Abstract
Kidney disease is a recognised risk factor for poor COVID-19 outcomes. Up to 30 June 2020, the UK Renal Registry (UKRR) collected data for 2,385 in-centre haemodialysis (ICHD) patients with COVID-19 in England and Wales. Overall unadjusted survival at 1 week after date of positive COVID-19 test was 87.5% (95% CI 86.1–88.8%); mortality increased with age, treatment vintage and there was borderline evidence of Asian ethnicity (HR 1.16, 95% CI 0.94–1.44) being associated with higher mortality. Compared to the general population, the relative risk of mortality for ICHD patients with COVID-19 was 45.4 and highest in younger adults. This retrospective cohort study based on UKRR data supports efforts to protect this vulnerable patient group.
Introduction
Coronaviruses (CoVs) are important pathogens in both humans and other vertebrate animals. In their reservoirs, CoV infections mainly affect respiratory, gastrointestinal, liver and central nervous systems [1]. At the end of 2019, a novel coronavirus called Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) started spreading across the world, causing a substantive number of cases. The new infectious disease was named COVID-19.
Current evidence shows that comorbidities, such as diabetes, hypertension and chronic kidney disease, and advanced age, are risk factors associated with worse outcomes from COVID-19 [2–4]. Children appear to be less affected than adults [5, 6], although coexisting kidney disease is reported among cases of children requiring intensive care support [7].
A recent meta-analysis reported that patients with COVID-19 developing acute kidney injury had significant 4-fold increased risk of death than patients without acute kidney injury [8].
In-centre haemodialysis (ICHD) patients regularly visit hospital for their treatment and are at especially high risk, not just because of older age, kidney failure and higher frequency of comorbidities [9], but also because COVID-19 is more likely to spread among hospitalised patients [10]. Moreover, patients with end-stage kidney disease have impairment in both innate and adaptive immunity in uremic state with decreased endocytosis, impaired maturation of monocytes and dendritic cells and malfunction of toll-like receptors [11].
The aim of this retrospective cohort study was to describe the features and mortality of patients on ICHD in England and Wales who had laboratory-confirmed COVID-19.
Methods
On behalf of the Renal Association, the UK Renal Registry (UKRR) collects patient data without consent under section 251 from the Health Research Authority’s Confidentiality Advisory Group. The data were pseudonymised prior to being analysed. This study was approved by the North East Newcastle & North Tyneside 1 Research Ethics Committee (16/NE/0042).
Data on ICHD patients with a positive laboratory test for SARS-CoV-2 were collected by the UK Renal Registry (UKRR) between 26 March and 30 June 2020 using weekly returns from renal centres in England and Wales about each patient (NHS number, date of birth and date of positive test). This collection included all paediatric cases and covered the 18-week period from 3 March to 30 June.
Data were checked and NHS numbers validated, with queries returned to the submitting centre. Using NHS number and date of birth, the Demographics Batch Service was used to retrieve sex, postcode and date of death, if applicable, for every patient in England and Wales. Postcode was used to determine the lower super output area and the associated Index of Multiple Deprivation (IMD) [12].
The Demographics Batch Service is only available in the UK for England and Wales–it was therefore not possible to include in this analysis data from Northern Ireland and Scotland. In addition, Scotland only reports aggregated COVID-19 data to the UK Renal Registry (UKRR).
For survival analysis, patients with a test date after 23 June 2020 were excluded to allow for at least 7 days of follow-up time. Survival time was calculated from the date of positive test to either the date of death or the end of follow-up (30 June). Kaplan Meier unadjusted survival and Cox proportional-hazards models were used to describe survival and hazard ratios. The assumption of proportional hazards was tested and met for the Cox model. To investigate if vintage (time on renal replacement treatment) was associated with an increased risk of mortality, vintage was divided into 3 categories: pre-2016, 2016–2018 and 2019 onwards.
Relative risk of death for English ICHD patients by age and English NHS region were calculated using the England ICHD population (end of 2018, the most recent data available), England mid-year 2018 general population (based on the 2011 census), England ICHD COVID-19 deaths (3 March to 30 June) and England general population COVID-19 deaths (3 March to 30 June).
Analyses were performed using SAS version 9.4. Alpha level of 0.05 and two-sided tests were used throughout.
Results
At the end of 2018, there were 21,509 adult ICHD patients alive in England and Wales. Between 3 March and 30 June 2020, 50 of 51 renal centres in England and 5 of 5 in Wales reported 2,385 adult ICHD patients with COVID-19 to the UKRR. London had the highest percentage of ICHD patients with COVID-19 (18.7%), with a range of 10.4–24.0% among its 7 renal centres. The remaining regions ranged from 3.5%–12.2% of ICHD patients with COVID-19. Three COVID-19 cases in ICHD patients aged <18 years were reported from a prevalent paediatric ICHD cohort of 116 (2.6%).
Among adults, most patients with COVID-19 were aged 60–79 years (50.8%) and 18.5% were aged ≥80 years. 62.6% were male, which was just above the proportion of ICHD male patients in the UK (61.8%). A similar proportion of patients that tested positive for SARS-CoV-2 were from ethnic minorities (15.2% were Asian and 11.6% were Black), compared to the overall ICHD population in England and Wales (14.7% Asian and 11.9% Black, respectively) (Table 1).
Table 1. Demographic comparison between adult patients on ICHD in England and Wales at the end of 2018 and adult patients on ICHD in England and Wales with COVID-19 from 3 March to 23 June 2020.
| Variable | ICHD adults end 2018 (n = 21,509)a | ICHD adults with COVID-19b (n = 2,385)c |
|---|---|---|
| Age, y | ||
| Median (IQR) | 67 (55–77) | 68 (55–77) |
| 18–39 (%) | 7 | 5 |
| 40–59 (%) | 27 | 26 |
| 60–79 (%) | 48 | 51 |
| ≥80 (%) | 18 | 18 |
| Male (%) | 62 | 63 |
| Ethnicity (%) | ||
| White | 69 | 70 |
| Asian | 15 | 15 |
| Black | 12 | 12 |
| Other | 4 | 3 |
| Most deprived quintile (%) | 30 | 31 |
ICHD, in-centre haemodialysis
aPercentages exclude missing data: there were 3% of patients with missing ethnicity and <1% with missing deprivation.
bFor UK renal centres that submitted patients with COVID-19 to the UKRR.
cPercentages exclude missing data: there were 3% with missing ethnicity and 1% with missing deprivation.
dExcluded 3 patients aged <18 and 9 patients without at least 1 week follow-up.
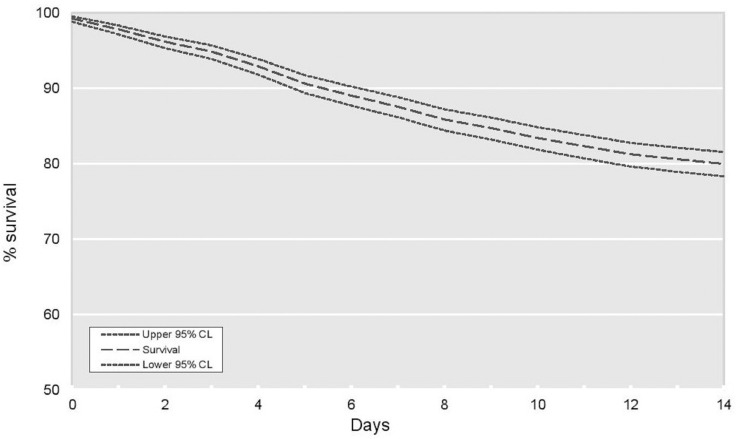
Survival (unadjusted) at 1 week from the date of a positive SARS-CoV-2 test was 87.5% (95% CI 86.1–88.8%) and 80.0% at 2 weeks (95% CI 78.3–81.5%) (Fig 1).
Fig 1. Kaplan Meier unadjusted survival for Sars-CoV-2 positive patients—2-week survival.
There were no deaths in children. Patients on ICHD with COVID-19 aged ≥80 years had a mortality risk of about 4.2 times that of those aged 18–59 years (Table 2). There was weak evidence of males with COVID-19 on ICHD doing worse than females (HR 1.19, 95% CI 1.01–1.40). Asian patients on ICHD with COVID-19 had a borderline 16% higher mortality risk than White patients, with no difference seen between Black and White patients. Deprivation was not associated with mortality on ICHD and no interactions were observed. Patients on renal replacement treatment for more than 5 years had a 42% higher mortality risk compared to patients who started dialysis during the last year.
Table 2. Multivariable analysis of time to death amongst ICHD adult patients in England and Wales with COVID-19 positive test results, 3 March to 30 June 2020.
| Variable | No. of patients | No. of deaths | Hazard ratio | 95% CI |
|---|---|---|---|---|
| Age, y | ||||
| 18–59 | 718 | 86 | 1.00 | |
| 60–79 | 1,190 | 340 | 2.57 | 2.03–3.26 |
| ≥80 | 428 | 187 | 4.24 | 3.28–5.49 |
| Sex | ||||
| Male | 1,461 | 398 | 1.19 | 1.01–1.40 |
| Female | 875 | 215 | 1.00 | |
| Ethnicity | ||||
| White | 1,638 | 424 | 1.00 | |
| Asian | 353 | 107 | 1.16 | 0.94–1.44 |
| Black | 277 | 60 | 0.86 | 0.65–1.14 |
| Other | 68 | 22 | 1.36 | 0.89–2.10 |
| Vintage | ||||
| <2016 | 887 | 276 | 1.42 | 1.15–1.75 |
| 2016–18 | 788 | 196 | 1.12 | 0.90–1.39 |
| ≥2019 | 661 | 141 | 1.00 |
aAll variables in the table were mutually adjusted for each other.
bPatients with missing ethnicity data were excluded n = 49.
Compared to the general population in England with COVID-19, the relative risk of death in English ICHD patients with COVID-19 was 45.4 (95% CI 41.9–49.1), and decreased with age from a peak in the 20–39 years age group to 9.8 times the risk of death in the general population at ≥80 years (Table 3), with a high interregional variability.
Table 3. Relative risk of death for ICHD patients with COVID-19 by age group and NHS region in England.
| Variable | England COVID-19 death rate per 10,000a | ICHD COVID-19 death rate per 10,000b | Relative risk | |
|---|---|---|---|---|
| ICHD/England COVID-19 death rates | 95% CI | |||
| Age, y | ||||
| 20–39 | 0.1 | 60.5 | 432 | 213.4–873 |
| 40–59 | 1.5 | 143.4 | 94.1 | 75.1–118 |
| 60–79 | 10.5 | 346.9 | 33.1 | 29.7–36.9 |
| ≥80 | 55.7 | 548.5 | 9.8 | 8.5–11.3 |
| Region | ||||
| East of England | 5.4 | 253.2 | 46.7 | 33.5–65.2 |
| London | 6.9 | 433.3 | 63.2 | 55.8–71.7 |
| Midlands | 5.4 | 293.7 | 54.6 | 45.7–65.2 |
| North East & Yorkshire | 5.2 | 267.7 | 51.5 | 40.9–65 |
| North West | 6.5 | 223.7 | 34.5 | 26.1–45.8 |
| South East | 3.7 | 276.5 | 73.9 | 57.3–95.2 |
| South West | 2.3 | 130.6 | 57.7 | 36.8–90.5 |
ICHD, in-centre haemodialysis
aNumber of deaths recorded 3 March to 30 June 2020 in England divided by the England mid-2018 population estimate.
bNumber of deaths recorded 3 March to 30 June 2020 in the English ICHD population divided by the end-2018 prevalent English ICHD population.
Discussion
The relative risk of death associated with COVID-19 among ICHD patients was much higher than that of the general population in England, especially among those of younger age. So far, and in contrast to the adult population, no deaths have been reported in paediatric patients aged <18 years. There was borderline evidence both for males with COVID-19 on ICHD doing worse than females and Asian patients having a 16% higher mortality than White patients.
As observed in other countries, to now, most deaths in the UK have been in people aged ≥50 years, with 55% of these males [13]. Data from the UK Intensive Care National Audit and Research Centre, indicate that among patients with COVID-19 admitted to intensive care, 1.7% had a history of kidney replacement therapy, 70.3% were male and there was an over-representation of those of Asian and Black ethnicities [14], similar to what we report for the ICHD population.
ICHD increases the risk of transmission of infection among patients and the high relative risk of death among younger individuals with COVID-19 on ICHD highlights their extreme vulnerability.
Despite level of deprivation correlating to the percentage of ICHD patients with COVID-19, deprivation was not a major predictor of mortality from COVID-19 on ICHD.
Previous studies have demonstrated the effects of length of time spent on dialysis treatment (vintage) on mortality, concluding that prolonged dialysis increases the mortality risk of patients receiving haemodialysis [15, 16]. A few studies have also shown the specific association between length of time on dialysis and higher risk for infection-related mortality [17, 18].
Moreover, a recent retrospective cohort study in a single centre in Spain analysed the clinical course and outcomes of 36 maintenance haemodialysis patients hospitalised with COVID-19 during the period March to April 2020. The authors concluded that none of the classical cardiovascular risk factors in the general population were associated with higher mortality, and that compared to survivors, non-survivors had significantly longer dialysis vintages [19]. In line with these results, in our study we found a positive association between treatment vintage and survival of ICHD patients with COVID-19.
To better understand the potentially higher mortality from COVID-19 seen for the Asian group, but not in the Black group, other factors such as comorbidities and their effect on survival of COVID-19 patients should be investigated. People of Asian origin are the UK’s largest ethnic minority in several cities [20] and type 2 diabetes is up to 6 times more common in Asian than White people [20, 21], which translates to a higher prevalence of diabetes as a cause of requiring ICHD [22].
Although the multivariable analysis was controlled for important factors related to the outcomes, the possibility of residual confounding from unmeasured variables cannot be excluded. We were unable to adjust for comorbidities and/or biochemical data for which both factors detailed comparison data for the general population were not available at the time of our analysis.
Moreover, we could not compare to other treatment modalities, such as peritoneal dialysis or transplantation, because reporting of COVID-19 in these populations is currently unreliable but may be better investigated in future thanks to development of further linkage of UKRR dataset to the national test result data. Data on mortality in ICHD patients as a result of causes not directly related to COVID-19 were not available, but in the future will explain the real burden of mortality associated with COVID-19 among ICHD patients in the UK.
Conclusions
Despite some limitations, results of this study show the extremely high relative mortality of COVID-19 patients on ICHD and are important to support collective efforts to minimise risk of transmission in this very vulnerable patient group.
Acknowledgments
We thank staff at all adult and paediatric renal centres in the UK who submit data to the UKRR and who care for kidney patients affected by COVID-19. We are also grateful to the Renal Association COVID-19 National Renal Data Coordinating Group for their guidance on this analysis: Paul Cockwell, Ron Cullen, Rachel Gair, Daniel Gale, Matt Graham-Brown, Thomas Hiemstra, Toby Humphrey, Carol Inward, Rachel Johnson, Graham Lipkin, Fiona Loud, Stephen Marks, Lisa Mumford, Matthew Robb, Adnan Sharif, Neil Sheerin, Laurie Tomlinson and Charlie Tomson.
Data Availability
The data underlying the results are available from the UK RENAL registry (contact ukrr-research@renalregistry.nhs.uk) for researchers who meet the criteria for access to confidential data.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Xu J, Zhao S, Teng T, Abdalla AE, Zhu W, Xie L, et al. Systematic comparison of two animal to human transmitted human coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses. 2020; 12(2): 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan J. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID 2019) Outbreak in China: Summary of a Report of 72,314 Cases from the Chinese Centre for Disease Control and Prevention. JAMA. 2020; 323(13): 1239–1242. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 3.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395(10229): 1054 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. March 2020. 10.1002/jmv.25757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ludvigsson JF. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. Mar 2020. 10.1111/apa.15270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR. Are children less susceptible to COVID-19? J. Microbiol. Immunol. February 2020. 10.1016/j.jmii.2020.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, et al. SARS-CoV-2 infection in children. N. Engl. J. Med. April 2020. 10.1056/NEJMc2005073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali H, Daoud A, Mohamed MM, Salim SA, Lenar Yessayan L, Baharani J, et al. Survival rate in acute kidney injury superimposed COVID-19 patients: a systematic review and meta-analysis. Ren. Fail. 2020; 42(1): 393–7. 10.1080/0886022X.2020.1756323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with Acute Respiratory Distress Syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Inter. Med. May 2020. 10.1016/j.kint.2020.0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naicker S, Yang CW, Hwang SJ, Liu BC, Chen JH, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. May 2020. 10.1016/j.kint.2020.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salim AS, Akula YV, Noszály NB, Afshan S, Agarwal M, Fülöp T. Potential role of plasmapheresis in severe cytomegalovirus infection with ongoing immunomediated hemolysis and low complement level. J Renal Inj Prev. 2017; 7(3): 206–10. [Google Scholar]
- 12.Noble M, Wright G, Smith G, Dibben C. Measuring multiple deprivation at the small-area level. Environ Plann A. 2006; 38: 169–85. [Google Scholar]
- 13.Office for National Statistics. Weekly provisional figures on deaths registered in the UK. 2020. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/weeklyprovisionalfiguresondeathsregisteredinenglandandwales [Accessed 16 July 2020].
- 14.Intensive Care National Audit and Research Centre. ICNARC Case Mix Programme Database 2020. Available from: https://www.icnarc.org/Our-Audit/Latest-News/2020/04/10/Report-On-3883-Patients-Critically-Ill-With-Covid-19 [Accessed 16 July 2020]. [DOI] [PMC free article] [PubMed]
- 15.Chertow GM, Johansen KL, Lew N, Lazarus M, Lawrie EG. Vintage, nutritional status, and survival in hemodialysis patients. Kidney Int. 2000; 57: 1176–1181. 10.1046/j.1523-1755.2000.00945.x [DOI] [PubMed] [Google Scholar]
- 16.Iseki K, Tozawa M, Takishita S. Effect of the duration of dialysis on survival in a cohort of chronic haemodialysis patients. Nephrol Dial Transplant. 2003; 18: 782–787. 10.1093/ndt/gfg145 [DOI] [PubMed] [Google Scholar]
- 17.Sumida K, Yamagata K, Iseki K, Tsubakihara Y. Different impact of hemodialysis vintage on cause-specific mortality in long-term hemodialysis patients, Nephrol Dial Transplant. 2016; 31(2): 298–305. 10.1093/ndt/gfv402 [DOI] [PubMed] [Google Scholar]
- 18.Allon M, Depner TA, Radeva M, Bailey J, Beddhu S, Butterly D, et al. Impact of dialysis dose and membrane on infection-related hospitalization and death: Results of the HEMO Study. J Am Soc Nephrol. 2003; 14: 1863–1870. 10.1097/01.asn.0000074237.78764.d1 [DOI] [PubMed] [Google Scholar]
- 19.Goicoechea M, Sánchez Cámara LA, Nicolás Macías N, Munoz de Morales A, Gonzalez Rojas A, Bascunana A, et al. COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int. 2020; 98(1): 27–34. 10.1016/j.kint.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dixon AN, Raymond NT, Mughal S., Rahim A, O’ Hare JP, Kumar S, et al. Prevalence of microalbuminuria and hypertension in South Asians and white Europeans with type 2 diabetes: a report from the United Kingdom Asian Diabetes Study (UKADS). Diabetes Vasc. Dis. Res. 2006; 3(1): 22–25. [DOI] [PubMed] [Google Scholar]
- 21.Mather HM, Chaturvedi N, Kehely AM. Comparison of prevalence and risk factors for microalbuminuria in South Asians and Europeans with Type 2 diabetes mellitus. Diabet. Med. 2018; 15(8): 672–677. [DOI] [PubMed] [Google Scholar]
- 22.Udayaraj U, Pruthi R, Casula A, Roderick P. UK Renal Registry 16th Annual Report: Chapter 6 Demographics and outcomes of patients from different ethnic groups on renal replacement therapy in the UK. Nephron Clin Pract. 2013; 125: 111–125. 10.1159/000360025 [DOI] [PubMed] [Google Scholar]