Summary
Background
Parents' use of food as reward has been linked to children's dietary intake, but the association with children's eating behaviour and overweight risk is less clear.
Objectives
To examine the temporal association of using food as reward with eating behaviour, body mass index (BMI) and weight status of children.
Methods
Participants were 3642 children of the population‐based Generation R Study in the Netherlands (8.3% overweight/obese). Repeated assessments were collected at child ages 4 and 9 years, including measured anthropometrics and parent reports on feeding practises and eating behaviour.
Results
Linear regressions and cross‐lagged models indicated that parents' use of food as reward at child age 4 years predicted Emotional Overeating and Picky Eating at age 9 years. Reversely, higher Emotional Overeating and Food Responsiveness scores were associated with more use of food as reward over time. Using food as reward was not associated with children's satiety response, BMI or overweight risk.
Conclusions
A vicious cycle may appear in which children who display food approach behaviour are rewarded with food by their parents, which in turn might contribute to the development of unhealthy eating habits (emotional eating, fussiness). These findings warrant further research, to facilitate evidence‐based recommendations for parents.
Keywords: BMI, eating behaviour, emotional eating, fussy, instrumental feeding, using food as reward
1. BACKGROUND
Parents play a key role in the development of their children's dietary patterns and eating habits. These habits are important for immediate health and weight, 1 but evidence also suggests that eating behaviour adopted in early life track into adolescence and adulthood. 2 Parents influence their children's food intake through rule setting, role modelling and organising the family environment. 3 Importantly, feeding strategies may contribute to children's development of both healthy and unhealthy eating behaviour and subsequent risk of underweight or obesity. 4 , 5 , 6
Most research on feeding has focused on controlling feeding practises, which are used to influence the quality and quantity of children's food intake. 4 , 5 , 6 , 7 Despite its frequent occurrence, less attention has been paid to parents' use of food for non‐nutrient purposes, including the use of food as a reward to motivate, promote and reinforce good behaviour and proper performances, 8 , 9 also called “instrumental feeding.” In a qualitative study of low‐income focus groups in the USA, mothers indicated that they commonly used favourite foods and sweets as bribes or rewards when their children cooperated with them in various settings, such as at the physician's office, at mealtimes, or in the car. 8 While this reinforcement may reflect positive parenting and seems harmless in the short term, it may also have undesired effects. As the offered food usually contains high levels of sugar (eg, ice cream and sweets), 10 it has been postulated that the frequent offering of food in return for positive behaviour could be a risk factor for developing adiposity in childhood. Indeed, research has found that the use of food as reward is associated with a higher body mass index (BMI) 11 , 12 and risk of overweight, 13 although other studies did not confirm these findings. 14 , 15 , 16 , 17 Any potential link between using food as reward and children's BMI may also be explained by habitual consumption patterns of children: evidence suggests that children who are frequently being rewarded with food, tend to eat more (energy dense) snacks in general, 11 , 18 , 19 and also to consume more sugar containing beverages and less fruit. 11 , 17 , 20
Besides a direct relation with higher intake of unhealthy foods, frequent use of food as reward may also increase the risk of overweight through long‐term effects on eating behaviour. It is commonly assumed that through instrumental feeding practises, children may learn to associate eating with feelings and behaviour unrelated to hunger and satiety. Indeed, in a lab‐based study, Farrow, Haycraft and Blissett 21 showed that 5 to 7 year old children whose parents used food as a reward when the children were 3 to 5 years old, were more likely to eat in response to negative emotions. Likewise, Puhl and Schwartz reported that adults' recalls about parental rules to use food as reward or as punishment during their childhood, were associated with relatively high levels of restrained eating and binge eating. These studies suggest that parental feeding behaviour may shape children's eating behaviour. However, based on these studies, it cannot be argued that instrumental feeding strategies cause more unhealthy eating behaviour. In fact, reverse causality is possible with certain eating habits of children eliciting parents' use of food as reward, in line with a child‐responsive model that has been implicated for other feeding strategies in recent years. 22 , 23 , 24 , 25 Indeed, both a longitudinal study 26 and a discordant twin analysis 27 showed that parents use more food as reward if they perceive their child as a fussy eater, providing evidence that parents adapt their feeding practises in response to their child's behaviour.
Together these findings suggest that the feeding ‐ eating behaviour association might be bi‐directional, but until now, only three studies provided a more comprehensive overview of mechanisms by examining both directions of the association in the same study. In a study of 222 Australian preschoolers, Rodgers et al 28 found that child food approach behaviour predicted more use of food as reward by the parents 1 year later. No association was found in the other direction, that is, from feeding to eating behaviour, when adjusting for baseline levels of children's eating behaviour. In a Norwegian sample of 797 6 to 8 year old children, Steinsbekk, Belsky and Wichstrom 29 conducted an even more comprehensive analysis by examining the feeding ‐ eating behaviour association using cross‐lagged modelling. In this type of path analysis, the opposing prospective associations (lagged effects) between feeding and eating behaviour are examined in one model, while accounting for cross‐sectional associations and continuity between repeated assessments over time. In contrast with the study of Rodgers et al, 28 Steinsbekk and colleagues found that using food as reward predicted more food responsiveness and emotional eating in children, while no evidence was found for the reverse. Furthermore, despite a cross‐sectional association, they found no longitudinal association between food as reward and satiety responsiveness. In another Australian study amongst 207 2‐year‐olds followed up after 1.5 and 3 years, Mallan et al 30 focused on children's food fussiness and the use of food as reward in return for good behaviour and for eating separately. Also using a cross‐lagged modelling approach, they showed that parents of fussy eaters tended to reward their children with favourite food in return for eating other ‐ probably less liked ‐ foods. Reversely, the use of food as reward for good behaviour, but not for eating, predicted more fussiness in children over time.
In sum, studies confirmed links between parental use of food as reward and child eating behaviour, but firm, consistent evidence as to whether parents should be discouraged to use food as reward is lacking. In this large, population‐based study, we prospectively examine both directions of the association of food as reward with eating behaviour and BMI/overweight across childhood. We hypothesised that the use of food as reward predicts less healthy eating behaviour (more food responsiveness, emotional eating and fussiness, poorer satiety responsiveness and a higher BMI) later in childhood, while reversely, we also expected that parents use food as reward as a response to their child's behaviour, including food approach behaviour and fussiness.
2. METHODS
2.1. Design and study population
This study was embedded in Generation R, a population‐based cohort on health and development from foetal life onwards. 31 All pregnant women living in Rotterdam, the Netherlands, with an expected delivery date between April 2002 and January 2006 were invited to participate (participation rate: 61%). The study was conducted in accordance with the guidelines proposed in the World Medical Association Declaration of Helsinki and has been approved by the Medical Ethical Committee of the Erasmus Medical Centre Rotterdam. Written informed consent was obtained from parents of all children.
Full consent for participation in early (age 0‐5 years) and middle childhood (5‐9 years) in the Generation R Study was obtained from 6036 children and their parents (see also a flow chart in Figure S1). The current study uses data collected at child ages 4 (mean = 4.05 years, SD = 0.09) and 9 years (mean = 9.70 years, SD = 0.28). At age 4 years, data on parents' food as reward and at least one of the children's eating behaviour was available for 4543 children. Because of missing data on food as reward or all eating behaviour and BMI/overweight at age 9 years, 901 children were excluded. This results in a final sample of 3642 families with repeated measures of food as reward and repeated measures of at least one of the eating behaviour or BMI assessments, for the current study. As data on eating behaviour and BMI/overweight was not complete for all children, the study population varies slightly per analysis (n varies between 3486 for BMI and 3624 for Food Responsiveness).
A non‐response analysis (Table S1) indicated that children without data at 9 years (n = 901) were more often of non‐Western origin and had lower educated mothers and fathers than children with available information at both ages 4 and 9 years (n = 3642). In the excluded sample, mothers, fathers and children also had a higher mean BMI.
2.2. Using food as reward
Using food as reward was defined by two items taken from the Child Feeding Questionnaire (CFQ) 7 which was assessed at ages 4 and 9 years. The items are “I offer my child his/her food in exchange for good behaviour,” and “I offer sweets (candy, ice‐cream, cake, pastries) to my child as a reward for good behaviour.” Parents answered the CFQ items on a five‐point Likert scale from 1 = Disagree to 5 = Agree. The questionnaires were mostly filled out by the mothers (86.4% at 4 years; 97.8% at 9 years). At both ages, the two items are summed into a scale score, ranging from 0 to 8. Only for descriptive purposes, the sum score at child age 4 years was categorised as “No use” for sum scores below 1, as “A little” for scores 1 to 4, and as “Yes” for score above 4. The two selected items are part of the larger validated Restriction scale (8 items) 7 and have, to our knowledge, not been previously used as a separate scale. Figure S2 shows the distribution of the food as reward scale score at both ages. The internal consistency of the food as reward scales in our sample was good at 4 years (α = 0.71) and moderate at 9 years (α = 0.63). In general, the CFQ has good concurrent validity with actual observations of maternal feeding behaviour. 32
2.3. Eating behaviour
The child eating behaviour questionnaire (CEBQ) was used to assess Food Responsiveness, Emotional Overeating and Satiety Responsiveness at ages 4 and 9 years. 33 Fussy eating was assessed with the Food Fussiness scale of the CEBQ at 4 years and with the Picky Eating scale of the Stanford Feeding Questionnaire (SFQ) 34 at 9 years ‐ when referring to these specific age assessments, these differential scale names are used. All questionnaires were filled out by parents, mostly the mothers (86.4% at 4 years; 97.8% at 9 years). Examples of items in the CEBQ are “Even if my child is full up, he/she finds room to eat his/her favourite food” (Food Responsiveness, 5 items in total), “My child eats more when upset” (Emotional Overeating, 4 items), “My child is quickly full” (Satiety Responsiveness, 9 items), “My child enjoys tasting new foods” (reverse coded; Food Fussiness, CEBQ, 4 items) and “My child eats a limited number of types of food” (Picky Eating, SFQ, 4 items). All items were answered on a five‐point Likert scale. The CEBQ has a good internal consistency, concurrent validity with actual eating behaviour, test‐retest consistency, and stability over time. 33 , 35 , 36 The SFQ also has a good concurrent validity and stability. 34 , 37 The internal consistency of the scales in our sample were good to high at 4 years (Emotional Overeating, α = 0.85; Food Responsiveness, α = 0.84; Satiety Responsiveness, α = 0.75; Food Fussiness, α = 0.90) and high at 9 years (Emotional Overeating, α = 0.91; Food Responsiveness, α = 0.86; Satiety Responsiveness, α = 0.84; Picky Eating, α = 0.84).
2.4. Child BMI
Children's growth characteristics were measured at the municipal Child Health Centres as part of a routine health care programme at age 4 years. At age 9 years, children's growth characteristics were measured at the Generation R research Centre. At both assessments, trained staff measured children's height and weight using standard procedures. Height was measured in standing position using a Harpenden stadiometer. Weight was measured with light clothing using a mechanical personal scale. BMI was calculated as weight/height2 (kg/m2). Sex‐ and age‐ adjusted BMI z‐scores were calculated according to the Dutch reference growth curves. 38 We used the internationally‐recognised IOTF cut offs to categorise weight status of children, which is based on extrapolation of the cut offs used for adults to age‐ and sex‐specific cut offs for children. 39 Children were categorised as having a normal weight (including underweight) or having overweight/obesity.
Based on international age‐ and sex‐specific cut offs, children were categorised as having a normal weight (including underweight) or having overweight/obesity. 39
2.5. Covariates
Several possible confounding factors were included in the analyses. Information on child sex was obtained from hospital/midwife registries. Child ethnicity was based on (grand)parents' country of birth and categorised as Dutch, other Western and non‐Western. The highest attained educational level of mothers and fathers was assessed by postal questionnaire during pregnancy. Education was categorised as low (3 years of secondary school or less), mid‐low (>3 years of secondary school; intermediate vocational training; first year of higher vocational training), mid‐high (higher vocational training; Bachelor's degree) and high (university level). Mothers' and fathers' height and weight were measured at the Generation R research Centre at enrollment in the first trimester of pregnancy, which was used to calculate BMI (kg/m2).
2.6. Statistical analyses
Descriptive statistics were run to describe the covariates in the complete study population and by the use of food as reward, using ANOVAs for continuous variables and χ2‐tests for categorical variables. Next, linear regression analyses were conducted to examine (a) associations of using food as reward at 4 years with child eating behaviour, BMI and weight status at age 9 years, and (b) associations of eating behaviour, BMI and weight status at 4 years with the use of food as reward at 9 year. For each child outcome/determinant, three models were run: (a) an unadjusted model, (b) a model accounting for potential confounding factors, and (c) a model additionally adjusted for the baseline assessment (at 4 years) of the outcome under study.
Finally, we applied a cross‐lagged modelling approach to better understand the temporal directionality between parental use of food as reward and each child eating behaviour scale or BMI. In this type of path analysis, linear regressions are used to study opposing directions of associations (lagged effects) simultaneously, meaning that each lagged effect is accounted for any potential temporal association in the reverse direction within the same period. The models also account for cross‐sectional associations and continuity within constructs (repeated assessments) over time. Differences between the two opposing lagged coefficients were tested using Wald tests. Covariates were regressed on using food as reward and eating behaviour/BMI at age 4 years. We did not run a cross‐lagged model for overweight/obesity, given that a categorical variable complicates the comparison of the cross‐lagged effects.
Models were estimated using the maximum likelihood estimation with robust standard errors (MLR) to account for non‐normality of the data. Full Information Maximum Likelihood (FIML) was used to account for missing values of the covariates. Given the large number of missings on child BMI at age 4 years (n = 1201), available information on BMI at ages 3 and 5 years was used to inform the FIML procedure. Descriptive analyses were run in SPSS version 24.0 (IBM Corp.). All regression and cross‐lagged analyses were performed with Mplus, version 7.13 (Muthèn & Muthèn).
3. RESULTS
About two third of the parents reported using food as reward at child age 4 years, while one third never used food as reward. At child age 9 years, slightly more than half of the parents did not use food as reward (Figure S2). General characteristics of the families in the current study are shown in Table 1. Of the parents, 20.5% reported to use food as reward, while 33.5% indicated to not use this feeding strategy when children were 4 years old. Parents with a low educational background used food as reward slightly more often than highly educated parents (eg, 23.9% often use by low educated mothers vs 16.9% and 20.9% by mid‐high and high educated mothers, respectively). Boys and children with a non‐Western background (22.3% and 27.9%, respectively) were more often exposed to the use of food as reward than girls and children with a Dutch background (18.8% and 18.3%). Parents' and children's BMI were not associated with the use of food as reward.
TABLE 1.
General characteristics of the total study population and by using food as reward categories
| % or mean (SD) | |||||
|---|---|---|---|---|---|
| Total study | By using food as reward category at 4 years | ||||
| Maternal characteristics | population (n = 3642) | No use (n = 1219) | A little (n = 1675) | Yes (n = 748) | P‐value a |
| Educational level (%) | |||||
| Low | 10.7 | 27.7 | 48.4 | 23.9 | <.001 |
| Mid‐low | 27.3 | 35.2 | 42.5 | 22.4 | |
| Mid‐high | 26.7 | 38.1 | 44.9 | 16.9 | |
| High | 35.3 | 31.0 | 48.1 | 20.9 | |
| BMI (kg/m2) | 24.2 (3.9) | 24.3 (4.0) | 24.2 (3.7) | 24.1 (4.1) | .674 |
| Paternal characteristics | |||||
| Educational level (%) | |||||
| Low | 14.6 | 31.2 | 43.8 | 25.0 | .044 |
| Mid‐low | 26.9 | 33.9 | 45.5 | 20.5 | |
| Mid‐high | 22.3 | 37.1 | 43.7 | 19.2 | |
| High | 36.2 | 32.3 | 47.9 | 19.8 | |
| BMI (kg/m2) | 25.1 (3.2) | 25.0 (3.1) | 25.1 (3.2) | 25.2 (3.2) | .812 |
| Child characteristics | |||||
| Sex (%) | |||||
| Boy | 49.3 | 32.6 | 45.1 | 22.3 | .032 |
| Girl | 50.7 | 34.3 | 46.9 | 18.8 | |
| Ethnicity (%) | |||||
| Dutch | 70.6 | 37.1 | 44.7 | 18.3 | <.001 |
| Other Western | 9.1 | 27.5 | 50.8 | 21.8 | |
| Non‐Western | 20.3 | 23.8 | 48.4 | 27.9 | |
| BMI at 4 years | 15.8 (1.3) | 15.8 (1.3) | 15.7 (1.2) | 15.8 (1.3) | .058 |
| BMI SD score at 4 years | 0.07 (0.92) | 0.11 (0.92) | 0.02 (0.92) | 0.11 (0.92) | .075 |
| Weight status at 4 years (%) | |||||
| Normal weight | 91.7 | 33.1 | 45.7 | 21.2 | .141 |
| Overweight/Obese | 8.3 | 38.6 | 38.6 | 22.8 | |
Note: Some variables had missing values: maternal educational level (n = 126), maternal BMI (n = 396), paternal educational level (n = 96), paternal BMI (n = 870), child ethnicity (n = 9) and child BMI/weight status (n = 1257).
P‐value for heterogeneity: ANOVA for continuous variables, χ 2 for categorical variables.
Table 2 shows that parental use of food as reward at age 4 years was associated with higher levels of Emotional Overeating and Picky Eating when children were 9 years old. These associations remained statistically significant after adjusting for covariates and baseline assessments of the outcomes (eg, β for Emotional Overeating at 9 years = 0.07, 95% CI: 0.04, 0.11). Using food as reward was also associated with more Satiety Responsiveness at 9 years, but this association attenuated to non‐significance after accounting for baseline Satiety Responsiveness. No significant relations were found for instrumental feeding with Food Responsiveness, BMI z‐score or weight status.
TABLE 2.
Associations of using food as reward with child eating behaviour a and BMI/overweight at 9 years
| β (95%CI) for child outcome at age 9y | Odds ratio (95%) for overweight/obese at age 9y | |||||
|---|---|---|---|---|---|---|
| Using food as reward at age 4y | Emotional overeating | Food responsiveness | Satiety responsiveness | Picky eating | BMIz | |
| Unadjusted | 0.10 (0.07, 0.13) | 0.02 (−0.02, 0.05) | 0.08 (0.04, 0.11) | 0.11 (0.08, 0.15) | −0.00 (−0.04, 0.04) | 1.02 (0.98, 1.07) |
| Adjusted for covariates b | 0.10 (0.06, 0.13) | 0.02 (−0.01, 0.05) | 0.08 (0.04, 0.11) | 0.11 (0.07, 0.14) | −0.03 (−0.06, 0.00) | 0.99 (0.94, 1.04) |
| Additionally adjusted for eating behaviour (or BMI) at baseline c | 0.07 (0.04, 0.11) | −0.01 (−0.04, 0.02) | 0.02 (−0.01, 0.05) | 0.05 (0.02, 0.08) | −0.02 (−0.05, 0.01) | 0.99 (0.95, 1.05) |
Note: Effect estimates are standardised linear regression coefficients and 95% confidence intervals.
All eating behaviour scales assessed with the Child Eating behaviour Questionnaire, except for Picky Eating which was assessed with the Stanford Feeding Questionnaire.
Adjusted for maternal and paternal educational level, maternal and paternal BMI, and child sex and ethnicity.
Additionally adjusted for baseline assessment of outcome (ie, eating behaviour or BMI assessed at age 4 years).
Table 3 shows the results of the regression analyses of eating behaviour and BMI in early childhood with parental use of food as reward at 9 years as outcome. Children with higher scores on Emotional Overeating, Food Responsiveness, Satiety Responsiveness and Food Fussiness at age 4 years were relatively often given food as reward by their parents when they were 9 years old, after accounting for covariates. However, for Satiety Responsiveness and Food Fussiness, the association attenuated to non‐significance when accounting for baseline levels of parental feeding. Child BMI and weight status were not associated with later use of food as reward.
TABLE 3.
Association of child eating behaviour a and BMI/overweight with using food as reward at 9 years
| β (95%CI) for using food as reward at age 9y | |||
|---|---|---|---|
| Child eating behaviour / BMI at age 4 year | Unadjusted | Adjusted for covariates b | Additionally adjusted for food as reward at baseline c |
| Emotional Overeating | 0.12 (0.09, 0.16) | 0.11 (0.07, 0.14) | 0.05 (0.02, 0.09) |
| Food Responsiveness | 0.08 (0.04, 0.11) | 0.07 (0.04, 0.10) | 0.04 (0.01, 0.07) |
| Satiety Responsiveness | 0.04 (0.00, 0.07) | 0.04 (0.01, 0.07) | −0.01 (−0.04, 0.03) |
| Food Fussiness | 0.07 (0.04, 0.10) | 0.07 (0.04, 0.10) | 0.03 (−0.00, 0.06) |
| BMIz | 0.00 (−0.04, 0.05) | −0.01 (−0.05, 0.03) | −0.00 (−0.04, 0.04) |
| Overweight/obese | −0.01 (−0.05, 0.03) | −0.02 (−0.06, 0.02) | −0.01 (−0.05, 0.03) |
Note: Effect estimates are standardised linear regression coefficients and 95% confidence intervals.
All eating behaviour scales assessed with the Child Eating behaviour Questionnaire.
Adjusted for maternal and paternal educational level, maternal and paternal BMI, and child sex and ethnicity.
Additionally adjusted for use of food as reward assessed at age 4 years.
In Figures 1, 2, 3, 4 (eating behaviour) and Figure 5 (BMI), the results of the cross‐lagged models are presented. For all eating behaviour, BMI and use of food as reward, stability paths showed moderate stability over time (eg, Satiety Responsiveness β = 0.49, 95% CI: 0.46, 0.51; for using food as reward β = 0.37, 95% CI: 0.34, 0.40), except for Emotional Overeating which was less stable over time (β = 0.17, 95% CI: 0.13, 0.21). The results of the lagged effects were very comparable with the reported unidirectional associations (Tables 2 and 3). For Emotional Overeating, both lagged effects were significant, with the path from using food as reward to Emotional Overeating being slightly stronger than the reversed path (Wald test for comparing lagged effects: P‐value = .016). Food Responsiveness at 4 years was associated with more use of food as reward at age 9 years (β = 0.04, 95% CI: 0.01, 0.08), while no association was observed in the reverse direction. For Fussy/Picky Eating, we also found a unidirectional path: using food as reward preceded more Picky Eating (β = 0.06, 95% CI: 0.03, 0.09), rather than reverse. For both Satiety Responsiveness and child BMI, no significant lagged effects with the use of food as reward were found.
FIGURE 1.
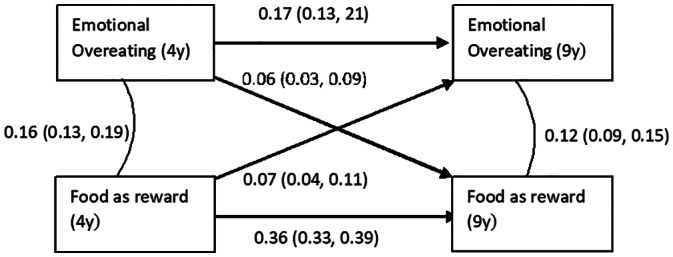
Cross‐lagged model of association between the use of food as reward with child Emotional Overeating. Values represent standardized linear regression coefficients (95% confidence intervals) and are adjusted for covariates. N = 3511, model fit: RMSEA = 0.022, CFI = 0.959 and TLI = 0.907. Wald test comparing lagged pathways: P = .016
FIGURE 2.
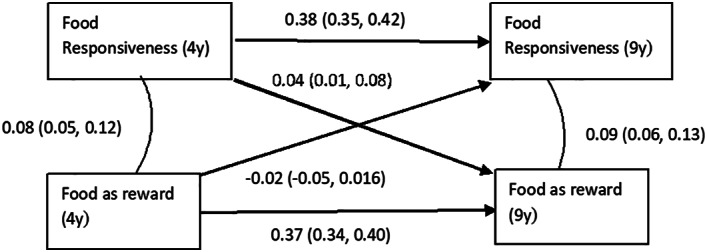
Cross‐lagged model of association between the use of food as reward with child Food Responsiveness. Values represent standardized linear regression coefficients (95% confidence intervals) and are adjusted for covariates. N = 3624, model fit: RMSEA = 0.035, CFI = 0.923 and TLI = 0.826. Wald test comparing lagged pathways: P = .004
FIGURE 3.
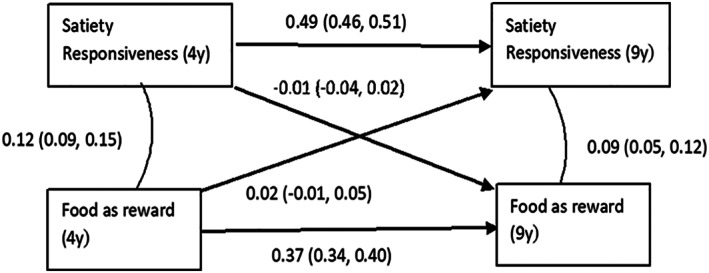
Cross‐lagged model of association between the use of food as reward with child Satiety Responsiveness. Values represent standardized linear regression coefficients (95% confidence intervals) and are adjusted for covariates. N = 3616, model fit: RMSEA = 0.027, CFI = 0.966 and TLI = 0.923. Wald test comparing lagged pathways: P = .43
FIGURE 4.
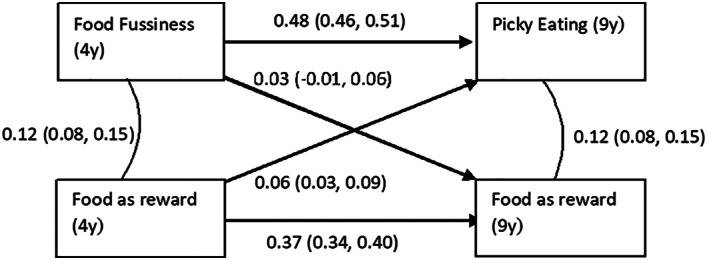
Cross‐lagged model of association between the use of food as reward with child Food Fussiness/Picky Eating. Values represent standardized linear regression coefficients (95% confidence intervals) and are adjusted for covariates. N = 3620, model fit: RMSEA = 0.026, CFI = 0.970 and TLI = 0.932. Wald test comparing lagged pathways: P = .501
FIGURE 5.
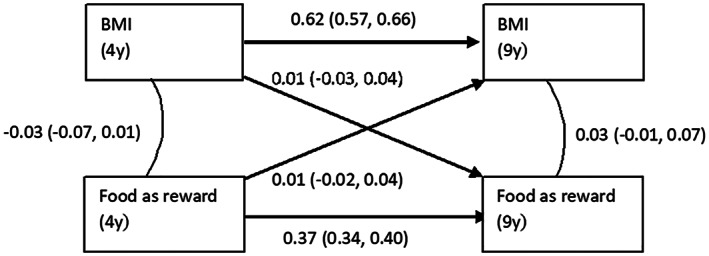
Cross‐lagged model of association between the use of food as reward with child BMI. Values represent standardized linear regression coefficients (95% confidence intervals) and are adjusted for covariates. N = 3486, model fit: RMSEA = 0.144, CFI = 0.300 and TLI = 0.000. Wald test comparing lagged pathways: P = .771
4. DISCUSSION
Findings from this large, longitudinal study across childhood suggest that parental use of food as reward is differentially related to various eating behaviour of children. Results aligned well across diverse modelling strategies and indicated that parents' use of food as reward predicted more emotional eating and more picky eating amongst children over a five‐year time period. However, in line with the child‐responsive model, parents also tended to adapt their strategies of using food as reward in response to child eating behaviour. In particular, parents more often reported to use food as reward when their children exhibit food approach behaviour, that is, higher Food Responsiveness and Emotional Overeating scores. In our sample with a relatively low percentage of children with overweight or obesity as compared to other Western countries, 40 no associations were found for using food as reward with child satiety response and BMI or weight status.
4.1. Comparison of findings with previous studies
Our results support common thinking that feeding partly shapes child eating behaviour, although we only found such evidence for selected eating habits, namely emotional eating and fussy eating, and not for food and satiety responsiveness. Our results for emotional eating are in line with two longitudinal studies in the UK (n = 41, 3‐5 years at baseline) 21 and Norway (n = 797, 6‐8 years at baseline), 29 which also reported that the use of food as reward was associated with more emotional eating in children at follow up. Potentially, because of being rewarded with food, children may learn to associate the used food ‐ most likely unhealthy food high in fat and sugar 10 ‐ with emotions. However, the CEBQ scale Emotional Overeating measures only the tendency to eat in response to negative emotions (anxious, annoyed, worried and being bored), while food as reward is mostly used in case of good behaviour or high achievements, which implicates positive emotions. Yet, the link between positive emotions and eating may spill over to negative emotions as well. Alternatively, parents may also give sweets or other favourite foods as a bribe to prevent negative behaviour. Indeed, in a focus study in the USA, mothers explained to give food in return for good behaviour, mostly meant as “sops” to avoid negative behaviour in situations that may trigger irritations and tantrums. 8 For instance, lollipops may help avoid that children become bored or annoyed when travelling in the car for a long time. As such, children may also learn that eating could be a way to cope with stressors and looming negative emotions.
Next to emotional eating, we also found that the use of food as reward was associated with more fussiness in children 5 years later. To our knowledge, only one study explored both directions of this association 30 and reported the same temporal relationship as we did. A potential explanation for this finding relates to the observation that children mostly receive sweets and snacks as a reward, rather than healthy foods. 10 While most children already favour candies, cookies and chips over vegetables, fruit and other healthy products, this reward strategy may further increase the likability of rewarded food and simultaneously decrease the attractiveness of healthy food. Although we did not specifically study reward for eating, this divergence in food preferences may even worsen in case children are being rewarded with food (eg, having a dessert) for eating or finishing other, disliked foods (eg, vegetables). Such counterproductive effect has been described for other feeding strategies, like pressure to eat, in previous experimental 41 and cohort studies. 23 The association from food as reward to fussiness might also partly be explained by the dynamics in the parent‐child relationship. From a dialectical perspective, feeding not only concerns food intake, but also regards the relationship between parent and child. 22 When using food as reward (or controlling feeding strategies), a parent may compromise a child's independence as to when and what to eat. 42 As a counteract to parents' power and in an attempt to gain autonomy over eating again, children may show food fussiness. 42 Besides the parent‐to‐child association, we found no indication for a reverse direction of effect, which contrasts with previous evidence that parents use more food as reward in response to children's fussiness. 26 , 27 , 30 While two of these studies 26 , 27 did not examine the reverse direction, it does not seem plausible that the focus on a unidirectional analysis explains the difference in findings. In our unidirectional analysis ‐ which closely matches the analyses of Byrne et al 26 ‐ we found that child fussiness predicted later use of food as reward, but that association disappeared when we adjusted for baseline use of food as reward. This suggests there was already an association at baseline (age 4 years), which may have arisen in earlier childhood. Indeed, these three previous study samples included younger children who were 1 to 2 years old. In these years, fussy eating also peaks, 43 , 44 which may drive parents to use strategies ‐ including using food as reward ‐ to get their children to eat.
For the two food approach scales of the CEBQ that we studied, we found indications that parents adapt their feeding strategies in response to children's behaviour: children of mothers who used food as reward displayed more emotional eating and food responsiveness. This finding is in line with a longitudinal Australian study amongst 222 2 to 3 year‐olds, 28 but contrasts with the abovementioned Norwegian study. 29 This contrast in findings might be explained by several factors, including the differences in statistical modelling and covariates. For instance, the Norwegian study included all feeding strategies and eating behaviour in one model and included child BMI as a covariate, 29 while in this study, we examined separate models and did not adjust for child BMI, but rather investigated BMI separately. The intuitive explanation for our finding is that, if a child likes to eat, food is a logical and easy reward for parents to give. In these families, food may also be more commonly used for non‐nutritional purposes, perhaps including the use of food to comfort and soothe (another instrumental feeding strategy). In previous work of our group, findings suggested that the use of food as a way to soothe infants was associated with more emotional eating up to 9 years later (food responsiveness was not studied). 45
The current study found no evidence for a longitudinal association between feeding and children's satiety responsiveness, while we hypothesised that a feeding practise such as the use of food as reward may override children's natural feelings of satiety and hunger and their responsiveness to these feelings. The absence of an association between instrumental feeding and satiety responsiveness was also observed in the study amongst 6 to 8 year old Norwegian children. 29 However, in our sample, a cross‐sectional association and a longitudinal association in both directions were found, but the longitudinal associations attenuated to non‐significance once adjusted for baseline levels of the outcome under study. This suggests that a link between parents' feeding practises and children's responses to satiety and hunger may have been formed in earlier childhood. Unfortunately, as the Generation R sample has not collected data on these specific feeding strategies and eating behaviour prior to age 4 years, these associations in younger children warrant further attention.
Considering the different findings regarding children's eating behaviour, the lack of an association between food as reward and child BMI is perhaps not surprising. For instance, more use of food as reward was associated with higher levels of picky eating and emotional overeating. If anything, picky eaters tend to have a lower weight, 46 while emotional overeaters are more likely to have a higher weight status. 47 However, with such potential masking effect of different eating behaviour, one would expect much variation in BMI in the group of children who are exposed to food as reward, but this was not the case (SD for BMI is similar for those exposed and not exposed to food as reward, both SD = 1.3). Another reason for the lack of an association with adiposity may be that the quantity and quality of sweets and other favourite foods offered in return for good behaviour might have such a subtle effect on weight development that it only becomes visible at the longer term, after years of cumulative exposure. Indeed, while several studies amongst preschool aged children found no association, a retrospective study amongst adults 12 as well as a prospective study amongst 11 to 12 year old children 11 , 48 reported that parents' use of food as reward was associated with a higher BMI. Reversely, while an increasing number of studies indicated that parents might adjust their feeding strategies to children's weight status, 23 , 25 , 49 our findings with the use of food as reward do not reflect this, that is, we found no association from children's BMI nor overweight status to subsequent instrumental feeding. However, in these previous studies, parents' controlling feeding strategies were examined and were seemingly aimed at improving children's unhealthy weight development while the use of food as reward is likely to have a different, non‐nutritional purpose.
4.2. Methodological considerations
Strengths of the current study are the large, population‐based sample and the repeated assessments of both the use of food as reward and eating behaviour. However, some limitations should be considered as well. First, we constructed a scale that measured the use of food as reward based on two items of the CFQ. The external validity of this self‐constructed scale is unknown, although the moderate to good internal reliability suggests the two items measure a similar underlying concept. Second, feeding and eating behaviour were both assessed using mother reports which may induce reporter bias and socially desirable answers. Although results were corrected for various maternal characteristics, reporter bias cannot be ruled out completely. Therefore, we recommend future studies to incorporate multiple informants. Third, our study was limited by the use of two different scales to assess fussiness in children, namely the CEBQ Food Fussiness scale at 4 years and the SFQ Picky Eating subscale at 9 years. Not using the same instrument at repeated assessments is suboptimal for longitudinal and cross‐lagged analyses. However, the autoregressive coefficient between the two time points showed adequate stability and the model fit was good. Fourth, although cross‐lagged models with two time‐points are useful to study reciprocal effects, these cannot differentiate within‐person effects from between‐person effects. 48 Future studies with at least three time points are needed to examine intra‐individual changes over time. Finally, while BMI is the most common measure to indicate adiposity in population‐based studies, the use of measurements that can distinguish fat mass from fat free mass are preferential because these better reflect the level of adiposity, especially amongst paediatric populations. Measurements of body composition are available in the Generation R Study, but unfortunately not at the age of 4 years.
4.3. Implications
This longitudinal study in a rather healthy population shows a complex relationship between parents' use of food as reward and children's eating habits: our findings suggest a vicious cycle may appear in which children who like to eat are more likely to be rewarded with food by their parents, which in turn seems to contribute to the development of unhealthy eating habits ‐ emotional eating and fussiness. We acknowledge that the reported associations reflect small effect sizes, potentially due to the relatively low number of children with adiposity. These small effect sizes may, however, represent larger individual differences. Therefore, it is probably best to limit the use of food as reward and to encourage parents to reward children with other means than with food. Health care professionals involved in the care of young children and families may encourage parents to adopt strategies to encourage and praise children in a non‐nutrient way. Such rewards could include compliments, earning a sticker or quality time to do something fun with a parent like singing a song, telling jokes or playing a game. Although we examined the use of food within a family context, it is known that within schools, sweets and cookies are also often given to children in return for good behaviour and achievements. 50 , 51 As it seems likely that this reward system is related to children's eating behaviour in a similar way as parental feeding strategies, teachers should also be aware of the link of food as reward with unhealthy eating behaviour in children. Nevertheless, given our assessment of using food as reward with a non‐validated scale, and considering the large gap between the two repeated time points, we emphasise the need for replication of our findings in future longitudinal studies, preferably in samples including more children at the high end of the BMI spectrum, and using precise, repeated assessments of feeding practises from birth onwards. Particularly studies in the first 4 years of life are needed, when eating and feeding habits are being shaped. Also, picky eating peaks in this period, 43 , 44 which may provoke parents to use food as reward. Together such studies can provide an evidence base regarding the origin and temporal direction of the association and any causal effects.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
AUTHOR CONTRIBUTIONS
Pauline W. Jansen designed and conducted the study, supervised the statistical analyses and wrote the manuscript. Ivonne P. M. Derks and Yuchan Mou conducted the analyses and wrote parts of the manuscript. Elisabeth H. M. van Rijen contributed interpreting the results and wrote parts of the manuscript. Romy Gaillard, Trudy Voortman and Manon H. J. Hillegers contributed to the conceptualization and design of the Generation R Study, and helped interpreting the results. Nadia Micali critically reviewed the statistical analyses and contributed interpreting the results. All authors critically reviewed the manuscript, approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Supporting information
Table S1. Comparison of the included sample with children with baseline data but without follow up data at 9 years.
Figure S1. Flow chart of the study population.
Figure S2. Distribution of using food as reward at child ages 4 and 9 years.
ACKNOWLEDGEMENTS
The general design of Generation R Study is made possible by financial support from the Erasmus Medical Centre and the Erasmus University Rotterdam, the Netherlands Organisation for Health Research and Development (ZonMW), the Netherlands Organisation for Scientific Research (NWO), the Ministry of Health, Welfare and Sport and the Ministry of Youth and Families. The current study was made possible by grants from the Netherlands Organisation for Health Research and Development (Mental Health Care Research Program ‐ Fellowship 636320005 to PWJ; NWO, ZonMW, grant number 543003109 to RG), from the China Scholarship Council (PhD Fellowship 201806240125 for YM, CSC URL: http://www.csc.edu.cn/), from the Dutch Heart Foundation (grant number 2017 T013 to RG), and from the Dutch Diabetes Foundation (grant number 2017.81.002 to RG). The funders had no role in the design and conduct of the study or the writing of the report.
Jansen PW, Derks IPM, Mou Y, et al. Associations of parents' use of food as reward with children's eating behaviour and BMI in a population‐based cohort. Pediatric Obesity. 2020;15:e12661 10.1111/ijpo.12662
Funding information China Scholarship Council, Grant/Award Number: 201806240125; Dutch Diabetes Foundation, Grant/Award Number: 2017.81.002; Dutch Heart Foundation, Grant/Award Number: 2017T013; Netherlands Organization for Health Research and Development, Grant/Award Numbers: 543003109, 636320005
REFERENCES
- 1. Nguyen AN, Jen V, Jaddoe VWV, et al. Diet quality in early and mid‐childhood in relation to trajectories of growth and body composition. Clin Nutr. 2019;39(3):845‐852. [DOI] [PubMed] [Google Scholar]
- 2. Schwartz C, Scholtens PA, Lalanne A, Weenen H, Nicklaus S. Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite. 2011;57(3):796‐807. [DOI] [PubMed] [Google Scholar]
- 3. Bandura A. Social Foundation of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 4. Patrick H, Hennessy E, McSpadden K, Oh A. Parenting styles and practises in children's obesogenic behaviour: scientific gaps and future research directions. Child Obes. 2013;9:S73‐S86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vaughn AE, Tabak RG, Bryant MJ, Ward DS. Measuring parent food practises: a systematic review of existing measures and examination of instruments. Int J Behav Nutr Phys Act. 2013;10:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Loth K. Associations between food restriction and pressure‐to‐eat parenting practises and dietary intake in children: a selective review of recent literature. Curr Nutr Rep. 2016;5:61‐67. [Google Scholar]
- 7. Birch LL, Fisher JO, Grimm‐Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the child feeding questionnaire: a measure of parental attitudes, beliefs and practises about child feeding and obesity proneness. Appetite. 2001;36(3):201‐210. [DOI] [PubMed] [Google Scholar]
- 8. Baughcum AE, Burklow KA, Deeks CM, Powers SW, Whitaker RC. Maternal feeding practises and childhood obesity: a focus group study of low‐income mothers. Arch Pediatr Adolesc Med. 1998;152(10):1010‐1014. [DOI] [PubMed] [Google Scholar]
- 9. Spence A, Campbell K, Hesketh K. Parental correlates of young children's deitary intakes: a review. Aust Epidemiologist. 2010;17(1):17‐20. [Google Scholar]
- 10. Raaijmakers LG, Gevers DW, Teuscher D, Kremers SP, van Assema P. Emotional and instrumental feeding practises of Dutch mothers regarding foods eaten between main meals. BMC Public Health. 2014;14:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodenburg G, Kremers SP, Oenema A, van de Mheen D. Associations of parental feeding styles with child snacking behaviour and weight in the context of general parenting. Public Health Nutr. 2014;17(5):960‐969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Puhl RM, Schwartz MB. If you are good you can have a cookie: how memories of childhood food rules link to adult eating behaviour. Eat Behav. 2003;4(3):283‐293. [DOI] [PubMed] [Google Scholar]
- 13. Hardy LL, King L, Hector D, Lloyd B. Weight status and weight‐related behaviour of children commencing school. Prev Med. 2012;55(5):433‐437. [DOI] [PubMed] [Google Scholar]
- 14. Blissett J, Haycraft E, Farrow C. Inducing preschool children's emotional eating: relations with parental feeding practises. Am J Clin Nutr. 2010;92(2):359‐365. [DOI] [PubMed] [Google Scholar]
- 15. Carnell S, Wardle J. Associations between multiple measures of parental feeding and children's adiposity in United Kingdom preschoolers. Obesity. 2007;15(1):137‐144. [DOI] [PubMed] [Google Scholar]
- 16. Haszard JJ, Russell CG, Byrne RA, Taylor RW, Campbell KJ. Early maternal feeding practises: associations with overweight later in childhood. Appetite. 2019;132:91‐96. [DOI] [PubMed] [Google Scholar]
- 17. Kroller K, Warschburger P. Associations between maternal feeding style and food intake of children with a higher risk for overweight. Appetite. 2008;51(1):166‐172. [DOI] [PubMed] [Google Scholar]
- 18. Vereecken CA, Keukelier E, Maes L. Influence of mother's educational level on food parenting practises and food habits of young children. Appetite. 2004;43(1):93‐103. [DOI] [PubMed] [Google Scholar]
- 19. Sleddens EF, Kremers SP, De Vries NK, Thijs C. Relationship between parental feeding styles and eating behaviour of Dutch children aged 6‐7. Appetite. 2010;54(1):30‐36. [DOI] [PubMed] [Google Scholar]
- 20. Inhulsen MM, Merelle SY, Renders CM. Parental feeding styles, young children's fruit, vegetable, water and sugar‐sweetened beverage consumption, and the moderating role of maternal education and ethnic background. Public Health Nutr. 2017;20(12):2124‐2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Farrow CV, Haycraft E, Blissett JM. Teaching our children when to eat: how parental feeding practises inform the development of emotional eating–a longitudinal experimental design. Am J Clin Nutr. 2015;101(5):908‐913. [DOI] [PubMed] [Google Scholar]
- 22. Walton K, Kuczynski L, Haycraft E, Breen A, Haines J. Time to re‐think picky eating?: a relational approach to understanding picky eating. Int J Behav Nutr Phys Act. 2017;14(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jansen PW, de Barse LM, Jaddoe VWV, Verhulst FC, Franco OH, Tiemeier H. Bi‐directional associations between child fussy eating and parents' pressure to eat: who influences whom? Physiol Behav. 2017;176:101‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jansen PW, Tharner A, van der Ende J, et al. Feeding practises and child weight: is the association bidirectional in preschool children? Am J Clin Nutr. 2014;100(5):1329‐1336. [DOI] [PubMed] [Google Scholar]
- 25. Derks IP, Tiemeier H, Sijbrands EJ, et al. Testing the direction of effects between child body composition and restrictive feeding practises: results from a population‐based cohort. Am J Clin Nutr. 2017;106(3):783‐790. [DOI] [PubMed] [Google Scholar]
- 26. Byrne R, Jansen E, Daniels L. Perceived fussy eating in Australian children at 14 months of age and subsequent use of maternal feeding practises at 2 years. Int J Behav Nutr Phys Act. 2017;14(1):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harris HA, Fildes A, Mallan KM, Llewellyn CH. Maternal feeding practises and fussy eating in toddlerhood: a discordant twin analysis. Int J Behav Nutr Phys Act. 2016;13:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rodgers RF, Paxton SJ, Massey R, et al. Maternal feeding practises predict weight gain and obesogenic eating behaviour in young children: a prospective study. Int J Behav Nutr Phys Act. 2013;10(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Steinsbekk S, Belsky J, Wichstrom L. Parental feeding and child eating: an investigation of reciprocal effects. Child Dev. 2016;87(5):1538‐1549. [DOI] [PubMed] [Google Scholar]
- 30. Mallan KM, Jansen E, Harris H, Llewellyn C, Fildes A, Daniels LA. Feeding a fussy eater: examining longitudinal bidirectional relationships between child fussy eating and maternal feeding practises. J Pediatr Psychol. 2018;43(10):1138‐1146. [DOI] [PubMed] [Google Scholar]
- 31. Kooijman MN, Kruithof CJ, van Duijn CM, et al. The generation R study: design and cohort update 2017. Eur J Epidemiol. 2016;31(12):1243‐1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Farrow CV, Blissett JM. Is maternal psychopathology related to obesigenic feeding practises at 1 year? Obes Res. 2005;13(11):1999‐2005. [DOI] [PubMed] [Google Scholar]
- 33. Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children's eating behaviour questionnaire. J Child Psychol Psychiatry. 2001;42(7):963‐970. [DOI] [PubMed] [Google Scholar]
- 34. Jacobi C, Agras WS, Bryson S, Hammer LD. behavioural validation, precursors, and concomitants of picky eating in childhood. J Am Acad Child Adolesc Psychiatry. 2003;42(1):76‐84. [DOI] [PubMed] [Google Scholar]
- 35. Sleddens EF, Kremers SP, Thijs C. The Children's eating behaviour questionnaire: factorial validity and association with body mass index in Dutch children aged 6‐7. Int J Behav Nutr Phys Act. 2008;5:49‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Viana V, Sinde S, Saxton JC. Children's eating behaviour questionnaire: associations with BMI in Portuguese children. Br J Nutr. 2008;100(2):445‐450. [DOI] [PubMed] [Google Scholar]
- 37. Micali N, Simonoff E, Elberling H, Rask CU, Olsen EM, Skovgaard AM. Eating patterns in a population‐based sample of children aged 5 to 7 years: association with psychopathology and parentally perceived impairment. J Dev Behav Pediatr. 2011;32(8):572‐580. [DOI] [PubMed] [Google Scholar]
- 38. Fredriks AM, van Buuren S, Burgmeijer RJ, et al. Continuing positive secular growth change in The Netherlands 1955‐1997. Pediatr Res. 2000;47(3):316‐323. [DOI] [PubMed] [Google Scholar]
- 39. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240‐1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Collaboration NRF . Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population‐based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627‐2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Galloway AT, Fiorito LM, Francis LA, Birch LL. ‘Finish your soup’: counterproductive effects of pressuring children to eat on intake and affect. Appetite. 2006;46(3):318‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bell R, Harper L. Child Effects on Adults. Hillside, NJ: Earlbaum; 1977. [Google Scholar]
- 43. Taylor CM, Wernimont SM, Northstone K, Emmett PM. Picky/fussy eating in children: review of definitions, assessment, prevalence and dietary intakes. Appetite. 2015;95:349‐359. [DOI] [PubMed] [Google Scholar]
- 44. Cardona Cano S, Tiemeier H, Van Hoeken D, et al. Trajectories of picky eating during childhood: a general population study. Int J Eat Disord. 2015;48(6):570‐579. [DOI] [PubMed] [Google Scholar]
- 45. Jansen PW, Derks IPM, Batenburg A, et al. Using food to soothe in infancy is prospectively associated with childhood BMI in a population‐based cohort. J Nutr. 2019;149(5):788‐794. [DOI] [PubMed] [Google Scholar]
- 46. de Barse LM, Tiemeier H, Leermakers ET, et al. Longitudinal association between preschool fussy eating and body composition at 6 years of age: the generation R study. Int J Behav Nutr Phys Act. 2015;12:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Derks IPM, Bolhuis K, Sijbrands EJG, Gaillard R, Hillegers MHJ, Jansen PW. Predictors and patterns of eating behaviour across childhood: results from the generation R study. Appetite. 2019;141:104295. [DOI] [PubMed] [Google Scholar]
- 48. Hamaker EL, Kuiper RM, Grasman RP. A critique of the cross‐lagged panel model. Psychol Methods. 2015;20(1):102‐116. [DOI] [PubMed] [Google Scholar]
- 49. Webber L, Cooke L, Hill C, Wardle J. Child adiposity and maternal feeding practises: a longitudinal analysis. Am J Clin Nutr. 2010;92(6):1423‐1428. [DOI] [PubMed] [Google Scholar]
- 50. Fedewa AL, Davis MC. How food as a reward is detrimental to Children's health, learning, and behaviour. J Sch Health. 2015;85(9):648‐658. [DOI] [PubMed] [Google Scholar]
- 51. Turner L, Chriqui JF, Chaloupka FJ. Food as a reward in the classroom: school district policies are associated with practises in US public elementary schools. J Acad Nutr Diet. 2012;112(9):1436‐1442. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Comparison of the included sample with children with baseline data but without follow up data at 9 years.
Figure S1. Flow chart of the study population.
Figure S2. Distribution of using food as reward at child ages 4 and 9 years.


