The coronavirus disease 2019 (COVID-19) pandemic has posed a significant burden on health systems across the globe by overwhelming the capacity for healthcare provision in high-income and low- and middle-income countries (LMICs) alike [1]. Healthcare institutions and regulators had to rapidly adapt or develop policies for patient care and issue specific infection prevention and control (IPC) guidance to mitigate and prevent SARS-CoV2 transmission within healthcare settings. This was due to the high number of cases and the potential for transmission of SARS-CoV2 between patients, from patient to healthcare workers and vice versa and between healthcare workers. While high-income countries usually have their own centralized institutions that issue recommendations for practice such as the Center for Disease Control and Prevention in the USA and Public Health England, LMICs look to the World Health Organization (WHO) for guidance. The WHO IPC recommendations [2] have proven to be an invaluable resource for many LMICs in preparing their response to the COVID-19 pandemic, and were swiftly adopted and implemented in many settings.
A shortcoming of this guidance, however, was the lack of emphasis on the need to develop setting-specific and individualized risk assessment tools and on tailoring preventative measures to the risk of exposure that healthcare workers may experience in their specific roles.
This has been particularly apparent with regards to the guidance on the use of personal protective equipment (PPE). The WHO guidance on the rational use of PPE for COVID-19 issued in April 2020 attempted to stratify PPE by setting, target personnel and activity [3]. However, neither target personnel nor activities are comprehensive and applicable to all settings and countries. While the WHO recommendations include healthcare workers and cleaners providing direct care in rooms occupied by patients with COVID-19 and advises on specific PPE, it does not for example include housekeepers serving food, handling linen or incinerator personnel. Their contact with patients is mostly at a distance and relatively short. Are gowns and eye protection really the appropriate level of PPE for this cadre of staff? Furthermore, the activities and degree of exposure of these cadres may differ across different settings. Similarly, doctors conducting ward rounds outside the intensive care setting or providing specialist input may only spend limited time in patients' rooms. They are unlikely to be exposed to splashes and hence goggles or face shields seem unnecessary. WHO guidelines are of course not meant to cover every eventuality and context. This is exactly the reason why locally adapted risk assessment tools are crucial to guide the decision on who should wear what level of PPE and when. The WHO document only mentions the word risk assessment in the context of outpatient consultations. Somewhat surprisingly, the WHO guidance document recommends level 2 PPE for laboratory technicians despite respiratory samples being processed in BSL-2 cabinets. This guidance does not align with standard laboratory practices which would usually include a thorough risk assessment with engineering and administrative controls taken into account.
Without awareness of the need to conduct detailed local risk assessments and in the absence of clear risk assessment tools [4] and definitions of exposures, healthcare institutions in some settings implemented blanket recommendations for PPE use not taking into account other IPC measures such as ventilation, job role, proximity and duration of patient contact and type of ‘care’ provided and aimed for maximum perceived security rather than evidence [5]. This in turn has led to confusion and incorrect perceptions of risk among staff, leading to the belief that everybody working in a building where patients with COVID-19 are admitted and cared for is at high risk of transmission and to fears of entering COVID-19 wards [6]. Because of that staff in non-patient facing roles such as security and kitchen personnel are often using the same level of PPE as nurses and doctors caring for COVID-19 patients (Fig. 1 ). PPE overuse and the focus on disposable gowns, full bodysuits and gloves (rather than hand hygiene and using cotton gowns which can be washed) has resulted in excess medical waste and in some instances shortages of PPE for those most in need of it [7]. Furthermore, excessive PPE may also increase the risk of exposure by incorrect doffing and detract from frequent hand hygiene.
Fig. 1.
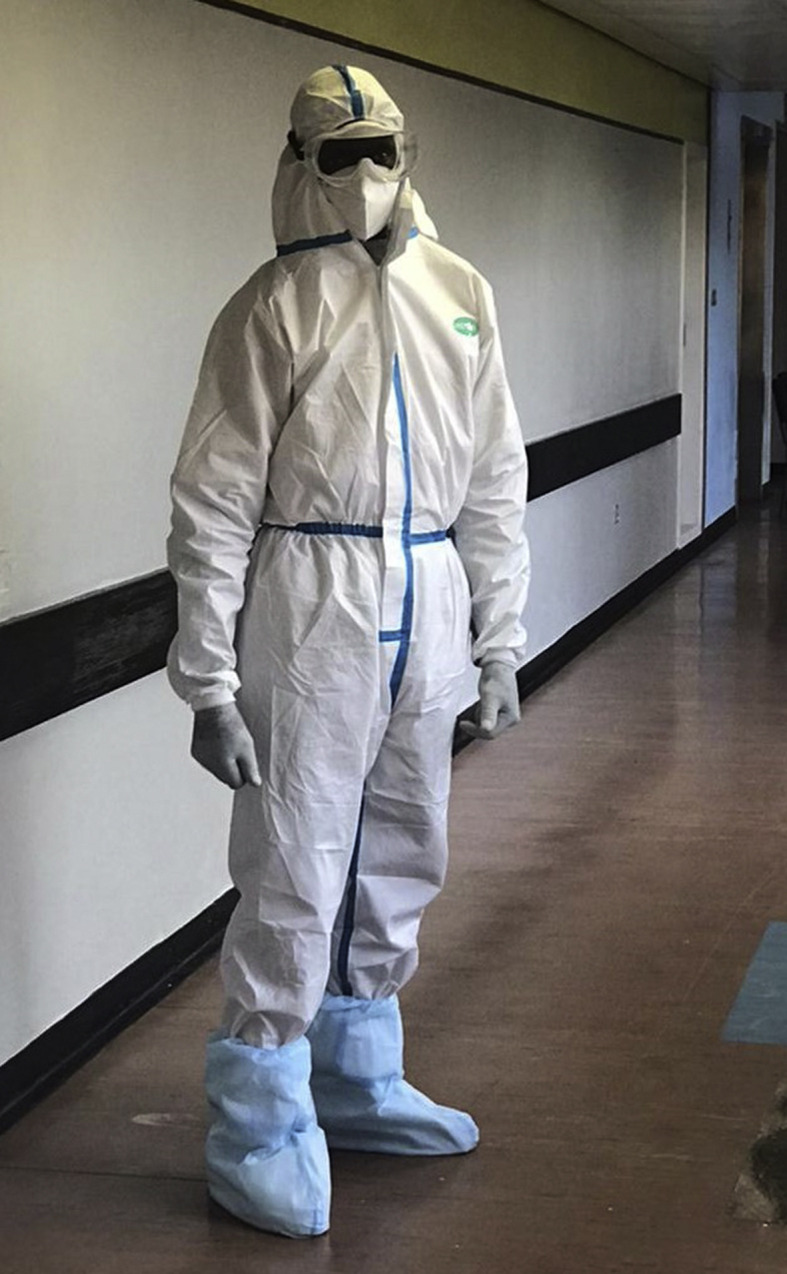
Security guard from a transit area who does not come in direct contact with COVID-19 patients (Harare, Zimbabwe).
Importantly, the scramble of high-income countries to procure PPE and the extensive media coverage on PPE shortages has conveyed the false image that PPE is the centrepiece of IPC measures for preventing SARS-CoV2 transmission.
However, PPE is the least effective IPC measure and at the bottom of the IPC hierarchy of measures to mitigate and prevent occupational hazards. Other IPC interventions such as engineering controls and administrative controls are considered to play a more important role in preventing transmission [8]. These controls include optimal ventilation, thorough and regular cleaning and disinfection of work areas and equipment, use of well-maintained BSL-2 cabinets in laboratories undertaking SARS-CoV2 testing, ensuring availability of hand sanitizer, soap and water for hand hygiene, patient triage according to risk and employee health monitoring [9].
Outside the workplace, healthcare workers and the general public are exposed to an abundance of inadequate messaging and (mis)information from non-expert sources [10]. Non-expert sources often overemphasize the risk of getting infected with SARS-CoV2 and developing severe disease and/or long-term sequelae. They tend to use words and images aimed at creating strong emotions, notably anxiety and fear. Images of people wearing level 3 PPE at state funerals [11] may further augment the impression of a highly transmissible ‘deadly’ virus. Inaccurate messaging may be stronger and have greater influence on healthcare workers from LMICs because of unavailability or poor access to information from other expert sources. This poses a particular challenge to IPC teams when training, informing and educating healthcare workers on SARS-CoV2 transmission and how best to prevent it. Their target audience may have already formed fixed opinions and beliefs, which are not necessarily grounded in scientific evidence. Furthermore, healthcare workers may feel extremely vulnerable and at high risk of SARS-CoV-2 infection. In these circumstances the rational (adequate) use of PPE is extremely difficult to implement.
Different groups involved within a country COVID-19 response have issued IPC guidelines including the use of PPE with slightly differing content and/or recommendations, which may have led to confusion among healthcare workers. This emphasizes the need for communication between different response teams and calls for joint efforts in rapid guideline development. Furthermore, there is a need for close collaboration between national outbreak response teams traditionally responsible for outbreak response (public health specialist working for governmental organizations) and those responsible for facility-based IPC programmes. Going forward the COVID-19 response provides a great opportunity to enhance collaborations and communication between these important expert groups.
To address the inappropriate use of PPE, policy makers and healthcare facilities need to endorse national and local IPC guidelines, which recommend levels of PPE based on risk assessment ultimately aiming to provide optimal PPE to all cadres of healthcare workers [12]. These recommendations then need to be adapted by facility-based IPC teams and embedded in IPC programmes covering all components of standard and transmission-specific based precautions. IPC guidelines need to emphasize the importance of non-PPE related control measures; regular monitoring of these measures needs to be implemented. Replacing disposable plastic gowns with reusable cotton gowns will ensure sustainability while providing the same level of protection [3]. Appropriate messaging is key in reassuring healthcare workers that the level of PPE is aimed at providing maximum protection rather than cost savings. There is also a need for tailored communication of risk and protective measures to different cadres of healthcare workers. Additionally, communication channels beyond conventional training sessions need to be considered for effective information, education and communication. This may include smartphone-based messaging groups chaired and monitored by IPC specialists, twitter and national radio and television. Ultimately the narrative around PPE will need to change from a resource which healthcare workers were deprived of early on in the pandemic and still are in some settings, to PPE being one of several control measures, which needs to be used rationally and in combination with other measures.
Transparency declaration
The authors declare that they have no conflicts of interest. Funding: I.D.O. received funding though the Wellcome Trust Clinical PhD Programme awarded to the London School of Hygiene & Tropical Medicine (grant number 203905/Z/16/Z).
Author contributions
I.D.O., K.K. and R.A.F. conceived the idea and drafted the manuscript; M.T.M., V.R. and V.M. reviewed and commented on the manuscript draft. All authors approved the final version of the manuscript.
Editor: L. Leibovici
References
- 1.World Health Organization . WHO; Geneva: 2020. COVID-19 strategy update.https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_19 April. Available from: [Google Scholar]
- 2.World Health Organization . WHO; Geneva: 2020. Infection prevention and control guidance - (COVID-19)https://www.who.int/westernpacific/emergencies/covid-19/technical-guidance/infection-prevention-control Available from: [Google Scholar]
- 3.World Health Organization . WHO; Geneva: 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. Interim guidance.https://www.who.int/publications April. Available from: [Google Scholar]
- 4.National guidelines on clinical management of coronavirus disease 2019 (Covid-19). Version 4.0. Disease Control Division, Directorate General of Health Services, Ministry of Health & Family Welfare, Government of the People's Republic of Bangladesh; 2020. http://www.mohfw.gov.bd/index.php?option=com_docman&task=doc_download&gid=22424&lang=en March. Available from: [Google Scholar]
- 5.Tartari E., Hopman J., Allegranzi B., Gao B., Widmer A., Cheng V.C. International Society of Antimicrobial Chemotherapy, I.-I.P.C.W.G. Prevention control, perceived challenges of COVID-19 infection prevention and control preparedness: a multinational survey. J Glob Antimicrob Resist. 2020;22:779–781. doi: 10.1016/j.jgar.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdel Wahed W.Y., Hefzy E.M., Ahmed M.I., Hamed N.S. Assessment of knowledge, attitudes, and perception of health care workers regarding COVID-19, a cross-sectional study from Egypt. J Community Health. 2020:1–10. doi: 10.1007/s10900-020-00882-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook T.M. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic - a narrative review. Anaesthesia. 2020;75:920–927. doi: 10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- 8.The National Institute for Occupational Safety and Health (NIOSH) Hierarchy of controls. Center for disease control and prevention. https://www.cdc.gov/niosh/topics/hierarchy/default.html Available from:
- 9.Islam M.S., Rahman K.M., Sun Y., Qureshi M.O., Abdi I., Chughtai A.A. Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: a global analysis. Infect Control Hosp Epidemiol. 2020:1–11. doi: 10.1017/ice.2020.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garrett L. COVID-19: the medium is the message. Lancet. 2020;395:942–943. doi: 10.1016/S0140-6736(20)30600-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chikwari C.D. Think Global Health; 2020. Coronavirus in Zimbabwe.https://www.thinkglobalhealth.org/article/coronavirus-zimbabwe August. Available from: [Google Scholar]
- 12.National Institute for Communicable Diseases . Department Health, Republic of South Africa; 2020. COVID-19 disease: infection prevention and control guidelines Version 2.https://www.nicd.ac.za/wp-content/uploads/2020/05/ipc-guidelines-covid-19-version-2-21-may-2020.pdf 21 May. Available from: [Google Scholar]


