Abstract
A rare case melanotic neuroectodermal tumor of infancy occurring in 2-year-old girl affecting left maxilla is described. Computed tomography showed benign expansile type of lesion affecting left maxilla. The lesion was surgically excised completely. Histopathology confirmed the diagnosis of melanotic neuroectodermal tumor. Four months' follow-up showed no recurrence.
Keywords: Benign tumor, infancy tumor, neuroectodermal tumor
Introduction
Melanotic neuroectodermal tumor of infancy (MNTI) is an extremely rare benign tumor that usually affects premaxilla in newborns of <1 year of age. Clinically, this tumor is expressed as nonulcerative, rapidly progressing, painless pigmented swelling on the anterior maxilla.[1,2,3,4] MNTI is known by many alternative names such as melanotic progonoma, pigmented epulis of infancy, pigmented ameloblastoma, and melanotic epithelial odontoma.[1] Besides the involvement of maxillary region (68%–80%), it also involves skull (10.8%), mandible (5.8%), and brain (4.3%).[5] The mean age of patients as reported in the literature is 4.3 months and having near-equal gender predilection ratio of 6:7.[6,7,8] We hereby present a case of MNTI treated with wide surgical excision along with review on recent histopathologic knowledge and treatment considerations.
Case Report
A 2-year-old female baby came to department of oral medicine and radiology with complain of swelling over the left maxillary region. Parents noted swelling 6 months before which was slowly growing initially and started progressing rapidly since 1½ month. There was no relevant medical or family history and development of child was normal for her age. On clinical examination, a single nonpedunculated, pigmented swelling of 4.5 cm × 3 cm seen without any ulceration or discharge seen over left maxillary region [Figure 1]. The swelling has obliterated labial vestibule uplifting upper lip and causing flaring of nose on the right side. Color of the overlying skin in the center and next to ala of nose on affected side changed to pinkish red. On palpation swelling was nontender, soft to firm in consistency, compressible, and non-fluctuant. Radiographic presentation of computed tomography images [Figure 2] showed a single expansile solid lesion in the right anterior maxilla with epicenter lying in the maxillary anterior alveolar ridge. The tumor mass surgically enucleated [Figure 3] and sent for histopathological examination. Histological features were consistent with a small round cell tumor favoring MNTI [Figures 4 and 5], displaying the biphasic population of cells. Immunohistochemical studies were done for confirmation. Thus, a final diagnosis of MNTI was made by correlating clinical, surgical findings, histopathological, and immunohistochemistry (IHC) findings.
Figure 1.

Clinical photograph showing swelling over the left side of face
Figure 2.
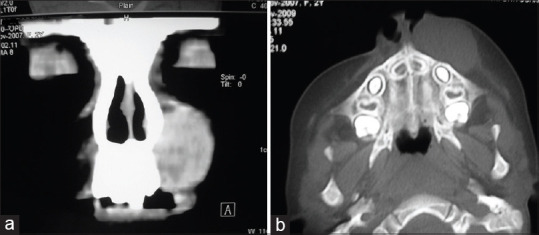
(a) Coronal computed tomography showing expansile lesion. (b) Axial computed tomography showing expansile lesion
Figure 3.
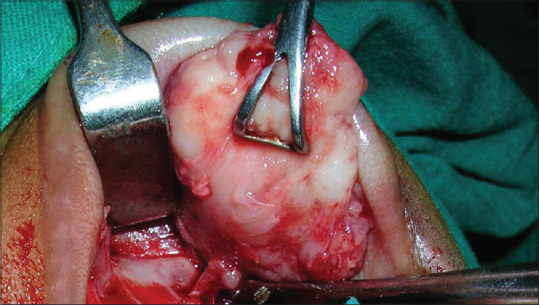
Surgically excised tumor mass
Figure 4.
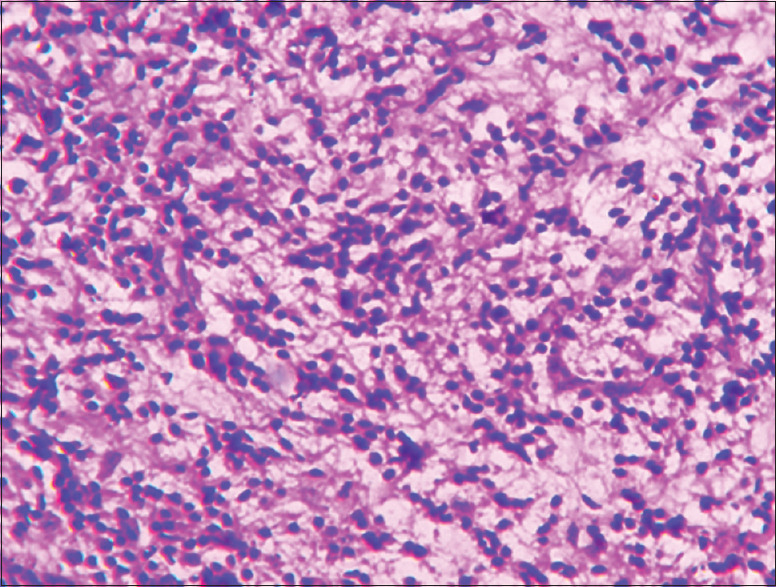
Small round tumor cells arranged in diffuse and alveolar pattern separated by thin fibrovascular stroma (H and E, ×10)
Figure 5.
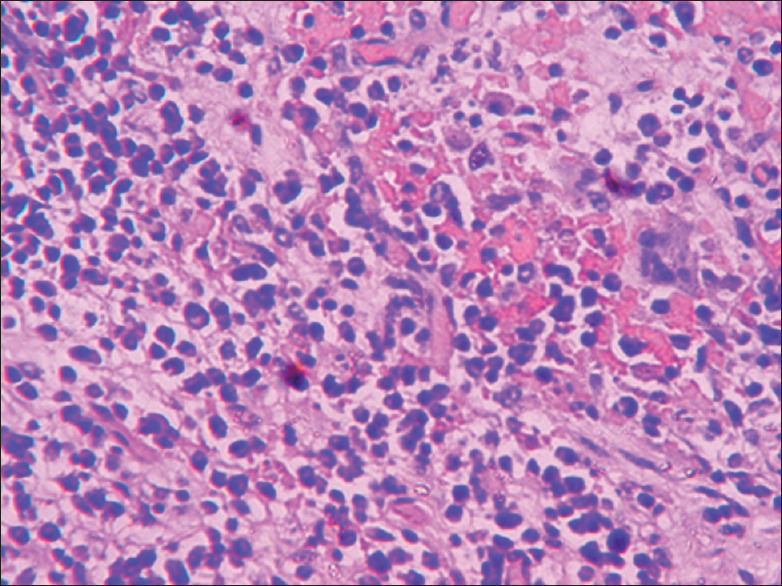
Two distinctive types of cells – large cells arranged peripherally with abundant cytoplasm, round vesicular nucleus and brown pigment; and small cells with scanty cytoplasm and hyperchromatic round nuclei were seen in the center (H and E, ×40)
Discussion
The very first case of MNTI reported in the literature in 1918 by Krompecher as “congenital melanocarcinoma.”[9] He described pigmented lesion associated with developing tooth in a 2-month-old infant. The origin of this tumor was thought to be from odontogenic epithelium or retinal rests acquiring many names such as pigmented ameloblastoma, melanotic adamantinoma, melanotic epithelial odontoma, retinal anlage tumor, retinal choristoma, melanotic progonoma, atypical ameloblastoma, pigmented teratoma, retinoblastic teratoma, and pigmented epulis. However, ultrastructural, IHC, and electron microscopic studies along with occasional increased urinary levels of vanillylmandelic acid (VMA),[10] it is now confirmed that this tumor originates from cells of neural crest origin. Borello and Gorlin,[10] in 1966, suggested the term “MNTI” which is now accepted worldwide. A high urinary secretion of VMA is found to be significant in diagnosing tumor of neural crest origin as reported in case series of Johnson et al. Clinical appearance of this tumor is a nonpedunculated solid swelling that involves premaxilla. The presence of discoloration over the surface may be attributed to melanin pigment giving bluish hue on some part of the swelling. One can notice obvious facial asymmetry, obliteration of vestibule, displacement of the teeth, and difficulty in feeding. There could be possibility of the formation of pseudo-encapsulated secondary to reactive bone formation though it is fast growing in nature, it is considered as benign. The differential diagnosis of MNTI relates to wide variety of lesions which includes developmental cysts: nasopalatine cyst and globulomaxillary cyst. Odontogenic lesions: Odontoma, ameloblastoma, ameloblastic fibroma, odontogenic myxoma, adenoameloblastoma, and odontogenic keratocyst. Nonodontogenic nonneoplastic lesion: Central giant cell granuloma, fibrous dysplasia, and arteriovenous malformation. Nonodontogenic neoplastic lesions: Rhabdomyosarcoma, Burkitt's lymphoma, Langerhans cell histiocytosis, and Ewing sarcoma. However, the above list can be reduced to few based on clinical and radiological findings. Conventional radiographs can reveal radiolucent lesion with or without defined borders. Computed tomography scan reveals hyperdense masses most frequently but hypodense masses are also reported. The extent and margin of the lesion is well detected on computed tomography which help the surgeon to perform precisely. IHC stains more precisely helps to arrive at diagnosis of MNTI.
Epithelioid cells stains positive commonly with epithelial membrane antigen, cytokeratin, vimentin, and HMB-45 that shows epithelial and melanotic differentiation. These cells are often nonreactive with protein S-100 which helps in differentiating lesions such as melanoma. Smaller cell nests are positive with neurogenic markers such as neuron-specific enolase, glial fibrillar acidic protein, and synaptophysin. Staining variability shows the multiphenotypical character of the tumor.[1] Electron microscopic studies show that there are group of neuroectodermal tumors that originates from neural crest cells. Elevated alpha flavoprotein level and positive c-myc staining also found to be associated with this tumor similar to other neuroectodermal tumors.[1] Although there are no similar genetic changes which can link MNTI to other neuroectodermal tumors. Recent studies shows recurrence rate of 10%–60% following conservative surgical excision with 6.5% cases that shows distant metastasis. Recurrence may be attributed to multicentric growth, invasion of tumor edge into bone and lack of proper encapsulation.[2] Surgical excision along with removal of 5 mm of healthy tissue surrounding the tumor is preferred treatment of choice to prevent recurrence of tumor. Average recurrence rate reported for MNTI is around 20%.[5] In cases of MNTI approximating vital structures chemotherapy or radiotherapy can be considered. However, this is controversial. Reconstruction of missing part such as portion of alveolus or missing teeth is delayed until the patient achieves skeletal maturity. Meanwhile, removable prosthesis can achieve functional purpose for patients.[4]
Conclusion
Although MNTI a benign lesion, early diagnosis is utmost important as it can cause local destruction. Considering occurrence of this tumor in growing age careful follow-up becomes necessary to check for recurrence and also to see any effect of surgical trauma on growth and development of maxilla-facial structures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kaya S, Unal OF, Saraç S, Gedikoǧlu G. Melanotic neuroectodermal tumor of infancy: Report of two cases and review of literature. Int J Pediatr Otorhinolaryngol. 2000;52:169–72. doi: 10.1016/s0165-5876(99)00302-x. [DOI] [PubMed] [Google Scholar]
- 2.Franchi G, Sleilati F, Soupre V, Boudjemaa S, Josset P, Diner PA, et al. Melanotic neuroectodermal tumour of infancy involving the orbit and maxilla: Surgical management and follow-up strategy. Br J Plast Surg. 2002;55:526–9. doi: 10.1054/bjps.2002.3910. [DOI] [PubMed] [Google Scholar]
- 3.Adad SJ, Pinheiro SW, Marinho EO, Reis MA, Rua AM, Rodrigues DB. Melanotic neuroectodermal tumor of infancy (MNTI) Diagn Cytopathol. 2004;30:67–9. doi: 10.1002/dc.10389. [DOI] [PubMed] [Google Scholar]
- 4.Chaudhary S, Manuja N, Ravishankar CT, Sinha A, Vijayran M, Singh M. Oral melanotic neuroectodermal tumor of infancy. J Indian Soc Pedod Prev Dent. 2014;32:71–3. doi: 10.4103/0970-4388.127064. [DOI] [PubMed] [Google Scholar]
- 5.Neven J, van der Kaa CH, Loonen JG, de Wilde PC, Merkx MA. Recurrent melanotic neuroectodermal tumor of infancy: A proposal for treatment protocol with surgery and adjuvant chemotherapy. Oral Surge Oral Med Oral Pathol Oral Radiol Endod. 2008;106:493–6. doi: 10.1016/j.tripleo.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Puchalski R, Shah UK, Carpentieri D, McLaughlin R, Handler SD. Melanotic neuroectodermal tumor of infancy (MNTI) of the hard palate: Presentation and management. Int J Pediatr Otorhinolaryngol. 2000;53:163–8. doi: 10.1016/s0165-5876(00)00315-3. [DOI] [PubMed] [Google Scholar]
- 7.Antunes AC, Freitas RM, Oliveira PP, Rebouças RG. Melanotic neuroectodermal tumor of infancy: Case report. Arq Neuropsiquiatr. 2005;63:670–2. doi: 10.1590/s0004-282x2005000400022. [DOI] [PubMed] [Google Scholar]
- 8.Tan O, Atik B, Ugras S. Melanotic neuroectodermal tumor in a newborn. Int J Pediatr Otorhinolaryngol. 2005;69:1441–4. doi: 10.1016/j.ijporl.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Krompecher E. Zur Histogenese and morphologic der adimantinome und sonstiger kiefergeschwülste. Beitr Path Anat. 1918;64:165–97. [Google Scholar]
- 10.Borello ED, Gorlin RJ. Melanotic neuroectodermal tumor of infancy-a neoplasm of neural crese origin. Report of a case associated with high urinary excretion of vanilmandelic acid. Cancer. 1966;19:196–206. doi: 10.1002/1097-0142(196602)19:2<196::aid-cncr2820190210>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]


