flexibility, despite the processes involved in psychological flexibility (e.g., psychological acceptance and values-consistent action) being explicitly enhanced with ABT skills only in the ABT condition. This finding, which is consistent with previous literature (Lillis et al., 2016; Tapper et al., 2009), may indicate that psychological flexibility is an active ingredient for behavior change, regardless of the specific type of treatment received. For example, individuals in non-ABT treatment may unknowingly be practicing skills for noticing and accepting uncomfortable internal experiences and be building efficacy to continue engaging in weight control behaviors in the presence of these experiences as they work to meet eating and physical activity goals. The observed increases in psychological flexibility among individuals in non-ABT may also be related to the face validity of the measures, as some items on the measures, especially those that measure food- and physical activity-related psychological flexibility, emphasize participant behaviors in the presence of internal experiences rather than specific ABT techniques. Therefore, these measures may partially capture broader success with weight control behaviors.
Our finding that general psychological flexibility did not increase to a greater extent in ABT relative to non-ABT is consistent with results from a prior weight loss study (Tapper et al., 2009). Lillis and colleagues (2017) similarly observed comparable increases in psychological flexibility between ABT and standard behavioral treatment when measuring flexibility with the Acceptance and Action Questionnaire-Weight (AAQ-W; Lillis & Hayes, 2007), which is a measure of psychological flexibility that is more specific to weight control than the AAQ-II but more general than the FAAQ and PAAQ (Lillis et al., 2017). It is also noteworthy that the correlations between general and domain-specific measures in the present study were quite low, which suggests that these measures assess distinct constructs. Given that individuals in ABT demonstrated significantly greater improvements on domain-specific measures of psychological flexibility than individuals in non-ABT in this study and in prior research (e.g., Forman et al., 2016), it may be that highly domain-specific measures of psychological flexibility are more sensitive to change in psychological processes that occur during treatment and are therefore better candidates for measures to study mechanisms of change in these trials. The greater improvements in domain-specific but not general psychological flexibility was likely also influenced by the way in which ABT skills were taught in the present intervention. In the current intervention and in several past trials of ABT (e.g., Forman et al., 2016), ABT skills were very closely tied to weight control behaviors (e.g., willingness as a skill to facilitate portion control); very little intervention time was devoted to discussing or fostering psychological flexibility toward broader experiences. It is thus possible that other versions of ABT that teach ABT skills from a broader framework would observe a different pattern of findings.
We found that greater improvements in domain-specific but not general psychological flexibility were related to greater weight loss across participants. Thus, it appears that individuals may not need to become psychologically flexible with regard to broad internal experiences in order to improve their weight control. If confirmed in future studies, ABT for obesity may be most effective in improving weight loss when it focuses on fostering psychological flexibility very specific to weight control behaviors. Because past studies have varied somewhat in their approach to teaching ABT skills and have observed positive outcomes (Forman et al., 2016; Lillis et al., 2016), research that more explicitly compares the efficacy of ABT that teaches skills in a more focused versus broader manner is warranted. Additionally, due to the correlational nature of these findings, it is also possible that weight loss led to participants reporting greater psychological flexibility. Research with frequent and early measurement of processes variables would be beneficial for clarifying causality for the relation between psychological flexibility and weight change.
Building on previously discussed findings, mediational analyses further revealed that increases in psychological flexibility toward food and physical activity experiences not only correlated with weight loss but also partially explained how participants in ABT successfully lost weight. Because there was no main effect on condition on weight loss (CITATION REMOVED FOR BLINDING), however, it appears that the greater improvements in psychological flexibility in ABT in the present trial were not sufficient to translate into significantly more weight loss among ABT participants. Nevertheless, the bootstrapped mediational analyses, which are statistically powerful, support psychological flexibility toward eating and physical activity experiences as mechanisms of change within ABT. Future studies on ABT may thus wish to target and further assess these constructs in order to improve weight loss outcomes and inform treatment development.
The current study has several strengths and limitations. To our knowledge, this is the first behavioral weight loss trial to analyze change in measures of both general and domain-specific psychological flexibility. Our analyses also evaluated theoretically-based behavior change mechanisms across time in a large sample using an objectively measured treatment outcome. With regard to limitations, all psychological flexibility measures were self-reported and may therefore have been subject to demand biases and recall error. The domain-specific measures used in this study may need further use and validation with other researchers. The present study also did not assess psychological flexibility using the AAQ-W, which limits direct comparisons with some previous findings, and only measures of psychological flexibility were examined as potential mechanisms of change. Additionally, weight loss was occurring for most participants during the first six months of treatment when change in psychological flexibility was assessed. Studies that repeatedly assess processes targeted by ABT early in treatment and that examine whether early change in these constructs predicts subsequent weight loss are needed to help confirm causality.
There are also limitations related to how missing data were handled. The mixed effects models assessing change in psychological flexibility during treatment may have led to biased estimates if data were missing not at random, and use of last-observation-carried-forward imputation for psychological flexibility measures in analyses examining weight loss may have impacted results. While a similar pattern of findings emerged when using completers only, results should be interpreted with some caution. Finally, it is important to note that comparable weight loss was observed between treatment groups in the parent study. If our trial had produced significantly better weight loss in ABT, the examination of the mediators or mechanisms explaining the superior treatment effect would have been more powerful and informative for future research and clinical practice. The lack of a condition effect on weight loss could be partially due to the emphasis on the home food environment in the ABT condition, which decreased the session time allocated to ABT skills and material.
In summary, the current study found that ABT led to weight loss partially through increases in food and physical-activity related, but not general, psychological flexibility. Change on measures of psychological flexibility occurred in both ABT and non-ABT, suggesting that psychological flexibility may be a mechanism of change across numerous intervention types, not just ABT. Together, findings suggest that it may be especially helpful to target and assess psychological flexibility specific to eating and physical activity in ABT for weight management. More research is needed to increase consensus regarding mechanisms of change in ABT and to further elucidate how different approaches to ABT may account for the mixed findings regarding when (e.g., for weight loss or weight loss maintenance) and for whom ABT may be most helpful. Better understanding mechanisms of change in ABT can guide intervention development and enhance treatment efficacy.
Highlights.
Participants reported increases on several measures of psychological flexibility
Acceptance-based treatment produced larger increases in domain-specific flexibility
Change in domain-specific flexibility during treatment related to weight loss
Domain-specific flexibility partially mediated weight loss outcomes
Change in general flexibility was not meaningfully related to weight loss
Acknowledgments
Funding Agencies:
National Institutes of Health R01DK092374
Footnotes
Declaration of Interest:
Dr. Butryn and Dr. Forman report royalties from books on acceptance based treatment published by New Harbinger and Oxford University Press.
The other authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, . . . Zettle RD (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. [DOI] [PubMed] [Google Scholar]
- Butryn ML, Arigo D, Raggio GA, Kaufman AI, Kerrigan SG, & Forman EM (2015). Measuring the ability to tolerate activity-related discomfort: Initial validation of the physical activity acceptance questionnaire (PAAQ). Journal of Physical Activity and Health, 12(5), 717–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn ML, Forman EM, Lowe MR, Gorin AA, Zhang F, & Schaumberg K (2017). Efficacy of environmental and acceptance based enhancements to behavioral weight loss treatment: The ENACT trial. Obesity, 25(5), 866–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrowski SU, Knittle K, Avenell A, Araujo-Soares V, & Sniehotta FF (2014). Long term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials. BMJ, 348, g2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, & Ogden CL (2016). Trends in obesity among adults in the United States, 2005 to 2014. JAMA: Journal of the American Medical Association, 315(21), 2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Juarascio AS, Bradley LE, Lowe MR, Herbert JD, & Shaw J (2013). The mind your health project: A randomized controlled trial of an innovative behavioral treatment for obesity. Obesity, 21(6), 1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, & Butryn ML (2015). A new look at the science of weight control: How acceptance and commitment strategies can address the challenge of self-regulation. Appetite, 84, 171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Manasse SM, & Bradley LE (2015). Acceptance-based behavioral treatment for weight control: a review and future directions. Current Opinion in Psychology, 2, 87–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Manasse SM, Crosby RD, Goldstein SP, Wyckoff EP, & Thomas JG (2016). Acceptance based versus standard behavioral treatment for obesity: Results from the mind your health randomized controlled trial. Obesity, 24(10), 2050–2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper; ]. Retrieved from http://www.afhayes.com/public/process2012.pdf. [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed). New York, NY: The Guillford Press. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press. [Google Scholar]
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, . . . Kushner RF (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology, 63(25), 2985–3023. [DOI] [PubMed] [Google Scholar]
- Juarascio AS, Forman EM, Timko CA, Butryn ML, & Goodwin C (2011). The development and validation of the food craving acceptance and action questionnaire (FAAQ). Eating Behaviors, 12(3), 182–187. [DOI] [PubMed] [Google Scholar]
- Kopelman P (2007). Health risks associated with overweight and obesity. Obesity Reviews, 8(s1), 13–17. [DOI] [PubMed] [Google Scholar]
- Lillis J, & Hayes SC (2007). Measuring avoidance and inflexibility in weight related problems. International Journal of Behavioral Consultation and Therapy, 4(1), 30–40. [Google Scholar]
- Lillis J, & Kendra KE (2014). Acceptance and Commitment Therapy for weight control: Model, evidence, and future directions. Journal of Contextual Behavioral Science, 3(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillis J, Niemeier HM, Thomas JG, Unick J, Ross KM, Leahey TM, . . . Wing RR (2016). A randomized trial of an acceptance based behavioral intervention for weight loss in people with high internal disinhibition. Obesity, 24(12), 2509–2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillis J, Thomas JG, Niemeier HM, & Wing RR (2017). Exploring process variables through which acceptance-based behavioral interventions may improve weight loss maintenance. Journal of Contextual Behavioral Science, 6(4), 398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP (2008). Introduction to statistical mediation analysis. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- National Center for Health Statistics (2017). Health, United States, 2016: With chartbook on long-term trends in health. Hyattsville, MD. [PubMed] [Google Scholar]
- Palmeira L, Cunha M, Pinto-Gouveia J, Carvalho S, & Lillis J (2016). New developments in the assessment of weight-related experiential avoidance (AAQW-Revised). Journal of Contextual Behavioral Science, 5(3), 193–200. [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, & Moore L (2009). Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite, 52(2), 396–404. [DOI] [PubMed] [Google Scholar]
- The Diabetes Prevention Program Research Group (1999). The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care, 22(4), 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Look AHEAD Research Group (2006). The Look AHEAD study: A description of the lifestyle intervention and the evidence supporting it. Obesity, 14(5), 737–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, ... & Stunkard AJ (2005). Randomized trial of lifestyle modification and pharmacotherapy for obesity. New England Journal of Medicine, 353(20), 2111–2120. [DOI] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, & Fava JL (2006). A self-regulation program for maintenance of weight loss. New England Journal of Medicine, 355(15), 1563–1571. [DOI] [PubMed] [Google Scholar]