Abstract
Purpose
The proportion of geriatric trauma patients (GTPs) (age ≥ 65 years old) with chest wall injury undergoing surgical stabilization of rib fractures (SSRF) nationally is unknown. We hypothesize a growing trend of GTPs undergoing SSRF, and sought to evaluate risk of respiratory complications and mortality for GTPs compared to younger adults (18–64 years old) undergoing SSRF.
Methods
The Trauma Quality Improvement Program (2010–2016) was queried for patients with rib fracture(s) who underwent SSRF. GTPs were compared to younger adults. A multivariable logistic regression analysis was performed.
Results
From 21,517 patients undergoing SSRF, 3,001 (16.2%) were GTPs. Of all patients undergoing SSRF in 2010, 10.6% occurred on GTPs increasing to 17.9% in 2016 (p < 0.001) with a geometric-mean-annual increase of 11.5%. GTPs had a lower median injury severity score (18 vs. 22, p < 0.001), but had a higher rate of mortality (4.7% vs. 1.2%, p < 0.001). After controlling for covariates, GTPs had an increased associated risk of mortality (OR 4.80, CI 3.62–6.36, p < 0.001). On a separate multivariate analysis for all trauma patients with isolated chest Abbreviated Injury Scale 3, GTPs were associated with a similar four-fold risk of mortality (OR 4.21, CI 1.98–6.32, p < 0.001).
Conclusion
Spanning 7 years of data, the proportion of GTPs undergoing SSRF increased by over 7%. Although GTPs undergoing SSRF had lesser injuries, their risk of mortality was four times higher than other adult trauma patients undergoing SSRF, which was similar to their increased background risk of mortality. Ultimately, SSRF in GTPs should be considered on an individualized basis with careful attention to risk–benefit ratio.
Electronic supplementary material
The online version of this article (10.1007/s00068-020-01526-7) contains supplementary material, which is available to authorized users.
Keywords: Surgical stabilization of rib fractures, Geriatric trauma patients, Rib fractures, Flail chest
Introduction
Thoracic trauma is a major contributor to trauma mortality, and accounts for 20–25% of trauma deaths overall [1]. Rib fractures are commonly seen after blunt chest trauma, and are found in up to 10% of all trauma patients, and up to 30% of thoracic trauma patients [2]. Rib fractures are often associated with pulmonary contusion, pneumothorax, hemothorax, and blunt cardiac injury, with increasing numbers of rib fractures associated with worsening morbidity and mortality in a “dose-dependent” manner [3, 4]. Flail chest physiology, significant chest wall instability, or pain refractory to pain management can all lead to pulmonary complications or respiratory failure requiring ventilator support. Surgical stabilization of rib fractures (SSRF) has been shown to improve pulmonary outcomes in select patients with chest wall injury [5–11].
SSRF began in the 1970s, initially to address paradoxical movement of the chest wall in thoracic injury. Paris et al. found that SSRF could avoid or reduce the use of mechanical ventilation [5]. Since that time, randomized prospective studies have demonstrated SSRF for flail chest can minimize ventilation requirements and intensive care unit stay [6–9]. As well, multiple meta-analyses have found improved outcomes for patients undergoing SSRF, particularly for flail chest, citing reduced pneumonia, chest deformity, intensive care unit (ICU)/length of stay (LOS) days, decreased need for tracheostomy, and decreased mortality [10, 11]. Thus, the indications for SSRF have expanded to include flail chest requiring mechanical ventilation, symptomatic non-union, severe displacement found during a thoracotomy for another reason, ≥ 3 ribs flail not requiring mechanical ventilation, ≥ 3 ribs with severely displaced fractures defined as bi-cortical displacement, or ≥ 3 rib fractures with mild to moderate displacement and less than 50% of expected forced vital capacity despite adequate pain management [4].
With the expanded criteria for SSRF, use of SSRF has increased. Studies have continued to show an overall mortality benefit. However, rib fractures within GTP have not been well studied on a national level. We wanted to evaluate the trends of GTPs undergoing SSRF, and concomitantly, evaluate the risk of respiratory complications (unplanned intubation, acute respiratory distress syndrome, and pneumonia) and mortality for GTPs compared to younger adults (18–64 years old) undergoing SSRF. We hypothesize a growing trend of GTPs undergoing SSRF, with higher risk of mortality in the GTP group compared to the non-geriatric trauma group (NGTP, younger adults aged 18–64).
Methods
We performed a retrospective analysis of the Trauma Quality Improvement Program (TQIP) over a seven-year period from 2010 to 2016 to identify trauma patients with rib fractures who underwent SSRF. Two groups were compared: GTPs (age ≥ 65 years old) and non-GTPs (NGTPs) (age 18–64 years old). All patients meeting the above criteria with complete information were included. The primary outcome was in-hospital mortality. Given that this was a retrospective analysis on a national database without patient identifiers, this study did not require informed or ethics consent and was exempt from Institutional Review Board review.
Patient demographic information was collected as well as pre-hospital comorbidities including congestive heart failure (CHF), cerebrovascular accident (CVA), end-stage renal disease (ESRD), and chronic obstructive pulmonary disease (COPD). Initial trauma injury profile, including Injury Severity Score (ISS) and Abbreviated Injury Scale (AIS) score was also collected. Secondary outcomes evaluated included length of stay (LOS), intensive care unit (ICU) days, as well as in-hospital complications, such as acute kidney injury (AKI), acute respiratory distress syndrome (ARDS), deep vein thrombosis (DVT), myocardial infarction (MI), and pulmonary embolism (PE). A complete list of variables is included in Appendix A. The only variable in the model with missing data was Glasgow Coma Scale (GCS); this information was missing for 4.9% of patients, and these patients were excluded from our regression analysis.
Descriptive statistics were performed for all variables. A Mann–Whitney U test was used to compare continuous variables and Chi-square test was used to compare categorical variables. Categorical data were reported as percentages, continuous data were reported as medians with interquartile range or means with standard deviation. The magnitude of the association between predictor variables and mortality was measured using a univariable logistic regression model. The variables were chosen based on a review of literature [10–16]. Covariates were then controlled for using a hierarchical multivariable logistic regression model. Two separate multivariable regression models were completed. One multivariable logistic regression analysis was completed for risk of mortality of all adult trauma patients with rib fractures undergoing SSRF. A second multivariable logistic regression analysis was completed for risk of mortality of all adult trauma patients with rib fractures and chest AIS of 3. We chose a chest AIS of 3 with no other injuries as we wanted to compare similarly injured GTPs to NGTPs with rib fracture injury that may benefit from SSRF. These were reported with an odds ratio (OR) and a 95% confidence intervals (CI). All p values were two-sided, with a statistical significance level of < 0.05. All statistical analyses were performed with IBM SPSS Statistics for Windows, Version 24 (Armonk, NY: IBM Corp).
Results
Patient demographics and national trends
From 21,517 trauma patients with rib fractures undergoing SSRF, 18,516 (86.1%) were NGTPs and 3001 (13.9%) were GTPs. There was a greater percentage of males for NGTPs (72.8% vs. 65.1%, p < 0.001). Median ISS was also greater for NGTPs (22 vs. 18, p < 0.001). NGTPs were also more likely to be alcohol or drug screen positive (alcohol: 23.3% vs. 6.5%, p < 0.001, drug: 27.5% vs. 15.0%, p < 0.001). However, NGTPs had a lower medium number of rib fractures (4 vs. 5, p < 0.001). On the other hand, GTPs had a greater rate of most comorbidities, including CHF (4.0% vs. 0.6%, p < 0.001), CVA (3.0% vs. 0.5%, p < 0.001), ESRD (1.2% vs. 0.3%, p < 0.001), DM (24.1% vs. 8.1%, p < 0.001), hypertension (56.8% vs. 18.9%), and COPD (10.7% vs. 5.4%, p < 0.001) (Table 1).
Table 1.
Demographics of adult patients with rib fractures undergoing rib fixation
| Characteristic | Age < 65 | Age ≥ 65 | p value |
|---|---|---|---|
| (n = 18,516) | (n = 3001) | ||
| Age, year, median (IQR) | 44 (31, 53) | 71 (67, 76) | < 0.001 |
| Male, n (%) | 13,479 (72.8%) | 1952 (65.1%) | < 0.001 |
| ISS, median (IQR) | 22 (14, 29) | 18 (14, 25) | < 0.001 |
| Teaching university, n (%) | 11,354 (61.3%) | 1736 (57.8%) | < 0.001 |
| Vitals on admission, median (IQR) | |||
| Systolic blood pressure | 127 (110, 143) | 131 (111, 150) | < 0.001 |
| Respiratory rate | 20 (16, 22) | 19 (16, 22) | < 0.001 |
| Pulse | 97 (83, 114) | 87 (75, 101) | < 0.001 |
| Glasgow coma scale score | 15 (14, 15) | 15 (15, 15) | 0.877 |
| Alcohol screen positive, n (%) | 4086 (23.3%) | 184 (6.5%) | < 0.001 |
| Drug screen positive, n (%) | 4572 (27.5%) | 412 (15.0%) | < 0.001 |
| Number of rib fractures, median (IQR) | 4 (2, 7) | 5 (3, 8) | < 0.001 |
| Comorbidities, n (%) | |||
| Congestive heart failure | 112 (0.6%) | 119 (4.0%) | < 0.001 |
| Cerebrovascular accident | 99 (0.5%) | 89 (3.0%) | < 0.001 |
| End-stage renal disease | 55 (0.3%) | 37 (1.2%) | < 0.001 |
| Diabetes | 1501 (8.1%) | 723 (24.1%) | < 0.001 |
| Hypertension | 3495 (18.9%) | 1705 (56.8%) | < 0.001 |
| COPD | 991 (5.4%) | 322 (10.7%) | < 0.001 |
| Smoker | 4671 (25.2%) | 307 (10.2%) | < 0.001 |
| Blunt mechanism, n (%) | 18,350 (99.5%) | 2970 (99.6%) | 0.418 |
| AIS (grade > 3), n (%) | |||
| Head | 2445 (13.2%) | 357 (11.9%) | 0.048 |
| Abdomen | 1510 (8.2%) | 97 (3.2%) | < 0.001 |
| Spine | 367 (2.0%) | 36 (1.2%) | 0.003 |
| Upper extremity | 12 (0.1%) | 3 (0.1%) | 0.498 |
| Lower extremity | 1442 (7.8%) | 172 (5.7%) | < 0.001 |
ISS injury severity score, IQR interquartile range, COPD chronic obstructive pulmonary disease
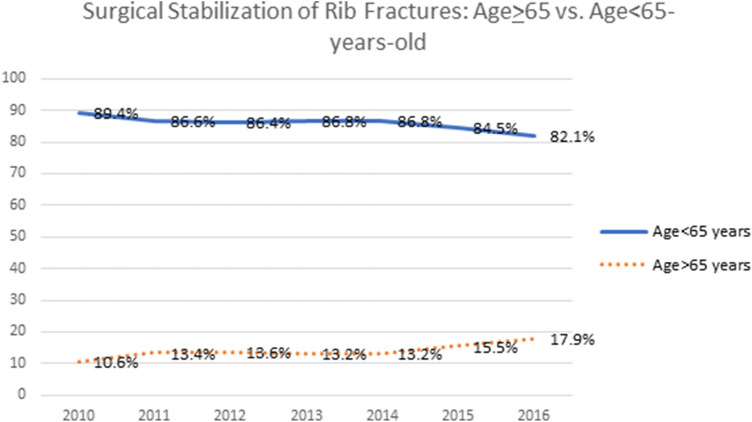
From 2010 to 2016, there was an increase in the proportion of SSRF in GTPs, with 10.6% of SSRF completed on GTPs in 2010, increasing to 17.9% of SSRF completed on GTPs in 2016 (Fig. 1).
Fig. 1.
Surgical stabilization of rib fractures: Age ≥ 65 vs. Age < 65-years-old
Mortality and other clinical outcomes of trauma patients with rib fractures undergoing SSRF
The rate of mortality was greater in GTPs with rib fractures undergoing SSRF than in NGTPs (4.7% vs. 1.2%, p < 0.001). GTPs also had a greater median LOS, ICU days, and ventilator days (LOS: 13 vs. 12 days, p < 0.001; ICU: 7 vs. 6 days, p < 0.001; ventilator: 8 vs. 7, p < 0.001) (Table 2).
Table 2.
Clinical outcomes in adult patients with rib fractures undergoing rib fixation
| Outcome | Age < 65 | Age ≥ 65 | p value |
|---|---|---|---|
| (n = 18,516) | (n = 3001) | ||
| LOS, days, median (IQR) | 12 (7, 20) | 13 (9, 20) | < 0.001 |
| ICU, days, median (IQR) | 6 (3, 13) | 7 (4, 15) | < 0.001 |
| Ventilator, days, median (IQR) | 7 (3, 13) | 8 (3, 15) | < 0.001 |
| Complications, n (%) | |||
| Acute kidney injury | 373 (2.0%) | 109 (3.6%) | < 0.001 |
| Acute respiratory distress syndrome | 662 (3.7%) | 119 (4.0%) | 0.289 |
| Deep vein thrombosis | 1027 (5.5%) | 227 (7.6%) | < 0.001 |
| Myocardial infarction | 49 (0.3%) | 49 (1.6%) | < 0.001 |
| Pulmonary embolism | 417 (2.3%) | 61 (2.0%) | 0.449 |
| Unplanned intubation | 699 (3.8%) | 229 (7.6%) | < 0.001 |
| Unplanned ICU admission | 491 (2.7%) | 139 (4.6%) | < 0.001 |
| Pneumonia | 2066 (11.2%) | 367 (12.2%) | 0.086 |
| Disposition, n (%) | < 0.001 | ||
| Home | 9633 (53.0%) | 652 (22.9%) | |
| Long term acute care | 6477 (35.6%) | 1293 (45.3%) | |
| Skilled nursing facility | 2052 (11.3%) | 892 (31.3%) | |
| Mortality, n (%) | 213 (1.2%) | 140 (4.7%) | < 0.001 |
LOS length of stay, IQR interquartile range, ICU intensive care unit
Overall, when compared to NGTPs, GTPs had an increased rate of in-hospital complications including AKI (3.6%vs. 2.0%, p < 0.001), DVT (7.6% vs. 5.5%, p < 0.001), MI (1.6% vs. 0.3%, p < 0.001), unplanned intubations (7.6% vs. 3.8%, p < 0.001), and unplanned ICU admissions (4.6% vs. 2.7%, p < 0.001). There was, however, no difference in the rate of ARDS (4.0% vs. 3.7%, p = 0.29) or pneumonia (12.2% vs. 11.2%, p = 0.086) between the cohorts.
Risk of mortality in trauma patients with rib fractures undergoing SSRF
After adjusting for covariates, the most significant risk factor for mortality was age ≥ 65 years old (OR = 4.80, CI 3.62–6.36, p < 0.001). This was followed by ESRD (OR 3.97, CI 1.80–8.74, p = 0.001), diabetes (OR 1.79, CI 1.23–2.32, p = 0.001), and COPD (OR 1.64, CI 1.11–2.43, p = 0.013). For each additional point of ISS, there was an increased risk of mortality (OR 1.04, CI 1.02–1.05, p < 0.001) (Table 3).
Table 3.
Multivariable logistic regression analysis for risk of mortality in adult patients with rib fractures undergoing rib fixation
| Risk factor | OR | CI | p value |
|---|---|---|---|
| Age ≥ 65 vs. Age < 65 years-old | 4.80 | 3.62–6.36 | < 0.001 |
| Systolic blood pressure | 0.99 | 0.98–0.99 | < 0.001 |
| Injury severity score | 1.04 | 1.02–1.05 | < 0.001 |
| Respiratory rate | 1.01 | 0.99–1.02 | 0.371 |
| Pulse | 1.01 | 1.00–1.01 | 0.063 |
| Glasgow coma scale | 0.92 | 0.89–0.95 | < 0.001 |
| AIS (grade > 3) | |||
| Head | 1.22 | 0.88–1.67 | 0.226 |
| Abdomen | 1.19 | 0.80–1.75 | 0.394 |
| Spine | 1.17 | 0.60–2.28 | 0.646 |
| Upper extremity | 0.98 | 0.78–1.23 | 0.878 |
| Lower extremity | 1.28 | 0.88–1.86 | 0.198 |
| Comorbidities | |||
| Congestive heart failure | 1.11 | 0.52–2.36 | 0.790 |
| Cerebrovascular accident | 0.87 | 0.34–2.20 | 0.760 |
| End-stage renal disease | 3.97 | 1.80–8.74 | 0.001 |
| Diabetes | 1.79 | 1.23–2.32 | 0.001 |
| Hypertension | 1.28 | 0.86–1.70 | 0.093 |
| COPD | 1.64 | 1.11–2.43 | 0.013 |
| Smoker | 0.76 | 0.54–1.06 | 0.108 |
AIS abbreviated injury scale, COPD Chronic Obstructive Pulmonary Disease
When evaluating the risk of mortality in adult trauma patients with a chest AIS of 3, age ≥ 65 years old was associated with an increased risk of mortality (OR 4.21, CI 1.98–6.32, p < 0.001) (Table 4).
Table 4.
Multivariable logistic regression analysis for risk of mortality in adult patients with isolated chest AIS = 3
| Risk factor | OR | CI | p value |
|---|---|---|---|
| Age ≥ 65 vs. Age < 65 years-old | 4.21 | 1.98–6.32 | < 0.001 |
Discussion
Our large national analysis, spanning 7 years of TQIP data, found an increase in the number of GTPs undergoing SSRF over time. When comparing GTPs to NGTPs, despite a lower ISS, there were more in-hospital complications, and ultimately an increased rate of mortality for GTPs. After adjusting for age, vitals, ISS, and comorbidities, GTPs undergoing SSRF were found to have an over four-fold increased associated risk of mortality, when compared to NGTPs undergoing SSRF. However, when comparing mortality risk between GTPs and NGTPs with a chest AIS of 3, GTPs were found to also have a four-fold increased associated risk of mortality. Given that the risk of mortality is the same between the two models, we would offer that SSRF does not add any additional risk of mortality.
As the literature continues to underscore the mortality benefit for SSRF, the use of SSRF has increased over time, particularly for GTPs [12]. In support of this, we found a greater than 7% increase from 2010 to 2016 in the use of SSRF for GTPs. Although we are the first study to show this national trend of SSRF in GTPs, other studies have provided data to support a growing interest in SSRF over time as the number of publications on SSRF has nearly increased tenfold over the past decade [4]. Likewise, SSRF has gained a significant boost from the introduction of dedicated new equipment and materials, with more surgeons becoming comfortable with the operative technique [17]. However, in Mullens et al.’s retrospective study using the Pennsylvania Trauma System Foundation database, only 57 patients underwent rib fixation out of 12,910 patients with multiple rib fractures in 2016–2017 [18], showing that regional trends still persist. Future research is needed to clarify whether this increase is related to a nation-wide increase in rate of SSRF in GTPs or simply increased volume at high-volume centers.
Multiple studies have shown that elderly patients in general have worse surgical or trauma outcomes, with higher rates of in-hospital complications and mortality. In Bulger et al.’s retrospective study comparing 277 GTPs to NGTPs, they found GTPs to have increased ventilator days, LOS, pneumonia, and a higher rate of mortality [13]. In support of this, we found that GTPs in general had a lower ISS, but had an increased rate of in-hospital complications, including nearly double the rate of AKI, nearly a five-fold rate of MI, and an almost 50% increase in rate of DVT. Furthermore, there was also a nearly four-fold increased rate of mortality. Although the GTP group had increased comorbidities, another likely cause is due to frailty, a decreased ability of the elderly patient to deal with stressors [19]. This decreased physiologic reserve, from less efficient adaptive and homeostatic mechanisms, likely contributes to an increased background rate of morbidity and mortality [20]. This is seen in Hashmi et al. systematic review and meta-analysis on GTPs, GTPs had a higher overall mortality rate than adult trauma patients; furthermore, patients older than 74 had a higher risk for mortality than the younger geriatric group [21].
Thus, even after controlling for multiple covariates, GTPs still have an increased risk of mortality. In a single-center retrospective study on rib fracture patients, Bergeron et al. found that GTPs had a lower ISS, however, a five-fold increased risk of mortality [22]. Furthermore, in our study, after controlling for age, ISS, vitals, and comorbidity, we found that GTPs undergoing SSRF still had an increased (greater than four-fold) associated risk of mortality when compared to NGTPs.
However, we wanted to clarify whether this increased risk of mortality was associated with SSRF rather than simply an increased risk of mortality from rib fracture alone. As we found that GTPs undergoing SSRF had a greater than four-fold risk of mortality in comparison to NGTPs, we ran a separate multivariate analysis comparing GTPs and NGTPs with chest AIS of 3 and no other injuries, and found that GTPs had a background four-fold risk of mortality than NGTPs. Given that there was a similar risk of mortality, we would offer than SSRF does not add significant risk of mortality to the GTP group. This is in line with an institutional experience by Fitzgerald et al. who first reported 23 GTPs who underwent SSRF, without any pneumonia or deaths within the operative group [14]. They went on to study 34 more GTPs who underwent SSRF, and also had no infections or deaths over a three-year span [20]. Although these were not compared to nonoperative controls, the rate of infection or death was significantly lower than expected from historic controls, and in the right patient, SSRF at least does not confer additional risk of mortality.
There are limitations to this study, including those inherent to a retrospective database study, such as missing data, input error, misclassification, and reporting bias. In addition, pertinent missing variables from this database include details of the SSRF operation, such as what prompted the decision to operate (flail chest or bi-cortical deformity), operative time, surgical service (trauma vs. orthopedic surgery vs. thoracic surgery) performing the operation, as well as timing to surgery. We are also missing data regarding withdrawal of care, time to death, and cause of death. Blood product transfusion data, chest tube insertion rate, empyema, and retained hemothorax were not available. As well, data regarding thoracic epidural catheter use, used stabilization systems, and incidence of flail chest were absent. Need for other surgery and incidence of video-assisted thoracoscopic surgery were also unavailable. Finally, as a retrospective study, we are unable to make conclusions regarding cause and effect.
Conclusion
From 2010 to 2016, the proportion of GTPs undergoing SSRF increased by over 7%. Although GTPs undergoing SSRF had lesser injuries, their risk of mortality was four times higher than other adult trauma patients undergoing SSRF, which was similar to their increased background risk of mortality found with a chest AIS of 3. Ultimately, SSRF in GTPs should be considered on an individualized basis with careful attention to risk–benefit ratio.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
All authors made a substantial contribution to this work. WD, AG, and SS were involved in idea conceptualization, data curation, formal analysis, and writing and review. JN, CF, AC, MD, and ML were involved in reviewing and editing of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Code availability
Not applicable.
Compliance with ethical standards
Conflicts of interest
The authors report no conflicts of interest, financial or otherwise.
Availability of data and material
Data was obtained from a national database without patient identifiers, Trauma Quality Improvement Program (2010–2016).
References
- 1.Ekpe E, Eyo C. Determinants of mortality in chest trauma patients. Niger J Surg. 2014;20(1):30–34. doi: 10.4103/1117-6806.127107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edgecombe L, Angus LD. Thoracic Trauma. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK534843. (Accessed 15 Mar 20). [PubMed]
- 3.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37(6):975–979. doi: 10.1097/00005373-199412000-00018. [DOI] [PubMed] [Google Scholar]
- 4.De Moya M, Nirula R, Biffl W. Rib fixation: who, what, when? Trauma Surg Acute Care Open. 2017;2:7. doi: 10.1136/tsaco-2016-000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paris F, Tarazona V, Blasco E, Canto A, Casillas M, Pastor J, Paris M, Montero R. Surgical stabilization of traumatic flail chest. Thorax. 1975;30:521–527. doi: 10.1136/thx.30.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52(4):727–732. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Int Cardio Thorac Surg. 2005;4(6):583–587. doi: 10.1510/icvts.2005.111807. [DOI] [PubMed] [Google Scholar]
- 8.Marasco S, Davies A, Cooper J, Varma D, Bennett V, Nevill R, Lee G, Bailey M, Fitzgerald M. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216(5):924–932. doi: 10.1016/j.jamcollsurg.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 9.Wu M, Yang Y, Gao Z, Zhao T, He W. Which is better to multiple rib fractures, surgical treatment or conservative treatment? Int J Clin Exp Med. 2015;8(5):7930–7936. [PMC free article] [PubMed] [Google Scholar]
- 10.Slobogean G, MacPherson C, Sun T, Pelletier M, Hameed SM. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg. 2013;2016(2):302–311. doi: 10.1016/j.jamcollsurg.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 11.Coughlin T, Ng J, Rollins K, Forward D, Ollivere B. Management of rib fractures in traumatic flail chest: a meta-analysis of randomized controlled trials. Bone Joint. 2016;98(8):1119. doi: 10.1302/0301-620X.98B8.37282. [DOI] [PubMed] [Google Scholar]
- 12.Kane E, Jeremitsky E, Bittner K, Kartiko S, Doben A. Surgical stabilization of rib fractures: a single institution experience. J Am Coll Surg. 2018;226(6):961–966. doi: 10.1016/j.jamcollsurg.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Bulger E, Arneson M, Mock C, Jurkovich G. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–1046. doi: 10.1097/00005373-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Fitzgerald M, Ashley D, Abukhdeir H, Christie DB., 3rd Rib fracture fixation in the 65 years and older population: a paradigm shift in management strategy at a Level I trauma center. J Trauma Acute Care Surg. 2017;82(3):524–527. doi: 10.1097/TA.0000000000001330. [DOI] [PubMed] [Google Scholar]
- 15.Lien Y, Chen C, Lin HC. Risk factors for 24-hour mortality after traumatic rib fractures owing to motor vehicle accidents: a nationwide population-based study. Ann Thorac Surg. 2009;88(4):1124–1130. doi: 10.1016/j.athoracsur.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Barnea Y, Kashtan H, Skornick Y, Werbin N. Isolated rib fractures in elderly patients: mortality and morbidity. Can J Surg. 2002;45(1):43–46. [PMC free article] [PubMed] [Google Scholar]
- 17.Bemelman M, de Kruijf M, van Baal M, Luke L. Rib fractures: to fix or not to fix? An evidence-based algorithm. Korean J Thorac Cardiovasc Surg. 2017;50(4):229–234. doi: 10.5090/kjtcs.2017.50.4.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mullens C, Seamon M, Shiroff A, Cannon J, Kaplan L, Pascual J, Holena D, Martin N. A statewide assessment of rib fixation patterns reveals missed opportunities. J Surg Res. 2019;244:205–211. doi: 10.1016/j.jss.2019.06.048. [DOI] [PubMed] [Google Scholar]
- 19.Mors K, Wagner N, Sturm R, Stormann P, Vollrath J, Marzi I, Relja B. Enhanced pro-inflammatory response and higher mortality rates in geriatric trauma patients. Eur J Trauma Emerg Surg. 2019;22:19–34. doi: 10.1007/s00068-019-01284-1. [DOI] [PubMed] [Google Scholar]
- 20.Christie B, Nowack T, Drahos A, Ashley D. Geriatric chest wall injury: is it time for a new sense of urgency? J Thorac Dis. 2019;11(8):S1029–S1033. doi: 10.21037/jtd.2018.12.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashmi A, Ibrahim-Zada I, Rhee P, Aziz H, Fain M, Friese RS, Joseph B. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76(3):894–901. doi: 10.1097/TA.0b013e3182ab0763. [DOI] [PubMed] [Google Scholar]
- 22.Bergeron E, Lavoie A, Clas D, Moore L, Ratte S, Tetreault S, Lemaire J, Martin M. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54(3):478–485. doi: 10.1097/01.TA.0000037095.83469.4C. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.