Abstract
Nitrotyrosine, a structural analogue of tyrosine, is present in cells in pathological conditions and is incorporated into tubulin to form tubulin tyrosine nitration, which disrupts the normal function of microtubules. There is limited research on the functional aspects of tubulin tyrosine nitration in different types of tumor. In the present study, the effect of tubulin tyrosine nitration and tubulin tyrosine ligase like 12 (TTLL12) on the proliferation of SCC-25 cells was investigated. TTLL12-overexpressing cell lines were constructed and used to assess the effect of tubulin tyrosine nitration and TTLL12 on the proliferation of SCC-25 cells via western blotting, immunofluorescent and MTT assays. An TTLL12-stably overexpressing SCC-25 cell line and the enzyme-linked immunosorbent assay were used to establish a novel experiment in vitro for screening anticancer drugs targeting tubulin tyrosine nitration by assessing its sensitivity, specificity and repeatability, and using it to find an effective drug. The results demonstrated that the proliferative rate of the control cells was notably inhibited in the presence of nitrotyrosine compared with that of TTLL12-overexpressing cells. The results of the MTT assay revealed that the proliferation of TTLL12-silenced cells was significantly inhibited compared with that of the control group. The sensitivity, specificity and repeatability of the experiment were positive. It was found that nocodazole could have better anticancer effect than paclitaxel. Taken together, the results of the present study suggest that TTLL12 enhances SCC-25 cell survival in the presence of nitrotyrosine by disrupting nitration of the tyrosine residues of tubulin, and tubulin tyrosine nitration may be developed for the basic research of anticancer drugs.
Keywords: oral squamous cell carcinoma, tubulin tyrosine ligase like 12, nitrotyrosine, chemotherapy, microtubule
Introduction
During inflammatory conditions, nitric oxide synthases (NOSs), which include endothelial, neuronal and the inducible isoform of NOS, use oxygen and nitrogen to catalyze the production of nitric oxide (NO) (1). NO reacts with another free radical, superoxide (•OO-) to form peroxynitrite (ONOO-) (2) and ONOO- can nitrate tyrosine or protein tyrosine residues to form nitrotyrosine (3). Nitrotyrosine is similar to tyrosine in structure and is incorporated into tubulin by the enzyme tubulin-tyrosine ligase to produce the nitrotyrosination of tubulin, a process which is irreversible (4). Nitrotyrosination of tubulin can induce cell death, which is a way for the human body to remove apoptotic and abnormal cells (5). Long-term chronic inflammation, such as ulcers, gingivitis and periodontitis, may be associated with the malignant transformation of cells, resulting in the occurrence of oral squamous cell carcinoma (OSCC) as the malignant transformation of cells is not effectively eliminated (6,7). Thus, nitrotyrosine is considered a biochemical marker for oral inflammation (8) and oral cancer prognosis (9).
OSCC is one of the most common malignant tumors of the head and neck region (10). The 5-year survival rate of OSCC remains ~50% and has not significantly improved in the past decades (11). The incidence of OSCC was >300,000 cases worldwide in 2017 (12) and is increasing annually (13). Previous studies have focused on OSCC due to its high risk of malignancy, invasion and metastasis (14,15). As it invades adjacent tissues, the tumor has been demonstrated to affect speech, eating, swallowing (16) and breathing (17), which causes the quality of life of patients to decrease substantially (18). Thus, there is an urgent need to identify and develop novel effective treatment for OSCC. The occurrence and development of OSCC is a complex biological process (19), in which the overexpression of oncogenes (for example Notch1, fibroblast growth factor receptor 4 and c-myc plays an important role (20,21). Recently, a novel gene called tubulin tyrosine ligase like 12 (TTLL12) has demonstrated great interest. TTLL12 expression is significantly upregulated in lung adenocarcinoma, colorectal cancer and prostate cancer, and is closely associated with poor prognosis of these patients (22–25). Previous studies have reported that the TTL domain of TTLL12 may be involved in microtubule modification (26,27). The aim of the present study was to investigate the function of TTLL12 and develop an experiment with a novel target (tubulin tyrosine nitration).
Materials and methods
Cell culture
The human OSCC cell line, SCC-25 was purchased from the Center Laboratory of Chongqing Medical University and maintained in DMEM (Sigma-Aldrich; Merck KGaA) supplemented with 10% fetal calf serum, 1 mM sodium pyruvate and 40 µg/ml gentamycin (all purchased from Gibco; Thermo Fisher Scientific, Inc.), at 37°C in 5% CO2.
Lentiviral transfection
hTTLL12 complementary DNA was cloned into pTY linkers (Sigma-Aldrich; Merck KGaA), which was transiently transfected into 293T cells (Shanghai Institute of Life Sciences; http://life.fudan.edu.cn/) using calcium phosphate-mediated transient transfection reagent. A lentivirus (Sigma-Aldrich; Merck KGaA) was transfected into SCC-25 cells. The TTLL12-overexpressing cell lines, TTLL12_A and TTLL12_B, and the control clones, control_A and control_B were constructed.
siRNA targeted against TTLL12
A total of two small interfering (si)RNA sequences targeting TTLL12 (siTTLL12-1; 5′-GAGUUCAUCCCCGAGUUUG-3′ and siTTLL12-2; 5′-GGAACGAGCUGUGCUACAA-3′), and two negative control sequences [siControl (CONTROL® Non-Targeting siRNA #1) and siLuciferase (GL2 luciferase siRNA)] were purchased from GE Healthcare Dharmacon, Inc. siRNA transfections were performed using Lipofectamine® 3000 (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. Briefly, 100,000 cells were seeded into a 12-well plate and incubated in modified Eagle's medium (Shanghai Institute of Life Sciences; http://life.fudan.edu.cn/) supplemented with 10% fetal calf serum (Shanghai Institute of Life Sciences), 1 mM sodium pyruvate, 40 µg/ml gentamycin (Shanghai Institute of Life Sciences) at a temperature of 37°C in an environment containing 5% CO2 for 18 h. Subsequently, cells were further incubated in OPTIMEM (Sigma-Aldrich; Merck KGaA) at a temperature of 37°C for 3 h, prior to transfection. A total of 10 nM siRNA was transfected per well. After 6 h, the medium was replaced with normal growth medium and cells were incubated until cell lysis. After 24 h, subsequent experimentation was performed.
Cell proliferation assay
In total, 10,000 cells were seeded into 96-well plates. Cell proliferation was assessed via the MTT-based colorimetric assay (Chemicon International), according to the manufacturer's instructions. Dimethyl sulfoxide was used to dissolve the purple formazan crystals. The optical density (OD) of the MTT reaction was measured at 450 nm.
Western blotting
Cells were lysed using 50 µl lysis buffer (Shanghai Institute of Life Sciences) (1 mM DTT, 0.125 mM EDTA, 5% glycerol, 1 mM PMSF, 1 lg/ml leupeptin, 1 lg/ml pepstatin, 1 lg/ml aprotinin and 1% Triton X-100 in 12.5 mM Tris-HCl buffer, pH 7.0) (Shanghai Institute of Life Sciences). Protein concentration was quantified using a BCA Protein Assay kit. The protein samples (20 µg/lane) were separated via SDS-PAGE on a 10% gel and subsequently transferred onto nitrocellulose membranes. The membranes were blocked with 5% dry milk at a temperature of 37°C for 45 min prior to incubation with primary antibodies against: TTLL12 (1:2,000; cat. no. ab154086; Abcam), tributyl phosphate (TBP) (1:800; cat. no. ab220788; Abcam) and nitrotyrosine (1:1,000; cat. no. ab110282; Abcam) at a temperature of 37°C for 3 h. Following the primary incubation, membranes were incubated with a horseradish peroxidase-conjugated secondary antibody (1:2,000; cat. no. ab6271; Abcam) at a temperature of 37°C for 1 h. Protein bands were visualized using the enhanced chemiluminescence kit (cat. no. 15159; Thermo Fisher Scientific, Inc.). The target bands were quantified using Image-Pro Plus J software (version 6.0; National Institutes of Health) with TBP as internal control.
Immunofluorescence
In total, 100,000 cells were cultured on glass coverslips with gelatin (Shanghai Institute of Life Sciences) at 37°C for 12 h, fixed with 4% cold paraformaldehyde at room temperature for 20 min and incubated with 2.5% bovine serum albumin in phosphate buffered saline (PBS) for 1 h. After washing with PBS twice, cells were incubated with primary antibodies against TTLL12 (1:2,000; cat. no. ab154086; Abcam), overnight at 4°C. Following the primary incubation, cells were incubated with a peroxidase-conjugated IgG secondary antibody (1:1,000; cat. no. A0545; Sigma-Aldrich; Merck KGaA) for 1 h at room temperature. Nuclei were counterstained with 1 µM DAPI at 37°C for 5 min and cells were observed under a Leica Sp8 confocal scanning laser microscope (magnification, ×400; Leica Microsystems, Inc.).
Determining negative and positive controls
Paclitaxel is known to exert a therapeutic effect on OSCC and increases tubulin tyrosine nitration (28,29); thus, it was used as a positive control in the present study. Thiirene was used as a negative control as it does not affect tubulin tyrosine nitration (30), and no evidence associating thiirene and tumor progression has been documented in the following: PubMed (https://pubmed.ncbi.nlm.nih.gov), Web of Science (http://login.webofknowledge.com), Ovid (http://ovidsp.ovid.com), Science Direct (https://www.sciencedirect.com), Wan Fang (http://www.cquc.net) or the China National Knowledge Infrastructure databases (https://www.cnki.net).
Stable TTLL12-overexpressing SCC-25 cells (experimental group) were treated with 400 µM nitrotyrosine and 100 µM paclitaxel or thiirene (all Shanghai Institute of Life Sciences) at 37°C for 24 h, while cells in the control group were treated with 400 µM nitrotyrosine at 37°C for 24 h. Cells were harvested in lysis buffer (Shanghai Institute of Life Sciences) (1 mM DTT, 0.125 mM EDTA, 5% glycerol, 1 mM PMSF, 1 lg/ml leupeptin, 1 lg/ml pepstatin, 1 lg/ml aprotinin and 1% Triton X-100 in 12.5 mM Tris-HCl buffer, pH 7.0) (Shanghai Institute of Life Sciences)and subjected to western blotting. Tubulin tyrosine nitration levels were quantified using Quantity One version 4.62 software (Bio-Rad Laboratories, Inc.) and normalized to TBP. Error bars represent the mean ± standard error of the mean (SEM) of three independent experiments.
Determining the optimum concentration of nitrotyrosine and drug
TTLL12-overexpressing cells were seeded into 96-well plates at a density of 1×104 cells/well and cultured in modified Eagle's medium supplemented with 10% fetal calf serum, 1 mM sodium pyruvate, 40 µg/ml gentamycin (Shanghai Institute of Life Sciences) in a 5% CO2 incubator at 37°C for 6 h. Different concentrations of nitrotyrosine (800, 400, 200, 100 and 50 µM) and paclitaxel or thiirene (40, 20, 10 and 5 µM) were added into the wells to determine the optimal concentration of nitrotyrosine and drug by square matrix titrimetry (31). After cells were cultured at 37°C for 24 h, the MTT assay was subsequently performed to assess cell proliferation.
In vitro experiment with novel target (tubulin tyrosine nitration) to screen anticancer drugs
Stable TTLL12-overexpressing SCC-25 cells were seeded into 96-well plates at a density of 10,000 cells/well and incubated in modified Eagle's medium supplemented with 10% fetal calf serum, 1 mM sodium pyruvate, 40 µg/ml gentamycin. (Shanghai Institute of Life Sciences) at 37°C for 6 h. MEM (Shanghai Institute of Life Sciences) (20 µl) supplemented with nitrotyrosine (final concentration, 400 µM) and anticancer drugs (final concentration, 10 µM) was added to the cells and further incubated at 37°C for 24 h. Paclitaxel and thiirene were used as the positive and negative controls, respectively. Following incubation, the upper medium was gently removed and 100 µl buffer [90 mM Mes pH 6.7, 1 mM EGTA, 1 mM MgCl2, 10% (v/v) glycerol and 0.5% (v/v) Triton X-100; Shanghai Institute of Life Sciences] was added to the cells and further incubated at 37°C for 3 min. Once again, the upper medium was gently removed and 100 µl PBS supplemented with 3.7% paraformaldehyde and 0.05% Tween-20 (Shanghai Institute of Life Sciences) was added. Following incubation at 37°C for 10 min, the upper medium was gently removed and cells were further incubated with 100 µl PBS containing anti-nitrotyrosine antibody (1:1,000; cat. no. 16-207, clone 1A6, HRP conjugate, Sigma-Aldrich; Merck-KGaA) for 1 h at room temperature. Once again, the upper medium was gently removed and well was washed once with 200 µl PBS supplemented with 0.05% Tween-20. Finally, the upper medium was gently removed and 100 µl OPD-H2O2 (Shanghai Institute of Life Sciences) was added at 37°C for 3 min, prior to addition of 50 µl H2SO4 (Shanghai Institute of Life Sciences) (2 mol/l) at 37°C for 3 min. The absorbance was detected at a wavelength of 450 nm, using a microplate reader (Thermo Fisher Scientific, Inc.). The Nitrotyrosine ELISA kit (K4158-100, Hycult Biotech Inc.) was used for detection in strict accordance with the manufacturer's instructions and repeated three times.
Sensitivity, specificity and repeatability of the experimental method
In vitro experiments must have good sensitivity, specificity and repeatability, therefore the following experiments are done.
Sensitivity of the experiment
Stable TTLL12-overexpressing SCC-25 cells were seeded into 96-well plates at a density of 10,000 cells/well and incubated in modified Eagle's medium supplemented with 10% fetal calf serum, 1 mM sodium pyruvate, 40 µg/ml gentamycin (Shanghai Institute of Life Sciences) at 37°C for 6 h. The following concentrations of nitrotyrosine (80, 40, 20, 10, 5 and 2.5 µM) were added to the cells. Paclitaxel and thiirene were used as the positive and negative controls, respectively. Following incubation, the upper medium was gently removed and 100 µl buffer [90 mM Mes pH 6.7, 1 mM EGTA, 1 mM MgCl2, 10% (v/v) glycerol and 0.5% (v/v) Triton X-100; Shanghai Institute of Life Sciences] was added to the cells and further incubated at 37°C for 3 min. Once again, the upper medium was gently removed and 100 µl PBS supplemented with 3.7% paraformaldehyde and 0.05% Tween-20 (Shanghai Institute of Life Sciences) was added. The Nitrotyrosine ELISA kit (cat. no. K4158-100; Hycult Biotech Inc.) was used for detection in strict accordance with the manufacturer's instructions and repeated three times.
Specificity of the experiment
It is well-known that carboplatin (CDDP), 5-fluorouracil (5-FU), cyclophosphamide (CTX) and methotrexate (MTX) exert notable effects on cancer development but have no effects on microtubules (32–35). Stable TTLL12-overexpressing SCC-25 cells were seeded into 96-well plates at a density of 10,000 cells/well and incubated in modified Eagle's medium supplemented with 10% fetal calf serum, 1 mM sodium pyruvate, 40 µg/ml gentamycin. (Shanghai Institute of Life Sciences) at 37°C for 6 h. MEM (Shanghai Institute of Life Sciences) (20 µl) supplemented with nitrotyrosine (final concentration, 400 µM) and anticancer drugs (CDDP, 5-FU, CTX and MTX) (Shanghai Institute of Life Sciences) (final concentration, 10 µM) was added to the cells and further incubated at 37°C for 24 h. The rest of the experiment was performed as aforementioned.
Repeatability of the experiment
Stable TTLL12-overexpressing SCC-25 cells were seeded into 96-well plates at a density of 10,000 cells/well and incubated in modified Eagle's medium supplemented with 10% fetal calf serum, 1 mM sodium pyruvate, 40 µg/ml gentamycin (Shanghai Institute of Life Sciences) at 37°C for 6 h. MEM (Shanghai Institute of Life Sciences) (20 µl) supplemented with nitrotyrosine (final concentration, 400 µM) and samples (Paclitaxel, thiirene, CDDP, 5-FU and CTX) (final concentration, 10 µM) was added to the cells and further incubated at 37°C for 24 h. The rest of the experiment was performed as aforementioned. It was the intra-batch assay. The same experiment was subsequently done over 4 different days for the inter-batch assay.
Determining the validity of the experiment
In total, 40 compounds were randomly selected by Shanghai Institute of Life Sciences and assessed in the experiment. Stable TTLL12-overexpressing SCC-25 cells (experimental group) were treated with 400 µM nitrotyrosine and 10 µM nocodazole (Shanghai Institute of Life Sciences) at 37°C for 24 h, while cells in the control group were treated with 400 µM nitrotyrosine at 37°C for 24 h. Cells were harvested in buffer and subjected to western blotting. Tubulin tyrosine nitration levels were quantified using Quantity One software and normalized to TBP. Error bars represent the mean ± SEM of three independent experiments.
Statistical analysis
Each experiment was repeated three times. Statistical analysis was performed using SPSS 10.0 software (SPSS, Inc.). Tubulin tyrosine nitration levels and the ratio of optical density (OD) 450 nm are presented as the mean ± standard deviation. One-way analysis of variance followed by Tukey's post hoc test was used to compare differences between multiple groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Effect of different concentrations of nitrotyrosine on the proliferation of SCC-25 cells
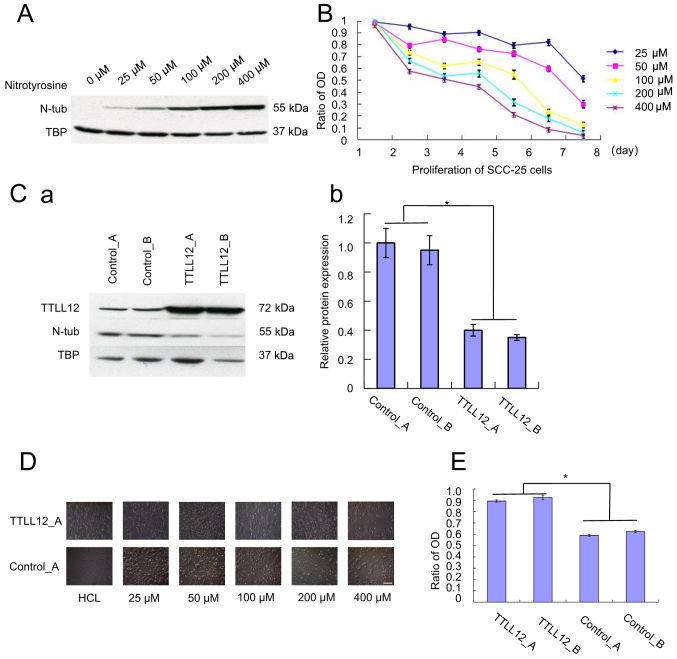
SCC-25 cells were treated with different concentrations of nitrotyrosine (0–400 µM) to determine the concentration of nitrotyrosine that effects tubulin tyrosine nitration. Western blot analysis demonstrated that the concentration of tubulin tyrosine nitration increased in relation to the concentration of nitrotyrosine (Fig. 1A). The proliferation of SCC-25 cells was assessed for 7 days via the MTT assay every 24 h. The results demonstrated that the proliferation of SCC-25 cells was inhibited following treatment with nitrotyrosine, whereby the higher the concentration of nitrotyrosine, the greater the inhibition of proliferation of SCC-25 cells (Fig. 1B). The tyrosine residues of tubulin were nitrated to form tubulin tyrosine nitration, which causes cells to die (36).
Figure 1.
Effect of overexpressing TTLL12 and nitrotyrosine on the proliferation of SCC-25 cells. (A) Cells were subjected to western blot analysis to determine protein expression. (B) Cell proliferation was assessed via the MTT assay every 24 h. The ratio of OD 450 nm was calculated as OD assay/OD control. Error bars represent the mean ± SEM of three independent experiments. (C) TTLL12-overexpressing clones, TTLL12_A and TTLL12_B, as well as control_A and control_B cells were treated with 400 µM nitrotyrosine for 24 h. (Ca) Cells from each group were subjected to western blot analysis to determine protein expression. (Cb) The blots were quantified via densitometry and normalized to TBP. Tubulin tyrosine nitration levels of all groups are presented relative to the average tubulin tyrosine nitration level of control_A. Error bars represent the mean ± SEM of three independent experiments. (D) TTLL12_A and control_A cells were cultured in different concentrations of nitrotyrosine (0–400 µM) for 24 h. Scale bar, 100 µm. (E) TTLL12_A, TTLL12_B, control_A and control_B cells were treated with 20 µl modified Eagle's medium supplemented with 400 µmol/l nitrotyrosine for 24 h, while the untreated group received medium supplemented with HCl. Cells proliferation was assessed via the MTT assay. The ratio of OD 450 nm represents the OD 450 nm of treated cells normalized to that of untreated cells. Error bars are represent the mean ± SEM of three independent experiments. *P<0.05. TTLL12, tubulin tyrosine ligase like 12; OD, optical density; TBP, tributyl phosphate, SEM, standard error of the mean; N-tub, nitrotyrosine tubulin.
Effect of overexpressing TTLL12 on tubulin tyrosine nitration and SCC-25 cell proliferation
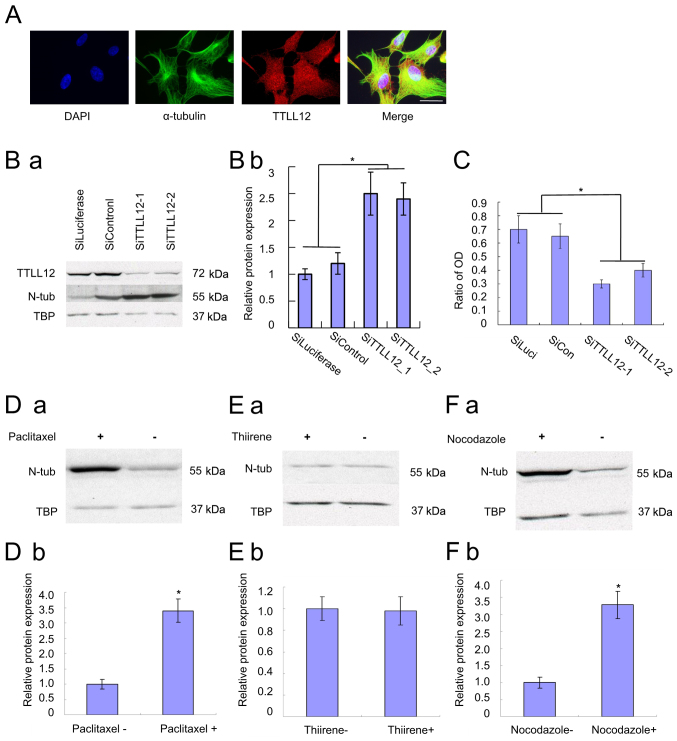
The TTLL12-overexpressing cell lines, TTLL12_A and TTLL12_B, and the control clones, control_A and control_B were constructed, and maintained in medium supplemented with 400 µM nitrotyrosine for 24 h. The results demonstrated that tubulin tyrosine nitration was significantly lower in TTLL12-overexpressing clones compared with the control clones (P<0.05; Fig. 1C). Subsequently, in order to assess the effect of overexpressing TTLL12 on cell proliferation, TTLL12_A and control_A cells were treated with different concentrations of nitrotyrosine (0–400 µM) for 24 h and observed under an inverted microscope. The results demonstrated that the proliferation of the control cells was notably inhibited following treatment with nitrotyrosine compared with the TTLL12-overexpressing cells (Fig. 1D). TTLL12-overexpressing and control clones were treated with 400 µM nitrotyrosine for 24 h. The results demonstrated a statistically significant increase in the proliferation of TTLL12-overexpressing clones compared with the control clones (P<0.05; Fig. 1E). TTLL12 localization was assessed via immunofluorescence. Nuclei were stained with DAPI (blue), TTLL12 stained red and α-tubulin stained green (Fig. 2A).
Figure 2.
Immunofluorescence of TTLL12, and the effects of TTLL12 silencing and drugs on nitrotyrosine tubulin. (A) Overexpressing cells were used for the immunofluorescence assay to investigate the localization of TTLL12. Scale bar, 25 µm. (B) siTTLL12-1, siTTLL12-2, siLuciferase and siControl cells were treated with 400 µM nitrotyrosine for 24 h. (Ba) Cells from each group were subjected to western blot analysis to determine protein expression. (Bb) The blots were quantified via densitometry and normalized to TBP. Tubulin tyrosine nitration levels of all groups are presented relative to the average tubulin tyrosine nitration level of control siRNAs. Error bars represent the mean ± SEM of three independent experiments. (C) SiTTLL12-1, SiTTLL12-2, SiLuciferase and SiControl cells were treated with 20 µl modified Eagle's medium supplemented with 400 µmol/l nitrotyrosine or 400 µmol/l HCl for 24 h. Cell proliferation was assessed via the MTT assay. The ratio of OD represents the OD 450 nm of treated cells normalized to that of untreated cells. Error bars represent the mean ± SEM of three independent experiments. (D) Stable TTLL12-overexpressing SCC-25 cells were treated with 400 µM nitrotyrosine. Paclitaxel (10 µM) was added to cells in the experimental groups, while nothing was added to the control cells. (a) After 24 h, cells from each group were subjected to western blot analysis to determine protein expression. (b) The blots were quantified via densitometry and normalized to TBP. Nitrotyrosine tubulin levels are presented relative to the average of control. Error bars represent the mean ± SEM of three independent experiments. (E) Cells were treated with 10 µM thiirene. (F) Cells were treated with 10 µM nocodazole. Nitrotyrosine tubulin levels were compared with the treatment and control groups. *P<0.05. TTLL12, tubulin tyrosine ligase like 12; si, small interfering; SEM, standard error of the mean; OD, optical density; TBP, tributyl phosphate; N-tub, nitrotyrosine tubulin.
Effect of silencing TTLL12 on tubulin tyrosine nitration and SCC-25 cell proliferation
TTLL12 expression was downregulated following siRNA transfection, which was verified via western blotting. The TTLL12-silenced cell lines, siTTLL12-1 and siTTLL12-2, and control cells, siLuciferase and siControl, were treated with 400 µM nitrotyrosine for 24 h. Western blot analysis demonstrated that tubulin tyrosine nitration was significantly higher in TTLL12-silenced cells compared with the control cells (P<0.05; Fig. 2B). Furthermore, downregulation of TTLL12 led to an increase in tubulin tyrosine nitration. The results of the MTT assay demonstrated that the proliferation of TTLL12-silenced cells was significantly inhibited compared with the control cells (P<0.05; Fig. 2C). In addition, downregulation of TTLL12 decreased cell proliferation of TTLL12-silenced cells compared with the control cells (Fig. 2C).
Effects of paclitaxel and thiirene on tubulin tyrosine nitration
Western blot analysis demonstrated that tubulin tyrosine nitration increased in cells treated with paclitaxel, suggesting a positive association between the two (Fig. 2D). Thus, paclitaxel was used as a positive control. Conversely, the results demonstrated no significant differences in tubulin tyrosine nitration in cells without or with thiirene (Fig. 2E), suggesting that thiirene does not affect the level of tubulin tyrosine nitration. Thus, thiirene was used as a negative control.
Determining the optimum concentration of nitrotyrosine and drug
The results of the square matrix titrimetry assay demonstrated that the OD 450 nm value of 400 µM nitrotyrosine and 10 µM paclitaxel was ~1.0, while the OD 450 nm value of thiirene was lower, and the ratio of the positive to negative control (P/N value) was the highest. Thus, 400 µM was considered the optimal concentration of nitrotyrosine, and 10 µM the optimal concentration of drug (Table I).
Table I.
Determining the optimum concentration of nitrotyrosine and drug.
| Concentration of nitrotyrosine | ||||||
|---|---|---|---|---|---|---|
| Concentration of drug | 50 µM | 100 µM | 200 µM | 400 µM | 800 µM | |
| 5 µM | Paclitaxel | 0.427±0.031 | 0.596±0.043 | 0.714±0.052 | 0.846±0.061 | 1.126±0.109 |
| Thiirene | 0.187±0.011 | 0.195±0.009 | 0.224±0.019 | 0.253±0.022 | 0.225±0.021 | |
| 10 µM | Paclitaxel | 0.647±0.041 | 0.864±0.061 | 1.110±0.129 | 1.097±0.055 | 1.230±0.097 |
| Thiirene | 0.110±0.009 | 0.126±0.011 | 0.130±0.014 | 0.122±0.011 | 0.147±0.015 | |
| 20 µM | Paclitaxel | 0.801±0.067 | 1.104±0.096 | 1.135±0.109 | 1.116±0.091 | 1.235±0.115 |
| Thiirene | 0.108±0.091 | 0.124±0.011 | 0.132±0.012 | 0.126±0.014 | 0.139±0.012 | |
| 40 µM | Paclitaxel | 0.810±0.064 | 1.130±0.122 | 1.180±0.096 | 1.281±0.108 | 1.332±0.113 |
| Thiirene | 0.110±0.089 | 0.129±0.093 | 0.133±0.101 | 0.147±0.107 | 0.149±0.112 | |
Sensitivity, specificity and repeatability of the experiment
The results of the sensitivity assay demonstrated that the OD 450 nm value of paclitaxel with a minimum concentration of 2.5 µM was 0.681, which was higher than the OD 450 nm value of 10 µM thiirene (0.122) (Table II). Thus, the sensitivity of the novel experiment was considered positive.
Table II.
Sensitivity assay results.
| Concentration of nitrotyrosine | 80 µM | 40 µM | 20 µM | 10 µM | 5 µM | 2.5 µM |
|---|---|---|---|---|---|---|
| OD, 450 nm | 1.330±0.119 | 1.291±0.107 | 1.118±0.113 | 1.086±0.064 | 0.846±0.076 | 0.681±0.054 |
OD, optical density.
The results of the specificity assay demonstrated that the OD 450 nm value of paclitaxel (1.102) was considerably higher compared with the other drugs (Thiirene, 0.157; CDDP, 0.108; 5-FU, 0.179; CTX, 0.207; MTX, 0.251; Table III). Thus, the specificity of the novel experiment was considered positive (Table III).
Table III.
Specificity assay results.
| Paclitaxel | Thiirene | CDDP | 5-FU | CTX | MTX | |
|---|---|---|---|---|---|---|
| OD, 450 nm | 1.102±0.042 | 0.157±0.012 | 0.108±0.014 | 0.179±0.011 | 0.207±0.014 | 0.251±0.017 |
OD, optical density; CDDP, carboplatin; 5-FU, 5-fluorouracil; CTX, cyclophosphamide; MTX, methotrexate.
The results of the repeatability assay demonstrated that the coefficient of variation (CV) of the intra-batch assay was 3.50–7.87%, while the CV of the inter-batch assay was 2.86–6.99%. Given that both values were <10%, the repeatability of the experiment was considered positive (Table IV).
Table IV.
Intra-batch and inter-batch reproducibility assay results.
| Intra-batch assay (OD, 450 nm) | Inter-batch assay (OD, 450 nm) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | CV | Mean | SD | CV | |
| Paclitaxel | 1.107 | 0.047 | 4.25 | 1.084 | 0.031 | 2.86 |
| Thiirene | 0.163 | 0.011 | 6.75 | 0.143 | 0.006 | 4.20 |
| CDDP | 0.114 | 0.004 | 3.50 | 0.121 | 0.007 | 5.79 |
| 5-FU | 0.186 | 0.008 | 4.30 | 0.179 | 0.011 | 6.15 |
| CTX | 0.216 | 0.017 | 7.87 | 0.229 | 0.016 | 6.99 |
OD, optical density; SD, standard deviation, CV, coefficient of variation; CDDP, carboplatin; 5-FU, 5-fluorouracil; CTX, cyclophosphamide.
Application of the experiment
The results of the last experiment demonstrated that the OD 450 nm value of most samples was <0.452 (Table V), and only the OD 450 nm value of sample no. 14 was >1 (1.043; Table V), showing that shwed nocodazole could have an improved anticancer effect compared with paclitaxel. Western blot analysis demonstrated that tubulin tyrosine nitration increased in cells treated with nocodazole, suggesting a positive association between the two (Fig. 2F).
Table V.
Novel experiment results.
| Sample | OD, 450 nm | Sample | OD, 450 nm | Sample | OD, 450 nm | Sample | OD, 450 nm |
|---|---|---|---|---|---|---|---|
| Paclitaxel | 1.091±0.043 | 1 | 0.132±0.010 | 2 | 0.147±0.013 | 3 | 0.151±0.011 |
| 4 | 0.129±0.012 | 5 | 0.136±0.013 | 6 | 0.158±0.018 | 7 | 0.235±0.019 |
| 8 | 0.321±0.025 | 9 | 0.351±0.027 | 10 | 0.358±0.029 | 11 | 0.247±0.021 |
| 12 | 0.241±0.019 | 13 | 0.411±0.037 | 14 | 1.043±0.042 | 15 | 0.412±0.022 |
| 16 | 0.314±0.019 | 17 | 0.452±0.031 | 18 | 0.189±0.009 | 19 | 0.338±0.026 |
| 20 | 0.371±0.019 | 21 | 0.121±0.011 | 22 | 0.365±0.024 | 23 | 0.146±0.015 |
| 24 | 0.352±0.029 | 25 | 0.347±0.017 | 26 | 0.122±0.009 | 27 | 0.157±0.014 |
| 28 | 0.163±0.013 | 29 | 0.221±0.019 | 30 | 0.289±0.017 | 31 | 0.113±0.008 |
| 32 | 0.167±0.009 | 33 | 0.148±0.011 | 34 | 0.128±0.012 | 35 | 0.168±0.014 |
| 36 | 0.278±0.016 | 37 | 0.263±0.019 | 38 | 0.410±0.031 | 39 | 0.247±0.022 |
| 40 | 0.162±0.011 |
OD, optical density.
Discussion
Microtubules are the basic units of the cytoskeleton, which exist in all eukaryotic cells (37). They are polymerized by microtubule protein and can be assembled into cilia, flagella, axon, neural tube, basal granule, centriole and spindle (38). Microtubules participate in the formation of the cytoskeleton, maintenance of cell morphology, cell contraction, pseudopodia movement, material transport and cell division (39,40). Prior to functioning, microtubules need to be coated with tubulin tyrosine ligase (TTL) (41). TTL is involved in nitrotyrosine-mediated post-translational modification of tubulin (4,42). In the presence of nitrotyrosine, TTL induces tubulin tyrosine nitration, which significantly changes the structure of microtubules, decreases the adhesive ability of cells, causes cell deformation and intracellular transport obstacle, and eventually leads to cell apoptosis and organ function loss (43,44).
Previous studies have detected nitrotyrosine in fresh-frozen human tissue samples and have demonstrated that nitrotyrosine is an important marker for oral cancer prognosis and survival (9). However, there is a lack of studies assessing the effect of nitrotyrosine on the proliferation of oral cancer cells. The results of the present study demonstrated that the proliferation inhibition of SCC-25 cells was proportional to the content of nitrotyrosine, which suggest that nitrotyrosine inhibits SCC-25 cell proliferation. TTLL12-overexpressing clones (TTLL12_A and TTLL12_B) and control clones (control_A and control_B) were constructed and treated with nitrotyrosine. The results demonstrated that TTLL12 promoted the proliferation of SCC-25 cells by inhibiting the formation of tubulin tyrosine nitration. Furthermore, TTLL12-silenced clones (siTTLL12-1 and siTTLL12-2) and control clones (siLuciferase and siControl) were constructed and treated with nitrotyrosine. The results demonstrated that tubulin tyrosine nitration formation increased, and the proliferation of SCC-25 cells was inhibited in TTLL12-silenced cell lines compared with the control cells. Following overexpression of TTLL12, tubulin tyrosine nitration formation decreased, and cells continued to proliferate by escaping the attack of tubulin tyrosine nitration. Conversely, TTLL12 silencing increased tubulin tyrosine nitration and inhibited cell proliferation. Taken together, these results suggest that TTLL12 may function as a potential oncogene. Although the immunofluorescence results demonstrated that TTLL12 appeared to overlap with α-tubulin, the molecular mechanism by which TTLL12 regulates tubulin tyrosine nitration remains unclear and requires further investigation. It can be hypothesized that TTLL12 and nitro have the same binding site on α-tubulin, and thus competes with α-tubulin. It was hypothesized that when TTLL12 is overexpressed, it becomes difficult to nitrate the tyrosine residues of tubulin, thus tubulin tyrosine nitration decreases.
Malignant tumors (for example oral, liver and gastric cancer) seriously threaten the well-being and quality of life of affected patients (45). Currently, there are no effective treatments for cancer, and comprehensive treatment is extensively applied in the clinical setting (46). Chemotherapy, as the only effective systemic treatment, began in 1948 (folic acid antagonists were used as antitumor drugs to treat leukemia), which plays an irreplaceable role in the comprehensive treatment of cancer (47). Due to the heterogeneity of tumors (48), different individuals have different reactions to the same drug, which affects the treatment outcome. In response to this problem, some medical studies have proposed to use a drug sensitivity experiment to provide individualized treatment to improve the clinical efficacy (49,50). In vitro drug sensitivity experiments have been extensively used in the last century due to their effective and efficient outcomes (51). However, the microenvironment in vivo may lead to the emergence of drug resistance (52), which decreases the efficacy of drug sensitivity experiments in vitro to guide clinical individualized treatment. However, effective methods (drug sensitivity experiments in vitro and in vivo) to identify potential effective anticancer reagents remain (53,54).
The majority of drug sensitivity experiments in vitro aim to assess the anticancer effect of drugs by detecting the ratio of living cells to dead cells after the tumor cells are cultured with drugs (55). Novel effective drugs that can kill tumors are identified by drug sensitivity experiments; however, the anticancer molecular mechanism of these drugs remains unknown. This notably disrupts the clinical application of novel drugs. Thus, additional experiments are required to identify the anticancer molecular mechanism of novel drugs, which are time consuming and expensive, and delay the treatment of patients.
Based on this concept, the present study established a novel type of drug sensitivity test targeting tubulin tyrosine nitration in vitro by combining the research results with the enzyme-linked immunosorbent assay (ELISA). This novel assay can screen out new effective anticancer drugs and determine the anticancer molecular mechanism of these drugs. Paclitaxel exerts a notable therapeutic effect on OSCC and increases tubulin tyrosine nitration (28,29); thus, it was used as a positive control in the present study. Conversely, thiirene is not associated with tumors and does not affect tubulin tyrosine nitration (30); thus, it was used as a negative control in the present study. TTLL12-overexpressing cells were treated with the samples and nitrotyrosine, and tubulin tyrosine nitration was detected via ELISA. If the OD value of the samples was greater than that of the positive control, the samples were considered to have a positive anticancer effect. The results of the experiment demonstrated that nocodazole increased tubulin tyrosine nitration, and its OD 450 nm value was high, thus, it may be considered a promising anticancer drug.
The novel experiment has the following characteristics: It is simple, sensitive, fast, specific, cheap, stable and easy to be popularized. This experiment consists of a few steps and simple technologies, including cell culture and ELISA, which are both easy to perform. The highly efficient biocatalysis of enzymes is used in the novel experiment, so that markedly low contents of tubulin tyrosine nitration can be detected, and the novel experiment has high sensitivity. The experiments lasts for ~32 h and detection occurs using a 96-well plate, thus, the overall time required is relatively short and the experiment is fast. The combination of anti-nitrotyrosine antibody and tubulin tyrosine nitration is that of antibody and antigen, thus, the experiment has high specificity. Special or valuable materials are not involved, thus the materials are easily attained and affordable. The experiment comprises only a few steps, few reagents and few variation factors, which facilitates good repeatability and stability. Considering the aforementioned advantages, the experiment can be easily popularized and used for large-scale screening. The experiment can automatically and mechanically detect multiple 96-well plates simultaneously, whereby one 96-well plate can analyze 16 samples at a time. Thus, if multiple 96-well plates are detected in parallel, hundreds of samples can be detected within 32 h. This high-throughput test has another benefit in that the results of the experiment not only present the anticancer effect of the sample, but also reveal its anticancer molecular mechanism. If the sample participates in the process of microtubule modification, whereby it can promote the formation of tubulin tyrosine nitration, tumor cells will experience apoptosis. Simultaneously, tubulin tyrosine nitration will combine with the antibody, which will eventually increase the OD value (56). If the OD value of the sample is higher than that of the positive control, this suggests that the sample is a promising anticancer drug. Such a drug can kill cancer cells, and its anticancer effect may even be better than that of paclitaxel; its anticancer molecular mechanism involves its participation in the process of microtubule modification, which promotes the formation of tubulin tyrosine nitration, thus causing tumor cell apoptosis. This information can greatly speed up the application of the drug in the clinical setting, and is expected to improve patients survival outcomes. To the best of our knowledge, the present study was the first to use TTLL12-overexpressing cell lines to screen anticancer drugs, paving the way for future research on novel anticancer drugs targeting the microtubule system. However, our results need to be verified in vivo in the future.
In conclusion, the results of the present study demonstrated that TTLL12 promoted SCC-25 cell survival in the presence of nitrotyrosine by decreasing the formation of tubulin tyrosine nitration. The novel experiment described in the present study is simple, sensitive, rapid, specific, affordable, stable and easy to be popularized, and has good application for basic research on anticancer drugs.
Acknowledgements
Not applicable.
Funding
The present study was partly funded by the Natural Science Foundation Project of CQ CSTC (grant no. cstc2018jcyjAX0763) and the Chongqing Municipal Health Bureau (grant no. 2017HBRC004).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Authors' contributions
YL designed the present study. CF and WC participated in statistical analyses. CF interpreted the western blot results. WC performed immunofluorescence assessment of the cells. YL, LX and YZ interpreted the results, and prepared and drafted the initial manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Anavi S, Tirosh O. iNOS as a metabolic enzyme under stress conditions. Free Radic Biol Med. 2020;146:16–35. doi: 10.1016/j.freeradbiomed.2019.10.411. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein S, Merényi G. The chemistry of peroxynitrite: Implications for biological activity. Methods Enzymol. 2008;436:49–61. doi: 10.1016/S0076-6879(08)36004-2. [DOI] [PubMed] [Google Scholar]
- 3.Wang B, Wang Y, Wang Y, Zhao Y, Yang C, Zeng Z, Huan S, Song G, Zhang X. Oxygen-embedded pentacene based near-infrared chemiluminescent nanoprobe for highly selective and sensitive visualization of peroxynitrite in vivo. Anal Chem. 2020;92:4154–4163. doi: 10.1021/acs.analchem.0c00329. [DOI] [PubMed] [Google Scholar]
- 4.Eiserich JP, Estévez AG, Bamberg TV, Ye YZ, Chumley PH, Beckman JS, Freeman BA. Microtubule dysfunction by posttranslational nitrotyrosination of alpha-tubulin: A nitric oxide-dependent mechanism of cellular injury. Proc Natl Acad Sci USA. 1999;96:6365–6370. doi: 10.1073/pnas.96.11.6365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartesaghi S, Radi R. Fundamentals on the biochemistry of peroxynitrite and protein tyrosine nitration. Redox Biol. 2018;14:618–625. doi: 10.1016/j.redox.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tampa M, Mitran MI, Mitran CI, Sarbu MI, Matei C, Nicolae I, Caruntu A, Tocut SM, Popa MI, Caruntu C, Georgescu SR. Mediators of inflammation-A potential source of biomarkers in oral squamous cell carcinoma. J Immunol Res. 2018;2018:1061780. doi: 10.1155/2018/1061780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee BJ, Chan MY, Hsiao HY, Chang CH, Hsu LP, Lin PT. Relationship of Oxidative Stress, Inflammation, and the Risk of Metabolic Syndrome in Patients with Oral Cancer. Oxid Med Cell Longev. 2018;2018:9303094. doi: 10.1155/2018/9303094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaiyarit P, Ma N, Hiraku Y, Pinlaor S, Yongvanit P, Jintakanon D, Murata M, Oikawa S, Kawanishi S. Nitrative and oxidative DNA damage in oral lichen planus in relation to human oral carcinogenesis. Cancer Sci. 2005;96:553–559. doi: 10.1111/j.1349-7006.2005.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silva Servato JP, Ueira Vieira C, de Faria PR, Cardoso SV, Loyola AM. The importance of inducible nitric oxide synthase and nitrotyrosine as prognostic markers for oral squamous cell carcinoma. J Oral Pathol Med. 2019;48:967–975. doi: 10.1111/jop.12942. [DOI] [PubMed] [Google Scholar]
- 10.Olek M, Kasperski J, Skaba D, Wiench R, Cieślar G, Kawczyk-Krupka A. Photodynamic therapy for the treatment of oral squamous carcinoma-clinical implications resulting from in vitro research. Photodiagnosis Photodyn Ther. 2019;27:255–267. doi: 10.1016/j.pdpdt.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Irani S. Pre-cancerous lesions in the oral and maxillofacial region: A literature reviewwith special focus on etiopathogenesis. Iran J Pathol. 2016;11:303–322. [PMC free article] [PubMed] [Google Scholar]
- 12.Vucicevic Boras V, Fucic A, Virag M, Gabric D, Blivajs I, Tomasovic-Loncaric C, Rakusic Z, Bisof V, Novere NL, Velimir Vrdoljak D. Significance of stroma in biology of oral squamous cell carcinoma. Tumori. 2018;104:9–14. doi: 10.5301/tj.5000673. [DOI] [PubMed] [Google Scholar]
- 13.Bao X, Liu F, Lin J, Chen Q, Chen L, Chen F, Wang J, Qiu Y, Shi B, Pan L, et al. Nutritional assessment and prognosis of oral cancer patients: A large-scale prospective study. BMC Cancer. 2020;20:146. doi: 10.1186/s12885-020-6604-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang SS, Zheng M, Pang X, Zhang M, Yu XH, Wu JB, Gao XL, Wu JS, Yang X, Tang YJ, et al. Macrophage migration inhibitory factor promotes the invasion and metastasis of oral squamous cell carcinoma through matrix metalloprotein-2/9. Mol Carcinog. 2019;58:1809–1821. doi: 10.1002/mc.23067. [DOI] [PubMed] [Google Scholar]
- 15.Ortiz RC, Lopes NM, Amôr NG, Ponce JB, Schmerling CK, Lara VS, Moyses RA, Rodini CO. CD44 and ALDH1 immunoexpression as prognostic indicators of invasion and metastasis in oral squamous cell carcinoma. J Oral Pathol Med. 2018;47:740–747. doi: 10.1111/jop.12734. [DOI] [PubMed] [Google Scholar]
- 16.Romer CAE, Broglie Daeppen MA, Mueller M, Huber GF, Guesewell S, Stoeckli SJ. Long-term speech and swallowing function after primary resection and sentinel node biopsy for early oral squamous cell carcinoma. Oral Oncol. 2019;89:127–132. doi: 10.1016/j.oraloncology.2018.12.027. [DOI] [PubMed] [Google Scholar]
- 17.Deng W, Yang L, Xie C, Lu H, Xiao Y, Zeng B, Liang Y, Liao G. Prediction of postoperative lower respiratory tract infections in tongue cancer patients based on pretreatment swallowing function. Oral Dis. 2020;26:537–546. doi: 10.1111/odi.13270. [DOI] [PubMed] [Google Scholar]
- 18.Goswami S, Gupta SS. How cancer of oral cavity affects the family caregivers? -A cross-sectional study in Wardha, India, using the caregiver quality of life index-cancer questionnaire. South Asian J Cancer. 2020;9:62–65. doi: 10.4103/sajc.sajc_331_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun Y, Liu N, Guan X, Wu H, Sun Z, Zeng H. Immunosuppression induced by chronic inflammation and the progression to oral squamous cell carcinoma. Mediators Inflamm. 2016;2016:5715719. doi: 10.1155/2016/5715719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu L, Hou TJ, Yang P. Mechanism of lncRNA FEZF1-AS1 in promoting the occurrence and development of oral squamous cell carcinoma through targeting miR-196a. Eur Rev Med Pharmacol Sci. 2019;23:6505–6515. doi: 10.26355/eurrev_201908_18534. [DOI] [PubMed] [Google Scholar]
- 21.Xiao T, Sun J, Xing Z, Xie F, Yang L, Ding W. MTFP1 overexpression promotes the growth of oral squamous cell carcinoma by inducing ROS production. Cell Biol Int. 2020;44:821–829. doi: 10.1002/cbin.11278. [DOI] [PubMed] [Google Scholar]
- 22.Sanada H, Seki N, Mizuno K, Misono S, Uchida A, Yamada Y, Moriya S, Kikkawa N, Machida K, Kumamoto T, et al. Involvement of dual strands of miR-143 (miR-143-5p and miR-143-3p) and their target oncogenes in the molecular pathogenesis of lung adenocarcinoma. Int J Mol Sci. 2019;20:4482. doi: 10.3390/ijms20184482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu J, Li H, Shen S, Sun L, Yuan Y, Xing C. Alternative splicing events implicated in carcinogenesis and prognosis of colorectal cancer. J Cancer. 2018;9:1754–1764. doi: 10.7150/jca.24569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wen R, Xiao Y, Zhang Y, Yang M, Lin Y, Tang J. Identification of a novel transcript isoform of the TTLL12 gene in human cancers. Oncol Rep. 2016;36:3172–3180. doi: 10.3892/or.2016.5135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Massoner P, Lueking A, Goehler H, Höpfner A, Kowald A, Kugler KG, Amersdorfer P, Horninger W, Bartsch G, Schulz-Knappe P, Klocker H. Serum-autoantibodies for discovery of prostate cancer specific biomarkers. Prostate. 2012;72:427–436. doi: 10.1002/pros.21444. [DOI] [PubMed] [Google Scholar]
- 26.Li H, Huang Y, Yu Y, Li G, Karamanos Y. Self-catalyzed assembly of peptide scaffolded nanozyme as a dynamic biosensing system. ACS Appl Mater Interfaces. 2016;8:2833–2839. doi: 10.1021/acsami.5b11567. [DOI] [PubMed] [Google Scholar]
- 27.Wasylyk C, Zambrano A, Zhao C, Brants J, Abecassis J, Schalken JA, Rogatsch H, Schaefer G, Pycha A, Klocker H, Wasylyk B. Tubulin tyrosine ligase like 12 links to prostate cancer through tubulin posttranslational modification and chromosome ploidy. Int J Cancer. 2010;127:2542–2553. doi: 10.1002/ijc.25261. [DOI] [PubMed] [Google Scholar]
- 28.Robert BM, Dakshinamoorthy M, Ganapathyagraharam Ramamoorthy B, Dhandapani M, Thangaiyan R, Muthusamy G, Nirmal RM, Prasad NR. Predicting tumor sensitivity to chemotherapeutic drugs in oral squamous cell carcinoma patients. Sci Rep. 2018;8:15545. doi: 10.1038/s41598-018-33998-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wood SC, Tang X, Tesfamariam B. Paclitaxel potentiates inflammatory cytokine-induced prothrombotic molecules in endothelial cells. J Cardiovasc Pharmacol. 2010;55:276–285. doi: 10.1097/FJC.0b013e3181d263f7. [DOI] [PubMed] [Google Scholar]
- 30.Zhou X, Wu J, Hao Y, Zhu C, Zhuo Q, Xia H, Zhu J. Rational design and synthesis of unsaturated se-containing osmacycles with σ-aromaticity. Chemistry. 2018;24:2389–2395. doi: 10.1002/chem.201703870. [DOI] [PubMed] [Google Scholar]
- 31.Ensafi AA, Dadkhah-Tehrani S, Karimi-Maleh H. Voltammetric determination of glutathione in haemolysed erythrocyte and tablet samples using modified-multiwall carbon nanotubes paste electrode. Drug Test Anal. 2012;4:978–985. doi: 10.1002/dta.347. [DOI] [PubMed] [Google Scholar]
- 32.Miyawaki A, Hijioka H, Ikeda R, Ishida T, Nozoe E, Nakamura N. Analysis of the outcome of concurrent neoadjuvant chemoradiotherapy with S-1 compared to super-selective intra-arterial infusion for oral squamous cell carcinoma. Oncol Lett. 2012;3:995–1001. doi: 10.3892/ol.2012.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feng X, Luo Q, Zhang H, Wang H, Chen W, Meng G, Chen F. The role of NLRP3 inflammasome in 5-fluorouracil resistance of oral squamous cell carcinoma. J Exp Clin Cancer Res. 2017;36:81. doi: 10.1186/s13046-017-0553-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim J, Chan JJ. Cyclophosphamide in dermatology. Australas J Dermatol. 2017;58:5–17. doi: 10.1111/ajd.12406. [DOI] [PubMed] [Google Scholar]
- 35.Olasz L, Orsi E, Markó T, Szalma J. Induction chemotherapy response and recurrence rates in correlation with N0 or N+ stage in oral squamous cell cancer (OSCC) Cancer Metastasis Rev. 2010;29:607–611. doi: 10.1007/s10555-010-9259-7. [DOI] [PubMed] [Google Scholar]
- 36.Blanchard-Fillion B, Prou D, Polydoro M, Spielberg D, Tsika E, Wang Z, Hazen SL, Koval M, Przedborski S, Ischiropoulos H. Metabolism of 3-nitrotyrosine induces apoptotic death in dopaminergic cells. J Neurosci. 2006;26:6124–6130. doi: 10.1523/JNEUROSCI.1038-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goodson HV, Jonasson EM. Microtubules and Microtubule-Associated Proteins. Cold Spring Harb Perspect Biol. 2018;10:a022608. doi: 10.1101/cshperspect.a022608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akhmanova A, Steinmetz MO. Control of microtubule organization and dynamics: Two ends in the limelight. Nat Rev Mol Cell Biol. 2015;16:711–726. doi: 10.1038/nrm4084. [DOI] [PubMed] [Google Scholar]
- 39.Magiera MM, Singh P, Gadadhar S, Janke C. Tubulin posttranslational modifications and emerging links to human disease. Cell. 2018;173:1323–1327. doi: 10.1016/j.cell.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 40.Janke C, Montagnac G. Causes and consequences of microtubule acetylation. Curr Biol. 2017;27:R1287–R1292. doi: 10.1016/j.cub.2017.10.044. [DOI] [PubMed] [Google Scholar]
- 41.Nieuwenhuis J, Brummelkamp TR. The tubulin detyrosination cycle: Function and enzymes. Trends Cell Biol. 2019;29:80–92. doi: 10.1016/j.tcb.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 42.Kalisz HM, Erck C, Plessmann U, Wehland J. Incorporation of nitrotyrosine into alpha-tubulin by recombinant mammalian tubulin-tyrosine ligase. Biochim Biophys Acta. 2000;1481:131–138. doi: 10.1016/S0167-4838(00)00110-2. [DOI] [PubMed] [Google Scholar]
- 43.Song W, Cho Y, Watt D, Cavalli V. Tubulin-tyrosine ligase (TTL)-mediated increase in tyrosinated α-tubulin in injured axons is required for retrograde injury signaling and axon regeneration. J Biol Chem. 2015;290:14765–14775. doi: 10.1074/jbc.M114.622753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rivelli JF, Ochoa AL, Santander VS, Nigra A, Previtali G, Casale CH. Regulation of aldose reductase activity by tubulin and phenolic acid derivates. Arch Biochem Biophys. 2018;654:19–26. doi: 10.1016/j.abb.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 45.Bajaj S, Roy PP, Singh J. 1,3,4-oxadiazoles as telomerase inhibitor: Potential anticancer agents. Anticancer Agents Med Chem. 2018;17:1869–1883. doi: 10.2174/1871521409666170425092906. [DOI] [PubMed] [Google Scholar]
- 46.Zugazagoitia J, Guedes C, Ponce S, Ferrer I, Molina-Pinelo S, Paz-Ares L. Current challenges in cancer treatment. Clin Ther. 2016;38:1551–1566. doi: 10.1016/j.clinthera.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 47.De Marchi P, Melendez ME, Laus AC, Kuhlmann PA, de Carvalho AC, Arantes LMRB, Evangelista AF, Andrade ES, de Castro G Junior, Reis RM, et al. The role of single-nucleotide polymorphism (SNPs) in toxicity of induction chemotherapy based on cisplatin and paclitaxel in patients with advanced head and neck cancer. Oral Oncol. 2019;98:48–52. doi: 10.1016/j.oraloncology.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 48.Fugazzola L, Muzza M, Pogliaghi G, Vitale M. Intratumoral genetic heterogeneity in papillary thyroid cancer: Occurrence and clinical significance. Cancers (Basel) 2020;12:383. doi: 10.3390/cancers12020383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mimoto R, Yogosawa S, Saijo H, Fushimi A, Nogi H, Asakura T, Yoshida K, Takeyama H. Clinical implications of drug-screening assay for recurrent metastatic hormone receptor-positive, human epidermal receptor 2-negative breast cancer using conditionally reprogrammed cells. Sci Rep. 2019;9:13405. doi: 10.1038/s41598-019-49775-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoffman RM, Tanino H. Clinical usefulness of the histoculture drug response assay for breast cancer. Methods Mol Biol. 2018;1760:93–100. doi: 10.1007/978-1-4939-7745-1_10. [DOI] [PubMed] [Google Scholar]
- 51.Franck S, Fuhrmann-Selter T, Joseph JF, Michelet R, Casilag F, Sirard JC, Wicha SG, Kloft C. A rapid, simple and sensitive liquid chromatography tandem mass spectrometry assay to determine amoxicillin concentrations in biological matrix of little volume. Talanta. 2019;201:253–258. doi: 10.1016/j.talanta.2019.03.098. [DOI] [PubMed] [Google Scholar]
- 52.Wu CP, Lusvarghi S, Tseng PJ, Hsiao SH, Huang YH, Hung TH, Ambudkar SV. MY-5445, a phosphodiesterase type 5 inhibitor, resensitizes ABCG2-overexpressing multidrug-resistant cancer cells to cytotoxic anticancer drugs. Am J Cancer Res. 2020;10:164–178. [PMC free article] [PubMed] [Google Scholar]
- 53.Dhiman N, Kingshott P, Sumer H, Sharma CS, Rath SN. On-chip anticancer drug screening-recent progress in microfluidic platforms to address challenges in chemotherapy. Biosens Bioelectron. 2019;137:236–254. doi: 10.1016/j.bios.2019.02.070. [DOI] [PubMed] [Google Scholar]
- 54.Mourelatos D. Sister chromatid exchange assay as a predictor of tumor chemoresponse. Mutat Res Genet Toxicol Environ Mutagen. 2016;803:1–12. doi: 10.1016/j.mrgentox.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 55.Zhang L, Li B, Zhang B, Zhang H, Suo J. miR-361 enhances sensitivity to 5-fluorouracil by targeting the FOXM1-ABCC5/10 signaling pathway in colorectal cancer. Oncol Lett. 2019;18:4064–4073. doi: 10.3892/ol.2019.10741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sticozzi C, Aiello F, Andreasi RB, Muresan XM, Belmonte G, Cervellati F, Maellaro E, Maioli E, Valacchi G. Antitubulinic effect of new fluorazone derivatives on melanoma cells. Anticancer Agents Med Chem. 2016;16:601–608. doi: 10.2174/1871520615666150909120014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.