Highlights
-
•
In situ pulmonary thrombosis may exist in COVID-19 pneumonia patients with the feature of peripheral distribution.
-
•
Some thrombi located just within the consolidation lesions of the infected lungs, likely due to active local inflammation.
-
•
Some thrombi located in non-consolidation area, likely due to hypercoagulability caused by systemic inflammation.
-
•
We hypothesize different phenotypes of in situ thrombosis may exist and need different intensity of anticoagulant therapy.
Dear Editor,
We read with great interest the recent article by L.F. van Dam et al. entitled “Clinical and computed tomography characteristics of COVID-19 associated acute pulmonary embolism: A different phenotype of thrombotic disease?” [1]. They reported the pulmonary emboli in COVID-19 affected patients are more likely to be located in the peripheral lung segments and are less extensive compared to those in patients without COVID-19 pneumonia and theorized the existence of in situ pulmonary thrombosis in patients with COVID-19 pneumonia.
Several researchers have proposed this concept [2,3] based on the reported absence of deep venous thrombosis (DVT) in the majority of patients with pulmonary embolism (PE), the higher incidence of PE but not DVT in patients with COVID-19 compared to those without COVID-19 [[4], [5], [6]], and pathologic findings of thrombosis within the pulmonary arteries in the absence of DVT in autopsy studies [7]. However, the clinical and radiological characteristics of in situ pulmonary thrombosis have not been analyzed in patients in whom DVT has been excluded.
The findings reported by L.F. van Dam et al. did reveal some different computed tomography manifestations between the PE in the patients with COVID-19 pneumonia and the ones without, which supported the possibility of the presence of in situ pulmonary thrombosis. However, they did not systematically screen for DVT in their study population. If the study could prove a higher incidence of PE without DVT in the patients with COVID-19 pneumonia, their speculation about in situ pulmonary thrombosis would be more convincing. This study also found that all thrombotic lesions in patients with COVID-19 pneumonia were in lung parenchyma affected by COVID-19. However, more detailed radiologic information about the relationship between the location of thrombotic pulmonary arteries and COVID-19 affected lung lesions was not provided.
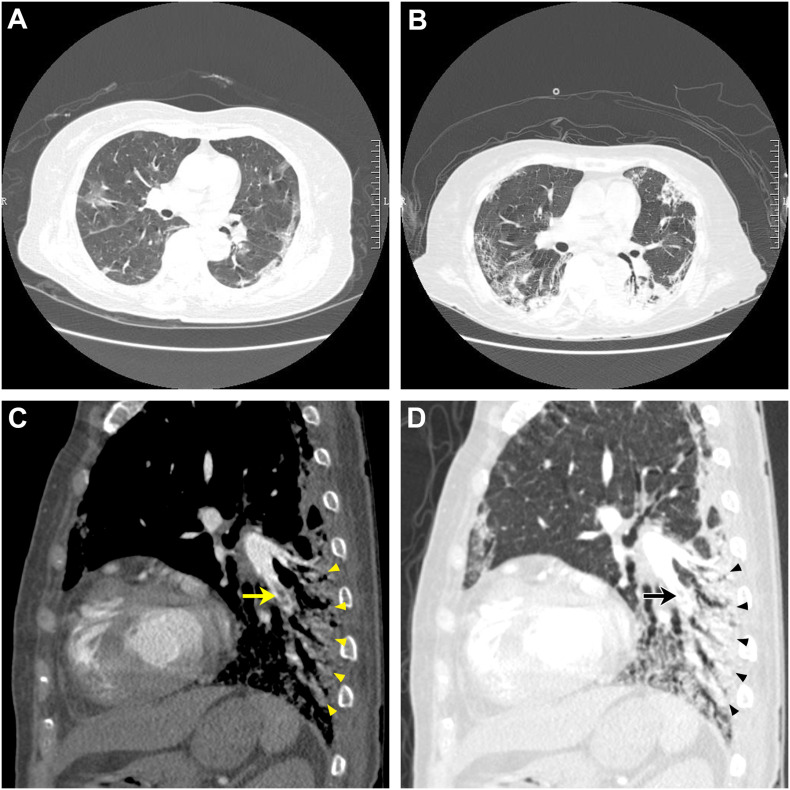
We are able to provide details about four intubated patients with severe COVID-19 pneumonia who were diagnosed with PE by computed tomography pulmonary angiography (CTPA) and who had negative lower extremity venous duplex ultrasounds. All of them had received prophylactic anticoagulation treatment before performing CTPA. Similar to the findings of L.F. van Dam et al., all the thrombotic lesions in these patients were segmental or subsegmental. However, unlike van dam and colleagues, who reported thrombotic arteries around which there was no apparent consolidation, we found some clogged segmental arteries located just within the consolidation lesions of the infected lungs (Fig. 1 ). We speculate this close relationship between the location of thrombus and consolidation may be an additional characteristic of in situ pulmonary thrombosis in patients with severe COVID-19 pneumonia. The thrombi may form in the vessels around which the local inflammatory responses of infected lung lesions are active or severe, with associated pulmonary endothelial damage due to inflammatory infiltration and stimulation resulting from the proliferation of lung parenchyma inflammation. We noticed that our patients also had segmental or subsegmental thrombi located in non-consolidation areas. The formation of these thrombi may due to hypercoagulability caused by systemic inflammation since all of the four patients had a significantly higher level of D-dimer. Therefore, we hypothesize that different phenotypes of in situ thrombosis may exist in patients with COVID-19 pneumonia.
Fig. 1.
Computed tomography (CT) and computed tomography pulmonary angiography (CTPA) of a 69 years old female patient with COVID-19 pneumonia: Panel A: Axial unenhanced chest CT scan at admission showed bilateral peripheral ground-glass opacities; Panel B: Axial unenhanced chest CT scan obtained at the same time of CTPA revealed progression of ground-glass opacities with fibrosis and consolidation; Panel C and D: CTPA scan demonstrated segmental filling defects in the left pulmonary artery (arrows), which was just within the consolidation lesions of the infected lungs (triangles).
If confirmed, what may these findings suggest? First, we should not simply exclude pulmonary thrombosis when the result of DVT screening is negative in patients with COVID-19 pneumonia, especially in those with severe pneumonia admitted to the intensive care unit. In situ pulmonary thrombosis needs to be considered and CTPA undertaken, particularly in patients with the following features: clinical deterioration, markedly elevated D-dimer level, and extensive lung consolidation. Secondly, it is interesting to hypothesize that the different pathogenic mechanisms of in situ pulmonary thrombosis may necessitate different treatment recommendations. If the thrombi are mainly located in areas where the lung parenchyma is not affected, therapeutic anticoagulation may be more appropriate since these thrombi are the reflection of systemic hypercoagulability; whereas if the thrombi mainly form in vessels within the areas of pulmonary consolidation, a prophylactic dose may be sufficient if combined with potent anti-inflammatory treatment because of the causative role of local inflammation in the pathogenesis of thrombosis.
Further studies with larger samples are needed to confirm the extent of in situ pulmonary thrombosis in patients with COVID-19 pneumonia and to clarify possible phenotypes. Basic research studies are also needed to explore the pathophysiological mechanisms and causal relationship between COVID-19 and PE or in situ pulmonary thrombosis. Both lines of investigation will be key to developing rational anticoagulant treatment for pulmonary thromboembolic disease in patients with COVID-19 pneumonia.
Declaration of competing interest
The authors have no conflict of interest to declare.
References
- 1.van Dam L.F., Kroft L.J.M., van der Wal L.I., Cannegieter S.C., Eikenboom J., de Jonge E., Huisman M.V., Klok F.A. Clinical and computed tomography characteristics of COVID-19 associated acute pulmonary embolism: a different phenotype of thrombotic disease? Thromb. Res. 2020;193:86–89. doi: 10.1016/j.thromres.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gabrielli M., Lamendola P., Esperide A., Valletta F., Franceschi F. COVID-19 and thrombotic complications: pulmonary thrombosis rather than embolism? Thromb. Res. 2020;193:98. doi: 10.1016/j.thromres.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Price L.C., McCabe C., Garfield B., Wort S.J. Thrombosis and COVID-19 pneumonia: the clot thickens! Eur. Respir. J. 2020;56(1):2001608. doi: 10.1183/13993003.01608-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Helms J., Tacquard C., Severac F., Leonard-Lorant I., Ohana M., Delabranche X., Merdji H., Clere-Jehl R., Schenck M., Fagot Gandet F., Fafi-Kremer S., Castelain V., Schneider F., Grunebaum L., Anglés-Cano E., Sattler L., Mertes P.M., Meziani F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lodigiani C., Iapichino G., Carenzo L., Cecconi M., Ferrazzi P., Sebastian T., Kucher N., Studt J.D., Sacco C., Alexia B., Sandri M.T., Barco S. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thrombosis Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demelo-Rodríguez P., Cervilla-Muñoz E., Ordieres-Ortega L., Parra-Virto A., Toledano-Macías M., Toledo-Samaniego N., García-García A., García-Fernández-Bravo I., Ji Z., de Miguel-Diez J., Álvarez-Sala-Walther L.A., Del-Toro-Cervera J., Galeano-Valle F. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thrombosis Res. 2020;192:23–26. doi: 10.1016/j.thromres.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lax S.F., Skok K., Zechner P., Kessler H.H., Kaufmann N., Koelblinger C., Vander K., Bargfrieder U., Trauner M. Pulmonary Arterial Thrombosis in COVID-19 With Fatal Outcome : Results From a Prospective, Single-Center, Clinicopathologic Case Series. Ann Intern Med. 2020;173(5):350–361. doi: 10.7326/M20-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]