Abstract
The COVID-19 outbreak has led to fundamental disruptions of health care and its delivery with sweeping implications for patients and physicians of all specialties, including neurosurgery. In an effort to conserve hospital resources, neurosurgical procedures were classified into tiers to determine which procedures have to be performed in a timely fashion and which ones can be temporarily suspended to aid in the hospital's reallocation of resources when equipment is scarce. These guidelines were created quickly based on little existing evidence, and thus were initially variable and required refinement. As the early wave can now be assessed in retrospect, the authors describe the lessons learned and the protocols established based on published global evidence to continue to practice neurosurgery sensibly and minimize disruptions. These operational protocols can be applied in a surge of COVID-19 or another airborne pandemic.
Key words: COVID-19, Guidelines, Neuroanesthesia, Neurosurgical practice, Protocols
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; HEPA, High efficiency particulate air; ICU, Intensive care unit; PPE, Personal protective equipment
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) in December 2019 has led to fundamental disruptions of health care and its delivery affecting every medical specialty. The rapid spread of COVID-19 around the globe caused unprecedented overburdening of our health care system, particularly in regions of extreme virus prevalence. To avert a collapse of the hospital system due to insufficient ventilators and overrun intensive care units (ICUs), stay-at-home orders were instituted to counteract the spread of disease. In addition, hospitals quickly developed new guidelines based on little existing evidence, and thus had to adapt “on the fly.” This had sweeping implications for patients and physicians greatly affecting surgical specialties, including neurosurgery because elective neurosurgical activity was reduced or eliminated to limit the exposure of both health care workers and patients and to protect limited resources for the treatment of patients who contracted the virus. As the early wave can now be assessed in retrospect, it becomes increasingly apparent that the health care system was not prepared for a pandemic of this magnitude, which resulted in countless lives lost. Nevertheless, the end of COVID-19 is not yet in sight.
The complications caused by COVID-19 affect a wide range of organ systems. There is accumulating evidence that suggest the presence of a hypercoagulable and inflammatory state that can result in acute stroke or intracranial hemorrhage even in patients without obvious risk factors.1, 2, 3, 4, 5, 6 Because of the significant implications on neurovascular practices with spikes in case volumes in certain regions, the development of well-defined procedural protocols are of utmost importance. This is key for both the safety of medical staff and patients, as well as hospital operations. It is also important to categorize neurosurgical disease into different tiers to continue to treat patients with neurosurgical disease in a timely fashion before they develop irreversible neurologic deficits.
As more evidence and real-world experience continue to refine the guidelines, the authors describe the lessons learned and the protocols established for the continued sensible neurosurgical practice, which should be applied in a surge of COVID-19 or another airborne pandemic.
Categorizing Neurosurgical Disease into Tiers Based on Severity and Urgency
In the wake of the first wave of COVID-19, institutions created a tiered system in accordance with published guidelines by the American College of Surgeons7 and international neurosurgical societies8, 9, 10 in an effort to conserve hospital resources. This strategy requires the suspension of some surgical procedures based on the urgency of the underlying disease. Following those guidelines, neurosurgical procedures can be classified into tiers.11 , 12 Tier 1 is comprised of neurosurgical emergencies, such as aneurysmal subarachnoid hemorrhage, ischemic stroke, or traumatic spinal cord compression (Table 1 ). These continue to have the highest priority and patients presenting with these conditions are tested for COVID-19 on admission along with routinely obtained blood work. The patients undergo the required treatment as presumptively COVID-19 positive under full precautions. This is done before the test results are obtained to avoid any delay and further neurologic deterioration.
Table 1.
Categorizing Neurosurgical Disease into Tiers Based on Severity and Urgency
| Tier 1 | Tier 2 | Tier 3 |
|---|---|---|
|
|
|
| Treatment is performed with full PPE regardless of COVID-19 status | Patients should be screened and tested for COVID-19 prior to their procedure, and precautions determined after test results are obtained | |
PPE, personal protective equipment.
Patients with primary or metastatic brain tumors near eloquent structures who are deteriorating from mass effect and those with unstable spinal pathology without immediate compromise are classified under tier 2 and should be treated on an urgent or semiurgent basis within 24–72 hours. Such patients are screened with epidemiologic history including recent travel, fever, cough, shortness of breath, et cetera, and are additionally tested with widely available rapid tests. However, because newly developed tests are fraught with relatively high false-negative rates, staff are still instructed to be fully compliant with personal protective equipment (PPE). However, having a documented negative test partially relieves staff from the mental stress that is derived from uncertainty and helps ensure that the patient is not an asymptomatic carrier who can spread the disease to others during their hospital course.
Tier 3 is comprised of conditions that are considered “elective.” A generally accepted notion are patients who are unlikely to suffer neurologic deterioration and include patients scheduled for pain-relief procedures (e.g., spinal cord stimulators, pain pump implants, or lumbar discectomy) or long-term diagnostic testing for epilepsy (such as stereo-encephalography), vagal nerve stimulator placement, or cranioplasty. Surgeries in this category are important to recognize as their temporary suspension aids in the hospital's reallocation of resources when ventilators or PPEs are scarce and are needed to treat critically-ill patients.
Anesthesia Protocols for Safely Performing Neurosurgical Emergencies
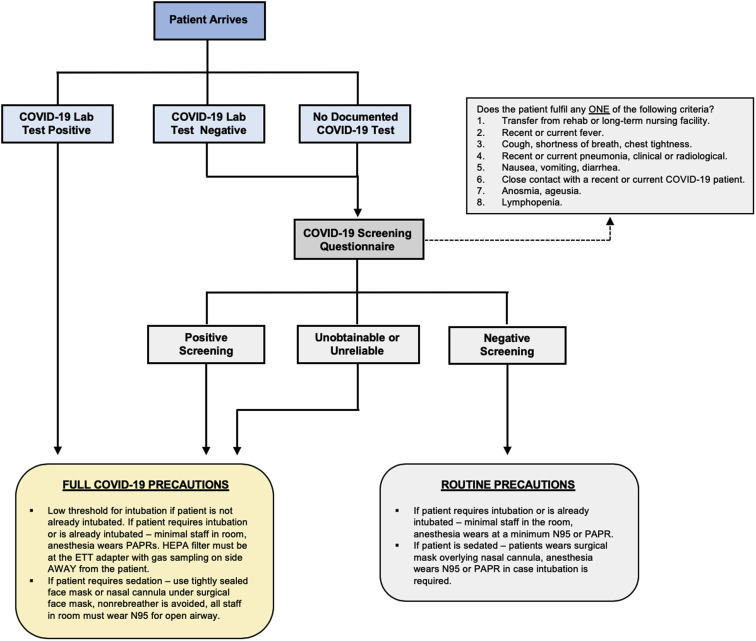
A number of studies have demonstrated that COVID-19 has neuroinvasive potential that leads to an increased risk of cerebrovascular disease, particularly ischemic stroke.2 , 13, 14, 15 However, even in patients with acute neurologic deterioration not related to COVID-19, algorithms have to be implemented to ensure timely triage and treatment of such patients while simultaneously protecting the medical staff. A crucial component is the neuroanesthesia protocol (Figure 1 ).
Figure 1.
Flow chart illustrating the systematic approach to a patient with neurosurgical disease planned for a procedure. PAPR, powered air purifying respirator; HEPA, high efficiency particulate air; ETT, endotracheal tube.
The general consensus is that emergent cases are treated as presumed COVID positive until proven otherwise.16 , 17 In all such cases, full COVID-19 precautions are taken, including the use of N95 masks and face shields, by all personnel present in the operating room or interventional suite. Traditional surgical masks are worn over the N95 mask to avoid getting blood or other bodily fluids on the N95 to maximize their use period. If the patient arrives intubated, it should be ensured to minimize operating room or interventional suite staff and shift changes during a procedure, as well as the attachment of a high efficiency particulate air (i.e., HEPA) filter at the endotracheal tube. If the patient arrives nonintubated, a series of questions can determine if the patient is at high-risk for COVID-19.18 , 19 These include nursing home residents, recent or current fever, cough, shortness of breath or labored breathing, gastrointestinal symptoms (diarrhea, nausea/vomiting), close contact with a COVID-19 patient, anosmia/hypogeusia, or lymphopenia on complete blood count. If the patient is deemed high-risk, a low threshold for intubation should be maintained even if the procedure does not normally require intubation. This is important because if the patient were to deteriorate and emergent intubation becomes necessary under suboptimal conditions (insufficient planning and PPE use), the risk of aerosolization is high, which puts all present staff at risk of contracting the infection. If the patient is deemed low-risk and the procedure does not require intubation (e.g., mechanical thrombectomy for ischemic stroke), then the procedure can proceed in accordance with the protocol for non-COVID-19 care. However, all staff should wear N95 masks and eye protection, and the patient should wear a surgical mask overlying the nasal cannula both during the procedure and transport within the hospital.
The Implementation of Telemedicine in Neurosurgical Practice
One of the most drastic changes in neurosurgery on the stay-at-home orders was the transition to telemedicine. Although telemedicine has been used for Medicare patients since the late 1990s, its utilization did not become widespread until the lockdown measures were implemented at our institution on March 13, 2020. Since then, telemedicine has been used to assess patients in both the inpatient and outpatient settings across all divisions of neurosurgery throughout the country. Our department experienced a tremendous surge in telemedicine use in the span of 1 week, and a number of adjustments were made to minimize the exposure risk for both patients and health care providers.
A study published by our group demonstrated that telemedicine was used for an average of 4.5 ± 0.9 visits per week prior to the COVID-19 lockdown measures, but significantly rose to 180.4 ± 13.9 weekly visits since March 13, 2020 (P < 0.001).20 Highest surge was seen in the spine division (76.8 ± 8.2 vs. 1.2 ± 1.1, P < 0.001) followed by tumor (69.8 ± 21.2 vs. 1.8 ± 1.6, P = 0.002). A significant proportion of these telemedicine visits have been for new patient visits, ranging from 12.9%–32.2% across the 4 divisions of neurosurgery, whereas no new patients were seen via telemedicine prior to the pandemic (P < 0.05).20
Telemedicine for Outpatient Care
There are a number of telemedicine software that enable for video communication with patients from the safety of their home. Our department has used the Teladoc Health (Teladoc Health, Purchase, Harrison, New York, USA) and the VidyoConnect (Vidyo Health, Rochelle Park, New Jersey, USA) telemedicine platforms, integrated within the EPIC electronic health records (Epic Systems Corporation, Verona, Wisconsin, USA). To maintain an efficient clinic schedule, we established a telemedicine environment at home that was comprised of a computer (desktop or laptop) with remote access to the hospital intranet to access the electronic health records and communicate with the patient and a second device (laptop or tablet) to communicate with the nursing staff in parallel. This set-up allows for a 360° communication between the neurosurgical team and the patient. Imaging was reviewed with the patient via the share-screen functionality of the telemedicine software. Nursing joins the physician-patient encounter when needed to assist with scheduling future appointments or imaging. Anytime technical issues are encountered, HIPAA-compliant smartphone applications such as Doximity (Doximity, San Francisco, California, USA) can be used to carry out the telemedicine visit.
Establishing an online outpatient practice allows for more flexible scheduling. Starting telemedicine visits early in the day (e.g., 6:30 AM) can be beneficial to accommodate patients who cannot miss work, as well as help avoid the network congestion noted later in the day when the rest of the hospital enterprise logs on to carry out their telemedicine visits. Furthermore, preferences on telemedicine scheduling varied among providers; some faculty performed telemedicine visits only on their clinic days, whereas others saw patients on their operative days, before or after cases, or even on the weekends if necessary.
Additionally, at our institution we have begun to incorporate both fellows and residents on telemedicine to see patients. Neurosurgery is also a select rotation in which medical students participate in telemedicine visits with attending, and this provides an educational opportunity for students to be able to practice history taking skills in a virtual setting. The educational opportunities for telemedicine are tremendous and make clinic exposure more accessible to trainees.
Inpatient Telemedicine Rounding
Telemedicine has also been beneficial in the inpatient setting as well. As neurosurgeons, we are often required to examine patients in a number of settings within a single day: operating room, emergency department, ICU, and clinic. To minimize the risk of viral exposure, we have utilized technologies such as the InTouch Health Robot (iRobot, Bedford, Massachusetts, USA) and Zoom (Zoom Video Communications, San Jose, California, USA) for remote inpatient rounding. More specifically, the health robot has been instrumental in remotely assessing high-risk patients in the ICU or the emergency department. It allows for audio and video conferencing with the patient and family while keeping the health care personnel needed to enter the patient room to a minimum. Additionally, a more affordable and easy-to-use option has been HIPAA-compliant video-conferencing software such as Zoom used via a tablet or a smartphone. Not only does this allow physician-patient communication, but it also seamlessly facilitates multidisciplinary meetings between our team, our colleagues from other services, family members and the patient in one online discussion.
Redistribution of Residents in a Pandemic Surge
One of the most unsettling components of COVID-19 is seeing subspecialty residents redeployed to any unit where help is needed. When considering where residents will be reassigned and distributed in different phases of the pandemic surge, it is important to consider the skill set of the neurosurgery residents and where they can be of most value. Neurosurgery residents also take pride in being some of the brightest and most efficient workers in the hospital. They are particularly facile in stressful situations, such as in the ICU setting.
Therefore it is prudent that in a pandemic, neurosurgery residents lend their service in a niche where they could put these skills to use. This could include working alongside other resident physicians to be part of a “line service” to place central and arterial lines in all COVID-19 patients throughout the ICUs in the hospital.11
Although no subspecialty department wishes to put their residents at unnecessary risk, in a pandemic situation, exposure to COVID-19 patients is somewhat unavoidable. The ACGME (Accreditation Council for Graduate Medical Education) has taken a clear stance and offers several guidelines for residents/fellows who require reassignment of clinical duties during this time.21 To keep resident physicians safe, it is important to provide them with educational materials to properly don and doff PPE, as well as mandatory in-person sessions with trained clinical staff.
At our institution, none of the neurosurgery residents developed symptoms concerning for COVID-19. Residents were instructed on symptom screening and twice-daily temperature checks if inadvertently exposed to a COVID-19-positive patient. Due to an outbreak at one of the facilities among nursing staff in June 2020, all neurosurgery residents were swabbed for COVID-19 around the time of the outbreak, and every resident had a negative result. Although this is certainly a unique circumstance, we do recommend that leadership of neurosurgical departments be prepared to handle a potential outbreak among faculty or resident physicians. This includes providing fast and efficient testing, which was done for all the residents at a central testing site on campus. Not only is this important to quarantine any team members who are asymptomatic carriers, but it also gives residents “peace of mind” in times when mental health is already at risk.
Preserving Residency Education During the COVID-19 Pandemic
Conference cancellations, travel restrictions, and limited in-person gatherings act as barriers to academic learning and compromise resident education. Because COVID-19 is an ongoing issue and surge in pandemic cases can lead to the suspension of nonemergent surgeries, our department has transitioned to recurrent didactic events using videoconference software (e.g., Zoom Video Communications). This includes weekly grand rounds, case conferences, and journal clubs led by neurosurgical faculty. Prior to each didactic event, review materials were sent out via email to ensure active participation and contribution of a lively discussion. To simplify participation, all didactic events were scheduled at the same times as preexisting programs and recurrent events had the identical log-in identifier from week to week.
It goes without saying that videoconference meetings and group discussions do not replace the training in the operating room. However, they keep the residents' engaged and improve their critical thinking and surgical planning in times of a reduced case volume. Future advancements could be made by the implementation of augmented reality platforms to improve anatomic knowledge and surgical skills. Finally, video conference meetings are also instrumental in future resident and fellow recruitment.22
Another cornerstone of resident and department camaraderie is the implementation of video meetings via Zoom twice a week, which is particularly useful when elective surgeries are placed on hold. These meetings include the residents, as well as the chairman and residency program director, to transparently discuss any new measures taken by administration. The meetings also serve to build team morale as personal interaction is naturally reduced when elective surgeries are placed on hold.
A limitation of our article may be the limited applicability to neurosurgical practice in developing countries.
Conclusions
The COVID-19 pandemic caused fundamental disruptions of neurosurgical practice. However, the instituted protocols proved to be efficient in providing a safe environment to continue to provide neurosurgical care to patients and help facilitate resident education. Unfortunately, the end is not yet in sight, but the lessons learned from this pandemic can be applied to a future airborne pandemic or a second wave for better damage control.
CRediT authorship contribution statement
Fadi Al Saiegh: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Nikolaos Mouchtouris: Formal analysis, Visualization, Investigation, Writing - review & editing. Omaditya Khanna: Visualization, Investigation, Writing - review & editing. Michael Baldassari: Formal analysis, Visualization, Investigation, Writing - review & editing. Thana Theofanis: Data curation, Writing - review & editing. Ritam Ghosh: Formal analysis, Writing - review & editing. Stavropoula Tjoumakaris: Data curation, Writing - review & editing. Michael Reid Gooch: Writing - review & editing. Nabeel Herial: Writing - review & editing. Hekmat Zarzour: Writing - review & editing. Victor Romo: Data curation, Writing - review & editing. Michael Mahla: Data curation, Writing - review & editing. Robert Rosenwasser: Writing - review & editing. Pascal Jabbour: Conceptualization, Methodology, Supervision, Writing - review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Al Saiegh F., Ghosh R., Leibold A., et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J Neurol Neurosurg Psychiatry. 2020;91:846–848. doi: 10.1136/jnnp-2020-323522. [DOI] [PubMed] [Google Scholar]
- 2.Belani P., Schefflein J., Kihira S., et al. COVID-19 is an independent risk factor for acute ischemic stroke. AJNR Am J Neuroradiol. 2020;41:1361–1364. doi: 10.3174/ajnr.A6650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta P., McAuley D.F., Brown M., et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sweid A., Hammoud B., Weinberg J.H., et al. Letter: thrombotic neurovascular disease in COVID-19 patients. Neurosurgery. 2020;87:E400–E406. doi: 10.1093/neuros/nyaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sweid A., Jabbour P., Tjoumakaris S. Letter to the Editor: incidence of acute ischemic stroke and rate of mechanical thrombectomy during the COVID-19 pandemic in a large tertiary care telemedicine network. World Neurosurg. 2020;140:491–492. doi: 10.1016/j.wneu.2020.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoelscher C., Sweid A., Ghosh R., et al. Cerebral deep venous thrombosis and COVID-19: case report [e-pub ahead of print] J Neurosurg. 2020:1–4. doi: 10.3171/2020.5.JNS201542. accessed November 11, 2020. [DOI] [PubMed] [Google Scholar]
- 7.Brindle M.E., Gawande A. Managing COVID-19 in surgical systems. Ann Surg. 2020;272:e1–e2. doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.(DGNC) GSoN https://www.dgnc.de/fileadmin/media/dgnc_homepage/publikationen/downloads/DGNC_BDNC_non-elective_surgical_interventions.pdf Available at:
- 9.Fontanella M.M., De Maria L., Zanin L., et al. Neurosurgical practice during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic: a worldwide survey. World Neurosurg. 2020;139:e818–e826. doi: 10.1016/j.wneu.2020.04.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fontanella M.M., Saraceno G., Lei T., et al. Neurosurgical activity during COVID-19 pandemic: an expert opinion from China, South Korea, Italy, United Stated of America, Colombia and United Kingdom. J Neurosurg Sci. 2020;64:383–388. doi: 10.23736/S0390-5616.20.04994-2. [DOI] [PubMed] [Google Scholar]
- 11.Theofanis T.N., Khanna O., Stefanelli A., et al. Letter: neurosurgery residency in the COVID-19 era: experiences and insights from Thomas Jefferson University Hospital, Philadelphia, Pennsylvania. Neurosurgery. 2020;87:E249. doi: 10.1093/neuros/nyaa211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burke J.F., Chan A.K., Mummaneni V., et al. Letter: the coronavirus disease 2019 global pandemic: a neurosurgical treatment algorithm. Neurosurgery. 2020;87:E50–E56. doi: 10.1093/neuros/nyaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhaskar S., Sharma D., Walker A.H., et al. Acute neurological care in the COVID-19 era: the pandemic health system resilience program (REPROGRAM) consortium pathway. Front Neurol. 2020;11:579. doi: 10.3389/fneur.2020.00579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klironomos S., Tzortzakakis A., Kits A., et al. Nervous system involvement in COVID-19: results from a retrospective consecutive neuroimaging cohort [e-pub ahead iof print] Radiology. 2020 doi: 10.1148/radiol.2020202791. accessed November 11, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spence J.D., de Freitas G.R., Pettigrew L.C., et al. Mechanisms of stroke in COVID-19. Cerebrovasc Dis. 2020;49:451–458. doi: 10.1159/000509581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma D., Rasmussen M., Han R., et al. Anesthetic management of endovascular treatment of acute ischemic stroke during COVID-19 pandemic: consensus statement from Society for Neuroscience in Anesthesiology & Critical Care (SNACC): endorsed by Society of Vascular & Interventional Neurology (SVIN), Society of NeuroInterventional Surgery (SNIS), Neurocritical Care Society (NCS), European Society of Minimally Invasive Neurological Therapy (ESMINT) and American Association of Neurological Surgeons (AANS) and Congress of Neurological Surgeons (CNS) cerebrovascular section. J Neurosurg Anesthesiol. 2020;32:193–201. doi: 10.1097/ANA.0000000000000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandey A.S., Ringer A.J., Rai A.T., et al. Minimizing SARS-CoV-2 exposure when performing surgical interventions during the COVID-19 pandemic. J Neurointerv Surg. 2020;12:643–647. doi: 10.1136/neurintsurg-2020-016161. [DOI] [PubMed] [Google Scholar]
- 18.Wang W., Xin C., Xiong Z., et al. Clinical characteristics and outcomes of 421 patients with coronavirus disease 2019 treated in a mobile cabin hospital. Chest. 2020;158:939–946. doi: 10.1016/j.chest.2020.05.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li J., Gao R., Wu G., et al. Clinical characteristics of emergency surgery patients infected with coronavirus disease 2019 (COVID-19) pneumonia in Wuhan, China. Surgery. 2020;168:398–403. doi: 10.1016/j.surg.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mouchtouris N., Lavergne P., Montenegro T.S., et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ACGME . 2020. Stage 3 pandemic emergency status guidance.https://acgme.org/Stage-3-Pandemic-Emergency-Status-Guidance Available at: [Google Scholar]
- 22.Al Saiegh F., Ghosh R., Stefanelli A., et al. Virtual residency training interviews in the age of COVID-19 and beyond. World Neurosurg. 2020;143:641–643. doi: 10.1016/j.wneu.2020.08.144. [DOI] [PMC free article] [PubMed] [Google Scholar]