Abstract
Background
Technology has changed the way that men who have sex with men (MSM) seek sex. More than 60% of MSM in the United States use the internet and/or smartphone-based geospatial networking apps to find sex partners. We correlated use of the most popular app (Grindr) with sexual risk and prevention behavior among MSM.
Methods
A nested cohort study was conducted between September 2018 and June 2019 among MSM receiving community-based human immunodeficiency virus (HIV) and sexually transmitted infection (STI) screening in central San Diego. During the testing encounter, participants were surveyed for demographics, substance use, risk behavior (previous 3 months), HIV pre-exposure prophylaxis (PrEP) use, and Grindr usage. Participants who tested negative for HIV and who were not on PrEP were offered immediate PrEP.
Results
The study included 1256 MSM, 1090 of whom (86.8%) were not taking PrEP. Overall, 580 of 1256 (46%) participants indicated that they used Grindr in the previous 7 days. Grindr users reported significantly higher risk behavior (greater number of male partners and condomless sex) and were more likely to test positive for chlamydia or gonorrhea (8.6% vs 4.7% of nonusers; P = .005). Grindr users were also more likely to be on PrEP (18.7% vs 8.7% of nonusers; P < .001) and had fewer newly diagnosed HIV infections (9 vs 26 among nonusers; P = .014). Grindr users were also nearly twice as likely as nonusers to initiate PrEP (24.6% vs 14%; P < .001).
Conclusions
Given the higher risk behavior and greater acceptance of PrEP among MSM who used Grindr, Grindr may provide a useful platform to promote HIV and STI testing and increase PrEP uptake.
Keywords: HIV risk, dating app, pre-exposure prophylaxis, substance use, risk behavior
Grindr users took more sexual risks than those who did not use the app. However, Grindr users were also more likely to use, or be open to using, HIV pre-exposure prophylaxis, suggesting the app could be a platform to encourage HIV prevention.
Men who have sex with men (MSM) represent the predominant risk group for human immunodeficiency virus (HIV) infection in the United States, and technology has changed the way MSM socialize and seek sex [1]. While social media networks mostly reflect real-world offline relationships, dating apps focus on meeting new sexual partners. More than 60% of MSM in the United States have used a dating app to meet a sexual partner in the past year [2–5]. Grindr, a sophisticated geosocial networking app, is the most frequently used dating app in the United States [6].
The risk of HIV infection within MSM is not uniform [7]. Although there are conflicting data regarding whether this translates into increased HIV acquisition, studies have indicated that MSM who use Grindr have a greater frequency of condomless anal intercourse, a higher incidence of sexually transmitted infections (STIs), and more sexual partners [3, 8–11]. Meeting partners over Grindr or other geosocial networking apps may also facilitate serostatus disclosure, serosorting, negotiation regarding condom usage, discussion of sexual practices, and user risk assessment, therefore lowering overall risk [6, 12, 13]. Although Grindr may also serve as a forum to discuss HIV, the use of pre-exposure prophylaxis (PrEP) [14, 15] among Grindr users remains a underexplored topic [16].
We aimed to assess Grindr activity among MSM undergoing HIV and STI screening in San Diego, California. We then examined how Grindr use correlated with risk and prevention behavior, particularly focusing on PrEP use. We believe that this information can be used both to characterize HIV risk in this population and advance strategies to use geosocial networking apps as platforms to promote HIV prevention.
MATERIALS AND METHODS
Setting and Participants
The study was conducted between September 2018 and June 2019 and leveraged our “Good to Go” HIV and STI screening study for participant recruitment. Formerly named the Early Test, this community-based HIV and STI screening program provides free testing to adult MSM and transgender women participants who are willing to enroll and answer risk-related questions [17, 18]. The program utilizes a point-of-care rapid HIV test followed by routine reflex to individual donation HIV nucleic acid amplification testing in persons with negative rapid test results. STI screening assessments include syphilis (using the reverse screening algorithm [19]), Chlamydia species, and gonorrhea by nucleic acid amplification test of urine, pharyngeal, and rectal swab specimens (Cepheid Xpert CT/NG, Sunnydale, California). Data are collected by bilingual (Spanish and English) testing staff before each testing encounter including demographics, sexual risk, number of sex partners, substance use (all in the previous 3 months), and PrEP use [18]. Participants who test positive for HIV or STIs are offered immediate treatment at no cost. Those at substantial risk for HIV acquisition [20] who test negative for HIV and are not currently prescribed emtricitabine/tenofovir disoproxil fumarate (FTC/TDF) for PrEP are offered immediate PrEP.
Measures
Assessment of Grindr Activity, HIV Risk, and PrEP Use
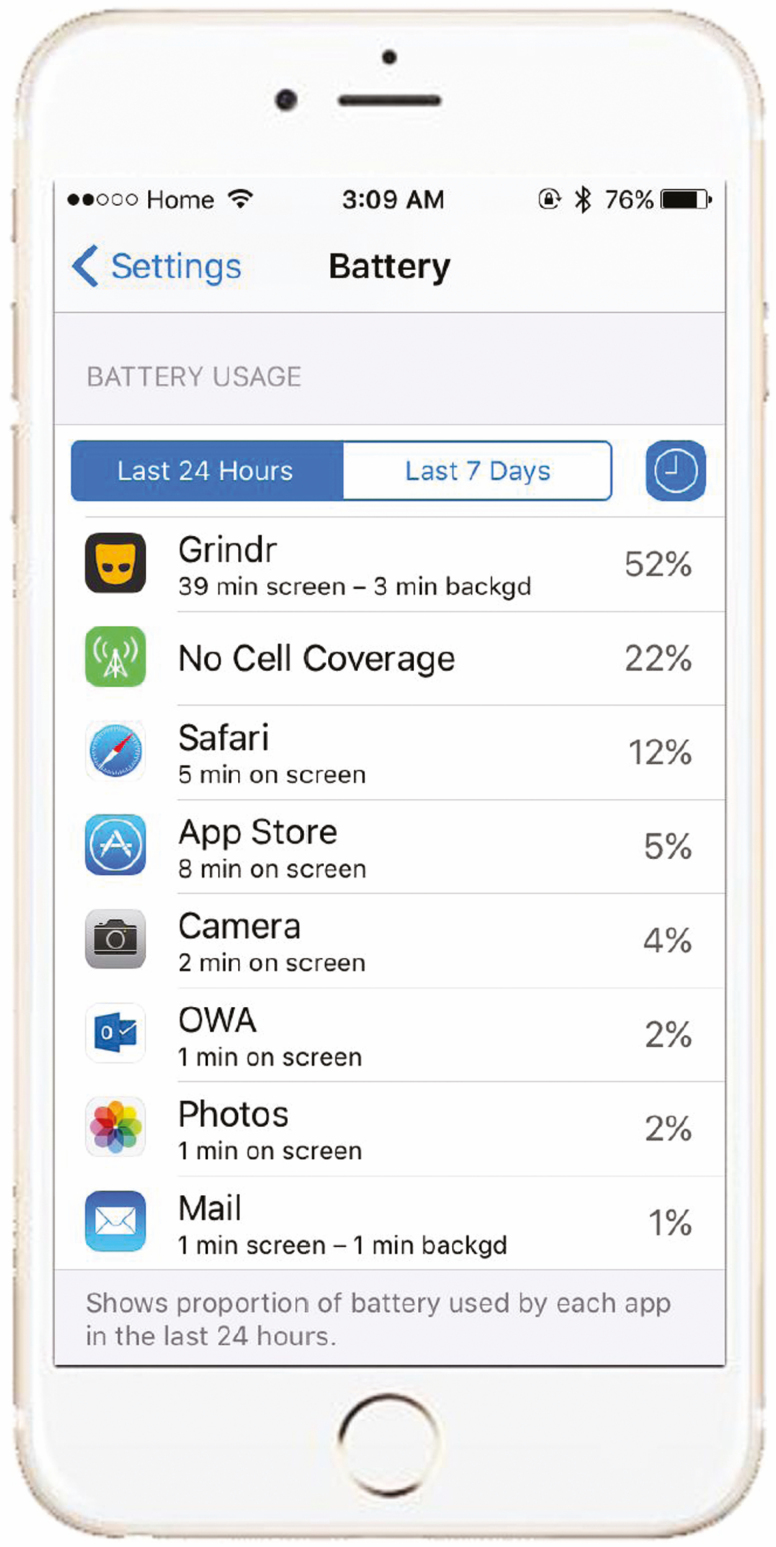
During their testing encounter, all MSM and transgender women participants presenting for “Good to Go” were surveyed for Grindr usage (ie, opening Grindr on their mobile device during the previous 7 days), demographics, substance use, and HIV risk behavior during the previous 3 months, and PrEP use (ie, any PrEP intake during the last 14 days). Participants with iPhones were instructed on how to assess Grindr on-screen activity (ie, time on screen during the last 7 days; automatically recorded by phones) on their phones, and provided that data via the questionnaire (Figure 1).
Figure 1.
iPhone system app that assesses Grindr on-screen activity.
Classification of Risk Behavior
This study utilized the San Diego Early Test (SDET) score as a measure of risk behavior for the target MSM population [7, 21]. The score focuses on current risk for HIV acquisition among MSM: condomless receptive anal intercourse (CRAI) with an HIV-positive MSM, combination of CRAI plus number of male partners, and recent bacterial STI [7, 21]. In the derivation and validation cohorts used to derive the score, symptoms and risk behaviors were both assessed for the 12 months prior to the testing encounter. To take into account the 3-month risk reporting period in “Good to Go,” we created an “adjusted SDET” by adjusting 2 original variables: “the combination of CRAI plus ≥5 male partners in the previous 12 months” to “the combination of CRAI plus ≥2 male partners in the previous 3 months,” and “≥10 male partners in the previous 12 months” to “≥5 male partners in the previous 3 months,” as described elsewhere [22]. We also combined self-reported recent STI with new STI diagnosis at the testing encounter into 1 variable that informed SDET calculation. While the score focused on sexual risks, changes in sexual behavior associated with substance use were also captured [23].
PrEP Initiation
All participants with HIV risk behavior who tested negative for HIV and reported no PrEP use during the last 14 days were offered immediate PrEP beginning in November 2018. For these participants, the first 30 days of PrEP were provided via the “Good to Go” study.
Statistical Analysis
All statistical analyses were conducted using SPSS 25 software (SPSS Inc, Chicago, Illinois). Demographics, PrEP use, PrEP initiation, substance use, risk behaviors, adjusted SDET scores, and HIV/STI diagnoses were compared between participants who reported recent Grindr use vs those who did not using Fisher exact test/χ 2 test for categorical variables and Student t test/Mann-Whitney U test for continuous variables. Univariate and multivariable logistic regression analyses assessed predictors of initiating PrEP after the testing encounter. Variables with a P value <.2 in univariate analysis were included in the multivariable model. Variables in the final model were selected with a stepwise forward procedure. Model discrimination was assessed by the goodness-of-fit Hosmer-Lemeshow statistics. Odds ratios (ORs) and adjusted odds ratios (aORs) including 95% confidence intervals (CIs) were calculated and a P value of <.05 was considered statistically significant. The study was approved by the University of California, San Diego institutional review board and written informed consent was obtained from all participants.
RESULTS
Survey data were collected from 1256 consecutive MSM and transgender women who participated in the “Good to Go” study between September 2018 and June 2019 (Table 1). Median age was 32 years (range, 18–78 years); 421 (33.5%) reported Hispanic ethnicity, 532 were non-Hispanic white (42.3%), 140 non-Hispanic Asian (11.1%), 80 non-Hispanic black (6.4%), and 83 (6.6%) non-Hispanic mixed or other races. The majority identified as male (n = 1237 [98.5%]), and 1017 participants (81%) reported their sexual orientation as gay, 187 (14.9%) as bisexual, 21 (1.7%) heterosexual, and 31 another sexual orientation (2.5%), with all 1256 participants reporting sex with men.
Table 1.
Demographic Data, Risk Behavior, Substance Use Characteristics, and Testing Outcomes of Participants Who Did and Did Not Report Recent Grindr Use
| Variable | Grindr Usersa (n = 580) | Grindr Nonusersa (n = 676) | P Value |
|---|---|---|---|
| Gender | .976 | ||
| Male | 571 (98) | 666 (99) | |
| Transgender female | 5 (1) | 6 (1) | |
| Other nonbinary identity | 4 (1) | 4 (1) | |
| Age, y, mean (SD) | 35 (12) | 38 (13) | < .001 |
| Race/ethnicity | .502 | ||
| White | 371 (64) | 420 (62) | |
| Hispanic | 200 (34) | 221 (33) | .555 |
| Adjusted SDET score, median (IQR) | 2 (0–5) | 0 (0–3) | < .001 |
| Male sex partners (recent 3 mo), median (IQR) | 4 (2–7) | 2 (1–4) | < .001 |
| No. reporting condomless anal intercourse (recent 3 mo) | 297 (51) | 310 (46) | .059 |
| Substance useb | 113 (19) | 105 (16) | .065 |
| Self-reported PrEP intake within last 14 d | 107 (18) | 59 (9) | < .001 |
| Self-reported recent bacterial STI diagnosis (recent 3 mo) | 22 (3.8) | 21 (3.1) | .505 |
| Testing positive for HIV | 9 (6) | 26 (3.8) | .014 |
| Testing positive for chlamydia or gonorrhea | 50 (8.6) | 32 (4.7) | .005 |
| Testing positive for syphilis | 13 (2.2) | 11 (1.6) | .428 |
| Testing positive for HCV | 0 | 4 (0.6) | .129 |
Data are presented as no. (%) unless otherwise indicated.
Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus; IQR, interquartile range; PrEP, pre-exposure prophylaxis; SD, standard deviation; SDET, San Diego Early Test; STI, sexually transmitted infection.
aDefined as within last 7 days.
bSubstances: metamphetamine, cocaine, GHB, poppers, ecstasy, ketamine.
Grindr Use, Risk Behavior, and Testing Outcomes
A total of 580 of 1256 (46%) participants (including 571 men, 5 transgender women, and 4 who identified as other gender) indicated that they had opened Grindr during the previous 7 days. Demographic data, risk behavior, and substance use in participants with and those without recent Grindr use are displayed in Table 1.
Grindr users had higher adjusted SDET risk behavior scores than those not using Grindr (median SDET score, 2 [interquartile range {IQR}, 0–5] vs 0 [IQR, 0–3]; P < .001), driven mostly by having more male sexual partners (median number of male sex partners in the last 3 months, 4 [IQR, 2–7] vs 2 [IQR, 1–4]; P < .001). There were also tendencies toward Grindr users more frequently reporting CRAI (297/580 [51.2%] vs 310/676 [45.9%]; P = .059) or recent illicit substance use (113/580 [19.5%] vs 105/676 [15.5%]; P = .065), whereas there was no difference in self-report of recent bacterial STI diagnosis (3.4% of study population; P = .5).
Grindr users were more likely to test positive for chlamydia or gonorrhea at their testing encounter (50/556 [8.6%] tested positive for 1 or both vs 32/676 [4.7%] of Grindr nonusers; P = .005). Grindr users were overall less likely to test positive for HIV (9/580 [1.6%] vs 26/676 [3.8%] of Grindr nonusers tested positive; P = .014), whereas no difference was observed for syphilis and HCV diagnoses (Table 1).
Grindr Use and PrEP
Of 1256 participants, 1090 (86.8%) reported that they were not taking PrEP (defined as no PrEP intake within last 14 days). Grindr users were more likely to be taking PrEP than Grindr nonusers (107/580 [18.4%] among Grindr users vs 59/676 [8.7%] nonusers; P < .001). Overall, 472 of 1087 (43.4%) of participants who were not taking PrEP reported recent Grindr use. Among those participants who were not taking PrEP, Grindr users had significantly higher sexual risk behavior (median SDET score, 2 [IQR, 0–5] vs 0 [IQR, 0–3] among Grindr users vs nonusers, respectively; P < .001; median numbers of male sex partners, 4 [IQR, 2–6] vs 2 [IQR, 1–4]; P < .001), but no difference was observed regarding CRAI and recent illicit substance use.
From November 2018 when immediate PrEP was made available at our community-based program, PrEP-eligible Grindr users were nearly twice as likely to start PrEP after the testing encounter compared to nonusers (100/406 [24.6%] of Grindr users started PrEP vs 72/514 [14.0%] of nonusers; P < .001). In the multivariable logistic regression analysis, recent Grindr use (OR, 1.61), adjusted SDET score (OR, 1.20 per score point), younger age (OR, 0.96 per year), and diagnosis of chlamydia or gonorrhea infection at “Good to Go” testing encounter (OR, 2.00) were significant and independent predictors of PrEP initiation (Table 2).
Table 2.
Univariate and Multivariable Binary Logistic Regression Models for Predicting Initiation of Pre-exposure Prophylaxis (PrEP) Among Participants Offered PrEP Through the Total Test (n = 920, of Whom 172 Initiated PrEP)
| Univariate Model | Multivariable Modela | |||||
|---|---|---|---|---|---|---|
| Model | OR | (95% CI) | P Value | aOR | (95% CI) | P Value |
| Recent Grindr use | 2.006 | (1.433–2.808) | < .001 | 1.611 | (1.129–2.299) | .009 |
| Adjusted SDET score (per point) | 1.250 | (1.174–1.331) | < .001 | 1.196 | (1.116–1.282) | < .001 |
| Age (per year) | 0.960 | (.944–.976) | < .001 | 0.964 | (.948–.981) | < .001 |
| Substance use last 3 mo | 1.634 | (1.090–2.450) | .017 | NS | … | |
| Diagnosis of chlamydia or gonorrhea infection at testing encounter | 3.751 | (2.139–6.576) | < .001 | 1.996 | (1.076–3.701) | .028 |
| Hispanic ethnicity | 1.381 | (.983–1.940) | .063 | NS | … | |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; NS, not significant; OR, odds ratio; SDET, San Diego Early Test.
aχ 2 = 6.077, P = .639, Hosmer-Lemeshow; forward Wald binary logistic regression.
Grindr On-screen Activity
Of 580 MSM who indicated recent Grindr use, 376 (64.8%) were iPhone users, of which 340 had their iPhone with them at the testing encounter. This allowed us to objectively assess screen time on Grindr. Median on-screen activity during the previous 7 days was significantly higher in those who reported PrEP use within the last 14 days (60/340 [18%]), compared with those who did not (280/340 [82%]); median on-screen time over the previous 7 days was 244 minutes (IQR, 75–534) in those with PrEP vs 142 minutes (IQR, 47–360) in those without (P = .017).
Overall, there was no significant correlation between adjusted SDET scores and Grindr on-screen activity among those not on PrEP (P > .5); however, those at highest risk for HIV (SDET score ≥8), had a trend toward being the highest Grindr utilizers (ie, >90th percentile of time on screen corresponding to >660 minutes during the last 7 days; 5/25 [25%] of those with highest sexual risk vs 21/255 [8.2%] of those with lower sexual risk; P = .053).
DISCUSSION
Over the last decade, MSM have increasingly utilized geosocial dating apps to find sex partners [24]. This study assessed use of the most popular app in 1256 MSM and transgender women undergoing community-based HIV and STI screening in San Diego. In our sample, those who use Grindr reported behaviors that placed them at greater risk for HIV. Although Grindr users were more likely than nonusers to be taking PrEP, more than 8 in 10 were not using FTC/TDF at the time of their testing encounter. Grindr users were more likely to initiate PrEP after the testing encounter, indicating that Grindr could serve as a platform for educating those at high risk for HIV about the benefits of PrEP and linking users to programs that offer PrEP.
Consistent with previous reports, Grindr users in our study had higher sexual risk and were more likely to test positive for chlamydia and gonorrhea infections [4, 10, 11]. Additionally, we found that Grindr users were more likely to have taken PrEP within 2 weeks before the testing encounter (18.7% among Grindr users vs 8.7% among nonusers) and were overall—possibly as a consequence—less likely to test positive for HIV (9 new diagnoses among Grindr users vs 26 new diagnoses among nonusers). Importantly, the majority of Grindr users (81.3%) were not on PrEP, despite having significantly higher sexual risk behavior compared to nonusers. After the testing encounter, Grindr users were more likely to start PrEP through our program (24.6% of Grindr users started PrEP vs 14% of nonusers), and Grindr use remained an independent predictor of PrEP initiation in multivariate analysis (other predictors were higher sexual risk, younger age, and chlamydia/gonorrhea diagnosis). One explanation for the comparatively high rate of PrEP initiation among Grindr users despite low current PrEP usage is that PrEP has simply not been previously made readily available to them before—a linkage that may have been enhanced by HIV testing and counseling, review of HIV risks, or a positive STI screen.
This study also introduced an objective measure of Grindr on-screen activity, allowing quantification of active Grindr use in minutes. Among Grindr users, those with the highest sexual risk behavior were found to be actively using Grindr significantly more compared to those with lower sexual risk behavior. Characterization of Grindr on-screen activity may be a useful tool for identifying MSM and transgender women who may benefit the most from PrEP and more frequent STI testing.
Given the higher risk behavior and greater acceptance of PrEP among Grindr users, PrEP promotional messages and linkages to care on the Grindr platform could enhance PrEP uptake, as well as increase testing for HIV and STIs. The surge of dating apps and their association with high-risk sex offers unique opportunities for broad delivery of prevention messages [11, 25]. Grindr may provide a real opportunity to reach those at risk and substantially increase PrEP awareness and uptake. However, how to effectively deliver these messages on Grindr needs to be further evaluated. Grindr commercially offers banner ads, which can convey an HIV prevention message allowing messages to be targeted toward specific regions with messages that are tailored toward specific PrEP providers. Previous studies evaluated Grindr ads for recruitment for HIV prevention interventions [26–30], and found that Grindr ads can help recruitment for HIV prevention efforts, particularly among older MSM. However, generic banner ads may be less effective at reaching hidden populations [28, 30–32], and ad costs are generally predicted to increase [25, 28, 31]. Banners and advertisements generally do not harness the social dimension of geospatial networking apps. Behavior and behavior change diffuse through social networks of close ties and are affected by individuals’ perceptions of what their network members do [33–35]. Therefore, a more personalized delivery of prevention messages, for example, via advertisement on profile pictures of selected opinion leaders, may be more effective than banner ads for delivering prevention messages to Grindr users. Indeed, network-based recruitment has proven very effective at locating people with undiagnosed HIV infections [36, 37]. To further enhance PrEP use, Grindr profiles could potentially also incorporate a function that allows users to disclose whether they are on PrEP. Each of these approaches warrant further investigation.
There are important limitations to this study. The study took place at a single community-based testing site; thus, our findings might not be generalizable to other locations and populations. Furthermore, slight modifications of the previously validated SDET risk score were necessary to fit our available data and analyses. PrEP use was evaluated based on self-reported PrEP intake during the last 14 days only. Therefore, the study may have not consistently captured on demand PrEP users [38], and thereby slightly underestimated the number of PrEP users among both Grindr users and nonusers. Future studies should consider assessing on-demand PrEP use and to also incorporate objective measures of PrEP use to help establish if Grindr also translates to higher adherence. We also did not collect data on the usage of other geospatial networking app platforms (such as Scruff, Hornet, etc), which may be used by persons who have a higher risk profile or had a similar risk profile and biased the results of comparisons between Grindr users and nonusers toward the null. Nevertheless, with Grindr being the most popular app, it is likely that users of these other apps were also Grindr users. Finally, our subanalysis on on-screen activity was limited to iPhone users.
In conclusion, Grindr users took more sexual risks and had more partners than those who did not use the geosocial networking app, but they also were more likely than nonusers to take PrEP or initiate PrEP. These findings suggest that Grindr could be an effective vehicle for reaching people at risk for contracting HIV or other STIs, to encourage HIV and STI testing, and to engage them to start PrEP.
Notes
Presented in part: IDWeek 2019, Washington, District of Columbia, 5 October 2019. Presentation number 1961.
Financial support. This work was primarily supported by the National Institutes of Health (Primary Infection Research Consortium grant number AI106039). In addition, the work was partially supported by other grants from the National Institutes of Health (grant numbers MH113477, AI 036214, AI064086, MH081482, DA023606, and MH062512) and the California HIV Research Program (grant numbers PR15-SD-021 and HD15-SD-059).
Potential conflicts of interest. M. H. and S. J. L have received grant funding from Gilead Sciences. D. G. has consulted for Greenwich Biosciences. D. M. S. has consulted for the AIDS Healthcare Foundation. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Martin TCS, Chaillon A, Graves SK, et al. Genetic network analysis to assess the risk of human immunodeficiency virus transmission among men who have sex with men seeking partners on the internet [manuscript published online ahead of print 6 April 2019]. Clin Infect Dis 2019. doi:10.1093/cid/ciz278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Phillips G 2nd, Magnus M, Kuo I, et al. Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington, DC. AIDS Behav 2014; 18:1630–7. [DOI] [PubMed] [Google Scholar]
- 3. Beymer MR, Weiss RE, Bolan RK, et al. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect 2014; 90:567–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Winetrobe H, Rice E, Bauermeister J, Petering R, Holloway IW. Associations of unprotected anal intercourse with Grindr-met partners among Grindr-using young men who have sex with men in Los Angeles. AIDS Care 2014; 26:1303–8. [DOI] [PubMed] [Google Scholar]
- 5. Lehmiller JJ, Ioerger M. Social networking smartphone applications and sexual health outcomes among men who have sex with men. PLoS One 2014; 9:e86603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rendina HJ, Jimenez RH, Grov C, Ventuneac A, Parsons JT. Patterns of lifetime and recent HIV testing among men who have sex with men in New York City who use Grindr. AIDS Behav 2014; 18:41–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hoenigl M, Weibel N, Mehta SR, et al. Development and validation of the San Diego Early Test Score to predict acute and early HIV infection risk in men who have sex with men. Clin Infect Dis 2015; 61:468–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eaton LA, Maksut JL, Gamarel KE, Siembida EJ, Driffin DD, Baldwin R. Online sex partner meeting venues as a risk factor for testing HIV positive among a community-based sample of black men who have sex with men. Sex Transm Dis 2016; 43:360–4. [DOI] [PubMed] [Google Scholar]
- 9. Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care 2007; 19:822–7. [DOI] [PubMed] [Google Scholar]
- 10. Chan PA, Crowley C, Rose JS, et al. A network analysis of sexually transmitted diseases and online hookup sites among men who have sex with men. Sex Transm Dis 2018; 45:462–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Landovitz RJ, Tseng CH, Weissman M, et al. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. J Urban Health 2013; 90:729–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Paz-Bailey G, Hoots BE, Xia M, et al. Trends in internet use among men who have sex with men in the United States. J Acquir Immune Defic Syndr 2017; 75(Suppl 3):S288–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cruess DG, Burnham KE, Finitsis DJ, et al. Online partner seeking and sexual risk among HIV+ gay and bisexual men: a dialectical perspective. Arch Sex Behav 2017; 46:1079–87. [DOI] [PubMed] [Google Scholar]
- 14. Hoenigl M, Jain S, Moore D, et al. Substance use and adherence to HIV preexposure prophylaxis for men who have sex with men. Emerg Infect Dis 2018; 24. doi:10.3201/eid2412.180400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hoenigl M, Hassan A, Moore DJ, et al. Predictors of long-term HIV pre-exposure prophylaxis adherence after study participation in men who have sex with men. J Acquir Immune Defic Syndr 2019; 81:166–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Holloway IW, Dougherty R, Gildner J, et al. Brief report: PrEP uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. J Acquir Immune Defic Syndr 2017; 74:15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoenigl M, Graff-Zivin J, Little SJ. Costs per diagnosis of acute HIV infection in community-based screening strategies: a comparative analysis of four screening algorithms. Clin Infect Dis 2016; 62:501–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoenigl M, Anderson CM, Green N, Mehta SR, Smith DM, Little SJ. Repeat HIV-testing is associated with an increase in behavioral risk among men who have sex with men: a cohort study. BMC Med 2015; 13:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention. Discordant results from reverse sequence syphilis screening—five laboratories, United States, 2006–2010. MMWR Morb Mortal Wkly Rep 2011; 60:133–7. [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention. US Public Health Service: preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. Atlanta, GA: CDC, 2018.
- 21. Dijkstra M, Lin TC, de Bree GJ, Hoenigl M, Schim van der Loeff MF. Validation of the San Diego Early Test score for early HIV infection among Amsterdam men who have sex with men [manuscript published online ahead of print 10 September 2019]. Clin Infect Dis 2019. doi:10.1093/cid/ciz895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cohen SE, Vittinghoff E, Philip SS, et al. Sexual risk behaviors and sexually transmitted infections among MSM participating in the US PrEP Demo Project. In: World HIV and STD Congress, Brisbane, Australia, 2015.
- 23. Hoenigl M, Chaillon A, Moore DJ, Morris SR, Smith DM, Little SJ. Clear links between starting methamphetamine and increasing sexual risk behavior: a cohort study among men who have sex with men. J Acquir Immune Defic Syndr 2016; 71:551–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men’s use of the Internet: research from the 1990s through 2013. J Sex Res 2014; 51:390–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Holloway IW, Rice E, Gibbs J, Winetrobe H, Dunlap S, Rhoades H. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav 2014; 18:285–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alarcón Gutiérrez M, Fernández Quevedo M, Martín Valle S, et al. Acceptability and effectiveness of using mobile applications to promote HIV and other STI testing among men who have sex with men in Barcelona, Spain. Sex Transm Infect 2018; 94:443–8. [DOI] [PubMed] [Google Scholar]
- 27. Burrell ER, Pines HA, Robbie E, et al. Use of the location-based social networking application Grindr as a recruitment tool in rectal microbicide development research. AIDS Behav 2012; 16:1816–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huang E, Marlin RW, Young SD, Medline A, Klausner JD. Using Grindr, a smartphone social-networking application, to increase HIV self-testing among black and Latino men who have sex with men in Los Angeles, 2014. AIDS Educ Prev 2016; 28:341–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sun CJ, Stowers J, Miller C, Bachmann LH, Rhodes SD. Acceptability and feasibility of using established geosocial and sexual networking mobile applications to promote HIV and STD testing among men who have sex with men. AIDS Behav 2015; 19:543–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rosengren AL, Huang E, Daniels J, Young SD, Marlin RW, Klausner JD. Feasibility of using Grindr(TM) to distribute HIV self-test kits to men who have sex with men in Los Angeles, California. Sex Health 2016. doi:10.1071/SH15236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Badal HJ, Stryker JE, DeLuca N, Purcell DW. Swipe right: dating website and app use among men who have sex with men. AIDS Behav 2018;22:1265–72. [DOI] [PubMed] [Google Scholar]
- 32. Lampkin D, Crawley A, Lopez TP, Mejia CM, Yuen W, Levy V. Reaching suburban men who have sex with men for STD and HIV services through online social networking outreach: a public health approach. J Acquir Immune Defic Syndr 2016; 72: 73–8. [DOI] [PubMed] [Google Scholar]
- 33. Schneider JA, Zhou AN, Laumann EO. A new HIV prevention network approach: sociometric peer change agent selection. Soc Sci Med 2015; 125:192–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Laumann EO, Gagnon JH, Michael RT, Michaels S. The social organization of sexuality: sexual practices in the United States. Chicago, IL: University of Chicago Press, 2000. [Google Scholar]
- 35. Laumann EO. Network analysis in large social systems: Some theoretical and methodological problems. New York: Academic Press, 1979. [Google Scholar]
- 36. Smyrnov P, Williams LD, Korobchuk A, et al. Risk network approaches to locating undiagnosed HIV cases in Odessa, Ukraine. J Int AIDS Soc 2018; 21. doi:10.1002/jia2.25040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nikolopoulos GK, Pavlitina E, Muth SQ, et al. A network intervention that locates and intervenes with recently HIV-infected persons: the Transmission Reduction Intervention Project (TRIP). Sci Rep 2016; 6:38100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Molina JM, Capitant C, Spire B, et al. ANRS IPERGAY Study Group On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med 2015; 373:2237–46. [DOI] [PubMed] [Google Scholar]