Abstract
Background and Purpose: Patients with severe, progressive multiple sclerosis (MS) have complex physical and psychosocial needs, typically over several years. Few treatment options are available to prevent or delay further clinical worsening in this population. The objective was to develop an evidence-based clinical practice guideline for the palliative care of patients with severe, progressive MS.
Methods: This guideline was developed using the Grading of Recommendations Assessment, Development and Evaluation methodology. Formulation of the clinical questions was performed in the Patients–Intervention–Comparator–Outcome format, involving patients, carers and healthcare professionals (HPs). No uniform definition of severe MS exists: in this guideline, constant bilateral support required to walk 20 m without resting (Expanded Disability Status Scale score >6.0) or higher disability is referred to. When evidence was lacking for this population, recommendations were formulated using indirect evidence or good practice statements were devised.
Results: Ten clinical questions were formulated. They encompassed general and specialist palliative care, advance care planning, discussing with HPs the patient's wish to hasten death, symptom management, multidisciplinary rehabilitation, interventions for caregivers and interventions for HPs. A total of 34 recommendations (33 weak, 1 strong) and seven good practice statements were devised.
Conclusions: The provision of home-based palliative care (either general or specialist) is recommended with weak strength for patients with severe, progressive MS. Further research on the integration of palliative care and MS care is needed. Areas that currently lack evidence of efficacy in this population include advance care planning, the management of symptoms such as fatigue and mood problems, and interventions for caregivers and HPs.
Keywords: clinical practice guideline, GRADE assessment, multiple sclerosis, palliative care
Introduction
Multiple sclerosis (MS) is a chronic neurological disease affecting 2.3 million people worldwide. It has a variety of clinical presentations, an unpredictable disease course, and is the most common cause of neurological disability in young adults in many western countries.1 Around 15% of MS patients have a progressive course from the outset (primary progressive MS); a further 40% develop progressive disease after 15 years with relapsing–remitting disease (secondary progressive MS).2 No uniform definition of severe MS exists: in this guideline, patients needing constant bilateral support (cane, crutch or braces) to walk 20 m without resting [i.e. Expanded Disability Status Scale (EDSS) score >6.0]3 or higher disability are referred to. A significant proportion of such patients need assistive devices4 and they are at risk of death from aspiration pneumonia, urinary tract infections, complications of falls and fractures, and sepsis secondary to pressure ulcers.5,6 Nevertheless, some patients with severe, progressive MS (hereafter, severe MS) live for many years, and most die in hospital rather than at home.7,8 The provision of palliative care (PC) has been proposed to help respond to the complex and varying bio-psychosocial needs of patients with severe MS, for whom few treatment options are currently available to delay or prevent further clinical worsening.9–12
Scope
This guideline was devised by an international task force (TF) appointed by the European Academy of Neurology (EAN) in partnership with the European Association for PC (EAPC) and the European Network for Best Practice and Research in MS Rehabilitation (RIMS). TF members were also appointed by the MS International Federation (MSIF) and by the European Committee for Treatment and Research in MS (ECTRIMS). This collaborative, multiple stakeholder approach was adopted to reflect practice across a variety of healthcare systems in Europe.
The aim was to focus on outcomes that are important for patients and useful for caregivers and healthcare professionals (HPs). To ensure this, the clinical questions were formulated via direct engagement of MS patients and caregivers.13 The primary intended audience is clinicians working in MS care, PC, emergency medicine, nursing, rehabilitation and related disciplines. In addition, policy-makers, charities and other stakeholders may find this guideline useful for informing and planning policies.
A pertinent document to the guideline is the EAN consensus review on PC for patients with chronic and progressive neurological diseases.10
Methods
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology and the updated EAN recommendations were followed.14 A TF of 21 members from nine European countries and three disciplines (neurology, PC, rehabilitation) was assembled, with invitations from the chair (AS) on the basis of expertise in MS care. JD, IM, RM, RV and DO were appointed by the EAN; SV, RV and DO by the EAPC; MAB, JD and JSG by the RIMS, and JSG and RV by the ECTRIMS (Appendix S1).
The clinical questions
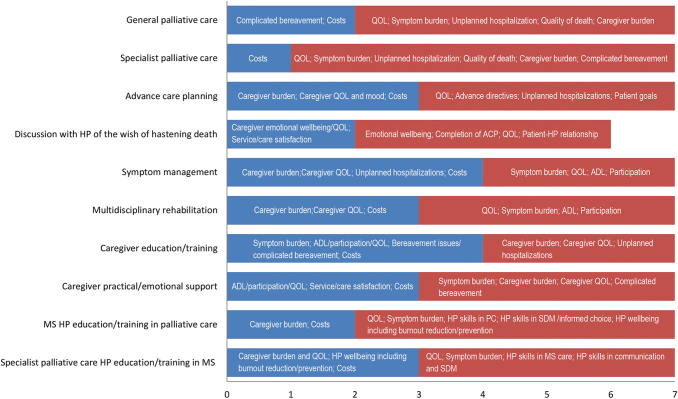
Ten clinical questions were formulated by the TF in Patients–Intervention–Comparator–Outcome (PICO) format (Appendix S2). The formulation was guided by literature search, MS expert survey (47 participants), MS patients and caregivers online survey (1119 participants) and five focus group meetings (three of MS patients, two of caregivers; overall 35 participants). The TF, originally organized into a Guideline Working Panel and a Methodological Panel, added a Client Consultation Panel to help with this phase, which took place between April 2017 and February 2018 and is detailed in a dedicated paper.13 In October 2018, TF members independently rated the importance of the outcomes identified for each clinical question on a 9-point scale15 (Fig. 1): all outcomes were considered as critical (score range 7–9) or important but not critical (score range 4–6).
FIG. 1.
Outcomes identified as important (score range 4–6; blue bars) or critical (score range 7–9; red bars) by the task force for each clinical question on a 9-point scale.15 ADL, activities of daily living; HP, healthcare professional; MS, multiple sclerosis; QOL, quality of life; SDM, shared decision-making.
Literature search
Seven electronic databases were searched from inception to October 2018: MEDLINE (OVID), PubMed, Embase, PsycINFO, CINAHL, Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews. The search strategies were developed in collaboration with two information specialists. The full MEDLINE search strategies are provided in Appendix S3. The search was expanded by looking at the references in the studies selected and at citations in the Web of Science Citation Index; by hand search of the online material available for major PC and MS journals; and by search on clinical trials registries and guideline (www.guidelines.gov) and health technology assessment (www.inahta.org) websites.
Study selection and data extraction
Between July and December 2018, two TF members independently reviewed the titles and abstracts identified and discarded the clearly irrelevant ones and those that did not meet the inclusion criteria. Any discrepancy at this stage was resolved by consensus. Full text of the selected studies was then reviewed independently by the two reviewers. Any disagreement regarding inclusion of individual studies was resolved by consensus; if agreement was not obtained, the full-text study was sent to a third independent reviewer for adjudication. Full details of the literature selection results for each clinical question are presented in Appendix S4.
Data from each included study were extracted by one TF member using an electronic form. A second member checked the data and disagreement was resolved by consensus; if consensus was not obtained, a third TF member was involved. Two TF members assessed the quality of evidence of the included studies using the Cochrane tool for risk of bias (randomized controlled trials, RCTs)16 and the CASP 10-item tool (qualitative studies, http://www.casp-uk.net/#!casp-tools-checklists/c18f8). Any disagreement was resolved by consensus; if consensus was not obtained, a third TF member was involved.
Data synthesis
For general and specialist PC (clinical questions 1 and 2), an individual participant data meta-analysis (IPDMA)17 was used to estimate the overall effect of the three RCTs currently available,18–20 one of which enrolled a mixed population of participants with neurodegenerative disorders, including MS (18/ 49, 37%).19 The baseline scores (T0) and the end-of-study scores (T1, at 12 weeks for the UK,18 16 weeks for the NE-PAL trial19 and 24 weeks for the PeNSAMI trial20) were considered. Domains that were assessed by all the studies were identified. For each domain, multivariate linear regression models were used to estimate the variability of the weighted score difference between PC and usual care groups, controlling for study, baseline EDSS score and baseline domain score. The one-stage approach was selected as it provides a more exact likelihood in the case of small studies.21 Our primary IPDMA analysis was intention-to-treat, with multiple imputations of the missing data via logistic regression models.22 A per-protocol analysis was also performed. Further, a sensitivity analysis was performed after exclusion of the PeNSAMI trial,20 to check whether the results obtained from all three studies (clinical questions 1 and 2) were consistent with those of the two studies on specialist PC (clinical question 2).
It was not possible to perform a quantitative synthesis on the other clinical questions, except for nabiximols for spasticity (clinical question 5) where a random-effects model meta-analysis was used. The effect on spasticity (patient-reported numerical rating scale, NRS) and caregiver-reported global impression of change (CGIC) scores were considered as they were used in all three included studies.23–25 The mean NRS differences between end of study and baseline reported in each study and, for CGIC, the odds ratios of nabiximols versus placebo were estimated. Between-study heterogeneity was assessed by Higgins I2 statistic with 95% confidence intervals (CIs). The meta-analyses were performed by an independent statistician (MC) and an EAN methodologist (KA). The preliminary and final results of the IPDMA were shared with the authors of the included studies. The IPDMAs were performed using STATA 16 (STATA College Station, TX, USA) and meta-analyses using RevMan 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Formulation of recommendations
Two TF members from the methodological panel formulated the preliminary wording and grading for each recommendation. Agreement upon the direction (‘for’ or ‘against’) and the strength (‘strong’ or ‘weak’) of each recommendation was obtained via teleconferences and electronic discussions, using a modified Delphi method.26 Agreement was reached after one clinical round for recommendations pertaining to clinical questions 7–10, after two rounds for recommendations pertaining to clinical questions 1–4 and 6, and after two to three rounds for recommendations pertaining to clinical question 5.
Ethics statement
The guideline protocol was approved by the ethics committee of the Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy (ref. no. 34, 2016).
Results
General and specialist palliative care (clinical questions 1 and 2)
PC seeks to improve the quality of life of patients and their families facing a life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.27 The PC provided by HPs who specialize in this discipline is known as specialist PC. Special PC services are characterized by a multiprofessional team approach and interdisciplinary mode of work.28 General PC can be provided by primary and specialist HPs who have attained PC competences but do not provide PC as the main focus of their work.
Ten publications on PC interventions were found: two described a qualitative study assessing the experiences of nine MS patients participating in a PC daycare programme29,30 and eight described three RCTs.18–20,31–35 The characteristics of the RCTs, and participants, are reported in Table 1.
Table 1.
Characteristics of the Trials on General/Specialist Palliative Care (Clinical Questions 1 and 2) and of Trial Participants
| Study |
|
|
|
|
MS patients (%) |
Carers (%) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Country (name) | No. of centres | Length (weeks) | Risk of bias (low/high) | No. | Age3 | Women | EDSSb | No. | Agea | Women | Relation |
| Specialist PC home-based | UK - | 1 | 12 | Selection (low)c Selection (low)d Performance (high) Detection (high) Attrition (low) Reporting (low) Other (low) | 52 | 53.0 (33–75) | 36 (69) | 7.5 (5.5–9.5) | 43 | - | - | Partner/spouse 29 (67) Son/daughter 7 (16) Parent 4 (10) Other relative 3 ( 7) Paid carer 0(0) |
| Specialist PC home-based | Italy (NE-PAL) | 1 | 16 | Selection (low)c Selection (low)d Performance (high) Detection (high) Attrition (low) Reporting (low) Other (low) | 18 | 54.2 (40–71) | 10 (56) | 8.5 7.0–9.5) | 18 | - | 14 (78) | Partner/spouse 11 (61) Son/daughter 1 ( 5) Parent 2 (10) Other relative 1 ( 5) Paid carer 3 (17) |
| General PC home-based | Italy (PeNSAMI) | 3 | 24 | Selection (low)c Selection (low)d Performance (high) Detection (low) Attrition (low) Reporting (low) Other (low) | 76 | 59.2 (41–80) | 43 (57) | 8.5 (8.0–9.5) | 76 | 60.3 (23–84) | 47 (62) | Partner/spouse 40 (53) Son/daughter 8(11) Parent 12 (16) Other relative 13 (17) Paid carer 3(4) |
EDSS, Expanded Disability Status Scale; MS, multiple sclerosis; PC, palliative care. aMean (range). bMedian (range). cRandom sequence generation. dAllocation concealment.
The UK trial18,32,33 and NE-PAL19 were single-centre RCTs comparing home-based specialist PC to usual care (1:1 ratio). PeNSAMI20,34 was a multicentre RCT comparing home-based general PC to usual care (2:1 ratio). The intervention lasted 12 weeks in the UK trial, 16 weeks in the NE-PAL trial and 24 weeks (with a 12-week assessment) in the PeNSAMI study. The risk of bias was low overall except for performance bias (all studies) and detection bias (UK and NE-PAL). UK trial participants were slightly younger (mean age 53 years), less severely affected (median EDSS 7.5) and predominantly women (68%) compared to participants in the other two studies (Table 1). Each patient had a caregiver who participated in the trial (in most instances a woman, and patient spouse or partner).
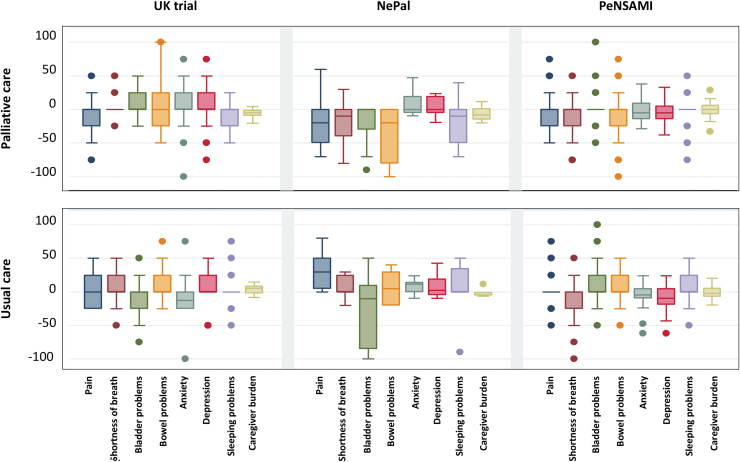
Eight domains were assessed by all the studies (Table 2): pain, shortness of breath, bladder problems, bowel problems, anxiety, depression, sleeping problems and caregiver burden. Figure 2 illustrates the mean changes in these domains by study arm across the three studies.
Table 2.
Summary of Findings for General/Specialist)
| Outcomes | Description | Participants PC/UC (studies) | Certainty of the evidence (GRADE) |
|---|---|---|---|
| Symptom burden (Edmonds et al., 2010,18 Veronese et al., 2017,19 Solari et al., 201820) | Of seven symptoms assessed by all three RCTs using different measures (MS-POS-5S, Core-POS, POS-S-MS, POS-8, VAS) there was a significant improvement in the PC group but not in the UC group over follow-up for pain and sleeping problems, whilst there was no difference between groups for shortness of breath, bladder problems, bowel problems, anxiety and depression | 143 86/57 (3 RCTs) |
⊕⊕⊖⊖ LOWb,c |
| Quality of life (Veronese et al., 2017,19 Solari et al., 201820) | SEIQOL-DW was used in both RCTs. No differences were found on mean change in SEIQOL-DW total score over 16/24 weeks between the PC group and the UC group in both RCTs (P = 0.13/P = 0.88) | 71 43/28 (2 RCTs) |
⊕⊕⊖⊖ LOWb,c |
| Unplanned hospitalizations (Veronese et al., 2017,19 Solari et al., 201820) | In Veronese et al.19 there was one unplanned hospitalization (UC group) versus none in the PC group over 16 weeks. In Solari et al.20 there were 12 (24%) unplanned hospitalizations in the PC group versus seven (27%) in the UC group (P = 0.78) over 24 weeks | 94 60/34 (2 RCTs) |
⊕⊕⊕⊖ MODERATEc |
| Hospital deaths (Edmonds et al., 2010,18 Veronese et al., 2017,19 Solari et al., 201820) | There were five deaths overall: two in Edmonds et al., 201018 (one in the PC group, at the patient's home; one in the UC group, place not specified); none in Veronese et al., 201719; three in Solari et al., 201820 (three in the PC group: two in hospital and one at the patient's home) | 143 86/57 (3 RCTs) |
⊕⊕⊖⊖ LOWb,c |
| Quality of death/dying Complicated bereavement Costs (Higginson et al., 200933) | Not reported Not reported Statistically significant mean total cost saving per patient over 12 weeks of £1789 for PC versus UC (including inpatient and informal caregiver savings). No statistical differences were found for PC (versus UC) in community costs per patient and in costs to informal caregivers; the saving appeared to be mainly due to a lower use of primary and acute hospital services | 52 25/21 (1 RCT) |
⊕⊕⊖⊖ LOWb,c |
| Caregiver quality of life (Solari et al., 201820) | There was no effect of PC (versus UC) on both SF-36 PCS score (P = 0.87) and MCS score (P = 0.96) | 76 50/26 (1 RCT) | ⊕⊕⊖⊖ LOWb,c |
| Caregiver mood (Solari et al., 201820) | There was no effect of PC (versus UC) on both HADS anxiety score (P = 0.50) and HADS depression score (P = 0.45) | 76 50/26 (1 RCT) | ⊕⊕⊖⊖ LOWb,c |
| Caregiver burden (Edmonds et al., 2010,18 Veronese et al., 2017,19 Solari et al., 201820) | The three studies used different measures (CBI, ZBI-12, ZBI-22) and there was no effect of PC (versus UC) in the combined analysis (P = 0.46). For specialist PC data (2 RCTs), there was a reduction in caregiver burden versus no change in UC (ITT analysis only; P = 0.019) | 124 73/51 (3 RCTs) |
⊕⊖⊖⊖ VERY LOWa,c |
Patient or population: patients with severe multiple sclerosis. Setting: home-based patient care. Intervention: palliative care (PC). Comparison: usual care (UC). GRADE Working Group grades of evidence. High certainty: there is great confidence that the true effect lies close to that of the estimate of the effect. Moderate certainty: there is moderate confidence in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: there is very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. CBI, Caregiver Burden Index; Core-POS, Core Palliative Outcome Scale; HADS, Hospital Anxiety and Depression Scale; ITT, intention to treat; MCS, Mental Composite Scale; MS-POS-5S, Multiple Sclerosis Palliative Outcome Scale 5 Symptoms; PCS, Physical Composite Scale; POS-8, Eight-item Palliative outcome Scale; POS-S-MS, Palliative Outcome Scale Symptoms Multiple Sclerosis; RCT, randomized controlled trial; SEIQOL-DW, Schedule for the Evaluation of Individual Quality of Life Direct Weight; SF-36, 36-item Short Form Health Survey; VAS, Visual Analogue Scale; ZBI-12, 12-item Zarit Burden Index; ZBI-22, 22-item Zarit Burden Index. aVery serious risk of bias. bSerious risk of bias. cImprecision.
FIG. 2.
Boxplots of the 0/100 transformed score changes in each of the eight domains, by arm and across the three studies (per-protocol data). The top and bottom of each box are the 25th and 75th percentiles; the horizontal line inside the box is the median; the whiskers are the upper and lower adjacent values; the dots are outlier values.
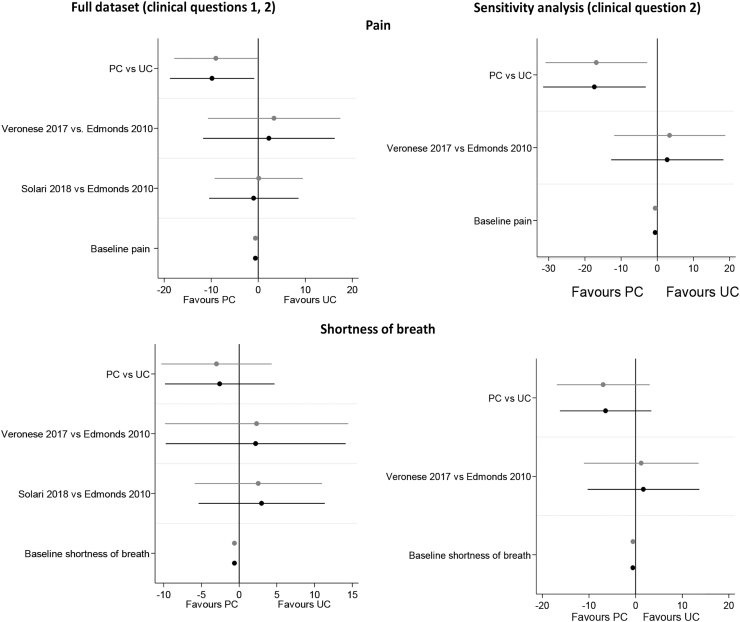
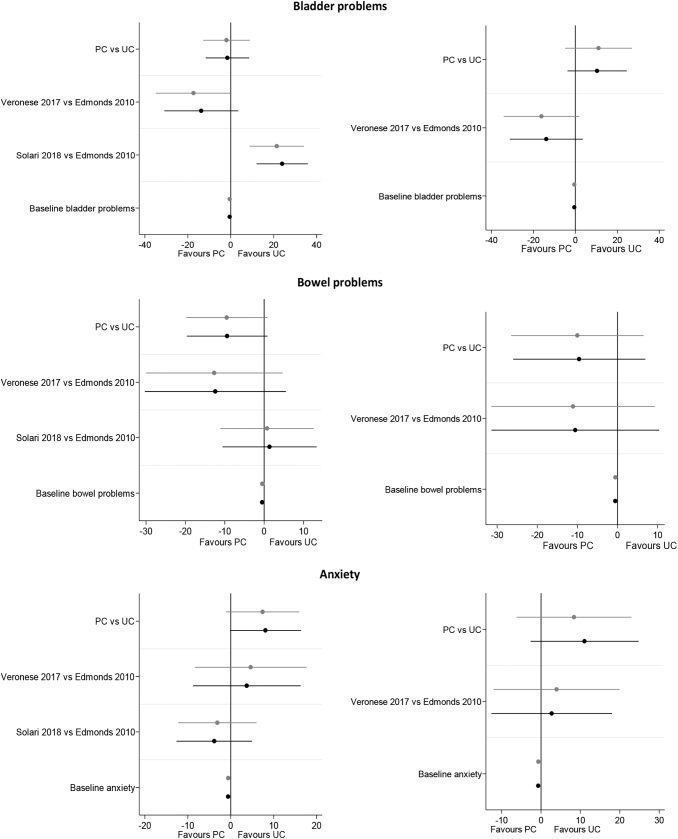
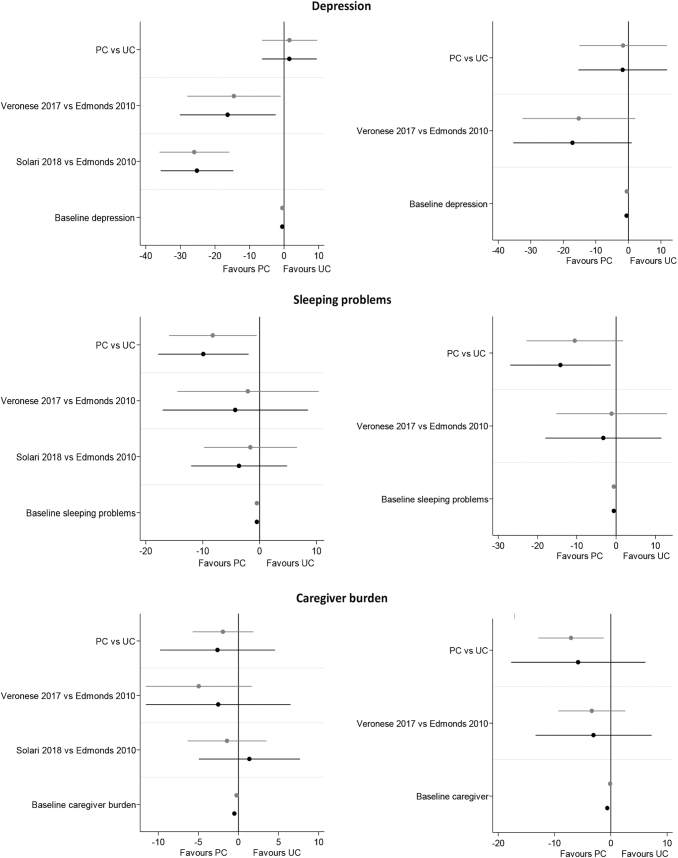
Individual participant data meta-analysis results are reported in Fig. 3 and Table 3, which provide data for the intention-to-treat and per-protocol analyses considering both the full dataset and the sensitivity analyses. Besides the intervention, in each regression model two covariates were retained: the study and the baseline domain score (results with the baseline EDSS score included were similar; data not shown). A statistically significant effect in favour of PC was found on pain (regression coefficient —17.36; 95% CI —31.54 to —3.18) and sleeping problems (regression coefficient —14.15; 95% CI —26.93 to —1.36), whilst there was no effect on the remaining five symptoms and on caregiver burden (Fig. 3; Table 3).
FIG. 3.
Individual participant data meta-analysis results. Intention-to-treat results are reported in black, and per-protocol results are reported in grey. In each model the dependent variable is the 0/100 transformed score change on the domain; the independent variables are the intervention, the study and the 0/100 transformed baseline score. PC, palliative care; UC, usual care.
Table 3.
Individual Participant Data Meta-Analysis Results, with Data Adjusted for Study and Baseline Score
| Domain | Full dataset (clinical questions 1 and 2) |
Sensitivity analysis (clinical question 2) |
||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | P value | 95% CI | Coefficient | SE | P value | 95% CI | |
| Intention to treat | ||||||||
| Pain | 9.81 | 4.52 | 0.032 | −18.76 to −0.85 | −17.36 | 7.09 | 0.017 | −31.54 to −3.18 |
| Shortness of breath | −2.57 | 3.67 | 0.485 | −9.83 to 4.69 | −6.41 | 4.89 | 0.195 | −16.20 to 3.37 |
| Bladder problems | 8.11 | 4.16 | 0.054 | −0.15 to 16.37 | 11.06 | 6.84 | 0.111 | −2.62 to 24.74 |
| Bowel problems | −1.52 | 5.12 | 0.768 | −11.65 to 8.62 | 10.39 | 7.06 | 0.146 | −3.73 to 24.51 |
| Anxiety | −9.38 | 5.19 | 0.073 | −19.65 to 0.88 | −9.56 | 8.22 | 0.249 | −26.03 to 6.90 |
| Depression | 1.54 | 3.99 | 0.700 | −6.37 to 9.44 | −1.74 | 6.79 | 0.798 | −15.38 to 11.89 |
| Sleeping problems | −9.88 | 4.01 | 0.015 | −17.81 to −1.94 | −14.15 | 6.39 | 0.031 | −26.93 to −1.36 |
| Caregiver burden | −2.61 | 3.53 | 0.465 | −9.78 to 4.56 | −5.80 | 5.76 | 0.325 | −17.72 to 6.12 |
| Service satisfactiona | 9.81 | 9.50 | 0.307 | −9.26 to 28.88 | ||||
| Per protocol | ||||||||
| Pain | −8.98 | 4.49 | 0.048 | −17.87 to −0.10 | −16.83 | 7.03 | 0.020 | −30.89 to −2.77 |
| Shortness of breath | −3.00 | 3.70 | 0.420 | −10.31 to 4.32 | −6.94 | 4.97 | 0.168 | −16.89 to 3.01 |
| Bladder problems | −1.94 | 5.49 | 0.724 | −12.81 to 8.93 | 11.09 | 7.96 | 0.170 | −4.89 to 27.06 |
| Bowel problems | −9.50 | 5.20 | 0.070 | −19.79 to 0.79 | −10.02 | 8.24 | 0.229 | −26.50 to 6.47 |
| Anxiety | 7.42 | 4.30 | 0.087 | −1.11 to 15.95 | 8.39 | 7.26 | 0.253 | −6.17 to 22.95 |
| Depression | 1.57 | 4.01 | 0.697 | −6.37 to 9.52 | 1.61 | 6.72 | 0.811 | −15.09 to 11.86 |
| Sleeping problems | −8.22 | 3.90 | 0.037 | −15.92 to −0.51 | −10.50 | 6.16 | 0.093 | −22.82 to 1.82 |
| Caregiver burden | −1.92 | 1.91 | 0.318 | −5.72 to 1.87 | −7.07 | 2.84 | 0.019 | −12.88 to −1.26 |
| Service satisfactiona | 13.68 | 9.92 | 0.174 | −6.22 to 33.59 | ||||
Statistically significant values are reported in bold; CI, confidence interval. aNot assessed in the PeNSAMI study.
The per-protocol analysis was consistent with intention-to-treat findings except for a significant reduction in caregiver burden (mean coefficient —7.07; 95% CI —12.88 to —1.26) in the sensitivity analysis.
In conclusion, three RCTs reporting on the effectiveness of PC services compared to usual care were found. Two studies assessed home-based specialist PC18,19 and one study home-based general PC.20 Studies differed in length of follow-up (12–24 weeks) but were considered sufficiently homogeneous for a quantitative synthesis. Overall, there is low certainty in our findings, mostly due to risk of bias and imprecision. Also, publication bias cannot be ruled out.
A statistically significant effect in favour of PC was found for two of the eight domains considered, pain and sleeping problems. A per-protocol analysis additionally found a reduction in caregiver burden, for specialist PC only. There is no evidence of effects on quality of life and on the other outcomes. No studies were found on inpatient or outpatient PC.
Recommendation
It is suggested that home-based PC is offered to patients with severe MS, either by HPs with good basic PC skills and knowledge (general PC) or by multi-professional teams of PC specialists (specialist PC) (weak recommendation, low certainty evidence).
Good practice statement
It is suggested that inpatient or outpatient PC is offered to patients with severe MS. Patient preference, living conditions and availability of PC services should be taken into account.
Recommendations pertaining to clinical questions 3–10 are reported below. A full report which also contains the references of the included studies for these questions is available in Appendix S5.
Advance care planning (clinical question 3)
According to the EAPC, advance care planning (ACP) is a process that enables individuals who have decisional capacity to identify their values, to reflect upon the meanings and consequences of serious illness scenarios, to define goals and preferences for future medical treatment and care, and to discuss these with family and HPs. ACP addresses individuals' concerns across the physical, psychological, social, and spiritual domains. It encourages individuals to identify a personal representative and to record and regularly review any preferences, so that their preferences can be taken into account should they, at some point, be unable to make their own decisions.36
Of 617 records screened, seven were assessed as full text and excluded from the final selection (Appendix S5). From a systematic review,37 there is no evidence of the effects of ACP for people with neurological diseases, including MS. However, there is some evidence from other progressive and life-threatening illnesses that ACP decreases the use of life-sustaining treatment, increases hospice/PC, reduces hospitalizations and increases compliance with patients' end-of-life wishes.37
Concerning MS, there is evidence that patients and caregivers often would like to discuss the issues of death and dying and HPs should acknowledge and encourage these discussions.38,39 Often professionals leave discussions until the later stages of progression in MS.40 Patients react in different ways on discussion of future planning: a small study showed that some MS patients made clear decisions, some undertake some planning but without a clear advance directive and some were still ‘hoping for a cure’ and did not wish to look ahead.41 However, caregivers may be left having difficult decisions if no planning has taken place and this is stressful for caregivers.42
Good practice statements
-
1.
It is suggested that early discussion of the future with ACP is offered to patients with severe MS.
-
2.
It is suggested that regular communication about the future progression of MS is undertaken with patients and families/caregivers.
Patient discussion with HPs of their wish to hasten death (clinical question 4)
Healthcare professionals' acknowledgment of, and open discussion about, the patient's wish to hasten death and related issues emerged as key from both TF members (chiefly PC physicians) and MS patients.13 Of 491 records screened, seven were assessed as full text and excluded from the final selection (Appendix S5). Berkman et al.43 reported that 33% of MS patients considered suicide or assisted dying. In more recent studies, 22% of MS patients had suicidal intention,44 and 7% would consider suicide and 65% assisted dying if they had unbearable pain.45 Suicidal ideation or consideration of assisted dying was related to depression, hopelessness, MS affecting leisure time and feeling socially isolated.11,46 Access to PC expertise has been recommended for individuals requesting euthanasia or physician-assisted suicide as further assessment and management of symptoms, psychosocial or spiritual distress.47
Good practice statements
-
1.
Patients should be encouraged to discuss their wishes about future care, including the restriction of treatment and interventions and the wish for hastened death.
-
2.
Healthcare professionals should be aware of the risk factors for the wish for hastened death – including depression, isolation, restricted abilities – and encourage the discussion of these issues and the appropriate management.
Symptom management (clinical question 5)
This patient population is characterized by the presence of multiple symptoms, in variable combinations between patients and in the same patient over time (Table 4). The management of pain and other symptoms is at the core of PC. Nevertheless, some symptoms (e.g. spasticity, fatigue) typically affect MS patients and were not addressed in clinical questions 1 and 2. Patients with severe MS should be carefully and regularly assessed in order to proactively detect their bio-psychosocial symptoms. Whenever necessary (e.g. in patients with severe cognitive compromise or communication problems), interviews with patient caregivers and the use of proxy versions of symptom scales should be added to patient assessment.
Table 4.
Publications Found for Each Specified Symptom (10 Out of 43 Trials Addressed More Than One Symptom)
| Symptom | Publications | Trials | Publication year (min–max) |
|---|---|---|---|
| Spasticity | 32 | 31 | 1975–2017 |
| Fatigue | 10 | 9 | 2001–2017 |
| Paina | 7 | 6 | 2003–2017 |
| Sleeping problemsa | 6 | 5 | 2003–2017 |
| Bladder problemsa | 6 | 4 | 1996–2006 |
| Mobility/transfer | 5 | 5 | 1996–2017 |
| Tremor | 4 | 3 | 2003–2009 |
| Balance | 1 | 1 | 2015 |
| Arm function | 1 | 1 | 2018 |
| Swallowing (e.g. dysphagia) | 0 | − | − |
| Bowel problemsa | 0 | − | − |
| Communication (e.g. dysarthria) | 0 | − | – |
| Depressed mooda | 0 | – | – |
| Cognitive problems | 0 | – | – |
| Sexual problems | 0 | – | – |
| Shortness of breath/ dyspnoeaa | 0 | – | – |
| Nausea, vomiting | 0 | – | – |
| Poor appetite/anorexia | 0 | – | – |
| Mouth problems | 0 | – | – |
Also addressed in clinical questions 1 and 2 (general and specialist palliative care).
Of 7195 records screened, 530 were assessed as full text and 44 (43 trials) were included. Ten publications addressed more than one symptom. The symptom with the highest number of publications was spasticity, followed by fatigue and pain (Table 4).
Considering the type of intervention, 32/43 trials (75%) were on pharmacological interventions, 10 (23%) on non-pharmacological approaches and one (2%) was a trial assessing a combination of botulinum toxin A and physiotherapy. No studies on interventions targeted to the management of 10/19 pre-specified symptoms were found in our literature search (Table 4). Further, the included studies reported on few of our predefined outcomes. Recommendations on four symptoms (spasticity, fatigue, pain and bladder problems) were produced. For each symptom, a full report is available in Appendix S5 and summary of findings tables in Appendix S6.
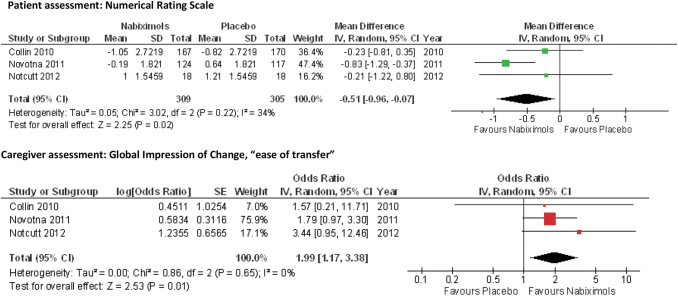
Spasticity
The majority of the included publications (32/44, 73%; 31 trials) addressed spasticity as an outcome. Of these, 26 trials (84%) addressed drugs (baclofen, benzodiazepines, cannabinoids, GABAergics, tizanidine and botulinum toxin) and five trials addressed nonpharmacological treatments (exercise, radial shock wave therapy and transcutaneous electrical nerve stimulation). A meta-analysis was performed for nabiximols: all the three RCTs23–25 shared the patient-reported NRS for spasticity and CGIC ‘ease of transfer’ (Table 5). Mean NRS spasticity difference favoured nabiximols (—0.51; 95% CI —0.96 to —0.07); and the odds ratio for CGIC ‘ease of transfer’ improvement was 1.99 (95% CI 1.17–3.38) for nabiximols versus placebo (Fig. 4).
Table 5.
Summary of Findings for Nabiximols to Treat Spasticity (Clinical Question 5)
| Outcomes | Description | No. of participants IG/CG (studies) | Certainty of the evidence (GRADE) |
|---|---|---|---|
| Symptom burden (meta-analysis) (Collin et al., 2010,23 Novotna et al., 2011,24 Notcutt et al., 201225) | The meta-analysis showed a significant difference between groups for spasticity NRS (mean difference −0.51, 95% CI −0.96 to −0.07) | 614 309/305 (3 RCTs) |
⊕⊕⊕⊖ MODERATEa |
| Symptom burden (MAS) (Collin et al., 2010,23 Novotna et al., 2011,24 Notcutt et al., 201225) | There were no significant differences between groups in the MAS scores | 614 309/305 (3 RCTs) | ⊕⊕⊕⊖ MODERATEa |
| Symptom burden (SGIC) (Novotna et al., 2011,24 Notcutt et al., 201225) | There were significant differences between groups favouring nabiximols | 277 142/135 (2 RCTs) | ⊕⊕⊕⊖ MODERATEa |
| ADL (Collin et al., 2010,23 Novotna et al., 201124) | There was a significant difference between groups in Novotna et al. favouring nabiximols, but not in Collin et al. | 578 291/287 (2 RCTs) |
⊕⊕⊖⊖ LOWa,b |
| QOL (Collin et al., 2010,23 Novotna et al., 201124) | There was no difference between groups in Collin et al. (EQ-5D, MSQOL-54) and Novotna et al. (EQ-5D, SF-36) | 578 291/287 (2 RCTs) | ⊕⊕⊕⊖ MODERATEa |
| CGIC (ease of transfer, meta-analysis) (Collin et al., 2010,23 Novotna et al., 2011,24 Notcutt et al., 201225) | The meta-analysis of CGIC showed a significant difference between groups (OR 1.99, 95% CI 1.17–3.38) | 614 309/305 (3 RCTs) | ⊕⊕⊕⊖ MODERATEa |
| Adverse events (Collin et al., 2010,23 Novotna et al., 2011,24 Notcutt et al., 201225) | Collin et al.: A total of 55 patients (16%) discontinued treatment early; 35 (21%) in the nabiximols group and 20 (12%) in the placebo group. Of these 55 patients, 32 (58%) withdrew from the study. The primary reason given for withdrawal was AE occurrence: nine patients (5%) on nabiximols and five (3%) on placebo. The following AEs were reported more frequently in the nabiximols group compared to placebo: dizziness [53/167 (32%) vs. 17/170 (10%)], fatigue [42/167 (25%) vs. 32/170 (19%)], somnolence [24/167 (14%) vs. 7/170 (4%)], nausea [53/ 167 (32%) vs. 17/170 (10%)], asthenia [26/167 (16%) vs. 11/170 (6%)] and vertigo [19/167 (11%) vs. 7/170 (4%)]. Two subjects died from cancer during the study: neither death was considered to be related to the (active) study medication Notcutt et al.: There was one SAE (pain in hip and thigh and lumbar spinal stenosis) in a patient on nabiximols, which was considered unrelated to study medication. The only AE reported in association with abnormal laboratory values was a mild increase in gamma-glutamyl transferase in one patient on nabiximols. Novotna et al.: 17 patients discontinued the treatment early (7%); 15 were on nabiximols (four due to AEs, 11 due to withdrawal of consent). AEs were overall few and similar between nabiximols and placebo, with no single event occurring at a rate >10% in either group; the most common AEs were vertigo (6% nabiximols vs. 1% placebo) and fatigue (5% vs. 1%) |
614 309/305 (3 RCTs) |
⊕⊕⊕⊖ MODERATEa |
Patient or population: people with severe multiple sclerosis (and spasticity). Setting: research hospitals, outpatients. Intervention: nabiximols (2.7 mg D9-tetrahydrocannabinol and 2.5 mg cannabidiol, up to 24 sprays in 24 h) for 4–15 weeks. Comparison: placebo. GRADE Working Group grades of evidence. High certainty: there is great confidence that the true effect lies close to that of the estimate of the effect. Moderate certainty: there is moderate confidence in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: there is very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of the effect. ADL, activities of daily living; AE, adverse event; CG, control group; CGIC, carer global impression of change; CI, confidence interval; EQ-5D, EuroQol-5 Dimensions; IG, intervention group; MAS, modified Ashworth scale; MSQOL-54, Multiple Sclerosis Quality of Life 54 items; NRS, numerical rating scale; OR, odds ratio; QOL, quality of life; RCT, randomized controlled trial; SAE, serious adverse event; SF-36, 36-item Short Form Health Survey; SGIC, subjective global impression of change. aSevere risk of bias. bInconsistency.
FIG. 4.
Efficacy of nabiximols (versus placebo) to treat spasticity: forest plots of patient and caregiver assessments. CI, confidence interval; df, degree of freedom; IV, instrumental variable.
Recommendations
-
1.
Nabiximols are recommended to reduce spasticity in patients with severe MS. Drug availability, the presence of other symptoms and possible adverse events should be considered in treatment decision-making (strong recommendation/moderate certainty evidence).
-
2.
Oral baclofen is suggested to reduce spasticity in patients with severe MS (weak recommendation/ very low certainty evidence). Presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
3.
Intrathecal baclofen is suggested to reduce spasticity in patients with severe MS (weak recommendation/very low certainty evidence). The presence of other symptoms and possible adverse events (related to the drug and to pump and catheter placement/replacement) should be considered in treatment decision-making.
-
4.
Tizanidine is suggested to reduce spasticity in patients with severe MS (weak recommendation/ low certainty evidence). The presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
5.
GABAergic drugs are suggested to reduce spasticity in patients with severe MS (weak recommendation/low or very low certainty evidence). The presence of other symptoms and possible adverse events should be considered in treatment decisionmaking.
-
6.
Other cannabinoids (D9-tetrahydrocannabinol or cannabis sativa plant extract) are suggested to reduce spasticity in patients with severe MS (weak recommendation/moderate certainty evidence). Drug availability, the presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
7.
Botulinum toxin A is suggested to reduce hip adductor spasticity in patients with severe MS (weak recommendation/low certainty evidence). The presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
8.
Exercise is suggested to reduce spasticity in patients with severe MS (weak recommendation/ very low certainty evidence), considering patient preferences and resource availability.
-
9.
Transcutaneous electrical nerve stimulation is suggested to reduce spasticity in patients with severe MS (weak recommendation/very low certainty evidence), considering patient preferences and resource availability.
-
10.
It is suggested that benzodiazepines are not used to reduce spasticity in patients with severe MS due to insufficient evidence for efficacy and frequent adverse events (weak recommendation/very low certainty evidence).
Fatigue
In total, 10/44 publications (nine trials) addressed fatigue as an outcome. Five of these publications (four trials) considered drugs (cannabinoids and 4-aminopyridine) and five publications considered exercise (Appendices S5, S6). Because of the limited direct evidence on the efficacy of interventions for fatigue in this population, the TF decided to include indirect evidence available from the National Institute for Health and Care Excellence (NICE) guidance on the management of MS in primary and secondary care48 and the Cochrane review on exercise therapy for fatigue in MS.49
Recommendations
-
1.
D9-tetrahydrocannabinol or cannabis plant extract (weak recommendation/low certainty evidence) or 4-aminopyridine (weak recommendation/very low certainty evidence) is suggested to treat fatigue in patients with severe MS. Drug availability, the presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
2.
Exercise training is suggested to treat fatigue in patients with severe MS. This includes robot-assisted gait training, inspiratory muscle training, upper body endurance training and manual wheelchair propulsion training (weak recommendation/ very low certainty evidence). Patient preferences and the setting and availability of the apparatus should be considered in decision-making.
-
3.
It is suggested that nabiximols are not used to treat fatigue in patients with severe MS (weak recommendation/low certainty evidence).
Additional recommendations based on indirect evidence (weak recommendations/very low certainty evidence)
-
1.
It is suggested that amantadine is used to treat fatigue in patients with severe MS.
-
2.
Mindfulness-based training, cognitive behavioural therapy, fatigue management programmes or other exercise training is suggested to treat fatigue in patients with severe MS. Patient preferences and the setting and availability of the programme should be considered in decision-making.
Pain
Seven full-text publications (six trials) addressed pain as an outcome: five were on drugs (cannabinoids) and two on non-pharmacological treatments (Appendices S5, S6). Because of the limited direct evidence on the efficacy of interventions for pain in this population, the TF decided to include indirect evidence available from pertinent EAN and NICE guidelines.50–52
Recommendations
-
1.
Any of the three different cannabinoid preparations (D9-tetrahydrocannabinol, cannabis sativa plant extract or nabiximols) are suggested to reduce pain in patients with severe MS (weak recommendation/low certainty evidence). Drug availability, the presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
2.
Radial shock wave therapy (weak recommendation/low certainty evidence) or transcutaneous electrical nerve stimulation (preferably 8-h application time; weak recommendation/very low certainty evidence) are suggested to reduce pain in patients with severe MS. Patient preferences and treatment availability should be considered in treatment decision-making.
Additional recommendations based on indirect evidence (weak recommendations/very low certainty evidence)
-
1.
Gabapentin, pregabalin, amitriptyline, duloxetine or lamotrigine is suggested to reduce pain in patients with severe MS. The presence of other symptoms and possible adverse events should be considered in treatment decision-making.
-
2.
Opioids might be considered if long-term pain treatment is not an issue.
-
3.
Carbamazepine or oxcarbazepine is suggested for patients with severe MS and trigeminal neuralgia. Second choice drugs might be lamotrigine, gabapentin, botulinum toxin type A, pregabalin, baclofen and phenytoin, used either alone or as add-on therapy. Surgery might be offered if medical treatment is not effective or is poorly tolerated.
Bladder problems
Bladder symptoms are present in over 90% of patients with progressive MS. Difficulty with storage control (urinary frequency, urgency and incontinence) is the most common symptom, caused by neurogenic detrusor overactivity. Approximately half of the patients have coexistent voiding difficulty due to detrusorsphincter-dyssynergia.53
Six of the 44 included publications (four trials) addressed drugs to improve urinary continence in severely affected MS patients (Table 4). Two studies were crossover RCTs: one compared antimuscarinics for urinary incontinence and one desmopressin intranasal spray to placebo for nocturia. Two studies were RCTs on cannabinoids which included urinary symptoms as secondary outcomes. These drugs are generally used in combination with (self-)catheterization. A range of other drugs (e.g. new antimus-carinics, mirabegron) and neurostimulation/ neuromodulation approaches are now available, which need to be proved effective in this population (Appendices S5, S6). Because of the limited direct evidence on the efficacy of interventions for bladder symptoms in this population, the TF decided to include indirect evidence available from the NICE guideline on urinary incontinence in neurological disease.54
Recommendations
-
1.
Antimuscarinic drugs are suggested to improve urinary continence in patients with severe MS (weak recommendation/very low certainty evidence). The presence of other symptoms (e.g. cognitive problems) and possible adverse events should be considered when deciding on the most suitable preparation, dose and route of administration.
-
2.
D9-tetrahydrocannabinol or cannabis extract is suggested to improve urinary continence in patients with severe MS (weak recommendation/low certainty evidence). Drug availability, the presence of other symptoms and possible adverse events should be considered in decisionmaking.
-
3.
Desmopressin intranasal spray is suggested for nocturia in patients with severe MS (weak recommendation/very low certainty evidence). The drug should not be offered to patients with uncontrolled hypertension, cardiovascular and/or renal diseases. Possible adverse events should be considered in decision-making.
-
4.
It is suggested that nabiximols are not used to improve urinary continence in patients with severe MS due to insufficient evidence for efficacy (weak recommendation/low certainty evidence).
Additional recommendations based on indirect evidence (weak recommendations/very low certainty evidence)
-
1.
Behavioural management programmes (e.g. timed voiding, bladder retraining or habit retraining) are suggested to improve urinary continence in patients with severe MS.
-
2.
Pelvic floor muscle training – alone or in combination with biofeedback and/or electrical stimulation of the pelvic floor – is suggested to improve urinary continence in patients with severe MS.
-
3.
It is suggested that patients with severe MS with a persistent residual volume >100 ml are offered the opportunity to learn clean intermittent self-catheterization. If self-catheterization is not possible, a patient carer can be trained to catheterize the patient.
-
4.
If clean intermittent (self-)catheterization is no longer possible, a long-term indwelling catheter (preferably suprapubic) might be offered.
-
5.
Patients with severe MS in whom antimuscarinic drugs have proved to be ineffective or poorly tolerated might be offered intradetrusor injections of botulinum toxin A.
Multidisciplinary rehabilitation (clinical question 6)
According to Wade55 rehabilitation is a problem-solving educational process aimed at reducing symptoms and limitations at the level of activity and participation. Multidisciplinary rehabilitation encompasses different interventions applied by a number of different (health) professionals, including physiotherapists, physicians, nurses, occupational therapists, psychologists. It is frequently delivered in rehabilitation clinics on an inpatient or outpatient basis and sometimes at community centres or the patients' home. Khan et al.56 defined multidisciplinary (also called interdisciplinary) rehabilitation as ‘an inpatient, outpatient, home or community-based coordinated intervention, delivered by two or more disciplines in conjunction with physician consultation (neurologist or rehabilitation medicine physician), which aims to limit patient symptoms, and enhance functional independence and maximize participation, as defined by ICF [International Classification of Functioning, Disability and Health].’57
Eleven publications were found reporting on nine trials (eight RCTs and one controlled clinical trial) that differed in terms of setting, intervention (components, duration and intensity), outcomes and length of follow-up. Therefore it was not possible to perform meta-analyses, and results were summarized descriptively (Appendices S5, S6).
Recommendations
-
1.
It is suggested that multidisciplinary rehabilitation is offered to patients with severe MS (weak recommendation/very low or low certainty evidence).
-
2.
Multidisciplinary rehabilitation might be offered either as inpatient, outpatient or home-based rehabilitation or as a combination (weak recommendation/very low or low certainty evidence). Patients' preference and other circumstances (transport, situation at home and resources) should be taken into account when deciding on the setting.
Interventions for caregivers (clinical questions 7 and 8)
Two clinical questions concerned interventions for caregivers, in terms of structured education and training programmes on caregiving, and of structured, practical and/or emotional support programmes (Appendix S2). One RCT58 comparing a 2-year, community-based, comprehensive care programme for MS patients and caregiver units to usual care were included. The trial (also included in clinical question 6 on multidisciplinary rehabilitation) addressed both clinical questions 7 and 8, as the programme included education as well as practical and emotional support for caregivers (Appendix S5).
Recommendations
-
1.
It is suggested that caregivers of patients with severe MS are offered education and training programmes on caregiving (weak recommendation/ very low certainty evidence). Caregivers' preferences and habits should be taken into account when deciding on the setting of the programme, e.g. hospital based, home based or online.
-
2.
It is suggested that caregivers of patients with severe MS are offered practical and emotional support (weak recommendation/very low certainty evidence). Caregivers' preferences and habits should be taken into account when deciding on the setting of the support programme.
Interventions for HPs (clinical questions 9 and 10)
Finally, two clinical questions concerned education and training for HPs: one concerned training in PC/ specialist PC for MS HPs, and one training in MS for PC HPs (Appendix S2). No evidence was found regarding the effectiveness of any of these training programmes (of 37 records screened, two were assessed as full text and excluded from the final selection; Appendix S5). There is increasing discussion of the need for close collaboration between PC and neurology, and for neurologists to receive training in basic PC principles.59–62 It has been recommended that neurologists should have familiarity and comfort with communicating bad news, engaging in end-of-life conversations and ACP, caregiver assessment and other PC skills. On the other hand, PC teams may also need specialized training for managing MS patients. The required competences can be achieved through enhanced joint training within the two specialties.62 Despite efforts to improve the PC training of neurology residents,63 there is no evidence available as to its use or effectiveness and recommendations can only be made by consensus using the evidence from the literature.10
Good practice statements
-
1.
It is suggested that the principles of PC are included in the training and continuing education of neurologists and other HPs involved in MS care.
-
2.
It is suggested that the principles of the management of MS patients are included within the training and continuing education of specialist PC professionals.
Discussion
Recognizing significant variation in the PC of patients with severe MS across Europe, the EAN assembled a TF to summarize the existing evidence and develop a clinical practice guideline. To ensure client involvement the TF included a person with MS who participated in all aspects of the development of the guideline; in addition, MS patients and caregivers were involved via an international online survey and focus group meetings in the formulation of the 10 clinical questions.13
For four clinical questions (1, 2, 5 and 6) the TF produced 34 recommendations (one of which was a strong recommendation) and one good practice statement. For interventions for caregivers (clinical questions 7 and 8) only one study was found. No research evidence was found for four clinical questions: ACP (3), discuss with HPs the wish to hasten death (4), and interventions for HPs (9, 10). For these four clinical questions, the TF produced six good practice statements. Thus, there is currently a knowledge gap on many questions in this population, and on several outcomes considered as important by stakeholders (Fig. 1).
Two pertinent studies have been published since the search was closed. One was a Cochrane review on PC in MS patients, which included the same RCTs as in our IPDMA.64 It should be noted, however, that in this systematic review pain and sleeping problems were considered as PC adverse events and the pre-specified secondary outcome measures included relapse-free survival, progression-free survival, neuropsychological assessment and the EDSS.64 The other study was a pragmatic RCT from the UK, which demonstrated that a standing frame programme significantly increased motor function in people with severe MS and was cost-effective in comparison to standard care.65
The limited evidence on PC in MS (and in other neurological conditions) contrasts with the situation in oncology.10 The TF agreed on the formulation of good practice statements (instead of abstaining from any recommendation) in response to clinical questions where evidence was lacking. This was the case for ACP where, besides the all-important differences in clinical features, commonalities may exist in the psychosocial and spiritual needs across patient populations. Whilst emphasizing the need to produce evidence in MS, consensus documents on ACP and interventions currently available for other conditions can inspire MS clinicians to have effective conversations with their patients and patient significant others and stimulate research in this area.37,66,67
Conclusion
This clinical practice guideline provides evidence-based recommendations of PC in severely affected MS patients. Areas that currently lack evidence of efficacy include ACP, the management of symptoms such as fatigue and mood problems in this population, and interventions for caregivers and HPs. Further research on the integration of PC and MS care is needed, including consideration of the various models of PC provision.
Supplementary Material
Acknowledgments
This is a joint initiative of the EAN (approval date: February 27, 2020), the EAPC RIMS(approval date: February 22, 2020) and the RIMS (approval date: February 24, 2020), and has been endorsed by the ECTRIMS and by the MSIF. Irene Higginson is thanked for providing patient individual data of the UK trial on PC for MS patients. The persons with MS, the caregivers and the HPs who provided their valuable input are thanked. The Bulgarian Movement Disorders and MS Society, the Bulgarian MS Patient Association, the Danish MS Society, the Dutch MS Society, the German MS Society, the Israel MS Society, the Italian MS Society, the Serbian MS Society, the Spanish MS Society and the UK MS Society are also thanked. The guideline was funded by the EAN and by the Foundation of the Italian MS Society (FISM grant number 2017/S/2). Travel expenses (two people participating in a task force meeting) were covered by the RIMS.
Contributor Information
Collaborators: on behalf of the Guideline Task Force
Data Availability Statement
The data that support the findings of this guideline are available in the Supplementary Material of this article.
Author Disclosure Statement
Dr Solari reports grants from the FISM and the European Academy of Neurology, during the conduct of the study; other from Merck Serono and Novartis; and personal fees from Almirall, Excemed, Genzyme, Merck Serono and Teva, outside the submitted work. Dr Sastre-Garriga reports grants and personal fees from Genzyme, Biogen, Merck, Almirall, Novartis, Roche, TEVA and Celgene; other from Revista de Neurologia, and Multiple Sclerosis Journal, outside the submitted work. Dr Kleiter reports personal fees from Bayer, Biogen, Novartis, IQVIA, Merck, Sanofi Genzyme, Roche, Mylan, Alexion and Celgene; grants and personal fees from Chugai; grants from Diamed, outside the submitted work. Dr Drulovic reports personal fees from Bayer Schering, Merck Serono, Sanofi Genzyme, Teva Actavis, Novartis and Medis; grants from the Ministry of Education, Science, and Technical Development, Republic of Serbia, outside the submitted work. Dr Milo reports personal fees from Actelion, Biogen and Medison Pharma; grants, personal fees and other from Merck Serono and Teva; personal fees and other from Novartis, Roche; other from TG Therapeutics and MAPI-Pharma, outside the submitted work. Dr Pekmezovic reports grants from the Ministry of Education, Science and Technological Development of the Republic of Serbia; personal fees from Teva Actavis, Merck and Roche, outside the submitted work. Dr Patti reports personal fees from Almirall, Bayer, Celgene, Roche, Novartis, Sanofi and TEVA; grants and personal fees from Biogen and Merck; grants from Reload Onlus, FISM and MIUR, outside the submitted work. Dr Voltz reports personal fees from Prostrakan, Pfizer, MSD Sharp&-Dome and AOK; grants from TEVA/EffenDys, Otsuka, and DMSG/Hertie Stiftung, outside the submitted work. All the other authors have nothing to declare.
Supplementary Material
References
- 1. Filippi M, Bar-Or A, Piehl F, et al. : Multiple sclerosis. Nat Rev Dis Primers 2018;4:43. [DOI] [PubMed] [Google Scholar]
- 2. Scalfari A, Neuhaus A, Daumer M, et al. : Onset of secondary progressive phase and longterm evolution of multiple sclerosis. J Neurol Neurosurg Psychiatry 2014;85:67–75 [DOI] [PubMed] [Google Scholar]
- 3. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 1983;33:1444–1452 [DOI] [PubMed] [Google Scholar]
- 4. Fraser R, Ehde D, Amtmann D, et al. : Self-management for people with multiple sclerosis: Report from the first international consensus conference. Int J MS Care 2013;15:99–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hirst C, Swingler R, Compston DA, et al. : Survival and causes of death in multiple sclerosis: A prospective population-based study. J Neurol Neurosurg Psychiatry 2008;79:1016–1021 [DOI] [PubMed] [Google Scholar]
- 6. Sumelahti ML, Hakama M, Elovaara I, et al. : Causes of death among patients with multiple sclerosis. Mult Scler 2010;16:1437–1442 [DOI] [PubMed] [Google Scholar]
- 7. Lunde HMB, Assmus J, Myhr KM, et al. : Survival and cause of death in multiple sclerosis: A 60-year longitudinal population study. J Neurol Neurosurg Psychiatry 2017;88:621–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Campbell CW, Jones EJS, Merrills J. Palliative and end-of-life care in advanced Parkinson's disease and multiple sclerosis. J Clin Med 2010;10:290–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sleeman KE, Ho YK, Verne J, et al. : Place of death, and its relation with underlying cause of death, in Parkinson's disease, motor neuron disease, and multiple sclerosis: A population-based study. Palliat Med 2013;27:840–846 [DOI] [PubMed] [Google Scholar]
- 10. Oliver DJ, Borasio GD, Caraceni A, et al. : A consensus review on the development of palliative care for patients with chronic and progressive neurological disease. Eur J Neurol 2016;23:30–38 [DOI] [PubMed] [Google Scholar]
- 11. Strupp J, Ehmann C, Galushko M, et al. : Risk factors for suicidal ideation in patients feeling severely affected by multiple sclerosis. J Palliat Med 2016;19:523–528 [DOI] [PubMed] [Google Scholar]
- 12. de Groot V. There is an urgent need for palliative care specialists in MS—Commentary. Mult Scler 2019;25:1713–1714 [DOI] [PubMed] [Google Scholar]
- 13. Köpke S, Giordano A, Veronese S, et al. : Patient and caregiver involvement in formulation of guideline questions: Findings from the EAN guideline on palliative care of people with severe multiple sclerosis. Eur J Neurol 2019;26:41–50 [DOI] [PubMed] [Google Scholar]
- 14. Leone MA, Keindl M, Schapira AH, et al. : Practical recommendations for the process of proposing, planning and writing a neurological management guideline by EAN task forces. Eur J Neurol 2015;22:1505–1510 [DOI] [PubMed] [Google Scholar]
- 15. Guyatt GH, Oxman AD, Kunz R, et al. : GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol 2011;64:395–400 [DOI] [PubMed] [Google Scholar]
- 16. Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (eds). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 ed. Chichester: The Cochrane Collaboration and John Wiley & Sons Ltd, 2011, pp. 187–242 [Google Scholar]
- 17. Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: Rationale, conduct, and reporting. BMJ 2010;340:c221. [DOI] [PubMed] [Google Scholar]
- 18. Edmonds P, Hart S, Gao Wei, et al. : Palliative care for people severely affected by multiple sclerosis: Evaluation of a novel palliative care service. Omega J Death Dying 2010;16:627–636 [DOI] [PubMed] [Google Scholar]
- 19. Veronese S, Gallo G, Valle A, et al. : Specialist palliative care improves the quality of life in advanced neurodegenerative disorders: NE-PAL, a pilot randomised controlled study. BMJ Support Palliat Care 2017;7:164172. [DOI] [PubMed] [Google Scholar]
- 20. Solari A, Giordano A, Patti F, et al. : Randomized controlled trial of a home-based palliative approach for people with severe multiple sclerosis. Mult Scler 2018;24:663–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: One-stage and two-stage approaches, and why they may differ. Stat Med 2017;36:855–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Donders AR, van der Heijden GJ, Stijnen T, et al. : Review: A gentle introduction to imputation of missing values. J Clin Epidemiol 2006;59:1087–1091 [DOI] [PubMed] [Google Scholar]
- 23. Collin C, Ehler E, Waberzinek G, et al. : A double-blind, randomized, placebo-controlled, parallel-group study of Sativex, in subjects with symptoms of spasticity due to multiple sclerosis. Neurol Res 2010;32:451–459 [DOI] [PubMed] [Google Scholar]
- 24. Novotna A, Mares J, Ratcliffe S, et al. : A randomized, double-blind, placebo-controlled, parallel-group, enriched-design study of nabiximols* (Sativex®), as add-on therapy, in subjects with refractory spasticity caused by multiple sclerosis. Eur J Neurol 2011;18:1122–1131 [DOI] [PubMed] [Google Scholar]
- 25. Notcutt W, Langford R, Davies P, et al. : A placebo-controlled, parallel-group, randomized withdrawal study of subjects with symptoms of spasticity due to multiple sclerosis who are receiving long-term Sativex® (nabiximols). Mult Scler 2012;18:219–228 [DOI] [PubMed] [Google Scholar]
- 26. Hsu CC, Sanford BA. The Delphi technique: Making sense of consensus. Pract Assess Res Eval 2007;12:1–8 [Google Scholar]
- 27. Sepulveda C, Marlin A, Yoshida T, et al. : Palliative care: The World Health Organization's global perspective. J Pain Symptom Manage 2002;24:91–96 [DOI] [PubMed] [Google Scholar]
- 28. Radbruch L, Payne S. White paper on standards and norms for hospice and palliative care in Europe: Part 1. Eur J Palliat Care 2009;16:278–289 [Google Scholar]
- 29. Embrey N. Exploring the lived experience of palliative care for people with MS, 2: Therapeutic interventions. Br J Neurosci Nurs 2009;5:311–318 [Google Scholar]
- 30. Embrey N. Exploring the lived experience of palliative care for people with MS, 3: Views of group support. Br J Neurosci Nurs 2009;5:402–408 [Google Scholar]
- 31. Borreani C, Bianchi E, Pietrolongo E, et al. : Unmet needs of people with severe multiple sclerosis and their carers: Qualitative findings for a home-based intervention. PLoS One 2014;9:e109679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Higginson IJ, Hart S, Burman R, et al. : Randomised controlled trial of a new palliative care service: Compliance, recruitment and completeness of follow-up. BMC Palliat Care 2008;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Higginson IJ, McCrone P, Hart SR, et al. : Is short-term palliative care cost-effective in multiple sclerosis? A randomized phase II trial. J Pain Symptom Manage 2009;38:816–826 [DOI] [PubMed] [Google Scholar]
- 34. Solari A, Giordano A, Grasso MG, et al. : Home-based palliative approach for people with severe multiple sclerosis and their carers: Study protocol for a randomized controlled trial. Trials 2015;16:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Giovannetti AM, Borreani C, Bianchi E, et al. : Participant perspectives of a home-based palliative approach for people with severe multiple sclerosis: A qualitative study. PLoS One 2018;13:e0200532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rietjens JAC, Sudore RL, Connolly M, et al. : Definition and recommendations for advance care planning: An international consensus supported by the European Association for Palliative Care. Lancet Oncol 2017;18:e543–e551 [DOI] [PubMed] [Google Scholar]
- 37. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: A systematic review. Palliat Med 2014;28:1000–1025 [DOI] [PubMed] [Google Scholar]
- 38. Golla H, Mammeas S, Galushko M, et al. : Unmet needs of caregivers of severely affected multiple sclerosis patients: A qualitative study. Palliat Support Care 2015;13:1685–1693 [DOI] [PubMed] [Google Scholar]
- 39. Golla H, Galushko M, Strupp J, et al. : Patients feeling severely affected by multiple sclerosis: Addressing death and dying. Omega J Death Dying 2016;74:275–291 [Google Scholar]
- 40. Walter HAW, Seeber AA, Willems DL, de Visser M. The role of palliative care in chronic progressive neurological diseases—A survey amongst neurologists in the Netherlands. Front Neurol 2019;14:1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chen H, Habermann B. Ready or not: Planning for health declines in couples with advanced multiple sclerosis. J Neurosci Nurs 2013;45:38–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McCurry MK. An exploratory study of decision making by informal caregivers of individuals with multiple sclerosis. J Neurosci Nurs 2013;45:52–60 [DOI] [PubMed] [Google Scholar]
- 43. Berkman CS, Cavallo PF, Chesnut WC, Holland NJ. Attitudes toward physician-assisted suicide among persons with multiple sclerosis. J Palliat Med 1999;2:51–63 [DOI] [PubMed] [Google Scholar]
- 44. Strupp J, Voltz R, Golla H. Opening locked doors: Integrating a palliative care approach into the management of patients with severe multiple sclerosis. Mult Scler 2016;22:13–18 [DOI] [PubMed] [Google Scholar]
- 45. Marrie RA, Salter A, Tyry T, et al. : High hypothetical interest in physician-assisted death in multiple sclerosis. Neurology 2017;88:1528–1534 [DOI] [PubMed] [Google Scholar]
- 46. Hall L. Factors that predict desire for hastened death in individuals with multiple sclerosis dissertation abstracts international: section B. Sci Eng 2005;66(4–B):2307 [Google Scholar]
- 47. Radbruch L, Leget C, Bahr P, et al. : Euthanasia and physician-assisted suicide: A white paper from the European Association for Palliative Care. Palliat Med 2016;30:104–116 [DOI] [PubMed] [Google Scholar]
- 48. Heine M, van de Port I, Rietberg MB, et al. : Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev 2015;CD009956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. NICE. Multiple Sclerosis in Adults: Management (CG186). London: NICE, 2014 [Google Scholar]
- 50. Attal N, Cruccu G, Baron R, et al. : EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol 2010;17:1113–1123 [DOI] [PubMed] [Google Scholar]
- 51. NICE. Neuropathic Pain in Adults: Pharmacological Management in Non-Specialist Settings (CG173). London: NICE, 2013 [PubMed] [Google Scholar]
- 52. Bendtsen L, Zakrzewska JM, Abbott J, et al. . European Academy of Neurology guideline on trigeminal neuralgia. Eur J Neurol 2019;26:831–849 [DOI] [PubMed] [Google Scholar]
- 53. Phé V, Chartier-Kastler E, Panicker JN. Management of neurogenic bladder in patients with multiple sclerosis. Nat Rev Urol 2016;13:276–288 [DOI] [PubMed] [Google Scholar]
- 54. NICE. Urinary Incontinence in Neurological Disease: Management of Lower Urinary Tract Dysfunction in Neurological Disease (CG148). London: NICE, 2012 [PubMed] [Google Scholar]
- 55. Wade DT. Measurement in Neurological Rehabilitation. Oxford: Oxford University Press, 1992 [PubMed] [Google Scholar]
- 56. Khan F, Turner-Stokes L, Ng L, Kilpatrick T. Multidisciplinary rehabilitation for adults with multiple sclerosis. Cochrane Database Syst Rev 2007;2:CD006036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. World Health Organisation (WHO). International Classification of Functioning, Disability and Health (ICF). Geneva: WHO, 2001 [Google Scholar]
- 58. Guagenti-Tax EM, DiLorenzo TA, Tenteromano L, et al. : Impact of a comprehensive long-term care program on caregiver and person with multiple sclerosis. Int J MS Care 2000;2:5–18 [Google Scholar]
- 59. Turner-Stokes L, Sykes N, Silber E, et al. : From diagnosis to death: Exploring the interface between neurology, rehabilitation and palliative care in managing people with long-term neurological conditions. Clin Med 2007;7:129–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Dallara A, Tolchin DW. Emerging subspecialties in neurology: Palliative care. Neurology 2014;82:640–642 [DOI] [PubMed] [Google Scholar]
- 61. Robinson MT, Barrett KM. Emerging subspecialties in neurology: Neuropalliative care. Neurology 2014;82:e180–e182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Boersma I, Miyasaki J, Kutner J, Kluger B. Palliative care and neurology: Time for a paradigm shift. Neurology 2014;83:561–567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Creutzfeldt CJ, Gooley T, Walker M. Are neurology residents prepared to deal with dying patients? Arch Neurol 2009;66:1427–1428 [DOI] [PubMed] [Google Scholar]
- 64. Latorraca CO, Martimbianco ALC, Pachito DV, et al. : Palliative care interventions for people with multiple sclerosis. Cochrane Database Syst Rev 2019;10:CD012936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Freeman J, Hendrie W, Jarrett L, et al. : Assessment of a home-based standing frame programme in people with progressive multiple sclerosis (SUMS): A pragmatic, multi-centre, randomised, controlled trial and cost-effectiveness analysis. Lancet Neurol 2019;18:736–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. van der Steen JT, Radbruch L, Hertogh CMPM, et al. : White paper defining optimal palliative care in older people with dementia: A Delphi study and recommendations from the European Association for Palliative Care. Palliat Med 2014;28:197–209 [DOI] [PubMed] [Google Scholar]
- 67. Curtis JR, Downey L, Back AL, et al. : Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med 2018;178:930–940 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this guideline are available in the Supplementary Material of this article.