Abstract
Acute kidney injury is a common complication in critically ill patients with sepsis and/or septic shock. Further, some essential antimicrobial treatment drugs are themselves nephrotoxic. For this reason, timely diagnosis and adequate therapeutic management are paramount. Of potential acute kidney injury (AKI) biomarkers, non-protein-coding RNAs are a subject of ongoing research. This review covers the pathophysiology of vancomycin and gentamicin nephrotoxicity in particular, septic AKI and the microRNAs involved in the pathophysiology of both syndromes. PubMED, UptoDate, MEDLINE and Cochrane databases were searched, using the terms: biomarkers, acute kidney injury, antibiotic nephrotoxicity, sepsis, miRNA and nephrotoxicity. A comprehensive review describing pathophysiology and potential biomarkers of septic and toxic acute kidney injury in septic patients was conducted. In addition, five miRNAs: miR-15a-5p, miR-192-5p, miR-155-5p, miR-486-5p and miR-423-5p specific to septic and toxic acute kidney injury in septic patients, treated by nephrotoxic antibiotic agents (vancomycin and gentamicin) were identified. However, while these are at the stage of clinical testing, preclinical and clinical trials are needed before they can be considered useful biomarkers or therapeutic targets of AKI in the context of antibiotic nephrotoxicity or septic injury.
Keywords: acute kidney injury, gentamicin, sepsis, miRNA, nephrotoxicity, vancomycin
1. Introduction
Acute kidney injury (AKI) is a common and mostly severe clinical syndrome complicating a number of critical illnesses. It has a highly negative impact on patient morbidity, mortality and clinical outcome. The diagnosis is generally based on evaluation of: (1) increase in serum creatinine and/or (2) decrease in urinary output. According to the KDIGO (Kidney Disease Improving Global Outcomes) classification of 2012, the severity of urinary output deterioration to terminal stages and presentation of an anuria and serum creatinine increase to 353.6 µmol/L is the most serious stage 3 [1]. Further, in 2017, new forms of acute renal impairment were described with AKI lasting at least 7 days after insult and acute kidney disease (AKD) lasting up to 90 days. Renal impairment and serum creatinine levels that had not returned to baseline levels by 90 days resulted in the need for renal replacement therapy (RRT) and/or progression to chronic kidney disease (CKD) [2]. Timely AKI diagnosis, especially in critically ill patients, would enable clinicians to better initiate preventive measures to avoid the need for RRT and obviate the risk of CKD. A number of promising new biomarkers may be able to predict the development or worsening of AKI in intensive care. The most highlighted of these in recent years are noncoding microRNAs in these circumstances. This review focuses on the pathophysiology and potential biomarkers in the detection of AKI after nephrotoxic drugs and/or septic insults with emphasis on specific microRNAs.
2. Epidemiology of Acute Kidney Injury
Acute kidney injury is a relatively frequent complication in critically ill patients in ICUs, especially in those with sepsis. The incidence of AKI in these circumstances, predominantly in situations with presentation of septic shock, may be as high as 47.5% and the overall mortality in critically ill patients with AKI may be more than 60% [3]. According to recent results of a multicenter Chinese study of patients hospitalized in ICUs, the incidence of AKI was 51%, with the majority occurring on the 4th day after admission [4]. A number of factors can contribute to AKI and progression to renal failure, including cardiovascular and hepatic disorders, malignancies, hypovolemia, intoxication, drug nephrotoxicity, anemia and surgical and vascular interventions. Further, many such patients need nephrotoxic iodine contrast drugs for CT scans and other radiological examinations. Therefore, the AKI is often a consequence of multiple factors.
3. Pathophysiology of Sepsis-Induced Acute Kidney Injury
Sepsis is generally characterized as a life-threatening condition induced by any type of infection (e.g., bacterial, viral, mycotic) and the dysregulated response of the host organism, with subsequent organ and tissue dysfunction or failure. The diagnosis has recently been redefined according to the SEPSIS-3 consensus (The Third International Consensus Definitions for Sepsis and Septic Shock) as an increase in the SOFA (Sequential Organ Failure Assessment) score of 2 points or more. For earlier clinical decision-making, the Quick SOFA (qSOFA) criteria can be used as evaluation of: altered mental status, a respiratory rate of 22/min or greater and a systolic blood pressure of 100 mmHg or less [5]. The pathophysiology of sepsis-induced AKI appears to be multifactorial, including, among others, deleterious inflammatory cascade [6]. Underlying explanations of septic AKI development include: (1) alteration of the renal macro- and microcirculation, with subsequent endothelial dysfunction, (2) damage of renal tubular epithelial cells, (3) a change in cellular metabolic pathways and energy consumption, (4) mitochondrial injury, (5) reactive oxygen species (ROS) production and (6) cycle cell arrest [7]. However, the exact mechanism of septic AKI is still unclear. Increase in inflammatory cytokine production and activation of leukocyte activity in the context of a dysregulated immunological and inflammatory response can lead to production of intravascular microthrombi and also reduce intrarenal blood flow and oxygen delivery [8]. Regulation of the immune and adaptive immunity response in renal tubular cells occurs due to activation of the Toll-like receptor (TLRs) family in the cell membrane. There are more than 13 members of this family and they are usually activated by endotoxins. They recognize pathogen-activated molecular patterns (PAMPs) and damage-associated pathogens (DAMPs) with the promotion of leukocyte and intrinsic renal cell activation. Renal tubular cells express TLR-1, -2, -3, -4 and -6, which can be substantially involved in the pathophysiology of tubular cell damage [9,10]. The most important receptor in septic AKI pathophysiology appears to be TLR-4, that can bind the endotoxin lipopolysaccharide (LPS), leading to activation of a number of intracellular signaling pathways via the nuclear-κB (NF-κB) transcription factor. NF-κB response to endotoxin stress leads to activation and release of the inflammatory cytokines TNFα, IL-1, IL-6 and IL-8 [11]. The activation of NF-κB depends on the phosphorylation and degradation of inhibitory κB proteins, triggered by specific kinases [9]. The basic explanation of the pathophysiological pathway in septic AKI development via activation of TLR-4 receptors in proximal tubular cells very likely lies in dysregulation of tubular integrity, with induction of tight junction disruption. This process may contribute to subsequent oliguria and decrease in renal function [12]. A recent animal study (Nakano et al., 2020), where conditional knockout of TLR-4 in proximal tubular cells reduced LPS-induced paracellular leakage of filtrate into the interstitium via TLR-4 showed that the interstitial leakage and accumulation of extracellular fluids lead to anuria and diminished the efficacy of volume resuscitation, which is frequently used in septic AKI to restore renal function [13].
4. Biomarkers of Sepsis-Induced Acute Kidney Injury
Many potential biomarkers have been studied in recent years in the context of sepsis and septic AKI. These can be divided into: (1) standard biomarkers, (2) additional urinary and/or serum biomarkers, (3) metabolomics, (4) other experimental proteomics and (5) microRNAs (miRNAs). Generally, AKI is diagnosed by the standard use of serum creatinine concentration and urinary output, as mentioned, with additional evaluation of serum concentration of urea. In addition, we can include Neutrophile gelatinase-associated lipocalin (NGAL), Cystatin C, Kidney Injury Molecule -1 (KIM-1), Interleukin 18 (IL-18), urinary Insulin-like growth factor-binding protein-7 (IGFBP-7), urinary tissue inhibitor of metalloproteinase 2 (TIMP-2), calprotectin, urine angiotensinogen and liver fatty acid binding protein [14]. In clinical practice, especially in patients with AKI in ICUs, it is very useful to have a biomarker capable of predicting the need for RRT initiation, renal recovery or transition to chronic nephropathy. According to a meta-analysis of 63 studies comprising 15,928 critically ill patients, the best evidence was for blood NGAL and Cystatin C followed by urinary TIMP-2 and IGFBP-7 [15]. However, decision-making in the case of RRT initiation is based on a number of clinical and laboratory findings, not only biomarkers, and none of these is specific to any particular type of AKI [16]. The major limitation of biomarkers in the AKI condition lies in comparing biomarkers to serum creatinine and diuresis, the basic diagnostic tools for AKI [17].
In recent experimental animal models of septic AKI, some potential novel metabolomic biomarkers have been identified using nuclear magnetic resonance spectroscopy on urine, renal tissue and in serum. Alterations in the concentration of several metabolites have been found e.g., lactate, N-acetylglutamine, alanine, pyruvate, myoinositol, glutamine, valine, glucose, ascorbic acid, aminoadipic acid, N-acetylaspartate and betaine and these correlate with serum creatinine and NGAL [18]. Further, many heat shock proteins (HSP) families and their bioactivity are described in various kidney diseases. In ischemic, toxic or other forms of AKI, the following have been found expressed in several renal cell types (podocytes, mesangial cells, tubular cells, fibroblasts, endothelial cells, macrophages): HSP27, HSP70, HSP60, HSP47, HSP90 and HSP32 [19]. Their main role in renal cytoprotection is still under investigation. However, many of them can block the apoptotic death pathway, oxidative stress, cell proliferation and differentiation, mediation of the inflammatory response and inhibit fibrogenesis [19]. A study of 56 critically ill patients, where 17 of them suffered from AKI, revealed that urinary HSP72 levels significantly increased in the period of three days before AKI and remained elevated during AKI diagnosis [20].
5. MiRNAs as Biomarkers of Septic Acute Kidney Injury
Research is currently focused on miRNAs as new potential biomarkers and/or therapeutic tools for many conditions including AKI. MiRNAs are small molecules (18–31 nucleotides) of noncoding RNAs, representing a large part of genetic information not translated from the DNA matrix into final protein production. The evidence of their abundance, developmentally regulated fashion and often subcellular localization points to their important biological role in many biochemical and pathophysiological processes and pathways on the cellular and molecular level [21]. Influence on post-transcriptional gene regulation, cell metabolism, cytokine production, cell differentiation and programmed cell death are only a small percentage of miRNAs’ effects and their target genes. In the AKI condition, some act protectively and can become potential therapeutic targets but others can increase the toxic activity and renal damage. Anti-inflammatory and/or anti-apoptotic activity in AKI has been described for the following miRNAs: miR-10a, miR-21, miR-26a, miR-122, miR-126, miR-146a, miR-199a, miR-296 and miR-494 [22]. Some miRNAs involved in the pathophysiological inflammatory process of sepsis based on endotoxin (LPS) activation of TLR4 in the signaling pathway of NF-κB activation, pro-inflammatory cytokine production (IL-6, IL-1β, TNFα) and subsequent neutrophil activation, damage of endothelial permeability and tissue injury are: miR-146 a/b, miR-223, miR-155, miR-203, miR-15a, miR-16, miR-126, miR-199a and miR-9. Each regulates positively or negatively a different part of the biochemical cascade to final cytokine production and tissue damage according to their target genes [23,24]. In the development of septic AKI, severe metabolic alterations of tubular epithelial cells may play a crucial role via miR-21-3p influence on the AKT/CDK2-FOXO1 pathway, with induction of cycle cell arrest and apoptosis [25]. According to one human study (Ge et al., 2017), many other signaling pathways are involved in septic AKI development, including oxidative stress and mitochondrial dysfunction pathways (HIF-1, PI3K-Akt, mTOR and TGFβ). In septic, critically ill patients, significantly overexpressed miR-4321 was observed, with the predicted oxidative-stress-associated target genes: AKT1, MTOR, NOX5, IL17RA and IL26 [26]. The mitochondrion is assumed to be a key organelle in the development of septic acute kidney injury, and has major pathophysiological significance in ROS production and apoptosis [27]. In one hybrid human and experimental study including 50 patients with sepsis, an effect was found of miR-106a on caspase-3 activity, BCl-2 expression and proinflammatory cytokine production after LPS stimulation [28]. The authors found an association between miR-106a and an aggravation of LPS-induced inflammation, and apoptosis in sepsis-induced AKI. A target gene for miR-106a was established as thrombospondin THBS2, which takes part in a number of processes such as regulation of cell motility, death and cytoskeleton formation [28].
6. Medication-Induced AKI in Septic Patients
Drug-induced nephrotoxicity varies from a relatively mild form of acute tubulointerstitial nephritis (ATIN), several types of glomerulonephritis, crystal nephropathy and osmotic nephrosis to acute tubular necrosis represented mostly by severe renal impairment with the need for RRT. The last-mentioned may be associated with development of chronic nephropathy and the need for chronic hemodialysis treatment. The incidence of medication-associated nephrotoxicity accounts for approximately 18–27% of all AKI patients in US hospitals—the main causative drugs are NSAIDs, aminoglycosides, amphotericin B and calcineurin inhibitors [29].
Potentially nephrotoxic medications, which are considered essential and commonly used in sepsis and critically ill patients, are antimicrobial agents (antibiotics, antiviral and antifungal treatment), human albumin in septic shock or proton pump inhibitors to prevent stress ulcers [30] (Table 1). Iodine contrast agents are used for radiocontrast imaging examinations in septic, critically ill patients when there is need for sepsis source finding or surgical interventions [31].
Table 1.
| Medications (Agents) | Clinical and Histological Presentation of Renal Toxicity |
|---|---|
|
Antimicrobials Aminoglycosides Glycopeptides (vancomycin) Polymyxins |
acute tubular necrosis, apoptosis, necroptosis, acute oxidative stress, cycle cell arrest |
|
Antimicrobials β-lactams Sulphonamides Macrolides Antiretrovirals (Acyclovir) Rifampin Fluoroquinolones Chloramphenicol Other medications Diuretics NSAIDs Proton pump inhibitors |
acute tubulointerstitial nephritis |
| Sulphonamides Antiretrovirals |
acute crystalline nephropathy |
| High-osmolar iodine radiocontrast agents Hydroxyethyl starches and gelatine solutions |
increase in ROS production, vasoconstriction, osmotic nephrosis |
| NSAIDs | altered renal hemodynamics |
NSAIDs—nonsteroidal anti-inflammatory drugs, ROS—reactive oxygen species.
The nephrotoxicity of some antimicrobial drugs is a common problem. Of these, the most nephrotoxic are: vancomycin, aminoglycosides and polymyxins, which cause acute tubular necrosis and apoptosis depending on dose, among other factors. Many antimicrobials and other drugs frequently used in critically ill patients can also cause ATIN, accounting for 60–70% of all ATIN cases [32].
7. Vancomycin-Induced Nephrotoxicity Pathophysiology and Biomarkers
Vancomycin is a glycopeptidic antimicrobial agent with substantial bactericidal effect on Gram-positive bacterial infections and is frequently used in the treatment of Methicillin-resistant Staphylococcus aureus (MRSA). It also acts against Streptococcus sp., Enterococcus sp., Actinomyces sp., Clostridium sp. and Eubacterium sp. Its pharmacokinetics and pharmacodynamics are time-dependent, but according to recommendations for vancomycin treatment, the best parameter for evaluating its efficacy is the ratio of the 24 h area under the curve (AUC) to the minimum inhibitory concentration of AUC/MIC ≥400 mg.h/L with an MIC of pathogen <2 mg/L [37,38]. Vancomycin is not metabolized in the human body and is eliminated renally by glomerular filtration. Its binding to plasma proteins is less than 50%, the elimination half-life ranges from 6 to 12 h and volume of distribution is 0.4–1.0 L/kg [37]. The recently revised consensus guidelines of the American Society of Health-System Pharmacists for vancomycin therapy and monitoring for serious MRSA infections (2020) recommends, in adults and pediatric patients, a daily AUC/MIC ratio between 400 to 600 mg.h/L. A higher loading dose (20–25 mg/kg based on actual body weight) should be considered in critically ill patients treated by any type of RRT or in need of continuous vancomycin infusion. In obese patients with serious infections, the maximum loading dose is 3000 mg intravenously [39]. However, vancomycin nephrotoxicity with risk of AKI development is usually associated with higher vancomycin exposure, as measured by AUC0–24. Additionally, a significantly increased risk for nephrotoxicity has been observed in patients with AUC0–24 of 563 mg.h/L [40]. However, higher trough vancomycin serum concentrations >16.5 mg/L are also at greatest risk for new onset of AKI in critically ill patients [41]. In these cases, it is very difficult, in clinical practice, to maximize antibiotic efficacy, and, at the same time, to minimize its nephrotoxicity. The pathophysiology of vancomycin nephrotoxicity has been intensively investigated mostly in experimental research. Sakamoto et al. (2017) uncovered the possible nephrotoxic effect based on peroxidation of the mitochondrial membrane cardiolipin by vancomycin-induced production of intracellular ROS and activation of apoptosis in proximal tubular cells [42]. Apoptotic cell death induced by vancomycin may be associated with activation of specific caspases: caspase 9 and caspase 3/7 and extensive ROS production [34]. In the prospective multicenter Sapphire study (NCT01209169 ClinicalTrials.gov) including 723 critically ill adult patients, the pharmacokinetics of two urinary biomarkers TIMP-2 and IGFBP7 were evaluated in patients receiving vancomycin, piperacilin-tazobactam, or their combination. The concentration of biomarkers and the risk of death or need for dialysis treatment within 9 months, were the highest in the combination group. However, the AKI progression to an aggravated stage 2/3 was comparable in vancomycin monotherapy and in the combination treatment [43]. Selected urinary AKI biomarkers—clusterin, cystatin C, NGAL/lipocalin-2, osteopontin and KIM-1—were investigated in animals receiving vancomycin. A higher vancomycin exposure presented by an AUC0–24 and maximum serum concentration significantly correlated with increase in urinary AKI biomarkers but did not correlate with histopathological score [44]. Serum creatinine, urinary NGAL and KIM-1 were measured in 87 patients without chronic kidney disease (12.6% developed AKI) before and during the vancomycin therapy. According to the results, both urinary biomarkers NGAL and KIM-1 successfully discriminated patients with and without vancomycin-induced AKI earlier than serum creatinine [45]. However, in one animal study (Pais et al., 2019) KIM-1 and clusterin were more sensitive to vancomycin-induced AKI than NGAL [46].
One possible explanation for vancomycin-induced AKI and tubular cell apoptosis is based on DNA methylation by activation of Methyl-CpG binding domain protein 2 (MBD2). Experimental inhibition of MBD2 can downregulate miR-301-5p with subsequent restoration of anti-apoptosis gene expression e.g., hepatoma-derived growth factor (HDGF) and microphthalmia-associated transcription factor (MITF) and can increase MDM-4 expression for reduction of p53 [47].
8. Gentamicin-Induced Nephrotoxicity Pathophysiology and Biomarkers
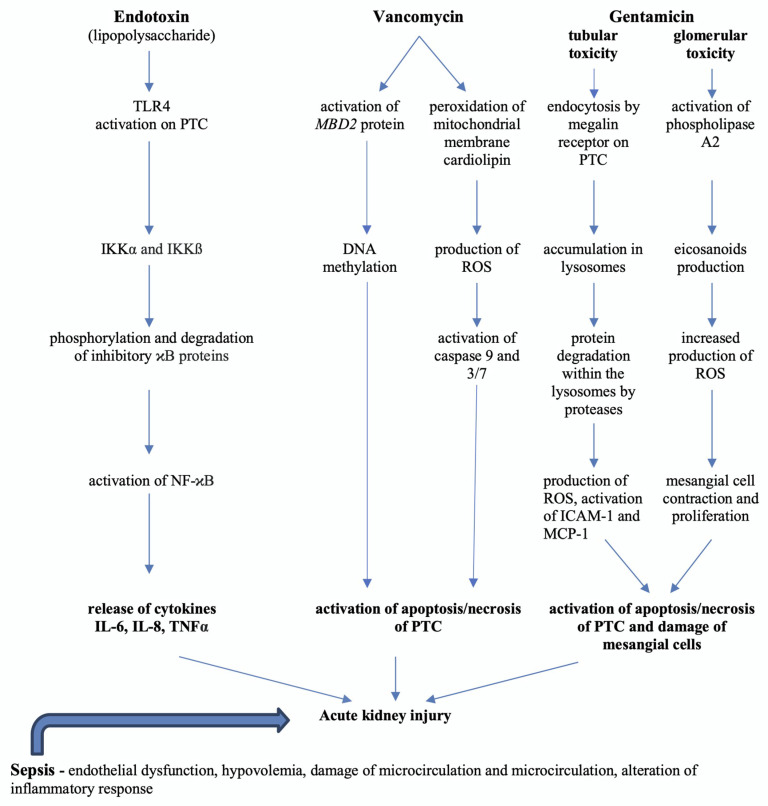
Gentamicin is an aminoglycoside concentration-dependent antibiotic agent with bactericidal effects against Gram-negative bacterial pathogens e.g., Escherichia coli, Pseudomonas aeruginosa, Proteus and Klebsiella. Renal elimination by glomerular filtration is the predominant type of removal of unchanged gentamicin from the human organism. Gentamicin enters to some extent the proximal tubular cells, where it is accumulated in the lysosomes with alteration of their enzymes [48]. The gentamicin volume of distribution is, approximately, an equivalent to the extracellular body weight, and it generally decreases with age. The gentamicin elimination half-life in adults with physiological renal function is very short and ranges between 2 and 3 h [49]. The incidence of acute renal failure during gentamicin treatment can account for approximately 10–20% of all cases [50]. The nephrotoxicity of gentamicin is a very complex pathophysiological process with both tubular and glomerular involvement (Figure 1). Besides the cellular uptake in proximal convoluted cells and acute tubular necrosis, it can induce mesangial cell contraction and proliferation mediated by platelet-activating factor and also an increase in free intracellular calcium concentration. Moreover, it can induce activation of the phospholipase A2 enzyme and increased production of eicosanoids in mesangial cells, production of ROS and mesangial cell apoptosis [51]. For early detection of progression from minimal to moderate kidney injury in animals treated by gentamicin, the urinary biomarkers clusterin, KIM-1, Cystatin C and NGAL were compared to serum BUN and creatinine. As predictable, all of these biomarkers showed earlier onset changes than the generally used serum BUN and creatinine in AKI diagnosis [52]. Another explanation of gentamicin nephrotoxicity is experimental evaluation of toxicity biomarkers through specific gene expression associated with apoptosis or cell necrosis. Of 10 analyzed genes associated with apoptosis, in four, TP53, CASP3, CASP8 and CASP9, an increase in expression was found. In addition, the regulation of these genes produced proteins capable of cleaving specific substrates leading to cell death. Moreover, a decrease in antiapoptotic genes e.g., BCL2L1 has been found [53]. In an experimental study carried out on drug-induced, predominantly tubular (gentamicin and cisplatine) and glomerular (puromycin and doxorubicin) kidney injury, among several commonly downregulated miRNAs, miR-143-3p and miR-122-5p were proposed as potential tubular and miR-3473 as glomerular biomarker candidates [54].
Figure 1.
Simplified pathophysiology of acute kidney injury development in sepsis and selected antibiotic treatment [6,10,42,47,48,51,55,56]. DNA—deoxyribonucleic acid, ICAM-1—intercellular adhesion molecule-1, IKK—I-kinase, IL-6—interleukin 6, IL-8—interleukin 8, MBD2—Methyl-CpG Binding Domain Protein 2, MCP-1—monocyte chemoattractant protein 1, NF-κB—nuclear factor—kappa B, PTC—proximal tubular cells, ROS—reactive oxygen species, TLR4—Toll-like receptor 4, TNFα—tumor necrosis factor alpha
9. MicroRNAs Associated with AKI Induced by Sepsis or Nephrotoxic Antibiotic Therapy
9.1. miR-15a-5p
The pathogenesis of sepsis AKI development is challenging, and many miRNAs likely participate in the pathophysiological and biochemical pathways involved. MiR-15a-5p in a regulatory axis with XIST (X inactive specific transcript)/CUL3 (cullin 3 gene) in septic AKI was investigated in a combined human and animal study from China with LPS as the endotoxin. The lipopolysaccharide inhibited the growth of animal podocytes besides the upregulation of XIST and CUL3 and downregulated miR-15a-5p. The inhibition of XIST and miR-15a-5p enhanced and preserved LPS-induced apoptosis significantly, while the miR-15a-5p inhibitor reversed the renal cell apoptosis. Furthermore, overexpression of the CUL3 gene considerably reduced the LPS and miR-l5a-5p-induced apoptosis [57]. Another explanation of sepsis pathophysiology is based on regulation of the crucial inflammatory response of damaged organs with the participation of miR-15a-5p. In one animal study (Lou et al., 2020), after the LPS stimulation of macrophages there was an increased expression of miR-15a-5p and a release of inflammatory cytokines IL-6, IL-1ß and TNFα in comparison to a control group. Moreover, it has been demonstrated that inhibition of miR-15a-5p can decrease the secretion of proinflammatory cytokines by blocking its targeting gene, TNFα induced protein 3-interacting protein 2 (TNIP2), and the NF-κB signaling pathway [58]. MiR-15a-5p regulates many genes affecting angiogenesis, hematopoietic cells and carcinogenesis and has the effect of suppressing inflammation and fibrosis of peritoneal mesothelial cells induced by peritoneal dialysis [59,60,61].
9.2. miR-192-5p
In a human study of critically ill patients with sepsis or the nonseptic systemic inflammatory response syndrome, miR-192-5p was one of six of the most important circulating RNAs that differentiated sepsis from the nonseptic inflammatory response. MiR-192-5p negatively correlated with concentrations of pro-inflammatory cytokines (IL-6, IL-1 and IL-8) and sepsis markers (e.g., CRP). However, no correlation between the miR-192-5p concentration and the generally used SOFA score was found [62]. In a proceeding human study, a positive correlation was revealed between miR-192-5p and the redox biomarker, peroxiredoxin-1, which is released by immune cells during inflammation [63]. Urinary miR-192-5p was studied in animals with ischemia-reperfusion-induced AKI, where its expression in urine was significantly elevated after the ischemic intervention. The results were validated with urine samples from 71 patients who underwent cardiac surgery. The elevation of miR-192-5p was detected earlier than KIM-1, that was previously established as a renal injury biomarker [64]. Some other experimental studies on miR-192-5p and renal diseases in association with diabetes, hypertension and drug nephrotoxicity, can be added to the complex clinical and pathophysiological review. For example, circulating RNA HIPK3 (homeodomain-interacting protein kinase 3) can bind miR-192-5p with upregulation of transcription factor FOXO1 (forkhead box protein O1) leading to hyperglycemia and insulin resistance [65]. In the kidney, miRNA-192-5p contributes to protection against hypertension through the target gene ATP1B1 (β1 subunit of Na+/K+-ATPase), and miR-192-5p levels are significantly decreased in humans with hypertension or hypertensive nephrosclerosis [66]. Conversely, there is contrasting data on the kidney-protective role of miR-192-5p in association with vancomycin-induced AKI. The antagonism of vancomycin-induced miR-192-5p by the miRNA inhibitor led to a decrease of apoptosis in HK2 cells. Moreover, inhibition of p53 can attenuate apoptosis by suppressing miR-192-5p in vancomycin-induced AKI [67].
9.3. miR-155-5p
According to the literature, miR-155 plays a critical role in various pathological and physiological processes, including immunity, inflammation, infection, cancers, hematopoietic cell differentiation, cardiovascular diseases and some genetic malformations [68].
The effects of activation and suppression of miR-155-5p in relation to various renal diseases and in sepsis have been investigated in a number of experimental studies [69,70]. Its role in the inflammatory process has been recently studied in an in vitro model of sepsis where inhibition of miR-155-5p reduced the expression of IL-6 and IL-8 as pro-inflammatory cytokines by 31% and 14%, respectively. Moreover, its inhibition can reduce the release of heat shock proteins, such as HSP10, by 69%. The latter is released from damaged cells as a stress signal [69]. The HSP10 inhibits lipopolysaccharide-induced inflammatory mediator production and NF-κB activation by inhibiting Toll-like receptor signaling in cell membranes [71]. Endogenous miR-155 participates on regulation of inflammation and is released from dendritic cells within exosomes. It is subsequently taken up by recipient dendritic cells. Exosomal miR-155 promoted endotoxin-induced (LPS) inflammation in one study (Alexander et al., 2015) by an increase in TNFα and subsequent increase in IL-6 serum concentration [70]. Gentamicin-induced nephrotoxicity and ischemia-reperfusion injury resulted in increased miR-155 and miR-18 in one rodent study [72]. With a higher dose of gentamicin, more significant injury and necrosis of renal epithelial cells were observed. However, contrary to ischemic injury, with the higher dose of gentamicin (300 mg/kg), both miRNAs decreased in the urine and increased in the renal cortex and medulla. The range of miR-155 target genes is very high, and includes genes for the regulation of e.g., mitochondrial processes, lipid metabolism, kinase-apoptotic pathways and cell proliferation [72].
Experimental modulation of gene expression in salt-sensitive hypertensive animals showed the important role of circular RNAs in the development of hypertensive kidney injury. The authors of one study (Lu et al., 2020) characterized a circular RNA called circNr1h4 derived from the Nr1h4 (nuclear receptor subfamily 1, group H, member 4) gene that binds to miR-155-5p and regulates expression of its target gene—fatty acid reductase 1 (Far1). The reaction between miR-155-5p and circNr1h4 is basically competitive, where the silencing of circNr1h4 or overexpression of miR-155-5p considerably decreased Far1 levels and increased ROS production. Therefore, miR-155-5p may be involved in the pathology of hypertensive kidney injury [73]. The involvement of miR-155-5p in the pathophysiological pathway to the development of diabetic kidney disease is probably explained by the signaling axis of p53 and sirt1 genes with regulation of autophagic and fibrotic processes in renal tubular injury. MiR-155-5p may be involved in the promotion of renal fibrosis under hypoxia and also in high blood glucose concentration, and is transcriptionally regulated by p53. This allows participation in the regulation of cell growth, the cell cycle, differentiation and apoptosis [74].
9.4. miR-486-5p
One of the most serious causes of acute kidney injury is ischemia-reperfusion injury, often resulting in tubular cell necrosis or apoptosis. In one experimental study (Viñas et al., 2016), the effect of exosomes with miR-486-5p derived from endothelial colony-forming cells (ECFCs) on protection against kidney injury was investigated in mice with induced renal ischemia. Infusion of ECFC exosomes into ischemic endothelial kidney cells had a strong functional and histological protective effect, associated with increased kidney miR-486-5p levels, decreased phosphatase and tensin homolog (PTEN) and activation of the Akt pathway [75]. In chronic kidney disease, miR-486-5p inhibits the forkhead transcription factor FOXO1 by downregulation of PTEN phosphatase, a negative regulator of Akt. FOXO1 appears to be the predominant mediator of muscle wasting in chronic nephropathy, accelerated by stimulating the ubiquitin proteasome system through activation, e.g., E3 ligases [76]. In one human study (Regmi et al., 2019) involving patients with diabetic nephropathy, decreased serum concentrations of miR-486-5p were found and, this negatively correlated with albuminuria, levels of fasting blood glucose and glycated hemoglobin [77].
The association between LPS-induced inflammation and miR-486-5p with target FOXO1 has been studied in vitro in nucleus pulposus cells and intervertebral disc degeneration. Experimentally, it was shown that miR-486-5p overexpression led to a decrease of LPS-induced production of inflammatory cytokines IL-1ß, IL-6 and TNFα and protected the nucleus pulposus cells against apoptosis [78].
9.5. miR-423-5p
Ischemia-reperfusion-induced AKI is one possible pathophysiological process, in which miR-423-5p may be substantially involved, along with other circulating miRNAs. Experimentally, it has been shown that miR-423-5p induces endoplasmic reticulum stress and reactive oxidative stress by inhibiting the GSTM1 (Glutathione-S-Transferase Mu 1) gene which encodes the glutathione-S-transferase M1 enzyme in ischemia-reperfusion injury [79]. Glutathione-S-transferase is a very potent detoxification enzyme that protects the renal tubular cells against oxidative stress and ROS. The considerable involvement of miR-423-5p in the regulation and activation of NF-κB signaling by the TNIP2 gene has been demonstrated in patients with lupus nephritis [80]. The TNIP2 gene increases IKKα kinase activity and phosphorylation and induces NF-κB target genes [80]. The exact pathogenesis and factors contributing to renal cell injury here are still under investigation. MiR-423-5p is postulated to suppress podocyte injury in conditions of high blood glucose levels. Overexpression of miR-423-5p by negatively regulated Nicotinamide adenine dinucleotide phosphate oxidase-4 (NOX4) gene can antagonize high glucose-induced podocyte injury. Moreover, it inhibits ROS production, cell apoptosis, inflammation and subsequent damage of renal cells [81].
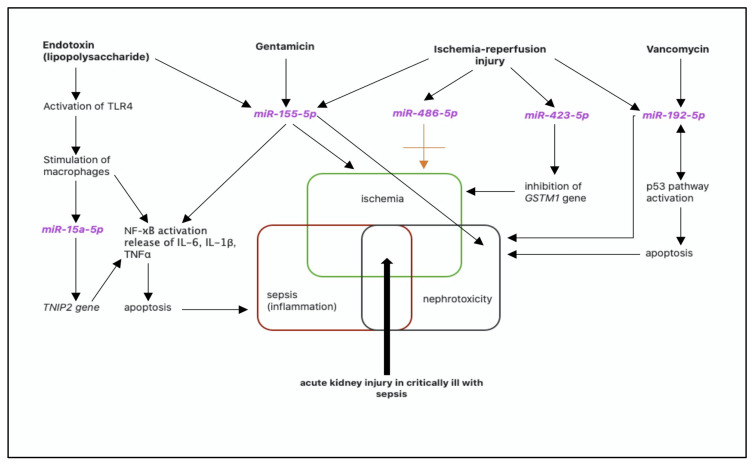
The schematic pathophysiology of acute kidney injury in a critically ill patient with sepsis and nephrotoxic antibiotic treatment with selected miRNAs is presented in Figure 2.
Figure 2.
Schematic pathophysiology of acute kidney injury in a critically ill patient with sepsis and nephrotoxic antibiotic treatment with selected miRNAs. AKI—acute kidney injury, GSTM1—glutathione-S-transferase Mu 1 gene, IL-6—interleukin 6, IL-1ß—interleukin 1ß, NF-κB—nuclear factor—kappa B, TNFα—tumor necrosis factor alpha, TNIP2—tumor necrosis factor alpha induced protein 3-interacting protein 2, TLR4—Toll-like receptor 4.
10. Therapeutic Approaches in Septic Patients with AKI
In the therapeutic approach to AKI in septic critically ill patients, it is essential for clinicians to decide between conservative or invasive measures. The first step is generally the treatment of sepsis by wide-spectrum antimicrobial agents, according to the epidemiologically assumed microbial [30]. Accordingly, there is a need to consider surgical or other intervention to eliminate the potential source of the sepsis. AKI severity, clinical and hemodynamic status as well as metabolic alterations are the basics for RRT or conservative therapy. Many experimental AKI biomarkers including miRNAs have an ancillary role in AKI diagnosis to assist clinicians in decision-making, in primarily preventive approaches. Usually this means dose adjustment of the nephrotoxic agents, stabilization of hemodynamics with controlled volume expansion if needed, preservation of urine output, adequate nutrition and treatment of any metabolic disorder. The crucial use of additive AKI biomarkers besides serum creatinine and urea, are the subject of ongoing research. During the first phase of septic AKI, of clinical importance is optimization of fluid management with adequate fluid resuscitation and avoidance of fluid overload. Physicians have to take into account patient’s volume status, urinary output, the type of intravenous fluids and infusion rates [82]. However, fluid overload due to loss of plasmatic proteins and increase in capillary permeability, can lead to fluid accumulation with a worsening of patient clinical status. In the renal parenchyma this increases the renal venous pressure, reduces the renal perfusion pressure and glomerular filtration rate with consequent retention of salt and water [83]. Fluid resuscitation with hemodynamic stabilization and choice of fluids play an important role in the therapeutic approach to both syndromes—sepsis and AKI. The preferred solutions are saline and balanced crystalloids, whereas hydroxyethyl starches and gelatin solutions can be associated with increased risk of AKI in septic patients. In the presence of septic shock, despite adequate volume resuscitation, there is a need for vasoactive drugs to restore renal parenchymal perfusion. In the case of sepsis, for this reason, commonly used drugs are norepinephrine, dopamine, vasopressin and phenylephrine [84].
With severe AKI, metabolic alterations and worsening hemodynamic instability, there is usually an increased need for RRT initiation in intermittent (IRRT) or continuous (CRRT) form. In physical principle and type of RRT or blood purification techniques, there are dialysis, hemofiltration, hemodiafiltration, hemoadsorption by CytoSorb (for severe sepsis) or plasmapheresis. Some RRT methods can be also combined according to clinical or laboratory findings. Close patient status monitoring and adequate supportive measures in cases with absence for urgent RRT initiation are the basic steps in conservative approaches. Thus, the timing for RRT initiation does not play a substantial role in survival in critically ill patients with AKI, especially in cases where conservative approaches can be successfully used [85]. A more comprehensive view was achieved after termination of the French AKIKI (Artificial Kidney Initiation in Kidney Injury) study (ClinicalTrials.gov NCT 01932190) performed in 620 critically ill patients with acute kidney injury. No significant difference in mortality between early and delayed strategies of RRT initiation with a decrease in need for RRT in the delayed approach was found [86]. Hemoadsorption with CytoSorb can be used predominantly in patients suffering from septic shock with careful decision-making, according to the APACHE II score. The basic principle of these blood purification devices, using more effective membranes or columns incorporated in CRRT, is removal of pro-inflammatory cytokines (e.g., IL-6, IL-8, TNFα) and endotoxins to stabilize the patient’s hemodynamics and decrease the need for vasopressor therapy [87]. Preserving adequate fluid balance, net ultrafiltration, treatment dose, nutritional support and antibiotic treatment are a vital component of the therapeutic approach in critically ill septic patients [88].
In patients with septic AKI on any type of RRT treatment, what is crucial is the antimicrobial treatment and therapeutic drug monitoring where possible. Many renally eliminated antimicrobial agents in these circumstances undergo changes in pharmacokinetics/pharmacodynamics parameters, including clearance, volume of distribution, binding to plasma proteins and elimination half-life. The dose adjustment has to be individualized according to serum concentration, to achieve the required pharmacodynamics parameters, drug efficacy and decrease the risk of toxicity [89,90]. Other preventive measures such as antioxidants in the case of antibiotic nephrotoxicity are still under investigation.
11. Conclusions
The early diagnosis of AKI, adequate preventive and therapeutic approaches in critically ill septic patients, are still a challenge for clinicians. Some experimental AKI biomarkers are undergoing research to help clinicians with essential, timely detection of renal injury. However, to date, there is no specific biomarker for particular toxic, septic or ischemic renal damage. None of them is able to distinguish between specific insult causing the AKI. For this reason, there is considerable current attention on miRNAs and their pathophysiological role in the human organism.
Author Contributions
N.P. wrote the main text of the manuscript, conceived and designed the underlying scientific project, A.M., J.Z. and D.S. reviewed the manuscript, I.K. contributed with pharmacological consultations, Z.S. and R.S. contributed with biochemical consultations. V.K. collected the scientific research data, M.K. and V.H. contributed with intensive care consultations. All authors have read and agreed to the published version of the manuscript.
Funding
The project is supported by the Ministry of Health Czech Republic—conceptual development of research organization (01-RVO-FNOs/2019).
Conflicts of Interest
The authors declare no conflict of interest related to this manuscript or project.
References
- 1.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int. Suppl. 2012;2:1–138. [Google Scholar]
- 2.Chawla L.S., Bellomo R., Bihorac A., Goldstein S.L., Siew E.D., Bagshaw S.M., Bittleman D., Cruz D., Endre Z., Fitzgerald R.L., et al. Acute kidney disease and renal recovery: Consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat. Rev. Nephrol. 2017;13:241–257. doi: 10.1038/nrneph.2017.2. [DOI] [PubMed] [Google Scholar]
- 3.Uchino S., Kellum J.A., Bellomo R., Doig G.S., Morimatsu H., Morgera S., Schetz M., Tan I., Bouman C., Macedo E., et al. Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 4.Jiang L., Zhu Y., Luo X., Wen Y., Du B., Wang M., Zhao Z., Yin Y., Zhu B., Xi X. Epidemiology of acute kidney injury in intensive care units in Beijing: The multi-center BAKIT study. BMC Nephrol. 2019;20:468. doi: 10.1186/s12882-019-1660-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D., Bauer M., Bellomo R., Bernard G.R., Chiche J.D., Coopersmith C.M., et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poston J.T., Koyner J.L. Sepsis associated acute kidney injury. BMJ. 2019;364:k4891. doi: 10.1136/bmj.k4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gómez H., Kellum J.A. Sepsis-induced acute kidney injury. Curr. Opin. Crit. Care. 2016;22:546–553. doi: 10.1097/MCC.0000000000000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ronco C., Bellomo R., Kellum J.A. Acute kidney injury. Lancet. 2019;394:1949–1964. doi: 10.1016/S0140-6736(19)32563-2. [DOI] [PubMed] [Google Scholar]
- 9.Anders H.J., Banas B., Schlöndorff D. Signaling danger: Toll-like receptors and their potential roles in kidney disease. J. Am. Soc. Nephrol. 2004;15:854–867. doi: 10.1097/01.ASN.0000121781.89599.16. [DOI] [PubMed] [Google Scholar]
- 10.Kawai T., Akira S. Signaling to NF-kappaB by Toll-like receptors. Trends Mol. Med. 2007;13:460–469. doi: 10.1016/j.molmed.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Morrell E.D., Kellum J.A., Pastor-Soler N.M., Hallows K.R. Septic acute kidney injury: Molecular mechanisms and the importance of stratification and targeting therapy. Crit. Care. 2014;18:501. doi: 10.1186/s13054-014-0501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei Q. Novel strategy for septic acute kidney injury rescue: Maintenance of the tubular integrity. Kidney Int. 2020;97:847–849. doi: 10.1016/j.kint.2019.12.024. [DOI] [PubMed] [Google Scholar]
- 13.Nakano D., Kitada K., Wan N., Zhang Y., Wiig H., Wararat K., Yanagita M., Lee S., Jia L., Titze J.M., et al. Lipopolysaccharide induces filtrate leakage from renal tubular lumina into the interstitial space via a proximal tubular Toll-like receptor 4-dependent pathway and limits sensitivity to fluid therapy in mice. Kidney Int. 2020;97:904–912. doi: 10.1016/j.kint.2019.11.024. [DOI] [PubMed] [Google Scholar]
- 14.Kashani K., Cheungpasitporn W., Ronco C. Biomarkers of acute kidney injury: The pathway from discovery to clinical adoption. Clin. Chem. Lab. Med. 2017;55:1074–1089. doi: 10.1515/cclm-2016-0973. [DOI] [PubMed] [Google Scholar]
- 15.Klein S.J., Brandtner A.K., Lehner G.F., Ulmer H., Bagshaw S.M., Wiedermann C.J., Joannidis M. Biomarkers for prediction of renal replacement therapy in acute kidney injury: A systematic review and meta-analysis. Intensive Care Med. 2018;44:323–336. doi: 10.1007/s00134-018-5126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schrezenmeier E.V., Barasch J., Budde K., Westhoff T., Schmidt-Ott K.M. Biomarkers in acute kidney injury-pathophysiological basis and clinical performance. Acta Physiol. 2017;219:554–572. doi: 10.1111/apha.12764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teo S.H., Endre Z.H. Biomarkers in acute kidney injury (AKI) Best Pract. Res. Clin. Anaesthesiol. 2017;31:331–344. doi: 10.1016/j.bpa.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Izquierdo-Garcia J.L., Nin N., Cardinal-Fernandez P., Rojas Y., de Paula M., Granados R., Martínez-Caro L., Ruíz-Cabello J., Lorente J.A. Identification of novel metabolomic biomarkers in an experimental model of septic acute kidney injury. Am. J. Physiol. Renal Physiol. 2019;316:F54–F62. doi: 10.1152/ajprenal.00315.2018. [DOI] [PubMed] [Google Scholar]
- 19.Chebotareva N., Bobkova I., Shilov E. Heat shock proteins and kidney disease: Perspectives of HSP therapy. Cell Stress Chaperones. 2017;22:319–343. doi: 10.1007/s12192-017-0790-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morales-Buenrostro L.E., Salas-Nolasco O.I., Barrera-Chimal J., Casas-Aparicio G., Irizar-Santana S., Pérez-Villalva R., Bobadilla N.A. Hsp72 is a novel biomarker to predict acute kidney injury in critically ill patients. PLoS ONE. 2014;9:e109407. doi: 10.1371/journal.pone.0109407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dozmorov M.G., Giles C.B., Koelsch K.A., Wren J.D. Systematic classification of non-coding RNAs by epigenomic similarity. BMC Bioinform. 2013;14:S2. doi: 10.1186/1471-2105-14-S14-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fan P.C., Chen C.C., Chen Y.C., Chang Y.S., Chu P.H. MicroRNAs in acute kidney injury. Hum. Genom. 2016;10:29. doi: 10.1186/s40246-016-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giza D.E., Fuentes-Mattei E., Bullock M.D., Tudor S., Goblirsch M.J., Fabbri M., Lupu F., Yeung S.J., Vasilescu C., Calin G.A. Cellular and viral microRNAs in sepsis: Mechanisms of action and clinical applications. Cell Death Differ. 2016;23:1906–1918. doi: 10.1038/cdd.2016.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benz F., Roy S., Trautwein C., Roderburg C., Luedde T. Circulating MicroRNAs as Biomarkers for Sepsis. Int. J. Mol. Sci. 2016;17:78. doi: 10.3390/ijms17010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin Z., Liu Z., Wang X., Qiu C., Zheng S. MiR-21-3p Plays a Crucial Role in Metabolism Alteration of Renal Tubular Epithelial Cells during Sepsis Associated Acute Kidney Injury via AKT/CDK2-FOXO1 Pathway. Biomed. Res. Int. 2019;2019:2821731. doi: 10.1155/2019/2821731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ge Q.M., Huang C.M., Zhu X.Y., Bian F., Pan S.M. Differentially expressed miRNAs in sepsis-induced acute kidney injury target oxidative stress and mitochondrial dysfunction pathways. PLoS ONE. 2017;12:e0173292. doi: 10.1371/journal.pone.0173292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ishimoto Y., Inagi R. Mitochondria: A therapeutic target in acute kidney injury. Nephrol. Dial. Transplant. 2016;31:1062–1069. doi: 10.1093/ndt/gfv317. [DOI] [PubMed] [Google Scholar]
- 28.Shen Y., Yu J., Jing Y., Zhang J. MiR-106a aggravates sepsis-induced acute kidney injury by targeting THBS2 in mice model. Acta Cir. Bras. 2019;34:e201900602. doi: 10.1590/s0102-865020190060000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taber S.S., Pasko D.A. The epidemiology of drug-induced disorders: The kidney. Expert Opin. Drug Saf. 2008;7:679–690. doi: 10.1517/14740330802410462. [DOI] [PubMed] [Google Scholar]
- 30.Rhodes A., Evans L.E., Alhazzani W., Levy M.M., Antonelli M., Ferrer R., Kumar A., Sevransky J.E., Sprung C.L., Nunnally M.E., et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 31.Wilhelm-Leen E., Montez-Rath M.E., Chertow G. Estimating the Risk of Radiocontrast-Associated Nephropathy. J. Am. Soc. Nephrol. 2017;28:653–659. doi: 10.1681/ASN.2016010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perazella M.A., Markowitz G.S. Drug-induced acute interstitial nephritis. Nat. Rev. Nephrol. 2010;6:461–470. doi: 10.1038/nrneph.2010.71. [DOI] [PubMed] [Google Scholar]
- 33.Petejova N., Martinek A., Zadrazil J., Teplan V. Acute toxic kidney injury. Ren. Fail. 2019;41:576–594. doi: 10.1080/0886022X.2019.1628780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arimura Y., Yano T., Hirano M., Sakamoto Y., Egashira N., Oishi R. Mitochondrial superoxide production contributes to vancomycin-induced renal tubular cell apoptosis. Free Radic. Biol. Med. 2012;52:1865–1873. doi: 10.1016/j.freeradbiomed.2012.02.038. [DOI] [PubMed] [Google Scholar]
- 35.Moledina D.G., Perazella M.A. PPIs and kidney disease: From AIN to CKD. J. Nephrol. 2016;29:611–616. doi: 10.1007/s40620-016-0309-2. [DOI] [PubMed] [Google Scholar]
- 36.Ong L.Z., Tambyah P.A., Lum L.H., Low Z.J., Cheng I., Murali T.M., Wan M.Q., Chua H.R. Aminoglycoside-associated acute kidney injury in elderly patients with and without shock. J. Antimicrob. Chemother. 2016;71:3250–3257. doi: 10.1093/jac/dkw296. [DOI] [PubMed] [Google Scholar]
- 37.Rybak M.J., Lomaestro B.M., Rotschafer J.C., Moellering R.C., Jr., Craig W.A., Billeter M., Dalovisio J.R., Levine D.P. Therapeutic monitoring of vancomycin in adults summary of consensus recommendations from the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2009;29:1275–1279. doi: 10.1592/phco.29.11.1275. [DOI] [PubMed] [Google Scholar]
- 38.Zamoner W., Prado I.R.S., Balbi A.L., Ponce D. Vancomycin dosing, monitoring and toxicity: Critical review of the clinical practice. Clin. Exp. Pharmacol. Physiol. 2019 doi: 10.1111/1440-1681.13066. [DOI] [PubMed] [Google Scholar]
- 39.Rybak M.J., Le J., Lodise T.P., Levine D.P., Bradley J.S., Liu C., Mueller B.A., Pai M.P., Wong-Beringer A., Rotschafer J.C., et al. Executive Summary: Therapeutic Monitoring of Vancomycin for Serious Methicillin-Resistant Staphylococcus aureus Infections: A Revised Consensus Guideline and Review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2020;40:363–367. doi: 10.1002/phar.2376. [DOI] [PubMed] [Google Scholar]
- 40.Chavada R., Ghosh N., Sandaradura I., Maley M., Van Hal S.J. Establishment of an AUC0-24 Threshold for Nephrotoxicity Is a Step towards Individualized Vancomycin Dosing for Methicillin-Resistant Staphylococcus aureus Bacteremia. Antimicrob. Agents Chemother. 2017;61 doi: 10.1128/AAC.02535-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hanrahan T.P., Kotapati C., Roberts M.J., Rowland J., Lipman J., Roberts J.A., Udy A. Factors associated with vancomycin nephrotoxicity in the critically ill. Anaesth. Intensive Care. 2015;43:594–599. doi: 10.1177/0310057X1504300507. [DOI] [PubMed] [Google Scholar]
- 42.Sakamoto Y., Yano T., Hanada Y., Takeshita A., Inagaki F., Masuda S., Matsunaga N., Koyanagi S., Ohdo S. Vancomycin induces reactive oxygen species-dependent apoptosis via mitochondrial cardiolipin peroxidation in renal tubular epithelial cells. Eur. J. Pharmacol. 2017;800:48–56. doi: 10.1016/j.ejphar.2017.02.025. [DOI] [PubMed] [Google Scholar]
- 43.Kane-Gill S.L., Ostermann M., Shi J., Joyce E.L., Kellum J.A. Evaluating Renal Stress Using Pharmacokinetic Urinary Biomarker Data in Critically Ill Patients Receiving Vancomycin and/or Piperacillin-Tazobactam: A Secondary Analysis of the Multicenter Sapphire Study. Drug Saf. 2019;42:1149–1155. doi: 10.1007/s40264-019-00846-x. [DOI] [PubMed] [Google Scholar]
- 44.Rhodes N.J., Prozialeck W.C., Lodise T.P., Venkatesan N., O’Donnell J.N., Pais G., Cluff C., Lamar P.C., Neely M.N., Gulati A., et al. Evaluation of Vancomycin Exposures Associated with Elevations in Novel Urinary Biomarkers of Acute Kidney Injury in Vancomycin-Treated Rats. Antimicrob. Agents Chemother. 2016;60:5742–5751. doi: 10.1128/AAC.00591-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pang H.M., Qin X.L., Liu T.T., Wei W.X., Cheng D.H., Lu H., Guo Q., Jing L. Urinary kidney injury molecule-1 and neutrophil gelatinase-associated lipocalin as early biomarkers for predicting vancomycin-associated acute kidney injury: A prospective study. Eur. Rev. Med. Pharmacol. Sci. 2017;21:4203–4213. [PubMed] [Google Scholar]
- 46.Pais G.M., Avedissian S.N., O′Donnell J.N., Rhodes N.J., Lodise T.P., Prozialeck W.C., Lamar P.C., Cluff C., Gulati A., Fitzgerald J.C., et al. Comparative Performance of Urinary Biomarkers for Vancomycin-Induced Kidney Injury According to Timeline of Injury. Antimicrob. Agents Chemother. 2019;63 doi: 10.1128/AAC.00079-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang J., Li H., Qiu S., Dong Z., Xiang X., Zhang D. MBD2 upregulates miR-301a-5p to induce kidney cell apoptosis during vancomycin-induced AKI. Cell Death Dis. 2017;8:e3120. doi: 10.1038/cddis.2017.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olbricht C.J., Fink M., Gutjahr E. Alterations in lysosomal enzymes of the proximal tubule in gentamicin nephrotoxicity. Kidney Int. 1991;39:639–646. doi: 10.1038/ki.1991.76. [DOI] [PubMed] [Google Scholar]
- 49.Gentamicin 40 mg/mL Injection. [(accessed on 7 July 2020)]; Available online: https://www.medicines.org.uk/emc/product/6531/smpc.
- 50.Romero F., Pérez M., Chávez M., Parra G., Durante P. Effect of uric acid on gentamicin-induced nephrotoxicity in rats-role of matrix metalloproteinases 2 and 9. Basic Clin. Pharmacol. Toxicol. 2009;105:416–424. doi: 10.1111/j.1742-7843.2009.00466.x. [DOI] [PubMed] [Google Scholar]
- 51.Martínez-Salgado C., López-Hernández F.J., López-Novoa J.M. Glomerular nephrotoxicity of aminoglycosides. Toxicol. Appl. Pharmacol. 2007;223:86–98. doi: 10.1016/j.taap.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 52.Udupa V., Prakash V. Gentamicin induced acute renal damage and its evaluation using urinary biomarkers in rats. Toxicol. Rep. 2018;6:91–99. doi: 10.1016/j.toxrep.2018.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Campos M.A.A., de Almeida L.A., Grossi M.F., Tagliati C.A. In vitro evaluation of biomarkers of nephrotoxicity through gene expression using gentamicin. J. Biochem. Mol. Toxicol. 2018;32:e22189. doi: 10.1002/jbt.22189. [DOI] [PubMed] [Google Scholar]
- 54.Kagawa T., Zarybnicky T., Omi T., Shirai Y., Toyokuni S., Oda S., Yokoi T. A scrutiny of circulating microRNA biomarkers for drug-induced tubular and glomerular injury in rats. Toxicology. 2019;415:26–36. doi: 10.1016/j.tox.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 55.Hori Y., Aoki N., Kuwahara S., Hosojima M., Kaseda R., Goto S., Iida T., De S., Kabasawa H., Kaneko R., et al. Megalin Blockade with Cilastatin Suppresses Drug-Induced Nephrotoxicity. J. Am. Soc. Nephrol. 2017;28:1783–1791. doi: 10.1681/ASN.2016060606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Balakumar P., Rohilla A., Thangathirupathi A. Gentamicin-induced nephrotoxicity: Do we have a promising therapeutic approach to blunt it? Pharmacol. Res. 2010;62:179–186. doi: 10.1016/j.phrs.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 57.Xu G., Mo L., Wu C., Shen X., Dong H., Yu L., Pan P., Pan K. The miR-15a-5p-XIST-CUL3 regulatory axis is important for sepsis-induced acute kidney injury. Ren. Fail. 2019;41:955–966. doi: 10.1080/0886022X.2019.1669460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lou Y., Huang Z. microRNA-15a-5p participates in sepsis by regulating the inflammatory response of macrophages and targeting TNIP2. Exp. Ther. Med. 2020;19:3060–3068. doi: 10.3892/etm.2020.8547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang Z.M., Wan X.H., Sang G.Y., Zhao J.D., Zhu Q.Y., Wang D.M. miR-15a-5p suppresses endometrial cancer cell growth via Wnt/β-catenin signaling pathway by inhibiting WNT3A. Eur. Rev. Med. Pharmacol. Sci. 2017;21:4810–4818. [PubMed] [Google Scholar]
- 60.Chen D., Wu D., Shao K., Ye B., Huang J., Gao Y. MiR-15a-5p negatively regulates cell survival and metastasis by targeting CXCL10 in chronic myeloid leukemia. Am. J. Transl. Res. 2017;9:4308–4316. [PMC free article] [PubMed] [Google Scholar]
- 61.Shang J., He Q., Chen Y., Yu D., Sun L., Cheng G., Liu D., Xiao J., Zhao Z. miR-15a-5p suppresses inflammation and fibrosis of peritoneal mesothelial cells induced by peritoneal dialysis via targeting VEGFA. J. Cell. Physiol. 2019;234:9746–9755. doi: 10.1002/jcp.27660. [DOI] [PubMed] [Google Scholar]
- 62.Caserta S., Kern F., Cohen J., Drage S., Newbury S.F., Llewelyn M.J. Circulating Plasma microRNAs can differentiate Human Sepsis and Systemic Inflammatory Response Syndrome (SIRS) Sci. Rep. 2016;6:28006. doi: 10.1038/srep28006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Caserta S., Mengozzi M., Kern F., Newbury S.F., Ghezzi P., Llewelyn M.J. Severity of Systemic Inflammatory Response Syndrome Affects the Blood Levels of Circulating Inflammatory-Relevant MicroRNAs. Front. Immunol. 2018;8:1977. doi: 10.3389/fimmu.2017.01977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zou Y.F., Wen D., Zhao Q., Shen P.Y., Shi H., Zhao Q., Chen Y.X., Zhang W. Urinary MicroRNA-30c-5p and MicroRNA-192-5p as potential biomarkers of ischemia-reperfusion-induced kidney injury. Exp. Biol. Med. 2017;242:657–667. doi: 10.1177/1535370216685005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cai H., Jiang Z., Yang X., Lin J., Cai Q., Li X. Circular RNA HIPK3 contributes to hyperglycemia and insulin homeostasis by sponging miR-192-5p and upregulating transcription factor forkhead box O1. Endocr. J. 2020;67:397–408. doi: 10.1507/endocrj.EJ19-0271. [DOI] [PubMed] [Google Scholar]
- 66.Baker M.A., Wang F., Liu Y., Kriegel A.J., Geurts A.M., Usa K., Xue H., Wang D., Kong Y., Liang M. MiR-192-5p in the Kidney Protects Against the Development of Hypertension. Hypertension. 2019;73:399–406. doi: 10.1161/HYPERTENSIONAHA.118.11875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen J., Wang J., Li H., Wang S., Xiang X., Zhang D. p53 activates miR-192-5p to mediate vancomycin induced AKI. Sci. Rep. 2016;6:38868. doi: 10.1038/srep38868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elton T.S., Selemon H., Elton S.M., Parinandi N.L. Regulation of the MIR155 host gene in physiological and pathological processes. Gene. 2013;532:1–12. doi: 10.1016/j.gene.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 69.Pfeiffer D., Roßmanith E., Lang I., Falkenhagen D. miR-146a, miR-146b, and miR-155 increase expression of IL-6 and IL-8 and support HSP10 in an In vitro sepsis model. PLoS ONE. 2017;12:e0179850. doi: 10.1371/journal.pone.0179850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alexander M., Hu R., Runtsch M.C., Kagele D.A., Mosbruger T.L., Tolmachova T., Seabra M.C., Round J.L., Ward D.M., O’Connell R.M. Exosome-delivered microRNAs modulate the inflammatory response to endotoxin. Nat. Commun. 2015;6:7321. doi: 10.1038/ncomms8321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Johnson B.J., Le T.T., Dobbin C.A., Banovic T., Howard C.B., Flores F.D.M.L., Vanags D., Naylor D.J., Hill G.R., Suhrbier A. Heat shock protein 10 inhibits lipopolysaccharide-induced inflammatory mediator production. J. Biol. Chem. 2005;280:4037–4047. doi: 10.1074/jbc.M411569200. [DOI] [PubMed] [Google Scholar]
- 72.Saikumar J., Hoffmann D., Kim T.M., Gonzalez V.R., Zhang Q., Goering P.L., Brown R.P., Bijol V., Park P.J., Waikar S.S., et al. Expression, circulation, and excretion profile of microRNA-21, -155, and -18a following acute kidney injury. Toxicol. Sci. 2012;129:256–267. doi: 10.1093/toxsci/kfs210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lu C., Chen B., Chen C., Li H., Wang D., Tan Y., Weng H. CircNr1h4 regulates the pathological process of renal injury in salt-sensitive hypertensive mice by targeting miR-155-5p. J. Cell. Mol. Med. 2020;24:1700–1712. doi: 10.1111/jcmm.14863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang Y., Zheng Z.J., Jia Y.J., Yang Y.L., Xue Y.M. Role of p53/miR-155-5p/sirt1 loop in renal tubular injury of diabetic kidney disease. J. Transl. Med. 2018;16:146. doi: 10.1186/s12967-018-1486-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Viñas J.L., Burger D., Zimpelmann J., Haneef R., Knoll W., Campbell P., Gutsol A., Carter A., Allan D.S., Burns K.D. Transfer of microRNA-486-5p from human endothelial colony forming cell-derived exosomes reduces ischemic kidney injury. Kidney Int. 2016;90:1238–1250. doi: 10.1016/j.kint.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 76.Xu J., Li R., Workeneh B., Dong Y., Wang X., Hu Z. Transcription factor FoxO1, the dominant mediator of muscle wasting in chronic kidney disease, is inhibited by microRNA-486. Kidney Int. 2012;82:401–411. doi: 10.1038/ki.2012.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Regmi A., Liu G., Zhong X., Hu S., Ma R., Gou L., Zafar M.I., Chen L. Evaluation of Serum microRNAs in Patients with Diabetic Kidney Disease: A Nested Case-Controlled Study and Bioinformatics Analysis. Med. Sci. Monit. 2019;25:1699–1708. doi: 10.12659/MSM.913265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chai X., Si H., Song J., Chong Y., Wang J., Zhao G. miR-486-5p Inhibits Inflammatory Response, Matrix Degradation and Apoptosis of Nucleus Pulposus Cells through Directly Targeting FOXO1 in Intervertebral Disc Degeneration. Cell. Physiol. Biochem. 2019;52:109–118. doi: 10.33594/000000008. [DOI] [PubMed] [Google Scholar]
- 79.Yuan X.P., Liu L.S., Chen C.B., Zhou J., Zheng Y.T., Wang X.P., Han M., Wang C.X. MicroRNA-423-5p facilitates hypoxia/reoxygenation-induced apoptosis in renal proximal tubular epithelial cells by targeting GSTM1 via endoplasmic reticulum stress. Oncotarget. 2017;8:82064–82077. doi: 10.18632/oncotarget.18289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang W., Gao J., Wang F. MiR-663a/MiR-423-5p are involved in the pathogenesis of lupus nephritis via modulating the activation of NF-κB by targeting TNIP2. Am. J. Transl. Res. 2017;9:3796–3803. [PMC free article] [PubMed] [Google Scholar]
- 81.Xu Y., Zhang J., Fan L., He X. miR-423-5p suppresses high-glucose-induced podocyte injury by targeting Nox4. Biochem. Biophys. Res. Commun. 2018;505:339–345. doi: 10.1016/j.bbrc.2018.09.067. [DOI] [PubMed] [Google Scholar]
- 82.Montomoli J., Donati A., Ince C. Acute Kidney Injury and Fluid Resuscitation in Septic Patients: Are We Protecting the Kidney? Nephron. 2019;143:170–173. doi: 10.1159/000501748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.O’Connor M.E., Prowle J.R. Fluid Overload. Crit. Care Clin. 2015;31:803–821. doi: 10.1016/j.ccc.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 84.Bellomo R., Kellum J.A., Ronco C., Wald R., Martensson J., Maiden M., Bagshaw S.M., Glassford N.J., Lankadeva Y., Vaara S.T., et al. Acute kidney injury in sepsis. Intensive Care Med. 2017;43:816–828. doi: 10.1007/s00134-017-4755-7. [DOI] [PubMed] [Google Scholar]
- 85.Gaudry S., Hajage D., Benichou N., Chaïbi K., Barbar S., Zarbock A., Lumlertgul N., Wald R., Bagshaw S.M., Srisawat N., et al. Delayed versus early initiation of renal replacement therapy for severe acute kidney injury: A systematic review and individual patient data meta-analysis of randomised clinical trials. Lancet. 2020;395:1506–1515. doi: 10.1016/S0140-6736(20)30531-6. [DOI] [PubMed] [Google Scholar]
- 86.Gaudry S., Hajage D., Schortgen F., Martin-Lefevre L., Pons B., Boulet E., Boyer A., Chevrel G., Lerolle N., Carpentier D., et al. Initiation Strategies for Renal-Replacement Therapy in the Intensive Care Unit. N. Engl. J. Med. 2016;375:122–133. doi: 10.1056/NEJMoa1603017. [DOI] [PubMed] [Google Scholar]
- 87.Karkar A., Ronco C. Prescription of CRRT: A pathway to optimize therapy. Ann. Intensive Care. 2020;10:32. doi: 10.1186/s13613-020-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Romagnoli S., Ricci Z., Ronco C. CRRT for sepsis-induced acute kidney injury. Curr. Opin. Crit. Care. 2018;24:483–492. doi: 10.1097/MCC.0000000000000544. [DOI] [PubMed] [Google Scholar]
- 89.Petejova N., Martinek A., Zahalkova J., Duricova J., Brozmannova H., Urbanek K., Grundmann M., Plasek J., Kacirova I. Vancomycin pharmacokinetics during high-volume continuous venovenous hemofiltration in critically ill septic patients. Biomed. Pap. Med. Faculty Univ. Palacky Olomouc Czech Repub. 2014;158:65–72. doi: 10.5507/bp.2012.092. [DOI] [PubMed] [Google Scholar]
- 90.Petejova N., Zahalkova J., Duricova J., Kacirova I., Brozmanova H., Urbanek K., Grundmann M., Martinek A. Gentamicin pharmacokinetics during continuous venovenous hemofiltration in critically ill septic patients. J. Chemother. 2012;24:107–112. doi: 10.1179/1120009X12Z.0000000006. [DOI] [PubMed] [Google Scholar]